Abstract
Background
During the Coronavirus disease 2019 pandemic, ambulatory pediatric rheumatology healthcare rapidly transformed to a mainly telehealth model. However, pediatric patient and caregiver satisfaction with broadly deployed telehealth programs remains largely unknown. This study aimed to evaluate patient/caregiver satisfaction with telehealth and identify the factors associated with satisfaction in a generalizable sample of pediatric rheumatology patients.
Methods
Patients with an initial telehealth video visit with a rheumatology provider between April and June 2020 were eligible. All patients/caregivers were sent a post-visit survey to assess a modified version of the Telehealth Usability Questionnaire (TUQ) and demographic and clinical characteristics. TUQ total and sub-scale (usefulness, ease of use, effectiveness, satisfaction) scores were calculated and classified as “positive” based on responses of “agree” or “strongly agree” on a 5-point Likert scale. Results were analyzed using standard descriptive statistics and Wilcoxon signed rank testing. The association between demographic and clinical characteristics with TUQ scores was assessed using univariate linear regression.
Results
597 patients/caregivers met inclusion criteria, and the survey response rate was 42% (n = 248). Juvenile idiopathic arthritis was the most common diagnosis (33.5%). The majority of patients were diagnosed greater than 6 months previously (72.6%) and were prescribed chronic medications (59.7%). The median total TUQ score was 4 (IQR: 4–5) with positive responses in 81% of items. Of the subscales, usefulness scores were lowest (median: 4, p < 0.001). Telehealth saves time traveling was the highest median item score (median = 5, IQR: 4–5). Within subscales, items that scored significantly lower included convenience, providing for needs, seeing rheumatologist as well as in person, and being an acceptable way to receive rheumatology services (all p < 0.001). There were no significant demographic or clinical features associated with TUQ scores.
Conclusions
Our results suggest telehealth is a promising mode of healthcare delivery for pediatric rheumatic diseases but also identifies opportunities for improvement. Innovation and research are needed to design a telehealth system that delivers high quality and safe care that improves healthcare outcomes. Since telehealth is a rapidly emerging form of pediatric rheumatology care, improved engagement and training of patients, caregivers, and providers may help improve the patient experience in the future.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12969-021-00649-4.
Keywords: COVID-19, Patient satisfaction, Telehealth, Telehealth usability questionnaire, Pediatric rheumatology
Background
In the wake of the Coronavirus disease 2019 (COVID-19) pandemic, ambulatory pediatric rheumatology healthcare delivery rapidly transformed to a mainly telehealth model at many centers using telephone and web-based video platforms [1]. Optimally used, telehealth may improve access to care, reduce time traveling to and from office visits, and improve cost-effectiveness. Potential drawbacks may include lower quality patient/clinician interactions and less accurate medical assessments [2, 3]. Given its widespread implementation and perceived feasibility [3], telehealth will be more commonly used in the future. However, the impact on patient satisfaction in pediatric rheumatology is unknown.
While telehealth has been examined in adult rheumatology and other pediatric subspecialties [4–6], studies characterizing and assessing pediatric rheumatology telehealth implementation are sparse and were conducted prior to the COVID-19 pandemic. In one study, families completed a survey that demonstrated a preference for in-person visits, but most respondents were not familiar with telemedicine as a modality [7]. A second study assessed differences in costs associated with telemedicine and found that pediatric rheumatology patients traveling to a remote site with a nurse-facilitator accrued lower costs and fewer hours of missed school and work [8]. Of eligible respondents receiving standard in-person care, only 42% expressed an interest in a telemedicine model [8]. To date, no studies have systematically evaluated patient/caregiver telehealth satisfaction in a diverse sample of pediatric rheumatology patients.
The purpose of this survey study was to evaluate pediatric rheumatology telehealth visits from the patient/caregiver perspective after telehealth implementation during the COVID-19 pandemic. Our specific objectives were to assess telehealth usefulness, ease of use, effectiveness, and satisfaction and identify clinical characteristics associated with overall satisfaction from the patient/caregiver perspective.
Methods
Study participants
All patients, both new and existing, with an initial telehealth video visit with a Children’s Hospital of Philadelphia (CHOP) rheumatology provider between 4/8/2020 and 6/30/2020 and had a valid email address in their medical record were eligible. Approximately 4% of patients did not have a valid email address, and therefore, did not receive the survey. Patients 18 years of age or older were allowed to complete the survey independently. Otherwise, a parent/caregiver completed the survey. This study was reviewed by the Children’s Hospital of Philadelphia Institutional Review Board (IRB) and was deemed not human subjects research since no protected health information was collected.
Telehealth visit process
During the Spring of 2020, we developed a new telehealth visit process in response to the COVID-19 pandemic. Upon scheduling a video visit, a clinic coordinator ensured registration with the electronic health record (EHR) portal and distributed a standard set of pre-visit recommendations. Using the built-in telehealth capabilities of the health system’s EHR, the patient/family accessed the visit through the portal using a mobile phone, tablet, laptop, or desktop computer. The provider accessed the visit using either a mobile phone or tablet using mobile EHR functionality. Patient after-visit instructions were available through the EHR portal. Between 3/16/2020–4/13/2020, approximately 10% of visits were in-person, which included new patient and emergent patient visits. On 4/14/2020, new patient visits were also converted to telehealth, and thereby, received the survey.
Survey administration
Within one day of completing the telehealth visit, all patients/caregivers were sent an anonymous post-visit Research Electronic Data Capture (REDCap©) telehealth satisfaction survey composed of a modified version of the Telehealth Usability Questionnaire (TUQ) and the Telemedicine Satisfaction and Usefulness Questionnaire (TSUQ) [9, 10]. Patient demographic and disease-related questions such as age, race, rheumatologic condition, diagnosis within past 6 months, and current rheumatologic medication(s) were included. After beginning survey administration, an additional question was added to differentiate between new and existing patients [see Additional file 1 for the complete survey]. The survey was automatically resent to patients/caregivers weekly up to three times until completed without the ability to skip questions.
Data collection
The TUQ was chosen to assess telehealth usefulness, ease of use, effectiveness, reliability, and satisfaction. The TUQ has shown good internal consistency and independent content validity [9]. The TUQ includes 21 questions that are grouped into the five domains/sub-scales. Standardized Cronbach’s coefficient alpha values for the usefulness, ease of use, effectiveness, reliability, and satisfaction sub-scales are 0.85, 0.93, 0.87, 0.81, and 0.92, respectively [9]. The usefulness sub-scale gauges how the patient or parent perceives potential intended benefits of the telehealth system and whether the degree to which the healthcare interaction or service is similar to the in-person encounter. The ease of use sub-scale quantifies the patient or parent perception of how easy the telehealth system is to learn and whether the interaction with the telehealth interface is enjoyable. The effectiveness sub-scale assesses the quality of the telehealth interaction, specifically around audio and visual communication. Finally, the satisfaction sub-scale evaluates the patient’s overall satisfaction and willingness to use the system in the future [9]. We adapted the TUQ to include 14 questions focusing on our assessment priorities and eliminated telehealth platform questions less germane to our clinic-based improvement efforts. We substituted one item of the TUQ (“telehealth improves my access to health services”) with one item from the TSUQ (“video visits are a convenient form of healthcare delivery for me”) in the usefulness domain, since it assessed the information we were seeking to obtain from patients and families more clearly. Survey questions were delivered using a 5-point Likert scale with anchors strongly disagree [1] and strongly agree [5] and was only available in English.
Survey analysis
Standard descriptive statistics were used to characterize the study population respondent demographic, disease- and medication related variables along with TUQ total and sub-scale scores. Likert scale responses of agree or strongly agree were classified as positive. Responses of neither agree or disagree, disagree, or strongly disagree were classified as neutral or negative. The Wilcoxon signed rank test was used to assess differences between individual survey items within each sub-scale and differences between total sub-scale scores. Univariate linear regression models were used to assess the association of demographic and underlying diagnosis with TUQ total and sub-scale scores. Bonferroni correction was used in the exploratory analysis of differences across clinical characteristics given there were multiple comparisons. Analyses were performed using IBM SPSS Statistics 20.0.
Results
Patient characteristics
We received responses from 42% (248/597) of patients and caregivers. The demographic, disease- and treatment characteristics, and visit type are detailed in Table 1. The most common rheumatic condition represented was juvenile idiopathic arthritis (JIA, 33.5%). Most were diagnosed with a rheumatologic condition greater than six months prior to the survey (76.2%) and were taking a medication prescribed by the rheumatologist (59.7%). Of those on medication, steroids were prescribed for 14.5%. Characteristics of the non-responders were not assessed, since the survey was anonymous.
Table 1.
Patient demographics, disease, and treatment characteristics
| Variable | N = 248a |
|---|---|
| Patient Age | |
| ≤ 5 years | 35 (14.1%) |
| 6–12 years | 68 (27.4%) |
| 13–17 years | 118 (47.6%) |
| ≥ 18 years | 27 (10.9%) |
| Race | |
| Caucasian | 188 (75.8%) |
| African American | 16 (6.5%) |
| Asian | 17 (6.9%) |
| Other | 27 (10.9%) |
| Condition | |
| Juvenile idiopathic arthritis | 83 (33.5%) |
| Systemic lupus erythematosus | 16 (6.5%) |
| Inflammatory diseaseb | 40 (16.1%) |
| Amplified musculoskeletal pain | 36 (14.5%) |
| Other/Unknown | 73 (29.4%) |
| Rheumatologic diagnosis in the past 6 months | 59 (23.8%) |
| Prescribed rheumatologic medication(s) | 148 (59.7%) |
| Glucocorticoid therapy for rheumatologic condition | 36 (14.5%) |
| Rheumatology new patient visit (n = 212) | 85 (40.1%) |
aUnless otherwise indicated
bDiagnoses included in the “inflammatory disease” category include Sjogren syndrome, vasculitis, juvenile dermatomyositis, chronic nonbacterial osteomyelitis, idiopathic uveitis, localized scleroderma, systemic sclerosis, Behcet syndrome, sarcoidosis, and periodic fever syndrome or auto-inflammatory disorder
Assessment of Total TUQ and sub-scale scores
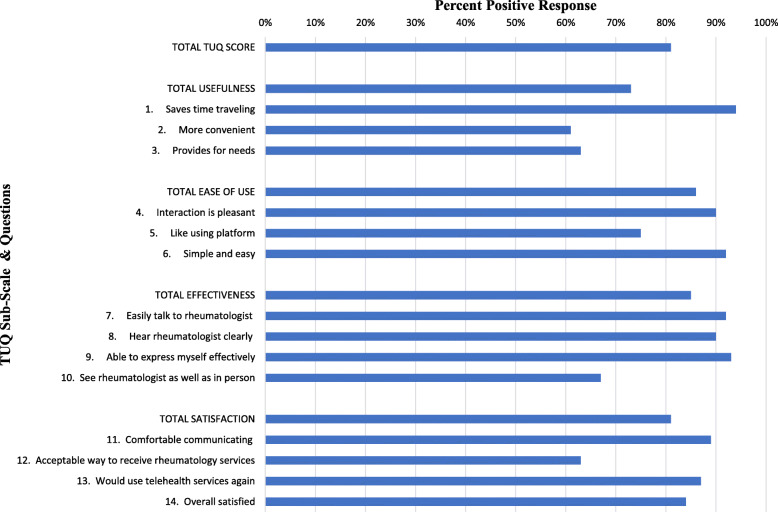
We graphically depicted positive responses across the total TUQ and subscales (Fig. 1). There was no statistically significant difference between positive responses of agree and strongly agree or negative responses of disagree or strongly disagree.
Fig. 1.
Graphic Depiction of Positive Response by Telehealth Usability Questionnaire (TUQ)
We then assessed the total TUQ and subscale scores to identify the determinants of the telehealth satisfaction (Table 2). The median total TUQ score was 4 (IQR: 4–5). Patients and caregivers provided positive responses in 81% of items. Of the subscales, usefulness scores were lowest (p < 0.001).
Table 2.
Total TUQ and Sub-Scale Scores
| Positive Responsea N (%) |
Neutral / Negative Response N (%) |
Mean (SD) | Median (IQR) | |
|---|---|---|---|---|
| Total TUQ Score | 201 (81%) | 47 (19%) | 4.18 (0.65) | 4 (4–5) |
| Usefulness | 181 (73%) | 67 (27%) | 4.04 (0.72) | 4 (4–5) b |
| 1. Saves time traveling | 233 (94%) | 15 (6%) | 4.62 (0.61) | 5 (4–5) |
| 2. More convenient | 151 (61%) | 97 (39%) | 3.77 (1.06) | 4 (3–5) c |
| 3. Provides for needs | 156 (63%) | 92 (37%) | 3.75 (0.95) | 4 (3–4) c |
| Ease of Use | 213 (86%) | 35 (14%) | 4.29 (0.69) | 4 (4–5) |
| 4. Interaction is pleasant | 223 (90%) | 25 (10%) | 4.42 (0.74) | 5 (4–5) |
| 5. Like using platform | 186 (75%) | 62 (25%) | 4.02 (0.95) | 4 (3–5) d |
| 6. Simple and easy | 228 (92%) | 20 (8%) | 4.40 (0.70) | 5 (4–5) |
| Effectiveness | 211 (85%) | 37 (15%) | 4.26 (0.77) | 5 (4–5) |
| 7. Easily talk to rheumatologist | 228 (92%) | 20 (8%) | 4.42 (0.84) | 5 (4–5) |
| 8. Hear rheumatologist clearly | 223 (90%) | 25 (10%) | 4.37 (0.92) | 5 (4–5) |
| 9. Able to express myself effectively | 231 (93%) | 17 (7%) | 4.50 (0.69) | 5 (4–5) |
| 10. See rheumatologist as well as in person | 166 (67%) | 82 (33%) | 3.77 (1.14) | 4 (3–5) e |
| Satisfaction | 201 (81%) | 47 (19%) | 4.12 (0.74) | 4 (4–5) |
| 11. Comfortable communicating | 221 (89%) | 27 (11%) | 4.31 (0.75) | 4 (4–5) |
| 12. Acceptable way to receive rheumatology services | 156 (63%) | 92 (37%) | 3.72 (1.09) | 4 (3–5) f |
| 13. Would use telehealth services again | 216 (87%) | 32 (13%) | 4.26 (0.81) | 4 (4–5) |
| 14. Overall satisfied | 208 (84%) | 40 (16%) | 4.20 (0.78) | 4 (4–5) |
a Positive response includes “agree” or “strongly agree”, while neutral/negative response includes “Neither agree nor disagree”, “disagree” and “strongly disagree”
b Median statistically significantly lower compared with ease of use, effectiveness, and satisfaction sub-scales
c Medians statistically significantly lower compared with item 1
d Median statistically significantly lower compared with items 4 and 6
e Median statistically significantly lower compared with items 7, 8, and 9
f Median statistically significantly lower compared with items 11, 13, and 14
We next assessed differences in domain-specific responses. Within the usefulness domain, a high proportion attested to telehealth visits saving time (median = 5, IQR: 4–5). However, scores for telehealth visits being more convenient (median = 4, IQR: 3–5) and providing for rheumatology needs (median = 4, IQR: 3–4) were significantly lower (p < 0.001 for both). Within the ease of use domain, a high proportion found the interaction pleasant and simple and easy (median = 5, IQR: 4–5 for both). Significantly lower scores were noted for “like using platform” (median = 4, IQR: 3–5); p < 0.001). Within the effectiveness domain, verbal communication items all received high scores (median = 5, IQR: 4–5), but the visual communication scores (median = 4, IQR: 3–5) were significantly lower (p < 0.001). Within the satisfaction domain, patients and caregiver scores for comfort communicating, future use, and overall satisfaction were high (median = 4, IQR: 4–5). However, when asked whether telehealth is an acceptable way to receive rheumatology services, scores (median = 4, IQR: 3–5) were significantly lower (p < 0.001).
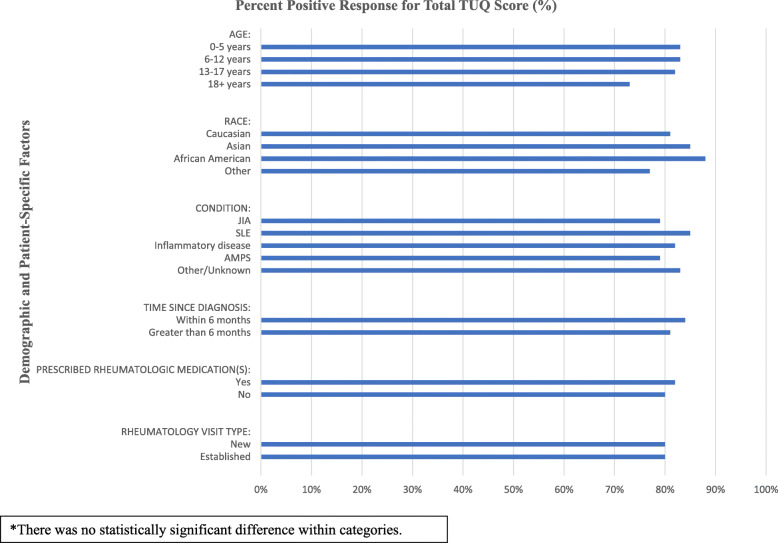
Clinical characteristics and satisfaction
Descriptive analysis of positive responses by demographic and clinical features across total and sub-scale TUQ scores are depicted in Table 3. We graphically depicted positive responses for total TUQ across demographic and patient-specific factors (Fig. 2).
Table 3.
Positive telehealth satisfaction according to demographic and patient-specific factors
| Variable | Total Score | Usefulness | Ease of Use | Effectiveness | Satisfaction/ Future Use |
|---|---|---|---|---|---|
| Age | |||||
| 0–5 years | 83% | 65% | 90% | 90% | 85% |
| 6–12 years | 83% | 73% | 87% | 87% | 86% |
| 13–17 years | 82% | 76% | 86% | 85% | 80% |
| 18+ years | 73% | 69% | 75% | 76% | 70% |
| Race | |||||
| Caucasian | 81% | 73% | 86% | 84% | 81% |
| African American | 88% | 77% | 90% | 97% | 88% |
| Asian | 85% | 79% | 86% | 90% | 84% |
| Other | 77% | 62% | 84% | 86% | 76% |
| Conditiona | |||||
| JIA | 79% | 68% | 85% | 84% | 80% |
| SLE | 85% | 81% | 88% | 88% | 83% |
| Inflammatory diseaseb | 82% | 73% | 89% | 84% | 82% |
| AMPS | 79% | 76% | 78% | 83% | 78% |
| Other/Unknown | 83% | 74% | 88% | 89% | 82% |
| Time since diagnosis | |||||
| Within 6 months | 84% | 76% | 89% | 86% | 84% |
| Greater than 6 months | 81% | 72% | 85% | 85% | 80% |
| Prescribed rheumatologic medication(s) | |||||
| Yes (n = 148) | 82% | 73% | 87% | 87% | 82% |
| Glucocorticoid therapy | 82% | 75% | 88% | 84% | 81% |
| No glucocorticoid therapy | 83% | 73% | 87% | 87% | 83% |
| No | 80% | 72% | 84% | 84% | 79% |
| Rheumatology visit type (n = 212) | |||||
| New | 80% | 70% | 86% | 86% | 79% |
| Established | 80% | 72% | 83% | 84% | 80% |
Positive satisfaction defined as responses of “agree” and “strongly agree”
aJIA: juvenile idiopathic arthritis; SLE: systemic lupus erythematosus; AMPS: amplified musculoskeletal pain syndrome
bDiagnoses included in the “inflammatory disease” category include Sjogren syndrome, vasculitis, juvenile dermatomyositis, chronic nonbacterial osteomyelitis, idiopathic uveitis, localized scleroderma, systemic sclerosis, Behcet syndrome, sarcoidosis, and periodic fever syndrome or auto-inflammatory disorder
Fig. 2.
Positive Telehealth Satisfaction Across Demographic and Patient-Specific Factors
The univariate regression model did not reveal differences in the telehealth satisfaction total or subscale scores according to age, race, rheumatologic condition, disease duration, glucocorticoid therapy or visit type.
Discussion
We completed a survey assessing telehealth satisfaction in a diverse sample of pediatric rheumatology patients during the COVID-19 pandemic. This is the first study of its type and is timely given the rapid and widespread telehealth implementation in the United States. The study is strengthened by the use of validated telehealth usability instruments. While overall satisfaction with video visits was high, our data suggest that purposeful efforts will be required to design a care experience to meet the needs of patients and families.
There are encouraging signs that telehealth may be a viable method to deliver pediatric rheumatology care in the future. Across all telehealth assessment sub-scales, the majority of patients and caregivers reported positive experiences. A high proportion considered video visits to be time saving as well as easy to learn and use. We did not identify significant differences in the satisfaction based on rheumatologic diagnoses (e.g. JIA or amplified musculoskeletal pain syndrome), medication treatments, or demographic factors, which should be promising for communities where access to pediatric rheumatology providers is limited.
Although generally well-received, there was a lower percentage of patients and caregivers who endorsed the visits as more convenient or as an “acceptable” way to receive pediatric rheumatology care. These findings are consistent with a previous survey performed at a pediatric rheumatology center demonstrating that in-person visits were preferred over telehealth regardless of the need for travel. However, patients and families who had more familiarity with telehealth care were more likely to consider it equal or preferable to in-person visits [7]. Acceptability may increase with greater exposure to video visits and application in more targeted use cases. In addition, our study was performed during a rapid implementation of video visits at the beginning of the COVID-19 pandemic. It is possible that acceptability will increase when pediatric rheumatology providers have more familiarity with telehealth delivery and identify more optimal use cases. Research and innovation are needed to determine how evolving telehealth technology can help providers perform virtual exams with high fidelity and safety, thereby improving pediatric rheumatology telehealth delivery [11].
Previous studies of patient satisfaction may help identify methods to improve telehealth implementation. While little has been published on the specific drivers of patient satisfaction with in-person pediatric rheumatology care, drivers of a positive patient experience in the pediatric literature include the efficiency of the visit and more important, communication between team members and between the patient, caregivers, and healthcare provider [12–14]. Within the realm of telehealth, the drivers of patient satisfaction are less defined. A systematic review of patient satisfaction with telehealth demonstrated its potential, documenting that it was convenient, easy to use, enhanced communication, and in some cases, improved outcomes [15]. In the included research studies, however, telehealth was mainly used to augment management in specific chronic diseases (e.g. sleep apnea) or support specific clinical functions (e.g. insulin therapy monitoring). Broader applications to general populations such as ours are less well studied. Pediatric subspecialty-specific guidance to enhance telehealth satisfaction has been published for gastroenterology and rheumatology [16, 17]. The authors suggest that close attention to the pre-visit process, patient-facing technology logistics, visit location, history and physical exam completeness, and post-visit recommendations are critical to achieve a positive patient experience. Provider and staff training will undoubtedly be required to perform these functions optimally.
Improved clinical evaluation tools and enhanced understanding of telehealth capabilities are needed to arrive at the ideal telehealth encounter for all pediatric rheumatology patients. Patient reported outcomes (PROs) are being increasingly used as clinical measures to assess disease activity in pediatric rheumatology. The Juvenile Arthritis Disease Activity Score (JADAS), for example, combines patient reported values with physician and physical exam values to calculate disease state in JIA [18]. Telehealth visits pose a challenge to the standard physical exam, which has been superior in care delivery. Therefore, alternative approaches may be needed to augment the clinical exam to improve satisfaction with the telehealth visit. Examples may include use of the Juvenile Arthritis Multidimensional Assessment Report (JAMAR) for patient-reported assessment of disease, the video paediatric gait arms legs and spine (v-pGALS) for virtual musculoskeletal examination, and personal devices such as blood pressure monitors and symptom trackers [17, 19]. Additionally, it will be important to address equity issues related to internet and hardware access, insurance status, limited language proficiency, and health literacy in future quantitative and qualitative work to ensure the telehealth experience is optimal for all patients requiring pediatric rheumatology care [20].
Our study had several limitations to consider. Given the telehealth platform was rapidly deployed and changed during the study period, improved training and implementation for patients, caregivers, and providers may help increase satisfaction in the future. Additionally, responses may have been influenced by the social context of the COVID-19 pandemic and therefore may not be generalizable. We received responses from 42% of patients and caregivers who may represent a more engaged cohort and be less representative of the pediatric rheumatology population. Since we did not have access to personal health information, we were unable to compare the demographics of patients that responded to the survey to those that did not respond. In addition, those unable to access care during the pandemic and those without an active email address were not included in the study. Therefore, it is possible that we are capturing a group of patients that were more likely to be satisfied with telehealth. For example, patients may have canceled or not participated in telehealth visits and would not have received a satisfaction survey. Also, the survey was only available in English, which may have excluded non-English speakers from responding. There was a brief period during survey administration where the type of visit was not assessed. However, analysis of visit type and satisfaction showed no significant difference indicating that it was appropriate to include all of the data together. There may be additional constructs of satisfaction with telehealth, such as technological reliability, that were not addressed by our survey that could benefit from future analysis. Finally, the physician perspective regarding usability of and satisfaction with telehealth for specific visit-level processes and patient populations was not assessed and would be impactful to include in future research studies.
Conclusions
These data provide the foundation for understanding patient and caregivers’ satisfaction with telehealth in pediatric rheumatology and suggest that it is a promising mode of healthcare delivery. Further work is needed to design specific telehealth processes for pediatric rheumatology populations and assess outcomes. Given that telehealth is a rapidly emerging form of pediatric rheumatology care, we will need to engage patients, caregivers, multidisciplinary healthcare providers, and our health network technology partners to design interventions to streamline care to improve patient satisfaction and overall experience.
Supplementary Information
Additional file 1. Telehealth Satisfaction Survey. This is a copy of the survey which was completed by patients and caregivers.
Acknowledgements
Not applicable.
Abbreviations
- WHO
World Health Organization
- CHOP
Children’s Hospital of Philadelphia
- IRB
Institutional Review Board
- REDCap
Research Electronic Data Capture
- TUQ
Telehealth Usability Questionnaire
- JIA
Juvenile Idiopathic Arthritis
- AMPS
Amplified Musculoskeletal Pain Syndrome
- IBD
Inflammatory Bowel Disease
- JADAS
Juvenile Arthritis Disease Activity Score
- JAMAR
Juvenile Arthritis Multidimensional Assessment Report
- v-pGALS
Video Paediatric Gait Arms Legs and Spine
Authors’ contributions
All authors participated in the design of the study and interpretation of the data; LWC performed the data collection and analysis; LWC drafted the manuscript; all authors revised the manuscript for key intellectual content. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This survey study was deemed not human subjects research by the Children’s Hospital of Philadelphia Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. The authors have no financial relationships relevant to this article to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Committee on Rheumatologic Care. Position Statement: Telemedicine. American College of Rheumatology. 2020. https://www.rheumatology.org/Portals/0/Files/Telemedicine-Position-Statement.pdf.
- 2.Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11(2):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 3.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knudsen LR, Thurah AD, Lomborg K. Experiences with telehealth Followup in patients with rheumatoid arthritis: a qualitative interview study. Arthritis Care Res. 2017;70(9):1366–1372. doi: 10.1002/acr.23483. [DOI] [PubMed] [Google Scholar]
- 5.McDougall JA, Ferucci ED, Glover J, Fraenkel L. Telerheumatology: a systematic review. Arthritis Care Res. 2017;69(10):1546–1557. doi: 10.1002/acr.23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ray KN, Ashcraft LE, Mehrotra A, Miller E, Kahn JM. Family perspectives on telemedicine for pediatric subspecialty care. Telemed J E Health. 2017;23(10):852–862. doi: 10.1089/tmj.2016.0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parent's perceptions of barriers to care and care preferences. Pediatric Rheumatology. 2017;15(55). 10.1186/s12969-017-0184-y. [DOI] [PMC free article] [PubMed]
- 8.Kessler EA, Sherman AK, Becker ML. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatric Rheumatology. 2016;14(54). 10.1186/s12969-016-0116-2 [DOI] [PMC free article] [PubMed]
- 9.Parmanto B, Lewis AN, Graham KM, Bertolet MH. Development of the telehealth usability questionnaire (TUQ) Int J Telerehabilitation. 2016;8(1):3–10. doi: 10.5195/ijt.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakken S, Grullon-Figueroa L, Izquierdo R, Lee NJ, Morin P, Palmas W, Teresi J, Weinstock RS, Shea S, Starren J. Development, validation, and use of English and Spanish versions of the telemedicine satisfaction and usefulness questionnaire. J Am Med Inform Assoc. 2006;13(6):660–667. doi: 10.1197/jamia.M2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pooni R, Sandborg C, Lee T. Building a viable telemedicine presences in pediatric rheumatology. Pediatr Clin N Am. 2020;67(4):641–645. doi: 10.1016/j.pcl.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pen FB, Burrows JF, Shirley ED, Rosen P. Unlocking the doors to patient satisfaction in pediatric orthopaedics. J Pediatr Orthop. 2018;38(8):398–402. doi: 10.1097/BPO.0000000000000837. [DOI] [PubMed] [Google Scholar]
- 13.Davis J, Burrows JF, Khallouq BB, Rosen P. Predictors of patient satisfaction in pediatric oncology. J Pediatr Oncol Nurs. 2017;34(6):435–438. doi: 10.1177/1043454217717239. [DOI] [PubMed] [Google Scholar]
- 14.Barsoom RR, Maugans TA, Burrows JF, Rosen P. Exploring patient and family satisfaction in pediatric neurological surgery. Interdiscip Neurosurg. 2017;7:1–3. doi: 10.1016/j.inat.2016.10.002. [DOI] [Google Scholar]
- 15.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg E, Picoraro J, Miller S, Srinath A, Franciosi J, Hayes C, et al. COVID-19--a guide to rapid implementation of telehealth services - a playbook for the pediatric gastroenterologist. J Pediatr Gastroenterol Nutr. 2020;70(6):734–740. doi: 10.1097/MPG.0000000000002749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster HE, Jandial S. pGALS – paediatric gait arms legs and spine: a simple examination of the musculoskeletal system. Pediatr Rheumatol Online J. 2013;11(1). 10.1186/1546-0096-11-44. [DOI] [PMC free article] [PubMed]
- 18.Consolaro A, Ruperto N, Bazso A, Magni-Manzoni S, Pelagatti MA, Pistorio A, et al. Final validation of a new composite disease activity score for juvenile idiopathic arthritis: the Juvenile Arthritis Disease Activity Score (JADAS). Pediatr Rheumatol Online J. 2008;6(Suppl 1), P115. 10.1186/1546-0096-6-S1-P115.
- 19.For the Paediatric Rheumatology International Trials Organization (PRINTO) Lovell DJ, Brunner HI, et al. The American English version of the juvenile arthritis multidimensional assessment report (JAMAR) Rheumatol International. 2018;38(Suppl 1):35–42. doi: 10.1007/s00296-018-3984-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shenoi S, Hayward K, Curran ML, Kessler E, Mehta JJ, Riebschleger MP, Foster HE. Telemedicine in pediatric rheumatology: this is the time for the community to embrace a new way of clinical practice. Pediatr Rheumatol. 2020;18(85). 10.1186/s12969-020-00476-z. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Telehealth Satisfaction Survey. This is a copy of the survey which was completed by patients and caregivers.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.