Abstract
Background
Technology is increasingly used in nursing education, particularly during the SARS-CoV-2 (COVID-19) pandemic. COVID-19 also brought new challenges to patient care and limited access to in-person clinical experiences for nursing students. Pivoting to virtual simulation (VS) for clinical was necessary during the height of the pandemic. With students' return to clinical settings, VS experiences continue to be needed, due to quarantine of clinical settings and/or shortage of available clinical sites. VS clinical experiences have been successfully utilized over the past decade; however, the literature lacks resources on the use of VS for delirium care of patients.
Method
In this article, the authors describe the creation and provision of a VS clinical day using interactive computer-based technology to educate nursing students to prevent, recognize, and manage delirium. The VS clinical was in conjunction with a Behavioral Health course.
Results
Evaluation of students demonstrated attainment of objectives. Students reported satisfaction with the VS experience.
Conclusion
Technology in nursing education and use of VS clinical provide effective strategies for clinical learning when in-person clinical experiences are unavailable, either due to access limitations or lack of patients with specific health needs.
Keywords: Virtual simulation, Nursing education, Delirium, COVID-19, Clinical experience, Technology
Online methods of teaching and the use of technology in nursing education have become increasingly important over the past two decades (Delva et al., 2019; King & Nininger, 2019; Smart et al., 2020; Yancey, 2018). The SARS-CoV-2 (COVID-19) pandemic created unprecedented opportunities and challenges for nursing education. The opportunities include implementing creative teaching modalities to continue to educate nursing students, both undergraduate and graduate, under conditions of isolation and quarantine. The challenges include access to in-person clinical experiences, technology for both students and faculty within their home environments (Smart et al., 2020; Yancey, 2018), quality control of online instructional materials (Delva et al., 2019; Huun, 2018; King & Nininger, 2019), orientation of students to the online milieu (Casida & Molen, 2018; Delva et al., 2019; Richter & Schuessler, 2019), and availability of technological and online support for faculty and students (Casida & Molen, 2018; Delva et al., 2019; Huun, 2018; King & Nininger, 2019; Richter & Schuessler, 2019; Smart et al., 2020; Stanley et al., 2018; Yancey, 2018).
Simulation in nursing education has evolved over time. The term simulation has a variety of definitions including a pedagogical approach utilizing multiple modalities to enhance knowledge acquisition (Kardong-Edgren et al., 2019; Lopreiato, 2016). According to Sofer (2018), the National Council of State Boards of Nursing (NCSBN) defines clinical simulation as “an activity or event replicating clinical practice using scenarios, high-fidelity manikins, medium-fidelity manikins, standardized patients, role playing, skills stations, and computer-based critical thinking simulations” (p.17). Virtual simulation (VS) as defined by NCSBN was used by the professors as a computer-based method utilizing educational platforms in combination with professors actively engaging with students in a synchronous learning environment. This clinical experience was in conjunction with the students' Behavioral Health didactic course. Current research indicates that interactive computer-based learning experiences promote acquisition and retention of content (Aredes et al., 2018; Kardong-Edgren et al., 2019; Padilha et al., 2019; Rourke, 2020). Simulated interactive computer-based learning experiences defines virtual simulation (Aredes et al., 2018; Kardong-Edgren et al., 2019; Padilha et al., 2019; Rourke, 2020). With the explosion of VS in nursing education these real-life clinical simulated educational experiences provide the undergraduate nursing student a safe environment to practice clinical skills, knowledge, and clinical judgement (Aredes et al., 2018; Kardong-Edgren et al., 2019; Padilha et al., 2019; Rourke, 2020). Below we describe an educational intervention for nursing students to learn about delirium utilizing virtual simulation through interactive computer-based technology using the above definition.
Simulations have been effectively utilized in both classroom and online educational environments to foster clinical decision-making skills in nursing students for a wide variety of medical conditions (Huun, 2018; Richter & Schuessler, 2019; Stanley et al., 2018). Simulation software may be utilized as an effective replacement for traditional clinical experiences (Huun, 2018; Stanley et al., 2018). In addition to providing students with a safe environment in which to practice their skills in patient care, VS also allows students to continue their clinical development if clinical experiences are not available or do not provide exposure to caring for persons with delirium (Huun, 2018; Richter & Schuessler, 2019; Stanley et al., 2018). Nursing educators can effectively mentor and facilitate the development of clinical judgement in nursing students using VS. Success requires proper attention to planning, implementation, and evaluation of VS activities and integrating other teaching modalities, such as synchronous (e.g., WebEx discussions) or asynchronous (e.g., discussion board posts) discussion groups and case study work (Delva et al., 2019; Smart et al., 2020).
Delirium is one of the many important medical conditions student nurses need to learn to recognize and manage. As a multifactorial condition that has been associated with poor prognosis in critically ill patients, prompt recognition and intervention for delirium is important (Kotfis et al., 2020). COVID-19 restricted access to clinical settings and in-person experiences. Thus, opportunities to develop competencies in delirium care were limited. We determined that use of a VS would provide student nurses a safe environment in which they could effectively develop the skills necessary to manage these patients. Post pandemic, VS can continue to be utilized as a supplement to in-person clinical activities if students are not able to observe patients with delirium in the clinical environment (Goncalves & Watson, 2019; Luckenbach et al., 2021).
Evidence-based use of technology as a teaching method
The use of technology and simulation in nursing education continues to evolve, as does the technology itself. Quarantine and isolation due to COVID-19 has accelerated the use of technology in formal education. Ensuring the quality and effectiveness of VS in nursing education is of the utmost importance (Huun, 2018).
There is a growing body of research demonstrating the effectiveness of VS in nursing education (Bruce et al., 2019; Cant & Cooper, 2019; Hardenberg et al., 2019; Tyler et al., 2019). Use of simulation as an effective teaching tool for assessment and management of delirium also has empirical evidence (Dwyer et al., 2019; Hirota, 2020; Lieow et al., 2019). Assessment of quality of VS, as well as online courses, is available through Quality Matters (QM™), a process used to evaluate online course objectives, content accessibility, and use of best practices in online education (Huun, 2018; Quality Matters, 2021). QM™ began as a grass roots effort among educators in Maryland seeking to measure and guarantee the quality of online courses. These educators have since obtained a grant from the United States Department of Education and support quality standards for online education throughout the country (Quality Matters™ 2021). Nursing educators require ongoing continuing education and institutional support to assure consistent quality and effectiveness of technology and simulation in nursing education (Bruce et al., 2019; Cant & Cooper, 2019; Dwyer et al., 2019; Hardenberg et al., 2019; Huun, 2018; Lieow et al., 2019).
Technology, teaching, & simulation in the context of COVID-19
Amid the COVID-19 pandemic, schools of nursing around the globe had to pivot abruptly to a distance platform. Professors had to become proficient utilizing virtual meeting software such as Zoom, WebEx®, and Blackboard Collaborate™; online classroom platforms such as Blackboard™; and multiple educational packages to deliver both clinical and didactic lessons. Our school of nursing, for example, utilized several educational software packages – Assessment Technologies Institute™ (ATI) live simulation, unfolding case studies from F.A. Davis, and Wolters Kluwer Virtual Simulation (vSim) for Nursing to reinforce clinical concepts. These resources were used in our school of nursing prior to the pandemic as supplementary content to traditional classroom and in-person clinical experiences. During the pandemic shutdown, these resources became the sole source of clinical experiences for some of our students. After the successful use of VS, faculty determined that continued use of focused VS for clinical, such as the patients in the vSIM for Nursing/Mental Health, would continue to be useful in partnership with live clinical in a post-pandemic world. Written work with faculty feedback (e.g., response to case study questions, conceptual model, brief care plan, mental status exam, and quiz results from the Wolters Kluwer vSims and ATI) were also completed by the students to assure objectives were met.
There are e-learning resources available for behavioral health topics and cognitive disorders such as Alzheimer's disease through ATI and Wolters Kluwer. However, we found few e-learning resources available for nursing students that focus on delirium. Detroyer et al. (2018) evaluated the use of an e-learning initiative and concluded that there is a need for more resources to educate both student nurses and nurses in the inpatient setting about recognizing and managing delirium.
When searching for resources, we reviewed the electronic databases of Cumulative Index of Nursing and Allied Health Literature (CINAHL), PubMed, PsycINFO and general subject inquiry, and identified only five articles on e-learning and COVID-19. None of these articles discussed delirium in the context of limited clinical experiences, due to COVID-19 or other limits. These results underscore the need for e-learning resources about delirium. The need for such resources is great considering the increased risk for delirium among patients with critical illness due to limited cognitive stimulation and the isolative state the patient is in while hospitalized.
Developing a delirium virtual simulation clinical day
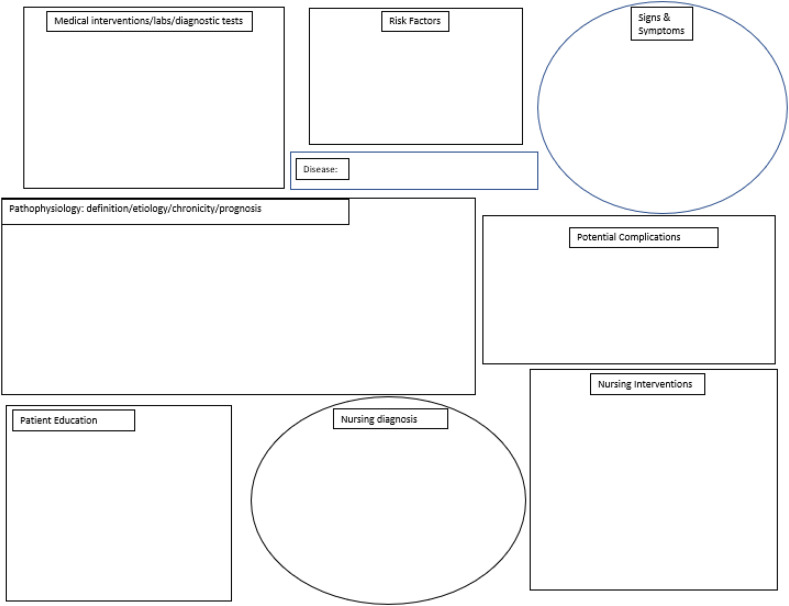
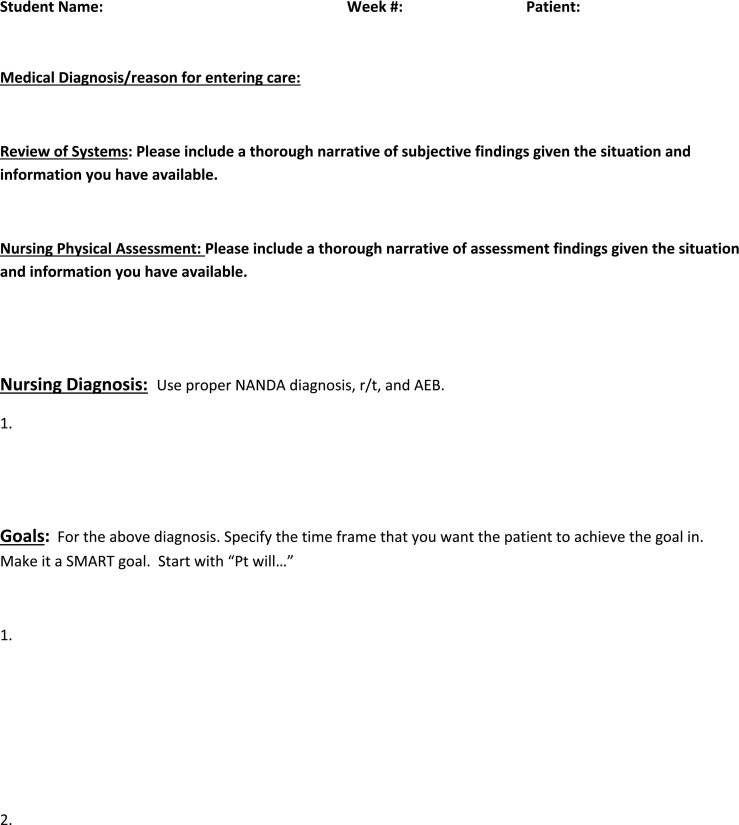
Given the lack of clinical opportunity during COVID-19 and lack of e-learning resources focused on delirium, we developed a VS experience for students to learn and apply critical thinking skills in assessing, completing a conceptual model (Appendix A), and developing a brief care plan (Appendix B) to manage patients with or at risk for delirium (Orsini-Garry, 2019, Orsini-Garry, 2020). The VS was built upon the foundation already present in the curriculum, which incorporated readings done individually by students, and classroom didactic lecture and discussion attended by all students together via a video platform. Foundational content included concepts such as defining delirium, numbers of patients affected, costs to individuals and the healthcare system, multifactorial causes, risk factors, how to assess for/identify delirium, and nursing interventions to mitigate delirium. The conceptual model provided a worksheet for students to identify various factors for the simulated patient and notations on nursing diagnosis, nursing interventions, and patient education to incorporate into their brief care plans.
We searched potential resources to identify “patients” that the students would be able to assess for delirium and then use as the case patient to develop brief care plans for implementing appropriate nursing interventions based on the patient's presentation. We wanted to include patients with presentations that students and nurses are likely to encounter in the clinical setting.
We selected three specific e-learning resources for the VS activities. First, we identified the Nurses Improving Care for Healthsystem Elders (NICHE) interactive modules. NICHE modules provide evidence-based integrated case study examples, literature resources, and VS featuring older adult patients in the vSIM for Nursing/Mental Health (Bricoli, 2020). Students were sent an activation email to set up their account with the NICHE Knowledge Center. The NICHE modules were then available for students to work on at their own pace (NICHE Homepage, 2021). The second resource we adopted was the Wolters Kluwer vSim scenarios for Mental Health (Wolters Kluwer, 2021). We included this resource because the scenarios include avatar patients with common medical problems seen in medical-surgical hospital units. The third resource included a short YouTube video of a person with delirium (Pinkhasov, 2019). Students completed the NICHE interactive modules independently prior to the clinical virtual simulation day. Both the vSims, ATI, and YouTube video were viewed by students together in their clinical groups during their VS clinical day.
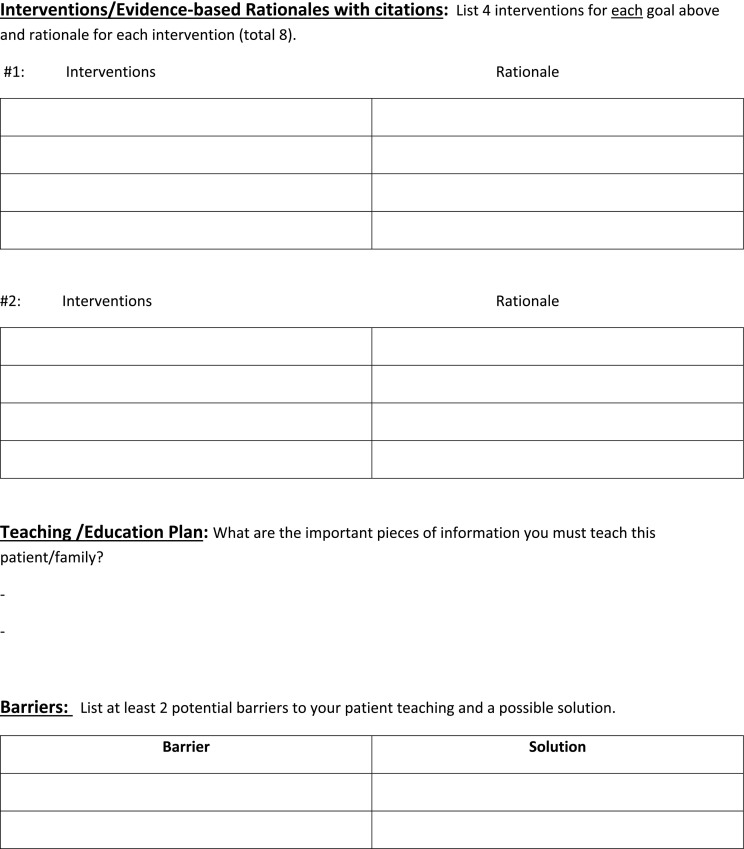
Next, we identified the activities that students would need to complete during the VS clinical day. The activities were designed so that each student would have the opportunity to apply nursing knowledge to effectively assess patients for delirium and plan for employing evidence-based interventions to mitigate delirium. We selected the Confusion Assessment Method (CAM) (Inova Health System, 2020; American Geriatrics Society [AGS], 2019) (Appendix C) for assessment and identification of delirium. The ‘4Ms’ model of care (Institute for Healthcare Improvement [IHI], 2019) and Hospital Elder Life Program (Delirium Prevention Toolkit, 2019; AGS coCare HELP™, 2019) strategies were adopted as evidence-based nursing interventions to mitigate delirium. Some of these strategies are presented in the AGS Delirium Prevention Tool Kit (AGS CoCare HELP™, 2019c), which we also adopted for use by the students in their VS clinical day. The brief care plan for employing the evidence-based strategies was developed using the conceptual model (Orsini-Garry, 2019). Costs for the VS activities, such as the Wolters Kluwer vSims, were included in the textbooks that students already purchase for the clinical practicum and related clinical didactic courses. There were no additional fees for participating in the VS.
Student evaluation, pre-briefing, and debriefing strategies were used to assure students met the objectives of 1) understanding key concepts related to delirium and 2) demonstrating how to apply the nursing process when caring for a patient at risk for or with delirium (see Table 1 ). Details of these activities are provided below.
Table 1.
Virtual simulation objectives and evaluation assessments.
| Objective | Assessment | Evaluation of/Feedback to Studenta |
|---|---|---|
| 1) Understanding key concepts related to delirium | Discussion in break-out groups and general VS engagement |
|
| Case study responses and quiz results |
|
|
| Completed conceptual model document |
|
|
| Brief care plan |
|
|
| 2) Demonstrating how to apply the nursing process when caring for a patient at risk for or with delirium | Discussion in break-out groups and general VS engagement |
|
| Case study responses and quiz results |
|
|
| Completed conceptual model document |
|
|
| Brief care plan |
|
Most work was ‘graded’ as pass/fail, students could resubmit if they did not meet the benchmark with first submissions.
Running a delirium virtual simulation clinical day
The delirium VS clinical day was a synchronous activity lasting approximately 4.5 h during which students and the clinical faculty member met together via a virtual platform such as WebEx or Blackboard Collaborate. Virtual clinical experiences are counted in a 1:2 ratio to in-person clinical, so 1 VS Day counted for 9 h of in-person clinical time. The day began with a pre-conference with pre-briefing provided by the clinical faculty member. Pre-briefing included discussion to identify the students' knowledge about delirium, how to assess for delirium, and planning interventions to mitigate delirium. The pre-brief intentionally included a review of content previously presented in readings and the didactic classroom, as well as a discussion about the content in the NICHE interactive modules. This assured that students had a similar foundational understanding about delirium and the nurse's role in preventing, identifying, and managing delirium at the start of the VS clinical day.
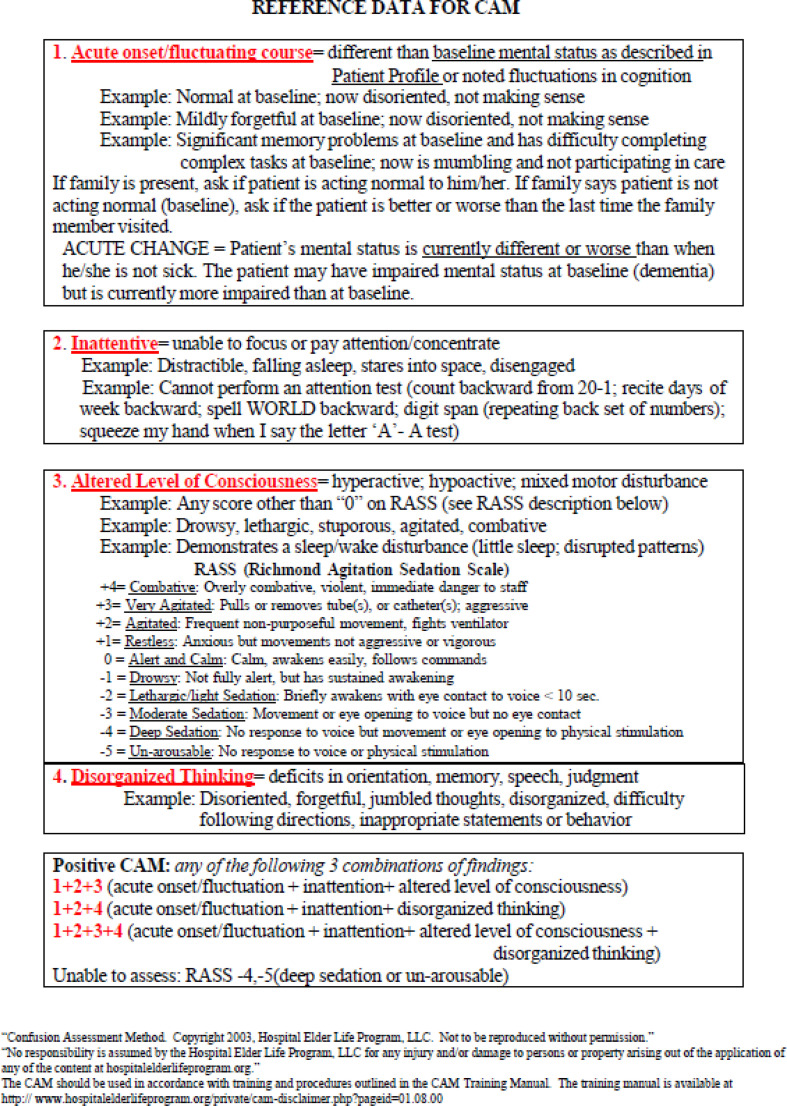
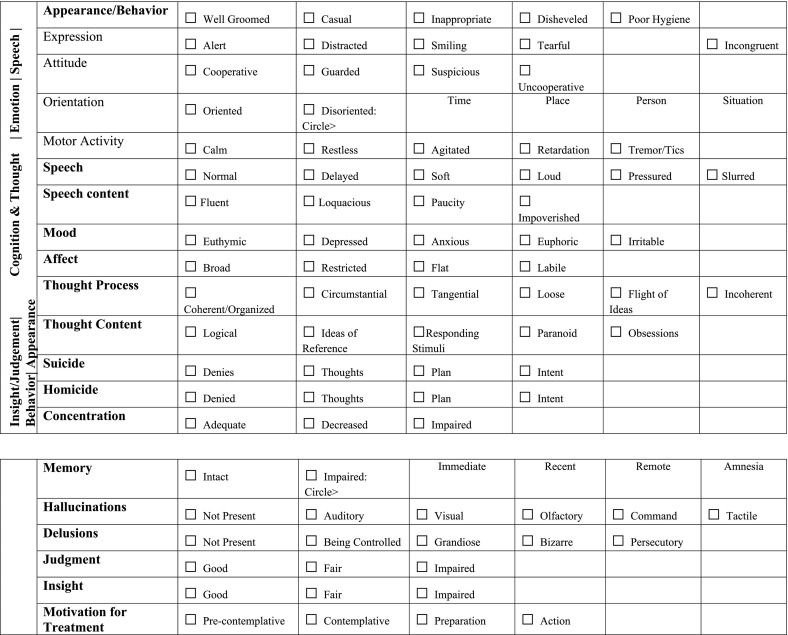
Following the pre-conference pre-briefing, a YouTube video was shown in which the CAM was demonstrated (Inova Health System, 2020). Developed and validated by Dr. Sharon Inouye, the CAM is a widely adopted instrument used since 1990 to identify delirium in the hospital setting (Inova Health System, 2020; Wei et al., 2008). The students used the CAM along with an adapted mental status exam form (Appendix D) as using both instruments can assist in confirming a diagnosis of delirium (Marcantonio, 2017). The CAM and process for conducting a mental status exam were introduced in the readings, discussed in the didactic class, reviewed in the pre-briefing, and then used by students to evaluate avatars and a YouTube video patient in the VS clinical day. The CAM was selected purposefully as students are likely to use it after graduation. The adapted mental status exam form was created by a faculty member from instruments with established reliability and validity, like the mental state exam (MSE), to facilitate use by students during the VS clinical day.
Two scenarios of patients exhibiting signs of delirium from the Wolters Kluwer vSims were used, one followed by the other, one ATI scenario, and the YouTube patient presentation video, if time permitted. Using these audio-visual platforms allowed the clinical faculty member to review and replay sections of the vSims, ATI scenario, or video, providing an opportunity to emphasize delirium prevention, intervention, and management practices during integrated debriefing.
There were 8 students in each clinical group with 1 instructor. Students collaboratively evaluated the avatar patients who were admitted to the virtual hospital. The ‘patients’ were presented as an unfolding case and had a diagnosis other than delirium but, like any patient, could develop delirium during their hospitalization. Students worked together to review the “patients” electronic medical records and complete the adapted mental status exam and CAM to determine risk for or presence of delirium in each. The same process was followed for the ATI scenario and YouTube video patient; however, no medical record data were provided beyond the video presentation.
Interwoven debriefing after the assessment included accuracy check by the clinical faculty member, identification of specific patient actions that would be consistent with a “yes” answer to the CAM evaluation questions, and review of the adapted mental status exam results for each avatar patient. An emphasis was placed on obtaining a baseline mental status prior to completing the CAM as this ensures a higher probability that the assessment is accurate. Students were encouraged to share their answers to the CAM evaluation questions and adapted mental status exam scoring. Students' responses provided opportunity for group discussion, questions, and answers, and “in the moment” feedback for students. Using this methodology, students were able to recognize key features in delirium, such as an acute change in mental status. The interwoven debriefing allowed students to critically think about the patient's current health status and assured that students were then able to make clinical judgements based upon the assessment to develop the brief care plan based on the conceptual model with accurate assessment data in mind (Orsini-Garry, 2019, Orsini-Garry, 2020; Pedersen et al., 2019).
The students then went into randomly assigned breakout sessions of 3 to 4 students each within the virtual platform. They worked together in small groups to complete the conceptual model (Orsini-Garry, 2019) and used that information to develop a brief care plan (Orsini-Garry, 2020). Completing the conceptual model required the students to do further research on delirium. They considered and integrated their evidence-based research information with data collected on the avatar patients (medical record review for avatars, mental status exam results, and CAM results) and foundational information on delirium management. They incorporated concepts from the NICHE interactive-module, pre-briefing discussion, and knowledge of the nursing process to complete the conceptual model and then develop the brief care plan (Orsini-Garry, 2019, Orsini-Garry, 2020). After completing these assigned activities, students returned to the “main room” in the virtual platform to discuss their work.
Integrated debriefing methods were used to guide the discussion about the students' conceptual model information and brief care plans (Orsini-Garry, 2019, Orsini-Garry, 2020). Use of integrated debriefing provided opportunity to review correct use of the adapted mental status exam form and CAM, patient specific factors related to delirium, and evidence-based strategies for mitigating delirium. In this way, students learned that multiple nursing interventions have been identified that help mitigate delirium. They were able to see how nurses can prevent 40% of delirium episodes by identifying patients at risk and implementing preventative nursing measures, which include nonpharmacological interventions (Casey, 2019; LaHue et al., 2020). This interactive method for identifying the conceptual model components and an appropriate brief care plan (Orsini-Garry, 2019, Orsini-Garry, 2020) made obvious the importance of implementing multi-component, multi-sensory interventions to prevent episodes of delirium.
We used the AGS Delirium Prevention Tool Kit (Delirium Prevention Toolkit, 2019; AGS coCare HELP™, 2019c) as a resource to identify evidence-based nursing interventions to mitigate delirium for the brief care plans. These included interventions used to implement the 4Ms developed by the IHI and the John A. Hartford Foundation (IHI, 2019). The 4Ms include four elements; mentation, what matters most to the patient, medication, and mobility (IHI, 2019). Students learned that the 4Ms framework has been adopted by many healthcare systems to achieve improved patient outcomes, providing a path to Magnet status (IHI, 2019). They were asked to identify ways this framework could be applied to the avatar, ATI, or video patient. The focus on expected patient outcomes encouraged critical thinking and developing clinical reasoning skills. Through these activities, students realized that this four-step care bundle increases awareness, prevention strategies, monitoring, and treatment of delirium by nurses in clinical practice (LaHue et al., 2020). Similarly, we also incorporated evidence-based strategies identified by HELP (Delirium Prevention Toolkit, 2019; AGS coCare HELP™, 2019c) such as having a clock in the patient's room and utilizing a white board in the room to assist the patient in remaining oriented to their plan of care, health care providers' names, date, and name of the hospital. Brief care plans included reviewing current medications, having personal pictures, playing music, using reminiscence items or memory books, encouraging mobility, and utilization of an iPad to video call family or friends as interventions to help provide cognitive stimulation to the patient, maintain family connection, and keep the patient oriented (Inouye et al., 2014; Kotfis et al., 2020). Through the interactive small group activities and integrated debriefing discussions, students understood that evidence-based HELP strategies such as these reduce both the severity and duration of delirium episodes and were included in the conceptual model and brief care plan (Orsini-Garry, 2019, Orsini-Garry, 2020).
Debriefing provided a discussion of the unfolding case that was presented in the VS within a group setting. The discussions were crafted to provide examples of evidence-based interventions for patients with delirium. Students' transfer of knowledge of actions in each area of the 4Ms framework and the HELP strategies for the avatar patients provided opportunity for synthesizing knowledge and provided examples of effective methods to decrease gaps in care. Discussions with the students regarding the rationale to develop competencies in using the 4 M framework model and implementing HELP strategies emphasized the growing trend of hospitals becoming more Age Friendly.
Students were also assigned reflective journaling to document their individual experiences identifying and assessing for delirium along with use of the CAM. These were submitted to the clinical faculty member and used for evaluation of the experience as described below.
At the completion of the VS clinical day, a post-conference was conducted with final debriefing to summarize the educational activities performed by students and underscore important concepts. The final debriefing provided a review of important content such as the definition of delirium, types, signs and symptoms, risk factors, and potential complications. Nursing activities were reviewed including methods for confirming delirium versus dementia, use of screening instruments, and options for nursing diagnoses, interventions, and patient/family education. The importance of assessing the patient's cognitive status was underscored throughout to avoid missing the first signs of delirium because of the focus on the primary medical-surgical diagnosis (Kotfis et al., 2020). Advocacy for timely intervention to prevent delirium was emphasized throughout the day.
Opportunities to discuss gaps in knowledge and “aha” moments were created by soliciting these from each student using a “round robin” method. Each student was also asked to state how they would use knowledge attained during the VS clinical day in their future nursing practice.
Evaluation of the virtual simulation clinical experience
Student evaluation
Clinical faculty professors were able to evaluate student knowledge and application throughout the day. For example, the students' understanding of the appropriate use of the CAM assessment in the VS was noted when students recognized and demonstrated the importance of obtaining a baseline mental status exam prior to a CAM assessment (Pedersen et al., 2019). Discussion was embedded throughout the experience. Knowledge acquisition was assessed throughout VS activities, in case study answers, and on course exams.
Further evaluation of the students' knowledge included review and feedback on completed conceptual model, brief care plans (Orsini-Garry, 2019, Orsini-Garry, 2020), and the students' journals. Faculty members identified key points that were to be included in the conceptual model and brief care plan for the VS case studies. VS and in-person clinical experiences are graded as ‘pass/fail.’ Students who participated fully and included the identified key points on their conceptual models and brief care plans achieved a grade of ‘pass.’ Reflective journaling is another key strategy in assuring that salient concepts taught are understood by students. Collectively, students reported that they recognized that the knowledge attained was transferrable to their practice as future nurses. While most were skeptical at first, they ultimately agreed that the experience provided them with a valuable opportunity to develop skills in assessing for and mitigating delirium.
Evaluation of the virtual simulation clinical day
Following the VS clinical day, clinical faculty discussed successes and challenges they encountered. Most of the issues raised were not related to the content or organization of the day. Rather, they were about technical challenges with connecting to the virtual platform, successfully transitioning students into and back out of breakout groups, or smoothly starting and running the vSim or YouTube videos. These issues were resolved either through demonstration by a colleague or with university instructional technology assistance. Overall, the clinical faculty agreed that the VS clinical day was a valuable learning experience for the students. It was particularly valuable to have the ability to effectively coach/facilitate critical thinking by the student through the VS at a pace that is individualized for the student(s).
Feedback on the experience was also obtained from students. The above-mentioned reflective journals had several positive comments such as how students appreciated the opportunity to apply their knowledge for specific patients [portrayed in the vSims, ATI and YouTube video] despite not being able to be in clinical settings due to COVID-19. Additionally, comments from the Student Evaluation of Teaching (SET) questionnaires completed by students at the end of the semester indicated a positive VS clinical experience, despite their universal preference to be able to have ‘live’ clinical as soon as possible.
Future plans
Based on student and faculty feedback and student performance we have identified improvements that we will incorporate for future delirium VS days. Students will have an opportunity to break into groups three times in the VS day. During the first breakout, early in the VS day they will be asked to do a role play educational activity. The role play will provide an opportunity for students to take on the role of the nurse and/or family member to increase their understanding of both perspectives. The next breakout will be to discuss evidence-based, non-pharmacologic nursing interventions for preventing or managing delirium. The final break out will remain as described above. In the breakout sessions students will address the three main presentations of delirium in patients (hyperactive, hypoactive, and mixed delirium). During debriefing the content of these additional breakout sessions will be addressed.
Conclusion
The VS delirium clinical day provided an opportunity to apply in a clinical virtual setting the foundational knowledge gained from readings and didactic classroom presentation and discussion. Students had the opportunity to use critical thinking skills and develop care plans for virtual patients to eliminate gaps in care (Oldham et al., 2018). The use of technology in nursing education is more important now than ever before. The COVID-19 pandemic created significant changes in both the formal education of nursing students as well as the clinical environments in which these students will soon be working.
Given the increasing focus on using competencies to evaluate student nurses, we will increase use of simulated experiences. COVID-19 created a need for VS, this technology will continue to be useful in a post pandemic world. VS clinical days provide an opportunity to expand nursing education in a cost-effective manner as recommended in The Future of Nursing Report (Institute of Medicine, 2010). VS clinical assures each student has a patient with the issue, diagnosis, or need under consideration. In any given semester, the students may not witness a patient exhibiting the first signs of delirium or diagnosed with delirium. The “on demand” nature of VS means the clinical faculty member is not reliant on a specific patient population that has all the symptoms needed to reach the relevant competencies associated with the clinical learning objectives. Establishing specific goals and planning the experience carefully provides a framework for embedded evaluation through integrated debriefing and related educational activities, such as the conceptual model and brief care plan. Using reflective journaling provides an added opportunity for assessment and evaluation. Leveraging simulation and technology will benefit student nurses, clinical care of patients, as well as the health care system.
Appendix A
Conceptual model
© Orsini-Garry, 2019, used with permission.
Appendix B
Brief Care Plan for Weekly Nursing Process and Teaching Plan
Appendix C
Appendix D
MENTAL STATUS EXAM Sheet
(Varcarolis, 2017) https://www.ncbi.nlm.nih.gov/books/NBK320/ https://www.aafp.org/afp/2016/1015/p635.html http://oscarcanada.org/oscar-users/emr-resource/eform/eform-examples/mental-health/amsit-mental-status-documentation/amsit-mental-status-documentation-example-pdf/view (Martin, 1990)
© Orsini-Garry, 2019, used with permission.
References
- AGS CoCare HELPTM . 2019. Delirium Prevention Toolkit Amidst COVID-19 (copyright HELP, 1999)https://help.agscocare.org/table-of-contents//H00107 Available at: [Google Scholar]
- American Geriatrics Society [AGS] CoCare Hospital Elder Life Program (HELP™) 2019. Confusion Assessment Method, Hospital Elder Life Program, LLC.https://help.agscocare.org/productAbstract/H00101 Available at: [Google Scholar]
- Aredes N.D.A., Dias D.M.V., Fonseca L.M.M., Campbell S.H., Martins J.C.A., Rodrigues M.A. E-baby skin integrity: Evidence-based technology innovation for teaching in neonatal nursing. Anna Nery School Journal of Nursing/Escola Anna Nery Revista de Enfermagem. 2018;22(3):1–9. doi: 10.1590/2177-9465-EAN-2017-0424. [DOI] [Google Scholar]
- Bricoli B. In: Nurses Improving Care for Healthsystem Elders. Fulmer T., Glassman K., Greenberg S., Rosenfeld P., Gilmartin M., Mezey M., editors. Springer; NY: 2020. Chapter 12: Program expansion in the age of digital learning and engagement; pp. 167–171. [DOI] [Google Scholar]
- Bruce R., Levett-Jones T., Courtney-Pratt H. Transfer of learning from university-based simulation experiences to nursing students' future clinical practice: An exploratory study. Clinical Simulation in Nursing. 2019;35(10):17–24. doi: 10.1016/j.ecns.2019.06.003. [DOI] [Google Scholar]
- Cant R.P., Cooper S.J. Bibliometric scan of the 100 most cited nursing simulation articles. Clinical Simulation in Nursing. 2019;36:1–7. doi: 10.1016/j.ecns.2019.06.004. [DOI] [Google Scholar]
- Casey G. Kai Tiaki Nursing New Zealand. 2019;25(10):20–24. [Google Scholar]
- Casida D., Molen J.V. Using storyboarding pedagogy to promote learning in a distance education program. Journal of Nursing Education. 2018;57(5) doi: 10.3928/01484834-20180420-14. 319-319. [DOI] [PubMed] [Google Scholar]
- Delirium prevention toolkit amidst COVID-19 American Geriatrics Society. 2019. https://help.agscocare.org/table-of-contents//H00107
- Delva S., Nkimbeng M., Chow S., Renda S., Han H., D'Aoust R. Views of regulatory authorities on standards to assure quality in online nursing education. Nursing Outlook. 2019;67(6):747–759. doi: 10.1016/j.outlook.2019.06.011. [DOI] [PubMed] [Google Scholar]
- Detroyer E., Dobbles F., Teodorczuk A., Deschodt M., Depaifve Y., Joosten E., Milisen K. Effect of an interactive e-learning tool for delirium on patient and nursing outcomes in a geriatric hospital setting: Findings of a before-after study. BMC Geriatrics. 2018;18 doi: 10.1186/s12877-018-0715-5. https://doi-org.ezproxy.lib.uconn.edu/10.1186/s12877-018-0715-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer T.A., Levett-Jones T., Flenady T., Reid-Searl K., Andersen P., Guinea S., Goodwin B.C. Responding to the unexpected: Tag team patient safety simulation. Clinical Simulation in Nursing. 2019;36:8–17. doi: 10.1016/j.ecns.2019.06.007. [DOI] [Google Scholar]
- Goncalves S.A., Watson S.M. Clinical conundrum? An innovative clinical makeup approach. Journal of Nursing Education. 2019;58(11):675. doi: 10.3928/01484834-20191021-13. [DOI] [PubMed] [Google Scholar]
- Hardenberg J., Rana I., Tori K. Simulation exposure improves clinical skills for postgraduate critical care nurses. Clinical Simulation in Nursing. 2019;28:39–45. doi: 10.1016/j.ecns.2018.12.007. [DOI] [Google Scholar]
- Hirota K. Preoperative management and postoperative delirium: The possibility of neurorehabilitation using virtual reality. Journal of Anesthesia. 2020;34(1):1–4. doi: 10.1007/s00540-019-02660-2. [DOI] [PubMed] [Google Scholar]
- Huun K. Virtual simulations in online nursing education: Align with quality matters. Clinical Simulation in Nursing. 2018;22:26–31. doi: 10.1016/j.ecns.2018.07.002. [DOI] [Google Scholar]
- Inouye S.K., Westendorp R.G.J., Saczynski J.S. Delirium in elderly people. The Lancet. 2014 doi: 10.1016/S0140-6736(13)60688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inova Health System. [Inova Health System] Confusion assessment monitoring (Old version) [Video]. YouTube. 2020, March 6. https://youtu.be/cRZtF9F1mJU Retrieved from.
- Institute for Healthcare Improvement Age-friendly health systems: Guide to using the 4Ms in the care of older adults. 2019. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHIAgeFriendlyHealthSystems_GuidetoUsing4MsCare.pdf
- Institute of Medicine The future of nursing: Leading change advancing health. 2010. https://books.nap.edu/openbook.php?record_id=12956&page=R1
- Kardong-Edgren S., Farra S.L., Alinier G., Young H.M. A call to unify definitions of virtual reality. Clinical Simulation in Nursing. 2019;31:28–34. [Google Scholar]
- King T.S., Nininger J.M. Quality improvement in online course development: Igniting the online teaching team. CIN:Computers, Informatics, Nursing. 2019;37(7):349–356. doi: 10.1097/CIN.0000000000000517. [DOI] [PubMed] [Google Scholar]
- Kluwer W. VSIM for nursing mental health. 2021. https://www.wolterskluwer.com/en/solutions/lippincott-nursing-faculty/vsim-for-nursing Retrieved from.
- Kotfis K., Williams Roberson S., Wilson J.E., Dabrowski W., Pun B.T., Ely E.W. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Critical Care. 2020;24(1) doi: 10.1186/s13054-020-02882-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaHue S.C., James T.C., Newman J.C., Esmaili A.M., Ormseth C.H., Ely E.W. Collaborative delirium prevention in the age of COVID-19. Journal of the American Geriatrics Society. 2020;68(5):947–949. doi: 10.1111/jgs.16480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieow J.L.M., Chen F.S.M., Song G., Tang P.S., Kowitlawakul Y., Mukhopadhyay A. Effectiveness of an advanced practice nurse-led delirium education and training programme. International Nursing Review. 2019;66(4):506–513. doi: 10.1111/inr.12519. [DOI] [PubMed] [Google Scholar]
- Lopreiato J.O. Agency for Healthcare Research and Quality, AHRQ Publication; 2016. Healthcare simulation dictionary. [Google Scholar]
- Luckenbach A., Nelson-Brantley H., Ireland-Hoffmann G. Affiliate faculty in nursing clinical education: Student and faculty perceptions. Nurse Educator. 2021;46:245–249. doi: 10.1097/NNE.0000000000000925. [DOI] [PubMed] [Google Scholar]
- Marcantonio E.R. Delirium in hospitalized older adults. The New England Journal of Medicine. 2017;377(15):1456–1466. doi: 10.1056/NEJMcp1605501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin D.C. In: Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd. Walker H.K., Hall W.D., Hurst JJ.W., editors. Butterworths; Boston: 1990. Chapter 207 the mental status examination.https://www.ncbi.nlm.nih.gov/books/NBK320/?_ga=2.192782250.1630237103.1638544284-748634468.1638544284 C [PubMed] [Google Scholar]
- Nurses Improving Care for Healthsystem Elders (NICHE) 2021. https://nicheprogram.org/
- Oldham M.A., Flanagan N.M., Khan A., Boukrina O., Marcantonio E.R. Responding to ten common delirium misconceptions with best evidence: An educational review for clinicians. Journal of Neuropsychiatry and Clinical Neurosciences. 2018;30(1):51–57. doi: 10.1176/appi.neuropsych.17030065. [DOI] [PubMed] [Google Scholar]
- Orsini-Garry A. University of Connecticut School of Nursing; Storrs:CT: 2019. Conceptual model. [Google Scholar]
- Orsini-Garry A. University of Connecticut School of Nursing; Storrs:CT: 2020. Nursing diagnosis sheet. [Google Scholar]
- Padilha J.M., Machado P.P., Ribeiro A., Ramos J., Costa P. Clinical virtual simulation in nursing education: Randomized controlled trial. Journal of Medical Internet Research. 2019;21(3) doi: 10.2196/11529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen I., Lee Solevåg A., Solberg M.T. Simulation-based training promotes higher levels of cognitive control in acute and unforeseen situations. Clinical Simulation in Nursing. 2019;34:6–15. doi: 10.1016/j.ecns.2019.05.003. [DOI] [Google Scholar]
- Pinkhasov A. What is delirium? [Video]. YouTube. 2019. https://www.youtube.com/watch?v=vHDNMsDXvSs Retrieved from.
- Quality MattersTM 2021. https://www.qualitymatters.org/why-quality-matters/about-qm
- Richter S.L., Schuessler J.B. Nursing faculty experiences and perceptions of online teaching: A descriptive summary. Teaching & Learning in Nursing. 2019;14(1):26–29. doi: 10.1016/j.teln.2018.09.004. [DOI] [Google Scholar]
- Rourke S. How does virtual reality simulation compare to simulated practice in the acquisition of clinical psychomotor skills for pre-registration student nurses? A systematic review. International Journal of Nursing Studies. 2020;102:1–7. doi: 10.1016/j.ijnurstu.2019.103466. [DOI] [PubMed] [Google Scholar]
- Smart D., Ross K., Carollo S., Williams-Gilbert W. Contextualizing instructional technology to the demands of nursing education. CIN:Computers, Informatics, Nursing. 2020;38(1):18–27. doi: 10.1097/CIN.0000000000000565. [DOI] [PubMed] [Google Scholar]
- Sofer D. The value of simulation in nursing education. AJN, American Journal of Nursing. 2018;118:17–18. doi: 10.1097/01.NAJ.0000532063.79102.19. [DOI] [PubMed] [Google Scholar]
- Stanley M.J., Serratos J., Matthew W., Fernandez D., Dang M. Integrating video simulation scenarios into online nursing instruction. Journal of Nursing Education. 2018;57(4):245–249. doi: 10.3928/01484834-20180322-11. [DOI] [PubMed] [Google Scholar]
- Tyler L., Joggyah R., Clemett V. Simulation-based nurse education for comorbid health problems: A systematic review. Clinical Simulation in Nursing. 2019;37(12):50–61. doi: 10.1016/j.ecns.2019.08.004. [DOI] [Google Scholar]
- Varcarolis E. Essentials of Psychiatric Mental Health Nursing: A Communication Approach to Evidence-Based Care. 3rd. Elsevier; 2017. Communication skills: medium for all nursing practice; p. 80. [Google Scholar]
- Wei L.A., Fearing M.A., Sternberg E.J., Inouye S.K. The confusion assessment method: A systematic review of current usage. Journal of the American Geriatrics Society. 2008;56(5):823–830. doi: 10.1111/j.1532-5415.2008.01674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey N.R. Technology and teaching-learning: Opportunities and restrictions. Nursing Science Quarterly. 2018;31(4):333–334. doi: 10.1177/0894318418792880. [DOI] [PubMed] [Google Scholar]