Abstract
Background:
Alcohol and other drug (AOD) use patterns have altered as a result of the coronavirus (COVID-19) pandemic restrictions. This study aimed to: (i) determine the impact of the pandemic on patterns of AOD use among individuals seeking treatment, (ii) identify which mental health and resilience factors were associated with changes in patterns of AOD use and (iii) evaluate changes in the contextual factors (eg, motivations) associated with use.
Methods:
Cross-sectional surveys were completed by clients (n = 325) who had sought AOD treatment from January 2020 onwards. We measured quantity and frequency of AOD use now compared to before the pandemic, mental health (depression, anxiety, trauma exposure), resilience and contextual factors related to AOD use.
Results:
Quantity of tobacco and cannabis use increased post-pandemic, while methamphetamine and alcohol did not change. Depression was associated with more frequent alcohol use now compared to before the pandemic, while anxiety and lower resilience were associated with less frequent cannabis use now. Lower resilience was associated changes in methamphetamine use. Depression was associated with using more frequently for enjoyment and to alleviate loneliness following the pandemic, and anxiety was associated with using earlier in the day and to alleviate boredom.
Conclusions:
The pandemic has led to increased frequency of AOD use for a subset of individuals seeking treatment. Depression, anxiety and resilience are important factors associated with altered AOD use, and changes in the motivations and control surrounding use. Special consideration of this should be considered during AOD treatment through the pandemic.
Keywords: Substance use, COVID-19, anxiety, depression, AOD treatment
Introduction
The coronavirus (COVID-19) pandemic is a worldwide crisis that has led to major concern on the impact on patterns of alcohol and other drug (AOD) use. 1 The uncertainty and stresses caused by the pandemic, coupled with social isolation and financial pressures, are likely to disproportionately impact individuals with substance use disorders (SUDs) due to increased incidence of mental and physical health problems, housing or financial insecurities and social inequalities. 2
Following the enforcement of social restrictions since January 2020, 3 many countries reported changes in AOD use. This included increased use of alcohol, cannabis and tobacco use among general4-8 and substance-using populations,9-13 and reductions in the availability and use of ‘party drugs’ such as MDMA 14 corresponded with reduced social settings where they are typically consumed. Community samples of Australians who regularly use AODs similarly reported increased use of cannabis and alcohol during the restrictions, 15 in addition to decreased use of MDMA, cocaine and ketamine. 16 Among people who inject drugs, the majority reported no change in heroin, methadone or buprenorphine-naloxone injection use and some who inject methamphetamines reported using less following pandemic restrictions. 17 Compared to pre-pandemic rates, similar patterns of methamphetamine and heroin use were reported across Australia among people who use illicit drugs; although some regions are beginning to show a drop in injecting as restrictions continue. 16 Research evaluating changes in AOD use specifically for clinical and treatment-seeking samples is comparatively sparse because this population is hard to reach, however determining how AOD use has been impacted among dependent or treatment-seeking populations is required to ensure treatment services are able to adapt appropriately.
Individuals with SUDs may be more susceptible to severe responses to COVID-19 due to a greater presence of physical and mental health comorbidities.18-21 This is additional to greater exposure to situations that increase the risk of contracting the virus, such as medical appointments or daily pharmacy visits for opioid agonist medications. 22 Exacerbation of mental health problems due to increased stress and psychological distress caused by the pandemic restrictions 23 may also increase AOD use and impact treatment among those with SUDs. 24 Targeting mental health factors through treatment may be an important avenue for attenuating the harms of the pandemic for people with SUDs. Among people who use drugs, depression and anxiety have been cited as major reasons for increased use following restrictions,17,25,26 yet little research has explored the links between these mental health factors and AOD use in treatment-seeking populations.
Changes in access to drugs, restrictions in social interactions and psychological stress following the pandemic are also likely to alter contextual factors surrounding AOD use. Increased loneliness and boredom have been cited as commonly reported reasons for increased AOD use, and changes in situational factors such as having more money, having more time, and spending more time with others who use AOD. 17 Understanding how the pandemic has altered the context of AOD use, and associations with mental health factors among treatment-seeking populations, will also be important for treatment services to adapt quickly and ensure that AOD-related harms are minimised.
The purpose of the current study was to: (i) explore the impact of COVID-19 on patterns of AOD use among people who had sought treatment for a SUD in Australia during the pandemic; (ii) identify whether mental health variables such as depression, anxiety, trauma and resilience were associated with changes in AOD use and (iii) evaluate changes in contextual factors associated with AOD use. Insights from this research are integral for AOD services to adapt appropriately at all phases during the COVID-19 pandemic, which is imperative for future outbreaks and informative for other countries.
Methods
Participants
Participants were recruited from Lives Lived Well, a non-government organisation AOD services across Queensland and New South Wales, Australia, between July and August 2020. Clients were required to be aged 18+ years, and to have sought AOD treatment from 1st January 2020 onwards.
Measurements
Frequency and quantity of AOD use
AOD use was measures by the Australian Treatment Outcomes Profile (ATOP), 27 a brief measure of the frequency of use in the past 4-weeks which asked participants what substances they had used, in what quantity and how many days per week. The ATOP was adapted to also ask clients of the typical quantity of each substance used in the 4-weeks before pandemic restrictions were in place (23rd March 2020). In addition, we also asked participants to rate how frequently they use each substance now compared with before the pandemic on a 5-point Likert scale (1—a lot less frequently; 5—a lot more frequently) and whether quantity of use has changed now compared to before the pandemic (1—a lot less; 5—a lot more). These were retrospective reports of quantity and frequency of AOD use up to 4 to 6 months prior to the survey.
Depression, anxiety, resilience and trauma
Participants completed: the Patient Health Questionnaire (PHQ-9) 28 (9-item measure of depression over the past 2 weeks); the Generalised Anxiety Disorder Scale (GADS) 29 (7-item measure of generalised anxiety over the past 2 weeks); the primary care PTSD screen (PC-PTSD-5) 30 (5-item measure of symptoms associated with prior experiences of trauma) and the Brief Resilience Scale (BRS) 31 (5-item measure of the ability to bounce back and cope with difficult or stressful situations).
Context of AOD use
Contextual factors were measured by asking how much of the time participants engaged in different AOD-related behaviours now compared with before the pandemic. Responses were recorded on 6-point Likert Scale (1—none of the time; 6—all of the time), and asked clients how frequently they were using earlier in the day and finding it difficult to stop (control), using alone and using with others (social context), using less safely (safety) and using to increase enjoyment, reduce boredom, reduce stress and reduce loneliness (motivational context). We also asked how easy it is to obtain each substance used following the pandemic (1—much easier; 5—much harder).
Socio-demographic characteristics
Socio-demographic covariates included age, sex, levels of education, indigenous Australian status, employment status and receipt of government benefits. Financial distress was measured using a subscale adapted from the Psychiatric Epidemiology Research Interview Life Events Scale, 32 which assessed the frequency of financial events which may have caused distress as a consequence of the pandemic.
Procedure
An SMS was sent to LLW clients who fitted the eligibility criteria on the 14th July 2020 inviting them to take part in an anonymous survey on the impact of the COVID-19 pandemic on their AOD use. The SMS contained a link to the participant information sheet and consent form, followed by the study questions. Responses from those who consented were collected between July and August 2020. The median time to complete the survey was 16 minutes. Following completion, participants were invited to enter a prize draw to receive 1 of 3 $100 gift cards. The current study obtained ethics approvals (No. 2020000949) from The University of Queensland HREC and the participating AOD service.
Statistical analyses
Data were analysed using SPSS Version 25. Skewness and kurtosis were assessed. Extreme outliers were winsorized, or non-parametric tests were used. Missing data were observed for some variables, but were not associated with socio-demographic or substance use characteristics of the participants (SM1); cases were retained pair-wise where possible because they provided valuable information on AOD use. The alpha criterion for significance was P < .05.
Patterns of AOD use and contextual factors were presented descriptively (Aims I-III). T-tests were used to analyse changes in reported quantities, and were followed-up with pairwise comparisons (Bonferroni-corrected). Non-parametric data were analysed using the Wilcoxon signed-rank test with 2 levels. Reported frequency/quantity of AOD use was divided into 3-categories (using more; no change; using less) and contextual factors were divided into 2-catergories (none of the time; some of the time or more). Mental health associates (depression, anxiety, trauma and resilience) were pre-selected due to their clinical importance, and specified prior to analyses. Logistic regressions were used for dichotomous outcomes, and multinomial logistic regressions for categorical outcomes with >2 levels, with ‘no change’ entered as the reference category, and ‘using more’ and ‘using less’ as outcomes. These analyses controlled for: age; baseline quantity of AOD use to adjust for actual levels of use when accessing changes in their use; ease of obtaining AOD and financial distress. Pearson’s correlations were conducted for associations between variables, where Spearman’s Rho correlations were used in cases where normality was violated.
Results
Recruitment and participant characteristics
A SMS invite for the study was sent to 5063 clients in treatment, where 4177 (83%) of these messages were successfully received, however 886 (17%) did not reach the individual due to invalid phone numbers. Of the messages successfully received, 396 (10%) individuals consented to take part, and 325 (8%) were included in the final analyses after removing individuals who did not adequately complete the survey. Participants had a mean age of 36.71 years (SD = 10.95), and 57% (n = 185) were female. Just over 17% (n = 56) identified as Indigenous Australians, 69% (n = 225) were employed and 80% (n = 259) were receiving government benefits. Further descriptive findings are reported in SM1.
The majority of respondents (n = 286, 88%) reported using: tobacco (70%, n = 227), alcohol (58%, n = 187), cannabis (39%, n = 128), methamphetamine (25%, n = 80) and other illicit drugs (18%, n = 57). Thirty-nine (12%) reported not having used any substances in the prior 28 days.
Patterns of AOD use (Aim I)
Adapted ATOP: AOD quantities and days used
Estimated quantities of AOD use now compared with before the pandemic showed that number of cigarettes per day significantly increased, alongside a significant change in cannabis use (grams) (see Table 1).
Table 1.
ATOP outcomes: current and retrospective substance use before the pandemic.
| Use in past 28 days |
Quantity |
Test statistic | P | |||
|---|---|---|---|---|---|---|
| n (%) | Days used | Before | Now | |||
| M (SD) | ||||||
| Tobacco | 227 (69.8) | |||||
| Cigarettes (n/day) a | 14.09 (8.32) | 15.39 (9.87) | t = 2.33 | .021* | ||
| Vaping (ml/day) b | 5.00 (6.50) | 5.00 (8.50) | Z = 0.52 | .606 | ||
| Alcohol (units/day) b | 187 (57.5) | 12.21 (9.63) | 5.00 (10.00) | 5.00 (8.00) | Z = 0.79 | .937 |
| Cannabis (g/day)b,c | 128 (39.4) | 16.21 (10.14) | 1.00 (1.75) | 1.00 (2.75) | Z = 2.94 | .003** |
| Meth. (g/day) b | 80 (24.6) | 9.64 (9.40) | 0.20 (0.45) | 0.25 (0.40) | Z = 1.18 | .238 |
| Other illicit drugs | 57 (17.5) | 8.21 (7.89) | ||||
Abbreviations: g, grams; ml, millilitres.
Questions adapted from the ATOP. n = used in the past 28 days.
Data for quantity met assumptions of normality; a t-test was conducted and means and standard deviations were reported.
Data for quantity violated assumptions of normality and a Wilcoxon signed-rank test was used, median and interquartile range are reported.
The median was 1.00 overall before and after, but 22.9% reported a lower amount, 32.2% reported the same and 44.9% reported a larger amount after.
P < .05. **P < .01.
Change in perceived frequency and quantity of AOD use compared with before the pandemic
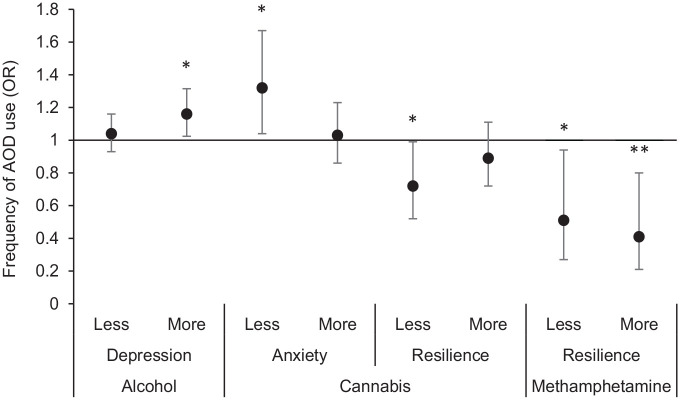
Of those who expressed using the different substances, perceived change in frequency and quantity differed by substance. Similar proportions of respondents indicated that both the frequency and quantity of alcohol increased, decreased or experienced no change. For cannabis, the largest category of participants reported an increase in frequency (45.63%, n = 47) and quantity (39.81%, n = 41) (Figure 1). For methamphetamines, the majority reported using less frequently (49.25%, n = 33) and in less quantities (53.73%, n = 36). For other illicit drug use, the many participants reported using more frequently (43.90%, n = 18), however a similar proportion also reported using less in quantity (39.02%, n = 16).
Figure 1.
Participant changes in reported (a) frequency and (b) quantity of AOD use now compared to before the pandemic restrictions, divided by drug type. We received responses for reported alcohol use (n = 156), cannabis use (n = 103), methamphetamine use (n = 67) and other illicit drug use (n = 41). The sample size for individuals who used less, more or experienced no change as a consequence of the pandemic are reported within each of the bars.
Associations between mental health and AOD use (Aim II)
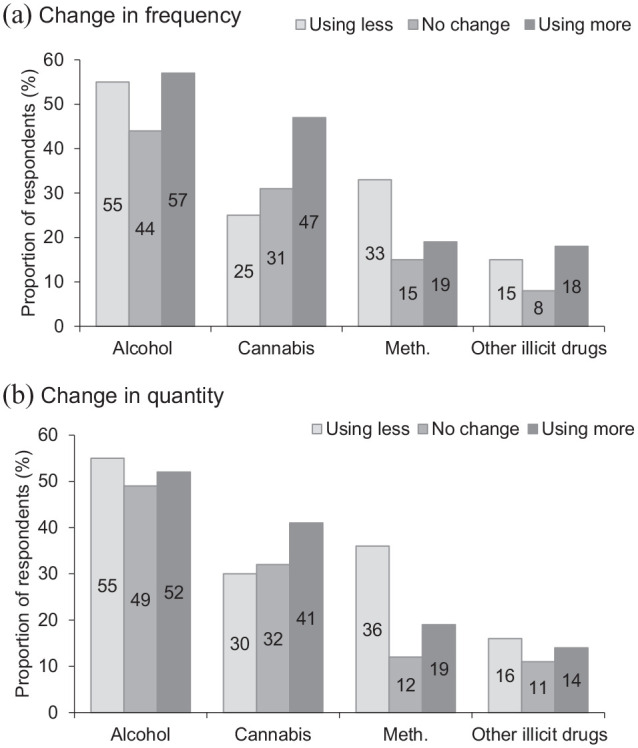
Multinomial logistic regressions indicated significant associations between some mental health variables with changes in the frequency of AOD use now compared to before the pandemic, but not with quantity of AOD use. Figure 2 displays the significant associations between mental health variables and the change in frequency of AOD use (using less/more/same as before) following onset of pandemic restrictions (see SM3 for full table of results). Adjusted ORs indicated there was a 16% increase in the odds of more frequent alcohol use, compared to no change with each unit increase in depression score (P = .020). For frequency of cannabis use, there was a 32% increase in the odds of using less than before with each unit increase in anxiety score (P = .025), alongside a 72% decrease in the odds of using less frequently for each unit increase in resilience score (P = .043). For methamphetamine use, there was a 41% decrease in the odds of using methamphetamine more frequently for each unit increase in resilience score (P = .009), and a 51% decrease in the odds of using less frequently (P = .031).
Figure 2.
Adjusted odds ratios (ORs) and 95% confidence intervals for mental health associates of changes in frequency of AOD use (using less or more frequently, compared with no change) divided by each drug type (x axis: 1 = no change in frequency, comparator group). Greater depression scores were associated with greater odds of using alcohol more frequently compared to no change. Greater anxiety was significantly associated with an increased odds of using cannabis less frequently compared to no change. Greater resilience was associated with a significant decreased odds of using cannabis and methamphetamines less frequently, as well as a decreased odds of using methamphetamines more frequently. *P < .05, **P < .010; see SM3 for table of full results.
Trauma was not associated with any change in the frequency of AOD use, and no other comparisons were significant (see SM3). Increased difficulty in obtaining cannabis was associated with lower odds of using less frequently (OR = 0.28; P = .025; see SM3/4), while increased ease of obtaining alcohol was associated with higher odds of using more quantity of alcohol (OR = 6.63; P = .019).
Changes in context of AOD use compared with before the pandemic, and associations with mental health (Aim III)
Contextual factors associated with AOD use was largely unchanged for approximately half of the participants (SM5 for descriptives). When examining links between these contextual factors and mental health, logistic regressions demonstrated significant associations between depression and anxiety with changes in the context of AOD use (Figure 3). Adjusted ORs indicated that each increase in anxiety score (GAD) was associated with a significant 9% increase in the odds of using earlier in the day (P = .033), and due to boredom (P = .038). Each increase in depression score (PHQ) was associated with an 11% increase in using for enjoyment more often (P = .007), and a 9% increase in odds of using for loneliness more often (P = .016). There were no other significant associations (see SM5 for full table of results). Ease of obtaining substances differed by drug (SM1).
Figure 3.
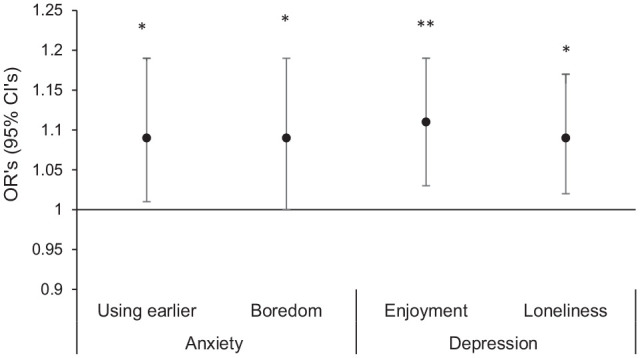
Adjusted ORs and 95% confidence intervals for the significant mental health associates of changes in the time spent engaging in contextual factors associated with AOD use following the pandemic. Contextual factors include using AOD earlier in the day, and using AOD more frequently to alleviate boredom, for enjoyment, and to alleviate loneliness (x axis: 1 = no change, comparator group). Greater anxiety was significantly associated with an increased odds of using AOD earlier in the day more often, and using for boredom more often. Greater depression was associated with significantly greater odds of using AOD for enjoyment more often, and to alleviate loneliness more often. *P < .05, **P < .010; see SM4 for full table of results.
Discussion
The current study aimed to understand the impact of the COVID-19 pandemic on (i) patterns of AOD use among clients who sought treatment for a SUD during the pandemic, (ii) mental health associates of changes in AOD use and (iii) changes in the contextual factors associated with AOD use. In a sample of recent treatment-seeking people, quantities of use increased for tobacco and cannabis following the pandemic. Self-reported frequency of cannabis use and other illicit drugs increased for the majority of these individuals, while frequency and quantity of methamphetamines decreased. Depression, anxiety and resilience were associated with changes in frequency of AOD use following the pandemic. Compared to AOD use before the pandemic, greater depression was associated with an increased frequency of alcohol use among clients, and using AOD more frequently for enjoyment and loneliness. Greater anxiety was associated with using cannabis less frequently. Regarding other substances, greater anxiety was also associated with using AOD earlier in the day and using for boredom more frequently following the pandemic. Resilience was most strongly linked with no change in the frequency of cannabis and methamphetamine use.
Retrospective estimates of AOD quantities used now compared to pre-pandemic were significantly increased for tobacco and cannabis, but estimates for alcohol and methamphetamines did not change. This partly supports prior reports that tobacco 33 and cannabis use15,33 use have increased following the pandemic. The lack of change in quantities of methamphetamine use may reflect market factors and the availability of the drug, where decreased availability has been cited as a common reason for using less. 17 The lack of change in the reported quantity of alcohol use in the current study does not concur with existing reports,8,14,15 however these previous studies are not within treatment-seeking populations. Prior researchers have proposed declines in AOD use following the pandemic in community and non-dependent samples, which are attributable to restricted social settings,16,34 compared with exacerbation of AOD use in dependent groups due to greater stress, financial pressure and uncertainty. 35 The current findings partly support this; however, alcohol use did not increase. This may suggest that alcohol use in treatment-seeking groups may differ to other non-treatment seeking substance-using populations, yet the non-probabilistic sample and small response rate in the current study limits generalisation to all people seeking treatment. It is also important to note that reported quantities of use in the current study were retrospective and recalled from 4 to 6 months prior to completing the survey, the accuracy of the pre-pandemic quantities may be susceptible to recall biases. Longitudinal assessments of AOD quantity that emerge following the pandemic will enable more definitive claims of individual change in AOD use among individuals in treatment for SUDs.
Reported changes in the perceived frequency and quantity of AOD use among the current participants following the pandemic differed across substances, and a subset of individuals reported using AODs more frequently and in higher quantities. The current findings indicated this may be attributable to different mental health risk factors and resilience. The association between depression and using alcohol more frequently indicates that low mood may be a risk factor for participants with alcohol use disorder following social distancing measures, including using alcohol to increase pleasure and cope with loneliness. Depression and loneliness during the pandemic have been argued to exert an impact on mental health and functioning,36,37 with heightened concerns for suicide risk in psychiatric and substance-using populations. 38 Loneliness has been correlated with depression and consequent risk for AOD use in young Americans during the pandemic period, 39 and the importance of social connection during the pandemic has been highlighted as pivotal in reducing harms associated with social distancing.40,41 Difficulty in obtaining cannabis was also associated with using more frequently, which may be because these individuals are needing to obtain the drug more often or needing higher quantities overall. AOD treatment and harm-reduction services should take extra precautions to alleviate social isolation and loneliness via regular meaningful contact with clients with SUDs.
In contrast, we found that greater anxiety predicted using cannabis less frequently now compared with before the pandemic. Cannabis is well-known for eliciting anxiety after acute 42 and chronic use, 43 and this finding may reflect using less frequently as a consequence of uncertainty around health during the pandemic period. Anxiety was also associated with using AOD earlier in the day more often, and using for boredom. Boredom may arise as a consequence of social distancing measures, and can be considered a stressor 44 that is associated with negative affect and depression. 45 Boredom is also a risk factor for relapse in SUDs.46,47 Strategies to enhance other rewarding activities in the social isolation environment during the pandemic period may serve to attenuate the negative impact of boredom on AOD use and low mood, with special consideration for participants seeking support who demonstrate high levels of anxiety.
An unexpected finding was that participants with lower resilience were more likely to use methamphetamine either less or more frequently. Resilience has previously been positively associated with less COVID-19-related stress, anxiety or depression. 48 Given that anxiety was also associated with less frequent cannabis use, it is possible that a subset of individuals with greater anxiety and reduced resilience experience a reduction in the frequency of use. Frequency and quantity of methamphetamine use may have also been affected by lower availability, as reported by 84% of people who reported using it in the current study. As the current study was cross-sectional, it is also possible that people who were experiencing changes in the frequency of cannabis or methamphetamine use may have experienced reduced resilience, as substance use is used as a coping mechanism throughout the pandemic.
Existing research has reported being anxious or depressed about COVID-19, loneliness, boredom, having more money, having more time and spending more time with others who inject drugs as the most common reasons given for increased use by people who inject substances. 17 The current study builds on this by demonstrating the role of mental health as associates of these, where depression, anxiety and resilience should be a primary consideration for assisting AOD treatment through the pandemic, given the increased rates of stress, financial pressures and social isolation. Mental health associates should be considered by treatment services throughout the pandemic via regular assessments with clients. Social-online or the continuation of mutual AOD support groups facilitated by telephones may also help reduce loneliness for this marginalised group.49,50
Prior researchers have suggested two long-term trajectories of AOD use as a consequence of the pandemic. 35 Declines in AOD use may be attributable to reduced social settings such as clubs and festivals.16,34 Conversely, exacerbation of AOD use in dependent groups may be attributable to greater stress, financial pressure and uncertainty. 35 The current study recruited people who had sought AOD treatment and reflects the latter group. These findings suggest that there are a subgroup of those, where important associates of changes in frequency of use include anxiety, depression and resilience, in addition to contextual factors (eg, loneliness and boredom). A large proportion of the sample did not experience changes to the frequency of use, and did not engage in more frequent AOD-related risk behaviours. This may indicate positive consequences of treatment during the pandemic, where greater efforts should be made to provide support and enrol new clients.
The study has several strengths and limitations. We recruited a sample of individuals who had sought AOD treatment in 2020, offering a unique opportunity to investigate the consequences of COVID-19 from this clinical perspective which can ultimately lead to enhanced care for SUDs. However, the small response rate (10%) may indicate selection biases that limit the generalisability of the findings, such as a self-selection bias and non-response bias. Further, a small and non-randomly stratified sample may limit the interpretability of the findings to a subsample of people seeking treatment through the pandemic. Nonetheless, the sample characteristics were representative of the full population of service client characteristics in terms of age, gender and mental health (normative data reported in SM2). Patterns of AOD use were lower than normative clients, yet the normative data reflects clients entering AOD treatment where it is expected that use would be higher. Alternatively, people with more severe use may have been less inclined to take part. Although some characteristics differed, the variation in relevant characteristics was sufficient to explore the aims of the study regarding the relation between mental health, contextual factors associated with AOD use and changes to AOD use during the pandemic. Our results may be underestimates given that individuals experiencing higher severity levels of psychological distress or substance use may be less likely to respond.
The current study highlighted the role of depression, anxiety and resilience in changes in the context and frequency of AOD use as a consequence of the pandemic, and emphasise the importance of different mental health concerns among people in treatment. People in treatment for AOD use problems are not a homogenous group, and these findings highlight the importance of understanding individual differences and contextual factors to reduce substance-related harms during the pandemic. Such research into the current pandemic climate is pivotal for informing treatment services internationally, where there are vast differences in social restrictions and the economic, health and social disruption caused by the COVID-19 pandemic is likely to be ongoing. This will likely have repercussions for the disease burden associated with substance use during a period where healthcare systems are already strained, but provide opportunities to enhance quality of life in AOD clients.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_11782218211061746 for Changes in Substance Use Among People Seeking Alcohol and Other Drug Treatment During the COVID-19 Pandemic: Evaluating Mental Health Outcomes and Resilience by Molly Carlyle, Janni Leung, Zoe C. Walter, Jennifer Juckel, Caroline Salom, Catherine A. Quinn, Lily Davidson, Rhiannon Ellem, Grace Newland and Leanne Hides in Substance Abuse: Research and Treatment
Acknowledgments
We would like to acknowledge Lives Lived Well, the collaborating treatment service, for facilitating the project.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by the Australian Government Department of Health awarded to the National Centre for Youth Substance Use Research (NCYSUR) under the Drug and Alcohol Prevention Programme. The funding source no involvement in the study design, collection, analysis and interpretation of data or writing of the report.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: MC, JL, ZCW, CAQ, and LH conceptualised and set up the project, analysed and interpreted the data, and contributed to writing of the manuscript. JJ, CS and LD assisted in the interpretation of the findings and writing of the manuscript. RE and GN assisted in the study set up, data collection, and interpreting the findings. All authors have read and approved the manuscript.
ORCID iDs: Molly Carlyle  https://orcid.org/0000-0002-8083-814X
https://orcid.org/0000-0002-8083-814X
Caroline Salom  https://orcid.org/0000-0002-8986-9735
https://orcid.org/0000-0002-8986-9735
Grace Newland  https://orcid.org/0000-0002-2414-2009
https://orcid.org/0000-0002-2414-2009
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Russell C, Ali F, Nafeh F, Rehm J, LeBlanc S, Elton-Marshall T. Identifying the impacts of the COVID-19 pandemic on service access for people who use drugs (PWUD): a national qualitative study. J Subst Abuse Treat. 2021;129:108374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jemberie WB, Stewart Williams J, Eriksson M, et al. Substance use disorders and COVID-19: multi-faceted problems which require multi-pronged solutions. Front Psychiatry. 2020;11:714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Milani F. COVID-19 outbreak, social response, and early economic effects: a global VAR analysis of cross-country interdependencies. J Popul Econ. 2020;34:223–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stanton R, To QG, Khalesi S, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17:1–13. doi: 10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boschuetz N, Cheng S, Mei L, Loy VM. Changes in alcohol use patterns in the United States during COVID-19 pandemic. WMJ. 2020;119:171–176. [PubMed] [Google Scholar]
- 6. Neill E, Meyer D, Toh WL, et al. Alcohol use in Australia during the early days of the COVID -19 pandemic: initial results from the COLLATE project. Psychiatry Clin Neurosci. 2020;74:542–549. Published online June 29, 2020. doi: 10.1111/pcn.13099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Correction: global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. JMIR Public Health Surveill. 2021;7:e31906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Naughton F, Ward E, Khondoker M, et al. Health behaviour change during the UK COVID-19 lockdown: findings from the first wave of the C-19 health behaviour and well-being daily tracker study. Br J Health Psychol. 2021;26:624–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Manthey J, Kilian C, Carr S, et al. Use of alcohol, tobacco, cannabis, and other substances during the first wave of the SARS-CoV-2 pandemic in Europe: a survey on 36,000 European substance users. Subst Abuse Treat Prev Policy. 2021;16:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mariottini C, Ojanperä I, Kriikku P. Increase in drugs-of-abuse findings in post-mortem toxicology due to COVID-19 restrictions—first observations in Finland. Drug Test Anal. 2021;13:867–870. [DOI] [PubMed] [Google Scholar]
- 11. van Laar MW, Oomen PE, van Miltenburg CJA, Vercoulen E, Freeman TP, Hall WD. Cannabis and COVID-19: reasons for concern. Front Psychiatry. 2020;11:601653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gupte HA, Mandal G, Jagiasi D. How has the COVID-19 pandemic affected tobacco users in India: lessons from an ongoing tobacco cessation program. Tob Prev Cessat. 2020;6:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cousijn J, Kuhns L, Larsen H, Kroon E. For better or for worse? A pre-post exploration of the impact of the COVID-19 lockdown on cannabis users. Addiction. 2021;116:2104–2115. Published online January 4, 2021. doi: 10.1111/add.15387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. European Monitoring Centre for Drugs and Drug Addiction and Europol. EU drug markets: impact of COVID-19. 2020. [Google Scholar]
- 15. Peacock A, Price O, Dietze P, et al. Impacts of COVID-19 and Associated Restrictions on People Who Use Illicit Stimulants in Australia: Preliminary Findings From the Ecstasy and Related Drugs Reporting System 2020. Drug Trends Bulletin Series. National Drug and Alcohol Research Centre, UNSW Sydney; 2020. [Google Scholar]
- 16. Sutherland R, Baillie G, Memedovic S, et al. Key findings from the ‘Australians’ Drug Use: Adapting to Pandemic Threats (ADAPT)’ study. ADAPT Bulletin No. 1. 2020. National Drug and Alcohol Research Centre, UNSW Sydney. [Google Scholar]
- 17. Daly C, Juckel J, Thomas N, Salom C. Australian Drug Trends 2019: Key Findings From the National Illicit Drug Reporting System (IDRS) Interviews. National Drug and Alcohol Research Centre, UNSW Sydney; 2020. [Google Scholar]
- 18. Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021;26:30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Plummer MP, Pellegrini B, Burrell AJ, Begum H, Trapani T, Udy AA. Smoking in critically ill patients with COVID-19: the Australian experience. Crit Care Resusc. 2020;22:281–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Da BL, Im GY, Schiano TD. Coronavirus disease 2019 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020;72:1102–1108. [DOI] [PubMed] [Google Scholar]
- 22. Melamed OC, Hauck TS, Buckley L, Selby P, Mulsant BH. COVID-19 and persons with substance use disorders: inequities and mitigation strategies. Subst Abuse. 2020;41:286–291. [DOI] [PubMed] [Google Scholar]
- 23. Bonsaksen T, Leung J, Schoultz M, et al. Cross-national study of worrying, loneliness, and mental health during the COVID-19 pandemic: a comparison between individuals with and without infection in the family. Healthcare. 2021;9:903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McKay D, Asmundson GJG. COVID-19 stress and substance use: current issues and future preparations. J Anxiety Disord. 2020;74:102274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67:354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ryan A, Holmes J, Hunt V, et al. Validation and implementation of the Australian treatment outcomes profile in specialist drug and alcohol settings. Drug Alcohol Rev. 2014;33:33–42. [DOI] [PubMed] [Google Scholar]
- 28. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder. Int Arch Med. 2006;166:1092–1097. [DOI] [PubMed] [Google Scholar]
- 30. Prins A, Bovin MJ, Smolenski DJ, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. 2016;31:1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. [DOI] [PubMed] [Google Scholar]
- 32. Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the PERI life events scale. J Health Soc Behav. 1978;19:205–229. [PubMed] [Google Scholar]
- 33. Salom C, Staton S, Coles L, Thorpe K. Understanding Social Impacts of COVID-19 Study (USIC). Institute for Social Science Research, UQ; 2020. [Google Scholar]
- 34. de Wit H, Sayette M. Considering the context: social factors in responses to drugs in humans. Psychopharmacology. 2018;235:935–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rehm J, Kilian C, Ferreira-Borges C, et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. 2020;39:301–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Policy. 2020;5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113:707–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID-19. J Psychoactive Drugs. 2021;53:1–9. [DOI] [PubMed] [Google Scholar]
- 40. Saltzman LY, Hansel TC, Bordnick PS. Loneliness, isolation, and social support factors in post-COVID-19 mental health. Psychol Trauma Theory Res Pract Policy. 2020;12:S55–S57. [DOI] [PubMed] [Google Scholar]
- 41. Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract. 2020;30;e3022008. doi: 10.17061/phrp3022008 [DOI] [PubMed] [Google Scholar]
- 42. Martin-Santos R, Crippa JA, Batalla A, et al. Acute effects of a single, oral dose of d9-tetrahydrocannabinol (THC) and cannabidiol (CBD) administration in healthy volunteers. Curr Pharm Des. 2012;18:4966–4979. [DOI] [PubMed] [Google Scholar]
- 43. Crippa JA, Zuardi AW, Martín-Santos R, et al. Cannabis and anxiety: a critical review of the evidence. Hum Psychopharmacol. 2009;24:515–523. [DOI] [PubMed] [Google Scholar]
- 44. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vodanovich SJ, Watt JD. Self-report measures of boredom: an updated review of the literature. J Psychol. 2016;150:196–228. [DOI] [PubMed] [Google Scholar]
- 46. Corvinelli A. Alleviating boredom in adult males recovering from substance use disorder. Occup Ther Ment Health. 2005;21:1–11. [Google Scholar]
- 47. Martínez-Vispo C, Senra C, López-Durán A, Fernández del Río E, Becoña E. Boredom susceptibility as predictor of smoking cessation outcomes: Sex differences. Pers Individ Dif. 2019;146:130–135. [Google Scholar]
- 48. Barzilay R, Moore TM, Greenberg DM, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry. 2020;10:291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liese BS, Monley CM. Providing addiction services during a pandemic: lessons learned from COVID-19. J Subst Abuse Treat. 2021;120:108156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bergman BG, Kelly JF. Online digital recovery support services: an overview of the science and their potential to help individuals with substance use disorder during COVID-19 and beyond. J Subst Abuse Treat. 2021;120:108152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_11782218211061746 for Changes in Substance Use Among People Seeking Alcohol and Other Drug Treatment During the COVID-19 Pandemic: Evaluating Mental Health Outcomes and Resilience by Molly Carlyle, Janni Leung, Zoe C. Walter, Jennifer Juckel, Caroline Salom, Catherine A. Quinn, Lily Davidson, Rhiannon Ellem, Grace Newland and Leanne Hides in Substance Abuse: Research and Treatment