Abstract
Several studies have found co-occurrence between substance abuse and mental health problems, as well as an association between treatment retention and psychological distress. The aim of this study was to investigate the association of possible protective factors with psychological distress. The present study tested physical activity, self-esteem and sense of coherence, and psychological distress level among inpatients in substance use treatment. The study design was cross-sectional and multicenter. Patients (N = 167) were recruited in 2018 from 10 Norwegian inpatient facilities. They self-reported on 3 validated measurement instruments: Rosenberg Self-Esteem Scale, Antonovsky’s Sense of Coherence Scale, and frequency of physical activity. The Hopkins Symptom Checklist-10 was used as an outcome variable of psychological distress. The associations were investigated with multiple linear and logistic regression methods. The results suggested that high self-esteem and sense of coherence were protective factors against high levels of psychological distress: self-esteem (β = −.39, P < .001) and sense of coherence (β = −.352, P < .001). The results offer support for a salutogenic approach in substance use disorder (SUD) treatment by enhancing individuals’ protective factors to reduce psychological distress.
Keywords: Inpatient treatment, protective factors, psychological distress, self-esteem, sense of coherence
Introduction
Substance use treatment drop-out and subsequent relapse is one of the major challenges in the field of substance abuse research. 1 Due to a lack of consensus on a definition of premature drop-out, the reported number of drop-outs varies with the different criteria. Brorson et al 2 reported a drop-out rate between 17% and 57%, whereas The Norwegian Health Directory reported that approximately 50% of patients in substance abuse inpatient treatment prematurely terminated their treatment stay. 3 Treatment retention has been found to have a positive association with treatment outcome, 4 which is one of the reasons for increased interest in research targeting drop-out.
There is a growing body of literature about possible factors that contribute to premature drop-out from inpatient treatment.2,5-11 The factors that contribute to predicting treatment retention fall into 2 main groups: treatment-related and patient-related characteristics. 10 One factor receiving increasing attention in the substance abuse disorder (SUD) literature is psychological distress in patients during treatment: several studies have found an association between high psychological and physiological stress levels and retention in inpatient substance abuse treatment.11-15 Research has found associations between stress and retention in inpatient substance abuse programs by using questionnaires that capture stress levels (eg, Symptom of Stress Inventory 13 ) and psychological distress (eg, Hopkins Symptom Checklist—HSCL).12-15
Findings from multiple studies over 25 years also testify to a general co-occurrence between substance use problems and mental health disorders, often referred to as dual diagnosis.15-19 The high co-occurrence between mental illness and substance abuse is in line with the self-medication hypothesis, an etiological explanation for co-occurring disorders.20-22 This hypothesis asserts that individuals use substances to relieve symptoms of mental or psychological distress and negative emotions. Hence, substance use or misuse could be interpreted as a maladaptive coping strategy, a lack of competence to cope with negative life events. 20
Possible protective factors of stress
The focus in the substance abuse literature has shifted from a focus on vulnerability and negative life events to a focus on what can promote recovery. 23 The focus on what promotes health, rather than on what causes disease, is in line with the salutogenic theory of Antonovsky.24-26 Important elements in salutogenic orientation view stimuli as challenges and see health as a continuum rather than as a dichotomy between “healthy” or “unhealthy.” 24
With an emphasis on salutogenic elements, Antonovsky developed the Sense of Coherence Scale (SOC) for measuring a person’s ability to cope with daily life stressors. 24 Findings from studies in substance abuse treatment settings have found positive associations between SOC and positive treatment outcomes.23,27,28 A Norwegian study found a 65% lower drop-out rate for patients with a normal SOC score than for patients with a lower score. 27 Another study found SOC to be a stable predictor of treatment retention and abstinence in heroin addicts. 28 A more recent cross-sectional study compared treatment-changers to non-treatment-changers, with a focus on the role of sense of coherence in recovery. 23 The authors of the study advocated that sense of coherence is more than a resource for coping with stress but can also be regarded as recovery capital in long-term recovery from substance addiction.
It has been suggested that sense of coherence, along with self-esteem and physical activity, work as protective factors against stress, and that these can function as protective moderators in the association between stress and negative health outcomes.29-31 Grant et al 32 reviewed 60 longitudinal studies on the association between stressors and psychological symptoms in adolescents. In 88% of the studies, a significant relationship was found. Many of the studies examined possible moderators of stress: gender, age, cognition, coping, and social support, among others. 32 Grant et al emphasized that many of the possible moderators that have been investigated are fixed, that is, they cannot be influenced by stressors. However, other factors linked to intrapersonal and interpersonal characteristics, such as self-esteem and sense of coherence, can change throughout life as a result of positive and negative experiences.33-35
Self-esteem (SE) is conceptualized as a positive or negative perception of self-worth. 36 As a negative perception, it has been found, in several studies, to be a predictor of alcohol and substance abuse problems. 37 Low self-esteem has been theorized to be one reason individuals seek ways to feel good about themselves, in line with the self-medication hypothesis. 38 Several studies have investigated the relationship between self-esteem and perceived stress, suggesting self-esteem as a possible moderator of stress.38,39 In a study from 2017, Reilly and co-workers used the Rosenberg Self-Esteem Scale (RSS) when investigating the relationship between self-esteem, personality, and perceived stress in individuals suffering from substance abuse who were living in recovery homes. 39 They found that a higher level of self-esteem and lower levels of perceived stress were associated with the personality trait Stability. 39 The RSS is the most widely used instrument measuring self-esteem, categorizing the results in 3 levels: low, medium, and high, although the global score is most used in research.36,40,41
It is well established that physical activity has several health benefits, including both physical and psychological health and wellbeing. 42 Studies have shown that individuals engaging in regular aerobic exercise have lower symptoms of anxiety and depression and are less likely to use illicit drugs.34,43,44 A recent cross-sectional study of adolescents in Spain found that engaging in physical activity was linked to lower psychological distress and that resilience and self-efficacy seemed to increase with physical activity. 45 Another study looked at physical activity and depression in men and found that increasing the duration and intensity of activity was associated with a reduction of depressive symptoms. 46 Self-report has been documented to be a reliable and valid method for assessment of physical activity. 47
Although there is a growing body of literature addressing the association between substance use, mental health, drop-out, and relapse, there are few studies that have investigated possible protective factors against psychological distress. A number of protective factors have been suggested,29-32 but, to our knowledge, no studies have investigated the relationship of the protective factors physical activity, sense of coherence, and self-esteem with psychological distress in substance abuse treatment inpatient settings. Findings from earlier studies indicate a relationship between psychological distress and relapse to substance use.1,48-51 Hence, with the aim of reducing drop-out and subsequent relapse, it is important to understand more about factors that contribute to psychological distress. Investigating dynamic factors, rather than static demographic factors, has the potential of identifying changeable factors that can be targeted for tailored treatment that results in improved outcomes.
In line with the recovery literature and positive psychology, the main aim of the present study, then, is to investigate 3 possible protective factors against psychological distress for inpatients in substance abuse treatment. To that end, we investigated whether physical activity (PA), self-esteem (SE), and sense of coherence (SOC) were protective factors against psychological distress and how these factors were associated with psychological distress level, measured with Hopkins Symptom Checklist 10 (HSCL-10). Our research questions were the following:
RQ1. Are there protective associations between physical activity, self-esteem, sense of coherence and psychological distress level?
RQ2. How accurately can measures of self-reported physical activity, self-esteem and sense of coherence explain a score above or below cut-off for severe psychological distress level?
Method
Study design and setting
The present study is a multicenter research study with a cross-sectional design. Ten inpatient clinics, offering treatment for substance addiction, agreed to participate. The clinics represent the largest treatment centers in the region of central Norway and cover most of the interdisciplinary specialized treatment provided in the country.
In Norway, having a substance use disorder (ICD-10) gives rights to treatment under the public health system, including free choice of hospital. Depending on the severity of substance use or life situation, patients can either seek out-patient treatment or apply for short- or long-term treatment at an inpatient facility. Referral is made by the specialized health services, general practitioners, or social services. For inpatient treatment, the patient is required to stay abstinent from substances during the stay and detoxification prior to intake is provided when needed. The 10 clinics included in this study are representative of the treatment options in Norway in general and builds upon a biopsychosocial understanding of addiction. They offer a combination of individual, milieu, and group therapy, as well as pharmacological treatment. The staff at each unit had multidisciplinary background, including psychologists, social workers, occupational therapists, nurses, physical therapists, and other trained staff. Individual adjustments to treatment are made according to patients’ needs and the main goal is to strengthen the individuals’ coping abilities in different settings. All programs also offered the opportunity to work out individually or in groups as part of the daily structure or as an option in the patients’ leisure time. Treatment length was from 2 to 6 months, with the possibility for extended stay and aftercare at the units offering long term treatment (>6 months).
The 10 units were contacted by email due to previous collaboration on research and development issues. It was considered that the 10 clinics would give a good representation of the different types of inpatient treatment options for substance addiction in Norway.
Recruitment and study participants
In order to get a representative sample of the clinical reality, the only inclusion criterion was admission. All study participants were above 18 years old.
Exclusion criteria: Patients in detoxification units and patients judged mentally or physically incapable of giving consent on the day of data collection. This decision was taken by clinical staff well acquainted with the actual person.
The patients were recruited in 2 steps. The staff of each institution first informed the patients about the study in general and that data collection would be conducted on a specific day. On this specific day, patients were asked to come to an information meeting, where they received both oral and written information about the study from one of the researchers (first author, KB). The questionnaires were then handed out to everyone participating in this meeting. They were informed that handing in the questionnaire served as a full consent for participation. The study was conducted from March to June 2018, when KB visited each institution and handed out and collected the questionnaires on the same day.
Measures
Five structured questionnaires written in Norwegian were used to collect data. Questionnaires were pen-and-pencil self-reports with predefined response alternatives for each question.
Sociodemographic form
We used a brief sociodemographic form developed for this study to obtain data concerning gender, age, substance use history, treatment history and psychiatric diagnosis (self-reported). The questions all had predefined categories, except for age and years of substance use. The predefined categories for substance use history were based on the classification from the Norwegian Directorate of Health 52 with the following categories: Alcohol, cannabis, stimulants, opioids, sedatives, solvents, and other. The respondents were asked to answer on a scale from “Never” to “Daily” for each substance or group of substances. This variable was then transferred to a continuous variable (Number of substances) for the analysis. The respondents were also asked how many years they have been addicted to substances (“How many years have you been addicted?”), how long they had been abstinent (predefined categories), and whether and how many times they had been admitted to inpatient treatment before. The questions about psychiatric diagnoses were transformed into a continuous variable (number of diagnoses) in the analysis.
Physical activity
Physical activity was assessed by self-report of frequency on 1 item with a 5-point scoring scale.31,47,53 The following question was formulated: “During the last four weeks, how many days a week did you engage in sports or physical activity so hard that you had high respiratory frequency, sweated, or had an increased heart rate for 20 minutes or more?” The response options were 1 (never), 2 (less than 1 day/week), 3 (1 day/week), 4 (2-3 days/week), and 5 (most days/week).
Self-esteem (SE)
The Norwegian translation 54 (10 items) of Rosenberg’s Self-Esteem Scale (RSE) was used to assess the level of self-esteem on a 4-point scale. RSE is a reliable and valid self-report instrument widely used for evaluation of self-esteem.41,54 The items were formed as positively or negatively words statements: “I certainly feel useless at times” from 1 = Strongly Agree to 4 = Strongly disagree. The RSE scale gives a sum score (global score) from 10 to 40, where a higher score indicates higher self-esteem. The global score can be divided into low score (10-25), medium score (26-29), and high score (30-40). 40 In the present study, the global score was used as the main criterion for interpreting the results of the RSE. The internal consistency was very high (Cronbach’s alpha = .87).
Sense of coherence (SOC)
The 13-item version (SOC-13) of Antonovsky’s Sense of Coherence Scale24,26 was used to measure sense of coherence. The scale measures a person’s ability to stabilize and make sense of oneself and others and is comprised of 3 components: cognitive (comprehensibility), behavioral (manageability), and motivational (meaningfulness). 55 The 13 items are presented as statements or questions where the respondent is asked to rate their feelings about them from 1 to 7, where 7 indicates extreme feelings. An example of a question from the scale is “When you talk to people, do you have the feeling that they do not understand you?,” and it is scored from 1 = never have this feeling to 7 = always have this feeling. The sum scores range from 13 to 91, where a higher score indicates higher sense of coherence. A sum score of 13 to 57 is considered low score; 58 to 74, medium score; and 75 to 91, high score. 56 In the present study the internal consistency of the SOC was .83 (Cronbach’s alpha).
Psychological distress
The outcome variable, psychological distress, was measured with the self-administered validated questionnaire Hopkins Symptom Checklist-10 (HSCL-10). 57 The patients completed the Norwegian version 58 of the 10-item scale to rate how frequently they had experienced symptoms of anxiety and depression during the past 7 days on a 4-point Likert scale, ranging from 1 (not at all) to 4 (extremely). The mean score was used as a continuous variable where high scores indicating severe mental distress. We also created a dichotomous variable for having an average score above 1.85, which is considered as a valid cut-off value for prediction of psychological distress. 58 In this study the internal consistency of the HSCL-10 was .88 (Cronbach’s alpha).
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics 27. Statistical significance was set to the P < .05 level. For categorical variables, descriptive statistics are presented as frequency distributions. For continuous variables, means, and SDs are presented. Normality of instrument measures was evaluated by inspection of normal probability plots.
Multiple linear regression was used to evaluate the impact of the explanatory variables (PA, SE, and SOC) on the sum score of the outcome variable, psychological distress (HSCL-10) (RQ1). The following variables were included as covariates: gender, age, time of abstinence from drugs, numbers of substances used, self-reported diagnoses, and long-term treatment.
Multiple logistic regression was performed to assess the association between physical activity, self-esteem, and sense of coherence, and a HSCL-10 score over or under cut-off (1.85) (RQ2). The same covariates as the multiple regression were used: gender, age, time of abstinence from drugs, numbers of substances used, the number of self-reported diagnoses and long-term treatment (yes/no). The variable time in treatment was not included in the regression analysis due to high missing percent (21%).
For the multiple linear regression, the assumption of normality of the residuals was studied by a normality probability plot. For both the linear and logistic regression, possible violations of linearity and homoscedasticity was studied by residual plots. Multicollinearity was examined based on variance inflation factors (VIF). VIF-scores ranged from 1.081 to 2.209, indicating no issue with multicollinearity. Possible influential cases were studied with Cook’s Distance, with no outliers detected. This was inspected separate for both regression models, with the criteria set to greater than 1.00.
Results
A total of 175 questionnaires were handed out and 167 were returned (response rate 95%). The sample featured 76% men (n = 127) and 21% women (n = 35). Age varied from 19 to 67 years, with a mean of 35.58 (SD = 10.12).
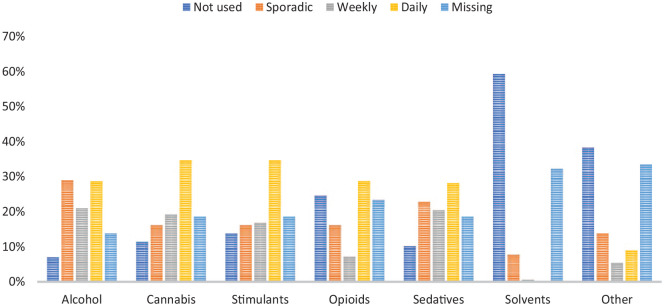
Figure 1 shows an overview of the substances that had been used prior to admission to the present inpatient stay. The most common substances used daily were cannabis (n = 58, 35%), stimulants (n = 58, 35%), alcohol (n = 48, 29%), opioids (n = 48, 29%), and sedatives (n = 47, 28%). Seventy-two percent (n = 120) of the respondents reported using more than 1 substance daily or weekly (polysubstance use), and 47% (n = 79) reported 3 or more substances daily or weekly.
Figure 1.
Substances used before admission to the current treatment stay.
For abstinence from substance use, 15.6% (n = 26) had been abstinent for a short time (less than 3 weeks); 63.5% (n = 106), for a medium amount of time (1-9 months); and 20.4% (n = 34), for long time (1 year or more).
Seventy-four percent (n = 123) of the sample reported that they had at least 1 psychiatric diagnosis. The most common self-reported diagnoses were anxiety (41%, n = 68), ADHD (30%, n = 50), depression (26%, n = 44), and PTSD (23%, n = 38); and 41% (n = 69) reported having 2 or more psychiatric diagnoses, 32% (n = 54) having only one diagnosis, and 26% (n = 44) reported 0 diagnoses.
Of the 167 respondents, 34% (n = 57) had been admitted to short-term inpatient treatment (<2 months) and 66% (n = 110) were in long-term treatment (>2 months). For the variable time in treatment (n = 132), 6% (n = 10) reported to have been in treatment for less than 3 weeks, 60% (n = 100) for 1 to 9 months, and 13.2% (n = 22) had been admitted for more than 1 year.
Physical activity (PA): 12% reported that they had never worked out during the past month, and most of the respondents (40%) had worked out between 1 and 3 days/week; 18.6% reported working out 4 to 5 days/week; and 6.6%, as much as 6 to 7 days/week.
Self Esteem (SE)/Rosenberg Self-Esteem Scale: Mean score for the sample was 26.19 (SD = 5.03; 95% CI = 25.39-26.93), which is considered to be at the lower end of the medium level of self-esteem.36,40,41
Antonovsky’s Sense of Coherence Scale (SOC): Mean score in our sample was 51.19 (SD = 13.15; 95% CI = 49.18-53.20), indicating low sense of coherence.
Psychological distress (HSCL-10)
Mean score on the HSCL-10 in our sample (N = 167), was 2.14 (SD = .66), which is over the cut-off at 1.85 for severe psychological distress. Dividing the sample into over or below cut-off at 1.85, the number of respondents having a score above 1.85 were 96 (59.6%). The score on HSCL-10 was used as a continuous variable for RQ1 and dichotomous variable (over/below cut-off) for RQ2.
RQ1. Are there protective associations between physical activity and self-esteem and sense of coherence and psychological distress levels?
Linear multiple regression was used to assess the association between possible protective factors against stress (physical activity, self-esteem, and sense of coherence) and levels of psychological distress (HSCL-10). We entered the following covariates: gender, age, long-term treatment, number of substances, abstinence, and number of diagnoses.
All variables were entered into the model simultaneously. A significant regression equation was found (F [9,144] = 28.301, P < .001) with an R 2 of .64, which means that 64% of the total variance in psychological distress is explained by the model.
RQ1 (Table 1) was partially confirmed for 2 of the protective factors: self-esteem and sense of coherence. They had a significant (P < .001) unique contribution of protection against psychological distress as measured by the HSCL-10. The largest β was −.417, for self-esteem, with sense of coherence reaching the value of β = −.327.
Table 1.
Multiple linear regression analysis of sociodemographic variables, self-reported physical activity, sense of coherence, and self-esteem as explanatory variables and psychological distress (HSCL-10) as outcome variable. .
| Model | Coefficients a | ||||||
|---|---|---|---|---|---|---|---|
| Unstandardized coefficients | Standardized coefficients | t | Significance | 95% Confidence interval for B | |||
| B | Std. error | β | Lower bound | Upper bound | |||
| (Constant) | 3.960 | 0.268 | 14.768 | .000 | 3.430 | 4.490 | |
| Gender | .191 | 0.085 | .120 | 2.249 | .026 | 0.023 | 0.358 |
| Age | .010 | 0.004 | .156 | 2.811 | .006 | 0.003 | 0.017 |
| Number of substances | .037 | 0.032 | .067 | 1.180 | .240 | −0.025 | 0.100 |
| Abstinence | −.072 | 0.058 | −.065 | −1.242 | .216 | −0.186 | 0.042 |
| Long-term treatment | .085 | 0.081 | .062 | 1.052 | .294 | −0.075 | 0.246 |
| Number of diagnoses | .099 | 0.027 | .198 | 3.650 | .000 | 0.046 | 0.153 |
| Physical activity (PA) | −.036 | 0.032 | −.058 | −1.115 | .267 | −0.100 | 0.028 |
| Self-esteem (SE) | −.055 | 0.010 | −.417 | −5.607 | .000 | −0.074 | −0.035 |
| Sense of coherence (SOC) | −.016 | 0.004 | −.327 | −4.242 | .000 | −0.024 | −0.009 |
Dependent variable: Psychological Distress (HSCL-10).
The third possible protective factor, physical activity, did not reach statistical significance, and thus did not make a significant unique contribution to the variance of predicted psychological distress (HSCL-10).
Of the background variables, age, gender, and number of diagnoses were significant (P < .05). They all had a small, but positive association with HSCL-10. Numbers of diagnoses had the strongest association of these variables (β = .198). The covariates long-term treatment, abstinence, and number of substances did not reach statistical significance (P > .05).
RQ2. How accurate can measures of self-reported physical activity, self-esteem and sense of coherence differentiate between a score above or below cut-off for severe psychological distress level?
Table 2 presents the explanatory variables and Exp (B) for the logistic regression with “Above cut-off” as the outcome variable. The model contained the same independent variables as the linear regression model: Gender, age, long-term treatment, abstinence, number of substances, physical activity, self-esteem, and sense of coherence.
Table 2.
Multivariate logistic regression with age, sex, self-reported physical activity, self-esteem, and sense of coherence as explanatory variables and above cut-off (mean score of 1.85) on the HSCL-10 as the outcome variable.
| Variables in the equation | ||||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | Wald | df | Significance | Exp (B) | 95% CI for Exp (B) | ||
| Lower | Upper | |||||||
| Step 1 a | ||||||||
| Gender (1) | −.947 | 0.712 | 1.769 | 1 | .183 | .388 | 0.096 | 1.566 |
| Age | .005 | 0.029 | 0.029 | 1 | .865 | 1.005 | 0.949 | 1.064 |
| Number of substances | −.316 | 0.240 | 1.736 | 1 | .188 | .729 | 0.455 | 1.167 |
| Long-term treatment (1) | −.509 | 0.640 | 0.631 | 1 | .427 | .601 | 0.171 | 2.110 |
| Abstinence | 2.493 | 2 | .287 | |||||
| Abstinence(1) | 1.348 | 0.854 | 2.491 | 1 | .115 | 3.848 | 0.722 | 20.520 |
| Abstinence (2) | .494 | 0.615 | 0.645 | 1 | .422 | 1.639 | 0.491 | 5.469 |
| Number of diagnoses | .576 | 0.258 | 4.994 | 1 | .025 | 1.780 | 1.073 | 2.950 |
| Self-Esteem (SE) | −.232 | 0.089 | 6.740 | 1 | .009 | .793 | 0.666 | 0.945 |
| Sense of Coherence (SOC) | −.090 | 0.029 | 9.862 | 1 | .002 | .914 | 0.864 | 0.967 |
| Physical Activity (PA) | −.070 | 0.241 | 0.084 | 1 | .772 | .933 | 0.582 | 1.495 |
| Constant | 11.774 | 2.986 | 15.550 | 1 | .000 | 129 887.548 | ||
Variable(s) entered on Step 1: gender, age, number of substances, long-term treatment, abstinence, number of diagnoses, self-esteem (SE), sense of coherence (SOC), physical activity (PA).
The full model containing all predictors was statistically significant, χ 2 (10, N = 142) = 84.71, P < .001, indicating that the model was able to distinguish between respondents who scored under and over cut-off (1.85) on the HSCL-10. The whole model explained 44.9% (Cox and Snell R 2 ) and 60.4% (Nagelkerke R 2 ) of the variance in HSCL-10 and correctly classified 79% of all cases. The Hosmer and Lemeshow Test also supported that the goodness of fit between observed and expected variance was good, with a non-significant value of .441.
The strongest predictor of having a HSCL-10 score above cut-off was the covariate number of substances (P < .05), recording an odds ratio of 1.78. The exploratory variables self-esteem and sense of coherence were also significant (P > .05) with odds ratios of .79 and .91, respectively. The exploratory variable physical activity did not yield statistical significance (P > .05). None of the covariates, except number of substances, was significant in the logistic model.
Discussion
In this cross-sectional study, we investigated the association between the possible protective factors of stress—physical activity, self-esteem, and sense of coherence—and psychological distress, measured with HSCL-10. Findings from multiple linear regression and logistic regression suggested that high scores on self-esteem and sense of coherence significantly lowered the degree of psychological distress. On the other hand, being a man, older age and number of psychiatric diagnoses were associated with an increase of psychological distress in the linear model. There were no significant findings for physical activity associated with levels of psychological distress, in either of the models.
A large portion of patients with SUD have co-occurring psychiatric disorders or suffer from high levels of psychological distress. 1 In addition to self-report of psychiatric diagnoses, the Hopkins Symptom Checklist (HSCL-10) was used, which has a cut-off at 1.85, for substantial symptoms of anxiety and depression. The mean score was 2.14 (SD = .66) in our sample and 96 respondents (59.6%) had a HSCL-10 score above the cut-off at 1.85. Hence, it is not a surprise that 74% of the respondents reported having a psychiatric diagnosis and is in line with previous research on the SUD population. 15 Having a psychiatric disorder is also associated with increased risk of relapse.1,15 In accordance with the recovery literature, 59 this study focused on possible factors that can moderate psychological distress.
The research on protective factors for stress has escalated in the past decades, and several possible moderators have been suggested. 32 This study focused on the possible protective factors physical activity (PA), self-esteem (SE), and sense of coherence (SOC). The descriptive statistics revealed that most of the respondents reported weekly physical activity, and the mean scores for SE and SOC were in the lower end of medium and low scores, respectively. Low to medium scores on SE and SOC are in line with research showing an association between these factors and risk of substance abuse 37 and recovery.27,28
This suggests that both SE and SOC can work as protective factors against psychological distress. High SE and SOC might protect you from experiencing a situation as stressful; the same event might be less stressful for an individual with high SE and SOC scores than for an individual with lower scores. In previous studies, SOC has been found to be a stable predictor of treatment outcome,23,27,28 and our findings hence support a salutogenic approach to treatment and recovery.
The variable physical activity did not reach a significant statistical effect on psychological distress, and no conclusion can therefore be drawn about this variable. However, there is a large body of evidence indicating that physical activity is good for mental health. 42
Strengths and limitations
This study has several strengths. The cross-sectional design made it possible to get a sufficiently large and representative sample size concerning: The variety of institutions, located across Norway with a mix of urban and non-urban areas, and with both long-term and short-term treatment. A variety regarding patient characteristics, polysubstance use, age, and gender reflected the diversity of the general inpatient treatment population. The high response rate (95%) is also an advantage, concerning internal validity and representativity. The same goes for the use of valid and reliable instruments for explanatory and outcome variables. The findings of the dynamic protective factors are in line with previous research, and this focus makes it possible to develop interventions to target improvement of these factors during the course of treatment.
Based on the number of patients attending the information meeting, the response rate was high (95%). Since it was up to the staff at each unit to recruit patients on the day of data collection, we do not know how many of the admitted patients attended this meeting. This leaves an uncertainty as to whether there were more patients eligible for recruitment and, if so, why they did not attend the information meeting. Still, it was important for us to implement the study this way in order to present correct information and secure anonymity for the participants.
Measures of physical activity did not reach statistical significance. This may be explained by the following 3 possible problems with the variable: First, only one item was used, and this limited the score distribution. Second, there still might be subjective interpretations in defining feeling of physical activity and third, the 1-item scale did not differentiate between aerobic and anaerobic exercise.
This study failed to provide the length of time in current treatment variable for 2 institutions because of the entry of this item took place after these 2 institutions had finished the survey. This caused 21% missing responses for this item and was therefore not included in the regression model. To control for another aspect of treatment time, the comparison of long-term (>2 months) versus short-term (<2 months) treatment was conducted. However, no significant difference was found.
This study only measured self-reported patient characteristics in relation to stress. In order to correct for social desirability and treatment-related reasons for psychological distress, monitoring possible biological explanatory variables and characteristics that target the social environment at the treatment site should have been included.
Implications
Despite its limitations, our study has several implications for further research and treatment. Based on the earlier identification of psychological distress as a risk factor for relapse and recurrence of substance abuse, and our protective factors SE and SOC, pre-treatment assessment with these instruments could possibly allow for immediate identification of possible clinical needs and/or treatment provisions. Increased understanding of the long-term associations between psychological distress and possible protective factors, polysubstance use, and time in treatment may contribute to more suitable pre-treatment assessments, treatment interventions, individually tailored treatment, and follow-up initiatives. This suggests possibilities for targeted and more individualized therapy focused on self-esteem and sense of coherence in both individual and milieu treatment. It also suggests potential for assisting treatment staff to better understand and build more emphatic relationships with individual patients and to inform tailored treatment plans.
Due to the cross-sectional design, all factors were measured simultaneously and the results do not imply causality. Future studies using a prospective design should investigate the association between protective factors and psychological distress at different timepoints during treatment. A comparison of stress levels in different treatment types, in respect to treatment length, during the course of treatment is also of interest. Toward the aim of developing more comprehensive understanding and efficient treatment, research should also strive to investigate the possible impact of biological and social factors, such as monitoring stress hormones and ward atmosphere. Combined with psychological factors, these may produce an informative bio-psycho-social model.
Conclusion
Psychological distress has been found to be a risk factor for drop-out and relapse in SUD treatment. Our results suggest that self-esteem and a sense of coherence might be protective factors for reducing psychological distress among SUD patients. Because of the cross-sectional design, we could not analyze the association between psychological distress and drop-out and relapse in this study. Still, therapy in SUD treatment may want to further focus on self-esteem and sense of coherence to help develop protective factors against psychological distress. Such a focus may build coping capacity and reduce the risk of recurrence and relapse.
Acknowledgments
We wish to thank all the patients for their contribution to this research. We also wish to express our particular thanks to the staff from all the clinics that participated for their contribution to the implementation of the study.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by grant from The Liaison Committee for Education (46055500-23), Research and Innovation in Central Norway.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: EO designed the study and wrote the protocol prior to funding with contributions from SKB. KB had the responsibility for implementation of the study and drafted the manuscript. KB took the main responsibility for the statistical analysis, under the guidance of EO and SKB. All authors contributed to the revision of the manuscript and have approved the final version.
Disclosure and Ethics: The authors declare that there is no conflict of interest and have provided the publisher with a signed confirmation of compliance with legal and ethical obligations. The study was approved by the Regional Committee for Medical Research Ethics in Central Norway in January 2018 (Approval # 2017/2058/REK-Midt).
ORCID iD: Kari Bøhle  https://orcid.org/0000-0001-7187-4010
https://orcid.org/0000-0001-7187-4010
References
- 1. Andersson HW, Wenaas M, Nordfjærn T. Relapse after inpatient substance use treatment: a prospective cohort study among users of illicit substances. Addict Behav. 2019;90:222-228. [DOI] [PubMed] [Google Scholar]
- 2. Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33:1010-1024. [DOI] [PubMed] [Google Scholar]
- 3. The Norwegian Directorate of Health. Rusbehandling - avbrudd i behandlingen - Helsedirektoratet. Accessed May 11, 2021. https://www.helsedirektoratet.no/statistikk/kvalitetsindikatorer/rusbehandling/avbrudd-i-tverrfaglig-spesialisert-rusbehandling
- 4. Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673-684. [DOI] [PubMed] [Google Scholar]
- 5. Stark MJ. Dropping out of substance abuse treatment: a clinically oriented review. Clin Psychol Rev. 1992;12:93-116. [Google Scholar]
- 6. Li X, Sun H, Purl A, Marsh DC, Anis AH. Factors associated with pretreatment and treatment dropouts among clients admitted to medical withdrawal management. J Addict Dis. 2007;26:77-85. [DOI] [PubMed] [Google Scholar]
- 7. López-Goñi JJ, Fernández-Montalvo J, Illescas C, Landa N, Lorea I. Determining socio-demographic predictors of treatment dropout: results in a therapeutic community. Int J Soc Welf. 2008;17:374-378. [Google Scholar]
- 8. López-Goñi JJ, Fernández-Montalvo J, Arteaga A. Addiction treatment dropout: exploring patients’ characteristics. Am J Addict. 2012;21:78-85. [DOI] [PubMed] [Google Scholar]
- 9. Baekeland F, Lundwall L. Dropping out of treatment: a critical review. Psychol Bull. 1975;82:738-783. [DOI] [PubMed] [Google Scholar]
- 10. Darke S, Campbell G, Popple G. Retention, early dropout and treatment completion among therapeutic community admissions. Drug Alcohol Rev. 2012;31:64-71. [DOI] [PubMed] [Google Scholar]
- 11. Andersson HW, Steinsbekk A, Walderhaug E, Otterholt E, Nordfjærn T. Predictors of dropout from inpatient substance use treatment: a prospective cohort study. Subst Abuse Res Treat. 2018;12:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Simpson DD, Joe GW, Rowan-Szal GA, Greener JM. Drug abuse treatment process components that improve retention. J Subst Abuse Treat. 1997;14:565-772. [DOI] [PubMed] [Google Scholar]
- 13. Marcus MT, Schmitz J, Moeller FG, et al. Stress and length of stay in therapeutic community treatment for adolescents with substance use disorders. Addict Disord Their Treat. 2013;12:175-182. [Google Scholar]
- 14. Hassel A, Nordfjærn T, Hagen R. Psychological and interpersonal distress among patients with substance use disorders: are these factors associated with continued drug use and do they change during treatment? J Subst Use. 2013;18:363-376. [Google Scholar]
- 15. Burdzovic Andreas J, Lauritzen G, Nordfjaern T. Co-occurrence between mental distress and poly-drug use: a ten year prospective study of patients from substance abuse treatment. Addict Behav. 2015;48:71-78. [DOI] [PubMed] [Google Scholar]
- 16. Bray JW, Aden B, Eggman AA, et al. Quality of life as an outcome of opioid use disorder treatment: a systematic review. J Subst Abuse Treat. 2017;76:88-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morisano D, Babor TF, Robaina KA. Co-occurrence of substance use disorders with other psychiatric disorders: implications for treatment services. Nord Stud Alcohol Drugs. 2014;31:5-25. [Google Scholar]
- 18. Henwood B, Padgett DK. Reevaluating the self-medication hypothesis among the dually diagnosed. Am J Addict. 2007;16:160-165. [DOI] [PubMed] [Google Scholar]
- 19. Andersen SL, Teicher MH. Desperately driven and no brakes: developmental stress exposure and subsequent risk for substance abuse. Neurosci Biobehav Rev. 2009;33:516-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nordfjaern T, Hole R, Rundmo T. Interrelations between patients’ personal life events, psychosocial distress, and substance use. Subst Use Misuse. 2010;45:1161-1179. [DOI] [PubMed] [Google Scholar]
- 21. Khantzian EJ, Mack JE, Schatzberg AF. Heroin use as an attempt to cope: clinical observations. Am J Psychiatr. 1974;131:160-164. [DOI] [PubMed] [Google Scholar]
- 22. Suh JJ, Ruffins S, Robins CE, Albanese MJ, Khantzian EJ. Self-medication hypothesis: connecting affective experience and drug choice. Psychoanal Psychol. 2008;25:518-532. [Google Scholar]
- 23. Chen G, Gueta K. Sense of coherence as a recovery capital in recovery from substance use disorders. J Addict Dis. 2020;38:529-539. [DOI] [PubMed] [Google Scholar]
- 24. Antonovsky A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. Jossey-Bass; 1987. [Google Scholar]
- 25. Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promot Int. 1996;11:11-18. [Google Scholar]
- 26. Torsheim T, Wold B. Adolescent coping and health: sense of coherence. In: Currie C (ed.), Health behaviour in school-aged children. Research protocol for the 1997–98 Survey. University of Edinburgh, Edinburgh; 1998: 79-83. [Google Scholar]
- 27. Andersen S, Berg JE. The use of a sense of coherence test to predict drop-out and mortality after residential treatment of substance abuse. Addict Res Theory. 2001;9:239-251. [Google Scholar]
- 28. Abramsohn Y, Peles E, Potik D, Schreiber S, Adelson M. Sense of coherence as a stable predictor for methadone maintenance treatment (MMT) outcome. J Psychoactive Drugs. 2009;41:249-253. [DOI] [PubMed] [Google Scholar]
- 29. Compas BE, Reeslund KL. Processes of risk and resilience during adolescence. In: Lerner RM, Steinberg L (eds) Handbook of Adolescent Psychology: Individual bases of adolescent development. John Wiley & Sons, Inc; 2009:561-588. [Google Scholar]
- 30. Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY. Stressors and child and adolescent psychopathology: measurement issues and prospective effects. J Clin Child Adolesc Psychol. 2004;33:412-425. [DOI] [PubMed] [Google Scholar]
- 31. Moksnes UK. Stress and Health in Adolescents: The Role of Potential Protective Factors. NTNU; 2011.
- 32. Grant KE, Compas BE, Thurm AE, et al. Stressors and child and adolescent psychopathology: evidence of moderating and mediating effects. Clin Psychol Rev. 2006;26:257-283. [DOI] [PubMed] [Google Scholar]
- 33. Schäfer SK, Schanz CG, Sopp MR, Lass-Hennemann J, Käfer M, Michael T. Pre-rehabilitation sense of coherence as a predictor of symptom change after rehabilitation. Stress Health. 2020;36:546-554. [DOI] [PubMed] [Google Scholar]
- 34. Ekeland E, Heian F, Hagen KB. Can exercise improve self esteem in children and young people? A systematic review of randomised controlled trials. Br J Sports Med. 2005;39:792-798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ellingsen MM, Johannesen SL, Martinsen EW, Hallgren M. Effects of acute exercise on drug craving, self-esteem, mood and affect in adults with poly-substance dependence: feasibility and preliminary findings. Drug Alcohol Rev. 2018;37:789-793. [DOI] [PubMed] [Google Scholar]
- 36. Rosenberg M, Schooler C, Schoenbach C, Rosenberg F. Global self-esteem and specific self-esteem: different concepts, different outcomes. Am Sociol Rev. 1995;60:141. [Google Scholar]
- 37. Samuels DJ, Samuels M. Low self-concept as a cause of drug abuse. J Drug Educ. 1974;4:421-438. [Google Scholar]
- 38. Carters MA, Byrne DG. The role of stress and area-specific self-esteem in adolescent smoking. Aust J Psychol. 2013;65:180-187. [Google Scholar]
- 39. Reilly A, Stevens EB, Jason LA. Personality, self-esteem, and perceived stress in communal residences supporting recovery. J Drug Educ. 2017;47:108-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. García JA, Y Olmos FC, Matheu ML, Carreño TP. Self esteem levels vs global scores on the Rosenberg self-esteem scale. Heliyon. 2019;5:e01378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rosenberg M. Society and the adolescent self-image. Science. 1965;148:10-1126. [Google Scholar]
- 42. Sfendla A, Hadrya F. Factors associated with psychological distress and physical activity during the COVID-19 pandemic. Health Secur. 2020;18:444-453. [DOI] [PubMed] [Google Scholar]
- 43. Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61. [DOI] [PubMed] [Google Scholar]
- 44. Jerstad SJ, Boutelle KN, Ness KK, Stice E. Prospective reciprocal relations between physical activity and depression in female adolescents. J Consult Clin Psychol. 2010;78:268-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. San Román-Mata S, Puertas-Molero P, Ubago-Jiménez JL, González-Valero G. Benefits of physical activity and its associations with resilience, emotional intelligence, and psychological distress in university students from southern Spain. Int J Environ Res Public Health. 2020;17:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Currier D, Lindner R, Spittal MJ, Cvetkovski S, Pirkis J, English DR. Physical activity and depression in men: increased activity duration and intensity associated with lower likelihood of current depression. J Affect Disord. 2020;260:426-431. [DOI] [PubMed] [Google Scholar]
- 47. Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1-14. [PubMed] [Google Scholar]
- 48. Dodge R, Sindelar J, Sinha R. The role of depression symptoms in predicting drug abstinence in outpatient substance abuse treatment. J Subst Abuse Treat. 2005;28:189-196. [DOI] [PubMed] [Google Scholar]
- 49. Blaine SK, Sinha R. Alcohol, stress, and glucocorticoids: from risk to dependence and relapse in alcohol use disorders. Neuropharmacol. 2017;122:136-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Daughters SB, Richards JM, Gorka SM, Sinha R. HPA axis response to psychological stress and treatment retention in residential substance abuse treatment: a prospective study. Drug Alcohol Depend. 2009;105:202-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology. 2001;158:343-359. [DOI] [PubMed] [Google Scholar]
- 52. The Norwegian Directorate of Health. 2.2 Rusmidlenes virkninger - Nasjonal faglig retningslinje for utredning, behandling og oppfølging av personer med samtidig ruslidelse og psykisk lidelse – ROP-lidelser. Accessed May 11, 2021. https://www.helsebiblioteket.no/retningslinjer/rop/2-definisjoner-metode/2.2-rusmidlenes-virkninger
- 53. Moksnes UK, Moljord IEO, Espnes GA, Byrne DG. Leisure time physical activity does not moderate the relationship between stress and psychological functioning in Norwegian adolescents. Ment Health Phys Act. 2010;3:17-22. [Google Scholar]
- 54. von Soest T. Rosenbergs selvfølelsesskala: validering av en norsk oversettelse|Tidsskrift for Norsk psykologforening. J Norwegian Psychol Assoc. 2005;42:226-228. [Google Scholar]
- 55. Eriksson M, Lindström B. Antonovsky’s sense of coherence scale and its relation with quality of life: a systematic review. J Epidemiol Community Health. 2007;61:938-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Holmefur M, Sundberg K, Wettergren L, Langius-Eklöf A. Measurement properties of the 13-item sense of coherence scale using Rasch analysis. Qual Life Res. 2015;24:1455-1463. [DOI] [PubMed] [Google Scholar]
- 57. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1-15. [DOI] [PubMed] [Google Scholar]
- 58. Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry. 2003;57:113-118. [DOI] [PubMed] [Google Scholar]
- 59. Kramer MM, Londgren J. Recovery’s got talent: a positive-psychology intervention for people living in recovery. Health Promot Pract. 2020;21:862-864. [DOI] [PubMed] [Google Scholar]