Abstract
Objectives
To compare the effects of early surgery (within 24 h) and delayed surgery on the outcomes of patients with acute cervical/thoracic spinal cord injury (SCI) in Beijing, China.
Methods
We conducted a clinical trial involving patients who were aged 16–85 years, had acute SCI from 1 June 2016 to 1 June 2019 in Beijing. The enrolled patients were divided into two groups according to the timing of surgical decompression. The primary outcome was the ordinal change in the American Spinal Injury Association Impairment Scale (AIS) grade. The secondary outcomes included the surgical time, volume of surgical bleeding, rate of admission to the intensive care unit (ICU), length of stay in the ICU, duration of mechanical ventilation, length of hospital stay, and postoperative complications. And the time consumption of different phases before operation was recorded for the patients transported to hospital by ambulance.
Results
A total of 148 patients were included in the study, including 55 in the early surgery group and 93 in the delayed surgery group. At 52 weeks post‐surgery, 27.3% of the patients in the early surgery group showed AIS improvement by at least two grades, compared to 8.7% of the patients in the delayed surgery group (P = 0.102). According to the logistic regression analysis, the odds of at least a two‐grade AIS improvement was six times higher among the patients who underwent early surgery than among those who underwent delayed surgery (OR = 6.66, 95%CI 1.14–38.84). The delay surgery group consumed significantly more time in the phases of transfer and inspection or examination than the early surgery group, and the Chinese regional trauma treatment system was widely used in the early surgery group.
Conclusion
Decompression within 24 h after SCI can improve patients' recovery of neurological function without increasing the incidence of postoperative complications and surgical risks. The Chinese regional trauma treatment system can improve the diagnosis and treatment efficiency of patients with acute SCI and speed up the operation timing.
Keywords: Prognosis, Spinal cord injury, Surgery, Time to treatment, Trauma treatment system
Decompression within 24 h after SCI can improve patients' recovery of neurological function without increasing the incidence of postoperative complications and surgical risks. The Chinese regional trauma treatment system can improve the diagnosis and treatment efficiency of patients with acute spinal cord injury and speed up the operation timing.
Introduction
Acute traumatic spinal cord injury (SCI) is a severe disease that affects individuals worldwide and is associated with a high rate of disability and mortality, leading to a heavy burden on individuals and society 1 , 2 . The incidence of acute SCI is 30–40 per million people in Europe and the United States, but it is 60.2 per million people in Beijing, China 3 , 4 , 5 . The average age of affected individuals is 33–41 years 4 , 5 , which means that most patients are young and middle‐aged. Surgical decompression and stabilization are still important procedures for patients with acute SCI 6 . However, the optimal timing for surgery remains controversial.
A number of studies have concluded that early surgical decompression can improve neurological outcomes 7 , 8 , 9 , 10 , 11 . The results of the latest meta‐analysis also suggest that early surgery (within 24 h) is beneficial for the prognosis of patients with acute SCI 12 . The theoretical reasoning for early surgery is derived from the pathophysiology, specifically the primary and secondary mechanisms, of acute SCI. The primary injury caused by rapid spinal cord compression and contusion initiates a signaling cascade of downstream events collectively known as secondary injuries 13 , 14 . Laboratory experiments and preclinical studies show that decompression after injury can effectively reduce secondary injuries 15 , 16 , and the strength of this neuroprotective effect is inversely correlated with time 17 , 18 . Many clinical studies have shown that compared with delayed surgery, early surgery (within 24 h) can yield better neurological prognoses and reduce the length of hospital stay and the medical burden. However, the differences shown in most studies are not statistically significant, and these studies have a relatively small sample size, so the results may be not generalizable to the broader population 7 , 8 , 9 , 10 , 11 , 19 .
No official clinical studies have been conducted in China to verify the effects of early surgery on the outcomes of patients with acute SCI. The important reason is that there is no effective trauma treatment system in China, which could guarantee that patients with acute spinal cord injury can receive surgical treatment within 24 h. But the Chinese regional trauma treatment system proposed by Jiang made it easier for the implementation of early surgery 20 , 21 .
Therefore, this is the first clinical trial on acute SCI in China, and we aimed to compare the effects of early surgery with those of delayed surgery on the outcomes of patients with acute SCI, including the ordinal change in the AIS grade, surgical time, volume of surgical bleeding, rate of admission to the ICU, length of stay in the ICU, duration of mechanical ventilation, length of hospital stay, and postoperative complications. Meanwhile, the factors leading to the delay of surgical treatment were analyzed.
Methods
Study Population
We conducted a prospective, multicenter nonrandomized controlled trial involving five hospitals in Beijing: (i) Peking University People's Hospital, (ii) Peking University Third Hospital, (iii) Beijing Friendship Hospital Affiliated to Capital Medical University, (iv) Chaoyang Hospital Affiliated to Capital Medical University, and (v) Chinese People's Liberation Army (PLA) General Hospital. All the hospitals recorded patients' information in a database specifically created for SCI cases. Prior to the start of the study, the protocol involving all five hospitals was approved by the Medical Ethics Committee of Peking University People's Hospital, China (approval number: 2016PHB136‐01). We enrolled patients with acute SCI hospitalized from 1 June 2016 to 1 June 2019. All patients were required to complete a medical history and undergo a physical examination and magnetic resonance imaging (MRI) scan so that the diagnosis of acute SCI could be confirmed. All patients enrolled in the study were required to meet the established inclusion and exclusion criteria strictly (Table 1). All patients signed informed consent forms before being enrolled.
TABLE 1.
Inclusion/exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| 1.Spinal cord injury patients will be evaluated as complete or incomplete (contusion) after admission using rectal examination, in accordance with American Spinal Injury Association and International Medical Society of Paraplegia (2000) | 1.Active or recent severe infection |
| 2.Final diagnosis by spine computed tomography (CT) and/or magnetic resonance imaging (MRI) | 2.Severe infectious diseases that need to be treated in infectious disease hospital |
| 3.Cervical, thoracic, and thoracolumbar fracture dislocation or without fracture dislocation but combined with spinal cord injury | 3.History of mental illness |
| 4.No other injury involving life, injury severity score < 16 29 | 4.History of metal allergy |
| 5.No anesthesia contraindication | 5.Long‐term alcohol abuse and drug abuse |
| 6.No local skin infection, no severe soft tissue contusion, soft tissue condition of the operation area met the operation requirements | 6.Do not agree to participate in this trial; the legal representative of the patient refuses to sign informed consent |
| 7.Age: 16–85 years old, irrespective of sex | 7.Poor compliance, cannot be followed up as required |
Grouping
The enrolled patients were divided into two groups according to the timing of surgical decompression. The early surgical cohort included patients who underwent surgery at or within 24 h postinjury, and the delayed surgical cohort consisted of patients who underwent surgery more than 24 h postinjury. The timing of the operation was determined by the time the patient arrived at the hospital after the injury, the time required for a diagnosis, and the preoperative evaluations and the discretion of the doctors in charge. Moreover, a professional orthopaedic surgeon conducted physical examinations to identify the patients' neurological level of injury, ASIA motion score (AMS), ASIA sensory score, and AIS grade. The time of admission, the time of the operation, the etiology, injury segments, age, sex, preoperative complications, and associated injuries were recorded in detail.
Surgery and Hospitalization
For the surgical approach used to treat the cases of cervical spine injury, the anterior, posterior, or combined anterior and posterior approach was selected on the basis of the displacement of the cervical spine injury, the damage to the structures and the location of spinal cord compression. For thoracic SCI, posterior decompression and internal fixation were performed. After the operation, mechanical ventilation was administered, and the patient was transferred to the ICU if necessary, according to the patient's state. The surgical time, volume of surgical bleeding, rate of admission to the ICU, length of ICU stay, and duration of mechanical ventilation were recorded. After discharge, all patients were transferred to the rehabilitation hospital to undergo personalized rehabilitation programs and take neurotrophic drugs. Methylprednisolone was administered as per the discretion of the treating team according to the recommendations of the NASCIS‐2 study 22 .
Follow‐Ups and Outcomes of Interest
All patients were followed up after the initial admission. The follow‐up time points included 6 weeks post‐surgery, 12 weeks post‐surgery, and 52 weeks post‐surgery. The primary outcome was the ordinal change in the AIS grade. The secondary outcomes included the surgical time, volume of surgical bleeding, rate of admission to the ICU, length of ICU stay, duration of mechanical ventilation, length of hospital stay, and postoperative complications. And the elapsed time of patients transported to hospital by ambulance at different phases was recorded, including the transfer, inspection or examination and the others. Whether the Chinese trauma treatment systems is used or not will also be recorded.
American Spinal Injury Association Impairment Scale (AIS) Grade (Updated 2015)
The AIS is the international gold standard for evaluation of spinal cord injuries 23 . The AIS is a standardized examination consisting of a myotomal‐based motor examination, dermatomal‐based sensory examination, and an anorectal examination. The AIS further classifies injuries as a complete or incomplete spinal cord injury. A complete spinal cord injury is defined as the absence of all motor and sensory functions, including sacral roots, distal to the site of injury. These injuries are designated as being Grade A on the AIS. Incomplete injuries are defined as those with some degree of retained motor or sensory function below the site of injury. Patients with AIS Grade B injuries have some sensory function but no motor function. AIS Grade C injuries have a motor grade less than 3 below the neurologic level of injury while AIS Grade D injuries have a motor grade of at least 3 below the neurologic level of injury. Patients with Grade E injuries have normal motor and sensory examinations, but still may have abnormal reflexes or other neurologic phenomena.
Surgical Time (Hours)
The surgical time was from the time the skin was cut through to the time the wound was closed at the end of the operation.
Volume of Surgical Bleeding (Milliliter)
Volume of surgical bleeding was defined as intraoperative blood loss, as the amount of fluid in the aspirator minus the amount of rinsed water.
Rate of Admission to the ICU (n%)
The rate of admission to the ICU was the proportion of patients admitted to the ICU immediately after surgery.
Length of ICU Stay (Hours)
Length of ICU stay was defined as the period of confinement of a patient to the ICU.
Duration of Mechanical Ventilation (Hours)
Duration of mechanical ventilation referred to the time that the patient needs to use mechanical ventilation after surgery due to medical factors.
Length of Hospital Stay (Days)
Length of hospital stay was defined as the period of confinement of a patient to the hospital.
Postoperative Complications (n%)
Postoperative complications were defined as the pathologic processes that affect patients after surgery, including infection, cardiovascular complication, poor wound healing, and so on.
Elapsed Time of Patients Transported to Hospital by Ambulance at Different Phases
The transfer phase referred to the time between the patient's call to the ambulance and the patient's arrival at the hospital. The inspection or examination phase was defined as the physical examination and ancillary examination that must be completed prior to surgery.
Statistical Analysis
All analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBMCorp., Armonk, N.Y., USA). The chi‐square test and Fisher exact test were used to compare the differences in sex, etiology, preoperative AIS grade, change in the AIS grade, preoperative complications, associated injuries, rate of admission to the ICU, and postoperative complications between the two groups. The T‐test was used to compare the differences in age, surgical time, volume of surgical bleeding, length of ICU stay, duration of mechanical ventilation, length of hospital stay, and the elapsed time at different phases between the two groups. We performed a generalized binary logistic regression analysis that was adjusted for the confounding variables. The alpha level was set to P < 0.05.
Results
Patients and Characteristics
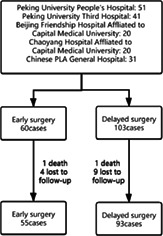
A total of 163 patients who had acute SCI and were hospitalized were enrolled, including 60 patients in the early operation group and 103 patients in the delayed operation group, and the final follow‐up time was 52 weeks. Two patients died and 13 patients were lost to follow‐up. In the end, there were 55 patients in the early group and 93 patients in the delayed group (Fig. 1).
Fig. 1.
Patient flow
The demographic and injury characteristics of the patients finally included in the early group and delayed group are shown in Table 2. The mean time to surgery was 13.7 h in the early group and 181.8 h in the delayed group. In the early surgery group, 72.7% of the patients were male and 27.3% were female, with an average age of 50.3 ± 13.3 years. In the delayed surgery group, 72% of the patients were male and 28% were female, with an average age of 55.6 ± 13.1 years. There was no difference in sex between the two groups, but the delayed group was 5.25 (95% CI 0.83–9.67) years older than the early group, which was significant. The most common etiology of SCI in the early group was a traffic accident (38.2%), and the most common etiology of SCI in the delayed group was a fall (35.5%). The incidence of preoperative complications and associated injuries was significantly higher in the early group than in the delayed group (10.9% vs 1.1%, P = 0.01; 43.6% vs 17.2%, P < 0.01, respectively). In terms of the preoperative AIS grade, the proportion of patients who were classified as Grade A was significantly higher in the early surgery group than in the delayed surgery group (32.7% vs 7.5%, P < 0.01), while the proportion of patients who were classified as Grade D was significantly lower in the early surgery group than in the delayed surgery group (40.0% vs 72.3%, P < 0.01). The injury segments of the two groups were mainly cervical vertebrae.
TABLE 2.
Patient demographics and injury characteristics
| The overall (N = 148) | Early surgery (N = 55) | Delayed surgery (N = 93) | P‐value | |
|---|---|---|---|---|
| Time to surgery (mean ± SD) | 119.3 ± 175.7 | 13.7 ± 7.2 | 181.8 ± 182.3 | |
| Age (years) | 53.6 ± 13.3 | 50.3 ± 13.3 | 55.6 ± 13.1 | 0.020 |
| Sex n (%) | 1.000 | |||
| Male | 107 (72.3%) | 40 (72.7%) | 67 (72.0%) | |
| Female | 41 (27.7%) | 15 (27.3%) | 26 (28.0%) | |
| Etiology | 0.046 | |||
| Slip | 25 (16.9%) | 6 (10.9%) | 19 (20.4%) | |
| Fall | 21 (14.2%) | 12 (21.8%) | 9 (9.7%) | |
| Tumble | 46 (31.1%) | 13 (23.6%) | 33 (35.5%) | |
| Traffic accident | 45 (30.4%) | 21 (38.2%) | 24 (25.8%) | |
| Crushed | 1 (0.7%) | 1 (1.8%) | 0 (0.0%) | |
| Assault | 4 (2.7%) | 0 (0.0%) | 4 (4.3%) | |
| Other | 6 (4.1%) | 2 (3.6%) | 4 (4.3%) | |
| Baseline AIS | <0.001 | |||
| A | 25 (16.9%) | 18 (32.7%) | 7 (7.5%) | |
| B | 3 (2%) | 2 (3.6%) | 1 (1.1%) | |
| C | 28 (18.9%) | 13 (23.6%) | 15 (16.1%) | |
| D | 92 (62.2%) | 22 (40.0%) | 70 (72.3%) | |
| Pre‐op complications | 7 (4.7%) | 6 (10.9%) | 1 (1.1%) | 0.011 |
| Associated injury | 40 (27.0%) | 24 (43.6%) | 16 (17.2%) | 0.001 |
| Injury segments | 0.053 | |||
| C | 119 (80.4%) | 40 (72.7%) | 79 (84.9%) | |
| T | 29 (19.6%) | 15 (27.3%) | 14 (15.1%) | |
| Surgical time (hours) | 2.7 ± 1.1 | 3 ± 1.3 | 2.5 ± 0.8 | 0.006 |
| Surgical bleeding (ml) | 309.9 ± 429 | 436.7 ± 403.0 | 234.8 ± 428.3 | 0.005 |
| Admission to ICU | 49 (33.1%) | 37 (67.3%) | 12 (12.9%) | <0.001 |
| length of ICU stay (hours) | 193.2 ± 665.8 | 217.6 ± 762.8 | 118.3 ± 148.6 | 0.658 |
| Mechanical ventilation time (hours) | 100.8 ± 199.5 | 92.2 ± 166.2 | 127.3 ± 286.7 | 0.601 |
| Length of hospital stay (days) | 14.6 ± 10.8 | 16.4 ± 11.9 | 13.6 ± 10.0 | 0.119 |
| Complications | 4 (2.7%) | 2 (3.6%) | 2 (2.2%) | 0.628 |
Abbreviations: AIS, ASIA impairment scale; ICU, the intensive care unit.
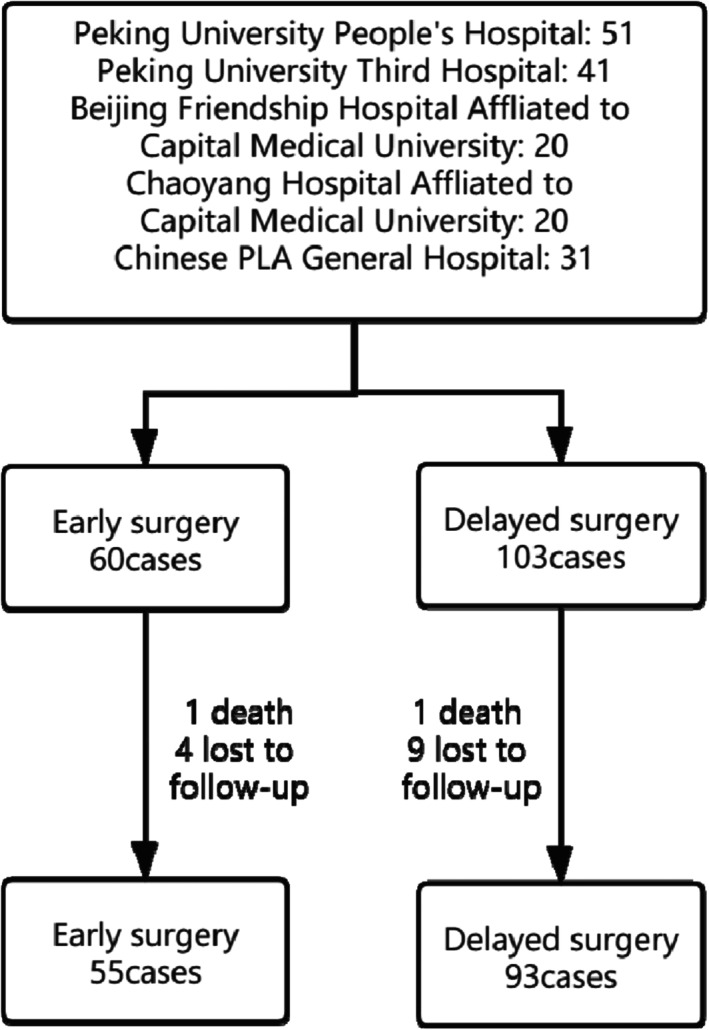
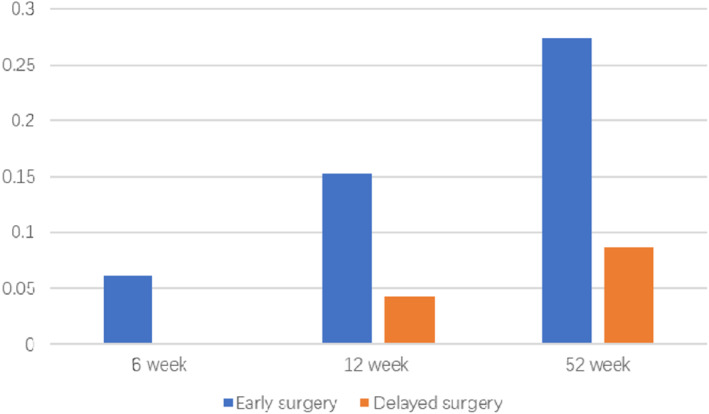
Ordinal Change in the AIS Grade
The variation in the AIS grade among the follow‐up time points is shown in Table 3. At 6 weeks post‐surgery, two (6.1%) cases in the early surgery group and zero (0%) cases in the delayed surgery group improved by at least two AIS grades (P = 0.51). At 12 weeks post‐surgery, five (15.2%) cases in the early surgery group and one (4.3%) case in the delayed surgery group improved by at least two AIS grades (P = 0.38). At 52 weeks post‐surgery, nine (27.3%) cases in the early surgery group and two (8.7%) cases in the delayed surgery group improved by at least two AIS grades (P = 0.10) (Fig. 2). Since Grade D patients could not improve by two AIS grades, we conducted a subgroup analysis of these patients (Fig. 3). At 6 weeks post‐surgery, six (27.3%) cases in the early surgery group and 22 (31.4%) cases in the delayed surgery group improved by one AIS grade (P = 0.71). At 12 weeks post‐surgery, 12 (54.5%) cases in the early surgery group and 39 (55.7%) cases in the delayed surgery group improved by one AIS grade (P = 0.92). At 52 weeks post‐surgery, 18 (81.8%) cases in the early surgery group and 51 (72.9%) cases in the delayed surgery group improved by one AIS grade (P = 0.40).
TABLE 3.
Variation of AIS grade at 6, 12, 52 weeks (the overall, the early surgery, the delayed surgery)
| Preoperative AIS grade | A | B | C | D | E | Total | |
|---|---|---|---|---|---|---|---|
| 6 weeks | |||||||
| The overall | A | 19 | 4 | 2 | 0 | 0 | 25 |
| B | 0 | 0 | 3 | 0 | 0 | 3 | |
| C | 0 | 0 | 6 | 22 | 0 | 28 | |
| D | 0 | 0 | 0 | 64 | 28 | 92 | |
| The early surgery | A | 14 | 2 | 2 | 0 | 0 | 18 |
| B | 0 | 0 | 2 | 0 | 0 | 2 | |
| C | 0 | 0 | 3 | 10 | 0 | 13 | |
| D | 0 | 0 | 0 | 16 | 6 | 22 | |
| The delayed surgery | A | 5 | 2 | 0 | 0 | 0 | 7 |
| B | 0 | 0 | 1 | 0 | 0 | 1 | |
| C | 0 | 0 | 3 | 12 | 0 | 15 | |
| D | 0 | 0 | 0 | 48 | 22 | 70 | |
| 12 weeks | |||||||
| The overall | A | 19 | 3 | 2 | 1 | 0 | 25 |
| B | 0 | 0 | 3 | 0 | 0 | 3 | |
| C | 0 | 0 | 5 | 20 | 3 | 28 | |
| D | 0 | 0 | 0 | 41 | 51 | 92 | |
| The early surgery | A | 14 | 1 | 2 | 1 | 0 | 18 |
| B | 0 | 0 | 2 | 0 | 0 | 2 | |
| C | 0 | 0 | 3 | 8 | 2 | 13 | |
| D | 0 | 0 | 0 | 10 | 12 | 22 | |
| The delayed surgery | A | 5 | 2 | 0 | 0 | 0 | 7 |
| B | 0 | 0 | 1 | 0 | 0 | 1 | |
| C | 0 | 0 | 2 | 12 | 1 | 15 | |
| D | 0 | 0 | 0 | 31 | 39 | 70 | |
| 52 weeks | |||||||
| The overall | A | 19 | 3 | 2 | 1 | 0 | 25 |
| B | 0 | 0 | 2 | 1 | 0 | 3 | |
| C | 0 | 0 | 4 | 17 | 7 | 28 | |
| D | 0 | 0 | 0 | 23 | 69 | 92 | |
| The early surgery | A | 14 | 1 | 2 | 1 | 0 | 18 |
| B | 0 | 0 | 1 | 1 | 0 | 2 | |
| C | 0 | 0 | 2 | 6 | 5 | 13 | |
| D | 0 | 0 | 0 | 4 | 18 | 22 | |
| The delayed surgery | A | 5 | 2 | 0 | 0 | 0 | 7 |
| B | 0 | 0 | 1 | 0 | 0 | 1 | |
| C | 0 | 0 | 2 | 11 | 2 | 15 | |
| D | 0 | 0 | 0 | 19 | 51 | 70 |
Abbreviations: AIS, ASIA impairment scale.
Fig. 2.
Improved by at least two AIS grades (for patients with preoperative A, B, or C grade)
Fig. 3.
AIS improved by one grade in the patients with preoperative D grade
In the binary logistic regression analysis, after the model was adjusted for preoperative complications, preoperative associated injuries, and AIS grades, the odds of at least a one‐grade AIS improvement were 2.283 (95%CI 0.79–6.58, P = 0.127) times higher among the patients who underwent early surgery than among those who underwent delayed surgery without statistical significance, and the odds of at least a two‐grade AIS improvement were 6.66 (95%CI 1.14–38.84, P = 0.035) times higher among those who underwent early surgery (table 4).
TABLE 4.
Results of binary logistic regression model assessing the effect of early vs late surgical decompression, adjusted for preoperative complications, preoperative associated injury, and AIS grades
| Odds ratio with 95% CI | P‐value | |
|---|---|---|
|
Early vs Late surgery ≥1 grades AIS improvement |
2.283 (95%CI 0.79–6.58) | 0.127 |
|
Early vs Late surgery ≥2 grades AIS improvement |
6.66 (95%CI 1.14–38.84) | 0.035 |
Abbreviations: AIS, ASIA impairment scale.
General Results
Compared to the delayed surgery group, the early surgery group had a significant 0.49 h (95% CI 0.15–0.84) longer surgical time, a significant 201.89 mL (95%CI 61.00–342.79) larger volume of surgical bleeding, and a significantly higher proportion of patients who were admitted to the ICU (67.3% vs 12.9%, P < 0.01). However, there was no difference in the length of ICU stay or duration of mechanical ventilation. There was no significant difference in the length of hospital stay between the early surgery group and the delayed surgery group.
Distribution of Elapsed Time (Hours)
The elapsed time of patients transported to hospital by ambulance at different phases is shown in Table 5. The delay surgery group consumed significantly more time in the phases of transfer (8.50 vs 4.47, P < 0.01) and inspection or examination (36.3 vs 5.2, P < 0.01) than the early surgery group. And the Chinese regional trauma treatment system was more widely used in the early surgery group than the delayed surgery group (46.5% vs 10.0%, P < 0.01).
TABLE 5.
The elapsed time of patients transported to hospital by ambulance at different phases (hours)
| Transfer | Inspection or examination | Other | Total | The use of Chinese RTTS | |
|---|---|---|---|---|---|
| Early surgery (n = 43) | 4.47 | 5.2 | 4.1 | 14.1 | 20 (46.5%) |
| Delayed surgery (n = 30) | 8.50 | 36.3 | 32 | 76.6 | 3 (10.0%) |
| P‐value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Abbreviations: RTTS, regional trauma treatment system.
Postoperative Complications
The incidence of postoperative complications was 3.6% in the early operation group and 2.2% in the delayed operation group, which was not significantly different, and all of the complications were pulmonary infections. All the complications were cured after systematic treatment.
Discussion
We successfully conducted a prospective, multicenter nonrandomized controlled trial on the effects of early surgery on the outcomes of patients with acute SCI. A total of 148 patients with acute SCI were included eventually, with a loss to follow‐up rate of 9.2%. Compared with other similar studies 7 , 8 , 9 , 10 , 11 , 19 , 24 , our study had a larger sample size, a lower missing rate, and relatively more comprehensive statistical records.
Controversial Optional Timing
The hypothesis that early surgery may be beneficial for patients with acute SCI is based on the pathophysiology of acute SCI and laboratory evidence 7 . The pathophysiology of acute SCI is considered to include primary and secondary mechanisms 13 , 14 . Animal experiments and preclinical studies have shown that decompression after injury can effectively reduce secondary injuries, and the strength of this neuroprotective effect is inversely correlated with time 15 , 16 , 17 , 18 . However, in animal models, the time between surgery and injury is usually less than 8 h 25 , which is inconsistent with that in clinical practice. The time between surgery and injury is delayed by the transit time, preoperative examination time, and other processes. Therefore, the exact timing of early surgery in clinical practice is quite controversial, and early surgery is mainly defined as surgery performed within 24 or 72 h after injury 26 , 27 . However, an increasing number of large studies 7 , 8 , 9 , 10 , 11 , 19 , 24 used 24 h as the threshold for early surgery. The results of the latest meta‐analysis 12 suggest that there are differences between patients who undergo surgery within 24 h or more than 24 h after injury in neurological functional recovery, postoperative complications, and the length of hospital stay. There are also clinical studies that have defined 8 h as the threshold for early surgery 28 , but it is usually difficult to perform surgery within 8 h in our clinical practice. Therefore, we chose 24 h as the early surgery threshold.
Acute SCI is often an emergency, and the patients included in the study were grouped by objective criteria. Therefore, the demographic and injury characteristics of the two groups in this study were significantly different. The most common etiology of SCI in the patients in the early group was a traffic accident, while it was a fall in the delayed group. The AIS grade of the early group was significantly lower than that of the delayed group, and the incidence of complications and associated injuries of the early group was significantly higher than that of the delayed group. Since the etiology of SCI was mainly a fall in the delayed surgery group, the patients had relatively minor injuries, there were few associated injuries and complications, and the AIS grade was relatively good. Thus, these patients did not go to the hospital in a timely manner and they could only be included in the delayed operation group.
Ordinal Change in the AIS Grade
In terms of AIS grade improvement, the AIS grade improved by at least one grade in more patients in the delayed surgery group than in the early surgery group among the follow‐up time points, but the difference between groups was not significant. However, considering the differences in injury characteristics between the two groups, this slight difference between groups does not indicate an advantage of delayed surgery. Since Grade D patients could not improve by two AIS grades, we conducted a subgroup analysis of these patients. At 52 weeks, the primary outcome of the early group was superior to that of the delayed group, but the difference was not statistically significant. In terms of AIS grade improvement, the AIS grade improved by at least two grades in more patients in the early surgery group than in the delayed surgery group among the follow‐up time points. Although the differences were not statistically significant, they were obvious. And in the binary logistic regression analysis, the odds of at least a two‐grade AIS improvement were 6.66 (95%CI 1.14–38.84, P = 0.035) times higher among those who underwent early surgery. Taking the differences in injury characteristics between the two groups into account, we believe that early surgery can help patients recover more quickly with better outcomes.
Wilson et al. 8 enrolled 55 patients with acute SCI, and the average follow‐up time was 89.6 days. A total of 40.9% of the patients in the early surgery group and 30.3% in the delayed surgery group showed AIS grade improvement by at least one grade, 27.2% in early surgery group and 3% in delayed surgery group showed improvement by at least two grades. The Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) 7 , a multicenter, international cohort study, concluded that the odds of AIS grade improvement by at least two grades was 2.8 times higher in the early group than in the delayed surgery group, with a loss to follow‐up rate of 27% at 6 months post‐surgery. Muhammad et al. 10 enrolled 98 patients with acute SCI, and the average follow‐up time was 6 months. A total of 23.3% of the patients in the early surgery group and 8.7% in the delayed surgery group showed improvement by at least two grades. This finding is consistent with our findings, which showed that early surgery is associated with better neurologic outcomes, as defined by at least a two‐grade AIS improvement.
General Indicator
In terms of the volume of surgical bleeding, surgical time, and rate of admission to the ICU, our results suggest that early surgery is worse than delayed surgery, which may be because early surgery is performed in the acute stage of injury when the condition of the patient is poor. Etienne et al. 24 concluded that the incidence of postoperative complications of the patients who underwent surgery within 24 h postinjury was much lower than that of the patients who underwent surgery more than 24 h postinjury. Our data suggest that the incidence of postoperative complications in the early group is lower than that in the delayed group, without a statistically significant difference.
In terms of medical burden, our data suggest that the mean lengths of ICU stay and hospital stay in the early group were slightly longer. This result was not consistent with the results of other studies. Dvorak et al. 11 and Mac‐Thiong et al. 19 suggest that resource utilization in terms of costs and the length of hospital stay is decreased with early surgery compared with delayed surgery after acute SCI. The inconsistency can be explained by the fact that the patients in the early surgery group in our study had more preoperative complications and associated injuries and worse conditions.
Regional Trauma Treatment System
The delay surgery group consumed significantly more time in the phases of transfer and inspection or examination than the early surgery group. In the early surgery group, 20 (46.5%) cases used the Chinese regional trauma treatment system, which was significantly higher than three (10%) cases in the delayed surgery group. The Chinese regional trauma treatment system can coordinate the pre‐hospital transport and in‐hospital medical resources, and the establishment of a mature trauma treatment system can improve the first aid awareness of medical staff, so that the transport and treatment efficiency of patients with acute SCI can be improved significantly 20 , 21 .
Limitations
Our study has many inherent limitations. The first limitation is the difference in the study populations from the five hospitals, which may affect the timing of surgery, postoperative nursing care, and the length of hospital stay. Furthermore, it is obvious that the differences in the demographic and injury characteristics between the two groups are large. The early surgery group had a lower AIS grade, more complications, and more associated injuries. Third, due to the complicated Chinese medical payment system, we excluded medical expenses in our research content.
Conclusion
Based on our results, we can conclude that for patients with acute SCI, surgical decompression performed at or before 24 h postinjury has the potential to result in superior neurological recovery compared with that of delayed surgery performed more than 24 h postinjury, without increases in the complication rate, medical burden, or risks of surgery. However, we still need to conduct studies with larger sample sizes, more detailed subgroup analyses, and more rigorous study designs to account for the demographic and injury differences caused by the use of objective criteria to group patients. The Chinese regional trauma treatment system can improve the diagnosis and treatment efficiency of patients with acute spinal cord injury and speed up the operation timing.
Authors' contributions
Baoguo Jiang and Dianying Zhang contributed to study design. Feng Xue and Sizheng Zhan contributed to study conception, data gathering, data interpretation, and article writing.
Authorship declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Statement of Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. The study protocol has been approved by the Medical Ethics Committee of Peking University People's Hospital, China (approval number: 2016PHB136‐01).
Acknowledgments
We are very grateful to HuiXin Liu for her help in data statistics.
Grant Sources: This study was supported by the Beijing Science and Technology Plan Project in China, No. D161100002816001 and Instituteof Trauma and Nerve Regeneration.
Disclosure: All authors declare that they have no conflict of interest.
References
- 1. Singh A, Tetreault L, Kalsi‐Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol, 2014, 6: 309–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci, 2013, 40: 456–464. [DOI] [PubMed] [Google Scholar]
- 3. Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord, 2014, 52: 110–116. [DOI] [PubMed] [Google Scholar]
- 4. Li J, Liu G, Zheng Y, et al. The epidemiological survey of acute traumatic spinal cord injury (ATSCI) of 2002 in Beijing municipality. Spinal Cord, 2011, 49: 777–782. [DOI] [PubMed] [Google Scholar]
- 5. Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey?. Spinal Cord, 2006, 44: 523–529. [DOI] [PubMed] [Google Scholar]
- 6. Fisher CG, Noonan VK, Dvorak MF. Changing face of spine trauma care in North America. Spine (Phila Pa 1976), 2006, 31: S2–S8; discussion S36. [DOI] [PubMed] [Google Scholar]
- 7. Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS One, 2012, 7: e32037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wilson JR, Singh A, Craven C, et al. Early versus late surgery for traumatic spinal cord injury: the results of a prospective Canadian cohort study. Spinal Cord, 2012, 50: 840–843. [DOI] [PubMed] [Google Scholar]
- 9. Rahimi‐Movaghar V, Niakan A, Haghnegahdar A, Shahlaee A, Saadat S, Barzideh E. Early versus late surgical decompression for traumatic thoracic/thoracolumbar (T1‐L1) spinal cord injured patients. Primary results of a randomized controlled trial at one year follow‐up. Neurosciences (Riyadh), 2014, 19: 183–191. [PMC free article] [PubMed] [Google Scholar]
- 10. Umerani MS, Abbas A, Sharif S. Clinical outcome in patients with early versus delayed decompression in cervical spine trauma. Asian Spine J, 2014, 8: 427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dvorak MF, Noonan VK, Fallah N, et al. The influence of time from injury to surgery on motor recovery and length of hospital stay in acute traumatic spinal cord injury: an observational Canadian cohort study. J Neurotrauma, 2015, 32: 645–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu JM, Long XH, Zhou Y, Peng HW, Liu ZL, Huang SH. Is urgent decompression superior to delayed surgery for traumatic spinal cord injury? A meta‐analysis. World Neurosurg, 2016, 87: 124–131. [DOI] [PubMed] [Google Scholar]
- 13. Amar AP, Levy ML. Pathogenesis and pharmacological strategies for mitigating secondary damage in acute spinal cord injury. Neurosurgery, 1999, 44: 1027–1039 discussion 39‐40. [DOI] [PubMed] [Google Scholar]
- 14. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg, 1991, 75: 15–26. [DOI] [PubMed] [Google Scholar]
- 15. Dolan EJ, Tator CH, Endrenyi L. The value of decompression for acute experimental spinal cord compression injury. J Neurosurg, 1980, 53: 749–755. [DOI] [PubMed] [Google Scholar]
- 16. Guha A, Tator CH, Endrenyi L, Piper I. Decompression of the spinal cord improves recovery after acute experimental spinal cord compression injury. Paraplegia, 1987, 25: 324–339. [DOI] [PubMed] [Google Scholar]
- 17. Carlson GD, Gorden CD, Oliff HS, Pillai JJ, LaManna JC. Sustained spinal cord compression: part I: time‐dependent effect on long‐term pathophysiology. J Bone Joint Surg Am, 2003, 85: 86–94. [PubMed] [Google Scholar]
- 18. Dimar JR, Glassman SD, Raque GH, Zhang YP, Shields CB. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976), 1999, 24: 1623–1633. [DOI] [PubMed] [Google Scholar]
- 19. Mac‐Thiong JM, Feldman DE, Thompson C, Bourassa‐Moreau E, Parent S. Does timing of surgery affect hospitalization costs and length of stay for acute care following a traumatic spinal cord injury? J Neurotrauma, 2012, 29: 2816–2822. [DOI] [PubMed] [Google Scholar]
- 20. Jiang B, Liang S, Peng Z‐R, et al. Transport and public health in China: the road to a healthy future. Lancet, 2017, 390: 1781–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang T, Jiang B. Road traffic mortality in China: good prospect and arduous undertaking. Lancet Public Health, 2019, 4: e214–e215. [DOI] [PubMed] [Google Scholar]
- 22. Bracken MB, Shepard MJ, Collins WF, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal‐cord injury. Results of the second national acute spinal cord injury study. N Engl J Med, 1990, 322: 1405–1411. [DOI] [PubMed] [Google Scholar]
- 23. Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American spinal injury association (ASIA) impairment scale. Clin Orthop Relat Res, 2017, 475: 1499–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bourassa‐Moreau E, Mac‐Thiong JM, Ehrmann Feldman D, Thompson C, Parent S. Complications in acute phase hospitalization of traumatic spinal cord injury: does surgical timing matter?. J Trauma Acute Care Surg, 2013, 74: 849–854. [DOI] [PubMed] [Google Scholar]
- 25. Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: an evidence‐based examination of pre‐clinical and clinical studies. J Neurotrauma, 2011, 28: 1371–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McKinley W, Meade MA, Kirshblum S, Barnard B. Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil, 2004, 85: 1818–1825. [DOI] [PubMed] [Google Scholar]
- 27. Vaccaro AR, Daugherty RJ, Sheehan TP, et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine (Phila Pa 1976), 1997, 22: 2609–2613. [DOI] [PubMed] [Google Scholar]
- 28. Jug M, Kejzar N, Vesel M, et al. Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma, 2015, 32: 1385–1392. [DOI] [PubMed] [Google Scholar]
- 29. Vaccaro AR, Zeiller SC, Hulbert RJ, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech, 2005, 18: 209–215. [PubMed] [Google Scholar]


