Lichen scrofulosorum is the most common tuberculid and its incidence in India is 2.38%. Tuberculosis is responsible for 77% of cases of phlyctenular keratoconjunctivitis (PKC). Both lichen scrofulosorum and PKC represent delayed hypersensitivity responses to Mycobacterium tuberculosis in skin and eyes, respectively. Previously PKC had been described in patients with underlying lichen scrofulosorum, papulonecrotic tuberculids, and in a single case of lupus vulgaris, with primary focus being pulmonary tuberculosis.[1,2,3,4] To the best of our knowledge, ocular examination (through dermoscope) has not been described in these cases, while dermoscopy of lichen scrofulosorum have been described in 2 cases only.[5] Our case is demonstrating this rare association along with their dermoscopy and ocular findings.
Ten-year-old girl complained of redness, watering, and photophobia in both eyes and multiple asymptomatic lesions on the trunk for past 1 week and 2 weeks, respectively. She gave history of weight loss, poor appetite, evening rise of temperature for past 2 months. The lesions were multiple, discrete to loosely aggregated at places, skin-colored to slightly erythematous pinhead-sized papules with fine white scaling, present on trunk and upper limbs [Figure 1] long with upper deep cervical lymphadenopathy. Examination by Ophthalmologist revealed bilateral conjunctival congestion along with phlycten at the 7o'clock limbus in the right eye. Rest of the systemic examination was normal.
Figure 1.

Clinical image of lichen scrofulosorum: multiple, discrete as well as loosely aggregated, skin-colored to slightly erythematous pinhead-sized papules with fine white scaling
Dermoscopy [AM7013MZTS (4S) Dino-Lite Premier, AnMo corporation, Taiwan] showed follicular and extrafollicular lesions with central cluster of brown clods along with halo of pallor with telangiectasias and marginal rim of white fine scales [Figure 2]. On eye dermoscopy, phlycten was seen at the right limbus as a structureless white area surrounded by dilated irregular conjunctival vessels of varying widths [Figure 3].
Figure 2.
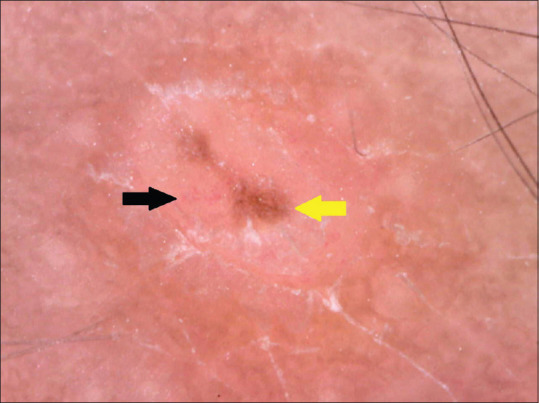
Dermoscopy of papules on back shows follicular as well as extrafollicular lesions with central cluster of brown clods (yellow arrow) along with halo of pallor with telangiectasias (black arrow) and rim of fine white scales (170× magnification, Polarized mode)
Figure 3.
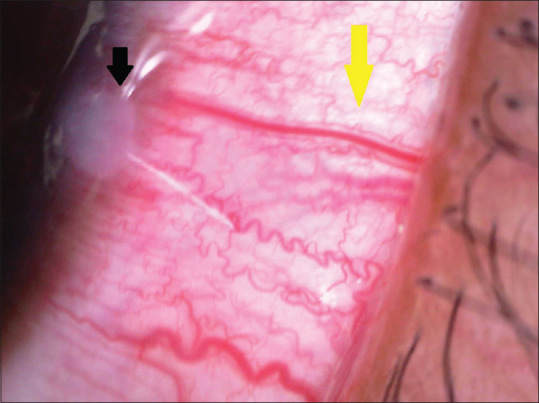
Eye dermoscopy reveals phlycten at 7o'clock right limbus as a structureless white area (black arrow) surrounded by dilated irregular conjunctival vessels (yellow arrow) of varying widths (70× magnification, Polarized mode)
Mantoux test showed ulceration and induration (20 × 20 mm). FNAC from the lymph nodes showed tubercular lymphadenitis and Ziehl-Neelsen stain was positive for acid fast bacilli. Skin biopsy from a papule on the back showed hyperkeratosis and perifollicular giant cell granulomas [Figure 4]. Chest X-ray did not reveal any abnormality. Based on above findings, we diagnosed lichen scrofulosorum secondary to tubercular lymphadenitis with PKC. Skin lesions responded within 1 month of the institution of ATT and phlycten responded to topical steroid eye drops.
Figure 4.
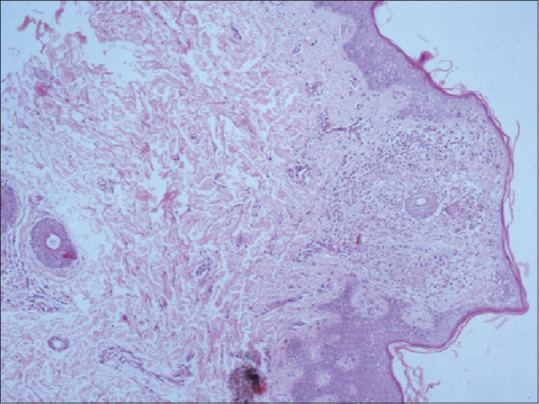
Skin biopsy from a papule on the back showed hyperkeratosis and perifollicular giant cell granulomas (400× magnification, H and E stain)
Lichen scrofulosorum is the most common tuberculid in Indian children. PKC has been described previously in conjunction with papulonecrotic tuberculids, lichen scrofulosorum, scrofuloderma and lupus vulgaris [Table 1].[1,2,3,4] The primary focus being pulmonary tuberculosis or tubercular lymphadenitis [Table 1].[1,2,3,4] Jassi et al. had reported pale round monomorphic grouped perifollicular large dots with central black follicular opening topped with a crust and marginal rim of fine white scaling and marginal hyperpigmentation (in one of the case) as dermoscopic findings of lichen scrofulosorum; however, we noticed follicular as well as extrafollicular lesions with central cluster of brown clods (instead of black follicular opening) and telangiectasia in addition to their findings.[5] Ocular findings of PKC on dermoscopy require further validation by more studies.
Table 1.
Various studies shows association of tuberculid with phlyctenular conjunctivitis, along with tuberculosis focus
| Study | Tuberculid (n)† | Phlyctenular conjunctivitis | Tuberculosis focus |
|---|---|---|---|
| Rauschkolb je[1] | Lichen scrofulosorum (11) | >50% | Pulmonary TB |
| Jordaan et al.[2] | Papulonecrotic tuberculid (8) | 37.5% | Pulmonary TB |
| Stein and Freiman[3] | Tuberculid (1) | present | Unknown |
| Singal et al.[4] | Lichen scrofulosorum (1) | present | Pulmonary TB and scrofuloderma |
†n - number of subjects
Lastly, PKC should be actively looked for, especially in the patients of cutaneous tuberculosis, as this association may be more common than described.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rauschkolb je. tuberculosis of the skin: A clinical report. Arch Derm Syphilol. 1934;29:398–407. [Google Scholar]
- 2.Jordaan HF, Schneider JW, Schaaf HS, Victor TS, Geiger DH, Van Helden PD, et al. Papulonecrotic tuberculid in children.A report of eight patients. Am J Dermatopathol. 1996;18:172–85. doi: 10.1097/00000372-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Stein H, Freiman I. Phlyctenular conjunctivitis in African children. Arch Dis Child. 1958;33:292–4. doi: 10.1136/adc.33.170.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singal A, Aggarwal P, Pandhi D, Rohatgi J. Cutaneous tuberculosis and phlyctenular keratoconjunctivitis: A forgotten association. Indian J Dermatol Venereol Leprol. 2006;72:290–2. doi: 10.4103/0378-6323.26726. [DOI] [PubMed] [Google Scholar]
- 5.Jassi R, Yadav A, Chander R. Dermoscopy of Lichen Scrofulosorum. Indian Dermatol Online J. 2020;11:876–7. doi: 10.4103/idoj.IDOJ_191_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


