Abstract
Despite recent advancements in global population well-being and food security, climate change threatens to undermine child nutritional health, particularly for marginalized populations in tropical low- and middle-income countries. South Asia is at particular risk for climate-driven undernutrition due to a combination of historical weather exposures, existing nutritional deficits, and a lack of sanitation access. Previous studies have established that precipitation extremes increase rates of undernutrition in this region, but the existing literature lacks adequate consideration of temperature anomalies, mediating social factors, and the developmentally-relevant timing of exposure. We combine high-resolution temperature and precipitation data with large-sample survey data on household demographics and child anthropometry, using an approach that incorporates three key developmental periods and a rigorous fixed effects design. We find that precipitation extremes in the first year of life significantly decrease children’s height-for-age (HAZ) in South Asia. The detrimental effects of extreme precipitation are especially concentrated in under-resourced households, such as those lacking access to proper sanitation and education for women, while anomalous heat is particularly harmful for children in Pakistan, though it tends to benefit children in some demographic groups. These results indicate that nutritional status in South Asia is highly responsive to climate exposures, and that addressing sanitation infrastructure and other development priorities is a pathway towards reducing this vulnerability.
Keywords: climate change, temperature, precipitation, child health, nutrition, anthropometry
Introduction
Global population well-being and food security have improved considerably over the past 50 years, but scholars are concerned that climate change will exacerbate recent trends towards deterioration, particularly for the world’s most vulnerable populations (Burke et al. 2015). Among the most vulnerable are marginalized populations in tropical and subtropical low- and middle-income countries, where baseline temperatures are high and community resources with which to respond are often few (IPCC, 2014; Frame et al. 2017; Mora et al. 2017). In these areas, population health and well-being are already threatened by rising global temperatures and increasingly variable rainfall patterns (Challinor et al. 2014; Mora et al. 2017; Spears et al. 2018), which in turn puts children’s food security and nutritional health at particular risk. Adequate nutrition for children under five years old is recognized as central to human development at the individual, national, and international levels (Horton, 2013), and chronic malnutrition in early childhood has been shown to cause irreparable damage to cognitive and physical development (Alderman, 2006; Black, 2013; Shively, 2017). Understanding the complex interactions between climate, nutrition, and social vulnerability in regions facing nutritional shortfalls is key to developing appropriate mitigation policy as the climate continues to cause more frequent and more intense extreme weather events (Frame et al. 2017).
Previous studies have examined the costs of precipitation extremes for child health at both the global and national scale (Grace et al. 2012; Arnell et al. 2016; Cooper et al. 2019; Frame et al. 2017; Kumar et al. 2016; Mora et al. 2017; Randell et al. 2020), but the role of childhood temperature exposures has been underexamined. Existing global and South Asian studies of climate shocks and childhood nutrition have instead focused exclusively on precipitation (Shively et al. 2015; Kumar et al. 2016; Mulmi et al. 2016; Tiwari et al. 2016; Cooper et al. 2019; Dimitrova & Bora, 2020; Dimitrova & Muttarak, 2020; Randell et al. 2021), ignoring the well-documented risks of temperature extremes (Davenport et al. 2016; Grace et al. 2021). Many studies have also not fully accounted for key biological periods of exposure to climate shocks, for potential vulnerability across different socio-demographic groups, or for spatial correlates of climate that might confound the results (Randell et al. 2020; Thiede & Gray, 2020; Nicholas et al. 2021).
To address these issues, we use data from the Demographic and Health Surveys extracted using IPUMS-DHS (Boyle et al. 2019) alongside temperature and precipitation data from the Climate Research Unit’s Time-Series (CRU; Harris et al. 2020) and the Climate Hazards Group Infrared Temperature & Precipitation with Stations (CHIRPS & CHIRTS; Funk et al. 2015; Funk et al. 2019). Using this linked dataset, we examine the effects of climate anomalies and daily extremes on height-for-age Z-scores and stunting (HAZ < −2) for 220 thousand children ages 2–5 in four South Asian countries (Bangladesh, India, Nepal and Pakistan). We separately examine climate exposures during the prenatal period, first year of life and second year of life, and use a fixed effects approach that accounts for spatial and temporal confounders to climate. Our findings indicate that child growth in South Asia is undermined when the first year of life is unusually wet or includes uncommonly wet or dry days, as well as when extreme temperatures occur in the first two years of life. We find that children with low toilet quality and low maternal education and who live in India and Pakistan are most vulnerable to harmful climate effects, as well as intriguing evidence for subpopulations that currently benefit from slightly higher-than-average temperatures. Taken together, these results indicate that nutritional status in South Asia is highly responsive to climate exposures and that ongoing nutritional improvements in South Asia are likely to be handicapped as climate change leads to more frequent and intense precipitation shocks.
Background
Over the past decade, a rich literature has established that global climate change affects health in powerful and calculable ways. Although much of this research focuses on high-income countries in Europe and North America, evidence shows that the consequences of climate change will emerge more quickly and be more virulent in countries closest to the equator (IPCC, 2014; Frame et al. 2017; Mora et al. 2017). The literature has established that nutritional health is highly vulnerable to environmental stressors in early childhood, which take their toll through heat stress, failing agriculture, the spread of disease, and household economic instability (Challinor et al. 2014; Burke et al. 2015; Spears et al. 2018). We also know that children’s vulnerability to climate shocks does not remain constant throughout their early years (Shrimpton et al. 2001, Victora et al. 2009, Headey et al. 2015). In some cases, partial or complete catch-up growth among affected children has been shown to reduce the harmful effects of shocks over time (Hoddinott & Kinsey 2001; Del Ninno & Lundberg 2004), though this phenomenon is sometimes limited to children belonging to households with more access to wealth and community support. At the same time, evidence shows that exposure to extreme weather during the first 1,000 days after conception can have adverse developmental effects that last into adulthood and are linked to educational, financial, and physical deficits (Rayco-Solon et al. 2005; Alderman, 2006; Ramakrishnan et al. 2012; Black, 2013; Nobles & Hamoudi, 2019). A handful of studies have taken this into account when examining the intersection of climate change and child malnutrition (Kumar et al. 2016; Randell et al. 2020, Grace et al. 2021; Nicholas et al. 2021) but the existing literature is largely lacking in consideration of timing of exposure. We address this gap by measuring exposure and subsequent nutritional outcomes for the prenatal period as well as the first and second years of life.
In general, scholars agree that warming trends—particularly in conjunction with dryness—increase rates of stunting in children under five, an important indicator of chronic undernutrition (Grace et al. 2012; Davenport et al. 2016; Randell et al. 2020; Thiede & Gray, 2020, Dimitrova 2021). The impacts of precipitation extremes are less clear-cut; periods of drying have been found to cause undernutrition in some studies (Hoddinott & Kinsey, 2001; Grace et al. 2012; Davenport et al. 2016; Kumar et al. 2016), while others have noted that excessive rain is more strongly associated with stunting (Del Ninno & Lundberg, 2005; Dimitrova & Muttarak, 2020; Thiede & Gray, 2020). Cooper et al. (2019) explored the nutritional effects of both precipitation extremes in 53 countries and found that while children’s height-for-age steadily declined as conditions got drier, they declined even more steeply during wet periods—but only when the rain was very extreme. Others have found mixed effects of climate shocks that vary significantly according to spatial location, demographic characteristics, timing of exposure, and proximity to other climate shocks (Shively et al. 2015; Grace et al. 2021; Nicholas et al. 2021; Randell et al. 2021). In linking climate with birth outcomes in Mali, Grace et al. (2021) found that precise metrics and consideration of exposure timing—down to the trimester level, for prenatal exposure—are especially important when analyzing the impacts of precipitation. Still other researchers have connected the timing of yearly monsoons with child undernutrition, finding that higher precipitation was good for health during the rainy agricultural season, while delays in rain onset increased stunting by harming harvests, agricultural livelihoods, and subsequent food security (Randell et al. 2020; Thiede & Gray, 2020).
A related body of literature has identified South Asia as a region where children’s health is particularly vulnerable to climate change due to a unique combination of extreme weather, existing nutritional deficits, and a lack of sanitation access. In quantifying India’s vulnerability to rising global temperatures, Lopalo et al. (2018) estimate that the damages of a business-as-usual scenario would be equivalent to a 29% per capita reduction in national GDP for twenty consecutive years, an effect which would be barely mitigated even if India ceased all greenhouse gas emissions immediately. This evidence drives home the fact that, however severe the negative impact of global climate change, high-temperature low- and middle-income regions like South Asia will bear the brunt of it. Up to now, precipitation shocks have been the primary focus of studies that explicitly seek to link climate events with child nutritional outcomes in South Asia (Del Ninno & Lundberg, 2005; Shively et al. 2015; Kumar et al. 2016; Tiwari et al. 2016). Evidence from this work shows that both extremes are bad for child health: early exposure to drought increases children’s risk of stunting and mortality in rural India (Kumar et al. 2016), as do flood events in both Nepal and Bangladesh (Del Ninno & Lundberg, 2005; Tiwari et al. 2016). The current study also considers the impacts of extreme precipitation but expands on previous research by jointly considering both wetness and dryness using in a nonlinear approach (Cooper et al. 2019), and by including temperature anomalies, whose impacts have been under-studied thus far (Randell et al. 2020; Thiede & Gray, 2020).
Our approach builds on several other existing studies of these issues in South Asia (Kumar et al. 2016; Mulmi et al. 2016; Cooper et al. 2019; Dimitrova & Bora, 2020; Dimitrova & Muttarak, 2020), but with several key distinctions. Both Cooper et al. (2019) and Dimitrova (Dimitrova & Bora, 2020; Dimitrova & Muttarak, 2020) use DHS survey data to measure HAZ, and the latter studies specifically analyze the 2014–15 Indian DHS. Through the use of an alternative approach to locating households, we extend the range of our study by including the three previous waves in India as well as ten waves from Pakistan, Nepal, and Bangladesh. Dimitrova & Muttarak (2020) also use CRU climate data, although they exclude climate data outside of the annual monsoon period, whereas we measure children’s exposure to climate anomalies year-round. We also consider daily climate extremes as well as monthly anomalies, thereby increasing the temporal resolution of our study relative to others that use monthly or yearly climate data only. Finally, each of the aforementioned studies focuses on the effects of precipitation extremes, only indirectly taking the role of temperature into account through drought indices or similar metrics. This study is therefore the first to focus on the direct impacts of temperature shocks on child height, perhaps making this our largest contribution to collective understanding of the impacts of a warming world on populations in this vulnerable region.
Although a growing literature has linked extreme weather and negative nutritional outcomes, one difficulty comes in identifying the precise mechanisms through which climate and child health interact. Randell et al. (2020) outline four of these pathways: agricultural livelihoods, heat stress, infectious disease transmission, and women’s time use (their own addition). When weather conditions are not conducive to crop growth, agricultural households lose crucial income and food security, even under projected scenarios that include stringent carbon reductions (Challinor et al. 2014; Hasegawa et al. 2018; Ray et al. 2019). Lasting high temperatures can impair fetal development and threaten the shared nutritional health of mothers and young children, which is especially delicate during the first 1,000 days of life (Rayco-Solon et al. 2005; Ramakrishnan et al. 2012). Temperature and precipitation can also have interactive effects; warm and wet conditions, for instance can increase the range of vector-borne diseases, which weaken children’s immune systems and prevent proper nutrition (Pruss-Ustun et al. 2008; Spears et al. 2018). Infants whose mothers must perform demanding physical work during pregnancy are at higher risk of low birthweights and subsequent stunting (Randell et al. 2020). Each of these is connected to child nutrition via changes in household health and economic security, and these pathways may often intersect or work in tandem with each other.
Strong evidence also exists to suggest that nutritional deficits among South Asian children can be partly explained by the interactions of poor sanitation, gender inequality, and infectious disease. Spears et al. (2018) argue that exposure to open defecation alone can account for the fact that the average adult in India is richer but shorter than the average adult in Sub-Saharan Africa—a phenomenon often called the “Asian enigma.” Toilet access is a key social determinant of nutritional health because germs in feces cause infectious diseases, often diarrheal, which prevent children from absorbing nutrients and energy from their food and leave them susceptible to further infections (Pruss-Ustun et al. 2008; Spears et al. 2018). The prevalence of open defecation is also closely connected to gender roles and equity in South Asia. In rural Uttar Pradesh, for example, low-caste women with no household toilet access are forced to search for remote (and often dangerous) open defecation sites for fear of being seen by men, a fact which was associated with weakness in pregnant mothers and infants alike (Khanna & Das, 2015). Similarly, Coffey et al. (2015) found that the children of women with low social status were shorter on average than their high-status counterparts, further suggesting a link between maternal status, malnutrition, and subsequent child health. The current study will advance this avenue of research by bringing climate into the mix—will the effects of temperature and precipitation extremes be compounded by lack of toilet access?
Data and Methods
This study draws on nationally representative data from the Demographic and Health Surveys (accessed via IPUMS-DHS) on child undernutrition in four South Asian countries (Bangladesh, India, Nepal, and Pakistan). DHS administers structured surveys using a standardized sample design, questionnaire, and implementation procedure (Boyle et al. 2019). This study includes all DHS rounds in these countries that collected child anthropometric data, totaling 18 rounds conducted since the 1990s: six rounds in Bangladesh (1996–97, 1999–2000, 2004, 2007, 2011, 2014), four in India (1992–93, 1998–99, 2005–06, 2015–16), five in Nepal (1996, 2001, 2006, 2011, 2016) and three in Pakistan (1990–91, 2012–13, 2017–18). In these surveys, nationally representative household samples were selected via stratified, multi-stage sampling designs, with enumeration areas as the smallest areal unit. We include sampling weights in all multivariate analyses in order to account for the clustered sampling design as well as imbalances in sample density across countries and time, with the 2015–16 Indian survey round making up over half of all observations (137,824). GPS locations of enumeration areas are only available for 10 of 18 rounds, but we are able to locate households in 41 time-standardized administrative units using shapefiles created by the IPUMS-DHS project (Figure 1), which account for changes in sub-national borders over time within our study period. By including all rounds and using province-level locations, we nearly double the number of survey rounds and specifically quadruple the number of rounds in India, the largest country. These spatial units (5 each in Bangladesh, Nepal, and Pakistan, and 26 in India) are roughly equivalent to provinces and we refer to them as such. We exclude four provinces (Puducherry in India; Gilgit Baltistan, Federally Administered Tribal Areas, and Azad, Jammu and Kasmir in Pakistan) because they were included in only one DHS round, making it impossible to compare survey results across time.
Figure 1.
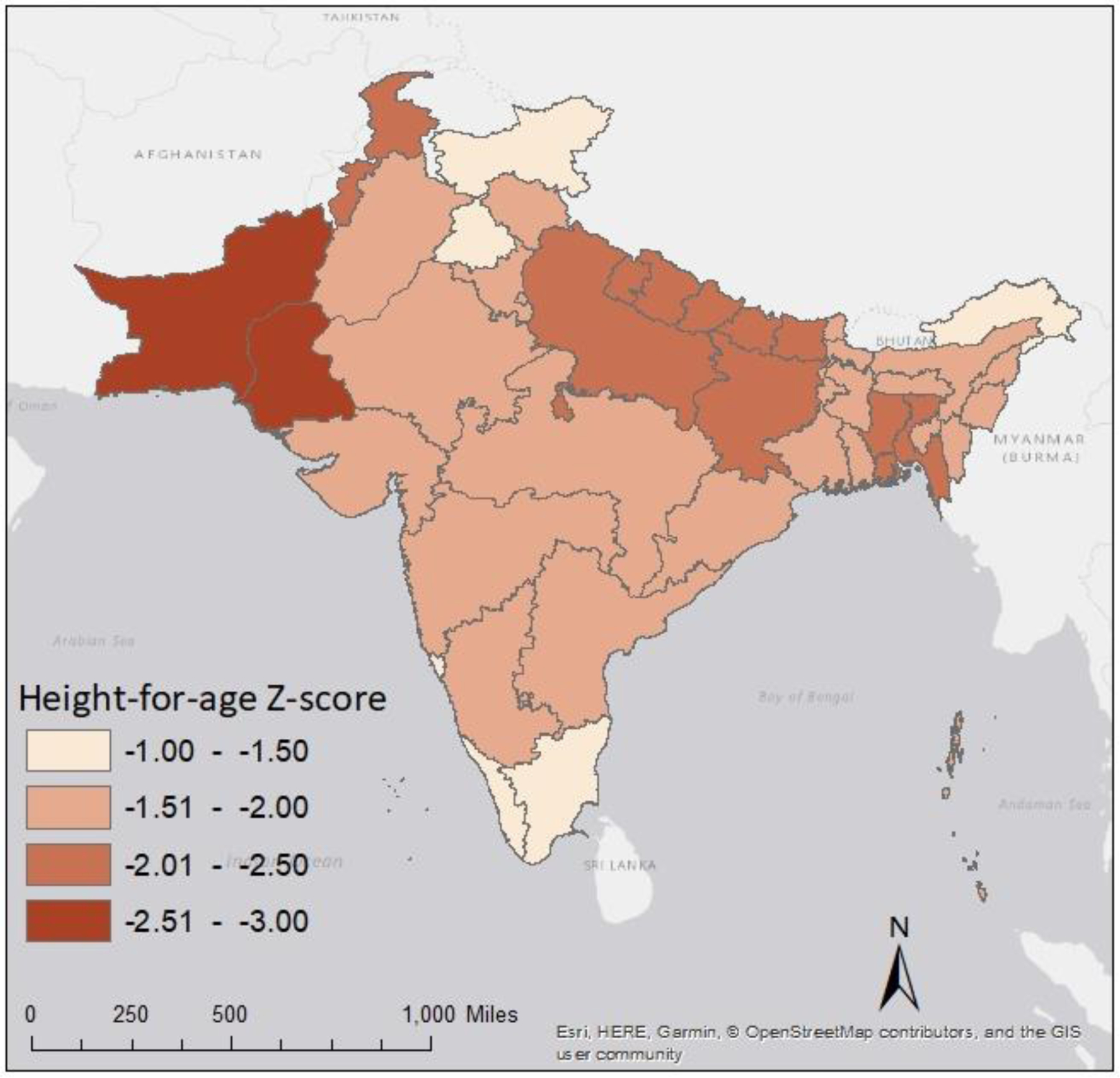
Height-for-age (HAZ) means among children ages 2–5 years, by province (Bangladesh 2014, India 2015–16, Nepal 2016, Pakistan 2017–18).
From these provinces and survey rounds, we extract data on 222,572 children (21,573 in Bangladesh, 184,177 in India, 10,896 in Nepal, and 5,926 in Pakistan) ages 24–59 months, the ages at which stunting typically becomes evident (Alderman & Headey, 2018). We focus on children’s exposure to climate extremes during the prenatal period and first 2 years of life, as these are the primary years during which children experience growth faltering (Shrimpton et al. 2001; Victora et al. 2009; Headey et al. 2015) and nutrition during this period has been shown to be a strong indicator of health and development well into adulthood (Rayco-Solon et al. 2005; Ramakrishnan et al. 2012). This study focuses predominantly on height-for-age, not weight-for-height, because HAZ is indicative of long-term malnutrition (Dearden et al. 2017). A child whose height-for-age is less than two standard deviations below the mean (HAZ < −2) is considered stunted, while a height-for-age value less than three standard deviations below the mean (HAZ < −3) implies severe stunting. Our core hypothesis is that prenatal and early life exposures to temperature and precipitation anomalies have jointly significant effects on height-for-age among South Asian children aged 2–5. Furthermore, we anticipate that exposures in the first year of life alone will significantly influence height-for-age among this population. We further explore these relationships by incorporating exposures to daily shocks, a nonlinear specification, interactions with the control variables, and population-weighted climate values.
Our analysis also includes a set of control variables that account for the most commonly identified socio-demographic characteristics of children, mothers, and households that contribute to undernutrition. Maternal controls include mother’s age at childbirth, marital status, level of education and number of children ever born; child controls include sex, age, month of birth, place of birth (health clinic or other), and birth order; and household and community controls include both household and community access to improved toilet infrastructure (such as flush toilets, pit latrines, or other improved non-flushing toilet system), as well as urban-rural status. There is some variation in the metric for urban-rural status between countries in our sample because DHS uses local definitions of urbanicity, but at minimum each country considers any place with a municipality, town committee, or cantonment board to be urban (Boyle et al. 2019). By controlling for child age and sex we account for biological factors influencing child anthropometry (Ssewanyana, 2003; Shrimpton et al. 2012), whereas our maternal and household controls add consideration of availability and allocation of family resources that have the potential to affect nutrition (De Silva & Sumarto, 2018). We add squared terms for children’s and mothers’ ages (in months and years, respectively) to allow their effect on child height to be nonlinear (Victoria et al. 2010). Indicators for month and place of birth further account for the influence of seasonality and health at birth (Lokshin & Radyakin, 2012). Missing values on “born in clinic” are accounted for by including a missing indicator in the regression.
To measure climate exposures, we first extract data on monthly mean temperature and precipitation rate from the Climate Research Unit (CRU), a project of the University of East Anglia. CRU collects data from weather stations around the world and then uses a spatial interpolation approach to create a global gridded dataset at 0.5° resolution (Harris et al. 2020), a pixel size which is small relative to our provinces. We use the time-standardized shapefiles described above to extract the spatial mean of temperature and precipitation values in each month from 1981–2018. In each province, we then create running 9-month and 12-month means and standardize these into temperature and precipitation anomalies using the historical mean and the historical standard deviation in each province for each running length. Relative to raw climate values, standardized climate anomalies have multiple advantages for analyses of climatic impacts on health: they are locally-meaningful deviations from familiar conditions, they can be interpreted as exogenous shocks, they are stronger predictors of social outcomes, and they have been previously been significantly associated with population health outcomes (Gray & Wise, 2016; Nordkvelle, Rustad, & Salmivalli, 2017; Mueller et al. 2020; Thiede & Strube 2020; Nicholas et al. 2021). Though some studies have used alternative metrics to transform the distribution of rainfall, the distribution of precipitation z-scores for our sample is approximately normal, with a low skewness value 0.1.
To supplement our main monthly climate anomalies, which are extracted with all pixels weighted equally, we construct a parallel set of population-weighted anomalies based on gridded population data provided by the Center for International Earth Science Information Network. Derived from global census inputs, these data are currently available at five-year intervals for the period from 2000–2020, and can be downloaded at multiple spatial resolutions; we choose 0.5° resolution to match the pixel size of our existing CRU climate dataset (CIESIN, 2016). First, we calculate the proportion of the provincial population that resides in a given pixel, using the most proximate round of population data (2000, 2005, 2010, or 2015). Next, we multiply the corresponding temperature and precipitation values by this proportion, sum the values for all proportioned pixels in the province, and then repeat the process described above to build running means and standardize them into anomalies based on population-weighted historical values. The supplementary use of population-weighted anomalies in our analysis serves as a robustness check for our primary results, ensuring that our findings are not driven by extreme climate values in largely unpopulated portions of South Asia.
With the monthly climate measures constructed, we then link the nine-month anomalies to the prenatal period of each child (9 months before birth to the month before birth) based on their month of birth and province of residence, and similarly link the 12-month anomalies to the first (0–11 months) and second (12–23) year of life of each child. We account for seasonal variation among 9-month prenatal periods in our analyses using month of birth fixed effects as described below. In all, this generates six climate values for each child: the standardized temperature and precipitation anomalies observed in the prenatal period, the first year of life and the second year of life. These periods correspond to the first 1000 days of life, the key period of child development (Schwarzenberg & Georgieff, 2018). Due to a lack of data on migration in all but one of the rounds in our sample, we are unable to account for the potential movement of young children between provinces, thus introducing potential measurement error in our climate variables. However, in the single round for which data on interprovincial migration is available (Nepal 2016), only 62 of 1,397 children ages 2–5 had mothers who had lived in the current place of residence for less than five years and a previous place of residence that was in a different region, which is analogous to a different province in our study. This value is consistent with a large body of research showing that interprovincial mobility is quite low in South Asia and the Global South more broadly (Bell et al. 2015; Charles-Edwards et al. 2019).
We further supplement these monthly measures using data on daily maximum temperature and precipitation rate with a pixel size of 0.05°. These temperature (precipitation) data come from the Climate Hazards Group Infrared Temperature (Precipitation) with Stations (CHIRTS and CHIRPS, respectively) datasets. CHIRTS and CHIRPS are high resolution, semi-global (50°S-50°N) data products created by a combination of satellite estimates and in situ observations (Funk et al. 2015; Davenport et al. 2017; Funk et al. 2019). We extract these daily data using the same time-standardized shapefiles and process described above for the years 1983–2016. Because CHIRTS is currently only available up to 2016, we exclude children who turned age 2 after December 2016 (N=626) from the supplementary analysis including these measures. We use the CHIRPS and CHIRTS values to generate counts of the number of extreme days (extremely hot, extremely wet, extremely cold, and extremely dry) in each of the three developmental periods described above. In this study, a day is considered extremely hot if it is above the 95th percentile for temperatures in a given province, relative to the entire temperature record (1983–2016). Similarly, an extremely wet day must exceed the 95th percentile for precipitation relative to the same time period, whereas a cold day is below the 5th percentile and a dry day is any day with zero precipitation, the lower bound for this value. This supplementary specification serves as another robustness check of our primary results, which use CRU monthly anomalies, and includes twelve new variables for each child: a count of extreme hot, wet, cold, and dry days for each of the prenatal period, the first year of life, and the second year of life.
With the climate and survey data thus linked, we use a set of fixed effects regressions to examine how child height is influenced by temperature and precipitation while accounting for potential spatial and temporal confounders. Using CRU anomalies in Specification 1 and CHIRPS/CHIRTS extreme days in Specification 2, we model HAZ using linear regression and then stunting and severe stunting using logistic regression. Coefficients from logistic regression are presented as odds ratios, which can be interpreted as the multiplicative effects of a one unit increase in the predictor on the odds of the outcome. All models include the following predictors: the climate exposures defined above, the socio-demographic controls defined above, fixed effects for provinces and month of birth, and a linear time trend for the survey year. The inclusion of fixed effects for the province accounts for all baseline differences between provinces including historical climate, whereas the inclusion the of the time trend captures changes in the macro-context of child nutrition over time due to such processes as urbanization and development. We also correct for clustering at the level of the province and include sampling weights as described above, thereby accounting for non-independence within provinces and non-equal sampling probabilities. Using Specification 1 and focusing on HAZ, we subsequently extend this analysis by (1) adding the square of the anomalies (a quadratic specification), allowing the climate effects to be nonlinear, and (2) adding interactions with five socio-demographic characteristics, one set at a time, thus allowing these characteristics to modify the climate effects.
Results
Table 1 contains unweighted descriptive statistics for all analytical variables including child anthropometric outcomes (HAZ, stunting, and severe stunting), climate exposures (anomalies and extreme days for the three relevant developmental periods as well as raw climate values for context), and socio-demographic controls. Several socio-demographic characteristics point to high rates of poverty and deprivation in this sample. For instance, 38% of children had mothers with no formal education, and only a small majority of children (56%) had access to improved toilet infrastructure. Additionally, 73% of children were in locations classified as rural by DHS, suggesting a reliance on agriculture for family income and food security. It is also notable that the means for both precipitation and temperature anomalies are positive for all identified exposure periods, implying that recent conditions in South Asia have been both somewhat hotter and wetter than their historical means, though with many values in the cool and dry range. There is also an unequal distribution of extreme days (Specification 2) throughout our sample, particularly in relation to precipitation. Because a dry day must be defined as any day with zero precipitation, dry days are much more common than wet days. Consequently, the average child in our sample experienced 90 extremely dry days in year one and only 19 extremely wet days. Hot and cold days are more even in this respect; the same child experienced 20 hot days and 21 cold days in year one. Perhaps most importantly, Table 1 reveals that the average child in our sample exhibits a height-for-age that is 1.88 standard deviations below the mean for other children their age. Furthermore, there are very high rates of child stunting across our sample, with half (47%) of all children classified as stunted and 21% as severely stunted.
Table 1.
Descriptive statistics for the predictors and outcomes (N = 222,572).
| Variable | Mean | Std. Dev. | Min. | Max. |
|---|---|---|---|---|
| Demographics – Child | ||||
| Height for age (HAZ) | −1.88 | 1.53 | −6 | 5.99 |
| Stunted | 0.47 | 0.50 | 0 | 1 |
| Severely stunted | 0.21 | 0.41 | 0 | 1 |
| Child’s age (months) | 40.58 | 10.34 | 24 | 59 |
| Child is a girl | 0.48 | 0.50 | 0 | 1 |
| Child is a twin | 0.01 | 0.11 | 0 | 1 |
| Child’s birth order | 2.50 | 1.70 | 1 | 17 |
| Born in clinic | 0.71 | 1.15 | 0 | 1 |
| Demographics – Family | ||||
| Mother’s age at child’s birth | 27.86 | 5.37 | 15 | 49 |
| Mother is married | 0.98 | 0.13 | 0 | 1 |
|
Mother’s caste
(India only: N = 184,177) |
||||
| Scheduled caste | 0.18 | 0.39 | 0 | 1 |
| Scheduled tribe | 0.19 | 0.39 | 0 | 1 |
| Other | 0.63 | 0.48 | 0 | 1 |
| Mother’s education | ||||
| None (reference) | 0.38 | 0.48 | 0 | 1 |
| Primary | 0.17 | 0.37 | 0 | 1 |
| Secondary | 0.38 | 0.49 | 0 | 1 |
| Higher | 0.08 | 0.27 | 0 | 1 |
| Children ever born | 2.92 | 1.72 | 1 | 17 |
| Improved toilet | 0.56 | 0.51 | 0 | 1 |
| Rural | 0.73 | 0.44 | 0 | 1 |
| Climate - anomalies | ||||
| Prenatal precipitation (mm) | 109.17 | 63.85 | 0.60 | 448.65 |
| Prenatal temperature (C) | 23.60 | 5.43 | −2.38 | 30.91 |
| 1st year precipitation (mm) | 108.14 | 50.77 | 1.84 | 340.72 |
| 1st year temperature (C) | 23.45 | 5.19 | 0.09 | 28.47 |
| 2nd year precipitation (mm) | 106.57 | 50.38 | 1.84 | 335.39 |
| 2nd year temperature (C) | 23.47 | 5.17 | 0.90 | 28.36 |
| Prenatal precipitation anomaly | 0.10 | 1.03 | −2.32 | 3.20 |
| Prenatal temperature anomaly | 0.13 | 0.92 | −2.26 | 2.43 |
| 1st year precipitation anomaly | 0.16 | 0.92 | −3.61 | 3.10 |
| 1st year temperature anomaly | 0.05 | 0.64 | −2.13 | 1.94 |
| 2nd year precipitation anomaly | 0.06 | 0.91 | −3.57 | 3.07 |
| 2nd year temperature anomaly | 0.07 | 0.49 | −1.71 | 2.32 |
| Climate – extreme days | ||||
| Prenatal wet days | 15.30 | 7.57 | 0 | 40 |
| Prenatal dry days | 68.21 | 39.99 | 1 | 247 |
| Prenatal hot days | 15.11 | 10.87 | 0 | 51 |
| Prenatal cold days | 14.23 | 9.22 | 0 | 45 |
| 1st year wet days | 20.11 | 5.92 | 0 | 41 |
| 1st year dry days | 87.20 | 50.49 | 4 | 308 |
| 1st year hot days | 19.94 | 9.19 | 0 | 53 |
| 1st year cold days | 20.22 | 7.86 | 0 | 60 |
| 2nd year wet days | 19.15 | 5.99 | 1 | 41 |
| 2nd year dry days | 84.12 | 51.74 | 3 | 308 |
| 2nd year hot days | 21.88 | 8.50 | 0 | 60 |
| 2nd year cold days | 21.04 | 9.57 | 0 | 60 |
Figure 1 shows the mean HAZ of children in each study province at the time of the most recent DHS interview, spanning 2014–2018 across countries. Notably, all provinces display mean HAZ values less than zero, meaning that the average child in our sample—regardless of where they live—is considerably shorter than the WHO reference populations (WHO, 2014). Across the sample, only six Indian provinces (Jammu and Kashmir, Punjab and Chandigarh, Arunachal Pradesh, Goa, Tamil Nadu, and Kerala and Lakshadweep) have an average HAZ greater than −1.5, while every country has at least two provinces in which the average child is considered stunted (HAZ < −2). The two provinces with the lowest mean HAZ values both fall in Pakistan (including the major city of Karachi), and are home to tens of millions of people.
Table 2 displays the effects of climate anomalies (Specification 1), extreme days (Specification 2), and the controls (displayed for Specification 1 only) on HAZ, stunting, and severe stunting in South Asia for children aged 2–5. The climate effects are jointly significant for all three outcomes under both climate specifications. Under Specification 1, neither temperature nor precipitation anomalies experienced during the prenatal period have a significant effect on child height-for-age at ages 2–5, and the impact instead occurs during the first and second years of life. A one unit increase in the precipitation anomaly (equivalent to one standard deviation of precipitation) during the first year of life decreases HAZ by 2.4% (p=0.016) increases the odds of stunting and severe stunting by 3.1% (p=0.001) and 2.4% (p=0.038), respectively. Meanwhile, every additional unit of second year precipitation increases the odds of severe stunting by 3.1% (p=0.033); however there is not a significant effect of second year precipitation on either HAZ or stunting. In contrast to precipitation’s detrimental impacts, we find a marginally and inconsistently significant positive relationship between anomalous heat during the first and second years of life and improved nutritional outcomes at ages 2–5 years. One additional unit of heat decreases the likelihood of stunting by 3.4% (p=0.078) and increases HAZ by 2.7% (p=0.055) when the anomaly occurs during the first and second years, respectively. Appendix Table 1, which uses our supplemental population-weighted monthly climate measures, reveals similar effects of all anomalies on height attainment.
Table 2.
Main regression results with alternative climate specifications.
| Variable | HAZ | Stunting | Severe Stunting |
|---|---|---|---|
| OLS/coeff. | Logit/OR | Logit/OR | |
| Climate – anomalies 1 | |||
| Prenatal precip. anomaly | −0.013 | 1.007 | 0.995 |
| Prenatal temp. anomaly | −0.009 | 0.982 | 0.971 |
| 1st year precip. anomaly | −0.024* | 1.031** | 1.024* |
| 1st year temp. anomaly | 0.018 | 0.966+ | 0.965 |
| 2nd year precip. anomaly | −0.012 | 1.019 | 1.031* |
| 2nd year temp. anomaly | 0.027+ | 0.977 | 0.988 |
| Demographics – Child | |||
| Child’s age (months) | −0.020*** | 1.025*** | 1.006 |
| Child’s age squared | 0.000*** | 1.000*** | 1.000* |
| Child is a girl | −0.007 | 1.032+ | 1.022 |
| Child is a twin | −0.230*** | 1.330*** | 1.480*** |
| Child’s birth order | −0.102*** | 1.131*** | 1.126*** |
| Born in clinic | 0.103*** | 0.871*** | 0.838*** |
| Demographics – Family | |||
| Mother’s age at child’s birth | 0.075*** | 0.911*** | 0.921*** |
| Mother’s age squared | −0.001*** | 1.001*** | 1.001*** |
| Mother’s education level | |||
| Primary | 0.124*** | 0.851*** | 0.765*** |
| Secondary | 0.367*** | 0.607*** | 0.533*** |
| Higher | 0.710*** | 0.375*** | 0.329*** |
| Mother is married | 0.017 | 0.946 | 0.996 |
| Children ever born | 0.010 | 0.992 | 1.002 |
| Improved toilet | 0.199*** | 0.757*** | 0.761*** |
| Rural | −0.084** | 1.096** | 1.009 |
| N | 222572 | 222572 | 222572 |
| Joint test of climate effects | 5.10*** | 27.31*** | 23.38*** |
| Climate – extreme days 2 | |||
| Prenatal wet days | −0.003** | 1.001 | 1.003 |
| Prenatal dry days | −0.001 | 1.000 | 1.000 |
| Prenatal hot days | −0.001 | 1.000 | 1.001 |
| Prenatal cold days | 0.000 | 1.000 | 0.999 |
| 1st year wet days | −0.006*** | 1.006*** | 1.004*** |
| 1st year dry days | −0.003*** | 1.002** | 1.002* |
| 1st year hot days | 0.001 | 0.999 | 0.999 |
| 1st year cold days | 0.000 | 0.998 | 0.996** |
| 2nd year wet days | −0.001 | 1.000 | 1.000 |
| 2nd year dry days | 0.001* | 0.998** | 0.998* |
| 2nd year hot days | 0.000 | 1.000 | 1.000 |
| 2nd year cold days | −0.001 | 1.001 | 1.001 |
| N | 221946 | 221946 | 221946 |
| Joint test of climate effects | 13.55*** | 151.48*** | 53.03*** |
p<0.10,
p<0.05,
p<0.01,
p<0.001
Anomalies specification: Constant, province indicators, month of birth indicators, born in clinic missing indicator, and a time trend term are included in the model but not shown.
Extreme days specification: Controls, constant, province indicators, month of birth indicators, missing indicators, and the time trend term are included in the model but not shown.
Consistent with Specification 1, the extreme days specification reveals that height-for-age is more reactive to precipitation shocks than to temperature extremes. Most notably, extreme wet days and dry days during the first year of life predict lower HAZ as well as higher stunting and severe stunting. When exposure occurs in the second year, however, dry days tend to improve nutritional outcomes—every additional dry day decreases the average child’s likelihood of stunting by 0.2% (p=0.005). We also find that every additional wet day during the prenatal period decreases the average child’s HAZ by 0.3% (p=0.003), though this effect does not carry over to stunting and severe stunting. Finally, the only temperature effect we observe under Specification 2 is a 0.4% (p=0.009) reduction in severe stunting odds with every additional cold day experienced during the first year of life.
In addition to these climate effects, Table 2 also reveals that many of our control variables also have statistically significant effects on HAZ, stunting, and severe stunting in the expected directions. Indicators of wealth, such as maternal education, access to health clinics for childbirth, and access to improved toilets, predict higher HAZ and lower rates of stunting and severe stunting. The prevalence of child stunting and severe stunting also significantly declines with mother’s age. With each additional year of a mother’s age at childbirth, her child is 8.9% less likely to be stunted when they are 2–5 years old (p<0.001). Finally, it is notable that the children of rural households display an 8.4% lower HAZ (p=0.002) and are 9.6% more likely to be stunted than their urban counterparts (p=0.001), though the significance of this relationship does not extend to severe stunting.
Specification 1 implicitly assumes that climate’s effects on child nutrition are linear. For instance, if a rise in precipitation increases the probability of stunting then a decline in precipitation must decrease it. To relax this assumption, Figure 2 displays predicted probabilities from a supplemental specification that includes a squared term for each climate anomaly, e.g. a quadratic transformation, focusing on HAZ. Here, we display only those results for which the linear and squared terms are jointly significant, in this case for temperature anomalies in the first and second years of life. The first panel of Figure 2 shows that both first-year temperature extremes tend to decrease children’s HAZ, though the margin of error is greater for cold temperatures than for heat as the former have been relatively uncommon during our study period. The effect of anomalous second-year heat on HAZ is largely similar to that of first-year heat, but extreme cold in the second year of life appears to have an even more harmful impact on height attainment (note that the margin of error is relatively wide as before).
Figure 2.
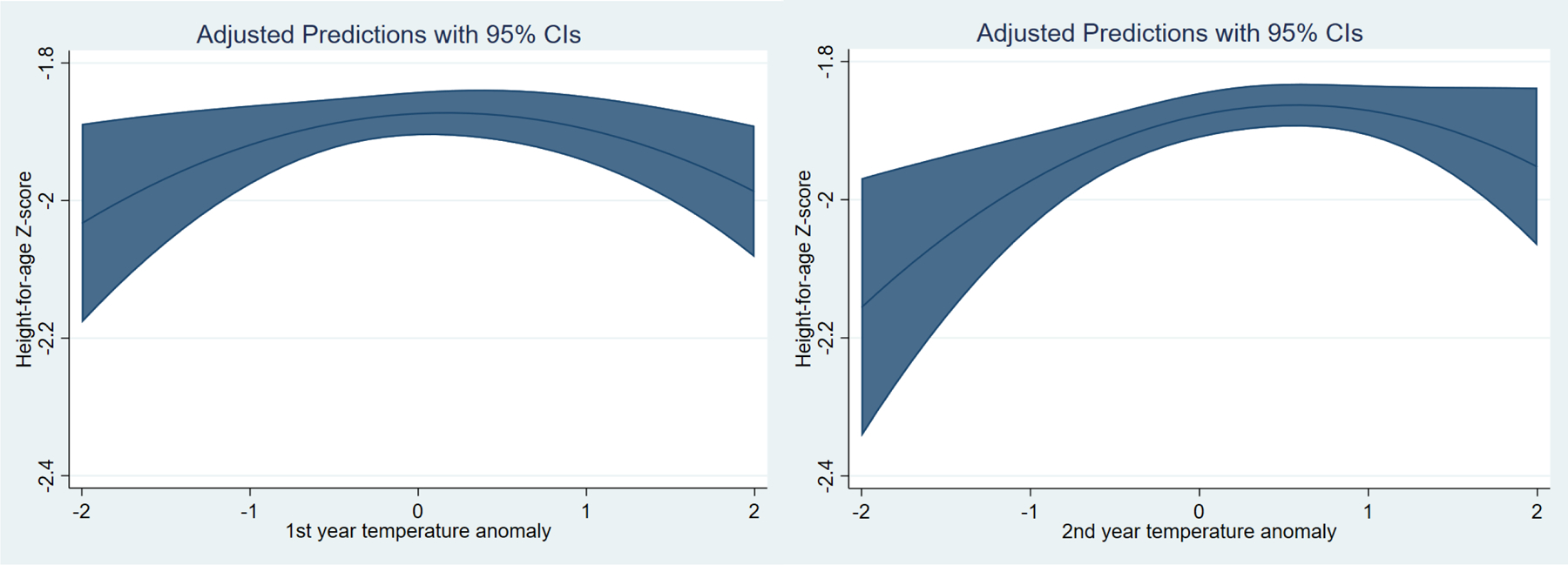
Statistically significant nonlinear effects of climate anomalies on HAZ.
To provide insight into heterogeneity in the effects from Specification 1, we also test for interactions between climate anomalies and five key socio-demographic variables (child’s sex, household toilet quality, mother’s education, country of residence, and caste/tribe among Indian children), again focusing on HAZ as the outcome (Table 3). Joint significance tests reveal that each of these variables significantly modifies the impacts of climate on HAZ. Interactions with urbanicity and between temperature and precipitation were also tested but were not jointly significant. First, anomalous prenatal precipitation modifies the climate effect on HAZ for girls only, who have a 2.7% (p=0.026) greater HAZ on average than girls who experienced no prenatal anomalies. First year precipitation, meanwhile, causes a marginally significant decrease in HAZ for both boys and girls. After birth, boys appear to benefit from higher-than-average temperatures—in particular, there is a 4.2% (p=0.014) increase in average HAZ among boys exposed two heat in year two. Next, while children with improved toilet systems are almost entirely unaffected by climate anomalies in any exposure period, children with unimproved toilets tend to benefit from heat anomalies and suffer from exposure to extreme precipitation after birth. Though each additional unit of precipitation during the prenatal period causes a 2.2% (p=0.048) increase in average HAZ for 2–5 year-olds lacking adequate toilet access, it has the opposite effect in the first year of life, decreasing HAZ by 3.2% (p=0.011). Each unit of the second-year heat anomaly, on the other hand, increases HAZ by 4.9% (p=0.043) for the same children. In keeping with these trends, the height-for-age of children with no maternal education (another indicator of poverty) are most reactive to climate anomalies. Compared with the children of higher-educated mothers, those of lower-educated mothers tend to be more vulnerable to the negative effects of extreme precipitation in the first year of life, and benefit more from the positive effects of heat across all developmental periods.
Table 3.
Statistically significant interactive effects of climate anomalies on HAZ.
| Variable | Prenatal anomalies | 1st year anomalies | 2nd year anomalies | Joint test | |||
|---|---|---|---|---|---|---|---|
| Precip. | Temp. | Precip. | Temp. | Precip. | Temp. | ||
| Child’s sex | p=0.026 | ||||||
| Boy | 0.011 | 0.013 | −0.021 + | 0.031 + | −0.012 | 0.042 * | |
| Girl | 0.027 * | 0.000 | −0.018 + | −0.005 | −0.011 | 0.033 | |
| Toilet quality | p<0.001 | ||||||
| Unimproved | 0.022 * | 0.024 + | −0.032 * | 0.019 | −0.026 + | 0.049 * | |
| Improved | 0.015 + | −0.011 | −0.007 | 0.010 | 0.003 | 0.022 | |
| Mother’s education | p<0.001 | ||||||
| None | 0.034 * | 0.033 + | −0.028 * | 0.038 * | −0.013 | 0.065 * | |
| Primary | 0.020 + | −0.010 | −0.012 | −0.001 | −0.004 | 0.020 | |
| Secondary | 0.000 | −0.008 | −0.007 | 0.002 | −0.022 | 0.020 | |
| Higher | 0.040 * | −0.039 ** | −0.029 | 0.008 | 0.020 | −0.021 | |
| Country of residence | p<0.001 | ||||||
| Bangladesh | 0.021 | −0.011 | 0.042 * | 0.011 | 0.042 + | 0.060 | |
| India | 0.018 + | 0.006 | −0.022 * | 0.026 | −0.017 | 0.059 ** | |
| Nepal | 0.015 | 0.031 | 0.003 | 0.028 | 0.004 | −0.055 * | |
| Pakistan | −0.048 | −0.011 | −0.086 * | −0.215 *** | −0.002 | −0.067 + | |
| Caste/Tribe | p<0.001 | ||||||
| Scheduled Caste | 0.007 | 0.008 | −0.037 *** | 0.018 | −0.026 | 0.068 | |
| Scheduled Tribe | 0.028 + | 0.004 | −0.038 | 0.056 | −0.071 | −0.075 | |
| Other | 0.022 * | 0.000 | −0.015 | 0.046 * | −0.009 | 0.076 *** | |
Each header presents results from one regression that includes interactions between that variable and the climate anomalies. The regressions additionally include all terms from specification 1 in Table 2. Caste/tribe includes India only (N=184177).
p<0.10,
p<0.05,
p<0.01,
p<0.001.
Additionally, the interaction between climate and country of residence reveals that climate’s effects on child height-for-age are most pronounced in India and Pakistan. From these results, it appears that the second-year temperature effect observed in previous interactions can be attributed to India, where a one unit increase in second-year heat corresponds to an increase in HAZ by 5.9% (p=0.006). This may reflect the fact that India constitutes the largest fraction of our total sample (184,177 out of 222,572 observations). In contrast to the benefits of warm temperatures observed in India, we find that exposure to anomalous heat has a strong detrimental health effect in Pakistan. This effect is particularly strong in the first year of life, when an additional unit of temperature anomaly reduces the average Pakistani child’s HAZ by 21.5% (p<0.000). Finally, the interaction between climate anomalies and caste/tribe in India (N=184,176) reveals that children of mothers belonging to scheduled castes are—like other under-resourced demographics observed in Table 3—especially vulnerable to the detrimental effects of extreme rain in the first year of life, when every additional unit of precipitation anomaly reduces HAZ by 3.7% (p=0.001). Furthermore, children of mothers belonging to scheduled castes and tribes do not experience the same benefits of some climate anomalies extended to other Indian children, whose HAZ significantly increases after exposure to prenatal precipitation anomalies and temperature anomalies in both the first and second years of life.
Discussion
Our results show that precipitation extremes during the first year of life decrease height-for-age and increase stunting for children in South Asia. This extends previous findings by Dimitrova & Bora (2020) and Dimitrova & Muttarak (2020) that were specific to India and did not account for correlated changes in temperature. The wide-reaching vulnerability to precipitation shocks in the first year may reflect the delicacy of nutritional health immediately after birth, when maternal and infant nutrition are still very closely linked and infants are being exposed to complex disease environments for the first time. For instance, infants ages 0–1 years may be more likely than other children to suffer from diarrheal disease and subsequent impaired nutrition after periods of heavy rainfall, which can contaminate drinking water (Carlton et al. 2014; Dimitrova & Bora 2020). We also find that the impacts of first year precipitation shocks are most pronounced in children who live in India or Pakistan, whose mothers have no education or belong to a disadvantaged Indian caste, or who do not have access to an adequate toilet. The latter three characteristics, all indicators of low socio-economic status, are likely correlated with increased odds of exposure to infectious disease. Indian children may be similarly vulnerable due to high rates of open defecation. In 2012, the WHO estimated that India accounted for 90% of the nearly 700 million people who practice open defecation in South Asia, and nearly 50% of Indian children in our sample had inadequate toilet access (UNICEF & WHO, 2012). Taken together, these results support previous connections drawn between flooding and undernutrition in this region (Del Ninno & Lundberg 2005; Tiwari et al. 2016) and complement existing evidence that sanitation access and social status play a significant role in determining nutritional outcomes in this region (Coffey et al. 2015; Khanna & Das, 2015; Spears et al. 2018).
Temperature anomalies appear to have weaker effects on child health than precipitation, but we find evidence that both hot and cold extremes in the first two years of life undermine child nutritional health (Figure 2). We also find intriguing evidence of subpopulations of children that benefit from moderate warming, particularly after birth. For children with unimproved toilets and mothers with no education—the same children who were most at risk of stunting after exposure to extreme rain—anomalous heat in years one and two increased HAZ. Temperature’s impacts on nutrition also vary significantly by country; Pakistani children in our sample are highly vulnerable to first-year heat, while Indian children may benefit from moderate warming. These varying consequences of temperature are consistent with other studies that have found child height to be both positively and negatively associated with temperature anomalies in different periods and contexts, possibly reflecting the fact that initial warming may result in some benefits for local agriculture (Nicholas et al. 2021; Randell et al. 2020). Indeed, the existing literature on climate change’s agricultural impacts in this region notes climate change’s mixed effects on South Asian crop yields to date (Ray et al. 2019). As temperatures continue to increase, however, the harmful effects of climate change on agricultural production and health will likely become more pronounced, likely overwhelming the effects of moderate warming that we observe.
Our results also provide important evidence that increasing access to basic resources can help protect vulnerable populations against climate change (Jongman et al. 2015; Mueller at al. 2020). We show that children with improved toilet facilities or with mothers who completed primary education were almost completely protected against climate shocks, similar to the results found by Dimitrova & Muttarak (2020) using a subset of the same data. Previously, Mulmi et al. (2016) also showed that access to improved toilets completely protected children’s height-for-age against vegetation greenness shocks in Nepal. These findings strongly support the idea that the widespread provision of basic sanitation and education services in South Asia will increase resilience to climate change. However, this result may not be globally generalizable, as similar studies in other settings have at times found that urban or otherwise advantaged populations were actually more exposed to climate-induced shocks to child health and well-being (Randell & Gray 2019; Thiede & Strube 2020; Nicholas et al. 2021). This may reflect additional costs of climate change in those contexts that accrue to areas with less vegetation or to populations more exposed to food price fluctuations.
Our study also emphasizes the power and utility of harmonized data for answering subcontinental-scale research questions of global importance. Via the IPUMS-DHS interface (Boyle et al. 2019), all 18 rounds of survey data that we use here can be downloaded as a single harmonized dataset with consistent formatting and variable names, accompanied by the time-standardized shapefiles that we use to link 220 thousand children to their climate exposures. It is also possible to download linked climate data for some survey rounds from the same interface, and to download linked CRU climate data from the connected IPUMS-Terra interface (Ruggles et al. 2018). Additionally, the main DHS project provides GPS locations for many survey rounds and has extracted their own publicly-available geospatial and environmental data for these locations (Mayala et al. 2018). These tools, and related tools for census data available from the IPUMS-International project (Minnesota Population Center 2018), represent a revolution in data availability on health and development for the Global South, and will be featured in an increasing fraction of climate vulnerability research going forward.
Appendix Table 1.
Alternative main regression results using population-weighted monthly climate anomalies.
| Variable | HAZ | Stunting | Severe Stunting |
|---|---|---|---|
| OLS/coeff. | Logit/OR | Logit/OR | |
| Climate – anomalies | |||
| Prenatal precip. anomaly | −0.010 | 1.003 | 0.991 |
| Prenatal temp. anomaly | −0.013 | 0.985 | 0.975 |
| 1st year precip. anomaly | −0.021* | 1.027** | 1.022* |
| 1st year temp. anomaly | 0.018 | 0.964+ | 0.967 |
| 2nd year precip. anomaly | −0.011 | 1.017 | 1.027+ |
| 2nd year temp. anomaly | 0.028* | 0.974+ | 0.983 |
| Demographics – Child | |||
| Child’s age (months) | −0.019*** | 1.025*** | 1.006 |
| Child’s age squared | 0.000*** | 1.000*** | 1.000* |
| Child is a girl | −0.007 | 1.032+ | 1.022 |
| Child is a twin | −0.230*** | 1.330*** | 1.480*** |
| Child’s birth order | −0.102*** | 1.131*** | 1.126*** |
| Born in clinic | 0.103*** | 0.871*** | 0.838*** |
| Demographics – Family | |||
| Mother’s age at child’s birth | 0.075*** | 0.911*** | 0.921*** |
| Mother’s age squared | −0.001*** | 1.001*** | 1.001*** |
| Mother’s education level | |||
| Primary | 0.124*** | 0.851*** | 0.765*** |
| Secondary | 0.368*** | 0.607*** | 0.532*** |
| Higher | 0.710*** | 0.375*** | 0.329*** |
| Mother is married | 0.018 | 0.946 | 0.996 |
| Children ever born | 0.010 | 0.992 | 1.002 |
| Improved toilet | 0.199*** | 0.757*** | 0.761*** |
| Rural | −0.084** | 1.095** | 1.009 |
| N | 222572 | 222572 | 222572 |
| Joint test of climate effects | 5.37*** | 29.53*** | 23.22*** |
p<0.10,
p<0.05,
p<0.01,
p<0.001
Appendix Table 2.
Main regression results with alternative climate specifications. Standard errors and confidence intervals included for linear and logistic regressions, respectively.
| Variable | HAZ | Stunting | Severe Stunting |
|---|---|---|---|
| OLS/coeff. | Logit/OR | Logit/OR | |
| Climate – anomalies 1 | |||
| Prenatal precip. anomaly | −0.013 (0.012) |
1.007
[−0.014, 0.027] |
0.995
[−0.050, 0.041] |
| Prenatal temp. anomaly | −0.009 (0.019) |
0.982
[−0.069, 0.033] |
0.971
[−0.095, 0.037] |
| 1st year precip. anomaly | −0.024* (0.009) |
1.031
**
[0.012, 0.049] |
1.024
*
[0.001, 0.047] |
| 1st year temp. anomaly |
0.018
(0.021) |
0.966
+
[−0.073, 0.004] |
0.965
[−0.086, 0.014] |
| 2nd year precip. anomaly | −0.012 (0.012) |
1.019
[−0.007, 0.043] |
1.031
*
[0.002, 0.058] |
| 2nd year temp. anomaly |
0.027
+
(0.014) |
0.977
[−0.051, 0.005] |
0.988
[−0.050, 0.025] |
| Demographics – Child | |||
| Child’s age (months) | −0.020*** (0.004) |
1.025
***
[0.015, 0.035] |
1.006
[−0.006, 0.019] |
| Child’s age squared |
0.000
***
(0.000) |
1.000
***
[0.000, 0.000] |
1.000
*
[−0.000, 0.000] |
| Child is a girl | −0.007 (0.011) |
1.032
+
[−0.004, 0.067] |
1.022
[−0.019, 0.062] |
| Child is a twin | −0.230*** (0.230) |
1.330
***
[0.154, 0.416] |
1.480
***
[0.265, 0.519] |
| Child’s birth order | −0.102*** (0.012) |
1.131
***
[0.080, 0.165] |
1.126
***
[0.077, 0.161] |
| Born in clinic |
0.103
***
(0.023) |
0.871
***
[−0.212, −0.064] |
0.838
***
[−0.238, −0.116] |
| Demographics – Family | |||
| Mother’s age at child’s birth |
0.075
***
(0.007) |
0.911
***
[−0.115, −0.072] |
0.921
***
[−0.103, −0.063] |
| Mother’s age squared | −0.001*** (0.000) |
1.001
***
[0.001, 0.001] |
1.001
***
[0.001, 0.001] |
| Mother’s education level | |||
| Primary |
0.124
***
(0.018) |
0.851
***
[−0.208, −0.115] |
0.765
***
[−0.320, −0.217] |
| Secondary |
0.367
***
(0.027) |
0.607
***
[−0.561, −0.439] |
0.533
***
[−0.683, −0.577] |
| Higher |
0.710
***
(0.054) |
0.375
***
[−1.093, −0.867] |
0.329
***
[−1.285, −0.938] |
| Mother is married |
0.017
(0.050) |
0.946
[−0.168, 0.058] |
0.996
[−0.121, 0.113] |
| Children ever born |
0.010
(0.014) |
0.992
[−0.055, 0.039] |
1.002
[−0.041, 0.046] |
| Improved toilet |
0.199
***
(0.034) |
0.757
***
[−0.343, −0.213] |
0.761
***
[−0.343, −0.202] |
| Rural | −0.084** (0.025) |
1.096
**
[0.036, 0.147] |
1.009
[−0.061, 0.079] |
| N | 222572 | 222572 | 222572 |
| Joint test of climate effects | 5.10*** | 27.31*** | 23.38*** |
| Climate – extreme days 2 | |||
| Prenatal wet days | −0.003** (0.001) |
1.001
[-0.001, 0.003] |
1.003
[−0.001, 0.006] |
| Prenatal dry days | −0.001 (0.001) |
1.000
[-0.001, 0.002] |
1.000
[−0.001, 0.001] |
| Prenatal hot days | −0.001 (0.001) |
1.000
[-0.002, 0.003] |
1.001
[−0.003, 0.005] |
| Prenatal cold days |
0.000
(0.001) |
1.000
[-0.003, 0.002] |
0.999
[−0.005, 0.002] |
| 1st year wet days | −0.006*** (0.001) |
1.006
***
[0.003, 0.008] |
1.004
***
[0.002, 0.007] |
| 1st year dry days | −0.003*** (0.001) |
1.002
**
[0.001, 0.003] |
1.002
*
[0.000, 0.004] |
| 1st year hot days |
0.001
(0.001) |
0.999
[-0.004, 0.001] |
0.999
[−0.005, 0.003] |
| 1st year cold days |
0.000
(0.001) |
0.998
[-0.004, 0.001] |
0.996
**
[−0.006, −0.001] |
| 2nd year wet days | −0.001 (0.001) |
1.000
[-0.003, 0.003] |
1.000
[−0.004, 0.005] |
| 2nd year dry days |
0.001
*
(0.001) |
0.998
**
[−0.003, −0.001] |
0.998
*
[−0.003, −0.000] |
| 2nd year hot days |
0.000
(0.001) |
1.000
[-0.002, 0.001] |
1.000
[−0.001, 0.002] |
| 2nd year cold days | −0.001 (0.001) |
1.001
[-0.001, 0.003] |
1.001
[−0.002, 0.003] |
| N | 221946 | 221946 | 221946 |
| Joint test of climate effects | 13.55*** | 151.48*** | 53.03*** |
p<0.10,
p<0.05,
p<0.01,
p<0.001
Anomalies specification: Constant, province indicators, month of birth indicators, born in clinic missing indicator, and a time trend term are included in the model but not shown.
Extreme days specification: Controls, constant, province indicators, month of birth indicators, missing indicators, and the time trend term are included in the model but not shown.
Appendix Table 3.
Statistically significant interactive effects of climate anomalies on HAZ. Standard errors included.
| Variable | Prenatal anomalies | 1st year anomalies | 2nd year anomalies | Joint test | |||
|---|---|---|---|---|---|---|---|
| Precip. | Temp. | Precip. | Temp. | Precip. | Temp. | ||
| Child’s sex | p=0.026 | ||||||
| Boy |
0.011
(0.007) |
0.013
(0.008) |
−0.021+ (0.011) |
0.031
+
(0.018) |
−0.012 (0.013) |
0.042
*
(0.017) |
|
| Girl |
0.027
*
(0.012) |
0.000
(0.013) |
−0.018+ (0.009) |
−0.005 (0.022) |
−0.011 (0.016) |
0.033
(0.022) |
|
| Toilet quality | p<0.001 | ||||||
| Unimproved |
0.022
*
(0.011) |
0.024
+
(0.014) |
−0.032* (0.012) |
0.019
(0.020) |
−0.026+ (0.015) |
0.049
*
(0.024) |
|
| Improved |
0.015
+
(0.008) |
−0.011 (0.010) |
−0.007 (0.012) |
0.010
(0.019) |
0.003
(0.014) |
0.022
(0.017) |
|
| Mother’s education | p<0.001 | ||||||
| None |
0.034
*
(0.013) |
0.033
+
(0.020) |
−0.028* (0.013) |
0.038
*
(0.018) |
−0.013 (0.016) |
0.065
*
(0.028) |
|
| Primary |
0.020
+
(0.011) |
−0.010 (0.013) |
−0.012 (0.012) |
−0.001 (0.020) |
−0.004 (0.011) |
0.020
(0.021) |
|
| Secondary |
0.000
(0.007) |
−0.008 (0.011) |
−0.007 (0.014) |
0.002
(0.022) |
−0.022 (0.015) |
0.020
(0.015) |
|
| Higher |
0.040
*
(0.018) |
−0.039** (0.012) |
−0.029 (0.023) |
0.008
(0.034) |
0.020
(0.034) |
−0.021 (0.064) |
|
| Country of residence | p<0.001 | ||||||
| Bangladesh |
0.021
(0.027) |
−0.011 (0.024) |
0.042
*
(0.021) |
0.011
(0.026) |
0.042
+
(0.024) |
0.060
(0.016) |
|
| India |
0.018
+
(0.009) |
0.006
(0.010) |
−0.022* (0.011) |
0.026
(0.021) |
−0.017 (0.014) |
0.059
**
(0.022) |
|
| Nepal |
0.015
(0.021) |
0.031
(0.030) |
0.003
(0.015) |
0.028
(0.032) |
0.004
(0.011) |
−0.055* (0.025) |
|
| Pakistan | −0.048 (0.036) |
−0.011 (0.016) |
−0.086* (0.038) |
−0.215*** (0.021) |
−0.002 (0.019) |
−0.067+ (0.036) |
|
| Caste/Tribe | p<0.001 | ||||||
| Scheduled Caste |
0.007
(0.011) |
0.008
(0.022) |
−0.037*** (0.009) |
0.018
(0.031) |
−0.026 (0.018) |
0.068
(0.046) |
|
| Scheduled Tribe |
0.028
+
(0.015) |
0.004
(0.021) |
−0.038 (0.040) |
0.056
(0.037) |
−0.071 (0.044) |
−0.075 (0.058) |
|
| Other |
0.022
*
(0.011) |
0.000
(0.008) |
−0.015 (0.011) |
0.046
*
(0.020) |
−0.009 (0.012) |
0.076
***
(0.021) |
|
Each header presents results from one regression that includes interactions between that variable and the climate anomalies. The regressions additionally include all terms from specification 1 in Table 2. Caste/tribe includes India only (N=184177).
p<0.10,
p<0.05,
p<0.01,
p<0.001.
References
- Alderman H, & Headey D (2018). The timing of growth faltering has important implications for observational analyses of the underlying determinants of nutrition outcomes. PloS one, 13(4), e0195904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderman H, Hoddinott J, & Kinsey B (2006). Long term consequences of early childhood malnutrition. Oxford economic papers, 58(3), 450–474. [Google Scholar]
- Arnell NW, Brown S, Gosling SN, Gottschalk P, Hinkel J, Huntingford C, & Osborne TM (2016). The impacts of climate change across the globe: a multi-sectoral assessment. Climatic Change, 134(3), 457–474. [Google Scholar]
- Bell M, Charles-Edwards E, Ueffing P, Stillwell J, Kupiszewski M, & Kupiszewska D (2015). Internal migration and development: Comparing migration intensities around the world. Population and Development Review, 41(1), 33–58. [Google Scholar]
- Boyle EH; King M; Sobek M (2019). IPUMS-Demographic and Health Surveys: Version 7. Minnesota Population Center and ICF International, 10.18128/D080.V7 [DOI] [Google Scholar]
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, … & Uauy R (2013). Maternal and child undernutrition and overweight in low-income and middle-income countries. The lancet, 382(9890), 427–451. [DOI] [PubMed] [Google Scholar]
- Burke M, Hsiang SM, & Miguel E (2015). Global non-linear effect of temperature on economic production. Nature, 527(7577), 235. [DOI] [PubMed] [Google Scholar]
- Carlton EJ, Eisenberg JN, Goldstick J, Cevallos W, Trostle J, & Levy K (2014). Heavy rainfall events and diarrhea incidence: the role of social and environmental factors. American journal of epidemiology, 179(3), 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for International Earth Science Information Network - CIESIN - Columbia University. (2016). Gridded Population of the World, Version 4 (GPWv4): Population Count. Palisades, NY: NASA Socioeconomic Data and Applications Center (SEDAC). 10.7927/H4X63JVC. [DOI] [Google Scholar]
- Challinor AJ, Watson J, Lobell DB, Howden SM, Smith DR, & Chhetri N (2014). A meta-analysis of crop yield under climate change and adaptation. Nature Climate Change, 4(4), 287. [Google Scholar]
- Charles-Edwards E, Bell M, Bernard A, & Zhu Y (2019). Internal migration in the countries of Asia: Levels, ages and spatial impacts. Asian Population Studies, 15(2), 150–171. [Google Scholar]
- Cooper MW, Brown ME, Hochrainer-Stigler S, Pflug G, McCallum I, Fritz S, … & Zvoleff A (2019). Mapping the effects of drought on child stunting. Proceedings of the National Academy of Sciences, 116(35), 17219–17224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport F, Grace K, Funk C, & Shukla S (2017). Child health outcomes in sub-Saharan Africa: A comparison of changes in climate and socio-economic factors. Global Environmental Change, 46, 72–87. [Google Scholar]
- Dearden KA, Schott W, Crookston BT, Humphries DL, Penny ME, & Behrman JR (2017). Children with access to improved sanitation but not improved water are at lower risk of stunting compared to children without access: a cohort study in Ethiopia, India, Peru, and Vietnam. BMC public health, 17(1), 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Ninno C, & Lundberg M (2005). Treading water: the long-term impact of the 1998 flood on nutrition in Bangladesh. Economics & Human Biology, 3(1), 67–96. [DOI] [PubMed] [Google Scholar]
- De Silva I, & Sumarto S (2018). Child malnutrition in Indonesia: can education, sanitation and healthcare augment the role of income?. Journal of International Development, 30(5), 837–864. [Google Scholar]
- Dimitrova A, & Bora JK (2020). Monsoon weather and early childhood health in India. PloS one, 15(4), e0231479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitrova A, & Muttarak R (2020). After the floods: Differential impacts of rainfall anomalies on child stunting in India. Global Environmental Change, 64. [Google Scholar]
- Dimitrova A, 2021. Seasonal droughts and the risk of childhood undernutrition in Ethiopia. World Development, 141, p.105417. [Google Scholar]
- Frame D, Joshi M, Hawkins E, Harrington LJ, & de Roiste M (2017). Population-based emergence of unfamiliar climates. Nature Climate Change, 7(6), 407. [Google Scholar]
- Funk C, Peterson P, Landsfeld M, Pedreros D, Verdin J, Shukla S, … & Michaelsen J (2015). The climate hazards infrared precipitation with stations—a new environmental record for monitoring extremes. Scientific data, 2(1), 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk C, Peterson P, Peterson S, Shukla S, Davenport F, Michaelsen J, … & Mata N (2019). A high-resolution 1983–2016 T max climate data record based on infrared temperatures and stations by the climate Hazard center. Journal of Climate, 32(17), 5639–5658. [Google Scholar]
- Grace K, Davenport F, Funk C, & Lerner AM (2012). Child malnutrition and climate in Sub-Saharan Africa: An analysis of recent trends in Kenya. Applied Geography, 35(1–2), 405–413. [Google Scholar]
- Grace K, Verdin A, Dorélien A, Davenport F, Funk C, & Husak G (2021). Exploring Strategies for Investigating the Mechanisms Linking Climate and Individual-Level Child Health Outcomes: An Analysis of Birth Weight in Mali. Demography, 58(2), 499–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray C, & Wise E (2016). Country-specific effects of climate variability on human migration. Climatic change, 135(3–4), 555–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris I, Osborn TJ, Jones P, & Lister D (2020). Version 4 of the CRU TS monthly high-resolution gridded multivariate climate dataset. Scientific data, 7(1), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R, Lo S (2013). Nutrition: a quintessential sustainable development goal. Lancet 382(9890):371–372 [DOI] [PubMed] [Google Scholar]
- Headey D, Hoddinott J, Ali D, Tesfaye R, & Dereje M (2015). The other Asian enigma: explaining the rapid reduction of undernutrition in Bangladesh. World Development, 66, 749–761. [Google Scholar]
- Hoddinott J, & Kinsey B (2001). Child growth in the time of drought. Oxford Bulletin of Economics and statistics, 63(4), 409–436. [Google Scholar]
- IPCC. (2014). Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II, and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. IPCC, Geneva, Switzerland. [Google Scholar]
- Jongman B, Winsemius HC, Aerts JC, De Perez EC, Van Aalst MK, Kron W, & Ward PJ (2015). Declining vulnerability to river floods and the global benefits of adaptation. Proceedings of the National Academy of Sciences, 112(18), E2271–E2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna T, & Das M (2016). Why gender matters in the solution towards safe sanitation? Reflections from rural India. Global public health, 11(10), 1185–1201. [DOI] [PubMed] [Google Scholar]
- Kumar S, Molitor R, & Vollmer S (2016). Drought and early child health in rural India. Population and Development Review, 53–68. [Google Scholar]
- Lokshin M, & Radyakin S (2012). Month of birth and children’s health in India. Journal of Human Resources, 47(1), 174–203. [Google Scholar]
- Lopalo M, Kuruc K, Budolfson M, & Spears D (2019). Quantifying India’s Climate Vulnerability. In India Policy Forum (Vol. 15, No. 1, pp. 107–148). National Council of Applied Economic Research. [Google Scholar]
- Mayala B, Fish T, Eitelberg D, Dontamsetti T (2018). The DHS Program Geospatial Covariate Datasets Manual (Second Edition). Rockville, Maryland, USA: ICF. [Google Scholar]
- Minnesota Population Center. (2018). Integrated Public Use Microdata Series, International: Version 7.1. 10.18128/D020.V7.1 [DOI]
- Mora C, Dousset B, Caldwell IR, Powell FE, Geronimo RC, Bielecki CR, … & Lucas MP (2017). Global risk of deadly heat. Nature Climate Change, 7(7), nclimate3322 [Google Scholar]
- Mueller V, Gray C, Handa S, & Seidenfeld D (2020). Do social protection programs foster short-term and long-term migration adaptation strategies?. Environment and development economics, 25(2), 135–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulmi P, Block SA, Shively GE, & Masters WA (2016). Climatic conditions and child height: Sex-specific vulnerability and the protective effects of sanitation and food markets in Nepal. Economics & Human Biology, 23, 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas K, Campbell L, Paul E, Skeltis G, Wang W, & Gray C (2021). Climate anomalies and childhood growth in Peru. Population and Environment, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobles J, & Hamoudi A (2019). Detecting the Effects of Early-Life Exposures: Why Fecundity Matters. Population Research and Policy Review, 38(6), 783–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordkvelle J, Rustad SA, & Salmivalli M (2017). Identifying the effect of climate variability on communal conflict through randomization. Climatic Change, 141(4), 627–639. [Google Scholar]
- Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, & Martorell R (2012). Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Pediatric and perinatal epidemiology, 26, 285–301. [DOI] [PubMed] [Google Scholar]
- Randell H, & Gray C (2019). Climate change and educational attainment in the global tropics. Proceedings of the National Academy of Sciences, 116(18), 8840–8845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randell H, Gray C, & Grace K (2020). Stunted from the start: Early life weather conditions and child undernutrition in Ethiopia. Social Science & Medicine, 261, 113234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randell H, Jiang C, Liang X, Murtugudde R, Sapkota A (2021). Food insecurity and compound environmental shocks in Nepal: Implications for a changing climate. World Development, 145, 105511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray DK, West PC, Clark M, Gerber JS, Prishchepov AV, & Chatterjee S (2019). Climate change has likely already affected global food production. PloS one, 14(5), e0217148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayco-Solon P, Fulford AJ, & Prentice AM (2005). Maternal preconceptional weight and gestational length. American journal of obstetrics and gynecology, 192(4), 1133–1136. [DOI] [PubMed] [Google Scholar]
- Ruggles S, Manson S, Kugler T, Haynes II D, Van Riper D, and Bakhtsiyarava M. (2018) IPUMS Terra: Integrated Data on Population and Environment: Version 2. 10.18128/D090.V2 [DOI]
- Schwarzenberg SJ, & Georgieff MK (2018). Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics, 141(2). [DOI] [PubMed] [Google Scholar]
- Shively G, Sununtnasuk C, & Brown M (2015). Environmental variability and child growth in Nepal. Health & Place, 35, 37–51. [DOI] [PubMed] [Google Scholar]
- Shively GE (2017). Infrastructure mitigates the sensitivity of child growth to local agriculture and rainfall in Nepal and Uganda. Proceedings of the National Academy of Sciences, 114(5), 903–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrimpton R, Victora CG, de Onis M, Lima RC, Blössner M, & Clugston G (2001). Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics, 107(5), e75–e75. [DOI] [PubMed] [Google Scholar]
- Spears D (2018). Exposure to open defecation can account for the Indian enigma of child height. Journal of Development Economics, 102277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssewanyana S (2003). Food security and child nutrition status among urban poor households in Uganda: Implications for poverty alleviation. African Economic Research Consortium. [Google Scholar]
- Thiede BC, & Gray C (2020). Climate exposures and child undernutrition: Evidence from Indonesia. Social Science & Medicine, 265, 113298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiede BC, & Strube J (2020). Climate variability and child nutrition: Findings from sub-Saharan Africa. Global Environmental Change, 65, 102192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari S, Jacoby HG, & Skoufias E (2017). Monsoon babies: rainfall shocks and child nutrition in Nepal. Economic Development and Cultural Change, 65(2), 167–188. [Google Scholar]
- UNICEF, W., World Health Organization, & UNICEF. (2012). Progress on drinking water and sanitation: 2012 update. United States: WHO/UNICEF; Joint Monitoring Programme for Water Supply and Sanitation. [Google Scholar]
- Victora CG, De Onis M, Hallal PC, Blössner M, & Shrimpton R (2010). Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics, 125(3), e473–e480. [DOI] [PubMed] [Google Scholar]
- WHO. (2014). WHO Child Growth Standards: Methods and development. WHO. [Google Scholar]


