Abstract
Background:
Regulatory analyses of air pollution policies require the use of concentration–response functions and underlying health data to estimate the mortality and morbidity effects, as well as the resulting benefits, associated with policy-related changes in fine particulate matter ()]. Common practice by U.S. federal agencies involves using underlying health data and concentration–response functions that are not differentiated by racial/ethnic group.
Objectives:
We aim to explore the policy implications of using race/ethnicity-specific concentration–response functions and mortality data in comparison to standard approaches when estimating the impact of air pollution on non-White racial/ethnic subgroups.
Methods:
Using new estimates from the epidemiological literature on race/ethnicity-specific concentration–response functions paired with race/ethnicity-specific mortality rates, we estimated the mortality impacts of air pollution from all sources from a uniform increase in concentrations and from the regulations imposed by the Mercury Air Toxics Standards.
Results:
Use of race/ethnicity-specific information increased premature mortality estimates in older populations by 9% and among older Black Americans by 150% for all-source pollution exposure. Under a uniform degradation of air quality and race/ethnicity-specific information, older Black Americans were found to have approximately 3 times higher mortality relative to White Americans, which is obscured under a non–race/ethnicity-specific modeling approach. Standard approaches of using non–racial/ethnic specific information underestimate the benefits of the Mercury Air Toxics Standards to older Black Americans by almost 60% and overestimate the benefits to older White Americans by 14% relative to using a race/ethnicity-specific modeling approach.
Discussion:
Policy analyses incorporating race/ethnicity-specific concentration–response functions and mortality data relative to nondifferentiated inputs underestimate the overall magnitude of mortality burden and the disparity in impacts on older Black American populations. Based on our results, we recommend that the best available race/ethnicity-specific inputs are used in regulatory assessments to understand and reduce environmental injustices. https://doi.org/10.1289/EHP9001
Introduction
Among the air pollutants regulated by the Clean Air Act of 1970 (CAA), prior studies find that fine particulate matter [particulate matter with an aerodynamic diameter of ()] is responsible for the largest share of estimated costs of air pollution (U.S. EPA 1999, 2011a; Muller et al. 2011). The bulk of costs are through premature deaths (U.S. EPA Agency 2011b); in 2011, an estimated 107,000 premature deaths in the United States were attributed to air pollution (Goodkind et al. 2019).
The U.S. Environmental Protection Agency (U.S. EPA) is required to carry out benefit–cost and regulatory impact analyses to assess the effects of the CAA and associated administrative rules (U.S. EPA 2012). Reductions in mortality are a major contributor to benefits of air pollution policies. Most analyses used by the U.S. EPA to quantify lowered mortality risks associated with reductions employ a log-linear concentration–response function (CRF) between exposure and mortality. Two such CRFs typically used are from the American Cancer Society (ACS) study (Krewski et al. 2009) and the Harvard Six Cities analysis (Lepeule et al. 2012). However, these studies evaluated populations composed of people of socioeconomic status (SES) higher than the national average, predominantly White populations in well-monitored urban areas (for example, Black Americans constitute only 4% of the population in ACS CPSII study) (Pope et al. 1995). Thus, these estimates provide limited information on the health effects of air pollution in rural areas, among racial/ethnic minorities, or in low-SES populations.
Recent evidence from a study of all Medicare beneficiaries (with 60,925,443 Americans) indicates that the impact of on mortality among older populations is 3 times higher for Black Americans than for White Americans, including at exposures below the current National Ambient Air Quality Standard (NAAQS) for (annual average ) (Di et al. 2017). Although multiple studies have demonstrated that people of color and other disadvantaged populations have disproportionately higher exposures to air pollution than White Americans (Hajat et al. 2015; Tessum et al. 2019), we incorporate and document the additional impact that higher baseline mortality rates and higher pollution susceptibility have on pollution-caused health outcomes across these racial/ethnic groups. Standard practice in most health risk assessments involves applying CRFs to all adult populations, assuming no differences in pollution-related risk of death across racial/ethnic groups and concentration levels and combined with population-weighted average mortality rates. We hypothesize that the use of CRFs and underlying health data that are not differentiated by racial/ethnic subgroup would lead to an underestimation of the health impacts of air pollution, especially for racial/ethnic minority communities.
This study contributes to the extant literature in several ways. First, we estimate air pollution deaths among older populations ( y of age) using the 2014 National Emissions Inventory (NEI), a comprehensive (economy-wide) inventory available for the United States (U.S. EPA 2016). Second, we capitalize on recent innovations in the epidemiological literature that report both nonlinear relationships between ambient concentrations and mortality risk faced by older individuals, as well as race/ethnicity-specific concentration–response functions (CRFs). Because this new epidemiological study relied on the Medicare population, we only estimate deaths for the relevant age groups (). Ours is the first study to use these new results in a national assessment of the health impact from among older populations. Furthermore, we employed baseline health data specific to subgroups of interest (specifically, the five largest racial/ethnic groups: White, Black American, Hispanic American, Asian American, and Native American). Third, partially motivated by increases in ambient concentrations between the years 2016 and 2018 (Clay and Muller 2019), we analyzed and quantify mortality impacts in older populations and associated costs from a simulated uniform -increase in and break these down by racial/ethnic group. Finally, we also explored the public health benefits of the Mercury and Air Toxics Standards (MATS). This aspect of the paper developed a “no-MATS” counterfactual, and it then assessed, on a county-level basis, the distribution of mortality risks and costs that MATS avoided.
Materials and Methods
-Attributable Premature Mortality
We first estimated premature mortality attributable to exposure. To do so, we employed the Air Pollution Emissions Experiments and Policy Analysis (APEEP) integrated assessment model [version 3 (AP3)] (Clay et al. 2019; Muller 2014). AP3 is an updated version of the second version of APEEP-AP2 (Holland et al. 2016; Jaramillo and Muller 2016). The model, run in MATLAB®, uses emissions of local air pollutants to estimate the ambient concentrations of , resulting exposures, mortality risks, and monetary costs. The model encompasses emissions of five pollutants: sulfur dioxide (), nitrogen oxides (), ammonia (), primary , and volatile organic compounds (VOC). All emissions of these pollutants reported by the U.S. EPA in the 2014 NEI released in the contiguous United States are included. AP3 differentiates emissions by source type and locations. It models nearly 700 individual point sources and attributes all remaining point source emissions reported by the U.S. EPA to the county in which the facility exists. The U.S. EPA reports ground-level, area source emissions (cars, trucks, trains, households, small businesses, and agriculture, among others) as aggregated county emissions. AP3 attributes these discharges to the county in which the U.S. EPA reports the release.
AP3 employs an air-quality model to link emissions to concentrations. Fundamentally, the model relies on Gaussian dispersion modeling. However, it employs simplified representations of the atmospheric chemical processes that link , , , and VOC emissions to ambient concentrations of secondary . The model uses rate constants along with a module applied in every receptor location which translates ambient predicted concentrations into ambient sulfate, ammonium nitrate, and ammonium. Each of these species are important constituents of total . The predictions of total ambient produced by AP3 have been evaluated against both monitoring data provided publicly by the U.S. EPA and predicted concentrations produced by chemical transport models in previous analyses (Gilmore et al. 2019). The comparison of predicted annual means from an earlier version of AP3 with ambient monitoring data revealed a correlation coefficient for total of about 0.60, which was on par with that from a chemical transport model included in the analysis.
AP3 is also equipped with detailed county-level vital statistics inclusive of population and mortality rate data for 19 different age groups and 5 different major racial/ethnic groups (Clay et al. 2019): Native Americans, Asian Americans, Black Americans, Hispanic Americans, and White Americans. We sourced the data on population and mortality rates for these five racial/ethnic groups from the U.S. Census Bureau and the Centers for Disease Control and Prevention (CDC) WONDER databases (https://wonder.cdc.gov/ Updated 22 December 2020; https://www.census.gov Updated 8 October 2021).
The CDC WONDER database classifies racial groups as follows: American Indian or Alaska Native, Asian or Pacific Islander, Black or African American, and White (corresponding to “Native Americans,” “Asian Americans,” “Black Americans,” and “White Americans,” respectively, in this paper). Furthermore, the database separates the results by Hispanic ethnicity. Thus, to create the non-Hispanic racial/ethnic groups, we chose the “non-Hispanic” designation for each of the four above-listed racial groups, and to classify “Hispanic Americans” as such, we used the “All Races” Hispanic or Latino classification. This approach created the five distinct racial/ethnic groups we present in this paper.
The U.S. Census Bureau’s classification of racial/ethnic groups (as described at https://www.census.gov/topics/population/race/about.html) are as follows: For non-Hispanic racial groups, we gathered data on populations of non-Hispanic “White alone,” “Black or African American alone,” “Asian alone,” and “American Indian and Alaska Native alone or in combination with other races.” For Hispanic or Latino ethnicities, the U.S. Census Bureau reports Hispanic populations, which can correspond to any of the races listed above. Given that the four racial groups described above were labeled “Non-Hispanic,” these five racial/ethnic categories are mutually exclusive.
We downloaded the 2014 data on county-level populations by age and racial/ethnic group from the Census (https://www2.census.gov/programs-surveys/popest/datasets/2010-2017/counties/asrh/cc-est2017-alldata.csv) and the 10-y average mortality for all causes of death at the county level, ending in 2014 from CDC WONDER. Table 1 reports the national average mortality rates by age and racial/ethnic group. Because we used publicly available data, we did not require informed consent protocols or internal review board or ethics approvals.
Table 1.
National baseline mortality rates 2005–2014, averages and variance.
| Racial/ethnic group | Age 65–74 y | Age 75–84 y | Age y |
|---|---|---|---|
| Native Americans | 0.021 (0.001) | 0.047 (0.004) | 0.109 (0.010) |
| Asian Americans | 0.009 (0.002) | 0.029 (0.007) | 0.091 (0.020) |
| Black Americans | 0.026 (0.002) | 0.056 (0.007) | 0.134 (0.017) |
| Hispanic Americans | 0.014 (0.002) | 0.037 (0.005) | 0.104 (0.015) |
| White Americans | 0.019 (0.000) | 0.049 (0.000) | 0.143 (0.000) |
Note: Data are from CDC WONDER, Compressed Mortality File 1999–2016 Series 20 No. 2U, 2016, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. The data reflect crude rates or the number of deaths per calendar year per 100,000 population [http://wonder.cdc.gov/cmf-icd10.html (accessed 22 June 2019)].
To estimate the premature mortality risk faced by individuals 65 y of age or older attributable to exposure to , AP3 uses a health impact function of the following form:
where equals premature deaths attributable to exposure for individuals 65 y of age or older, county (i), age cohort (a), at time (t); equals a statistically estimated coefficient from the epidemiological literature; equals population count for individuals 65 y of age or older, county (i), age cohort (a), at time (t); concentration, county (i), time (t); and equals baseline mortality rate for age cohort (a), county (i), time (t).
The AP3 model concludes by attributing a monetary value to mortality risk from by employing a Value of Statistical Life (VSL) approach (Viscusi and Aldy 2003). The VSL is the marginal rate of substitution between money (typically wage income) and mortality risk. It is not intended to reflect or capture the value of the prevention of certain death. It is a rate of exchange between money and small changes in risks of death. The VSL parameter used in AP3 is the U.S. EPA’s preferred value: about in 2014 U.S. dollars. The VSL is applied uniformly across persons of different incomes, ages, and racial/ethnic groups. We calculated per capita mortality costs by dividing the total mortality costs for each racial/ethnic group at the county level by the relevant population. We then mapped the county aggregate and per capita costs to demonstrate the geographic variability in pollution-related premature mortality impacts. Our maps divided the distribution of per capita costs into five classes, as defined by the Jenks classification method and portrayed in map legends. The highest class shows the price per capita for outlier counties and reflects the areas with the highest mortality costs per racial/ethnic group.
The focus of this analysis is to identify the influence of different CRFs and vital statistics on mortality estimates across different exposure levels and racial/ethnic groups. We used mortality CRFs from the recent cohort study of 60,925,443 Medicare beneficiaries across the United States followed over 13 y (2000 through 2012) (Di et al. 2017). The study used zip code annual average concentrations, predicted through the use of an artificial neural network that incorporated information such as satellite-based measurements, simulation outputs from a chemical transport model, land-use terms, and meteorological data. These were trained and validated against regulatory monitor data. The CRFs of the risk of death associated with a increase in were estimated using a two-pollutant Cox proportional-hazards model that controlled for ozone, sex, racial/ethnic group, Medicaid eligibility, 5-y categories of age at study entry, 15 zip code-level or county-level variables from various sources, and a regional dummy variable to account for compositional differences in across the United States.
From Di et al. (2017), we obtained two sets of estimates: a single linear () coefficient for the full cohort population, as well as race/ethnicity-specific subgroup () coefficients.
We coupled the use of these alternative CRF forms with different ways of including baseline mortality rates. In total, we considered the following four epidemiological strategies: the Di et al. (2017) linear, non–race/ethnicity-specific CRF with both population-weighted mortality rates and race/ethnicity-specific mortality rates, and the Di et al. (2017) race/ethnicity-specific linear CRFs with both population-weighted and race/ethnicity-specific mortality rates. All hazard ratios (HR) and their associated confidence intervals (CI) are listed in Table 2.
Table 2.
Concentration–response functions.
| Exposure | Racial/ethnic group | Hazard ratio (95% CI) | Reference |
|---|---|---|---|
| Linear across all levels | All | 1.06 (1.04, 1.08) | Krewski et al. 2009 |
| All | 1.073 (1.071, 1.075) | Di et al. 2017 | |
| White American | 1.063 (1.060, 1.065) | Di et al. 2017 | |
| Black American | 1.208 (1.199, 1.217) | Di et al. 2017 | |
| Asian American | 1.096 (1.075, 1.117) | Di et al. 2017 | |
| Hispanic American | 1.116 (1.100, 1.133) | Di et al. 2017 | |
| Native American | 1.100 (1.060, 1.140) | Di et al. 2017 |
Note: The reported hazard ratios are for mortality risk associated with increase in . CI, confidence interval.
Policy Scenario 1: Uniform Increase in Underlying Concentrations
Using the same model, CRFs, and data as in our analysis of premature mortality, we first modeled a scenario of air-quality degradation, in which all counties experience an increase of . To do so, we ran AP3 twice: first with the pollution baseline and once with an extra of pollution. The results are the difference in outcomes across the two scenarios. The average baseline concentration across counties (calculated at the population-weighted centroid of each county) is ; this scenario therefore represents an 18% change in air pollution on average, although given the variation in pollution across counties, the percentage increase can exceed 100%. The intent of this simulation is to isolate differences in modeling strategies across racial/ethnic groups and age groups. That is, by standardizing the change, we can clearly attribute differences in resulting mortality effects to the CRFs and vital statistics used.
Policy Scenario 2: MATS Abatement Technology
Our second scenario modeled the health effects of the MATS policy using AP3. Specifically, we used data on abatement technology adopted by generators in direct response to MATS policy. The U.S. Department of Energy’s Energy Information Administration Form 860 provides information at the power plant level on the first year in which the generators used MATS abatement technology for compliance with the policy. We used central engineering estimates of emissions reductions rates for the compliance technology (Kaminski 2003; U.S. EPA n.d.; Ake and Licata 2011) to infer what emissions of and would have been had firms not elected to use the technology.
For the MATS scenario, we employed only the race/ethnicity-specific mortality rates paired with both the race/ethnicity-nonspecific linear and the race/ethnicity-specific CRF from Di et al. (2017).
Results
-Attributable Premature Mortality
Total premature mortality attributable to exposure among people over the age of 65 y in 2014 across the United States ranged from 121,331 to 132,696 deaths (Table 3). Table 3 reports attributable mortality estimates for all racial/ethnic groups, using the six different CRF approaches discussed in the “Materials and Methods” section. The Di et al. (2017) linear CRF with mortality rates not differentiated by racial/ethnic group yielded an estimate of 121,331 deaths among persons over 65 y of age in 2014 (see Table 3, column 1).
Table 3.
Total estimated race/ethnicity-specific deaths among populations age 65 y and older in the United States using different concentration–response functions and baseline mortality rates.
| Race/ethnicity | Underlying mortality data | National share of older populations by racial/ethnic group, as a percentage of total population above 65 y of age | |||
|---|---|---|---|---|---|
| Population-weighted average | Race/ethnicity-specific | Population-weighted average | Race/ethnicity-specific | ||
| Native Americans | 850 (1%) | 632 (1%) | 1,136 (1%) | 846 (1%) | 1% |
| Asian Americans | 4,349 (4%) | 2,787 (2%) | 5,585 (4%) | 3,580 (3%) | 4% |
| Black Americans | 12,013 (10%) | 13,294 (11%) | 29,994 (23%) | 33,188 (25%) | 9% |
| Hispanic Americans | 7,600 (6%) | 6,011 (5%) | 11,581 (9%) | 9,161 (7%) | 8% |
| White Americans | 96,519 (80%) | 98,607 (81%) | 84,101 (64%) | 85,921 (65%) | 79% |
| All groups | 121,331 (100%) | 121,331 (100%) | 132,398 (100%) | 132,696 (100%) | 100% |
| Total costs (in 2014) | 1,059.1 | 1,059.1 | 1,155.7 | 1,158.3 | — |
| CRF employed | Linear | Linear | Race/ethnicity-specific | Race/ethnicity-specific | — |
We first examined the effect of imposing race/ethnicity-specific mortality rates relative to population-weighted average mortality rates. As Table 1 demonstrates, among people younger than 85 y, Black Americans have the highest mortality rates, and for those older than 85 y, White Americans have the highest mortality rates.
The use of race/ethnicity-specific mortality rates did not significantly affect the total number of deaths, but rather it distributed them differently across racial/ethnic groups by altering the race/ethnicity-specific distribution of premature mortality risk. Specifically, we found that using population-weighted average mortality rates underestimated the health effects of air quality on Black Americans by approximately 11%, regardless of the CRF function employed (comparing Table 3, column 1 to column 2; and column 3 to column 4). This approach also underestimated the health benefits of air-quality improvements on White Americans, although the effect was much smaller (2%), and it overestimated the impacts on other racial/ethnic groups.
Our next set of results demonstrated the effect of employing the race/ethnicity-specific linear CRFs (Table 3, columns 3 and 4) relative to linear, non–race/ethnicity-specific CRF (Table 3, columns 1 and 2). Using the race/ethnicity-specific CRF increased total deaths by 9% relative to the results under the linear CRF (comparing columns 1 to 3 and 2 to 4).
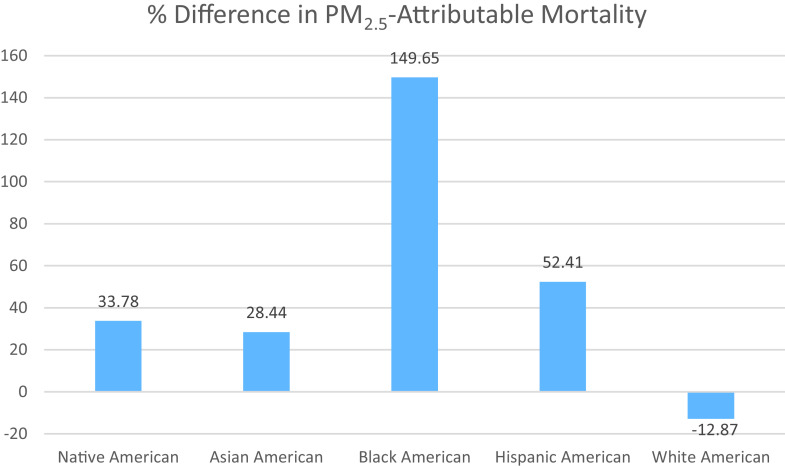
However, the difference across racial/ethnic groups was more pronounced. Figure 1 graphically shows how much the non–race/ethnicity-specific CRF from Di et al. (2017) misestimates the impacts across all racial/ethnic groups. The figure shows the percentage difference in mortality from using a race/ethnicity-specific CRF relative to the non–race/ethnicity-specific CRF. Using the race/ethnicity-specific linear CRFs resulted in significantly greater premature mortality for racial/ethnic minorities, with Black Americans having over 150% additional premature deaths than predicted using the non–subgroup-specific CRF. Similarly, Hispanic Americans had 52% additional premature deaths, and Native Americans and Asian Americans had approximately 30% additional premature deaths than predicted under the non–subgroup-specific CRF. However, White Americans had 13% fewer deaths under this approach.
Figure 1.
Percentage difference in premature mortality between the linear, non–race/ethnicity-specific Di et al. (2017) and the race/ethnicity-specific Di et al. (2017) CRFs. The figure represents the difference in -attributable mortality between using non–race/ethnicity-specific CRF and using race/ethnicity-specific CRFs. The baseline in the difference is non–racial/ethnic specific CRFs; thus the percentage represents how much higher the mortality estimate is when using a racial/ethnic-specific CRF. The relevant CRFs are from Di et al. (2017); see Table 2. Note: CRF, concentration–response function.
Further, under the race/ethnicity-specific CRF, the pollution-attributed premature mortality among older Black Americans accounted for as much as 25% of all deaths in populations over 65 y of age, although nationally, older Black Americans make up only 9% of the total population (this can be seen in Table 3, comparing the percentages in column 5 to the percentages in the other columns). In contrast, mortality was proportional to the population share for older White Americans in the scenarios without race/ethnicity-specific CRFs (see Table 3, columns 1–2), but this changed when we employed race/ethnicity-specific CRFs. As can be seen in Table 3, columns 3 and 4, the race/ethnicity-specific CRF for White Americans resulted in a mortality burden of only 65%, even though the population share of this group was roughly 80%.
Table 2 provides mortality risk HRs associated with a increase in (and corresponding 95% CIs) for the different CRFs. Table 4 presents the results from our analyses using the upper and lower bounds of the CRF CIs presented in Table 2.
Table 4.
Confidence intervals, deaths by racial/ethnic group for CRFs.
| Linear CRF point estimates | Race/ethnicity-specific linear CRF point estimates | |||||
|---|---|---|---|---|---|---|
| Race/ethnicity | Lower bound | Central | Upper bound | Lower bound | Central | Upper bound |
| Native Americans | 828 | 850 | 871 | 526 | 846 | 1,145 |
| Asian Americans | 4,238 | 4,349 | 4,459 | 2,858 | 3,580 | 4,271 |
| Black Americans | 11,708 | 12,013 | 12,316 | 32,016 | 33,188 | 34,340 |
| Hispanic Americans | 7,406 | 7,600 | 7,793 | 8,019 | 9,161 | 10,337 |
| White Americans | 94,048 | 96,519 | 98,973 | 82,061 | 85,921 | 88,465 |
| All racial/ethnic groups | 118,228 | 121,331 | 124,411 | 125,480 | 132,696 | 138,559 |
Some degree of overlap in CIs occurred in the case of Native Americans, given the large uncertainty around the race/ethnicity-specific CRF for this racial group. As shown in Table 4, the estimates for Native Americans had similar central estimates across the two CRFs (846 vs. 850), with the race/ethnicity-specific CRFs resulting in a CI of 526 to 1,145. All other racial/ethnic groups had clear differentiation between the results for the different CRFs employed.
We next estimated the cost of premature mortality in older populations by applying a uniform VSL to all premature deaths caused by pollution. Multiplying the total number of deaths across all racial/ethnic subgroups as listed in Table 3 by our VSL of approximately , we found that total mortality costs are between dollars (in 2014 U.S. dollars).
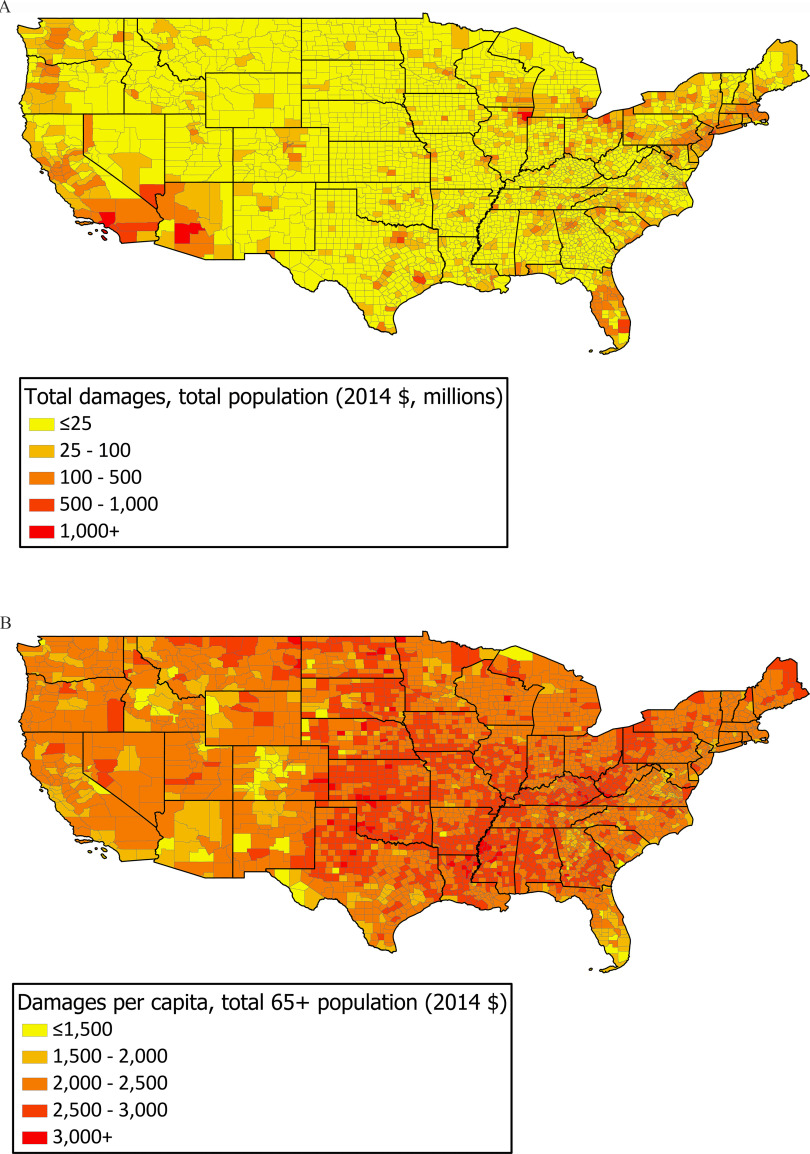
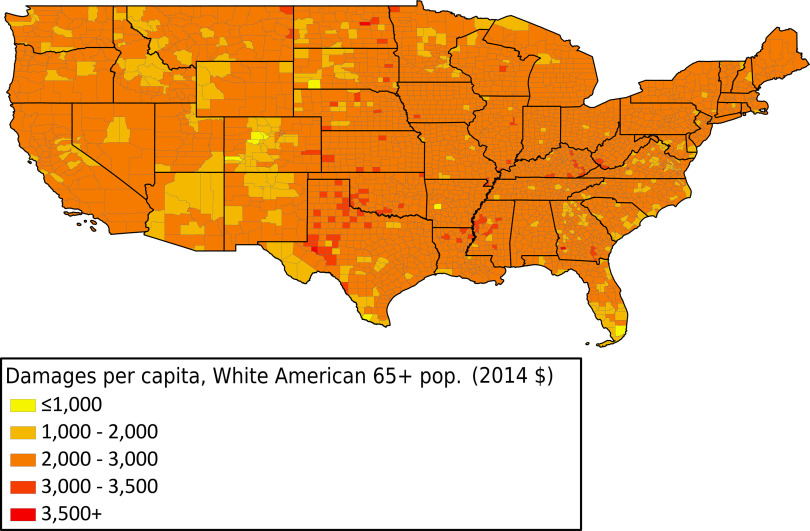
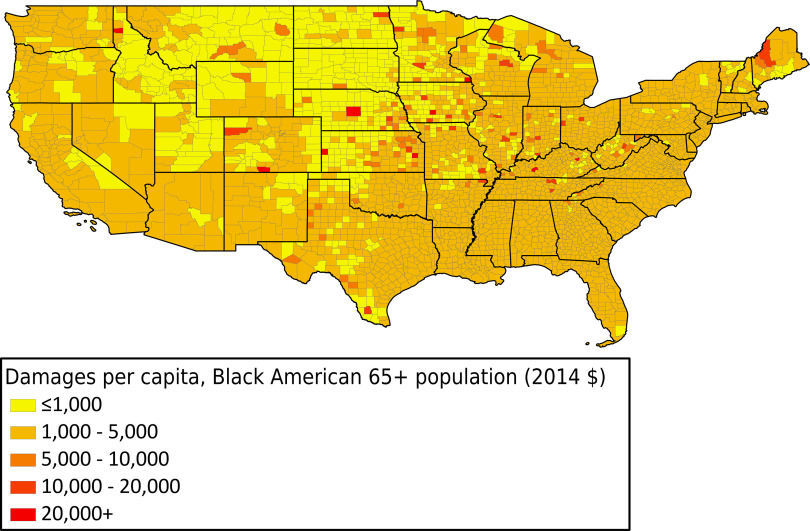
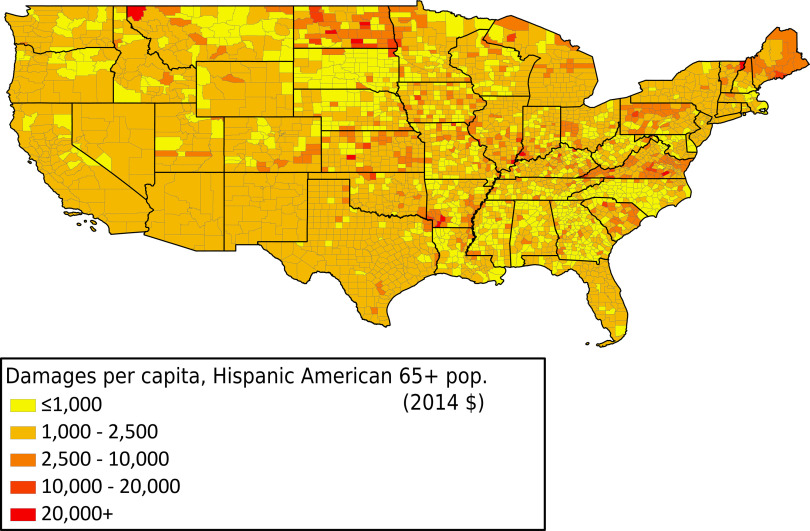
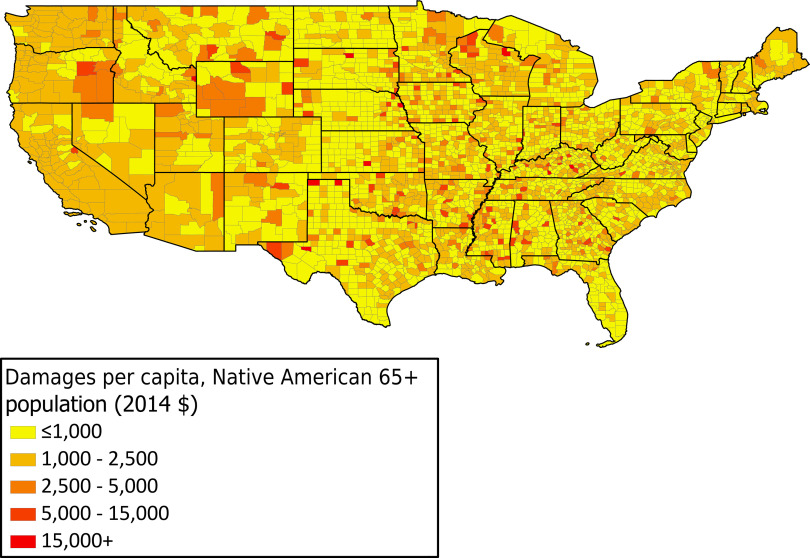
To demonstrate the geographic distribution of costs associated with premature mortality, we created maps depicting per capita mortality costs for each racial/ethnic group (Figures 2–7), using the race/ethnicity-specific Di et al. (2017) CRFs. Maps depicting aggregate mortality costs by race/ethnicity can be found in the supplemental material, Figures S1–S5. On a per-capita basis, costs exhibited a somewhat homogenous distribution across the country and across racial/ethnic groups, though the tails of the distributions differed significantly across race/ethnicity. Specifically, the highest per-capita mortality costs for non-White racial/ethnic groups ranged between 4 and 6 times higher than that for White Americans, as can be seen in the map legends. For example, the highest class of per capita mortality costs for Black Americans (Figure 3) and Hispanic Americans (Figure 5) was above , though the highest class of per capita costs for White Americans (Figure 7) was only above .
Figure 2.
aggregate and per capita damages, total population. (A) aggregate damages, total population. (B) per capita damages, total population.
Figure 7.
County per capita damages, White Americans.
Figure 3.
County per capita damages, Black Americans.
Figure 5.
County per capita damages, Hispanic Americans.
Figure 4.
County per capita damages, Asian Americans.
Figure 6.
County per capita damages, Native Americans.
Policy Scenario 1: Uniform Increase in Baseline Concentrations
Table 5 reports the aggregate exposure deaths among populations above 65 y of age in 2014 according to the different CRFs, and it then compares these to the deaths produced by a simulation in which is added to all county-level concentrations. Across all CRFs and underlying health data employed, we found that deaths would increase by approximately 10% nationally under this uniform air-quality degradation. Applying a uniform VSL to this increase in premature mortality resulted in approximately billion in mortality costs, although this amount can increase to , depending on the CRF and mortality rates employed (see Table 5, final column).
Table 5.
Change in -attributable deaths from uniform increase in .
| Functional form | Reference | Mortality rates | 2014 National Emissions Inventory (thousand deaths) | Plus (thousand deaths) | Difference, thousand deaths (%) | Monetary cost ( 2014) |
|---|---|---|---|---|---|---|
| Linear CRF | Di et al. 2017 | Weighted average | 121.3 | 134.2 | 12.9 (10.6) | 112,320 |
| Linear CRF | Di et al. 2017 | Race/ethnicity-specific | 121.3 | 134.2 | 12.9 (10.6) | 112,320 |
| Race/ethnicity-specific linear CRF | Di et al. 2017 | Weighted average | 132.4 | 145.9 | 13.5 (10.2) | 113,400 |
| Race/ethnicity-specific linear CRF | Di et al. 2017 | Race/ethnicity-specific | 132.7 | 146.2 | 13.5 (10.2) | 113,400 |
Table 6 continues to explore the mortality incidence of the uniform increase. In this table, the focus is on both incidence by racial/ethnic group and age group for populations over 65 y of age. The numbers in the table report the total mortality burden due to the uniform increase relative to White American populations, by age group (thus, all values for White American population mortality equal 1). Mortality burden was here defined as mortality risk from the change in pollution, specific to each demographic.
Table 6.
Race/ethnicity-specific burden from uniform increase in , relative to white Americans.
| Scenario | Racial/ethnic group | Age 65–74 y | Age 75–84 y | Age y |
|---|---|---|---|---|
| Linear CRF (Di et al. 2017), population–weighted average mortality rates | Native Americans | 1.069 | 1.039 | 1.021 |
| Asian Americans | 0.859 | 0.874 | 0.895 | |
| Black Americans | 1.060 | 1.010 | 0.973 | |
| Hispanic Americans | 0.919 | 0.912 | 0.923 | |
| White Americans | 1.000 | 1.000 | 1.000 |
| Racial/ethnic group | Age 65–70 y | Age 75–80 y | Age y | |
|---|---|---|---|---|
| Race/ethnicity-specific mortality rates and race/ethnicity-specific CRF (Di et al. 2017) | Native Americans | 1.550 | 1.361 | 0.995 |
| Asian Americans | 0.705 | 0.800 | 0.884 | |
| Black Americans | 3.631 | 2.946 | 2.434 | |
| Hispanic Americans | 1.284 | 1.265 | 1.205 | |
| White Americans | 1.000 | 1.000 | 1.000 |
These results demonstrate that under the linear [non–race/ethnicity-specific; Di et al. (2017)] CRF, there is little differentiation in mortality burden across racial/ethnic groups. Native Americans of all age groups had a slightly larger burden than White Americans of the same corresponding ages. Black Americans under 75 y of age also incurred a slightly larger mortality burden than White American populations of the same age (though results appear to equalize for older age groups). Furthermore, using this CRF resulted in Hispanic Americans and Asian Americans having a lower mortality burden than White Americans (with ratios less than 1 for all racial/ethnic group/age group combinations).
However, when we used race/ethnicity-specific CRFs, we found significantly different outcomes for all people of color, except for Asian Americans (a group that consistently had a lower pollution-related mortality burden than White Americans had, in part due to lower underlying mortality rates; see Table 1) from a uniform - increase in pollution. Black Americans of all ages above 65 y incurred mortality burdens up to 3 and one-half times greater than those of White Americans of the same age (the race/ethnicity-specific burden, relative to White Americans, presented in Table 6 for Black Americans is 2.4–3.6). Similarly, Hispanic Americans sustained a 20%–28% greater mortality burden than White Americans (as the race/ethnicity-specific burden, relative to White Americans, presented in Table 6 for Hispanic Americans is 1.205–1.284). Native American populations under the age of 85 y experienced a 36%–55% higher mortality burden than White Americans.
Policy Scenario 2: MATS Abatement Technology
In this scenario, we modeled how the abatement technology adopted due to MATS affected pollution and, in turn, premature mortality. Figure 8 shows that, had these technologies not been adopted, concentrations would have been on average higher across all counties, reflecting roughly a 5% increase. However, we report significant variation in this increase, with changes up to in counties near the Ohio River. Table 7 presents the changes in ambient concentrations under the MATS scenario and compares it to the uniform change in ambient concentration. On average, the increase is much smaller from the MATS relative to a uniform -change in concentrations, though the increase goes as high as 50% for some counties.
Figure 8.
![Figure 8 is a map of the United States of America depicting Mercury and Air Toxics Standards induced changes in 2016. The range denoting microgram per meter circumflex 3 is divided into six parts, namely, 0.0 to 0.05, 0.05 to 0.50, 0.50 to 0.75, 0.75 to 1.00, 1.00 to 1.50, and 1.50 to 3.00.] Note: MATS, Mercury and Air Toxics Standards.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/bdfd/8653772/a60c3dcb65e3/ehp9001_f8.jpg)
MATS-induced change in , 2016.
Table 7.
Changes in ambient concentration under two counterfactual scenarios.
| Scenario | Average increase in concentrations | % Increase, on average | % Increase, minimum | % Increase, maximum |
|---|---|---|---|---|
| Uniform degradation of air quality | 17.9% | 4.6% | 101.4% | |
| Removal of Mercury Air Toxics Standards (MATS) abatement technology | 3.3% | 0% | 50.6% |
Note: The minimum and maximum numbers reflect the percentage increase at the county with the lowest and highest increase, respectively.
We next calculated the benefits across racial/ethnic groups in terms of avoided premature mortality of MATS abatement technology. Table 8 shows the premature deaths avoided and monetary benefits of MATS abatement technology, under the linear and the race/ethnicity-specific CRFs from Di et al. (2017) (both of these results employ race/ethnicity-specific underlying mortality rates).
Table 8.
Deaths avoided and monetary benefits in older populations from MATS, 2015 and 2016.
| Deaths avoided | Monetary benefits ( 2014) | |||||||
|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2015 | 2016 | |||||
| Racial/ethnic group | Linear CRF | Racial/ethnic-specific CRF | Linear CRF | Racial/ethnic-specific CRF | Linear CRF | Racial/ethnic-specific CRF | Linear CRF | Racial/ethnic-specific CRF |
| Native Americans | 12 | 16 | 16 | 21 | 103 | 137 | 139 | 184 |
| Asian Americans | 24 | 31 | 54 | 69 | 211 | 268 | 473 | 600 |
| Black Americans | 280 | 658 | 413 | 961 | 2,440 | 5,746 | 3,600 | 8,388 |
| Hispanic Americans | 53 | 79 | 103 | 154 | 460 | 687 | 901 | 1,342 |
| White Americans | 2,262 | 1,980 | 3,494 | 3,057 | 19,800 | 17,285 | 30,490 | 26,683 |
| All groups | 2,631 | 2,763 | 4,079 | 4,261 | 22,970 | 24,122 | 35,610 | 37,197 |
We found that, across all racial/ethnic groups, abatement technology led to 2,631–2,763 avoided premature deaths in older populations in 2015 and 4,079–4,261 in 2016, depending on the CRF employed (see Table 8). As can be seen in Table 8, the vast majority (72%–85%) of estimated avoided deaths were for White American populations, followed next by 10%–23% of avoided deaths for Black American populations (the range depends on the CRF employed).
Importantly, the use of the linear, non–race/ethnicity-specific Di et al. (2017) CRF underestimated total avoided deaths due to MATS policy by about 4.4% (for both 2015 and 2016 combined), although this effect was much larger for certain racial/ethnic groups. Specifically, we found that using a linear, non–race/ethnicity-specific approach (as reported in Table 6, columns 1 and 3) would underestimate (relative to using race/ethnicity-specific data and CRFs) the benefits to older (above 65 y of age) Black American communities by almost 60%, whereas the benefits to older White American communities are overestimated by about 14%.
Applying a VSL of to these lives saved resulted in the linear non–racial/ethnic specific CRF approach underestimating the benefits of MATS abatement technology by at least from 2015 to 2016.
Discussion
Summary of Results
Our analysis demonstrated that the use of non–race/ethnicity stratified CRF estimates in air pollution policy assessments (an approach that ignores differences in vulnerability to impacts across racial/ethnic subgroups) resulted in underestimates of the health impacts overall and, in particular, the impact on Black American and Hispanic populations. By using race/ethnicity-specific CRFs we highlight in this paper the inequities of air pollution-related mortality and demonstrate that the common practice of not differentiating these CRFs by racial/ethnic group undervalues air-quality improvements to racial/ethnic minority communities.
Specifically, we found that by using race/ethnicity-specific CRFs and underlying health (mortality) data, rather than the prevalent approach used in most federal policy analyses, these changes a) caused an increase in the baseline estimates of aggregate deaths (by almost 10%); b) attributed a greater share of these baseline pollution-related deaths to Black American, Hispanic American, and Asian American populations; and c) implied that, in a reverse uniform pollution reduction scenario, benefits would accrue more to Black Americans (), Native Americans (), and Hispanic Americans () than to White Americans (see Table 6).
For Black American populations in particular, the effect of using race/ethnicity-specific exposure–response functions produces the largest changes in policy impacts: We found that the mortality burden for Black Americans can reach 25% of all deaths, although this group accounts for only 9% of total older populations (see Table 3, column 5).
Furthermore, using a real-world example of the MATS policy, we demonstrated how federal policy to improve air quality can produce measurable environmental justice improvements by reducing health disparities from air pollution exposure. It also showed that we will continue to significantly underpredict the environmental justice benefits of energy policies if we do not employ the most up-to-date assessments of CRFs that are specific to different racial/ethnic subgroups.
An assessment of the monetary cost of mortality in older populations attributed to a increase in (approximately ) underlined the general conclusion of other studies that pollution represents an enormous cost to society (Tschofen et al. 2019). For context, this cost amounts to approximately double the estimated cost of all major federal rules issued by the U.S. EPA from 2006 to 2016 (Office of Management and Budget 2017). This research thus highlights important inequities associated with current federal policy approaches, concerning pollution exposure for people of color, in particular for Black Americans.
External Validity of Results
Our estimate of approximately 100,000 premature deaths from exposure for populations over the age of 65 is in line with previous estimates. Tessum et al. (2019) estimated 131,000 deaths in 2015 using a different integrated assessment model and the Krewski et al. CRF (2009). Although this estimate included all persons over the age of 25, older individuals incur the majority of premature mortality risk. Further, Burnett et al. (2018) report a range of premature deaths from in the U.S. of between 121,000 and 213,000, inclusive of all age groups.
Regarding the results for the MATS analysis, our results are similar to EPA’s estimates in the lower bound of the 2011 MATS Regulatory Impact Analysis (4,400 avoided deaths for 2016, for ages above 30 y) (U.S. EPA 2011a). We would expect to find estimated avoided deaths at the lower bounds of the U.S. EPA’s estimates for two reasons. First, we estimated only the effects on age groups above 65 y, whereas the U.S. EPA estimated this for all ages above 30 y. Second, we modeled only the effect of abatement technology on reduced mortality and ignored any air-quality improvements that would arise from the exit of coal plants, which likely contributed to an even greater reduction in deaths.
Strengths and Limitations of Our Work
A strength of this study is that the Di et al. (2017) CRFs that we employed are from a large nationally representative longitudinal cohort study, including racial/ethnic minority and rural populations, in contrast to Krewski et al. (2009), which consisted of a predominantly urban White American population.
The Di et al. (2017) study also used fine-scale air pollution exposure estimates and may be less likely to be biased due to exposure misclassification and more likely to be representative of exposures and effects across the exposure range relevant to the United States than the CRFs presented in Krewski et al. (2009).
An additional strength of the present paper is our reliance on multiyear aggregated baseline mortality rates from the CDC. Our use of comprehensive, publicly available mortality data ensures that spatial distribution of mortality rates reflects robust patterns in risk and is not an artifact of events during a single year.
We note several limitations to our work. First, whereas the U.S. EPA’s NEI is a comprehensive source of national air pollution emissions (U.S. EPA 2016), our reliance on it introduced uncertainty in the baseline estimates of concentrations. As with any model, the manner in which the AP3 integrated assessment model (see “Material and Methods” section) links emissions to concentrations is not perfect. We note, however, that its performance against the U.S. EPA’s air-quality system monitoring network for and chemical transport models has been evaluated in prior work and found to be satisfactory for policy analysis (Gilmore et al. 2019).
Another limitation to our work is the geographic aggregation at the county level, given the structure of AP3. Intracounty concentrations may vary significantly, and Black Americans are generally more likely to live near highways and other major emissions sources within a county (Tian et al. 2013; Perlin et al. 1999). Furthermore, county-level mortality rates may overlook significant variation in mortality rates within the county itself, especially in larger counties (Southerland et al. 2021). Overall, this points to the need for investigation of these impacts at a scale finer in resolution than the county, and further research on identifying subcounty variation in pollution exposure is warranted (such as provided by the U.S. EPA’s Downscaler Model; U.S. EPA 2017). However, that research is outside the scope of this paper, and our current estimates are likely a lower bound on the actual health impacts of air pollution on Black American communities, because county averages will smooth over these hyperlocal differences in exposure and susceptibility.
Implications for Policy
Studies have shown that historically racist policies such as red lining and citing of highways and polluting facilities have resulted in racial/ethnic minority and other disadvantaged populations living in areas with a disproportionately higher number of emitting facilities (Mikati et al. 2018; Banzhaf et al. 2019) and facing higher exposure burden in comparison with White American populations. In addition, policies and actions to reduce air pollution are generally concentrated in wealthier and less diverse populations, resulting in widening disparities (Jbaily et al. 2020; Richmond-Bryant et al. 2020). Yet the issues of air pollution–related health impact inequities extend beyond exposure alone. Many of the same racist policies, institutional practices, and poor cultural representations have caused disinvestment in racial/ethnic minority communities, resulting in differential quality and distribution of housing, transportation, economic opportunity, education, food, access to health care, and beyond. All of these inequities manifest in health disparities, higher underlying mortality rates, and greater susceptibility to pollution-caused disease (Morello-Frosch et al. 2011; Payne-Sturges et al. 2021).
During the COVID-19 pandemic of 2020–2021, these same pathways contributed to Black Americans facing an inequitably larger mortality burden (2 times larger than for White Americans; APM Research Lab 2021) from SARS-CoV-2 (Afifi et al. 2020, Doumas et al. 2020, Persico and Johnson 2021) and were laid bare when race/ethnicity-specific data were collected and used. Though these issues are outside the scope of our study, our findings demonstrate the importance of collecting and using the most up-to-date race/ethnicity-specific data when considering policy-making decisions. In fact, the U.S. EPA’s own integrated science assessment concludes that “the evidence is adequate to conclude that non-Whites, particularly Blacks, are at increased risk for health effects based on studies examining differential exposure and health effects” (U.S. EPA 2019).
Our results emphasize the importance of conducting health impact assessments of air quality–related policies with a recognition of the underlying differences across racial/ethnic groups. An understanding that the marginal effect of air-quality changes will not affect all racial/ethnic groups in the same way is critical, particularly given the nation’s pervasive and systemic racial/ethnic injustices. Assuming that all racial/ethnic groups are equally affected by air pollution will continue to contribute to injustices faced by people of color, especially in light of policies that can alter the magnitude or distribution of pollution across racial/ethnic groups.
Fundamentally, the choice of which vital statistics and CRFs to use when estimating the effect of any air quality–related policy will directly affect its calculated benefits and resulting environmental justice implications. Several large-scale and notable federal benefit–cost analyses that assess mortality impacts generally use mortality rates that are averaged across all racial/ethnic groups and pair this with linear non–race/ethnicity-specific CRFs (see for example, U.S. EPA 2011a, 2011b, 2012), leading to a misrepresentation of the race/ethnicity-specific outcomes of policies.
Our results have particularly important implications for the NAAQS program of the CAA, which regulates particulate pollution. The law explicitly mandates that these standards must be set at a level that protects public health with an “adequate margin of safety” (National Primary and Secondary Ambient Air Quality Standards). In particular, the U.S. EPA must also consider the impacts on the health of vulnerable populations (Executive Order 12898; Executive Order 14008). Our study demonstrated the policy importance of recognizing the fact that air pollution risks differ by racial/ethnic group; thus, parameterization of overall national standards should be tailored to protect the most vulnerable subgroup. In addition, the NAAQS program is structured around air-quality criteria that are to be based on the best available science. To date, epidemiological studies were unable to reliably disaggregate CRFs specific to vulnerable subgroups. Given the recent innovations and statistical power of Di et al. (2017), and in light of the associated racial/ethnic disparities and underestimated aggregate mortality impacts, U.S. EPA should take these disparate impacts into consideration when making a determination regarding what is an adequately protective “margin of safety” in future NAAQS reviews.
This paper demonstrated the importance of choosing the most accurate specification when estimating health effects of air quality due to policy changes, because underlying mortality rates, pollution exposure, and pollution susceptibility differ significantly across racial/ethnic groups. Using generalized health data to estimate the benefits of air-quality policies will lead to incorrect estimates, and likely underestimate the benefits of these policies to most racial/ethnic minorities. Thus, it is essential that federal agencies perform regulatory impact analyses with the use of as much granular data as possible, both in terms of CRFs and mortality rates. Methods should adequately represent differences in health outcomes by demographic group and across ambient pollution levels, as demonstrated herein. Wherever such breakdowns are not possible, gap-filling using prior methods could be employed. These changes may significantly improve future air-quality policy outcomes and help reduce environmental justice disparities.
Supplementary Material
Acknowledgments
The authors would like to thank the following individuals for reviewing this work and providing excellent feedback: R. Romero, M. Harris, R. Fullmer, J. Fine, S. Kerr, T. Thompson, and M. Warner.
References
- Afifi RA, Novak N, Gilbert PA, Pauly B, Abdulrahim S, Rashid SF, et al. 2020. ‘Most at risk’ for COVID19? The imperative to expand the definition from biological to social factors for equity. Prev Med 139:106229, PMID: , 10.1016/j.ypmed.2020.106229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ake T, Licata A. 2011. Circulating Dry Scrubbers Comply with the EPA Maximum Achievable Control Technology Limits. Worcester, MA: Babcock Power Environmental Inc. https://www.babcockpower.com/wp-content/uploads/2018/02/circulating-dry-scrubbers-comply-with-the-epa-maximum-achievable-control-technology-limits.pdf [accessed 16 November 2020]. [Google Scholar]
- APM Research Lab. 2021. The color of corona virus: Covid-19 deaths by race and ethnicity in the US. https://www.apmresearchlab.org/covid/deaths-by-race [accessed 17 November 2021]. [Google Scholar]
- Banzhaf S, Ma L, Timmins C. 2019. Environmental justice: the economics of race, place, and pollution. J Econ Perspect 33(1):185–208, PMID: , 10.1257/jep.33.1.185. [DOI] [PubMed] [Google Scholar]
- Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA, et al. 2018. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci U S A 115(38):9592–9597, PMID: , 10.1073/pnas.1803222115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (U.S. Centers for Disease Control and Prevention). WONDER. https://wonder.cdc.gov/ [accessed 22 June 2021].
- Clay K, Jha A, Muller N, Walsh R. 2019. External costs of transporting petroleum products: evidence from shipments of crude oil from North Dakota by pipelines and rail. Energy J 40(1):, 10.5547/01956574.40.1.kcla. [DOI] [Google Scholar]
- Clay K, Muller NZ. 2019. Recent increases in air pollution: evidence and implications for mortality, 10.3386/w26381. [DOI]
- Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, et al. 2017. Air pollution and mortality in the Medicare population. N Engl J Med 376(26):2513–2522, PMID: , 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumas M, Patoulias D, Katsimardou A, Stavropoulos K, Imprialos K, Karagiannis A. 2020. COVID19 and increased mortality in African Americans: socioeconomic differences or does the renin angiotensin system also contribute? J Hum Hypertens 34(11):764–767, PMID: , 10.1038/s41371-020-0380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Executive Order 12898. 1994. Federal Actions To Address Environmental Justice in Minority Populations and Low-Income Populations. Fed Reg 59.
- Executive Order 14008. 2021. Tackling the Climate Crisis at Home and Abroad. Fed Reg 86(19).
- Gilmore EA, Heo J, Muller NZ, Tessum CW, Hill JD, Marshall JD, et al. 2019. An inter-comparison of the social costs of air quality from reduced-complexity models. Environ Res Lett 14(7):074016, 10.1088/1748-9326/ab1ab5. [DOI] [Google Scholar]
- Goodkind AL, Tessum CW, Coggins JS, Hill JD, Marshall JD. 2019. Fine-scale damage estimates of particulate matter air pollution reveal opportunities for location-specific mitigation of emissions. Proc Natl Acad Sci USA 116(18):8775–8780, PMID: , 10.1073/pnas.1816102116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, Hsia C, O’Neill MS. 2015. Socioeconomic disparities and air pollution exposure: a global review. Curr Environ Health Rep 2(4):440–450, PMID: , 10.1007/s40572-015-0069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland SP, Mansur ET, Muller NZ, Yates AJ. 2016. Are there environmental benefits from driving electric vehicles? The importance of local factors. Am Econ Rev 106(12):3700–3729, 10.1257/aer.20150897. [DOI] [Google Scholar]
- Jaramillo P, Muller NZ. 2016. Air pollution emissions and damages from energy production in the US: 2002–2011. Energy Policy 90:202–211, 10.1016/j.enpol.2015.12.035. [DOI] [Google Scholar]
- Jbaily A, Zhou X, Liu J, Lee T-H, Verguet S, Dominici F. 2020. Inequalities in air pollution exposure are increasing in the United States. medRxiv 10.1101/2020.07.13.20152942. [DOI] [Google Scholar]
- Kaminski J. 2003. Technologies and costs of SO2-emissions reduction for the energy sector. Applied Energy 75(3–4):165–172, 10.1016/S0306-2619(03)00029-1. [DOI] [Google Scholar]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y. 2009. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst (140):5–114, PMID: . [PubMed] [Google Scholar]
- Lepeule J, Laden F, Dockery D, Schwartz J. 2012. Chronic exposure to fine particles and mortality: an extended follow-up of the Harvard Six Cities study from 1974 to 2009. Environ Health Perspect 120(7):965–970, PMID: , 10.1289/ehp.1104660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikati I, Benson AF, Luben TJ, Sacks JD, Richmond-Bryant J. 2018. Disparities in distribution of particulate matter emission sources by race and poverty status. Am J Public Health 108(4):480–485, PMID: , 10.2105/AJPH.2017.304297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. 2011. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff (Millwood) 30(5):879–887, PMID: , 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- Muller NZ. 2014. Boosting GDP growth by accounting for the environment. Science 345(6199):873–874, PMID: , 10.1126/science.1253506. [DOI] [PubMed] [Google Scholar]
- Muller NZ, Mendelsohn R, Nordhaus W. 2011. Environmental accounting for pollution in the United States economy. Am Econ Rev 101(5):1649–1675, 10.1257/aer.101.5.1649. [DOI] [Google Scholar]
- National Primary and Secondary Ambient Air Quality Standards. 2019. 42 U.S. Code 85 Subchapter 1 (Part A) § 7409. Ithaca, NY: Cornell Law School Legal Information Institute. https://www.law.cornell.edu/uscode/text/42/7409 [accessed 22 June 2021]. [Google Scholar]
- Office of Management and Budget. 2017. 2017 Report to Congress on the Benefits and Costs of Federal Regulations and Agency Compliance with the Unfunded Mandates Reform Act. https://www.whitehouse.gov/wp-content/uploads/2019/12/2019-CATS-5885-REV_DOC-2017Cost_BenefitReport11_18_2019.docx.pdf [accessed 17 November 2021].
- Payne-Sturges DC, Gee GC, Cory-Slechta DA. 2021. Confronting racism in environmental health sciences: moving the science forward for eliminating racial inequities. Environ Health Perspect 129(5):55002, PMID: , 10.1289/EHP8186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlin SA, Sexton K, Wong DW. 1999. An examination of race and poverty for populations living near industrial sources of air pollution. J Expo Anal Environ Epidemiol 9(1):29–48, PMID: , 10.1038/sj.jea.7500024. [DOI] [PubMed] [Google Scholar]
- Persico CL, Johnson KR. 2021. The effects of increased pollution on COVID-19 cases and deaths. J Environ Econ Manage 107:102431, PMID: , 10.1016/j.jeem.2021.102431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CA 3rd, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE, et al. 1995. Particulate air pollution as a predictor of mortality in a prospective study of U.S. Adults. Am J Respir Crit Care Med 151:669–674, PMID: , 10.1164/ajrccm/151.3_Pt_1.669. [DOI] [PubMed] [Google Scholar]
- Richmond-Bryant J, Mikati I, Benson AF, Luben TJ, Sacks JD. 2020. Disparities in distribution of particulate matter emissions from US coal-fired power plants by race and poverty status after accounting for reductions in operations between 2015 and 2017. Am J Public Health 110(5):655–661, PMID: , 10.2105/AJPH.2019.305558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southerland VA, Anenberg SC, Harris M, Apte J, Hystad P, van Donkelaar A, et al. 2021. Assessing the distribution of air pollution health risks within cities: a neighborhood-scale analysis leveraging high-resolution data sets in the Bay Area, California. Environ Health Perspect 129(3):37006, PMID: , 10.1289/EHP7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessum CW, Apte JS, Goodkind AL, Muller NZ, Mullins KA, Paolella DA, et al. 2019. Inequity in consumption of goods and services adds to racial–ethnic disparities in air pollution exposure. Proc Natl Acad Sci USA 116(13):6001–6006, PMID: , 10.1073/pnas.1818859116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian N, Xue J, Barzyk TM. 2013. Evaluating socioeconomic and racial differences in traffic-related metrics in the United States using a GIS approach. J Expo Sci Environ Epidemiol 23(2):215–222, PMID: , 10.1038/jes.2012.83. [DOI] [PubMed] [Google Scholar]
- Tschofen P, Azevedo IL, Muller NZ. 2019. Fine particulate matter damages and value added in the US economy. Proc Natl Acad Sci U S A 116(40):19857–19862, PMID: , 10.1073/pnas.1905030116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. EPA (U.S. Environmental Protection Agency). 1999. Regulatory Impact Analysis for the Final Section 126 Petition Rule. https://www3.epa.gov/ttn/ecas/docs/ria/transport_ria_final-section-126-rule_1999-12.pdf. [accessed 17 November 2021].
- U.S. EPA. n.d. Air Pollution Control Technology Fact Sheet. https://www3.epa.gov/ttncatc1/dir1/ffdg.pdf. EPA-452/F-03-034 [accessed 17 November 2021].
- U.S. EPA. 2011a. Regulatory Impact Analysis for the Final Mercury and Air Toxics Standards.
- U.S. EPA. 2011b. The benefits and costs of the Clean Air Act from 1990 to 2020.
- U.S. EPA. 2012. Regulatory Impact Analysis for the Final Revisions to the National Ambient Air Quality Standards for Particulate Matter.
- U.S. EPA. 2016. 2014 National Emissions Inventory (NEI) Data. https://www.epa.gov/air-emissions-inventories/2014-national-emissions-inventory-nei-data [accessed 22 June 2021].
- U.S. EPA. 2017. Bayesian space-time downscaling fusion model (Downscaler)–Derived Estimates of Air Quality for 2013. EPA-450/R-17-001.
- U.S. EPA. 2019. Integrated Science Assessment (ISA) for Particulate Matter (Final Report).
- Viscusi WK, Aldy JE. 2003. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertain 27(1):5–76, 10.1023/A:1025598106257. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.