Abstract
Students with anxiety or mood issues tend to engage in more problematic drinking, but less is known about those students with co-occurring anxiety and mood symptoms. This study compares rates of weekly alcohol use, hazardous drinking, and alcohol-related negative consequences in a sample of 699 college students with symptoms of comorbid anxiety and depression (35% of the sample) compared to their non-symptomatic drinking peers, as well as the moderating role of gender. We found main effects of gender and comorbidity status such that participants with comorbid symptoms of anxiety and depression or who were male reported higher rates of weekly alcohol use, more hazardous drinking and more alcohol-related negative consequences than their non-symptomatic and female peers. We also found an interaction effect on alcohol-related negative consequences such that male participants with comorbid anxiety and depression reported more alcohol-related negative consequences than all other groups. These findings imply that while any student drinker with both anxiety and depression may be considered at higher risk for problematic drinking behavior, the risk of negative consequences in particular may be highest in the men of that group.
Keywords: anxiety, depression, alcohol use, college students, gender
Introduction
College student drinking is often perceived as a normal social behavior, with minimal concern about the associated risks. Approximately 53% of college students have reported past-month alcohol use, and almost 35% reported past-month binge drinking (i.e., 5/4 or more drinks in a one sitting for men/women; Center for Behavioral Health Statistics and Quality, 2018). Whereas weekly alcohol use does not necessarily result in negative outcomes, students who engage in binge drinking often report a myriad of consequences, including physical harm, academic failings, and sexual assault, among others (Perkins, 2002). Though many students “mature out” of heavy drinking after college (Linden-Carmichael & Lanza, 2018), roughly 30% of students meet criteria for an alcohol use disorder (AUD) each year, demonstrating the beginning of a long struggle that some students have with drinking. To better prevent students from developing longer-term drinking issues, it is critical to identify those students who may be more vulnerable to problematic drinking behaviors.
Students with elevated mental health issues are particularly vulnerable given their tendency to drink to manage their negative affect. Anxiety and mood issues are the two most common mental health complaints among college students, and existing work has demonstrated their high co-occurrence with each other, as well as with problematic drinking patterns (Auerbach et al., 2016). In the past year, 45.1% of students endorsed depressive symptoms and 65.7% endorsed overwhelming anxiety (American College Health Association, 2019), and rates of past-year comorbid depression and anxiety have ranged from 50–67.8% (Hirschfeld, 2001; Kessler et al., 2003). Further, as students experience more severe mental health issues, they are more likely to engage in problematic drinking (49% increase; Lo et al., 2013). Compounding these issues, students rarely seek formal mental health or substance use treatment (Blanco et al., 2008; Capron et al., 2018). Given the high prevalence of anxiety, depression and alcohol use among college students, it would be beneficial to investigate factors that influence the association between comorbid depression/anxiety and risky drinking patterns.
Existing work has largely focused on the distinct effects of depression and anxiety on problematic drinking patterns. For example, depression symptoms are consistently associated with riskier drinking patterns and developing an AUD among college students (Geisner et al., 2012; Holahan et al., 2003; Weitzman, 2004). Relatedly, evidence suggests that more anxiety symptoms are associated with more problematic alcohol use (Kushner et al., 2008). Coping-motivated alcohol use is one explanation for the high co-occurrence of anxiety or depression and alcohol use (Gonzalez et al., 2011; Kuntsche et al., 2005; Villarosa et al., 2017). However, these findings are less clear when gender is taken into account. Evidence suggests that the association between depression and problematic drinking may be stronger among men (e.g., Geisner et al., 2012) whereas the association between anxiety and drinking may be stronger among women (Norberg et al., 2010). Clarifying the role of gender on drinking patterns may be best achieved by examining those students who endorse both anxiety and depression.
College may be a time of prevalent social drinking, but it is also a bottleneck that presents a unique opportunity for screening and intervention. Understanding how college students experiencing comorbid anxiety and depression symptoms engage with alcohol is a vital component of our ability to develop targeted interventions. Gender is an important factor to consider given the differential associations between anxiety or depression on alcohol use. This study compares rates of weekly drinking, hazardous drinking, and alcohol-related negative consequences among college students with symptoms of comorbid anxiety and depression compared to their non-symptomatic peers. We hypothesized that men and students with comorbid anxiety and depression will drink more heavily and experience more negative consequences than women and non-symptomatic students.
Materials and Methods
Participants and procedures
Participants comprised 678 traditional-aged college students (M=20.08, SD=1.52) from a single university in the southeastern region of the US who endorsed alcohol use in the last month. The majority of the sample was female (69.5%) and non-Hispanic White (62.5%). Other racial categories include Black (29.6%), Hispanic (1.8%), American Indian/Alaska Native (1.2%), Asian (1%), Native Hawaiian/Pacific Islander (0.4%), and Other (3.4%). Recruitment was done through an online recruitment system (i.e., SONA), with class credit being given in exchange for participation. Interested participants were directed to a secure online system (Qualtrics) where they completed a University Institutional Review Board-approved informed consent, followed by a series of measures of mental health and drinking behaviors.
Measures
Alcohol Use Disorders Identification Test (AUDIT).
The AUDIT is a 10-item self-report measure developed by the World Health Organization to assess hazardous drinking (Flemming et al., 1991; Saunders et al., 1993). Respondents answer a series of questions related to their drinking, using a five-point scale. Example items and response options include “How often do you have a drink containing alcohol” (0 – never to 4 – 4 or more times a week) and “Have you or someone else been injured as a result of your drinking?” (0 – no to 4 – yes, during the last year). The AUDIT has been studied extensively and found to have strong psychometric properties (Reinert & Allen, 2002). Internal consistency with this sample was good (α = .81).
Daily Drinking Questionnaire (DDQ).
The DDQ was used to categorize respondents by how much alcohol they consume (Collins et al., 1985). Specifically, the DDQ measures weekly alcohol use with a self-report survey asking participants to indicate how many standard drinks they had in a typical week of the past month, producing an approximation of frequency and volume. Drinks are summed across days to calculate drinks per week. Weekly drinking has been found to be highly related to problems caused by alcohol (Borsari et. al., 2001).
Depression Anxiety Stress Scales (DASS).
The DASS is a 21-item self-report measure that assesses symptoms of stress, anxiety, and depression (Antony et al., 1998; Osman et al., 2012). Respondents indicate the extent to which each statement applies to them using a four-point scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). The current study used the depression and anxiety subscales. Example items include, “I felt I was close to panic” (anxiety) and “I could see nothing in the future to be hopeful about” (depression). The DASS-21 has demonstrated strong psychometric properties (Brown et al, 1997). Internal consistencies were good with this sample (anxiety = .87; depression = .87).
Rutgers Alcohol Problem Index (RAPI).
The RAPI (White & Labouvie, 1989) is a 23-item self-report scale that measures the frequency of negative alcohol-related consequences. The RAPI assesses consequences across multiple domains with items such as “neglected your responsibilities” and “had a fight, argument or bad feelings with a friend”. Respondents indicate the frequency of each consequence using a five-point scale (0: never to 4: 10 or more times). The RAPI has demonstrated strong psychometric properties (e.g., Neal et. al., 2006). Internal consistency with this sample was excellent (α = .95).
Planned analyses
A 2 (comorbid status: yes or no) x 2 (gender: men or women) multivariate analysis of variance (MANOVA) was conducted to examine mean differences on three drinking outcomes (i.e., weekly alcohol use, hazardous drinking, and alcohol-related consequences). Several descriptive analyses were performed to confirm the appropriateness of conducting a MANOVA. First, MANOVA involves several assumptions that were examined, including data normality, linearity and homogeneity of variances. Though violation of assumptions may weaken the power of the analysis, one potential explanation for such violations may be unequal sample sizes across groups. Next, bivariate correlations of the three dependent variables were performed to assure that the three drinking variables were not strongly associated and MANOVA, rather than ANOVA or a structural equation model (SEM) approach is appropriate. A MANOVA permits the evaluation of all three drinking outcomes simultaneously, offering important information about which of the drinking variables may be driving the difference between groups while also mitigating possible Type I error by conducting three separate analyses of covariance (ANOVAs). Finally, Eta-squared (η2) offers an effect size estimate such that η2 = .01 is a small effect, η2 = .06 is a medium effect, and η2 = .14 is a large effect (Cohen, 1988).
Results
Descriptive analyses
Means, standard deviations, and intercorrelations of study measures are presented in Table 1. Of the total sample, 300 participants (44.3%) endorsed no anxiety or depression symptoms, 234 (34.6%) endorsed symptoms of both anxiety and depression, and 143 (22.1%) endorsed symptoms of anxiety or depression. Given the small number of participants who endorsed only anxiety (n=38; 5.6%) or only depression (n=105; 15.5%), we restricted the primary analyses to participants with or without co-occurring anxiety and depression. Regarding drinking outcomes, 263 participants (38.8% of the total sample) exceeded the clinical cutoff score on the AUDIT (i.e., score>7), indicating hazardous drinking levels (Devos-Comby & Lang, 2008). The drinking variables were moderately associated (.43<r<.57), supporting the application of MANOVA.
Table 1.
Means, standard deviations, and intercorrelations of study measures
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
|
| |||||
| 1. Depression | --- | ||||
| 2. Anxiety | .74* | --- | |||
| 3. Weekly drinking | .13* | .18* | --- | ||
| 4. Hazardous drinking | .27* | .27* | .53* | --- | |
| 5. Negative Consequences | .37* | .44* | .43* | .57* | --- |
| Total: M (SD) | 5.21 (4.54) | 3.84 (4.26) | 14.67 (16.37) | 7.26 (5.35) | 10.95 (13.22) |
| Women: M (SD) | 5.20 (4.63) | 3.74 (4.28) | 11.78 (12.82) | 6.45 (4.77) | 9.32 (11.30) |
| Men: M (SD) | 5.25 (4.38) | 4.06 (4.23) | 21.42 (21.06) | 9.14 (6.10) | 14.80 (16.25) |
Note. Depression and anxiety refer to total scores on the DASS subscales
p < .001
Primary analyses
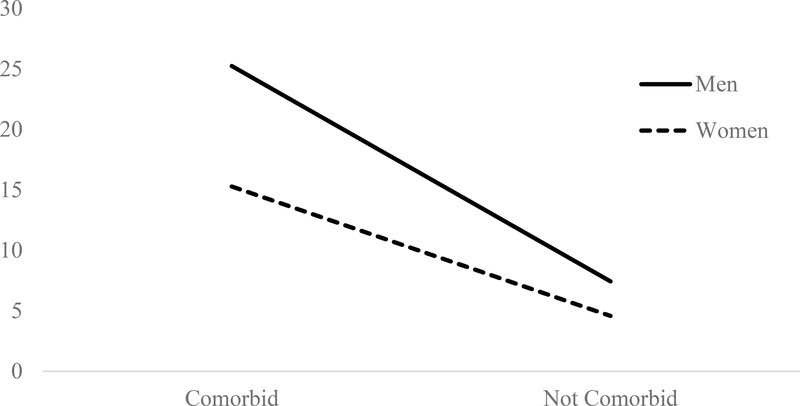
Results demonstrated significant multivariate main effects of comorbidity status (Wilk’s λ = .75, F (3, 526) = 57.39, p < .001) and gender (Wilk’s λ = .91, F (3, 526) = 17.18, p < .001), as well as an interaction effect between comorbidity status and gender (Wilk’s λ = .98, F (3, 526) = 4.17, p < .01) on drinking outcomes. An examination of univariate effects revealed significant differences in comorbidity status and gender on each of the three drinking outcomes (see Table 2). Specifically, participants with co-occurring anxiety and depression symptoms reported more weekly drinking (η2=.02), hazardous drinking (η2=.10), and alcohol-related consequences (η2=.24) than participants with no symptoms. Further, college men reported more weekly drinking (η2=.06), hazardous drinking (η2=.05), and alcohol-related consequences (η2=.06) than college women. The main effect on alcohol-related negative consequences was qualified by a significant interaction effect (F (1, 528) = 10.31, p < .001) such that participants who endorsed co-occurring anxiety and depression symptoms and were male reported the most alcohol-related consequences (η2=.02; see Figure 1).
Table 2.
Main effects of comorbid status and gender on drinking outcomes
| Comorbid status effects | Comorbid | Not comorbid | F-test | Eta-Squared | ||
|
| ||||||
| M | SD | M | SD | |||
| Weekly drinking | 18.43 | 20.09 | 12.86 | 14.30 | 12.92* | .024 |
| Hazardous drinking | 9.35 | 5.80 | 5.68 | 4.58 | 60.48* | .103 |
| Negative consequences | 18.47 | 16.14 | 5.43 | 7.71 | 165.41* | .239 |
| Gender effects | Men | Women | F-test | Eta-Squared | ||
|
| ||||||
| M | SD | M | SD | |||
| Weekly drinking | 21.74 | 21.98 | 12.44 | 13.84 | 34.80* | .062 |
| Hazardous drinking | 9.14 | 6.11 | 6.48 | 4.94 | 29.90* | .054 |
| Negative consequences | 15.59 | 17.20 | 9.20 | 11.42 | 33.52* | .06 |
Note. Findings obtained from 2 (comorbid status) × 2 (gender) ANOVA model
p < .001
Figure 1.
Interaction of comorbidity status and gender on raw mean scores for alcohol-related negative consequences.
Exploratory analyses
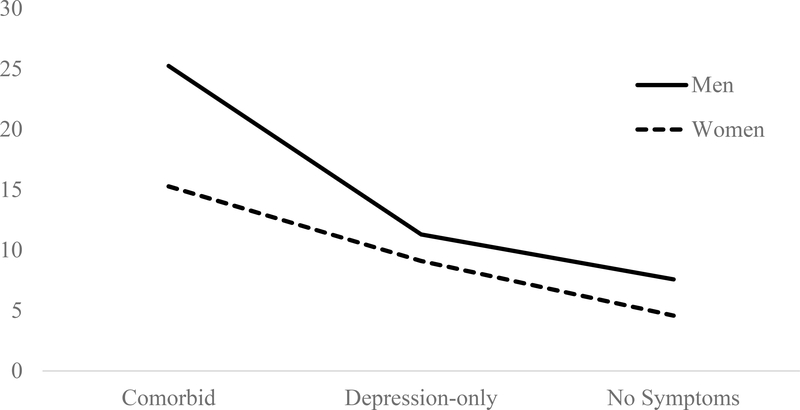
We performed an exploratory 3 (comorbid status: no, depression-only, depression and anxiety) x 2 (gender: men or women) MANOVA to determine if differences in drinking outcomes would emerge between participants with depression only and those with depression and anxiety. Multivariate analyses demonstrated significant main effects of comorbidity status (Wilk’s λ = .77, F (6, 1256) = 29.50, p < .001) and gender (Wilk’s λ = .93, F (3, 628) = 16.63, p < .001), as well as an interaction effect between comorbidity status and gender (Wilk’s λ = .97, F (6, 1256) = 2.88, p < .01). Univariate analyses also revealed significant main effects of comorbid status and gender on each drinking outcome (see Table 3). Post-hoc analyses revealed participants with comorbid anxiety and depression endorsed more weekly and hazardous drinking than participants in the depression-only and no symptoms conditions. Further, participants in the depression-only condition endorsed more hazardous, but not weekly drinking than participants in the no symptoms condition (see Table 3). A significant interaction was found on negative consequences (F (2, 630) = 6.47, p < .01) such that men with comorbid anxiety and depression reported more negative consequences than women with comorbid symptoms and participants with depression-only or no symptoms (η2=.02; see Figure 2).
Table 3.
Exploratory effects of comorbid status and gender on drinking outcomes
| Comorbid status effects | Comorbid | Depression-only | No Symptoms | F-test | Eta-Squared | Comparisons (p < .05) | |||
|
| |||||||||
| M | SD | M | SD | M | SD | ||||
| Weekly drinking | 18.43 | 20.09 | 12.97 | 11.77 | 12.86 | 14.30 | 7.72* | .024 | C > D; C > N |
| Hazardous drinking | 9.35 | 5.80 | 7.61 | 5.33 | 5.68 | 4.58 | 30.27* | .088 | C > D > N |
| Negative consequences | 18.47 | 16.14 | 9.73 | 9.58 | 5.43 | 7.71 | 88.8* | .22 | C > D > N |
| Gender effects | Men | Women | F-test | Eta-Squared | |||||
|
| |||||||||
| M | SD | M | SD | ||||||
| Weekly drinking | 21.47 | 21.14 | 12.05 | 13.08 | 38.86* | .058 | |||
| Hazardous drinking | 9.25 | 6.19 | 6.51 | 4.85 | 33.32* | .05 | |||
| Negative consequences | 14.92 | 16.45 | 9.18 | 11.03 | 21.03* | .032 | |||
Note. Findings obtained from 3 (comorbid status) × 2 (gender) ANOVA models
p < .001
Figure 2.
Interaction of comorbidity status (3 conditions) and gender on raw mean scores for alcohol-related negative consequences.
Discussion
Despite evidence demonstrating unique effects of anxiety and depression symptoms on problematic drinking among college students, less is known about the drinking patterns of those with both anxiety and depression. The current study evaluated the drinking patterns of students with anxiety and depression symptoms in comparison to their non-symptomatic peers. As hypothesized, participants with anxiety and depression symptoms and college men reported more problematic drinking than their non-symptomatic peers and college women. Gender impacted the relationship between mental health and alcohol-related negative consequences such that college men who endorsed co-occurring anxiety and depression symptoms endorsed the most negative consequences. Finally, exploratory analyses suggested that students with anxiety and depression engaged in more problematic drinking than students with only depression symptoms.
Our finding of higher weekly and hazardous drinking among students with anxiety and depression symptoms is consistent with prior work on the effects of depression or anxiety on drinking behavior (Geisner et al., 2012; Nourse et al., 2017). These students also endorsed more risky drinking than students with only depression symptoms, highlighting the need to focus on the composition of mental health issues. While the smaller sample of depression-only students is a notable limitation, examination of factors that may underlie depression, anxiety, and alcohol use is needed. Drinking to cope is one such established factor in substance use research (Ham & Hope, 2003; Park & Levenson, 2002). The students in this study with anxiety and depression symptoms likely experienced a more aversive mental state than their depression-only and non-symptomatic peers. While a higher motivation to drink to cope is one possible explanation, additional investigation of factors underlying anxiety/depression and alcohol use, particularly in contrast to depression and alcohol use, is needed.
Consistent with previous research, men in our study endorsed more problematic drinking patterns than women (Ham & Hope, 2003; O’Malley & Johnston 2002). Further, men with anxiety and depression symptoms reported more negative alcohol-related consequences than all other groups. In general, larger quantities of alcohol consumed leads to more consequences, but this interaction effect suggests other factors in the mix. Despite some consistency with prior studies (e.g., Geisner et al., 2004), our findings only revealed gender differences in alcohol-related consequences among participants with anxiety and depression, not those with depression only. It may be that men endorsing comorbid anxiety and depression symptoms were experiencing higher levels of psychological distress than their depression-only or non-symptomatic counterparts. The problematic outcomes for men in particular may also stem from gender differences in resource utilization. Specifically, women are more likely than men to seek support and professional help to manage their negative affect (Mackenzie et al., 2006; Taylor, 2011). Not utilizing such resources may leave men more vulnerable to substance use as a management strategy.
In this analysis, we assumed anxiety and depression were present prior to heavy drinking behavior, based on existing epidemiological and longitudinal studies (Cheng et al., 2004; Goodwin et al., 2004; Holahan et al., 2003). With anxiety, this pattern is fairly consistent in the research (e.g., Villarosa-Hurlocker et al., 2018). Drinking to cope with symptoms of depression is also common, although the temporal relationship is less clear. Some evidence suggests that alcohol use predicts later depression (Boden & Fergusson, 2011). One possible reason is that heavy drinking can induce depression. It is possible to distinguish between people experiencing depression induced by alcohol and those with depression independent from alcohol use, with the latter group displaying a weaker link between depressive symptoms and drinking behavior (Preuss et al, 2002; Schuckit et al, 2013). While these studies focused on clinical adults, it’s worth noting that the effect of depression predicted by alcohol use exists, and we may have ordered these two variables in the wrong direction.
There are several clinical implications of study findings. Anxiety, depression, and alcohol use disorders are the most prevalent mental health concerns among college students, in part due to their high comorbidity. Interventions for alcohol misuse alone are not effective in individuals with comorbid mood/anxiety issues (e.g., Terlecki et al., 2011). Best practices recommend that alcohol use and mental health symptoms be addressed simultaneously, as treatment of only one condition is unlikely to succeed. Screening students for problematic drinking and other mental health issues is an important first step. Further, incorporating mood and anxiety management strategies into alcohol interventions for these students may help assure positive outcomes. Our study also speaks to the need to target college men with awareness campaigns to mitigate negative alcohol-related consequences particularly during times of elevated depression/anxiety.
Limitations
This study did have some limitations. First, our self-report measure of depression and anxiety suggested the presence of anxiety and depression symptoms as opposed to the disorders themselves. While there are benefits to studying sub-clinical populations, use of self-report tools instead of a clinical interview prevents us from distinguishing between participants with clinically diagnosable mood or anxiety disorders. Second, while important information can be gleaned from our exploratory analyses, the number of participants who endorsed only depression warrants caution and future replication. Further, the very small proportion of participants with only anxiety precluded any exploratory analyses with this subgroup. Replication with a larger sample to compare students with no mood/anxiety, only mood, only anxiety, and both mood/anxiety symptoms will be critical to improve prevention and intervention efforts. Third, this study was cross-sectional in nature, precluding any causal interpretation of findings. Future work would benefit from experimental and longitudinal designs to evaluate the temporal association among depression, anxiety, and alcohol use. Finally, data was collected from a single institution and comprised primarily White, non-Hispanic women. Replication with a larger and more diverse sample is needed.
Future directions
This study leaves the door open for a variety of future directions. First, there are newer, effective methods to better capture college students’ dynamic drinking patterns. For example, our alcohol use tools were unable to differentiate between 6 drinks consumed over four hours and 4 drinks over ten minutes. Ecological momentary methods are one way to better capture student drinking habits, as well as the naturally fluctuating role of mood and anxiety symptoms. Another area of future study could focus on specific types of alcohol-related consequences and their relation to gender. For example, a more detailed examination of sexual assault-related consequences can help identify those students that are more vulnerable and more likely to sexual assault under the influence of alcohol regardless of gender (Abbey et al., 2004; Perkins, 2002).
Conclusion
Our findings highlight the importance of examining mental health when looking at student drinking. College drinkers with symptoms of anxiety and depression appear to be at higher risk for problematic drinking than their non-symptomatic peers. Our findings indicate that this high-risk group is fairly large, which is concerning given the growing number of students reporting anxiety/depression symptoms in conjunction with their generally heavy drinking behavior. College men with anxiety and depression appear at greatest risk for problematic drinking and prevention and intervention efforts should target these students.
Acknowledgments
Funding: This work was supported by the National Institutes of Health [L30 AA027026].
Footnotes
Declarations of Interest: None
References
- Abbey A, Zawacki T, Buck PO, Clinton AM, & McAuslan P (2004). Sexual assault and alcohol consumption: What do we know about their relationship and what types of research are still needed? Aggression and Violent Behavior, 9(3), 271–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association. (2019). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2019. Silver Spring, MD: American College Health Association. [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, & Swinson RP (1998). Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychological Assessment, 10, 176–181. [Google Scholar]
- Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, Kessler RC, Liu H, Mortier P, Nock MK, Pinder-Amaker S, Sampson NA, Aguilar-Gaxiola S, Al-Hamzawi A, Andrade LH, Benjet C, Caldas-de-Almeida JM, Demyttenaere K,…Bruffaerts R. (2016). Mental disorders among college students in the World Health Organization world mental health surveys. Psychological Medicine, 46(14), 2955–2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, & Olfson M (2008). Mental health of college students and their non–college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Archives of General Psychiatry, 65(12), 1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden JM, & Fergusson DM (2011). Alcohol and depression. Addiction, 106(5), 906–914. [DOI] [PubMed] [Google Scholar]
- Borsari B, Neal DJ, Collins SE, & Carey KB (2001). Differential utility of three indexes of risky drinking for predicting alcohol problems in college students. Psychology of Addictive Behaviors, 15(4), 321–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, & Barlow DH (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behavior Research and Therapy, 35, 79–89. [DOI] [PubMed] [Google Scholar]
- Capron DW, Bauer BW, Madson MB, & Schmidt NB (2018). Treatment seeking among college students with comorbid hazardous drinking and elevated mood/anxiety symptoms. Substance Use & Misuse, 53(6), 1041–1050. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2018). National Survey on Drug Use and Health 2016 (NSDUH-2016-DS0001). Retrieved from https://datafiles.samhsa.gov/.
- Cheng AT, Gau SF, Chen TH, Chang JC, & Chang YT (2004). A 4-year longitudinal study on risk factors for alcoholism. Archives of General Psychiatry, 61(2), 184–191. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Erlbaum, USA. [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53, 189–200. [DOI] [PubMed] [Google Scholar]
- Devos-Comby L, & Lang JE (2008). Standardized measures of alcohol-related problems: A review of their use among college students. Psychology of Addictive Behaviors, 22(3), 349–361. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Barry KL, & MacDonald R (1991). The Alcohol Use Disorders Identification Test (AUDIT) in a college sample. International Journal on Addiction, 26(11), 1173–1185. 10.3109/10826089109062153. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, & Neighbors C (2004). The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors, 29, 843–848. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Mallett K, & Kilmer JR (2012). An examination of depressive symptoms and drinking patterns in first year college students. Issues in Mental Health Nursing, 33(5), 280–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM, Reynolds B, & Skewes MC (2011). Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacology, 19(4), 303–313. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, & Horwood LJ (2004). Association between anxiety disorders and substance use disorders among young persons: results of a 21-year longitudinal study. Journal of Psychiatric Research, 38(3), 295–304. [DOI] [PubMed] [Google Scholar]
- Ham LS, & Hope DA (2003). College students and problematic drinking: A review of the literature. Clinical Psychology Review, 23(5), 719–759. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA (2001). The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Primary Care Companion Journal of Clinical Psychiatry, 3, 244–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, & Randall PK (2003). Drinking to cope and alcohol use and abuse in unipolar depression: A 10-year model. Journal of Abnormal Psychology, 112(1), 159–165. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, & Wang PS (2003). The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289(23), 3095–3105. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25(7), 841–861. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Krueger R, Frye B, & Peterson J (2008). Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In Stewart SH & Conrod PJ (Eds.), Anxiety and substance use disorders (pp 3–33). Springer. [Google Scholar]
- Linden-Carmichael AN, & Lanza ST (2018). Drinking patterns of college-and non-college-attending young adults: is high-intensity drinking only a college phenomenon? Substance Use & Misuse, 53(13), 2157–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo CC, Monge AN, Howell RJ, & Cheng TC (2013). The role of mental illness in alcohol abuse and prescription drug misuse: Gender-specific analysis of college students. Journal of Psychoactive Drugs, 45(1), 39–47. [DOI] [PubMed] [Google Scholar]
- Mackenzie CS, Gekoski WL, & Knox VJ (2006). Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging and Mental Health, 10(6), 574–582. [DOI] [PubMed] [Google Scholar]
- Neal DJ, Corbin WR, & Fromme K (2006). Measurement of alcohol-related consequences among high school and college students: Application of item response models to the Rutgers Alcohol Problem Index. Psychological Assessment, 18(4), 402–414. [DOI] [PubMed] [Google Scholar]
- Norberg MM, Norton AR, Olivier J, & Zvolensky MJ (2010). Social anxiety, reasons for drinking, and college students. Behavior Therapy, 41(4), 555–566. [DOI] [PubMed] [Google Scholar]
- Nourse R, Adamshick P, & Stoltzfus J (2017). College binge drinking and its association with depression and anxiety: a prospective observational study. East Asian Archives of Psychiatry, 27(1), 18–25. [PubMed] [Google Scholar]
- O’Malley PM, & Johnston LD (2002). Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Alcohol Supplement, 63(2), 23–40. [DOI] [PubMed] [Google Scholar]
- Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, & Lozano G (2012). The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. Journal of Clinical Psychology, 68, 1322–1338. [DOI] [PubMed] [Google Scholar]
- Park CL, & Levenson MR (2002). Drinking to cope among college students: prevalence, problems and coping processes. Journal of Studies on Alcohol, 63(4), 486–497. [DOI] [PubMed] [Google Scholar]
- Perkins HW (2002). Surveying the damage: a review of research on consequences of alcohol misuse in college populations. Journal of Studies on Alcohol, supplement, (14), 91–100. [DOI] [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith TL, Danko GP, Dasher AC, Hesselbrock MN, Hesselbrock VM, & Nurnberger JI (2002). A comparison of alcohol-induced and independent depression in alcoholics with histories of suicide attempts. Journal of Studies on Alcohol, 63, 498–502. [DOI] [PubMed] [Google Scholar]
- Reinert DF, & Allen JP (2002). The Alcohol Use Disorder Identification Test (AUDIT): A review of recent research. Alcoholism: Clinical and Experimental Research, 26(2), 272–279. [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, & Kalmijn J (2013). Relationships among independent major depression, alcohol use, and other substance use and related problems over 30 years in 397 families. Journal of Studies on Alcohol and Drugs, 74(2), 271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE (2011). Social support: A review. In Friedman HS (Ed.), Oxford library of psychology. The Oxford handbook of health psychology (pp. 189–214). Oxford University Press. [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, & Copeland AL (2011). The role of social anxiety in a brief alcohol intervention for heavy-drinking college students. Journal of Cognitive Psychotherapy, 25, 7–21. [Google Scholar]
- Villarosa MC, Messer MA, Madson MB, & Zeigler-Hill V (2017). Depressive symptoms and drinking outcomes: The mediating role of drinking motives and protective behavioral strategies among college students. Substance Use and Misuse, 53(1), 143–153. [DOI] [PubMed] [Google Scholar]
- Villarosa-Hurlocker MC, Whitley RB, Capron DW, & Madson MB (2018). Thinking while drinking: Fear of negative evaluation predicts drinking behaviors of students with social anxiety. Addictive Behaviors, 78, 160–165. [DOI] [PubMed] [Google Scholar]
- Weitzman E (2004). Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease, 192(4), 269–277. [DOI] [PubMed] [Google Scholar]
- White HR, & Labouvie EW (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50, 30–37. [DOI] [PubMed] [Google Scholar]