Abstract
Background
In the age of COVID-19 and enforced social distancing, changes in patterns of trauma were observed but poorly understood. Our aim was to characterize traumatic injury mechanisms and acuities in 2020 and compare them with previous years at our level I trauma center.
Material and methods
Patients with trauma triaged in 2016 through 2020 from January to May were reviewed. Patient demographics, level of activation (1 versus 2), injury severity score, and mechanism of injury were collected. Data from 2016 through 2019 were combined, averaged by month, and compared with data from 2020 using chi-squared analysis.
Results
During the months of interest, 992 patients with trauma were triaged in 2020 and 4311 in 2016-2019. The numbers of penetrating and level I trauma activations in January-March of 2020 were similar to average numbers for the same months during 2016 through 2019. In April 2020, there was a significant increase in the incidence of penetrating trauma compared with the prior 4-year average (27% versus 16%, P < 0.002). Level I trauma activations in April 2020 also increased, rising from 17% in 2016 through 2019 to 32% in 2020 (P < 0.003). These findings persisted through May 2020 with similarly significant increases in penetrating and high-level trauma.
Conclusions
In the months after the initial spread of COVID-19, there was a perceptible shift in patterns of trauma. The significant increase in penetrating and high-acuity trauma may implicate a change in population dynamics, demanding a need for thoughtful resource allocation at trauma centers nationwide in the context of a global pandemic.
Keywords: COVID-19, Trauma, Penetrating, High acuity, Gun violence
Introduction
The triage, stabilization, and care of patients with traumatic injuries place great demand on hospital resources. Understanding factors that influence the trauma incidence is essential for efficient resource allocation. Overall, traumatic injuries occur more often on warmer days, and penetrating trauma peaks in the early hours of the morning.1, 2, 3, 4, 5, 6 Motor vehicle collisions (MVCs) often surge during times of heavy traffic.1, 2, 3, 4, 5, 6 It is clear that a population's activity informs the trauma it sustains.
Northern California's Bay Area comprises nine socioeconomically diverse counties including and surrounding San Francisco. Bay Area firearm purchases increased after the start of the COVID-19 pandemic more than after any prior national event with an observed increased relative risk of firearm-related death or injury directly attributable to this new gun ownership.7 Trauma trends through the early months of the pandemic were mixed, varying between types of hospitals, their locations, and the populations they serve. Many centers across the United States observed a decrease in overall trauma, whereas a few hospital systems reported increased firearm trauma consistent with these changing purchasing trends.8, 9, 10
The COVID-19 pandemic served as an unprecedented agent of change. With the advent of social distancing, travel bans, and shelter-in-place restrictions, millions of people lost jobs and entered poverty, creating new socioeconomic stress.11 , 12 Shortages in personal protective equipment, changes to trauma team structure, and shifts in resource allocation altered the way providers cared for patients with trauma. Although the focus was on providers directly attending to patients with COVID-19, shortages in personal protective equipment or trauma-team staff can also impact the care of other critically ill patients. Exploring how trauma changed during the early months of the pandemic is vital to understanding the impact that reallocated resources and reduced staffing can have on the triage and management of patients with trauma.
The aim of this study was to investigate changes in distribution of mechanisms and acuities of traumatic injuries sustained by patients triaged to an urban, safety-net, level I trauma center during the COVID-19 pandemic. We hypothesized that the COVID-19 pandemic and its resulting societal stressors increased the incidence of penetrating trauma and overall trauma acuity.
Methods
We conducted a retrospective cohort study at our institution, Highland Hospital, located in Oakland, California. Highland Hospital is the only level I trauma center in Northern California's “East Bay,” serving an ethnically and socioeconomically diverse population. We have a retrospectively maintained trauma database (Trauma One) obtained from the electronic health record. This study was conducted as approved by the Alameda Health Institutional Review Board (institutional review board number: 20-05081A).
Patients triaged to Highland Hospital in the months of January through May in the years 2016 through 2020 were included in this study. Clinical and demographic data were collected using the Trauma One database. There were no exclusion criteria. As this was a retrospective review, informed consent was not obtained from patients with trauma studied, as approved by institutional review board waiver. Data collected consisted of patient demographics, injury acuity, mechanism class and type, injury severity score (ISS), arrival vital signs, and time to the operating room. Patients with the highest acuity traumatic injuries were triaged as “level I” on hospital arrival, and less acutely ill patients were triaged as “level II” (Table 1 ). Level II traumas require the presence of the trauma team which comprised four general surgery residents, a resuscitation resident (general surgery or emergency medicine), an intensive care unit–level trauma nurse, and an emergency medicine resident to perform a focused assessment with sonography in trauma examination. Level I traumas also activate trauma surgery, emergency medicine, and anesthesia attendings, an airway team (emergency medicine resident and attending, a respiratory therapist), a social worker, and a member of the blood bank staff.
Table 1.
Characteristics of level I trauma.
| Level I activation criteria |
|---|
| Penetrating injury of the head, neck, torso, or extremities proximal to and including elbow or knee |
| Paralysis (i.e. spinal cord injury) |
| Fracture of two or more long bones |
| Amputation proximal to the wrist or ankle |
| Burns ≥30% total body surface area (TBSA) |
| Systolic blood pressure <90 at any time |
| GCS 9 and under |
| Age 14 y or younger |
| Intubated before arrival |
| Respiratory rate <10 or >30, in need of an emergency airway |
Before analysis, data were divided by month to control for seasonal factors and allow direct comparison between each month of 2020 and the same month across 2016 through 2019. Patients were then divided into prepandemic (2016 through 2019) and pandemic cohorts (2020). The primary outcomes included numbers of penetrating and level I trauma activations, mechanisms of injury, and ISS. ISS data were divided into low and high groups with a low ISS defined as <15 and a high ISS defined as ≥ 15.13 The pandemic cohort was limited to January through May to limit the impact of the Black Lives Matter Movement as a confounding variable.
Descriptive statistics were reported with mean and standard deviation for normally distributed continuous variables, median and interquartile range for non-normally distributed continuous variables, and frequencies and percentages for categorical variables. For penetrating, level 1, and ISS analysis, data from the prepandemic cohort were aggregated and compared with those from the pandemic cohort. For mechanism analysis, 2020 data were split into two groups defined as pre-“shelter in place” (pre-SIP) and “shelter in place” (SIP) based on March 20th, when SIP restrictions were instituted by the state of California. All analyses were performed using a chi-squared test. A P value less than 0.05 was considered significant. All analyses were performed using IBM SPSS Statistics, version 25.0 (Chicago, Illinois).
Results
Demographics
A total of 5272 patients were triaged between January and May 2016 through 2020. Most patients were male (66.8%) with a median age of 45 y. Most trauma activations were the result of blunt injuries (83.8%), and 21.9% were triaged as level I. Characteristics of level I trauma are listed in Table 1. Level II trauma was defined as traumatic injuries not meeting level I criteria. The most common mechanisms of injury were fall (31.5%), followed by MVC (17.8%), pedestrian struck by automobile (auto-ped) (10.4%), and gunshot wound (GSW) (9.1%). Approximately 15.5% of patients with trauma required surgery during their hospitalization. Of these patients, 30.8% required emergent surgery within the first 2 h of arrival, and 41.3% required urgent surgery during the first 24 h of their admission (Table 2 ). There were no significant differences in baseline characteristics between prepandemic (2016 through 2019) and pandemic (2020) cohorts.
Table 2.
Patient characteristics.
| Demographic characteristics | N | % OR IQR |
|---|---|---|
| Total patients | 5271 | |
| # Male | 3521 | 66.80% |
| Median age | 45 | [29, 66] |
| Injury characteristics | ||
| Blunt | 4417 | 83.8% |
| Penetrating | 855 | 16.2% |
| Level I | 1152 | 21.85% |
| Level II | 3920 | 74.36% |
| Mechanism of injury | ||
| Fall | 1661 | 31.51% |
| MVC | 937 | 17.78% |
| Auto-ped | 546 | 10.36% |
| GSW | 477 | 9.05% |
| Assault | 457 | 8.67% |
| Stab wound | 209 | 3.97% |
| Other | 984 | 18.67% |
| Operative intervention | ||
| To the OR within 2 hrs of arrival | 252 | 30.81% |
| To the OR within 24 h of arrival | 338 | 41.32% |
| To the OR at > 24 h after arrival | 228 | 27.87% |
| Total | 818 | 15.52% |
OR = operating room.
Incidence of penetrating trauma
The absolute numbers of blunt and penetrating trauma activations did not differ significantly between prepandemic and pandemic cohorts for the months of January through March. In April and May, trauma distribution changed with a significant increase in incidence and proportion of penetrating trauma in the pandemic cohort (Table 3 ). In April, the pandemic cohort saw an increased incidence of penetrating trauma despite a lower absolute number of activations (169 versus 230 per mo averaged over 2016 through 2019). Forty-five of the total trauma activations were attributable to penetrating trauma compared with an average of 37 in the prepandemic cohort (26.6% versus 15.9%; P = 0.002).
Table 3.
Average number of blunt and penetrating trauma activations per month from 2016 to 2019 compared with total number per month in 2020.
| Mechanism | January |
February |
March |
April |
May |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Avg 2016-2019∗ | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | |
| Blunt | 170.3 | 151 | 0.17 | 168.5 | 179 | 0.82 | 181 | 148 | 0.28 | 185 | 124 | <0.01 | 202 | 192 | <0.01 |
| Penetrating | 28.5 | 34 | 44.8 | 33 | 36.3 | 37 | 36.5 | 45 | 31.3 | 54 | |||||
| Total | 199.5 | 185 | 198 | 212 | 216.8 | 181 | 230 | 169 | 233.5 | 245 | |||||
Bold denotes statistical significance (P < 0.05).
Number of activations per month averaged across 2016-2019.
In May, the total number of trauma activations in the pandemic cohort returned to prepandemic baseline (245 versus 233 per month), but a significantly increased incidence of penetrating trauma persisted. Fifty-four of the two hundred and forty-five traumas in the pandemic cohort were related to penetrating mechanisms compared with an average of 46 in the prepandemic cohort (22% versus 13.4%; P = 0.001) (Fig. 1 ).
Fig. 1.
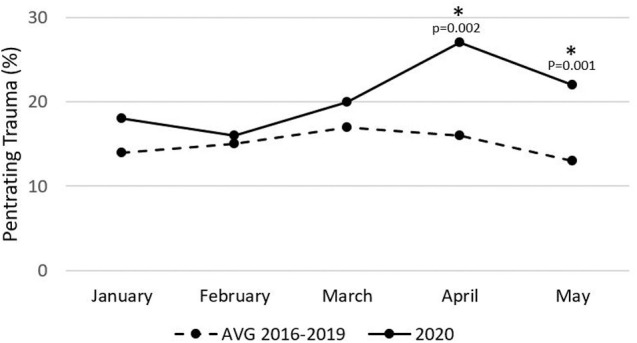
Percentage of penetrating trauma in 2020 versus 2016-2019. Data from 2016 to 2019 are denoted by a dashed line and data from 2020, by a continuous line. Asterisks are used to denote statistically significant increases in number of penetrating trauma activations (P value < 0.05). The April P value is 0.002, and the May P value is 0.001.
The incidence of level I trauma
Absolute numbers of level I and level II trauma activations were similar through the first 3 mo analyzed between both prepandemic and pandemic cohorts (Table 4 ). In April and May, the incidence of level I trauma activations rose significantly in the pandemic cohort. Fifty-four level I trauma activations were triaged in April of the pandemic cohort compared with an average of 31 in the prepandemic cohort (32% versus 20.1%; P = 0.003). Similarly, 78 level I trauma activations were triaged in May of the pandemic cohort compared with an average of 45 in the prepandemic cohort (31.8% versus 19.1%; P < 0.001) (Fig. 2 ).
Table 4.
Average number of level I and level II trauma activations per month from 2016 to 2019 compared with total number per month in 2020.
| Mechanism | January |
February |
March |
April |
May |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Avg 2016-2019∗ | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | Avg 2016 -2019 | 2020 | P value | |
| Level I | 34.8 | 43 | 0.27 | 38.5 | 54 | 0.11 | 32.5 | 46 | 0.65 | 46.3 | 54 | <0.01 | 44.5 | 78 | <0.01 |
| Level II | 152.8 | 152 | 158 | 142 | 158 | 130 | 166.5 | 112 | 179.5 | 159 | |||||
| Total | 199.5 | 185 | 198 | 212 | 216.8 | 181 | 230 | 169 | 233.5 | 245 | |||||
Bold denotes statistical significance (P < 0.05).
Number of activations per month averaged across 2016-2019.
Fig. 2.
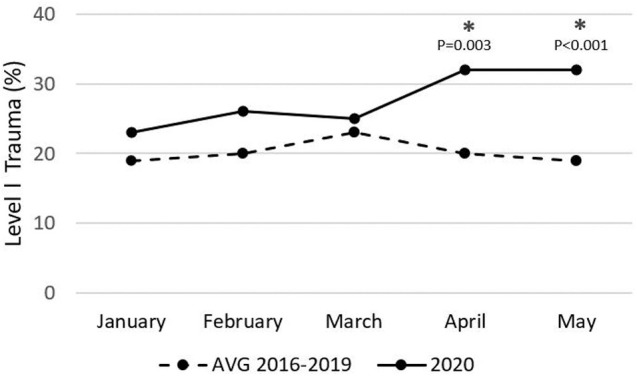
Percentage of level 1 trauma in 2020 versus 2016-2019. Data from 2016 to 2019 are denoted by a dashed line and data from 2020, by a continuous line. Asterisks are used to denote statistically significant increases in the number of level 1 trauma activations (P value < 0.05). The April P value is 0.003, and the May P value is less than 0.001.
Changes in mechanisms of trauma
To better identify the factors driving these observed increases in penetrating and high-acuity trauma, mechanisms of injury across 2016 through 2020 were investigated. The most common mechanisms of injury were falls, MVCs, assaults (with fists or blunt objects), auto-peds, and GSWs. The other injuries included accidental stabbings with other objects, bicycle- and motorcycle-related accidents, burns, hanging, drowning, and crush injuries.
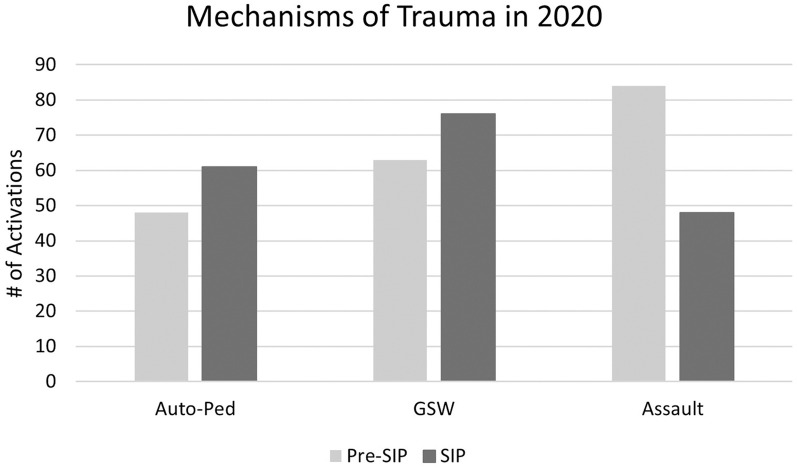
Table 5 shows that the incidence of three of these six mechanisms differed significantly before and after implementation of SIP restrictions. The incidence of assaults decreased (from 84 pre-SIP to 48 during SIP, P = 0.012), whereas that of GSW and auto-ped increased (63 to 76, P = 0.049 and 48 to 61, P = 0.047, respectively) (Fig. 3 ).
Table 5.
Incidence of most common mechanisms of traumatic injury during “pre-SIP” (January 1-March 19) and “SIP” (March 20-May 31) periods of 2020.
| Mechanism | Pre-SIP | SIP | P value |
|---|---|---|---|
| 1. Fall | 220 | 206 | 0.48 |
| 2. MVC | 95 | 94 | 0.41 |
| 3. Assault | 84 | 48 | 0.01 |
| 4. GSW | 63 | 76 | <0.05 |
| 5. Auto-ped | 48 | 61 | <0.05 |
| 6. Stab | 21 | 19 | 0.96 |
Bold denotes statistical significance (P < 0.05).
Fig. 3.
Volume of automobile versus pedestrian accidents (auto-peds), gunshot wounds (GSWs), and assaults during 2020. Pre-SIP was defined as occurring from January 1 to March 19 (date of shelter-in-place mandate), and SIP was defined as occurring from March 20 to May 31. The P value for auto-ped is 0.047, for GSW is 0.049, and for assault is 0.012.
Changes in the ISS
Unlike the results of penetrating and level I trauma analyses, there was no significant difference in the incidence of low or high ISS injuries between prepandemic and pandemic cohorts. There were more high ISS injuries after implementation of SIP restrictions; however, this increase was not statistically significant.
Discussion
The aim of this study was to investigate and quantify changing patterns of traumatic injury during the first months of the COVID-19 pandemic at an urban, safety-net, level I trauma center. Our study showed a statistically significant increase in the incidence of penetrating and high-level trauma in April and May 2020 compared with the same months in prior years. In April 2020, there was a significant increase in the incidence of penetrating and level I trauma triaged despite a decrease in absolute trauma volume. Although overall volume returned to baseline in May, we continued to observe a significantly higher incidence of penetrating and level I trauma. The ISS was not significantly different between prepandemic and pandemic cohorts, indicating that the increase in trauma observed in April and May 2020 did not necessarily correlate with higher-acuity injuries.
Our results are largely consistent with those published at other urban centers during the early months of the pandemic. Studies from Philadelphia and Los Angeles showed a decrease in absolute numbers of trauma activations with increased rates of penetrating and gun-related trauma, similar to our observations in Oakland.9 , 14 In nearby Santa Clara County, Forrester et al. reported a 4.8-fold decrease in trauma activations in the 15-day period after California's SIP went into effect.15 Although Highland Hospital initially also saw an absolute decrease in trauma volume, we later witnessed a significant increase in the incidence of penetrating and high-level trauma, opposite to what was observed in this nearby region. This highlights the importance of characterizing individual hospital experiences in the setting of the COVID-19 pandemic. Understanding the impact of COVID-19 on penetrating and high-level trauma in the event of future pandemic or national disaster is vital for public health officials and may allow for more thoughtful resource allocation based on individual center needs.
Societal stresses have been shown to play a role in increasing certain kinds of trauma. In the Bay Area, early economic models predicted a 10% increase in poverty across all nine Bay Area counties during a simulated 3-month quarantine with low-income workers disproportionately impacted.11 , 16 Job loss and socioeconomic distress are tied to domestic violence as well as to violent crime and penetrating trauma.17, 18, 19 Firearm ownership is also related to social stress and correlates directly with increased rates of homicide and suicide.20, 21, 22, 23 Firearm purchases increased significantly during the early months of the COVID-19 pandemic, more so than after other socially stressful national events like 9/11 or the Sandy Hook shooting. These 2.1 million additional firearms have been tied by researchers at UC Davis's Firearm Prevention Research Program to a small but significantly increased relative risk of firearm-related death or injury.7 Investigations analyzing these altered patterns of firearm acquisition during COVID-19 show the most common self-reported reasons for firearm purchase to be fear of lawlessness, prisoner release, and the government “going too far” or collapsing.24 The increase in social stressors related to the COVID-19 pandemic may explain observed increases in numbers of GSWs after implementation of SIP restrictions. Fewer people under the influence of drugs and alcohol out in close proximity to each other may have resulted in the decreased assault rate observed. Although it is difficult to explain the cause of increased auto-peds seen at our center during SIP, its significance lies in showing us that the effect that COVID-19 had on population dynamics extends beyond gun purchases and nightlife trends. We can apply what we observed during the COVID-19 pandemic to future incidents that induce significant socioeconomic stress or prolonged times of uncertainty so that under-resourced hospitals serving large catchment areas can be proactive and better equipped to serve their especially vulnerable populations.
This study has three main limitations. This is a retrospective, single-center study, which inherently limits generalizability. In addition, the duration of the study was limited to the first 2 mo of the pandemic in efforts to limit confounding by other national events. Understanding the effects of the Black Lives Matter Movement, the 2020 Presidential Election, and recurrent surges of COVID-19 on incidence of traumatic injury is a key future direction of this study. Despite these limitations, our investigation provides important insight into changes in population dynamics created by the COVID-19 pandemic and how these impact patterns of traumatic injury and subsequent resource requirements that affect the most jeopardized populations in our society.
Conclusion
Understanding factors that influence the burden of trauma sustained by a community is vital for effective resource allocation. At our safety-net, level I trauma center in Oakland, California, the incidence of penetrating and high-level trauma increased in the early months of the COVID-19 pandemic. Despite an overall decrease in the absolute number of trauma activations in April 2020, there were more level I and penetrating trauma activations than in prepandemic. In May 2020, we observed a return to baseline number of trauma activations with persistent increase in incidence of high-level and penetrating trauma.
Our study shows that despite pandemic conditions and a decrease in resources allocated to a trauma team, the numbers of critically ill patients with trauma do not decrease accordingly. In fact, our results suggest that some drivers of high-acuity trauma like firearm-related violence may increase. Our results have important implications for future national events that induce socioeconomic distress or change patterns of firearm purchase, particularly for under-resourced trauma centers serving vulnerable patient populations.
Acknowledgment
The author thanks her colleagues and mentors at Highland Hospital for their help with this project, many of whom are listed as authors. She is grateful for the guidance of Drs Timothy Browder and Gregory Victorino and for lending their insight and experience to her.
Authors' Contributions
J.D. was instrumental in the planning and carrying out of this project. She played major roles in data collection, IRB submission, and manuscript production. H.K. and K.B. assisted in coding data and writing this manuscript. C.M. also assisted in coding data. A.T. and C.C. provided vital research mentorship at all stages of this project, including planning, abstract submission, and manuscript editing. T.B. served as our principal investigator.
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- 1.Ali A.M., Willett K. What is the effect of the weather on trauma workload? A systematic review of the literature. Injury. 2015;46:945–953. doi: 10.1016/j.injury.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Lee H.J., Jin M.H., Lee J.H. The association of weather on pediatric emergency department visits in Changwon, Korea (2005-2014) Sci Total Environ. 2016;551-552:699–705. doi: 10.1016/j.scitotenv.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 3.Kieltyka J., Nicolson N.G., Crandall M. Seasonal and time of day variation related to the daily incidence of major traumatic injury in a large US city. Trauma. 2016;18:266–271. [Google Scholar]
- 4.Stonko D.P., Dennis B.M., Callcut R.A., et al. Identifying temporal patterns in trauma admissions: informing resource allocation. PLoS One. 2018;13:e0207766. doi: 10.1371/journal.pone.0207766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho V.P., Towe C.W., Chan J., Barie P.S. How’s the weather? Relationship between weather and trauma admissions at a level I trauma center. World J Surg. 2015;39:934–939. doi: 10.1007/s00268-014-2881-8. [DOI] [PubMed] [Google Scholar]
- 6.Lin L.-W., Lin H.-Y., Hsu C.-Y., Rau H.-H., Chen P.-L. Effect of weather and time on trauma events determined using emergency medical service registry data. Injury. 2015;46:1814–1820. doi: 10.1016/j.injury.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 7.Schleimer J.P., McCort C.D., Pear V.A., et al. Firearm purchasing and firearm violence in the first months of the coronavirus pandemic in the United States. Epidemiology. 2021;8:43. doi: 10.1186/s40621-021-00339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajput K., Sud A., Rees M., Rutka O. Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg. 2021;47:631–636. doi: 10.1007/s00068-020-01507-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qasim Z., Sjoholm L.O., Volgraf J., et al. Trauma center activity and surge response during the early phase of the COVID-19 pandemic—the Philadelphia story. J TraumaAcuteCare Surg. 2020;89:821–828. doi: 10.1097/TA.0000000000002859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hatchimonji J.S., Swendiman R.A., Seamon M.J., Nance M.L. Trauma does not quarantine: violence during the COVID-19 pandemic. Ann Surg. 2020;272:e53. doi: 10.1097/SLA.0000000000003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin A., Markhvida M., Hallegatte S., Walsh B. Socio-economic impacts of COVID-19 on household consumption and poverty. Econ Disasters Clim Change. 2020;23:1–27. doi: 10.1007/s41885-020-00070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fairlie R.W. The Impact of COVID-19 on Small Business Owners: The First Three Months After Social-Distancing Restrictions. National Bureau of Economic Research. 2020 doi: 10.1111/jems.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riuttanen A., Ponkilainen V., Kuitunen I., Reito A., Sirola J., Mattila V.M. Severely injured patients do not disappear in a pandemic: incidence and characteristics of severe injuries during COVID-19 lockdown in Finland. Acta Orthop. 2021;0:1–5. doi: 10.1080/17453674.2021.1881241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeates E.O., Grigorian A., Barrios C., et al. Changes in traumatic mechanisms of injury in Southern California related to COVID-19: penetrating trauma as a second pandemic. J TraumaAcuteCare Surg. 2021;90:714–721. doi: 10.1097/TA.0000000000003068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forrester J.D., Liou R., Knowlton L.M., Jou R.M., Spain D.A. Impact of shelter-in-place order for COVID-19 on trauma activations: Santa Clara County, California, March 2020. Trauma Surg Acute Care Open. 2020;5:e000505. doi: 10.1136/tsaco-2020-000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fairlie R. The impact of COVID-19 on small business owners: evidence from the first 3 months after widespread social-distancing restrictions. J Econ Manag Strategy. 2020 doi: 10.1111/jems.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider D., Harknett K., McLanahan S. Intimate partner violence in the great recession. Demography. 2016;53:471–505. doi: 10.1007/s13524-016-0462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cinat M.E. Significant correlation of trauma epidemiology with the economic conditions of a community. Arch Surg. 2004;139:1350. doi: 10.1001/archsurg.139.12.1350. [DOI] [PubMed] [Google Scholar]
- 19.Madan A.K., Sapozhnik J., Tillou A., Raafat A., McSwain N.E. Unemployment rates and trauma admissions. World J Surg. 2007;31:1930–1933. doi: 10.1007/s00268-007-9190-4. [DOI] [PubMed] [Google Scholar]
- 20.Monuteaux M.C., Lee L.K., Hemenway D., Mannix R., Fleegler E.W. Firearm ownership and violent crime in the U.S. Am J Prev Med. 2015;49:207–214. doi: 10.1016/j.amepre.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Siegel M., Rothman E.F. Firearm ownership and suicide rates among US men and women, 1981-2013. Am J Public Health. 2016;106:1316–1322. doi: 10.2105/AJPH.2016.303182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lang B.J., Lang M. Social Science Research Network; 2020. Pandemics, Protests and Firearms. [DOI] [Google Scholar]
- 23.Kellermann A.L., Rivara F.P., Somes G., et al. Suicide in the home in relation to gun ownership. N Engl J Med. 1992;327:1880. doi: 10.1056/NEJM199208133270705. [DOI] [PubMed] [Google Scholar]
- 24.Kravitz-Wirtz N., Aubel A., Schleimer J., Pallin R., Wintemute G. Public concern about violence, firearms, and the COVID-19 pandemic in California. JAMA Netw Open. 2021;4:e2033484. doi: 10.1001/jamanetworkopen.2020.33484. [DOI] [PMC free article] [PubMed] [Google Scholar]