Abstract
Purpose
Routine preoperative urinalysis has been the standard of care for the orthopedic population for decades, regardless of symptoms. Studies have demonstrated antibiotic overuse and low concordance between bacteria cultured from the surgical wound and the urine. Testing and treatment of asymptomatic urinary tract colonization before total joint arthroplasty (TJA) is unnecessary and increases patient risk. We investigated reducing antibiotic use by (1) modifying testing algorithms to target patients at risk, (2) modifying reflex to culture criteria, and (3) providing treatment guidelines.
Materials and Methods
A pre-post study was conducted to determine identify the impact of eliminating universal urinalysis prior to TJA on surgical site infection (SSI) and catheter-associated urinary tract infection (CAUTI) rates and number of antibiotic prescriptions. Patients who underwent primary hip or knee TJA or spinal fusions from February 2016 to March 2018 were included. Patient data was collected for pre- and post-practice change period (February 2016-October 2016 and August 2017-March 2018). Patient demographics, urinalysis results, cultures, and prescriptions were analyzed retrospectively from every tenth chart in the pre-period and prospectively on all patients in the post-period.
Results
A total of 4,663 patients were studied. There was a 96% decrease in urinalyses performed (P<0.0001), and a 93% reduction rate in antibiotic utilization (P<0.001). No significant difference in SSI and CAUTI rates was observed (P>0.05).
Conclusion
The elimination of routine urinalysis before orthopedic surgery resulted in a reduction in antibiotic utilization with no significant change in the SSI or CAUTI rates. Cost savings resulted from reduced antibiotic usage.
Keywords: Arthroplasty, Antimicrobial stewardship, Urinalysis, Surgical wound infection, Urinary tract infections
INTRODUCTION
Total joint arthroplasty (TJA) continues to be a successful surgery for improving pain and function, with projections of 4.052 million TJA procedures in the United States expected in 2030 alone1). Despite excellent results in outcomes for the majority of patients2), complications still occur. Prosthetic joint infection (PJI) is a dreaded complication, which affects approximately 1% of all cases3). As a result, routine preoperative management to mitigate risk factors such as diabetes and obese body mass index (BMI) is performed to improve outcomes of surgery4).
Prescreening urinalysis testing is one strategy for preoperative management. The genitourinary tract represents a potential source of bacteria seeding into a joint, perhaps first evidenced with a 1974 retrospective study showing a relationship between PJI and perioperative urinary tract infection (UTI)5). Although data associating preoperative screening with decreased rates of negative outcomes such as surgical site infections (SSIs) or catheter-associated UTIs (CAUTIs) is limited, other studies have reported increased rates of PJI in patients with UTI postoperatively6,7). This finding has led some surgeons and institutions to perform universal urinary screening before elective TJA. Evidence for efficacy of this practice for patients without any symptoms remains controversial. Despite recent evidence recommending against8), urinary screening prior to elective TJA and treatment of asymptomatic patients is still practiced. Such universal testing results in increased antibiotic prescription for asymptotic bacteriuria, producing increased antibiotic resistance, adverse drug effects, and cost9).
The purpose of this study was to evaluate the rates of SSIs, CAUTIs, and antibiotic prescriptions before and after elimination of universal prescreening urinalysis testing for elective TJA patients at a single-specialty orthopaedic hospital. The hypothesis of the study is that elimination of testing will not result in increased rates of SSIs or CAUTIs but will reduce antibiotic prescriptions.
MATERIALS AND METHODS
1. Quality Improvement Initiative
Preoperative antibiotics for urinary tract infection in the elective orthopedic surgery population was identified as a potential area of antibiotic overutilization in our hospital by the hospital's “Antibiotic Stewardship Committee”. A quality improvement initiative was developed with the aim of reducing unnecessary antibiotic use in this population. The program consisted of modifying testing algorithms, modifying reflex-to-culture criteria, and providing treatment guidelines to practitioners.
2. Study Design
A pre-post study was subsequently conducted to determine the impact of the protocol change on SSI and CAUTI rates and number of antibiotic prescriptions. The study was approved by the Institutional Review Board (IRB) of New England Baptist Hospital (No. 1090003), and the written informed consent was obtained from all patients. Data were collected from the hospital's patient database for a prepractice change period (February 2016 through October 2016), an intervention period (November 2016 through July 2017), and a post-practice change period (August 2017 through March 2018) for all patients undergoing a primary hip, revision hip, primary knee, revision knee, or spinal fusion procedure. The intervention period while the new practices were being executed was excluded from final data analysis.
Patient demographics, procedure-related variables, urinalysis results, urine culture results, and antibiotic prescriptions were collected from the hospital's orthopedic registry and patients’ electronic medical record retrospectively from every tenth chart in the pre-practice change period and measured prospectively on all patients in the post-practice change period. For the post-practice change period, data on symptoms was collected prospectively from “Prescreening Urine Analysis Guides” filled out by the hospital's Preadmission Screening Unit. SSI and CAUTI rates were extracted prospectively from infection control databases using Center for Disease Control and Prevention/National Healthcare Safety Network definitions.
3. Pre-period Protocol
Prior to November 2016, all patients undergoing the above mentioned procedures underwent routine urinalysis during the preadmission screening visit with a reflex to culture for the following variables: bacteria, leukocyte esterase or nitrate on the dipstick, or white blood cell count greater than 5/high powered field. A positive urine culture was treated at the discretion of the prescreening nurse practitioner.
4. Post-period Protocol
A “Prescreening Urine Treatment Guideline” was developed based on the current Infectious Diseases Society of America guidelines9). In addition to these guidelines, the criteria for a positive urinalysis with reflex to culture were modified to only reflex to culture for leukocyte esterase and/or white blood counts greater than five. Nurse practitioners were encouraged to follow a urine treatment guideline when deciding on treatment for patients with positive urine culture results or symptoms or urinary tract infection.
5. Statistical Analysis
All patient data was entered into a research electronic data capture database. Univariate analysis was performed for comparison of groups for differences in age, gender, diabetes, procedure mix, foley catheter utilization, and other variables that may affect the outcomes. All statistical tests were performed in SAS (ver. 9.3; SAS Institute, Cary, NC, USA). The univariate analysis utilized t-tests, chi-square tests, and Fisher exact tests as appropriate. A P≤0.05 was considered statistically significant.
RESULTS
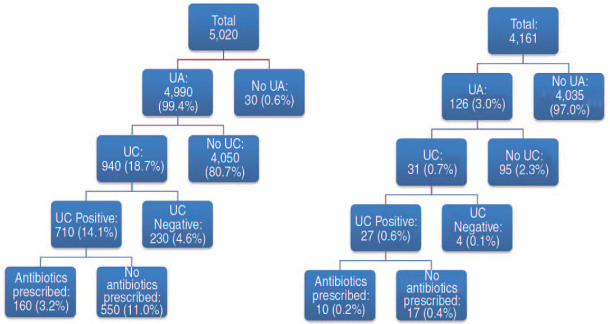
A total of 4,663 patients were analyzed during the study period, with 502 patients in the pre-period (every 10th patient from the 5,020-patient cohort) and 4,161 patients in the post-period (Fig. 1). In the pre- and post-period, patients did not differ significantly with regard to demographic data including age, sex, BMI, American Society of Anesthesiologists classification, or surgery type (P>0.05 for all; Table 1). Urinalysis was performed in 99% of cases before the intervention, compared to only 3% of cases after (P<0.001; Table 1). Both performed urine cultures and positive urine cultures showed a significant decrease after the intervention (P<0.001 for all; Table 1).
Fig. 1. Impact of prescreening urinalysis practice change in an elective orthopaedic population.
UA: urinalysis, UC: urine culture.
Table 1. Demographics and Impact of Prescreening Urinalysis Practice Change.
| Pre-period (n=502) | Post-period (n=4,161) | P-value | ||
|---|---|---|---|---|
| Age (yr) | 64.1±10.5 | 65.7±9.5 | 0.100 | |
| Female | 264 (52.6) | 2,276 (54.7) | 0.370 | |
| BMI (kg/m2) | 30.9±6.4 | 30.7±6.3 | 0.570 | |
| ASA | 0.016 | |||
| 1 | 16 (3.2) | 221 (5.3) | ||
| 2 | 383 (76.3) | 2,932 (70.5) | ||
| 3 | 101 (20.1) | 1,001 (24.1) | ||
| 4 | 2 (0.4) | 7 (0.2) | ||
| Knee arthroplasty | 234 (46.6) | 1,973 (47.4) | 0.878 | |
| Hip arthroplasty | 222 (44.2) | 1,862 (44.7) | ||
| Fusion | 46 (9.2) | 356 (8.6) | ||
| Urinalysis performed | 499 (99.4) | 126 (3.0) | <0.001 | |
| UC performed | 94 (18.7) | 31 (0.7) | <0.001 | |
| Positive UC | 71 (14.1) | 27 (0.6) | <0.001 | |
| UA resulted in antibiotic prescription | 16 (3.2) | 10 (0.2) | <0.001 | |
| Average catheter utilization rate* | 0.2 | 0.14 | <0.001 | |
| No. of CAUTI in each study period | 1 | 1 | ||
| CAUTI rate/1,000 device-days | 0.300 | 0.504 | 0.747 | |
| SSI rate/100 procedures | 0.35 | 0.24 | 0.303 | |
Values are presented as mean±standard deviation, number (%), rate, or number only.
Pre-period data reflects 1/10th of the total population in this period.
BMI: body mass index, ASA: American Society of Anesthesiologists, UC: urine culture, UA: urinalysis, CAUTI: catheter-associated urinary tract infection, SSI: surgical site infection.
*Catheter-days/patient-days.
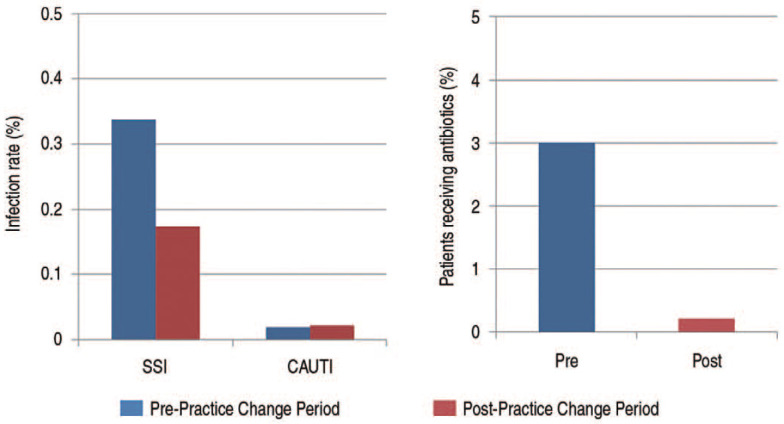
There were no significant differences in the rate of CAUTI per 1,000 device days nor SSI rate per 100 procedures before and after intervention (P>0.05; Table 1). Antibiotic prescription due to urine testing was significantly higher in the preperiod compared to post-period (P<0.001; Table 1, Fig. 2).
Fig. 2. Impact of prescreening urinalysis practice change on surgical site infection (SSI) rates, catheter-associated urinary tract infection (CAUTI) rates, and antibiotic prescriptions.
DISCUSSION
Infection after TJA is a difficult complication to treat, and prevention is paramount to a successful operation. Urinalysis is a routinely performed preoperative test and bacteria in the genitourinary tract are a potential target for preventing postoperative infections, but universal identification and treatment may not be recommended. Studies have shown that patients with a symptomatic UTI before surgery are at an increased risk for PJI7,10,11), and such infections should be treated before surgery12). However, assumptions of testing and treating asymptomatic patients to prevent PJI may not be warranted as this reflects a distinct clinical scenario.
Evidence for asymptomatic bacteriuria (ASB) and negative outcomes remains controversial. Up to 3-19% of patients undergoing elective TJA may have preoperative ASB8). Two studies demonstrated a higher risk of PJI in patients with ASB13,14). However, a study of over 20,000 patients found no association with positive urine culture prior to TJA and an increased risk of infection or PJI15). A 2019 meta-analysis showed that preoperative antibiotic therapy for ASB did not lower the risk of PJI8). Additionally, these authors showed that the cultured PJI bacteria were often different from isolates found in the urine of asymptomatic patients–suggesting further evidence against antibiotic treatment in these scenarios8). In agreement with other studies16,17,18), our findings show that discontinuing the practice of universal urinalysis testing for patients prior to TJA decreases antibiotic usage without increasing infection rates.
At this time, the American Academy of Orthopedic Surgeons recommends preoperative urine testing prior to elective TJA, but they state that the evidence is weak regarding bacteriuria and negative outcomes12). Testing for and treating asymptomatic urinary colonization before orthopedic joint replacement surgery is likely unnecessary and may put the patient at additional risk10,19,20). In addition, treating ASB can be associated with adverse outcomes such as increased antibiotic resistance, adverse drug side effects, and unnecessary supply and personnel costs9).
There are several limitations in the current study, including its retrospective nature and relatively small sample size. However, we were able to find significant differences within our sample population. Due to the retrospective nature, universally testing in the pre-period did not allow the granular data to differentiate between asymptomatic and symptomatic UTIs; however, this did not result in significantly different infection rates in the pre- and post-period. This study, in the context of its limitations, adds to the literature of evidence to support abandoning universal preoperative urinalysis screening and the treatment of ASB. Future guidelines should consider this information when developing screening and treatment practices prior to TJA.
CONCLUSION
Elimination of routine urinalysis before orthopedic surgery resulted in no change in SSI or CAUTI rates, but a 93% reduction in antibiotic utilization.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Shan L, Shan B, Suzuki A, Nouh F, Saxena A. Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am. 2015;97:156–168. doi: 10.2106/JBJS.M.00372. [DOI] [PubMed] [Google Scholar]
- 3.Uçkay I, Hoffmeyer P, Lew D, Pittet D. Prevention of surgical site infections in orthopaedic surgery and bone trauma: state-of-the-art update. J Hosp Infect. 2013;84:5–12. doi: 10.1016/j.jhin.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 4.Namba RS, Inacio MC, Paxton EW. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am. 2013;95:775–782. doi: 10.2106/JBJS.L.00211. [DOI] [PubMed] [Google Scholar]
- 5.Irvine R, Johnson BL, Jr, Amstutz HC. The relationship of genitourinary tract procedures and deep sepsis after total hip replacements. Surg Gynecol Obstet. 1974;139:701–706. [PubMed] [Google Scholar]
- 6.Punjani N, Lanting B, McClure JA, Winick-Ng J, Welk B. The impact of common urologic complications on the risk of a periprosthetic joint infection. J Bone Joint Surg Am. 2018;100:1517–1523. doi: 10.2106/JBJS.17.01405. [DOI] [PubMed] [Google Scholar]
- 7.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466:1710–1715. doi: 10.1007/s11999-008-0209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sousa RJG, Abreu MA, Wouthuyzen-Bakker M, Soriano AV. Is routine urinary screening indicated prior to elective total joint arthroplasty? A systematic review and meta-analysis. J Arthroplasty. 2019;34:1523–1530. doi: 10.1016/j.arth.2019.03.034. [DOI] [PubMed] [Google Scholar]
- 9.Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Errata: Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:1556. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 10.Cordero-Ampuero J, González-Fernández E, Martínez-Vélez D, Esteban J. Are antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria? Seeding risk with/without treatment. Clin Orthop Relat Res. 2013;471:3822–3829. doi: 10.1007/s11999-013-2868-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kong L, Cao J, Zhang Y, Ding W, Shen Y. Risk factors for periprosthetic joint infection following primary total hip or knee arthroplasty: a meta-analysis. Int Wound J. 2017;14:529–536. doi: 10.1111/iwj.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.David TS, Vrahas MS. Perioperative lower urinary tract infections and deep sepsis in patients undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2000;8:66–74. doi: 10.5435/00124635-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Sousa R, Muñoz-Mahamud E, Quayle J, et al. Is asymptomatic bacteriuria a risk factor for prosthetic joint infection? Clin Infect Dis. 2014;59:41–47. doi: 10.1093/cid/ciu235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weale R, El-Bakri F, Saeed K. Pre-operative asymptomatic bacteriuria: a risk factor for prosthetic joint infection? J Hosp Infect. 2019;101:210–213. doi: 10.1016/j.jhin.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Honkanen M, Jämsen E, Karppelin M, et al. The impact of preoperative bacteriuria on the risk of periprosthetic joint infection after primary knee or hip replacement: a retrospective study with a 1-year follow up. Clin Microbiol Infect. 2018;24:376–380. doi: 10.1016/j.cmi.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 16.Lamb MJ, Baillie L, Pajak D, et al. Elimination of screening urine cultures prior to elective joint arthroplasty. Clin Infect Dis. 2017;64:806–809. doi: 10.1093/cid/ciw848. [DOI] [PubMed] [Google Scholar]
- 17.Bailin S, Noiseux N, Pottinger JM, et al. Screening patients undergoing total hip or knee arthroplasty with perioperative urinalysis and the effect of a practice change on antimicrobial use. Infect Control Hosp Epidemiol. 2017;38:281–286. doi: 10.1017/ice.2016.272. [DOI] [PubMed] [Google Scholar]
- 18.Koulouvaris P, Sculco P, Finerty E, Sculco T, Sharrock NE. Relationship between perioperative urinary tract infection and deep infection after joint arthroplasty. Clin Orthop Relat Res. 2009;467:1859–1867. doi: 10.1007/s11999-008-0614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouvet C, Lübbeke A, Bandi C, et al. Is there any benefit in pre-operative urinary analysis before elective total joint replacement? Bone Joint J. 2014;96:390–394. doi: 10.1302/0301-620X.96B3.32620. [DOI] [PubMed] [Google Scholar]
- 20.Sendi P, Borens O, Wahl P, Clauss M, Uçkay I. Management of asymptomatic bacteriuria, urinary catheters and symptomatic urinary tract infections in patients undergoing surgery for joint replacement: a position paper of the expert group‘infection’ of swissorthopaedics. J Bone Jt Infect. 2017;2:154–159. doi: 10.7150/jbji.20425. [DOI] [PMC free article] [PubMed] [Google Scholar]