Abstract
Conventional wisdom often holds that the healthcare sector fares better than other sectors during economic downturns. However, little research has examined the relationship between local economic conditions and healthcare employment. Understanding how the healthcare sector responds to economic conditions is important for policymakers seeking to ensure an adequate supply of healthcare workers, as well as for those directing displaced workers into new jobs. We examine the impact of macroeconomic conditions on both the healthcare labor market and the pipeline of healthcare workers receiving healthcare degrees during 2005–2017 (the pre-COVID era). Our results indicate that the healthcare sector is stable across past business cycles. If anything, when areas experience more severe local economic downturns, healthcare employment increases. Much remains unknown about how the healthcare sector will fare during the current recession. Our study represents an important backdrop as policymakers consider ways to sustain the healthcare sector during current economic and public health turbulence.
Keywords: healthcare workforce, recession, healthcare education, employment, labor market
Highlights
-
What do we already know about this topic?
Healthcare as a sector continues to grow during times of economic contraction.
-
How does your research contribute to the field?
We document the relationship between the health of local economies and employment and education in the healthcare sector.
-
What are your research’s implications toward theory, policy or practice?
These results serve as a baseline for understanding how the broader economy impacts the healthcare labor market.
Introduction
The healthcare workforce comprised approximately 12% of all U.S. employment in 2018; jobs in healthcare grew almost 7 times faster than those in other sectors between 2006 and 2016.1,2 This growth has been attributed to increased healthcare utilization in the U.S following the Affordable Care Act, rapid expansions in healthcare technology, and individuals age 65 years and older making up an increasing share of the overall population.3–8 As older people often have chronic health conditions that necessitate additional health care, as investment in healthcare technology continues, and as the U.S faces public health crises,9,10 understanding the dynamics of the American healthcare workforce becomes increasingly important, in terms of both labor supply and the educational pipeline into the job market.
Several factors make the U.S. healthcare sector and its workforce unique. For one, health insurance pays for a large proportion of out-of-pocket healthcare cost, which makes patients less price sensitive, a feature that is uncommon in other sectors. 11 The healthcare labor market includes extensive licensing that protects healthcare tasks from being reallocated to other workers in response to cost pressures.12,13 Healthcare is also valued by many in society as a “merit good,” meaning that provision of healthcare to others may bring satisfaction to individuals not consuming the care themselves. 14
These factors raise the possibility that the healthcare workforce behaves differently across the business cycle: that the healthcare sector may enjoy some insulation from the factors that cause other sectors to experience expansions and contractions.15,16 For example, during the Great Recession, employment of Registered Nurses in the U.S. more than doubled employment projections. 17 It should be noted that this did not occur worldwide: there were many documented instances of healthcare workforce contractions in other economies, as well as instances of labor substitution toward less skilled forms of healthcare labor (ie, downskilling).18-20 This raises the question of how the healthcare workforce and its contributory educational pipeline react to changing local economic conditions in the U.S., and to what extent this sector does or does not follow the trajectory of the overall economy.
Ex ante, it is not clear whether or not employment in the healthcare sector would remain stable during economic downturns. As individuals’ ability to pay for healthcare depends partially on their income, falling personal financial resources during an economic downturn would be expected to reduce demand for healthcare and lead to decreases in healthcare employment. However, Medicare receipt does not depend on the business cycle, and Medicaid and other forms of insurance dampen the effects of private insurance loss that accompanies unemployment, which could partially mitigate reductions in the demand for healthcare.21,22 Additionally, recessions can have negative effects on health for certain subgroups of the population, 23 which could help to further prop up demand for healthcare services. It is also possible that due to shortages of healthcare workers, 24 temporary decreases in the demand for healthcare may have little effect on healthcare employment or the pipeline into the profession.
The relationship between the economy and healthcare education will be influenced by the local economy as well. The decision to obtain education in a given field is strongly related to the local economic prospects for that field.25,26 However, to the extent that healthcare employment is insulated from economic conditions, the field may be seen as a safe bet for individual human capital investments in education regardless of the overall economic outlook and may actually be more attractive to students during an economic downturn.
Regardless of the specific mechanism, results from this study will shed light on the prevailing relationships between local economic conditions and the healthcare workforce. While it will be several years before geographically disaggregated data is available to conduct similar analyses for the most recent COVID-19 induced recession, we already know that some healthcare-specific features of this economic downturn, such as severely curtailed demand for elective procedures, were not present in other recessions. 27 There is documented national unemployment growth information for several (but not all) healthcare professions, particularly at the lower end of the skill distribution. 28 The results to follow will provide an important backdrop for any future inquiries into the most recent recession and the healthcare workforce: understanding how this workforce behaves during “typical” economic cycles will allow for contrast to downturns driven in part by a healthcare-specific behavioral component.
New Contributions
This study provides a novel contribution to understandings of how labor and education markets react to overall and local economic conditions. While the general topic has been widely studied for the economy in general, in this study we demonstrate that the healthcare sector and the educational pipeline into that sector appear to be playing by a unique set of rules: specifically, that the healthcare sector is particularly stable with respect to economic turmoil. We then demonstrate which types of jobs and educational programs are the source of this stability. We are aware of only two other studies in this area: a longitudinal exploration of growth trends in the sector, 29 and a case study of new physicians in New York during the Great Recession. 30
Data
We draw data from several sources. Our main independent variable measuring the macro-economic climate, county unemployment rates from 2005 to 2017, comes from the Local Area Unemployment Statistics (LAUS), which the U.S. Bureau of Labor Statistics (BLS) creates using data from the Current Population Survey, the Current Employment Statistics survey, and state unemployment insurance systems. 31 The unemployment rates from the LAUS provide a measure of local economic activity that has frequently been used to examine impacts of business cycles.32–34 2005 serves as the first year of analysis data so that the study period includes multiple years prior to the Great Recession, and 2017 is the final year included in the analysis sample as it was the most recent year of data available across all data sets.
To measure health care employment, we draw on employment data from 2005–2017 from the Quarterly Census of Employment and Wage (QCEW). The QCEW is produced by the BLS using state and federal unemployment insurance records and reflects 95% of jobs in the United States. The employment data are available by industry, following the North American Industry Classification System (NAICS). We derive employment for the entire healthcare sector by using 3-digit NAICS codes of 621 (Ambulatory Health Care Services), 622 (Hospitals), and 623 (Nursing and Residential Care Facilities). Sub-industries within the healthcare sector can be identified by their 4-digit NAICS codes. For example, to look specifically at nursing homes, we can identify establishments with an NAICS code of 6231. We cannot reliably attain greater specificity as BLS uses a rule to preserve data confidentiality where cells that are provided by or substantially attributable to a single large employer are suppressed. While there are no missing/censored values at the county by 3-digit or 4-digit NAICS code level (which we use), at the county by 5-digit or 6-digit NAICS code level, almost 20% of the total employment in healthcare sector is suppressed.
The sub-industries we look at are Nursing Care Facilities, which includes establishments in NAICS of 6231, Home Health Care Services, which includes establishments in NAICS 6216, Office of Physicians, which includes establishments in NAICS 6211, and General Medical and Surgical Hospitals, which includes establishments in NAICS 6221. These 4 sub-industries accounted for the majority (63%) of total health care employment in 2017.
To analyze how educational outcomes change with local economic conditions, we utilize data on educational degree completion from the Integrated Postsecondary Education Data System (IPEDS) for school years that end in 2005–2017. In addition to containing information about each academic institution, such as its location, IPEDS contains information on the number of graduates receiving degrees from each of the school’s programs. This program-level information includes the Classification of Instructional Programs (CIP) codes, the number of years the program takes to complete, whether the program is online, and whether it is offered by a for-profit institution. IPEDS does not provide enrollment counts (as opposed to graduation counts) disaggregated by county and CIP code.
We limit the sample to healthcare professions, which are those with a two-digit CIP code of 51. This two-digit CIP code includes nearly all health care degrees, including for health care practitioners, health care administration, and public health. The most commonly awarded degrees are Registered Nursing, Nursing Administration, Nursing Research, Clinical Nursing, Practical Nursing, Vocational Nursing and Nursing Assistants (CIP code 51.38 and 51.39), and Health and Medical Administrative Service (CIP code 51.07 and 51.08). These 4 CIP codes contribute 60% of degrees in health care in 2017. For the heterogeneity analysis into education sector, we examine health care degrees in top 4 professions, degrees which take less than 1 year to complete, and degrees offered by for-profit institution.
From the above two sources of data (the QCEW and IPEDS), we construct the share of both employment and completed degrees accounted for by the healthcare sector in each county in each year. These variables serve as our outcomes of interest.
We also create additional variables that control for county-level time-varying factors that could potentially be related to employment and education. These variables include median household income, poverty rate, and the working-age (defined as between 19–64 years old) population count in each county in each year and come from the Small Area Estimates of Poverty and Inequality and the Population and Housing Census Estimates.35,36 To identify recessionary and recovery periods, we use the recession and expansion definitions for the nation as a whole from the National Bureau of Economic Research’s (NBER) Business Cycle Dating Committee, which defines recessions as the period between a peak of economic activity and the subsequent trough and expansions as the period between troughs and peaks.
Methods
We estimate multivariate regression models where we regress the share of employment or graduates in the healthcare sector on the local unemployment rate. It should be noted that when regressing the share of graduates, we employ county-level unemployment rate at time t−1 to capture the lag pattern of the effects on the share of graduates. All models control for a set of county-fixed effects and year-fixed effects. County-fixed effects remove the impact of any time invariant (over our sample) county-level factors relevant to health care employment such as the presence of a large hospital system or underlying population health. Year-fixed effects remove the impact of any nationwide factors relevant to the healthcare workforce common to all places in a given year, such as the presence of national components of the Affordable Care Act, changes in rules regarding for-profit colleges accessing federal financial aid, or changes in healthcare technology. All models also control for county level annual median household income, poverty rate, and the working-age (defined as between 19–64 years old) population count. To avoid over-counting effects from low-population areas, we weigh regressions using the county population by year from the Census of Housing and Population.
In addition to estimating this model for the entire sample period, we also estimate separate models for recessionary and expansionary periods, using the NBER’s national classifications of recessionary and expansionary periods described above. Note that because recessionary and recovery periods are defined for the nation as a whole, we can still identify the impact of the unemployment rate separately because counties experience differential unemployment changes within the recessionary or expansionary periods. Finally, we estimate the above models for subsets of healthcare employment and education. For healthcare employment, we look specifically at nursing care facilities, home health care services, offices of physicians (excluding mental health), and general medical and surgical hospitals. For healthcare education, we look specifically at the top 4 most common healthcare professions based on CIP codes, degrees that take 1 year or less to complete, and degrees at for-profit institutions.
Results
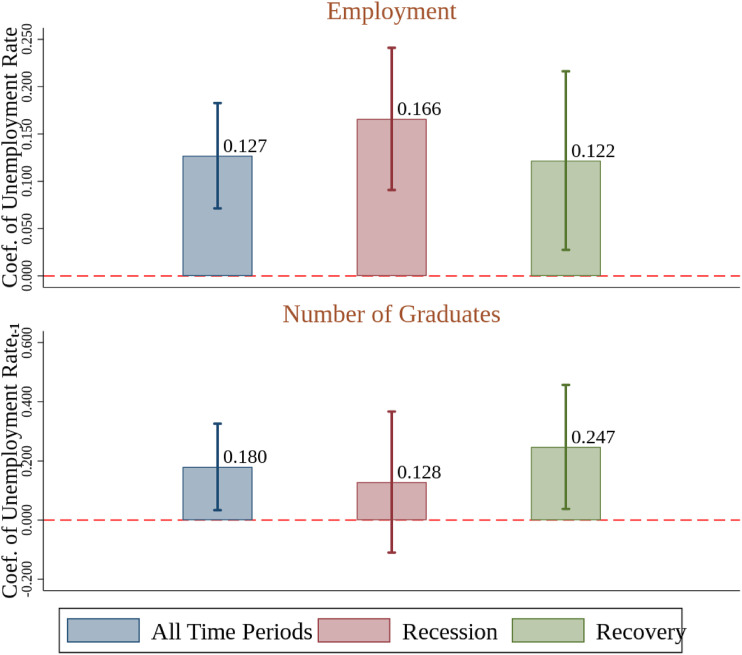
Figure 1 displays coefficients and 95 percent confidence intervals on the unemployment rate from the county-level regressions. The top panel of Figure 1 shows estimates with the share of healthcare employment as the dependent variable. Each bar shows the coefficients from a separate regression. All results are similar when analyses are conducted at the state rather than county level and are shown in Appendix A. Full regression results for all figures are presented in Appendix B.
Figure 1.
Share in Health Care Employment and Graduates vs. Unemployment Rate. Source: Quarterly Census of Employment and Wages (QCEW) 2005–2017, Integrated Post-Secondary Education Data System (IPEDS) 2005–2017, and U.S. Bureau of Labor Statistics (BLS) Local Area Unemployment Statistics (LAUS) (2005–2017). Notes: Figure shows coefficients and confidence intervals of the unemployment rate. For employment, unemployment rate is at time t. For number of graduates, unemployment rate is at time t−1. Regressions control for county and year-fixed effects. Regressions are weighted by population counts. Economic condition controls include median household income, poverty rate, and working age population. Recession refers to 2007–2009. Recovery refers to 2010–2017. 95% confidence intervals are obtained from heteroskedasticity robust standard errors clustered at state level. Health Care employment from QCEW refers to county establishments in NAICS 3-digit code 621, 622, and 623. HealthCare graduates from IPEDS refer to county graduates in CIP code 51.
Healthcare employment as a share of total county employment is positively related to the unemployment rate. The estimated coefficient on the unemployment rate is 0.127, implying that a 10-point increase in the local unemployment rate is associated with approximately a 1.27 percentage point increase in healthcare’s share of local employment. This relationship is different depending on the overall direction of the national economy: an increase in the local unemployment rate during a national recession is associated with stronger growth in the healthcare sector than a similar-sized increase in the local unemployment rate during a national expansionary period.
The bottom panel of Figure 1 shows estimates with the share of healthcare graduates as the dependent variable. Like in the case of healthcare employment, the share of healthcare graduates is also positively related to the unemployment rate. The estimated coefficient is 0.18, implying that a 10-point increase in the unemployment rate is associated with a 1.8 percentage point increase in healthcare’s share of postsecondary graduates. The relationship between unemployment and healthcare’s share of graduates is again different based on the state of the national economy, but the pattern is reversed relative to healthcare’s share of employment. Here, an increase in the local unemployment rate during a recession is associated with weaker growth in the healthcare sector than a similar-sized increase in the unemployment rate during an expansionary period.
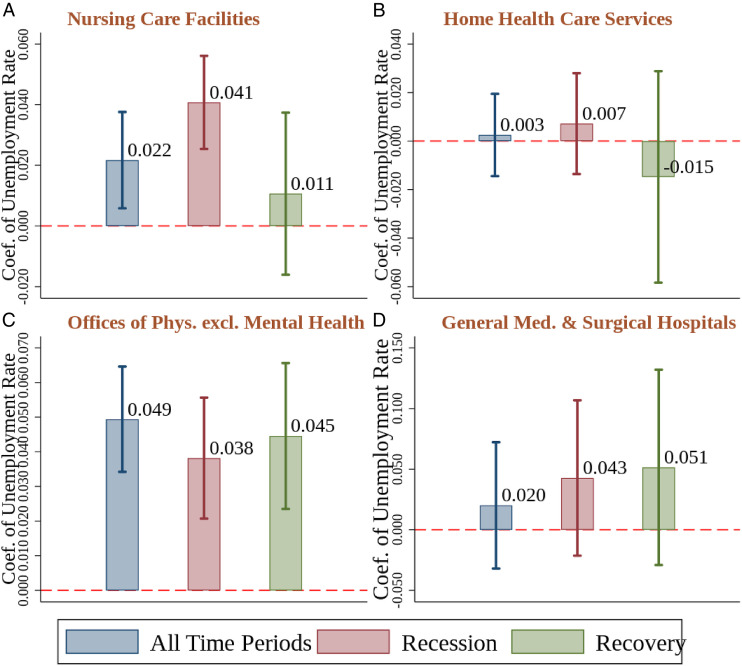
Figure 2 focuses on the largest classes of healthcare workforce employers, repeating the analyses reported in the top panel of Figure 1. The strongest relationship between local unemployment and healthcare’s share in employment is in physicians’ offices: a 10-point increase in the unemployment rate is associated with a 4.9 percentage point increase in the share of local employment in physicians’ offices. Among general medical and surgical hospitals as well as nursing care facilities, there is also a strong association between local unemployment and the subsectors’ share of local employment, with estimates implying a 2.0 and 2.1 percentage point increase in employment share for a 10-point increase in the unemployment rate, respectively. The share of employment in home healthcare services, on the other hand, seems largely unaffected by local unemployment. There is also interesting variation in the results based on whether the national economy is in recession or is expanding. Whereas the state of the local economy does not seem to have a strong effect on the share of the workforce employed by hospitals and physicians’ offices, nursing care facilities grow their share of the workforce more robustly when both the local and national economies are in a downturn.
Figure 2.
Share in Health Care Employment in Selected Industries vs. Unemployment Rate. Source: QCEW 2005–2017 and BLS LAUS (2005–2017). Notes: Figure shows coefficient and confidence interval of unemployment rate at time t. Regressions control for county and year-fixed effects. Regressions are weighted by population count. Economic condition controls include median household income, poverty rate, and working age population. 95% confidence intervals are obtained from heteroskedasiticy robust standard errors clustered at the state level. Health Care employment from QCEW refers to county establishments in NAICS 4-digit code 6231 for Nursing Care Facilities (Panel A), 6216 for Home Health Care Services (Panel B), 6211 for Offices of Physicians excl. Mental Health (Panel C), and 6221 for General Medical and Surgical Hospitals (Panel D).
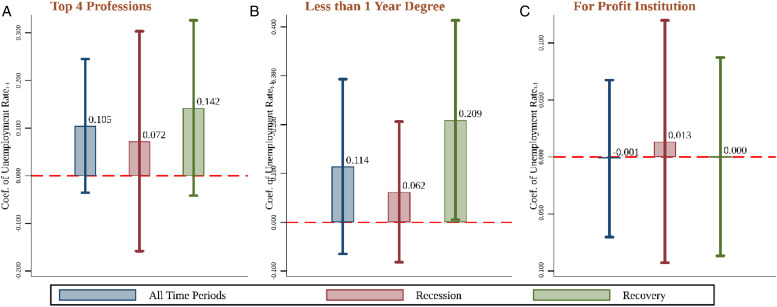
In Figure 3, we repeat the analyses reported in the bottom panel of Figure 1 for subsets of degrees: degrees in the four most common medical professions based on numbers of degrees, degrees that take less than 1 year to complete, and degrees awarded at for-profit educational institutions. The four most common professions are slightly less responsive to local unemployment than degrees as a whole, suggesting that the findings in Figure 1 may be due to less common degrees (although the confidence intervals on these estimates are quite wide). Likewise, degrees that take less than a year to complete are slightly less responsive than all degrees, although it is worth noting that these degrees are much more strongly related to local unemployment during national economic downturns. Finally, degrees at for-profit institutions appear to be unrelated to local economic conditions.
Figure 3.
Share of Health Care Graduates in Selected Industries vs. Lag of Unemployment Rate. Source: IPEDS 2005–2017, and BLS LAUS (2005–2017). Notes: Figure shows coefficients and confidence intervals of the unemployment rate at t−1. Regressions control for county and year-fixed effects. Regressions are weighted by population counts. Economic condition controls include median household income, poverty rate, and working age population. 95% confidence intervals are obtained from heteroskedasticity robust standard errors clustered at state level. Healthcare graduates in top 4 professions from IPEDS refer to county graduates with CIP codes 51.38, 51.39 for Registered, Practical Nursing, Nursing Admin and research and 51.8, 51.07 for Allied Health and Health Care Medical Admin Services (Panel A). Healthcare graduates in less than 1 year degree refer to county graduates with award degree equal to IPEDS category 1 (Panel B). Healthcare graduates in for profit institution refer to county graduates in IPEDS categories 3, 6, and 9 (Panel C).
Discussion
The results presented in this paper indicate that the healthcare sector is stable across the business cycle. If anything, when counties experience more severe economic downturns, healthcare employment seems to increase. Even during the Great Recession, which saw employment fall in most sectors, employment in healthcare held steady and grew as a share of all employment. This suggests that the healthcare workforce is systematically different than the U.S. workforce taken as a whole but does not necessarily generalize to any single sector-to-sector comparison with healthcare.
It should be noted that the analyses presented above capture employment levels in specific employment categories but are not capable of detecting changes in the composition of those jobs. For example, increases in employment could be among lower paid and less skilled classes of employees. Our analyses would not be able to detect this downskilling. The above analyses are also incapable of detecting any changes in job turnover.
We also note that high levels of healthcare employment are not necessarily an efficient use of resources. 37 However, some evidence suggests that higher staffing levels are associated with better care. 38 Whether the healthcare sector being generally stable or growing during a downturn is good for health outcomes is also an open question, although there is evidence that nursing facilities see better outcomes during economic downturns. 39
Our findings are also relevant for policymakers considering vocational rehabilitation programs for injured or displaced workers, or forming employment policy in response to structural shifts in the economy. Employment policy that encourages people to shift to the healthcare sector may optimize employment opportunities and lower people’s risk in future economic downturns. Nudging those who are particularly vulnerable to negative ramifications of job loss into a more stable sector could be welfare improving.
These results are highly relevant to public policy guidance and to academic research in light of the COVID-19 pandemic and the associated recession. Early analyses suggest that some parts of the healthcare sector were not insulated from this economic downturn as they had been previously. Home health services, hospitals, and physicians’ offices saw sizable decreases in economy-wide employment. 28 The COVID-19 recession has also been shown to have hit workers particularly hard in high contract and inflexible service occupations, including those working in long-term care. 40 While it will be several years before data that covers the entire pandemic recession with local disaggregation is available, the earliest findings suggest that the COVID-19 recession differs from other recessions, and that the stability of the prior 2 decades may not hold indefinitely as confidence in the sector’s ability to withstand economic shocks is shaken.
Acknowledgments
We thank Jeanette Samyn for comments.
Appendices: For “Is Healthcare Employment Resilient and “Recession Proof”?
Appendix A: State Level Relationships
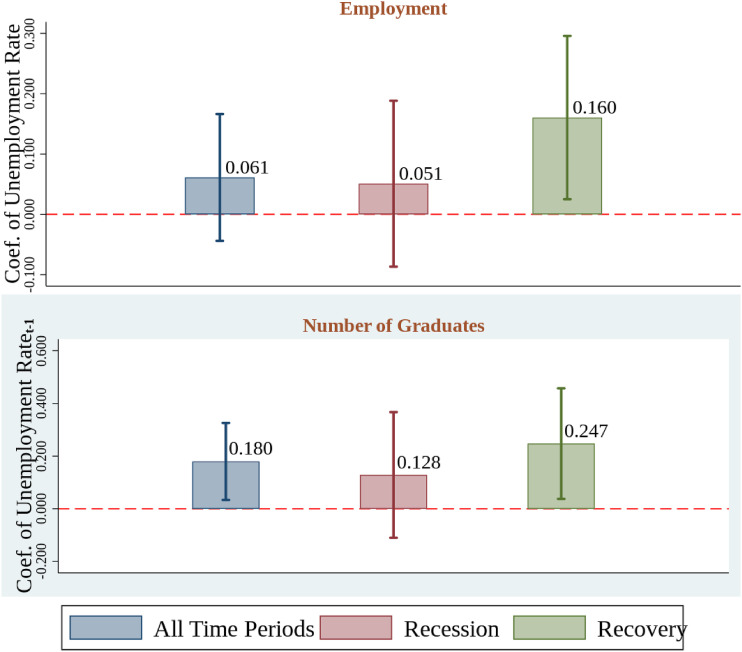
In Appendix A, we present the relationship between the share in health care and the unemployment rate at the state level. The coefficients are from a series of fixed effect regressions of the health care shares on the unemployment rate, controlling for state fixed effects, median income of households, poverty rate, and working population size.
Appendix Figure A.
Share in Health Care Employment and Graduates vs. Unemployment Rate. Source: QCEW 2005–2017, IPEDS 2005–2017, and BLS LAUS (2005–2017). Notes: Figure shows coefficients and confidence intervals of the unemployment rate. For employment, unemployment rate is at time t. For number of graduates, unemployment rate is at time t-1. Regressions control for state and year-fixed effects. Regressions are weighted by population counts. Economic condition controls include state median household income, poverty rate, and working age population. Recession refers to 2007–2009. Recovery refers to 2010–2017.95% confidence intervals are obtained from heteroskedasticity robust standard errors clustered at the state level. Health care employment from QCEW refers to county establishments in NAICS 3-digit code 621, 622, and 623.
Appendix B: Full Results for Fixed Effect Regressions
In Appendix B, we present a county-fixed effects regression examining the relationship between health care’s share in employment and graduates and the unemployment rate. Our analysis regresses the health care share on the unemployment rate controlling for county-fixed effects, median income of households, poverty rate, and working population. We also present the regression results for selected industries based on NAICS codes and selected education fields based on CIP codes.
Appendix Table B1.
Regression Results: Health Care Share of Employment vs. Unemployment Rate.
| Dependent Variable: Share of Employment | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| Un-weighted | No Controls | With Controls | Recession | Recovery | |
| Panel A. Health Care and Social Assistance | |||||
| Unemployment rate | 0.162*** | 0.056 | 0.072 | 0.163*** | −0.065 |
| (0.051) | (0.084) | (0.088) | (0.040) | (0.146) | |
| Mean | 14.62 | 14.62 | 14.62 | 13.38 | 15.40 |
| Number of Obs. | 80,166 | 80,132 | 80,132 | 30,784 | 49,348 |
| Panel B. Health Care | |||||
| Unemployment rate | 0.164*** | 0.127*** | 0.140*** | 0.166*** | 0.122** |
| (0.031) | (0.028) | (0.029) | (0.037) | (0.047) | |
| Mean | 11.76 | 11.76 | 11.76 | 10.99 | 12.24 |
| Number of Obs. | 39,920 | 39,904 | 39,904 | 15,328 | 24,567 |
| County-fixed effects | Yes | Yes | Yes | Yes | Yes |
| Year-fixed effects | Yes | Yes | Yes | Yes | Yes |
| Economic conditions | Yes | No | Yes | Yes | Yes |
| Weighted | No | Yes | Yes | Yes | Yes |
Source: QCEW 2005–2017 and BLS LAUS (2005–2017). Economic conditions include median household income, poverty rate, and working age population. Panel A includes county establishments in NAICS 2-digit code 62. Panel B includes NAICS 2 digit code 62 except 4-digit 6241, 6242, 6243, and 6244. Regressions are weighted by population when indicated. Standard errors, heteroskedasticity-robust and clustered by state, are in parentheses. *P < 0.10 **P < 0.05 ***P < 0.01.
Appendix Table B2.
Regression Results: Health Care Share of Employment vs. Unemployment Rate-Selected Subsectors.
| Dependent Variable: Share of Employment | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| Un-weighted | With Controls | No Controls | Recession | Recovery | |
| Panel A. Nursing Care Facilities | |||||
| Unemployment rate | 0.031** | 0.022*** | 0.024*** | 0.041*** | 0.011 |
| (0.014) | (0.008) | (0.008) | (0.008) | (0.013) | |
| Mean | 1.75 | 1.75 | 1.75 | 1.76 | 1.75 |
| Number of Obs. | 34,805 | 34,805 | 34,805 | 13,353 | 21,423 |
| Panel B. Home Health Care Services | |||||
| Unemployment rate | 0.017 | 0.003 | 0.001 | 0.007 | −0.015 |
| (0.028) | (0.008) | (0.009) | (0.010) | (0.022) | |
| Mean | 1.28 | 1.28 | 1.28 | 1.09 | 1.39 |
| Number of Obs. | 29,742 | 29,726 | 29,726 | 11,035 | 18,584 |
| Panel C. Offices of Physicians excl. Mental | |||||
| Unemployment rate | 0.071*** | 0.049*** | 0.053*** | 0.038*** | 0.045*** |
| (0.010) | (0.008) | (0.007) | (0.009) | (0.010) | |
| Mean | 2.59 | 2.59 | 2.59 | 2.49 | 2.65 |
| Number of Obs. | 37,467 | 37,451 | 37,451 | 14,486 | 22,931 |
| Panel D. Health General Medical & Surgical Hospitals | |||||
| Unemployment rate | 0.038** | 0.020 | 0.024 | 0.043 | 0.051 |
| (0.014) | (0.026) | (0.025) | (0.032) | (0.040) | |
| Mean | 2.24 | 2.24 | 2.24 | 2.21 | 2.26 |
| Number of Obs. | 24,575 | 24,575 | 24,575 | 9,235 | 15,302 |
| County-fixed effects | Yes | Yes | Yes | Yes | Yes |
| Year-fixed effects | Yes | Yes | Yes | Yes | Yes |
| Economic conditions | Yes | Yes | No | Yes | Yes |
| Weighted | No | Yes | Yes | Yes | Yes |
Source: QCEW 2005–2017 and BLS LAUS (2005–2017). Economic conditions include median household income, poverty rate, and working age population. Panel A. includes establishments in NAICS of 6231, Panel B in NAICS 6216, Panel C in NAICS 6211, and Panel D in 6221. Regressions are weighted by population. Standard errors, heteroskedasticity-robust and clustered by state, are in parentheses. *P < 0.10 **P < 0.05 ***P < 0.01.
Appendix Table B3.
Regression Results: Health Care Share of Graduates vs. Unemployment Rate.
| Dependent Variable: Share of Health Care Graduates | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| Un-weighted | With Controls | No Controls | Recession | Recovery | |
| Panel A. All Degree | |||||
| Unemployment Ratet-1 | 0.051 | 0.178** | 0.183** | 0.128 | 0.247** |
| (0.055) | (0.070) | (0.076) | (0.119) | (0.104) | |
| Mean | 12.22 | 12.22 | 12.22 | 12.36 | 12.13 |
| Number of Obs. | 13,555 | 13,555 | 13,555 | 4,738 | 8,803 |
| Panel B. Top 4 Professions | |||||
| Unemployment Ratet-1 | 0.023 | 0.101 | 0.116* | 0.072 | 0.142 |
| (0.058) | (0.066) | (0.066) | (0.115) | (0.091) | |
| Mean | 9.33 | 9.33 | 9.33 | 9.57 | 9.18 |
| Number of Obs. | 12,686 | 12,686 | 12,686 | 4,416 | 8,252 |
| Panel C. Less than 1 year Degree | |||||
| Unemployment Ratet-1 | 0.080 | 0.108 | 0.103 | 0.062 | 0.209** |
| (0.062) | (0.084) | (0.077) | (0.072) | (0.102) | |
| Mean | 4.63 | 4.63 | 4.63 | 5.15 | 4.34 |
| Number of Obs. | 7,985 | 7,985 | 7,985 | 2,510 | 5,419 |
| Panel D. For Profit Institution | |||||
| Unemployment Ratet-1 | −0.041 | 0.000 | 0.003 | 0.013 | 0.000 |
| (0.052) | (0.035) | (0.029) | (0.053) | (0.043) | |
| Mean | 4.05 | 4.05 | 4.05 | 3.62 | 3.62 |
| Number of Obs. | 5,415 | 5,415 | 5,415 | 1,727 | 3,675 |
| County-fixed effect | Yes | Yes | Yes | Yes | Yes |
| Year-fixed effect | Yes | Yes | Yes | Yes | Yes |
| Economic condition | Yes | Yes | No | Yes | Yes |
| Weighted | No | Yes | Yes | Yes | Yes |
Source: IPEDS 2005–2017 and BLS LAUS (2005–2017). Economic conditions include median household income, poverty rate, and working age population. Sample includes graduates in the health care sector (CIP code 51) (Panel A), graduates in CIP codes 51.38, 51.07, 51.08, and 51.39 (Panel B), graduates with award level equal to 1 (Panel C), and includes graduates in institutions with sector codes 3, 6, or 9 (Panel D). Unemployment rate is from Bureau of Labor Statistics-BLS). Regressions are weighted by population. Standard errors, heteroskedasticity-robust and clustered by state, are in parentheses. *P < 0.10 **P < 0.05 ***P < 0.01.
Appendix Table B4.
Regression Results: Health Care Share of Graduates vs. Unemployment Rate in Selected CIP Codes.
| Dependent Variable: Share of Health Care Graduates | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| Un-weighted | With Controls | No Controls | Recession | Recovery | |
| Panel A. Registered, Practical Nursing, Nursing Admin and Research | |||||
| Unemployment rate | −0.040 | 0.013 | −0.002 | −0.046 | 0.029 |
| (0.040) | (0.031) | (0.028) | (0.043) | (0.044) | |
| Mean | 6.99 | 6.99 | 6.99 | 7.25 | 6.85 |
| Number of Obs. | 11,957 | 11,957 | 11,957 | 4,099 | 7,840 |
| Panel B. Allied Health and Medical Assisting Services | |||||
| Unemployment rate | 0.064 | 0.080 | 0.095 | 0.105 | 0.082 |
| (0.060) | (0.063) | (0.058) | (0.085) | (0.069) | |
| Mean | 2.58 | 2.58 | 2.58 | 2.76 | 2.76 |
| Number of Obs. | 8,077 | 8,077 | 8,077 | 2,536 | 5,506 |
| Panel C. Health and Medical Administrative Services | |||||
| Unemployment rate | 0.029 | 0.023 | 0.038 | 0.089 | 0.029 |
| (0.020) | (0.024) | (0.026) | (0.055) | (0.034) | |
| Mean | 1.52 | 1.52 | 1.52 | 1.68 | 1.44 |
| Number of Obs. | 9,087 | 9,087 | 9,087 | 2,945 | 6,100 |
| County-fixed effect | Yes | Yes | Yes | Yes | Yes |
| Year-fixed effect | Yes | Yes | Yes | Yes | Yes |
| Economic condition | Yes | Yes | No | Yes | Yes |
| Weighted | No | Yes | Yes | Yes | Yes |
Source: IPEDS 2010–2017 and BLS LAUS (2010–2017). Economic conditions include median household income, poverty rate, and working age population. Sample includes graduates in CIPCODE 51.38 and 51.39 after 2010 and 51.16 before 2010 (Panel. A), graduates in CIPCODE 51.07 (Panel B) and graduates in CIPCODE 51.08 (Panel C). Regressions are weighted by population. 95% confidence intervals are obtained using state clustered heteroskedasticity robust standard errors.
Footnotes
Declaration of Conflicting Interests: The authors declare that there are no conflicts of interest with regards to this research.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Andrew Friedson https://orcid.org/0000-0001-7553-3213
References
- 1.Kaiser Family Foundation . State Health Fact. Health Care Employment as a percent of Total Employment. 2020. Accessed: May, 16, 2020] [Available from:. https://www.kff.org/other/state-indicator/health-care-employment-as-total/https://www.kff.org/other/state-indicator/health-care-employment-as-total/.
- 2.Salsberg E, Martiniano R. Health Care Jobs Projected To Continue To Grow Far Faster Than Jobs In The General Economy. Health Affs. Blog. 2018. [Available from. https://www.healthaffairs.org/do/10.1377/hblog20180502.984593/full/https://www.healthaffairs.org/do/10.1377/hblog20180502.984593/full/. Accessed May 16, 2020.
- 3.Cutler DM. Your Money or Your Life: Strong Medicine for America's Health Care System: Oxford University Press; 2005. [Google Scholar]
- 4.Smith S, Newhouse JP, Freeland MS. Income, Insurance, and Technology: Why Does Health Spending Outpace Economic Growth?. Health Aff. 2009;28(5):1276–1284. 10.1377/hlthaff.28.5.1276 [DOI] [PubMed] [Google Scholar]
- 5.Chernew M, May D. The Oxford Handbook of Health Economics: Oxford University Press; 2011.Health care cost growth. [Google Scholar]
- 6.Staiger DO, Auerbach DI, Buerhaus PI. Health Care Reform and the Health Care Workforce – The Massachusetts Experience. N Engl J Med: Perspect. 2011;365(121):e24. 10.1056/NEJMp1106616 [DOI] [PubMed] [Google Scholar]
- 7.Chandra A, Skinner J. Technology Growth and Expenditure Growth in Health Care. J Econ Lit. 2012;50(3):645-680. [Google Scholar]
- 8.Frogner BK, Spetz J, Parente ST, Oberlin S. The Demand for Health Care Workers Post-ACA. Int J Health Econ Manag. 2015;15:139-151. 10.1007/s10754-015-9168-y [DOI] [PubMed] [Google Scholar]
- 9.Vespa J, Armstrong DM, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060 WA, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2018. [Google Scholar]
- 10.Silicon Valley Bank . Healthcare Investments and Exits Report. 2020. [Available from. https://www.svb.com/globalassets/library/uploadedfiles/reports/healthcare-report-2020-annual_abr.pdf https://www.svb.com/globalassets/library/uploadedfiles/reports/healthcare-report-2020-annual_abr.pdf. Accessed June 12, 2020.
- 11.Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A. Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. ” Am Econ Rev; 1987:177, 251-277. [PubMed] [Google Scholar]
- 12.Garber AM, Skinner J. Is American Health Care Uniquely Inefficient?. J Econ Perspect. 2008;22(4):27–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiamondObama Care D., the Secret Job Program; 2016. July, 13, 2016. Politico. [Available from https://www.politico.com/agenda/story/2016/07/what-is-the-effect-of-obamacare-economy-000164/. Accessed June25, 2020.
- 14.Musgrave RA. The Theory of Public Finance; a Study in Public Economy. New York: McGraw-Hill Book Co.; 1956. [Google Scholar]
- 15.Dolfman ML, Insco M, Holden RJ. Healthcare Jobs and the Great Recession. ” Mon Labor Rev. Bureau of Labor Statistics; 2018. [Retrieved at https://www.bls.gov/opub/mlr/2018/article/healthcare-jobs-and-the-great-recession.htm. [Google Scholar]
- 16.Chappelow J. “Industries That Thrive During Recessions” Investopedia. 2020. [Retrieved at. https://www.investopedia.com/articles/stocks/08/industries-thrive-on-recession.asp https://www.investopedia.com/articles/stocks/08/industries-thrive-on-recession.asp.
- 17.Staiger DO, Auerbach DI, Buerhaus PI. Registered Nurse Labor Supply and The Recession—Are We in a Bubble. N Engl J Med. 2012;366(16):1463-1465. 10.1056/NEJMp1200641 [DOI] [PubMed] [Google Scholar]
- 18.Alameddine M, Baumann A, Laporte A, Deber R. A narrative review on the effect of economic downturns on the nursing labour market: implications for policy and planning. Hum Resour Health. 2012;10(1):1-7. 10.1186/1478-4491-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zabalegui A, Cabrera E. Economic crisis and nursing in Spain. J Nurs Manag. 2010;18(5):505-508. 10.1111/j.1365-2834.2010.01118.x [DOI] [PubMed] [Google Scholar]
- 20.Heitlinger A. The paradoxical impact of health care restructuring in Canada on nursing as a profession. Int J Health Serv. 2003;33(1):37-54. 10.2190/RMAY-NJA9-KFW7-1UEW [DOI] [PubMed] [Google Scholar]
- 21.Cawley J, Moriya AS, Simon K. The impact of the macroeconomy on health insurance coverage: Evidence from the great recession. Health Economics. 2015;24(2):206-223. 10.1002/hec.3011 [DOI] [PubMed] [Google Scholar]
- 22.Jacobs PD, Hill SC, Abdus S. Adults Are More Likely To Become Eligible For Medicaid During Future Recessions If Their State Expanded Medicaid. Health Affs. 2017;36(1):32-39. 10.1377/hlthaff.2016.1076 [DOI] [PubMed] [Google Scholar]
- 23.Crost B, Friedson A. Recessions and health revisited: New findings for working age adults. Econ Hum Biol. 2017;27:241-247. 10.1016/j.ehb.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 24.Seago JA, Ash M, Spetz J, Coffman J, Grumbach K. Hospital Registered Nurse Shortages: Environmental, Patient, and Institutional Predictors. Health Serv Res. 2001;36(5):831. [PMC free article] [PubMed] [Google Scholar]
- 25.Blom E, Cadena BC, Keys B. Investment over the Business Cycle: Insights from College Major Choice; 2015.Labor Econ 2021;39(4):1043-1082. [Google Scholar]
- 26.Hershbein BJ. Graduating High School in a Recession: Work, Education, and Home Production. B E J Econ Anal Pol. 2012;12(1):1-32. 10.1515/1935-1682.2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The Impact of the COVID-19 Pandemic on Outpatient Visits: Practices Are Adapting to the New Normal. Commonwealth Fund; 2020. June 2020). [Available from DOI: 10.26099/2v5t-9y63. [DOI] [Google Scholar]
- 28.Bhandari N, Batra K, Upadhyay S, Cochran C. Impact of COVID-19 on Healthcare Labor Market in the United States: Lower Paid Workers Experienced Higher Vulnerability and Slower Recovery. Int J Environ Res Publ Health. 2021;18(8):3894. 10.3390/ijerph18083894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wood CA. ” Monthly Labor Review Employment in health care: a crutch for the ailing economy during the 2007-09 recession; 2011:13-18. [Google Scholar]
- 30.Chen A, Lo Sasso A, Richards MR. Graduating into a downturn: Are physicians recession proof?. Health Econ. 2018;27:223-235. 10.1002/hec.3538 [DOI] [PubMed] [Google Scholar]
- 31.Bureau of Labor Statistics and U.S. Department of Labor . Local Area Unemployment Statistics; 2019. [Retrieved at https://www.bls.gov/lau/.
- 32.Ruhm CJ. Are Recessions Good for Your Health?. Q J Econ. 2000;115(2):617–650. [Google Scholar]
- 33.McInerney MP, Mellor JM. State Unemployment in Recessions during 1991–2009 Was Linked to Faster Growth in Medicare Spending. Health Aff. 2012;31(11):2464–2473. [DOI] [PubMed] [Google Scholar]
- 34.Hollingsworth A, Ruhm CJ, Simon KI. Macroeconomic Condition and Opioid Abuse. J Health Econ. 2017;56:222–233. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau . Population and Housing Unit Estimates, 2019. a. [Retrieved at https://www.census.gov/programs-surveys/popest.html.
- 36.United States Census Bureau . Small Area Income and Poverty Estimates (SAIPE) Program. 2019. b. [Retrieved at. https://www.census.gov/programs-surveys/saipe.html https://www.census.gov/programs-surveys/saipe.html.
- 37.Baicker K, Chandra A. The Health Care Jobs Fallacy. N Engl J Med. 2012;366(26):2433–2435. [DOI] [PubMed] [Google Scholar]
- 38.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-Staffing Levels and the Quality of Care in Hospitals. N Engl J Med. 2002;346:1715–1722. [DOI] [PubMed] [Google Scholar]
- 39.Stevens AH, Miller DL, Page ME, Filipski M. The best of times, the worst of times: understanding pro-cyclical mortality. Am Econ J Econ Pol. 2015;7(4):279–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albanesi S, Kim J. Effects of the COVID-19 Recession on the US Labor Market: Occupation, Family, and Gender. J Econ Perspect. 2021;35(3):3–24. [Google Scholar]