Since 2019, an epidemic of pneumonia of unknown cause occurred around the world.[1] The analysis of respiratory tract samples led to the identification of a novel coronavirus, which was named 2019 novel coronavirus (2019-nCoV). Epidemiological data showed that 2019-nCoV could spread rapidly from person to person and cause coronavirus disease-19 (COVID-19). The high infectivity of COVID-19 has led to a rapid increase in the number of cases and caused a global pandemic. To date, 2019-nCoV has infected millions of people and caused hundreds of thousands of deaths worldwide. These numbers are updated every day and are expected to increase further at a great rate. COVID-19 has now become a serious threat to public health worldwide.
The increasing number of cases worldwide has resulted in a large-scale shortage of medical resources. Treatment classification according to the severity of the patients’ condition has been widely used to ensure the rational use of medical resources. However, it should be noted that some patients with mild initial symptoms show rapid deterioration to asphyxia. Thus, it is important to accurately predict and evaluate the severity of illness on admission. Computed tomography (CT) images can objectively show lung changes in patients with COVID-19. Therefore, CT can be used for the rapid diagnosis and assessment of COVID-19 pneumonia.
We retrospectively collected data from pneumonia patients with confirmed COVID-19 admitted to a hospital in Wuhan City, Hubei Province, between January and March 2020. The study was approved by the Ethics Review Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 2020-NA-0127), and the need for informed consent was waived.
The definitions of confirmed 2019-nCoV infection were based on the interim guidance from the World Health Organization.[1] Throat swab specimens were collected from patients and analyzed using real-time reverse transcription-polymerase chain reaction (RT-PCR) using a standard RT-PCR protocol. Only patients with positive laboratory test results were included in this study. Patients who did not undergo chest CT were excluded. During the study period, 90 patients with laboratory-confirmed 2019-nCoV infection admitted to the designated tertiary hospitals in Wuhan were included. After treatment, all patients recovered and were discharged. We used standardized data forms to collect clinical data. The doctors who treated patients with COVID-19 on the front line collected and reviewed the data.
Parameters assessed at the time of hospital admission included demographic data (age and sex), clinical symptoms (fever, cough, sputum production, dyspnea, or respiratory distress, weakness, myalgia, and pharyngalgia), and comorbidities (chronic obstructive pulmonary diseases [COPD], hypertension, diabetes, cardiovascular conditions, chronic renal or liver insufficiency, and malignancies). The severity of illness on admission was measured according to the Diagnosis and Treatment Plan of Coronavirus Disease (seventh edition).
All patients underwent chest CT immediately after hospitalization. Chest CT images were reviewed by two experienced radiologists in consensus. Whenever a consensus could not be reached, a third experienced radiologist was consulted to reach the final decision. The radiologists were blinded to the patient's status and the severity of the patient's clinical symptoms.
The types of lesions on chest CT images, such as ground-glass opacities (GGOs), consolidation, reticular patterns, nodular opacities, and bronchiectasis, were evaluated as well as the type of lesion distribution (unilateral/bilateral, solitary/multiple/diffuse). A GGO is defined as a hazy area of increased lung opacity with indistinct margins of pulmonary vessels on radiography but with preserved bronchial and vascular margins on CT. Consolidation is defined as a homogeneous increase in parenchymal attenuation that obscures vessel margins and airway walls, and a nodular opacity is defined as a rounded opacity that is well or poorly defined. On CT, the diameter ratio of normal bronchus to accompanying pulmonary artery (measured from the outer wall to the opposite outer wall) is about 1:1. Bronchiectasis is defined as the diameter of the bronchus larger than that of the accompanying pulmonary artery. Bronchial wall thickening, mucus plug, and bronchial shadow in peripheral lung tissue are also auxiliary signs.
In total, 90 patients were included, of which 47 were male and 43 were female. The mean age was 55.1 ± 13.9 years. The results of the initial throat swab test were positive in 76 (87.4%) patients. Among these patients, 64 (73.6%) patients had mild or common disease, 23 (25.6%) had severe disease, and 3 (3.3%) had a critical disease. The most common presenting symptoms were fever (90.2%) and cough (68.9%), and 28 (31.1%) patients showed rapid progression to dyspnea (the meantime from onset of illness to dyspnea was 1.4 ± 2.9 days). Hypertension (22.2%) and diabetes (11.1%) were the most common comorbidities. In addition, two patients had COPD. One of them was assessed as a severe disease and the other was a critical disease. None of the patients were found to have a history of bronchiectasis.
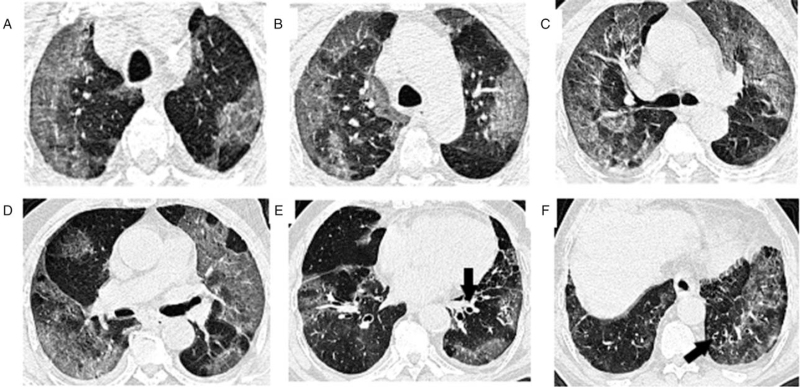
Regarding the CT findings, all patients presented with GGOs, and 70 (77.8%) patients had interstitial changes in their lungs. These two were the most common findings. Besides, 39 (43.3%) patients showed pulmonary consolidations, 18 (20.0%) patients showed local patchy shadowing, and 14 (15.6%) patients showed bronchiectasis. Other findings included bronchial wall thickening, a small pleural effusion, and a small pericardial effusion. Similar to chest imaging findings noted in viral pneumonia, bilateral GGOs, and/or unilateral pulmonary consolidation were observed in the majority of patients. Figure 1 shows the lung CT images of a critically ill patient.
Figure 1.
Lung CT images in patients with severe COVID-19 pneumonia: (A–F) different levels of unenhanced lung CT images of a 79-year-old man with confirmed COVID-19, assessed as a critical disease. CT images show multiple ground-glass opacities and consolidation changes. Bronchiectasis and thickening of the bronchial wall are also presented (arrow). CT: Computed tomography; COVID-19: Coronavirus disease 2019.
We further evaluated the correlation between CT findings and clinical severity. We found that bronchiectasis and pulmonary consolidation were associated with increased severity. A multivariable-adjusted model showed that these relationships persisted (odds ratio [OR]=3.78; 95% confidence interval [CI], 0.95–15.06; P = 0.050 for bronchiectasis; OR = 24.91; 95% CI, 5.07–122.28; P < 0.001 for pulmonary consolidation) after controlling for age, sex, COPD, hypertension, diabetes, cardiovascular conditions, chronic renal or liver insufficiency, and malignancies. The adjustments were made to eliminate the possible influence of these risk factors.
The study found that bronchiectasis on chest CT is observed more frequently in patients with severe COVID-19 disease than in those with mild or common COVID-19. The presence of bronchiectasis could be a useful marker for severe pulmonary damage caused by COVID-19. In a recent autopsy report, pathological examination confirmed that the iliac bronchioles and terminal iliac bronchioles were filled with dense thick “mucus plugs” obstructing the lower respiratory tract.[2] The exudation and necrosis of the bronchial mucosa lead to the accumulation and agglomeration of mucus in the bronchi. According to our chest CT findings and the pathological results from the autopsy study, bronchiectasis may be a result of the formation of mucus plugs in COVID-19 patients. Further analysis of the biochemical changes involved in bronchiectasis is needed to clarify the mechanism(s) underlying the above correlation.
In the past, some attention has been paid to CT findings in adults with COVID-19. Shi et al[3] reported rapid evolution from focal unilateral GGOs to diffuse bilateral GGOs and the co-existence of consolidations within 1 to 3 weeks of COVID-19 onset. Guan et al[4] extracted data on 1099 patients and found that when patients were initially admitted, GGO was the most common finding on chest CT.
The multivariable-adjusted model eliminates the possible impact of COPD on the prognosis of patients. However, because the number of patients with COPD is too small, the association between COPD and the severity of COVID-19 needs further study.
Compared to chest radiography, chest CT is more sensitive for the detection of GGOs and more effective in the early detection of COVID-19 pneumonia. Chest CT is easy to perform, fast, and highly sensitive for detecting COVID-19 pneumonia in the early stage. Therefore, it provides more accurate and timely information with respect to diagnosis, severity, and treatment. In patients with COVID-19, bronchiectasis, GGOs, and pulmonary consolidation on chest CT were associated with severity. This is of great significance with respect to the clinical diagnosis and severity staging of COVID-19 pneumonia. Chest CT can further help guide the provision of personalized and precise treatment.
Conflicts of interest
None.
Footnotes
How to cite this article: Peng P, Wang F, Tang ZR, Liu X, Zhang ZH, Song H, Zhu BL, Liu S, Liu Y, Xu XG, Liu MH, Zhou LF, Jiang T. Bronchiectasis is one of the indicators of severe coronavirus disease 2019 pneumonia. Chin Med J 2021;134:2486–2488. doi: 10.1097/CM9.0000000000001368
Peng Peng, Feng Wang, and Zi-Ren Tang contributed equally to this work.
References
- 1.Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (nCoV) Infection is Suspected: Interim Guidance. World Health Organization Web site, 2020. Available from: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-whennovel-coronavirus-(ncov)-infection-is-suspected. [Accessed January 11, 2020]. [Google Scholar]
- 2.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020; 8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi HS, Han XY, Jiang NC, Cao YK, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y, Liang WH, Zhong NS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]