Abstract
Aim
To perform a systematic review of cardiopulmonary resuscitation (CPR) and/or defibrillation in the prone position compared to turning the patient supine prior to starting CPR and/or defibrillation.
Methods
The search included PubMed, Embase, Web of Science, Cochrane, CINAHL Plus, and medRxiv on December 9, 2020. The population included adults and children in any setting with cardiac arrest while in the prone position. The outcomes included arterial blood pressure and end-tidal capnography during CPR, time to start CPR and defibrillation, return of spontaneous circulation, survival and survival with favorable neurologic outcome to discharge, 30 days or longer. ROBINS-I was performed to assess risk of bias for observational studies.
Results
The systematic review identified 29 case reports (32 individual cases), two prospective observational studies, and two simulation studies. The observational studies enrolled 17 patients who were declared dead in the supine position and reported higher mean systolic blood pressure from CPR in prone position (72 mmHg vs 48 mmHg, p < 0.005; 79 ± 20 mmHg vs 55 ± 20 mmHg, p = 0.028). One simulation study reported a faster time to defibrillation in the prone position. Return of spontaneous circulation, survival to discharge or 30 days were reported in adult and paediatric case reports. Critical risk of bias limited our ability to perform pooled analyses.
Conclusions
We identified a limited number of observational studies and case reports comparing prone versus supine CPR and/or defibrillation. Prone CPR may be a reasonable option if immediate supination is difficult or poses unacceptable risks to the patient.
Keywords: Advanced Life Support, Basic Life Support, Cardiac arrest, Prone, Cardiopulmonary resuscitation, Defibrillation, COVID-19, Systematic review, ILCOR
Introduction
Prone positioning is recommended for severe hypoxemic respiratory failure, based on clinical trial data showing decreased mortality with this treatment.1 It has been utilized increasingly since the COVID-19 pandemic for patients with acute respiratory distress syndrome (ARDS) and severe hypoxemia. Multiple investigators have reported improvements in hypoxemia related to COVID-19 with prone positioning in patients being treated with invasive mechanical ventilation, extracorporeal life support, and those on noninvasive respiratory support (e.g. high-flow nasal cannula or continuous positive airway pressure).2., 3., 4., 5. Due to this increased use of prone positioning, the question of how to proceed when a patient has a cardiac arrest while in the prone position has become increasingly relevant. Patients who are prone when they experience a cardiac arrest, especially if intubated and sedated, can be challenging to turn supine quickly. Furthermore, turning such a patient supine prior to starting cardiopulmonary resuscitation (CPR) will necessarily lead to some delay in chest compressions. The prior recommendation from the American Heart Association (AHA) has been to perform CPR in the supine position whenever possible, only performing CPR with a patient in the prone position if supination is not feasible or safe.6., 7. Interim COVID-19 guidance for cardiac arrest from the AHA states that leaving patients with an advanced airway in the prone position for CPR with hands in the standard position over the T7/10 vertebral bodies should be considered unless they can safely and rapidly be turned supine.8., 9. The interim guidance on COVID-19 from the International Liaison Committee on Resuscitation (ILCOR) did not provide any treatment recommendations regarding CPR in the prone position.10
In 2020, the ILCOR Advanced Life Support (ALS) and Basic Life Support (BLS) Task Forces determined that there was sufficient need for guidance on the best approach to initiating CPR in prone patients, and that a new Consensus on Science and Treatment Recommendations (CoSTR) should be developed. ILCOR generates CoSTRs, based on systematic reviews, to provide some guidance that can then be used for regional and national councils to develop their own guidelines as they deem appropriate. Two scoping reviews and one systematic review have been published recently on the topic of CPR in the prone position.11., 12., 13. However, the previous systematic review11 did not include patients who suffered from cardiac arrest while prone and were turned supine prior to initiation of CPR, limiting any ability to compare the two approaches. The scoping reviews12., 13. did not include bias assessments or certainty of evidence, and therefore cannot be used to generate new ILCOR treatment recommendations.
The ILCOR ALS and BLS Task Forces, together with the Paediatric Life Support Task Force, therefore proceeded with the following systematic review to determine whether performing CPR and/or defibrillation while the cardiac arrest patient remains in the prone position as compared to turning the patient supine prior to initiation of CPR and/or defibrillation improve clinical outcomes to inform the 2021 ILCOR CoSTR.14
Methods
Protocol and registration
The protocol for this review was prospectively submitted to the International Prospective Register of Systematic Reviews (PROSPERO) on January 11, 2021 (registration number CRD42021230691). The protocol is provided in the Supplemental contents. This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.15 The PRISMA checklist is provided in the Supplementary contents. This review was commissioned at no cost by ILCOR and was carried out by ILCOR Task Force (unpaid) members and other volunteers.
Eligibility criteria and outcomes
The study question was framed using the PICOST (Population, Intervention, Comparison, Outcome, Study Design, Time frame) format: in adults and children in any setting (in-hospital or out-of-hospital) with cardiac arrest occurring while in the prone position (P), does performing CPR and/or defibrillation while the patient remains in the prone position (I) as compared to turning the patient supine prior to initiation of CPR and/or defibrillation (C) improve clinical outcomes (O).
Relevant outcomes were prioritized by the ILCOR ALS and BLS Task Forces and based on the available literature. We included arterial blood pressure during CPR, time to initiation of CPR, time to defibrillation for shockable rhythms during CPR, end-tidal carbon dioxide (ETCO2) during CPR, return of spontaneous circulation (ROSC), survival and survival with favorable neurologic outcome to discharge, 30 days or longer.
Randomized controlled trials (RCTs) and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies), case series, case reports, simulation studies, and animal studies were eligible for inclusion. Case series and case reports were included as the writing group was aware that the human data on prone CPR are extremely limited, consisting primarily of case reports. Unpublished studies (e.g., conference abstracts, trial protocols) and editorials were excluded, although case reports published in letter form were included. Scoping reviews and systematic reviews were included for discussion and to assure no primary papers were missed, but data were not extracted from these reviews.
Information sources and search strategy
All years and languages were included as long as there was an English abstract. The search was conducted on December 9, 2020 and included the databases of PubMed, Embase, Web of Science, Cochrane, CINAHL Plus, and medRxiv. Clinicaltrials.gov and PROSPERO were searched for ongoing or other completed studies. The search strategy is provided in the Supplemental content.
Study selection
Two reviewers, using pre-defined screening criteria, independently screened all titles and abstracts retrieved from the systematic search. Any disagreements regarding inclusion or exclusion were resolved by discussion between the reviewers and with two additional reviewers as needed. The Kappa-values for interobserver variance were calculated. The two reviewers then reviewed the full text-reports of all potentially relevant publications passing the first level of screening. Any disagreement regarding eligibility was resolved by discussion.
Data collection
Two reviewers, using a pre-defined standardized data extraction form, extracted data from individual studies. Any discrepancies in the extracted data were identified and resolved by discussion and consensus.
Risk of bias in individual studies
Four investigators (working in pairs of two) independently assessed risk of bias using the ROBINS-I tool for observational studies16 and a tool adapted from Murad et al. to assess the methodological quality of case reports.17 For ROBINS-I, risk of bias is assessed within domains including: (1) bias due to confounding, (2) bias in selection of participants into the study, (3) bias in classification of interventions, (4) bias due to deviations from intended interventions (5) bias due to missing data, (6) bias in measurement of outcomes, (7) bias in selection of the reported result, and (8) overall bias.16 The methodological quality of case reports was assessed using four domains: selection, ascertainment, causality, and reporting.17 Disagreements were resolved by discussion. Risk of bias was assessed by outcome but reported by study, as the risk of bias was similar across outcomes.
Data synthesis and confidence in cumulative evidence
From the writing group’s knowledge of the evidence, it was thought that the risk of bias in the available evidence, consisting primarily of case reports and small observational studies, would be too high to allow for meta-analysis. A narrative synthesis was therefore the primary plan, but the approach to meta-analysis and assessment of heterogeneity in the case of evidence being more robust than anticipated was detailed in the protocol, which is provided in the Supplemental content. If feasible, we planned to provide the narrative synthesis for adult and paediatric studies separately, medical and surgical cases separately, as well as for the entire group.
Results
Study selection
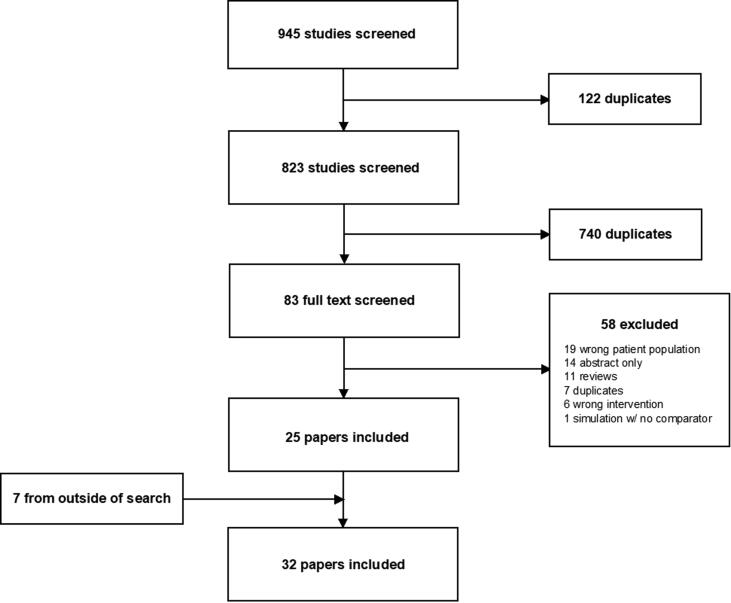
Our search identified 823 unique titles/abstracts, of which 738 were excluded based on initial review of the abstracts (Kappa = 0.66). After full-text review of 85 papers, an additional 60 studies were excluded, and 7 were added after review of bibliographies of prior review papers identified, leaving 32 studies for inclusion (Kappa for full text review = 0.94; Fig. 1 PRISMA). In total, 29 case reports (describing 32 individual cases), 2 prospective nonrandomized studies, one simulation study, and one simulation study reported in conjunction with one of the 29 case reports were included. A tabulated overview of these studies is provided in the Supplemental content.
Fig. 1.
PRISMA Diagram.
Observational studies
We identified only two human observational studies, enrolling a total of 17 patients in the intensive care unit who had already been declared dead due to failure to achieve ROSC with conventional CPR in the supine position.9., 18. These studies were deemed at critical risk of bias due primarily to confounding and, in the case of one study,18 incomplete reporting of the outcome (Table 1). Due to the critical risk of bias, no meta-analysis was performed. Certainty of evidence assessed as very low for both studies due to risk of bias, indirectness, and imprecision (Table 1). Blood pressure during CPR was the only reported outcome, and the investigators compared blood pressure achieved with prone compressions to blood pressure during compressions delivered with the patient supine. Both studies reported significantly higher mean systolic blood pressure during prone compressions (72 mmHg vs 48 mmHg, p < 0.0059, 79 ± 20 mmHg vs 55 ± 20 mmHg, p = 0.02818, while only one found a significant increase in mean diastolic pressure with prone compressions (34 mmHg vs 24 mmHg, NS9, 17 ± 10 mmHg vs 13 ± 7 mmHg, p = 0.02818. Supine data were missing in 3/11 patients from one study.18
Table 1.
Bias assessment for observational studies.
Case reports
All case reports were considered at critical risk of bias. Of the twenty adult case reports (Table 2), twelve had CPR commenced in prone position19., 20., 21., 22., 23., 24., 25., 26., 27., 28., 29., 30. and eight were supinated prior to commencement of CPR.31., 32., 33., 34., 35., 36., 37. Of the 12 paediatric case reports (Table 3), 11 had CPR commenced prone position29., 38., 39., 40., 41., 42., 43., 44., 45., 46. while one was supinated prior to initiation of CPR.47 Of the 32 case reports (20 adult and 12 paediatric), 31 cases (19 adult and 12 paediatric) were of patients in a prone position in the operating room, most often with head fixation or ongoing surgery or instrumentation that could considerably hinder the ability to safely and quickly turn the patients to supine position. Only one adult case was a patient in the prone position in the intensive care unit.22
Table 2.
Reported outcomes for CPR commenced in prone vs supine position: 20 adult cases.
| Adult: CPR commenced prone (n = 12)19., 20., 21., 22., 23., 24., 25., 26., 27., 28., 29., 30. |
Adult: patient supinated before CPR (n = 8)31., 32., 33., 34., 35., 36., 37. |
|||
|---|---|---|---|---|
| Studies reporting | Achieving outcome | Studies reporting | Achieving outcome | |
| ROSC | 12 | 12/12 | 8 | 3/8 |
| Survival to hospital discharge | 5 | 5/5 | 7 | 2/7 |
| Survival to 30 days or longer | 1 | 1/1 | 6 | 2/6 |
ROSC = return of spontaneous circulation.
Table 3.
Reported outcomes for CPR commenced in prone vs supine position: 12 paediatric cases.
| Paediatric: CPR commenced prone (n = 11)29., 38., 39., 40., 41., 42., 43., 44., 45., 46. |
Paediatric: patient supinated before CPR (n = 1)47 |
|||
|---|---|---|---|---|
| Studies reporting | Achieving outcome | Studies reporting | Achieving outcome | |
| ROSC | 11 | 10/11 | 1 | 1/1 |
| Survival to hospital discharge | 10 | 7/10 | 1 | 1/1 |
| Survival to 30 days or longer | 5 | 2/5 | 0 | NA |
ROSC = return of spontaneous circulation.
Resuscitation outcomes
Comparison of commonly reported outcomes from prone vs supine CPR are shown in Table 2 (adult case reports) and 3 (paediatric case reports). The critical outcome of time to CPR was reported in eight adult cases19., 22., 24., 27., 29., 30., 32., 35. and seven paediatric cases.29., 38., 39., 40., 43., 44. Time to CPR for all except for one adult case report35 were only reported qualitatively or not reported at all. ‘Immediate’ prone CPR was reported in six adult cases19., 22., 24., 27., 29., 30. and seven paediatric cases.29., 38., 39., 40., 43., 44. One adult case reported CPR ‘immediately’ after supination32 and one adult case reported CPR commenced after supination 6 min following cardiac arrest.35 Two simulation studies reported that the time to supinate the patient was 50 ± 34 s48 and 110 s.21 The mean time to start chest compressions in supine position was 77 ± 31 s in one simulation study.48
We identified one simulation study that reported time to prone defibrillation without chest compressions of 22 s (1 group) compared with a mean time of 108 ± 61 s (13 groups) when the patient was supinated for CPR and defibrillation.48 Time to defibrillation was not reported in any adult or paediatric case report.
Return of spontaneous circulation was reported in all studies. Occurrence of ROSC in those with CPR started prone vs supine is presented in Table 2, Table 3. ETCO2 during CPR in the prone position was reported in five adult cases,23., 24., 25., 30., 34. with values ranging from 15 mmHg30 to 33 mmHg25; and two paediatric cases both of which reported ETCO2 ≥ 10 mmHg with prone compressions.44., 46.
Outcomes at hospital discharge
Survival to hospital discharge with favourable neurological outcome was not explicitly reported in any adult or paediatric case. There were implicit reports of survival to hospital discharge with favourable neurological outcome in eight adult cases (‘without neurologic deficit’21; ‘no cerebral injury’20; ‘recovered uneventfully’23; ‘without deficits’33; ‘awake and well oriented at 7 days’22; ‘without sequelae’24; ‘could carry out simple tasks’25; and ‘discharged from hospital in a stable neurological condition’30) and seven paediatric cases (‘no evidence of significant cerebral dysfunction’38; ‘returned to baseline over two weeks’39; ‘recovered without sequelae’40; ‘no adverse neurological sequelae’41; ‘in good condition’47; ‘made an uneventful recovery’29; and ‘unchanged from preoperative status’42).
Survival to hospital discharge was explicitly reported in 13 adult cases20., 21., 23., 24., 28., 30., 31., 32., 33., 34., 35., 36. and 11 paediatric cases.29., 38., 39., 40., 41., 42., 43., 44., 45., 47. Survival to 30 days or longer was reported in only one adult case where CPR was initiated prone25 and six adult cases31., 32., 33., 34. supinated before CPR started. Five paediatric cases reported the outcome of survival to 30 days or longer.38., 40., 43., 44. Outcomes by prone/supine CPR initiation are summarized in Table 2, Table 3.
Outcomes at 30 days or longer
Survival with favourable neurological outcome at 30 days or longer was not explicitly reported in any adult or paediatric case. There were implicit reports of survival with favourable neurological outcome at 30 days or longer in two adult cases (‘without deficits’33; ‘able to perform his work and activities of daily living independently’35) and two paediatric cases (‘no abnormal neurological signs … within accepted limits for achondroplasia’38; ‘recovered without sequelae’40).
Discussion
In this systematic review on prone vs supine CPR/defibrillation, only a limited number of prospective nonrandomized studies, case reports, and simulation studies were identified. The lack of comparative studies examining any clinical outcomes leaves us without any real evidence for whether immediate supination or provision of chest compressions and/or defibrillation in the prone position is most beneficial. Supine CPR remains best practice and is known to be effective. However, the very limited evidence available suggests that prone CPR can produce adequate hemodynamics and may be a reasonable option if immediate supination is difficult or poses unacceptable risks to the patient.
The aetiology of cardiac arrest may also influence the urgency of supination. For example, a primary airway problem such as a dislodged tracheal tube may require immediate supination, whereas the need for haemorrhage control during surgery in the prone position may necessitate CPR in the prone position. The difficulty of supinating a patient will vary widely based on patient size, personnel immediately available, and interventions in place such as chest tubes, advanced airways, intravenous lines, personal protective equipment and isolation requirements, and potentially open wounds/exposed hardware (in the case of patients in the operating room).
The relative risk of delaying the initiation of CPR and defibrillation vs the possible risk of prone CPR/defibrillation being less effective remains unclear. In many intensive care units, patients who are prone and on mechanical ventilation are likely to already have continuous arterial blood pressure and ETCO2 monitoring, thus allowing for the rapid assessment of the effectiveness of prone compressions. These patients also often have severe hypoxemia and may have had tracheal tubes in place for prolonged periods, raising the possibility of airway dislodgement or blockage as a contributing factor to the cardiac arrest. Additional studies could include larger observational studies or case series representing the total experience of a center or centers, simulation studies, or even additional case reports that report quantitative metrics such as time to initiation of CPR/defibrillation in the prone position and ETCO2 and arterial blood pressure during prone compressions. More data on patients in intensive care units are especially needed as the vast majority of published case reports on prone CPR are from patients in a prone position for spinal or brain surgery in the operating room.
Limitations
This systematic review has several limitations. The lack of randomized controlled studies limited our ability to definitively compare the efficacy of prone vs supine chest compression or defibrillation. With one exception,22 the identified case reports described events and outcomes of operating room patients, thereby limiting our ability to extrapolate these findings to patients proned for hypoxemic respiratory failure in the emergency department or inpatient settings or out-of-hospital cardiac arrest patients found in a prone position. Finally, the significant risk of bias from the observational studies limited our ability to perform meta-analyses.
Conclusions
We identified a limited number of observational studies and case reports comparing prone vs supine CPR and defibrillation. Prone CPR may be a reasonable option if immediate supination is difficult or poses unacceptable risks to the patient.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CRediT authorship contribution statement
Cindy H. Hsu: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. Julie Considine: Methodology, Formal analysis, Investigation, Writing – original draft. Rahul D. Pawar: Formal analysis, Investigation, Writing – original draft. Jacqueline Cellini: Methodology, Resources, Writing – review & editing. Stephen M. Schexnayder: Writing – review & editing. Jasmeet Soar: Writing – review & editing. Theresa M. Olasveengen: Writing – review & editing. Katherine M. Berg: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Supervision.
Acknowledgments
Acknowledgement
The authors would like to thank Claudio Sandroni and Takahiro Nakashima for assistance with translation of non-English articles.
International Liaison Committee on Resuscitation’s (ILCOR)
Advanced Life Support Task Force: Lars W. Andersen, Katherine M. Berg, Bernd W. Böttiger, Clifton W. Callaway, Keith Couper, Charles D. Deakin, Michael W. Donnino, Ian R. Drennan, Karen Hirsch, Cindy H. Hsu, Peter Morley, Tonia C. Nicholson, Jerry P. Nolan, Brian J. O’Neil, Robert W. Neumar, Edison F. Paiva, Michael J. Parr, Joshua C. Reynolds, Claudio Sandroni, Jasmeet Soar, Tzong-Luen Wang, Michelle Welsford.
Basic Life Support Task Force: Theresa Olasveengen, Suzanne Avis, Sung Phil Chung, Katie Dainty, Fredrik Folke, Colina Malta Hansen, Kevin Hung, Takanari Ikeyama, Peter Kudnechuk, Anthony Lagina, Chika Nishiyama, Guiseppe Ristagno, Christer Smith, Micheal Smyth, Jane Wigginton, Tetsuo Hatanaka, Andrew Travers, Christian Vaillancourt.
Paediatric Life Support Task Force: Richard Aickin, Allan De Caen, Dianne Atkins, Ng Kee Chong, Gene Ong, Anne-Marie Guerguerian, Gabrielle Nuthall, Patrick van de Voorde, Bob Bingham, Janice Tijssen, Amelia Reis, Thomaz Bittencourt Couto, Stephen Schexnayder, Vinay Nadkarni, Ian Maconochie.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2021.100186.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Guérin C., Reignier J., Richard J.-C., et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 2.Coppo A., Bellani G., Winterton D., et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8:765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winearls S., Swingwood E.L., Hardaker C.L., et al. Early conscious prone positioning in patients with COVID-19 receiving continuous positive airway pressure: a retrospective analysis. BMJ Open Respir Res. 2020;7 doi: 10.1136/bmjresp-2020-000711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shelhamer M.C., Wesson P.D., Solari I.L., et al. Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: A cohort study and analysis of physiology. J Intensive Care Med. 2021;36:241–252. doi: 10.1177/0885066620980399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ehrmann S., Li J., Ibarra-Estrada M., et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cave D.M., Gazmuri R.J., Otto C.W., et al. Part 7: CPR techniques and devices. Circulation. 2010 doi: 10.1161/CIRCULATIONAHA.110.970970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Panchal A.R., Bartos J.A., Cabañas J.G., et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 8.Edelson D.P., Sasson C., Chan P.S., et al. Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates With Suspected or Confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazer S.P., Weisfeldt M., Bai D., et al. Reverse CPR: a pilot study of CPR in the prone position. Resuscitation. 2003;57:279–285. doi: 10.1016/s0300-9572(03)00037-6. [DOI] [PubMed] [Google Scholar]
- 10.Perkins G.D., Morley P.T., Nolan J.P., et al. International Liaison Committee on Resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. 2020;151:145–147. doi: 10.1016/j.resuscitation.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anez C., Becerra-Bolaños Á., Vives-Lopez A., Rodríguez-Pérez A. Cardiopulmonary resuscitation in the prone position in the operating room or in the intensive care unit: A systematic review. Anesth Analg. 2021;132:285–292. doi: 10.1213/ANE.0000000000005289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moscarelli A., Iozzo P., Ippolito M., et al. Cardiopulmonary resuscitation in prone position: A scoping review. Am J Emerg Med. 2020;38:2416–2424. doi: 10.1016/j.ajem.2020.08.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Douma M.J., MacKenzie E., Loch T., et al. Prone cardiopulmonary resuscitation: A scoping and expanded grey literature review for the COVID-19 pandemic. Resuscitation. 2020;155:103–111. doi: 10.1016/j.resuscitation.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berg K, Hsu CH, Considine J, et al. on behalf of the Advanced Life Support, Basic Life Support and Paediatric Life Support Task Forces at the International Liaison Committee on Resuscitation (ILCOR). Cardiopulmonary Resuscitation and Defibrillation for Cardiac Arrest when Patients are in the Prone Position Consensus on Science with Treatment Recommendations. ILCOR Consensus on Science with Treatment Recommendations (CoSTR). 2021 [cited 2021]. Available at: https://costr.ilcor.org/document/prone-cpr-als-systematic-review.
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sterne J.A.C., Hernán M.A., Reeves B.C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016 doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murad M.H., Sultan S., Haffar S., Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei J., Tung D., Sue S.-H., Wu S.-V., Chuang Y.-C., Chang C.-Y. Cardiopulmonary resuscitation in prone position: a simplified method for outpatients. J Chin Med Assoc. 2006;69:202–206. doi: 10.1016/S1726-4901(09)70219-9. [DOI] [PubMed] [Google Scholar]
- 19.Al Harbi M.K., Alattas K.A., Alnajar M., Albuthi M.F. Prone cardiopulmonary resuscitation in elderly undergoing posterior spinal fusion with laminectomy. Saudi J Anaesthesia. 2020 doi: 10.4103/sja.SJA_165_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brown J., Rogers J., Soar J. Cardiac arrest during surgery and ventilation in the prone position: a case report and systematic review. Resuscitation. 2001;50:233–238. doi: 10.1016/s0300-9572(01)00362-8. [DOI] [PubMed] [Google Scholar]
- 21.Bustillo M.A., Lien C.A., Mack P.F., et al. Optimizing patient access during an emergency while using intraoperative computed tomography. World Neurosurgery. 2019 doi: 10.1016/j.wneu.2018.09.134. [DOI] [PubMed] [Google Scholar]
- 22.Dequin P.F., Hazouard E., Legras A., Lanotte R., Perrotin D. Cardiopulmonary resuscitation in the prone position: Kouwenhoven revisited. Intensive Care Med. 1996;22:1272. doi: 10.1007/BF01709349. [DOI] [PubMed] [Google Scholar]
- 23.Dooney N. Prone CPR for transient asystole during lumbosacral spinal surgery. Anaesth Intensive Care. 2010;38:212–213. [PubMed] [Google Scholar]
- 24.Gomes D. de S., Souza Gomes D. de, Bersot C.D.A. Cardiopulmonary resuscitation in the prone position. Open J Anesthesiol. 2012 [Google Scholar]
- 25.Haffner E, Sostarich AM, Fösel T. Successful cardiopulmonary resuscitation in prone position. Anaesthesist Springer Science and Business Media LLC 2010;59:1099–101. [DOI] [PubMed]
- 26.Loewenthal A., De Albuquerque A.M., Lehmann-Meurice C., Otteni J.C. Efficacy of external cardiac massage in a patient in the prone position. Ann Fr Anesth Reanim. 1993;12:587–589. doi: 10.1016/s0750-7658(05)80627-6. [DOI] [PubMed] [Google Scholar]
- 27.Mishra N., Singh S., Elayat A., Kaushal A. Cardiac arrest in the prone position caused by central venous cannulation-induced cardiac tamponade. Korean J Anesthesiol. 2019;72:394–395. doi: 10.4097/kja.19105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miranda C.C., Newton M.C. Successful defibrillation in the prone position. Br J Anaesth. 2001;87:937–938. doi: 10.1093/bja/87.6.937. [DOI] [PubMed] [Google Scholar]
- 29.Sun W.Z., Huang F.Y., Kung K.L., Fan S.Z., Chen T.L. Successful cardiopulmonary resuscitation of two patients in the prone position using reversed precordial compression. Anesthesiology. 1992;77:202–204. doi: 10.1097/00000542-199207000-00027. [DOI] [PubMed] [Google Scholar]
- 30.Taylor J.C.L., Buchanan C.C.R., Rumball M.J. Cardiac arrest during craniotomy in prone position. Trends Anaesthesia Critical Care. 2013;3:224–226. [Google Scholar]
- 31.Albin M.S., Ritter R.R., Pruett C.E., Kalff K. Venous air embolism during lumbar laminectomy in the prone position: report of three cases. Anesth Analg. 1991;73:346–349. doi: 10.1213/00000539-199109000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Chen H.-L., Wong C.-S., Ho S.-T., Chang F.-L., Hsu C.-H., Wu C.-T. A lethal pulmonary embolism during percutaneous vertebroplasty. Anesth Analg. 2002;95:1060–1062. doi: 10.1097/00000539-200210000-00049. table of contents. [DOI] [PubMed] [Google Scholar]
- 33.Dumont T.M., Stockwell D.W., Horgan M.A. Venous air embolism: an unusual complication of atlantoaxial arthrodesis: case report. Spine. 2010;35:E1238–E1240. doi: 10.1097/BRS.0b013e3181f62600. [DOI] [PubMed] [Google Scholar]
- 34.Ewah B., Calder I. Intraoperative death during lumbar discectomy. Br J Anaesth. 1991;66:721–723. doi: 10.1093/bja/66.6.721. [DOI] [PubMed] [Google Scholar]
- 35.Miyakoshi N., Hongo M., Kasukawa Y., Ishikawa Y., Kudo D., Shimada Y. Intraoperative Visible Air Bubbling Recorded as a Sign of Massive Venous Air Embolism During Prone Position Surgery for Extensive Ossification of Spinal Ligaments: A Case Report with a Video Clip. World Neurosurg Elsevier. 2019;131:38–42. doi: 10.1016/j.wneu.2019.07.166. [DOI] [PubMed] [Google Scholar]
- 36.Pan Y., Qiu B., Yu F., Hu B. Fatal air embolism during endoscopic retrograde cholangio-pancreatography (ERCP): a case report. J Med Colleges PLA. 2012 [Google Scholar]
- 37.Pinheiro L.C., Carmona B.M., Fascio M. de N.C., Souza I.S. de, Azevedo R.A.A. de, Barbosa F.T. Cardiac arrest after epidural anesthesia for a esthetic plastic surgery: a case report. Rev Bras Anestesiol Sociedade Brasileira de Anestesiologia. 2017;67:544–547. doi: 10.1016/j.bjan.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Kelleher A., Mackersie A. Cardiac arrest and resuscitation of a 6-month old achondroplastic baby undergoing neurosurgery in the prone position. Anaesthesia. 1995 doi: 10.1111/j.1365-2044.1995.tb04615.x. [DOI] [PubMed] [Google Scholar]
- 39.Lee-Archer P.F., Chaseling B. Air Embolism During Posterior Spinal Fusion in a 10-Year-Old Girl: A Case Report. A A Case Rep. 2017;8:307–309. doi: 10.1213/XAA.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 40.Mayorga-Buiza M.J., Rivero-Garvia M., Gomez-Gonzalez E., Marquez-Rivas J. Cardiac pulmonary resuscitation in prone position. The best option for posterior fossa neurosurgical patients. Paediatr Anaesth. 2018;28:746–747. doi: 10.1111/pan.13448. [DOI] [PubMed] [Google Scholar]
- 41.Reid J.M., Appleton P.J. A case of ventricular fibrillation in the prone position during back stabilisation surgery in a boy with Duchenne’s muscular dystrophy. Anaesthesia. 1999;54:364–367. doi: 10.1046/j.1365-2044.1999.00835.x. [DOI] [PubMed] [Google Scholar]
- 42.Tobias J.D., Mencio G.A., Atwood R., Gurwitz G.S. Intraoperative cardiopulmonary resuscitation in the prone position. J Pediatric Surgery. 1994 doi: 10.1016/0022-3468(94)90208-9. [DOI] [PubMed] [Google Scholar]
- 43.Sutherland R.W., Winter R.J. Two cases of fatal air embolism in children undergoing scoliosis surgery. Acta Anaesthesiol Scand. 1997;41:1073–1076. doi: 10.1111/j.1399-6576.1997.tb04839.x. [DOI] [PubMed] [Google Scholar]
- 44.Burki A.M., Mahboob S., Fatima T. CPR in prone position during neurosurgery. Anaesth Pain & Intensive Care. 2017;21:275–278. [Google Scholar]
- 45.Kaloria N, Bhagat H, Singla N, Luthra A. Venous air embolism during removal of bony spur in a child of split cord malformation: A case report. 18th Annual Conference of Indian Society of Neuroanaesthesiology and Critical Care (ISNACC 2017). Thieme Medical and Scientific Publishers Private Ltd.; 2018.
- 46.Gueugniaud P.-Y., Muchada R., Bertin-Maghit M., Griffith N., Petit P. Non-invasive continuous haemodynamic andPetCO2 monitoring during peroperative cardiac arrest. Can J Anaesthesia. 1995 doi: 10.1007/BF03011039. [DOI] [PubMed] [Google Scholar]
- 47.Smelt W.L.H. Cardiac arrest during desflurane anaesthesia in a patient with Duchenne’s muscular dystrophy. Acta Anaesthesiol Scand. 2005;49:267–269. doi: 10.1111/j.1399-6576.2004.00596.x. [DOI] [PubMed] [Google Scholar]
- 48.Tofil N.M., Dollar J., Zinkan L., et al. Performance of anesthesia residents during a simulated prone ventricular fibrillation arrest in an anesthetized pediatric patient. Paediatr Anaesth. 2014;24:940–944. doi: 10.1111/pan.12406. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.