Abstract
Introduction
Nurse-run preanaesthesia assessment is well established in ambulatory surgery. However, in the Middle East the implementation of such a service is new and needed careful preparation. Aim of this audit is to assess the feasibility and the quality of preoperative assessments by the specially trained nurses, patient and nurse satisfaction and overall perioperative quality of recovery.
Methods
The nurses were selected and trained first in an accredited programme. Then an implementation period of 3 month was used for them to gain experience. Hereafter, we performed a four-step audit on the quality of preassessment, the patient’s satisfaction, the quality of recovery and adverse events if any. Finally, we also monitored the nurse’s satisfaction of their new advanced role.
Results
The quality of preanaesthesia assessment was high as with 95% compliance to the accepted standards. In the patient satisfaction survey, all 152 patients were either highly satisfied or satisfied with the nurse-run service. The nurses were also highly satisfied and felt that they were either highly or moderately valued. All the patients who were operated at the ambulatory care services were followed up postoperatively by telephone calls which revealed that most of them were highly satisfied. No major or minor adverse events occurred.
Conclusion
Our specially trained nurses perform preoperative assessments on high standard without adverse events, while patient and staff satisfaction is very high. Future projects will focus on reducing the rate of cancellation of surgeries, investigating the cost-effectiveness of this approach as well as training the specialised nurses for paediatric preoperative anaesthesia assessments. This model of care could induce further nurse-run models of care in the Middle East.
Keywords: anaesthesia, audit and feedback, nurses, patient-centred care
Introduction
Nurse-run preanaesthesia assessment came into practice since early 1990s. It is widely established since surgery moved away from prolonged in-hospital admission towards short-stay and day care pathways. Nowadays, in many centres, well-trained nurse specialists lead these services.1 2 They have responsibility for assessing a patient’s fitness for anaesthesia and surgery, risk stratification and organising the necessary investigations or referrals. Nurses may spend more time with the patients and so understand patients’ concerns and expectations better. In that sense, such a service can alleviate patients’ anxiety by providing adequate education or counselling.3 However, due to structural, logistical and cultural reasons this service needed careful implementation.4 Nurse-led initiatives are few and far between at present in the Middle East.5 Especially, Qatar has a diverse population including people from almost 75 countries in the world, making it a real multicultural community. Probably for this reason, we have noticed different levels of expectations, respect and trust towards nurses. We assumed this situation might become a problem when implementing a new service relying on nursing staff in a different, more responsible role. As a part of the expansion project of Hamad Medical Corporation (HMC), Doha, Qatar, the ambulatory care centre (ACC) was opened in June 2017. Here, all day surgery patients would receive their treatment within 1 day and in a single dedicated location.
To optimise the workflow the preoperative trajectory was smoothened in terms of patients having a single preoperative visit to the hospital only: first an appointment with the surgeon and thereafter the preanaesthesia assessment on the same day. Accordingly, reorganisation of the preanaesthesia assessment clinic came into focus. As a cornerstone, we planned to implement the concept of nurse run, consultant anaesthetist supervised preanaesthesia assessment clinics in ACC as a quality improvement initiative. This would be the first and only of its kind in the state of Qatar. In short words, the goals of the present pilot project are reducing patient waiting times, enhancing patient comfort, triaging of patient categories to deliver individualised care, reducing cancellations of operations standardisation of patient assessment, valorisation of nursing quality and detecting early postoperative complications.
The aim of this audit is to show the feasibility of Qatar’s first nurse-run preanaesthesia assessment and its impact on the overall perioperative quality of patient care. It was hypothesised that the patients who had a nurse-run preanaesthesia assessment had increased satisfaction and were well prepared for the surgery. In addition, this project could serve as proof of concept to support future nurse-led initiatives.
Initiation and implementation
In alliance with the departments of nursing education, nursing and anaesthesia, a new curriculum, approved by the Qatar Council of Health Care Practitioners (QCHP) was developed to train nurses in assessing patients’ fitness for anaesthesia. The curriculum included an introduction to the normal physical status of the patients, physical examination (especially the airway) as well as, different scenarios regarding the abnormal patient presentations (see online supplemental appendix). Twenty-five nurses with at least 3 years of clinical experience postqualification were selected. Prerequisite was a surgical preassessment or other perioperative background, a valid QCHP license and experience in managing the electronic medical records and documentation.
bmjoq-2020-001066supp001.pdf (4MB, pdf)
During the formal training, the nurses followed 25 hours of structured training and self-study. They were taught to use the NICE guidelines as a reference for ordering preoperative blood analysis or other investigations if required. They were also introduced to the hospital protocol for the preoperative management of diabetes mellitus and arterial hypertension management which they used as references for medication instructions. Hereafter a written and oral examination approved the nurses as specially trained for preanaesthesia assessment. Finally, simulation sessions were organised during a preimplementation period of 3 months, during which the nurses were assessing the patients under direct supervision of the consultant anaesthesiologist. This helped the nurses to gain valuable clinical experience and helped the administration to reorganise logistics of the clinics.
Officially, the nurse-run clinics started on 24 December 2017. All patients scheduled for elective short stay and ambulatory care surgery were screened for their risk factors and categorised according to the American Society of Anesthesiology (ASA) classification of physical status. Then low-risk to medium-risk patients (ASA 1 and 2) were assessed by the nurses under the indirect supervision of an anaesthesiologist. The nurses’ role was to interview the patients about their health, comorbidities and medications. Subsequently, they performed a physical examination and identification of individual risks. Finally, they proposed and discussed the individual perioperative management and explained the purpose of the preoperative and postoperative phone calls. However, the consent was obtained in the presence of the anaesthesiologist who in addition continued evaluating high risk patients (ASA 3 and higher). The nurses used our standardised preanaesthesia evaluation template. This template focussing on evidence based medicine was written by the committee for preoperative assessment which was comprised of senior consultants and consultants of our department. In addition, IT-specialists adapted the raw template to our electronic chart system (CERNER). The nurses have easy access to the patient’s chart and this template to fill in the necessary details. The doctors (both surgeons and anaesthetists) can easily log in to their account and read the notes. The patients were also informed verbally about the type of anaesthesia, fasting guidelines and medications.
Materials and methods
Audit design and subjects
This is a retrospective observational audit carried out at the ACC in four steps during the period of January 2018 to December 2018.
In the first step, patient files were randomly selected from the nurse-run preanaesthesia clinic for auditing the efficacy of preoperative assessment. The aim was to assess the completeness and quality of preoperative evaluations. The files were audited according to the data collection sheet.
In the second step, a patient satisfaction survey was conducted directly after the preanaesthesia assessment. Again, patients were randomly selected and their satisfaction regarding the quality of nurse-run preanaesthesia assessment was measured using a bilingual questionnaire (Arabic and English).
In the third step, a postoperative quality of recovery survey was conducted in patients who were also selected randomly. Following the surgery these patients received a telephone call from the nurses who assessed their postoperative quality of recovery using a standardised, internationally validated QoR 15 survey questionnaire.
Finally, as the fourth step, the satisfaction of the nurses who were actively involved in this project was assessed using a standardised questionnaire.
The anaesthetist’s performance was not part of this audit and was not subject of the investigation.
Statistical analysis
Since this is an audit to assess the quality of perioperative care, all the collected data were tabulated, analysed and expressed in percentages as usual in descriptive statistics.
Results
Quality of preanaesthesia assessment
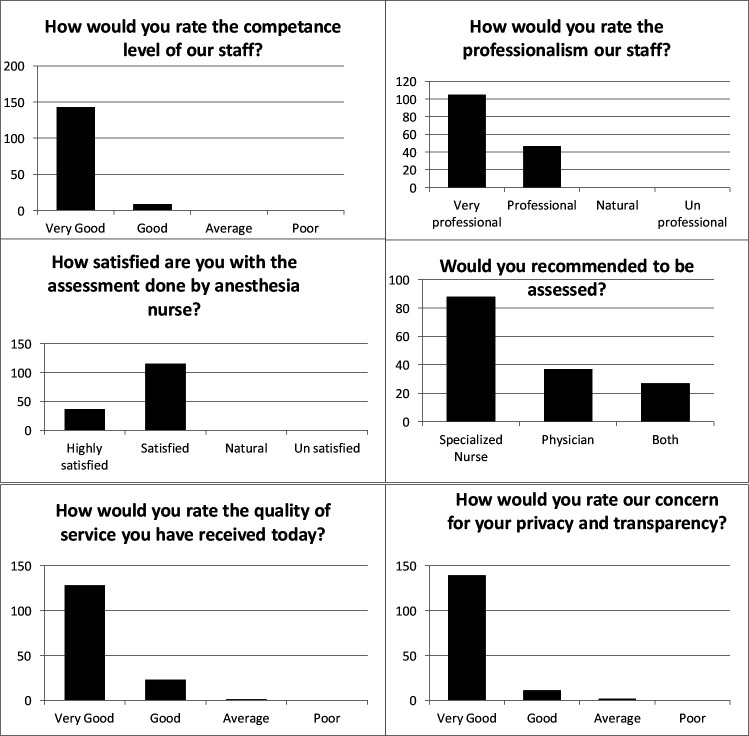
In all the selected 100 files, the preoperative assessment was performed by the specially trained nurses and documented accordingly. In 80% the cases, there was a brief summary at the beginning of each patient report (see figure 1). The documentation of specific anaesthesia history and co-morbidities was present in 100% of the cases and they were presented correctly. Regarding physical examination, body mass index and exercise tolerance were reported in 91% of the cases. Important factors like airway documentation and system-wise examination were reported in all the 100 files. Likewise, the current medications and presence of any allergy were correctly mentioned in 100% of the cases. Classification into appropriate ASA categories and its justification were done correctly in 93% and 91% of the cases, respectively. Risk assessment and planning of the anaesthesia were sufficient in 86% of the files and a plan for postoperative pain management was described in 98% of the files. None of the ASA-1 or ASA-2 patients required further assessment by the covering consultant anaesthetist. There were no specific instances where the process broke down. We just encountered one case which had to be cancelled due to high blood pressure on the day of surgery.
Figure 1.
Results in percentage of the reviewed 100 patient charts. ASA, ambulatory care centre; BMI, body mass index.
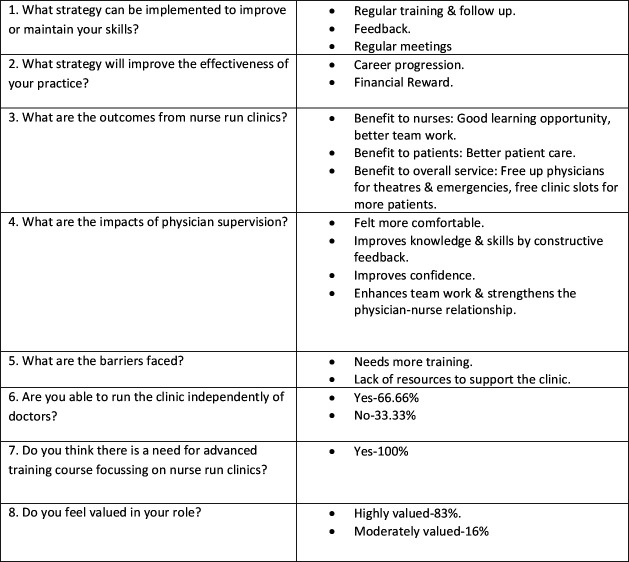
Patient satisfaction survey
Among the 152 patients who participated in the patient satisfaction survey, 84% of them rated the quality of service as very good while 15% rated it good (see figure 2). Ninety-one per cent of the patients felt that their privacy was respected and the service was transparent. 94% of the patients perceived the nurses were competent to perform the preanaesthesia assessment and all of them rated the nurses either professional or very professional. Moreover, all the patients were either satisfied or highly satisfied with the quality of care. Fifty-eight per cent of the patients would recommend others to the assessed by a specialised nurse, 24% would recommend a physician and 18% would recommend either a nurse or a physician.
Figure 2.
Patient satisfaction surveys.
Postoperative quality of recovery
Postoperative quality of recovery survey was an additional initiative introduced in February 2018. All the patients who had undergone a day care procedure or surgery should receive a telephone call postoperatively enquiring about their postoperative quality of recovery. Till January 2019, 816 patients answered the phone call out of 1331 patients (61%). Most of the patients (693/816, 85%) were highly satisfied with the overall perioperative experience and did not experience any complication.
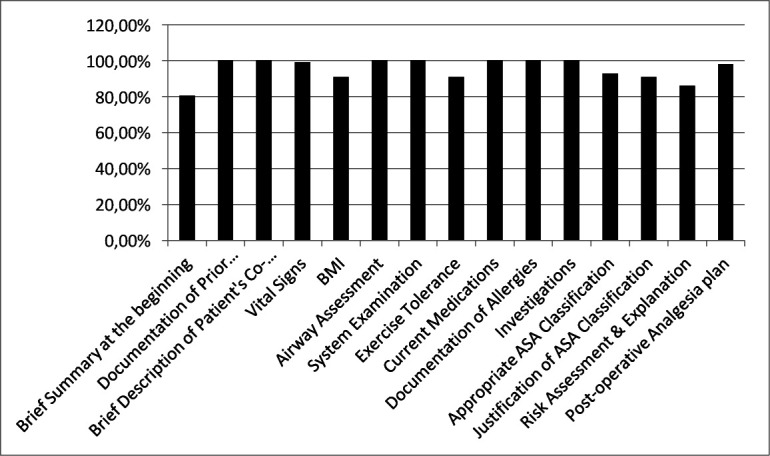
Nurses satisfaction survey
The satisfaction of the specialised nurses, who were the cornerstone of this project, was assessed and 11 nurses participated in this survey (see figure 3). The reason for this was that 14 nurses were transferred to different units after their training to initiate similar projects, without actively participating in the current project. However, from the remaining 11 nurses, 83% of them felt that they would profit from more training, frequent meetings, regular updates and constant feedback. All of them had the impression they could improve their clinical skills and medical knowledge with regular rigorous training. Likewise, they embraced an advanced training programme focusing on nurse-run preanaesthesia assessment. Eighty-three per cent of the nurses had the impression their service is highly valued by the multidisciplinary teams and 66% of them were confident that they can run clinic independently without direct support of the anaesthesiologist. All the involved nurses felt that it was an excellent opportunity to build up team work and clinical experience.
Figure 3.
Nurse satisfaction survey.
Discussion
As the organisation of our surgical service migrated more towards day care surgeries, we investigated the odds of the first nurse-run preanaesthesia assessment in the state of Qatar. Our results show clearly the feasibility of this practice with a high degree of acceptance and satisfaction on patient’s and nurses’ side.
We found the overall compliance with the required assessment was 95.3% within the ‘accepted standards. This implies the nurses were very meticulous in documenting the prior anaesthesia history, patients’ comorbidities, physical examination including the vital signs and airway assessment, medication history, allergies, the relevant investigations, ASA physical status and the type of anaesthesia as agreed by the patient. This is in agreement with previous literature showing nurses were more accurate than physicians in history taking.6 7 Although the appropriate ASA classification was found to be 93%, we still judge the general quality standards are met. In particular, if compared with a report from Helkin et al who mention a misclassification to the ‘wrong’ ASA score occurred in more than 18% of patients assessed by physicians.8 Globally the nurse preassessment results in a high degree of accuracy and reflects achievement of highest safety standards. Moreover, none of the patients underwent an adverse event during the operations or the procedures. This again supports the high quality and accuracy of nurse-led assessments. Although a systematic review on nurse-run versus doctor-run preoperative assessments, performed by Nicholson et al could not demonstrate that nurse-run assessments were superior to doctor-led assessments, many studies proved that nurse-run assessments were at least comparable to doctor-led assessments in terms of patient satisfaction, surgery cancellations and cost benefit.9 A recent systematic review on nurse-run preoperative assessment by Sau-man Conny and Wan-Yim confirms our findings.2 In addition, other authors describe lower surgery cancellation rates and reduction in the rate of postoperative mortality and length of hospital stay.6 10
The patient satisfaction survey also yielded encouraging results. All the 152 patients who participated in the survey were either satisfied or highly satisfied with the service they received. Eighty-four per cent of them rated the quality of service was very good. This is in agreement with a study from Shakeel et al. In their study, 88% responded to the questionnaire and 80% were satisfied with their treatment.11 Additionally, two systematic reviews on nurse-run assessments by Nicholson et al and Sau-man Conny and Wan-Yim demonstrated a high degree of patient satisfaction with these services.2 9 Our result is remarkable, because the acceptance of nurses’ role in our medical environment is still moderate. In a recent review by Arbabi et al the authors highlighted the importance and efficacy of preceptorship on nursing quality in Qatar.12
The introduction of other new initiatives, like a preoperative phone call, reduces cancellations due to unforeseen events like change in health state or even acute fear for the operation increasing the efficiency of the operating theatres and improving time management.13 While the postoperative call offers more patient safety in terms of detecting early postoperative complications and providing more effective postoperative pain management. We measured the quality of recovery and overall patient satisfaction with the postoprative QOR 15 score and found most of the patients were highly satisfied with the overall perioperative quality of care. No patient experienced any major or minor adverse event.
The nurse’s satisfaction survey is an equally important initiative, because their new function could overstress them leading to exhaustion and even burn out. From other studies, we know that hierarchical structures in big corporations like in healthcare have always yielded the dominance of the medical fraternity and suppressed the roles of nursing staff and other healthcare professionals. Choi et al demonstrated the triangulation of influence between job satisfaction, leadership in the organisation and job satisfaction among healthcare employees.14 However, the results reveal not only the sincerity, dedication and passion of the specialised nurses towards this new task to improve perioperative quality of care but also their determination to gain better knowledge. Most of them were recommending the requirement of constant feedback, advanced learning modules and continuing professional development sessions. It was clear in our research that the nurses who were only performing basic duties when given the opportunity were ready and willing to rise to the challenge thereby enhancing their morale and job satisfaction. There is a fine double edge to this though as overloading them with too many tasks beyond their capability would lead to stress and burn out. It was with this aspect in mind that our pilot for HMC was always designed as a nurse-run Pre-Anaesthesia-Assessment-Clinic (PAAC) rather than a nurse-led clinic model of care. On the other hand, we regard this project as a proof of concept highlighting the critical importance of alignment and coworking between the different key individuals and stake holders.15 In our case, we had hard evidence that nurse-led concepts work in other countries and the stake holders needed to align this to Middle East and HMC.
Although we could not find any prior literature regarding nurses’ satisfaction, we believe that it will be important in the planning and implementation of the future steps of this project as employees who are convinced about a concept will carry this out more effectively.
Another reason for implementing this project is that a nurse-run assessment might be more standardised leading to better coordination of patient flow and finally improving the quality of perioperative care.16 Such an approach could reduce patient waiting time, which directly enhances the comfort as the patients experience the so-called ‘one stop shop clinics’. This means the patients come directly after meeting their surgeon to the anaesthesia clinic and leave the hospital shortly thereafter with a schedule for surgery in hand. Indeed, it is possible to extend nurse assessment to ASA-3 patients as well. However, this will need further education and training regarding the management of coexisting major comorbidities in patients who are ASA-3 or above. In addition, nurse-run clinics are more cost-effective as they employ appropriately trained nurses instead of a consultant anaesthetist without compromising the quality of patient care.17
We conclude that our specially trained nurses perform preoperative assessments on a high-quality standard without adverse events, while patient and staff satisfaction is very high. Future projects will focus on reducing the rate of cancellation of surgeries, investigating the cost effectiveness of this approach as well as training the specialised nurses for paediatric preoperative anaesthesia assessments. This model of care could induce further nurse-run models of care in the Middle East.
Acknowledgments
The authors acknowledge the immense contribution of all staff and patients at the Ambulatory Care Centre in Doha, Qatar.
Footnotes
Contributors: All authors contributed to the paper directly. Marcus D Lance is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article. Upon request readers may get additional information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study does not involve human participants.
References
- 1.Hines S, Munday J, Kynoch K. Effectiveness of nurse-led preoperative assessment services for elective surgery: a systematic review update. JBI Database System Rev Implement Rep 2015;13:279–317. 10.11124/01938924-201513060-00016 [DOI] [PubMed] [Google Scholar]
- 2.Sau-Man Conny C, Wan-Yim I. The effectiveness of nurse-led preoperative assessment clinics for patients receiving elective orthopaedic surgery: a systematic review. J Perianesth Nurs 2016;31:465–74. 10.1016/j.jopan.2014.08.147 [DOI] [PubMed] [Google Scholar]
- 3.Malkin KF. Patients' perceptions of a pre-admission clinic. J Nurs Manag 2000;8:107–13. 10.1046/j.1365-2834.2000.00163.x [DOI] [PubMed] [Google Scholar]
- 4.Sahraoui A, Elarref M. Bed crisis and elective surgery late cancellations: an approach using the theory of constraints. Qatar Med J 2014;2014:1–11. 10.5339/qmj.2014.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hibbert D, Aboshaiqah AE, Sienko KA, et al. Advancing nursing practice: the emergence of the role of advanced practice nurse in Saudi Arabia. Ann Saudi Med 2017;37:72–8. 10.5144/0256-4947.2017.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed M, Wright S, Armitage F. Nurse-led general surgical pre-operative assessment clinic. J R Coll Surg Edinb 1997;42:310–3. [PubMed] [Google Scholar]
- 7.Whiteley M. The role of the nurse in the pre-admission clinic. Ann R Coll Surg Engl 1998;80:192. [PubMed] [Google Scholar]
- 8.Helkin A, Jain SV, Gruessner A, et al. Impact of ASA score misclassification on NSQIP predicted mortality: a retrospective analysis. Perioper Med 2017;6:23. 10.1186/s13741-017-0076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nicholson A, Coldwell CH, Lewis SR, et al. Nurse-Led versus doctor-led preoperative assessment for elective surgical patients requiring regional or general anaesthesia. Cochrane Database Syst Rev 2013:Cd010160. 10.1002/14651858.CD010160.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones A, Penfold P, Bailey M, et al. Pre-admission clerking of urology patients by nurses. Prof Nurse 2000;15:261–6. [PubMed] [Google Scholar]
- 11.Shakeel M, Newton JR, Clark D, et al. Patients' satisfaction with the nurse-led aural care clinic. J Ayub Med Coll Abbottabad 2008;20:81–3. [PubMed] [Google Scholar]
- 12.Arbabi H, Johnson J, Forgrave D. The effect of preceptorship on nurses’ training and preparation with implications for Qatar: A literature review. J Nurs Educ Pract 2018;8:44–50. 10.5430/jnep.v8n7p44 [DOI] [Google Scholar]
- 13.Appavu ST, Al-Shekaili SM, Al-Sharif AM, et al. The burden of surgical cancellations and No-Shows: quality management study from a large regional hospital in Oman. Sultan Qaboos Univ Med J 2016;16:e298–302. 10.18295/squmj.2016.16.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi SL, Goh CF, Adam MBH, et al. Transformational leadership, empowerment, and job satisfaction: the mediating role of employee empowerment. Hum Resour Health 2016;14:73. 10.1186/s12960-016-0171-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Passarelli M, Landi GC, Cariola A, et al. Open innovation in the new context of proof of concepts: evidence from Italy. EJIM 2021;24:735–55. 10.1108/EJIM-02-2020-0052 [DOI] [Google Scholar]
- 16.Edward GM, Razzaq S, de Roode A, et al. Patient flow in the preoperative assessment clinic. Eur J Anaesthesiol 2008;25:280–6. 10.1017/S0265021507003122 [DOI] [PubMed] [Google Scholar]
- 17.Kinley H, Czoski-Murray C, George S, et al. Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and pre-registration house officers in pre-operative assessment in elective general surgery. Health Technol Assess 2001;5:1–87. 10.3310/hta5200 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2020-001066supp001.pdf (4MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article. Upon request readers may get additional information.