Abstract
BACKGROUND
Virtual reality and hypnosis are little studied in complex contexts, such as intensive care, where patients need significant physical and psychological assistance.
OBJECTIVES
To compare and combine hypnosis and virtual reality benefits on anxiety and pain on patients before and after cardiac surgery.
DESIGN
Prospective randomised controlled clinical trial.
SETTING
The study was conducted in the University Hospital of Liege (Belgium) from October 2018 to January 2020.
PATIENTS
One hundred patients (66 ± 11.5 years; 24 women, 76 men) were included. Participants were adults undergoing cardiac surgery. Exclusion criteria: psychiatric diseases, claustrophobia, acrophobia, hearing loss, visual impairment, extreme fatigue, confusion surgery cancelled.
INTERVENTIONS
Patients were randomly assigned to four arms (control; hypnosis; virtual reality; virtual reality hypnosis) and had 20 min of one of the techniques the day before and the day after surgery.
MAIN OUTCOMES MEASURES
Anxiety, pain, fatigue, relaxation, physiological parameters, and opioid use were evaluated before and after each session.
RESULTS
The main results did not show any significant differences between the groups. In all groups, anxiety decreased and pain increased from baseline to the postoperative day. Relaxation increased in all groups in the pre-operative (P < 0.0001) and postoperative period (P = 0.03). There were no significant differences for fatigue, physiological measures, or opioid use.
CONCLUSION
As there were no significant differences between groups for the measured variables, we cannot affirm that one technique is better than another. Additional studies are required to compare and evaluate the cost-effectiveness of these techniques for critical care patients and caregivers.
TRIAL REGISTRATION
ClinicalTrials.gov: NCT03820700. https://clinicaltrials.gov/ct2/show/NCT03820700. Retrospectively registered on 29 January 2019.
Introduction
Patients who are undergoing cardiac surgery are exposed to psychological and physiological distress.1 Anxiety and catastrophising are associated with impaired recovery after surgery, for example, persistent pain.2–4 Moreover, the stay in intensive care units (ICU) is accompanied by additional stress, confusional states, cognitive dysfunction (e.g. memory decline, delusion, postoperative delirium) and depression.5
Today complementary techniques (e.g. music, relaxation, hypnosis) are used together with pharmacological treatment and have been shown to decrease peri-operative anxiety, pain, nausea and the use of analgesic medication.1,6–9 Hypnosis and virtual reality have been investigated in numerous studies in the medical field (e.g. algology, oncology, anaesthesia) to reduce pain and anxiety and increase patient comfort.10–13 Hypnosis is defined as a ‘state of modified consciousness involving focused attention and reduced peripheral awareness characterised by an enhanced capacity for response to suggestions’.14 The hypnotic state involves the capacities of absorption (tendency to be fully involved in a mental experience), dissociation (a mental separation from the environment) and suggestibility (the responsiveness and ability to follow hypnotic suggestions).15 Hypnosis can be used during surgery in combination with local anaesthesia and conscious sedation. This technique is called ‘hypnosedation’ and is effective in decreasing anxiety and pain and analgesic drug use, and it increases patient comfort, improves surgical conditions and aids a faster recovery.16 Several studies and a meta-analysis of 26 randomised clinical trials showed a large effect size in favour of hypnosis for the reduction of emotional distress among patients undergoing medical procedures, such as abdominal surgery.17–20 Despite the reduction in postoperative pain without adverse effects risks,16 hypnosis can be difficult to organise routinely as it is time-consuming and requires a therapist.20 Distractive virtual reality (e.g. a game) or contemplative virtual reality (e.g. relaxation) are techniques involving the ‘use of computer technology to create the effect of an interactive three-dimensional world in which the objects have a spatial presence’.21 Such virtual reality could reduce distress related to a medical procedure, without side effects and with no need for additional staff.22 Mosso-Vázquez et al.23 in 2014 gave 30 min of virtual reality (contemplation in a beautiful landscape) to 67 patients 24 h before cardiac surgery: 88% of patients reported a decreased level of pain post-virtual reality; 37% had a lower heart rate; 52% had reduced mean arterial pressure. As both virtual reality and hypnosis seem effective in the reduction of anxiety and pain, a few studies have compared and combined these techniques together. The combined technique is today known as virtual reality hypnosis (VRH).24 VRH has shown its success in the management of anxiety and pain in different medical contexts, such as physical trauma, chronic pain management or intensive care12,25–27 but randomised studies are needed to investigate and compare the effectiveness of these techniques in cardiac surgery and ICU.
As VRH reduces both clinical and experimental pain,28,29 our hypothesis was that VRH could be beneficial in the reduction of pain and anxiety before and after cardiac surgery.
Methods
Objectives
The aim was to identify the evolution of self-assessed anxiety, pain, fatigue and relaxation states of cardiac surgery patients before and after using hypnosis, virtual reality and virtual reality hypnosis as compared with a control group.
Registration and ethical approval
This trial was registered retrospectively on clinicaltrials.gov (NCT03820700). Registered on 29 January 2019, the recruitment started in October 2018 and closed in January 2020. The complete protocol of the study has previously been published.30 Ethical approval was provided by the Ethical Committee of Liege University Hospitals, Domaine Universitaire du Sart Tilman (B35) 4000 Liege, Belgium on 22 June 2018 (Ethical Committee N° B707201836498). Written informed consents were obtained from all patients before inclusion.
Recruitment and patient involvement
Before any patient recruitment, a pilot study was undertaken to refine the choice of the questionnaires and evaluate the virtual reality setting. Randomisation was undertaken in blocks of five patients. Inclusion criteria were: age more than 18 years, cardiac surgery [coronary artery bypass graft (CAB); mitral valve replacement (MVR); aortic valve replacement (AVR); other] at the University Hospital of Liege (Belgium), French speaking, Glasgow Coma Scale score greater than 14,31 Richmond Agitation-Sedation Scale score constituted of −1, 0 and +1,32 who have given their consent. Exclusion criteria were: psychiatric diseases, claustrophobia, acrophobia, hearing loss, visual impairment, extreme fatigue, confusion, surgery cancelled or postponed.
Intervention components
This study is a prospective single-centre randomised study with four arms: a control group and three experimental groups.
-
(1)
Control group: daily standard care.
-
(2)
Hypnosis: in addition to the daily standard care, a 20 min prerecorded hypnosis session. The audio track was created and recorded by M-EF and A-SN, both experts in clinical and experimental hypnosis. The recording included suggestions for positive body sensations along with an invitation to observe a sunrise and a beautiful landscape while relaxing in a white cloud chair.
-
(3)
Virtual reality: in addition to the daily standard care, a 20 min virtual reality session wearing a head-mounted display with goggles (Oncomfort). Participants watched a tridimensional graphical landscape, consisting of a mountain cabin near a lake at sunrise, followed by a relaxing moment in the clouds (Fig. 1). The display was visual and audio, with sounds of ambient nature but no voice.
-
(4)
Virtual reality hypnosis combination (VRH): in addition to the daily standard care, a 20 min VRH session. The recorded hypnosis session was combined with the virtual reality display.
Fig. 1.
Virtual reality and virtual reality hypnosis landscape designed by Oncomfort
Assessment
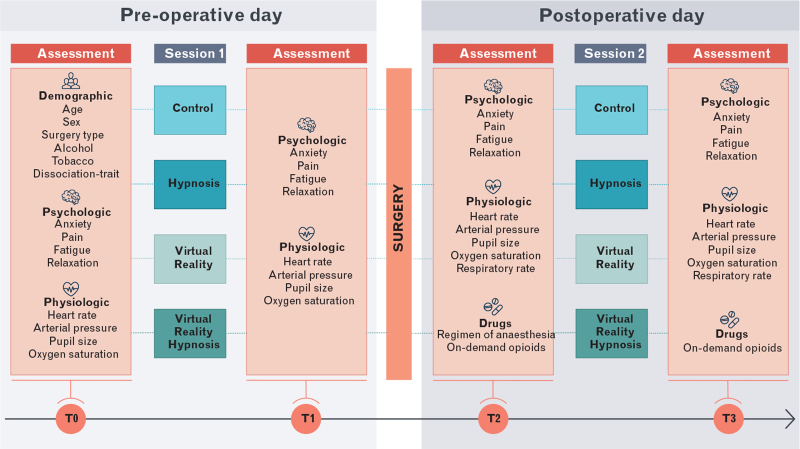
Before and after each session, variables were recorded (Fig. 2).
Fig. 2.
Study design, times and assessments
Patient characteristics integrated into the analysis included age and sex, dissociative profile with Dissociative Experience Scale (DES) (a mean score >30 is equal to a high dissociative profile, i.e. someone who often experiences dissociative events in the everyday life),33 cardiac surgery type, alcohol consumption, use of tobacco. Psychological variables, anxiety, pain, relaxation and fatigue were assessed with the Visual Analogic Scale (VAS, self-assessed scale that ranged from 0 to 10, 10 is the most pain imaginable) before and after each 20 min session. Physiological parameters (heart rate, arterial pressure, respiratory rate, pupil size and oxygen saturation) were recorded directly on the patient's bed monitor.
We also recorded whether patients received spinal morphine (0.5 mg). To examine the confounding effects of analgesic medication after surgery, the ‘on-demand’ opioid intake was recorded 2 h before the session and until 6 h after. Nurses and doctors usually administered ‘on-demand’ opioids during the day when pain intensity was greater than 3 on the VAS 10-point scale. Whenever pain was extreme, patient-controlled intravenous analgesia (PCIA) was administred.
Statistical analyses
The sample size calculation was based on repeated measures ANOVA test. Alpha was set at 0.05, power at 95% and the standardised effect size at 0.5. Studies which aim to assess the effect of hypnosis on patients’ presurgery anxiety define an effect size of 0.2 as small, 0.5 as moderate and 0.8 as large.1 With these parameters, 12 patients were required in each group, a total of 48 patients. We decided to enroll 100 patients (25 per group) to allow for dropouts on the postoperative day. The normality of data was assessed graphically with histograms and quantile-quantile plots, and was tested with the Shapiro–Wilk test. Continuous variables were reported as mean ± SD, or median [IQR] for skewed distributions whereas counts were used for qualitative variables. Categorical variables were compared using the χ2 test or Fisher's exact test. The homogeneity of the four groups were assessed with the chi-squared test for qualitative and dichotomous variables and with a one-way analysis of variance (ANOVA-1) or the nonparametric Kruskal–Wallis test for the quantitative variables. A repeated measures ANOVA test was used to compare the evolution of the parameters between the pre-operative day and the postoperative day according to the groups. This analysis was adjusted by potential confounding factors. Calculations were always carried out with the maximum data available. Results were considered as statistically significant at the 5% level (P < 0.05). Analyses were performed using R 3.5.3 (R Core Team) and the package Rcommander (Rcmdr) and using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Study population
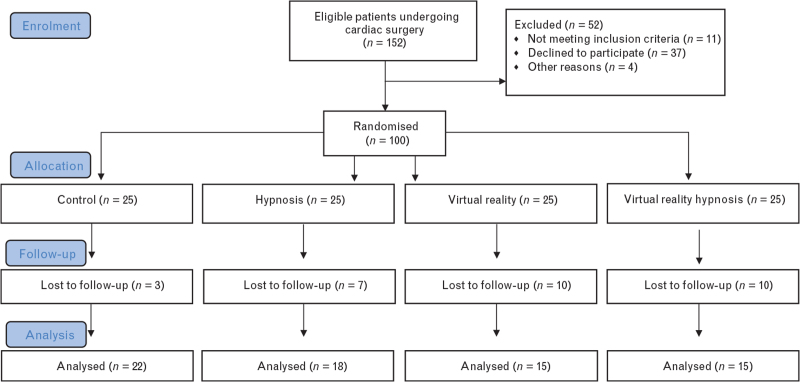
Between October 2018 and January 2020, 100 patients were randomised to the four arms. Analyses included data from 100 patients on the pre-operative day (T0, T1) and from 70 patients postsurgery (T2, T3) (Fig. 3).
Fig. 3.
CONSORT flow diagram
Dropouts
Data from 30 (30%) patients could not be collected after surgery because of patient fatigue, sedation or confusion; patients who were intubated and sedated or in the recovery room; patients who did not like hypnosis, virtual reality or VRH; or if patients were undergoing a medical or nursing procedure. There were no significant differences between the groups in the dropout rates (χ2 = 6.29, P = 0.09) (Fig. 3).
Patient characteristics
The patients initially recruited consisted of 24 women and 76 men. The mean age was 66 ± 11.5 years. Forty (40%) consumed more than three glasses of alcohol per week and 33 (33%) smoked. The patient characteristics were well balanced between the four arms and the dissociation-trait scores of patients ranged from 0 to 48.6. Spinal morphine was given to 47% of the patients and this was balanced across the groups. The type of surgery was heterogeneous between groups (P = 0.002) (Table 1). This was corrected in the analysis.
Table 1.
Patient characteristics across the groups on the pre-operative day
| Control | Hypnosis | VR | VRH | Total | ||
| Group intervention | (n = 25) | (n = 25) | (n = 25) | (n = 25) | 100 | P value |
| Age | 63.3 ± 11.5 | 67.6 ± 12.5 | 64.7 ± 13.4 | 68.4 ± 7.8 | 66 (±11.5) | 0.37 |
| Gender | 0.72 | |||||
| Male | 18 | 18 | 19 | 21 | 76 | |
| Female | 7 | 7 | 6 | 4 | 24 | |
| Alcohol consumers | 10 | 11 | 7 | 11 | 40 | 0.61 |
| Smokers | 4 | 5 | 8 | 4 | 33 | 0.45 |
| Dissociation-trait | 16.8 ± 12.5 | 21.4 ± 12.4 | 15.6 ± 12.2 | 17.9 ± 12.5 | 0.23 | |
| High dissociative profile (mean score >30) | 3 | 5 | 3 | 11 | 0.65 | |
| Spinal morphine | 10 | 13 | 12 | 11 | 46 | 0.85 |
| Surgery type | 0.002∗ | |||||
| Coronary artery bypass graft surgery | 10 | 15 | 17 | 15 | 57 | |
| Mitral valve replacement | 3 | 9 | 6 | 8 | 26 | |
| Mitral valve replacement | 6 | 1 | 0 | 2 | 9 | |
| Multiple interventions | 4 | 0 | 0 | 0 | 4 | |
| Others | 2 | 0 | 2 | 0 | 4 |
Data are mean ± SD or n. VR, virtual reality; VRH, virtual reality hypnosis.
P < 0.05.
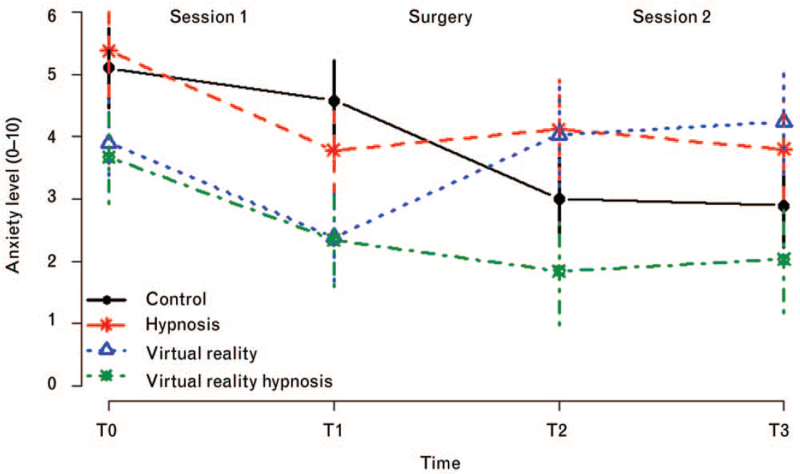
Anxiety
Age was significantly associated with anxiety (P = 0.017): older individuals were more anxious at baseline. Anxiety evolved differently over time (P = 0.023): patients in the hypnosis group reported significantly more anxiety than those in VRH group at all times, even at baseline (P = 0.007). Anxiety was higher at baseline (T0) than at T1 (P < 0.0001), T2 (P < 0.0001) and T3 (P < 0.0001) in all groups. Apart from the baseline difference between VRH and hypnosis and its durability over time, there were no significant differences between the groups (Fig. 4).
Fig. 4.
Evolution of anxiety during presurgery and postsurgery (by time by group)
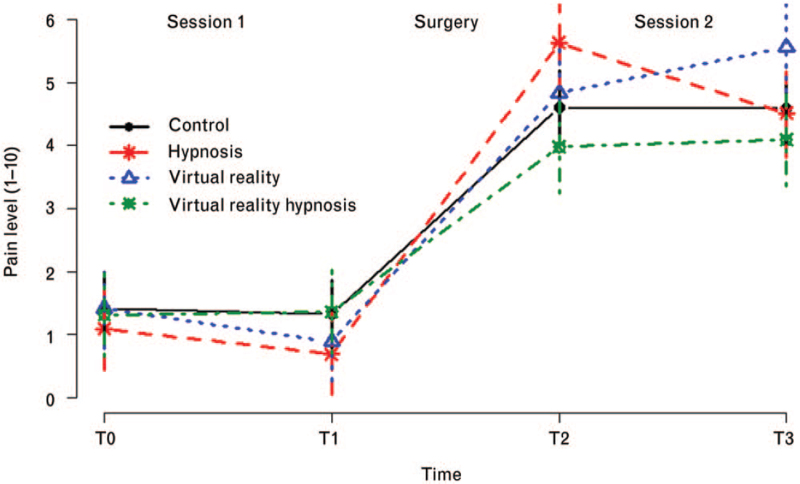
Pain
Pain correlated with time (P < 0.0001) and was lower at baseline (T0) and at T1 as compared with T2 and T3 in all groups (P < 0.0001). No patient factors correlated with pain. No significant differences in the pain scores were observed between the four groups (Fig. 5).
Fig. 5.
Evolution of pain during presurgery and postsurgery (by time by group)
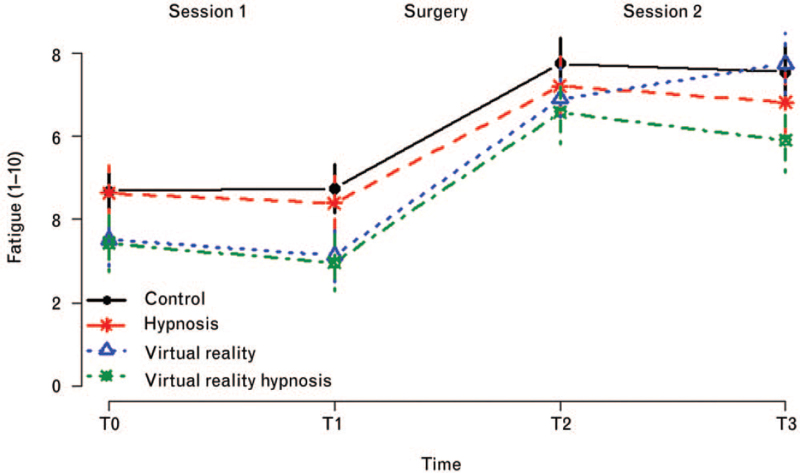
Fatigue
The patient's sex was associated with fatigue: women felt more fatigue than men irrespective of the time and group (P = 0.009). Fatigue correlated with time (P < 0.0001): levels of fatigue were lower at T0 and T1 than at T2 and T3 in all groups (P < 0.0001). No significant differences were found between T0 and T1. Levels of fatigue before and after surgery were not significantly different across the groups (Fig. 6).
Fig. 6.
Evolution of fatigue during presurgery and postsurgery (by time by group)
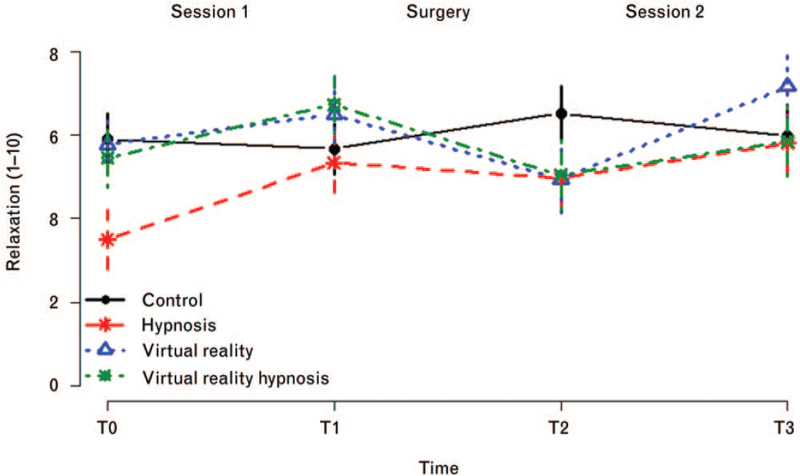
Relaxation
There were differences between times for patient relaxation (P = 0.013): patients at T0 were less relaxed than at T1 (P = 0.008) and T3 (P = 0.008) in all groups. After the surgery, patients felt more relaxed at T3 than at T2 in all groups (P = 0.039). There were no significant differences between groups at any time (Fig. 7).
Fig. 7.
Evolution of relaxation during presurgery and postsurgery (by time by group)
Physiological variables
Arterial pressure depended on the time of assessment. Levels of arterial pressure were more elevated at T0 than at T1 (P = 0.030), T2 (P < 0.0001) and T3 (P < 0.0001) in all groups. Heart rate was lower at baseline (T0) and at T1 (before surgery) than at T2 and T3 (after the surgery) (P < 0.0001). There were no significant differences across the groups at any time. The techniques did not influence pupil size, oxygen saturation or respiratory frequency at any time.
Opioids
On the postoperative day in ICU, all patients received paracetamol (4 × 1 g per day). No patients received PCIA and 48 patients out of the 70 (68.57%) received additional opioids ‘on-demand’. There were no significant differences across the groups in terms of on-demand opioids (P = 0.63) (Table 2).
Table 2.
Patients who received added opioids on postoperative day
| Control | Hypnosis | VR | VRH | Total | p value | |
| Opioids, yes | 15 (68) | 11 (61) | 12 (80) | 10 (67) | 48 (69) | .63 |
| Opioids, no | 5 (23) | 2 (11) | 1 (7) | 2 (13) | 10 (14) | |
| Missing data | 2 (9) | 5 (28) | 2 (13) | 3 (20) | 12 (17) | |
| Total | 22 (100) | 18 (100) | 15 (100) | 15 (100) | 70 (100) |
Data are n, and (%). VR, virtual reality; VRH, virtual reality hypnosis.
Discussion
In this study, we evaluated the influence of recorded hypnosis, virtual reality or VRH and compared these against each other and with a control group, on anxiety, pain, fatigue and relaxation, physiological parameters and use of opioids. The main results were that there were no significant differences among the four groups for any variable and none of the techniques was better than another, nor better than the control group – no treatment.
Our results are in contrast to some studies evaluating the effects of hypnosis in surgery or in the ICU (for a review, see Rousseaux et al.34). Montgomery et al.35 showed that a brief hypnosis session (15 min) performed within 1 h before breast surgery reduced pain, nausea, emotional upset and increased comfort. In a randomised trial of 50 patients, hypnosis was administered before and after coronary artery bypass surgery. Patients in the hypnosis group showed better coping strategies for emotional distress, and anxiety and depression were reduced compared with a control group.18 Another randomised trial of 60 patients in ICU investigated the benefits of therapy with positive hypnotic suggestions and showed a significant diminution of the ventilation period and the length of stay in ICU in the hypnosis group compared with the control group.36 Virtual reality was also documented as beneficial for reducing anxiety before surgery. In a prospective study of 20 patients undergoing maxillofacial surgery, 5 min of a virtual reality video significantly reduced the patients’ stress levels and salivary cortisol (a stress physiological indicator).2 In a recent review of the literature on virtual reality and hypnosis, authors reported pain and anxiety reduction in different clinical settings (chronic pain, burns pain, physical trauma)27, nevertheless a few studies investigated VRH in randomised trials. Most of these were case studies, and the results for VRH and pain did not show a consistent effect over patients and days.22,24,25 Another example, in a nonrandomised trial of 59 ICU patients showed significant reductions in anxiety and depression when virtual reality was combined with guided meditation every day for a week, but no effects were found for pain, sleep and physiological parameters.26
Anxiety and pain levels were low to moderate, and the variables evolved similarly in the four groups, suggesting that perhaps the usual medical treatment was already effective enough for these patients. In addition, the reduction of anxiety and increase in pain on the postoperative day is normal in association with cardiac surgery. One hypothesis regarding the reduction of anxiety in all groups between T0 and T1 would be that the investigator's input may have an influence on the patients’ feelings. Thus, the investigator visiting the patients before the surgery may have reassured them and decreased their anxiety, independently of the technique used.
These results did not show a higher benefit of adding virtual reality to hypnosis (or hypnosis to virtual reality), nor indeed any difference from the control group with no treatment. This question remains unsolved in the literature even for healthy participants. According to Enea et al. (2014), highly hypnotisable individuals reported less pain when using hypnosis and VRH, whereas low hypnotisable individuals reported less pain when using virtual reality and VRH than hypnosis alone or no treatment.28 Researchers hypothesised that the cognitive processes involved in distraction as well as the mechanisms of how pain is reduced during virtual reality differ from those involved in hypnosis.28,29 Nevertheless, phenomenological and psychological mechanisms of VRH have not yet been tested in randomised trials implying further studies are required.
This study has some limitations. First, the patient-dropout because of the inability to participate the day after surgery. Some of the patients expressed the fact that extreme fatigue as well as deep sedation because of surgery are a barrier to following hypnotic suggestions and virtual reality images. The second limitation is that given the nature of the techniques, neither patients nor the investigators were blinded to the treatment assignment. We can consider randomisation as a methodological strength and also a clinical limit. Standardisation of the techniques did not allow an adaptation to the patient situation.37 In our study, we used one design of ‘passive VR’ with no interactions and no user's control of the environment. Users’ interactions with the virtual reality environment and possibility of action (e.g. with eyes tracking or joystick) is an important factor that has a positive influence on immersion and presence in virtual reality.38
Future perspectives
Only a few studies have compared hypnosis, virtual reality and virtual reality hypnosis.28,29 More studies are required to improve the comparison of these complementary techniques in terms of efficacy and cost-effectiveness, cognitive functions and psychological mechanisms in healthy participants and patients.
Our randomised study investigated the clinical effectiveness of these techniques among patients in cardiac surgery and in ICU and the results challenge current perceptions around virtual reality in the medical field, the high expectations that stem from it, and the willingness to use it for assorted medical issues. Publications stating that hypnosis and virtual reality are effective techniques abound in the literature but this could be publication bias. It is important for our understanding that studies showing nonsignificant results are published more often. Only then, with the benefit of diversified information can we analyse for whom, and when these techniques work for critical care patients.
Another perspective to investigate in terms of the effectiveness of these techniques would be the importance of the psychologist's interaction with the patient, and how this affects the patient's motivation to use the technique. Future studies should consider this therapeutic relationship and include the investigator as a variable.
Most of the studies investigated the efficacy of these complementary techniques on pain reduction, and did not establish a global evaluation of their use. This study indicates a necessity to rethink protocols on hypnosis and virtual reality by using multidimensional evaluations with a view to assessing their real appropriateness for both health-care staff and patients’ needs. Such complementary techniques should also be compared in terms of applicability, agreeability, ease of use and adaptability to the situation. A recent meta-analysis showed that active peri-operative psychological interventions (behavioural therapy, relaxation, guided imagery) moderately reduced persistent postsurgical pain and physical impairment.39 The authors concluded that researchers and clinicians have to take into account individual pain and distress following cardiac surgery and identify patients who are more likely to benefit from psychotherapies and complementary techniques: in other words, to adapt the therapy to the patient.39
Conclusion
This randomised trial of cardiac surgery patients compared hypnosis, virtual reality and VRH given presurgery and postsurgery in ICU but results did not show any differences in effectiveness, either between the techniques themselves or between the techniques and no treatment (i.e. the control group). At a fundamental level, future randomised controlled trials could inform us as to the phenomenological differences between hypnosis, virtual reality and VRH. Regarding clinical practice, further studies should consider multidimensional measures to compare techniques in order to establish guidelines for virtual reality and hypnosis use in cardiac surgery or intensive care units.
Acknowledgements relating to this article
Assistance with the study: the authors would like to thank all departments of the University of Liege and University Hospital of Liege involved in the project: Psychology Faculty, Laboratory of Cognitive Ergonomics and Work Interventions, GIGA Consciousness, Cardiac Surgery Department, Algology Department, Department of Intensive Care Units. Thanks to Oncomfort Society (www.oncomfort.com) (Wavre) and Musicotherapy and Counselling (www.musicotherapeute.be) (Liege) for providing the material.
Financial support and sponsorship: funding cover fees of PhD student (FR), postdoc researcher (AV) and material. This work was supported by the University and University Hospital of Liege, the Benoit Foundation (Bruxelles, Belgium), the Non-Fria Grant (University of Liege, Belgium) and the Credits Sectoriels de la Recherche (University of Liege, Belgium). Researchers are independents from funders.
Conflicts of interest: M-EF is on the scientific board of Oncomfort society (www.oncomfort.com). The University of Liege and Hospital University of Liege undertake to mention in the relevant publications the use of a modified product compared with Oncomfort's commercial product. Other authors report no conflicts of interest in this work.
Presentation: preliminary results of this study have been presented in conferences in Hypnosis New Generation, Budapest, Hungary; Belgian Association for Psychological Science, Liege, Belgium and Belgian Pain Society Congress, Louvain, Belgium.
Footnotes
Published online 15 November 2021
References
- 1.Akgul A, Guner B, Çirak M, et al. The beneficial effect of hypnosis in elective cardiac surgery: a preliminary study. Thorac Cardiovasc Surg 2016; 64:581–588. [DOI] [PubMed] [Google Scholar]
- 2.Ganry L, Hersant B, Sidahmed-Mezi M, et al. Using virtual reality to control preoperative anxiety in ambulatory surgery patients: a pilot study in maxillofacial and plastic surgery. J Stomatol Oral Maxillofac Surg 2018; 119:257–261. [DOI] [PubMed] [Google Scholar]
- 3.Johansen A, Romundstad L, Nielsen C, et al. Persistent postsurgical pain in a general population: prevalence and predictors in the Tromso study. Pain 2012; 153:1390–1396. [DOI] [PubMed] [Google Scholar]
- 4.Mavros MN, Athanasiou S, Gkegkes ID, et al. Do psychological variables affect early surgical recovery? PLoS One 2011; 6:e20306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rovai D, Giannessi D, Andreassi M, et al. Mind injuries after cardiac surgery. J Cardiovasc Med (Hagerstown) 2015; 16:844–851. [DOI] [PubMed] [Google Scholar]
- 6.Ames N, Shuford R, Yang L, et al. Music listening among postoperative patients in the intensive care unit: a randomized controlled trial with mixed-methods analysis. Integr Med Insights 2017; 12:117863371771645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lang EV, Benotsch EG, Fick LJ, et al. Adjunctive nonpharmacological analgesia for invasive medical procedures: a randomised trial. Lancet 2000; 355:1486–1490. [DOI] [PubMed] [Google Scholar]
- 8.Meurisse M, Hamoir E, Defechereux T, et al. Bilateral neck exploration under hypnosedation: a new standard of care in primary hyperparathyroidism? Ann Surg 1999; 229:401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faymonville ME, Fissette J, Mambourg PH, et al. Hypnosis as adjunct therapy in conscious sedation for plastic surgery. Reg Anesth 1995; 20:145–151. [PubMed] [Google Scholar]
- 10.Grégoire C, Nicolas H, Bragard I, et al. Efficacy of a hypnosis-based intervention to improve well being during cancer: a comparison between prostate and breast cancer patients. BMC Cancer 2018; 18:677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Indovina P, Barone D, Gallo L, et al. Virtual reality as a distraction intervention to relieve pain and distress during medical procedures: a comprehensive literature review. Clin J Pain 2018; 34:858–877. [DOI] [PubMed] [Google Scholar]
- 12.Patterson DR, Jensen MP, Wiechman SA, et al. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int J Clin Exp Hypn 2010; 58:288–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vanhaudenhuyse A, Gillet A, Malaise N, et al. Psychological interventions influence patients’ attitudes and beliefs about their chronic pain. J Tradit Complement Med 2018; 8:296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elkins GR, Barabasz AF, Council JR, et al. Advancing research and practice: the revised APA division 30 definition of hypnosis. Int J Clin Exp Hypn 2015; 63:1–9. [DOI] [PubMed] [Google Scholar]
- 15.Spiegel D. Neurophysiological correlates of hypnosis and dissociation. J Neuropsychiatry Clin Neurosci 1991; 3:440–445. [DOI] [PubMed] [Google Scholar]
- 16.Faymonville ME, Meurisse M, Fissette J. Hypnosedation: a valuable alternative to traditional anaesthetic techniques. Acta Chir Belg 1999; 99:141–146. [PubMed] [Google Scholar]
- 17.Ashton RC, Whitworth GC, Seldomridge JA, et al. The effects of self-hypnosis on quality of life following coronary artery bypass surgery: preliminary results of a prospective, randomized trial. J Altern Complement Med 1995; 1:285–290. [DOI] [PubMed] [Google Scholar]
- 18.de Klerk JE, du Plessis WF, Steyn HS, et al. Hypnotherapeutic ego strengthening with male South African coronary artery bypass patients. Am J Clin Hypn 2004; 47:79–92. [DOI] [PubMed] [Google Scholar]
- 19.Faymonville EM, Mambourg HP, Joris J, et al. Psychological approaches during conscious sedation. Hypnosis versus stress reducing strategies: a prospective randomized study. Pain 1997; 73:361–367. [DOI] [PubMed] [Google Scholar]
- 20.Schnur JB, Kafer I, Marcus C, et al. Hypnosis to manage distress related to medical procedures: a meta-analysis. Contemp Hypn 2008; 25:114–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bryson S. Virtual reality: a definition history - a personal essay. ArXiv13124322 Cs. 2013. Available at: http://arxiv.org/abs/1312.4322. [Accessed 13 May 2020] [Google Scholar]
- 22.Patterson DR, Wiechman SA, Jensen M, et al. Hypnosis delivered through immersive virtual reality for burn pain: a clinical case series. Int J Clin Exp Hypn 2006; 54:130–142. [DOI] [PubMed] [Google Scholar]
- 23.Mosso-Vázquez JL, Gao K, Wiederhold BK, et al. Virtual reality for pain management in cardiac surgery. Cyberpsychology Behav Soc Netw 2014; 17:371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patterson DR, Tininenko JR, Schmidt AE, et al. Virtual reality hypnosis: a case report. Int J Clin Exp Hypn 2004; 52:27–38. [DOI] [PubMed] [Google Scholar]
- 25.Oneal BJ, Patterson DR, Soltani M, et al. Virtual reality hypnosis in the treatment of chronic neuropathic pain: a case report. Int J Clin Exp Hypn 2008; 56:451–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong TL, Ruppert MM, Akbar M, et al. Improving the intensive care patient experience with virtual reality—a feasibility study. Crit Care Explor 2020; 2:e0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rousseaux F, Bicego A, Ledoux D, et al. Hypnosis associated with 3D immersive virtual reality technology in the management of pain: a review of the literature. J Pain Res 2020; 13:1129–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Enea V, Dafinoiu I, Opriş D, et al. Effects of hypnotic analgesia and virtual reality on the reduction of experimental pain among high and low hypnotizables. Int J Clin Exp Hypn 2014; 62:360–377. [DOI] [PubMed] [Google Scholar]
- 29.Patterson DR, Hoffman HG, Palacios AG, et al. Analgesic effects of posthypnotic suggestions and virtual reality distraction on thermal pain. J Abnorm Psychol 2006; 115:834–841. [DOI] [PubMed] [Google Scholar]
- 30.Rousseaux F, Faymonville M-E, Nyssen A-S, et al. Can hypnosis and virtual reality reduce anxiety, pain and fatigue among patients who undergo cardiac surgery: a randomised controlled trial. Trials 2020; 21:330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet 1974; 304:81–84. [DOI] [PubMed] [Google Scholar]
- 32.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond agitation–sedation scale. Am J Respir Crit Care Med 2002; 166:1338–1344. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735. [DOI] [PubMed] [Google Scholar]
- 34.Rousseaux F, Bicego A, Malengreaux C, et al. Can hypnosis be used in intensive care units? Méd Intensive Réa 2020; 29:309–318. [Google Scholar]
- 35.Montgomery GH, Bovbjerg DH, Schnur JB, et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J Natl Cancer Inst 2007; 99:1304–1312. [DOI] [PubMed] [Google Scholar]
- 36.K. Szilágyi A, Diószeghy C, Benczúr L, et al. Effectiveness of psychological support based on positive suggestion with the ventilated patient. Eur J Ment Health 2007; 2:149–170. [Google Scholar]
- 37.Bicego A, Monseur J, Rousseaux F, et al. Drop-out from chronic pain treatment programmes: is randomization justified in biopsychosocial approaches? J Rehabil Med 2021; 53:jrm00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baños RM, Botella C, Garcia-Palacios A, et al. Presence and reality judgment in virtual environments: a unitary construct? Cyberpsychol Behav 2000; 3:327–335. [Google Scholar]
- 39.Wang L, Chang Y, Kennedy SA, et al. Perioperative psychotherapy for persistent postsurgical pain and physical impairment: a meta-analysis of randomised trials. Br J Anaesth 2018; 120:1304–1314. [DOI] [PubMed] [Google Scholar]