Key Points
Question
What are the outcomes associated with caustic ingestion in adults?
Findings
In this observational study, 1198 patients (34%) presented complications following caustic ingestion, mostly pulmonary; 388 (11%) required surgery for digestive necrosis; and 284 (8%) died. Severity of ingestion and hospital volume were associated with mortality.
Meanings
Emergency management of caustic injuries in high-volume centers may improve survival rates.
This study assesses outcomes associated with caustic ingestion in adults across a nationwide prospective database in France.
Abstract
Importance
Caustic ingestion in adults may result in death or severe digestive sequelae. The scarcity of nationwide epidemiological data leads to difficulties regarding the applicability of their analysis to less specialized centers, which are nevertheless largely involved in the emergency management of adverse outcomes following caustic ingestion.
Objective
To assess outcomes associated with caustic ingestion in adults across a nationwide prospective database.
Design, Settings, and Participants
Adult patients aged 16 to 96 admitted to the emergency department for caustic ingestion between January 2010 and December 2019 were identified from the French Medical Information System Database, which includes all patients admitted in an emergency setting in hospitals in France during this period.
Exposure
Esophageal caustic ingestion.
Main Outcomes and Measures
The primary end point was in-hospital patient outcomes following caustic ingestion. Multivariate analysis was performed to assess independent predictors of in-hospital morbidity and mortality.
Results
Among 22 657 226 patients admitted on an emergency outpatient basis, 3544 (0.016%) had ingested caustic agents and were included in this study. The median (IQR) age in this population was 49 (34-63) years, and 1685 patients (48%) were women. Digestive necrosis requiring resection was present during the primary hospital stay in 388 patients with caustic ingestion (11%). Nonsurgical management was undertaken in 3156 (89%). A total of 1198 (34%) experienced complications, and 294 (8%) died. Pulmonary complications were the most frequent adverse event, occurring in 869 patients (24%). On multivariate analysis, predictors of mortality included old age, high comorbidity score, suicidal ingestion, intensive care unit admission during management, emergency surgery for digestive necrosis, and treatment in low-volume centers. On multivariate analysis, predictors of morbidity included old age, higher comorbidity score, intensive care unit admission during management, and emergency surgery for digestive necrosis.
Conclusions and Relevance
In this study, referral to expert centers was associated with improved early survival after caustic ingestion. If feasible, low-volume hospitals should consider transferring patients to larger centers instead of attempting on-site management.
Introduction
Caustic ingestion in adults may result in death or severe digestive sequelae.1 Reported emergency mortality and morbidity rates after massive ingestion of strong caustic agents range from around 13% to 16% and 36% to 80%, respectively.1,2,3 Following initial conservative management, 14% to 37% of patients develop esophageal strictures.4,5 Both early and late complications associated with caustic ingestion require significant health care resource utilization and can have a long-term negative impact on patient survival and nutritional outcomes.3,6
One limitation in the literature is that the few studies focusing on this topic are reported from high-volume referral centers, which have important expertise in esophageal surgery. The scarcity of nationwide epidemiological data leads to difficulties regarding the applicability of their analysis to less-specialized centers, which are nevertheless frequently involved in the emergency treatment of patients following caustic ingestion. Several large epidemiological data sets worldwide have been reported,7,8,9 but their interpretation is hindered by the fact that those reports include all caustic injuries, with no specific focus on caustic ingestion.10 The aim of the present study was to analyze nationwide epidemiology and early outcomes associated with caustic ingestion in France across a 10-year period.
Methods
In line with legislation in France on noninterventional, retrospective data analyses, neither specific written consent nor approval by an independent ethics committee was required for the present study. The study followed the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) guidelines.11
Programme De Médicalisation Des Systèmes D’informations Database
Data were extracted from the French Medical Information System Database Programme De Médicalisation Des Systèmes D’informations (PMSI).12 PMSI is a national prospective database that includes patients from all public and private hospitals in France. It relies on standardized discharge reports following hospital admissions: each report is a collection of 1 or more summaries from each medical unit to which patients were referred to during their hospital stay. Diagnoses are coded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Therapeutic procedures are coded using the Classification Commune des Actes Médicaux (CCAM), which is a national standardized medical and surgical procedures classification.13 As patients may have several hospital stays, each patient is identified in PMSI using a unique anonymous identification number. This number is generated using the patient’s social security number, date of birth, and sex and allows for exhaustive life-long recording of all hospital admissions in France. Because all discharge reports are compulsory and represent the basis of hospitals fundings, the PMSI database is complete, and its validity has been confirmed by cross-referencing with other prospective cohort databases.14,15,16
Patient Identification
Data from January 2010 to December 2019 were extracted from the PMSI database. All patients admitted on an emergency outpatient basis for esophageal caustic ingestion were identified and included in the present study. Esophageal caustic ingestion was defined as primary diagnoses, coded T281 or T286 according to the ICD-10 classification. Pediatric patients aged 15 years and younger and patients with nonvalid unique identification numbers were excluded from the analysis.
Variable and Outcome Definitions
Data regarding patient demographic characteristics was extracted from the database. ICD-10 codes of the associated diagnoses were used to identify any associated psychiatric conditions or comorbidities, which were graded according to the Charlson comorbidity index17,18 (eTable 1 in the Supplement). Psychiatric disease and unintentional ingestion were also recorded (eTable 1 in the Supplement). The nature of ingestion (ie, unintentional or intentional) relied on reporting from patients and coded as X49 according to ICD-10. The presence of psychiatric disorders was defined by ICD-10 codes F0 through F7. These codes were independent. Intensive care unit (ICU) management was recorded together with artificial ventilator assistance and blood transfusion (eTable 2 in the Supplement).
All therapeutic procedures were identified according to the CCAM (eTable 2 in the Supplement). Emergency surgical procedures were categorized as esophagectomy; gastrectomy; colectomy; and small-bowel, spleen, and pancreatic resections. Removal of organs other than the stomach and the esophagus was defined as extended resection. Construction of feeding jejunostomy was also recorded. In the absence of transmural necrosis, patients were offered nonoperative treatment. This included on-demand ICU assistance of vital functions (kidney, circulatory, respiratory), nursing, psychological support, and gradual resumption of oral nutrition.
Mortality and morbidity were defined as in-hospital death and complications, respectively. Complications were recorded according to the ICD-10 codes shown in eTable 3 in the Supplement. Reconstructive surgery was defined as an esophagocoloplasty or gastroplasty procedure during the study period.
Center volume was defined as the number of caustic ingestion incidents per center during the study period. This variable was categorized using the cutoff of tercile to create 3 categories of similar size. According to the number of patients treated per year, centers were graded as low volume (fewer than 2 patients per year), middle volume (2 to 9 patients per year) and high volume (more than 9 patients per year). Using the same method, centers were also categorized by the number of oncologic esophageal resections performed yearly as low volume (fewer than 5 esophageal resections per year), middle volume (5 to 55 esophageal resections per year), and high volume (more than 55 esophageal resections per year). Data on patient referral to another center after initial admission were analyzed. To define center volumes and for further statistical analyses, patients were categorized by center of presentation.
Statistical Analysis
Statistical analysis was performed using R version 4.1.2 (the R Foundation). Descriptive analyses are presented as medians and IQRs or means and SDs for quantitative data and as numbers and percentages for categorical variables. Univariate analyses were performed with general linear models for binary outcomes and linear models for continuous outcomes using the publish package for R version 2020.12.23 (the R Foundation). Multivariate analysis was conducted according to a logistic resection, using a general linear model. All variables with a P value less than .20 in univariate analysis were included in the multivariate model. Multivariate analysis results are presented as odds ratios (ORs) with 95% CIs. All tests were 2-tailed with a level of significance set at P < .05. A correlation matrix was performed to assess collinearity.
Results
Patients
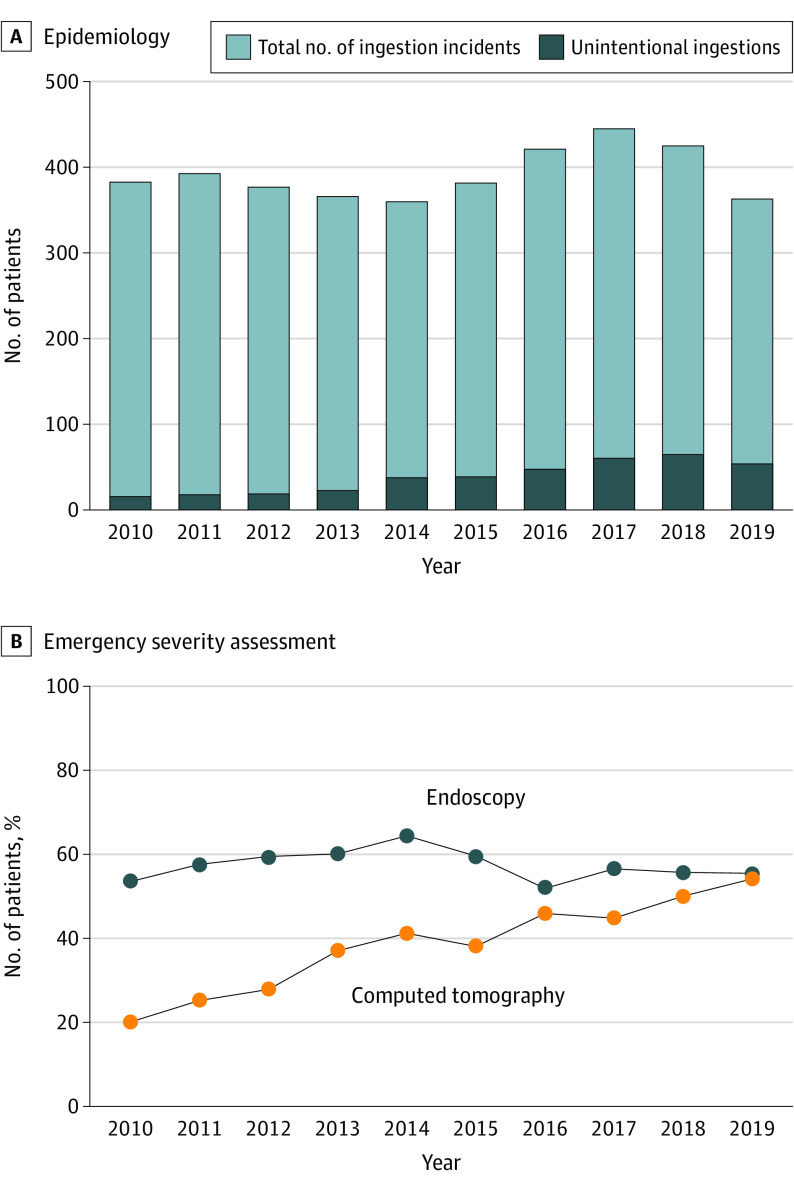
Across the study period, a total of 22 657 226 patients were admitted in hospitals in France on an emergency outpatient basis. Included in this study were 3544 patients (0.016%) who were admitted with caustic ingestion. These patients were treated in a total of 435 hospitals, including 404 low-volume centers (93%), 27 medium-volume centers (6%), and 4 high-volume centers (1%). Overall, 1124 patients (32%) were treated in low-volume centers, 1224 (34%) in medium-volume centers, and 1196 (34%) in high-volume centers. Of 2348 patients admitted in low- and medium-volume centers, 76 (3.2%) were transferred to a larger center; of these, 24 (1%) were transferred within 24 hours and 66 (2.8%) within 48 hours of caustic ingestion. Patient characteristics are shown in Table 1. The median (IQR) age was 49 (34-63) years, and 1685 patients (48%) were women. Ingestion was recorded as unintentional in 381 patients (11%), and 2546 patients (72%) had a history of psychiatric disease. The nature of the ingested agent was specified in 1185 (33%) patients and included 221 acids, 604 alkalis, and 360 other agents. The number of hospital admissions for caustic ingestion per year was stable, while the number of unintentional ingestion incidents increased steadily across the study period. Fewer than 5% (34 of 744) of ingestion incidents were unintentional at the beginning of the study period compared with nearly 20% (119 of 671) at the end of the study period (Figure, A).
Table 1. General Characteristics of 3544 Patients Treated for Caustic Ingestion.
| Characteristic | No. (%) |
|---|---|
| Age, median (range), y | 49 (34-63) |
| Female | 1685 (47.5) |
| Male | 1859 (52.5) |
| Comorbidities | |
| Charlson comorbidity index | |
| 0 | 2617 (73.8) |
| 1-2 | 545 (15.4) |
| 3-4 | 175 (4.9) |
| >4 | 207 (5.8) |
| Congestive heart failure | 81 (2.3) |
| Myocardial infarction | 71 (2.0) |
| Pulmonary disease | 188 (5.3) |
| Diabetes | 186 (5.2) |
| Kidney disease | 79 (2.2) |
| History of cancer | 283 (8.0) |
| Metastatic cancer | 113 (3.2) |
| Psychiatric disease | 2546 (71.8) |
| Unintentional ingestion | 381 (10.8) |
| Volume of caustic ingestion cases per center | |
| High (>9/y) | 1196 (33.7) |
| Middle (2-9/y) | 1224 (34.5) |
| Low (<2/y) | 1124 (31.7) |
| Indirect markers of severity | |
| Intensive care unit admission | 1418 (40.0) |
| Ventilatory assistance in the first 2 d of management | 370 (10.4) |
| Transfusion in the first 2 d of management | 122 (3.4) |
| Surgical management | |
| Emergency resection | 388 (10.9) |
| Esophagogastrectomy | 103 (27) |
| Isolated esophageal resection | 156 (40) |
| Isolated gastric resection | 98 (25) |
| Extended surgerya | 49 (1.4) |
| Aborted resection | 31 (0.9) |
| Nutritional enterostomy without resection | 245 (6.9) |
| Tracheostomy | 202 (5.7) |
Extended resection refers to resection of other organs (duodenum, pancreas, bowel, colon, or spleen) associated with esophageal and gastric resections.
Figure. Changes in Epidemiology and Emergency Severity Assessment Following Caustic Ingestion in Adults in France, 2010-2019.
Emergency Management
Endoscopy was used to assess the severity of caustic injuries in 2033 patients (57%) and computed tomography (CT) in 1355 (38%); 969 (27%) patients had neither CT nor endoscopy. The use of endoscopy was stable throughout the study period. The use of CT increased steadily from 23% (169 of 744 patients) from January 2010 to December 2011 to 52% (349 of 671 patients) from January 2018 to December 2019 (P < .001) (Figure, B).
Surgical resection was performed in 388 patients (11%) during the primary hospital stay and included 156 esophageal resections (40%), 103 esophagogastrectomies (27%), and 98 gastric resections (25%). Extended resection was undertaken in 49 patients (1%) and included 22 pancreatic, 13 colonic, 16 small-bowel, and 18 splenic resections. The resection procedure was aborted in 31 patients (8%) owing to extensive digestive necrosis.
Nonsurgical management was undertaken in 3156 patients (89%). Of these, 1047 patients (33%) were admitted to an ICU, 346 (11%) received vasopressors for circulatory failure, 236 (7.5%) required ventilatory assistance, and 24 (0.8%) underwent kidney filtration. Because of inability to resume oral nutrition, a feeding jejunostomy was constructed in 245 patients not undergoing surgical intervention.
Early Outcomes
A total of 1198 patients (34%) experienced complications, and 294 (8%) died. Pulmonary complications were the most frequent adverse events, occurring in 869 patients (24%). During emergent management, 1418 patients (40%) required ICU admission. Preoperative respiratory assistance was necessary in 370 patients (10%), and 122 patients (3%) required blood transfusion. Overall, 202 patients (6%) underwent tracheotomy for the management of respiratory complications.
Among patients who underwent surgery for digestive necrosis, 294 (76%) experienced complications, and 96 (25%) died. Mortality rates associated with esophagectomy, gastrectomy, esophagogastrectomy, extended resection, and aborted surgery were 17%, 17%, 21%, 37%, and 100%, respectively. Among 3156 patients who underwent nonsurgical treatment, in-hospital mortality and morbidity rates were 6% (n = 198) and 29% (n = 904), respectively (Table 2).
Table 2. Postingestion Outcomes in 3544 Patients Treated for Caustic Ingestion.
| Outcome | No. (%) | ||
|---|---|---|---|
| Overall population | Emergent surgical resection | ||
| Yes | No | ||
| No. | 3544 | 388 | 3156 |
| In-hospital mortality | 294 (8.3) | 96 (24.7) | 198 (6.3) |
| In-hospital morbidity | 1198 (33.8) | 294 (75.8) | 904 (28.6) |
| Hemorrhage | 64 (1.8) | 30 (7.7) | 34 (1.1) |
| Deep abscess | 124 (3.5) | 43 (11.1) | 81 (2.6) |
| DVT and PE | 147 (4.1) | 46 (11.9) | 101 (3.2) |
| Pulmonary complication | 869 (24.5) | 234 (60.3) | 635 (20.1) |
| Kidney failure | 204 (5.8) | 67 (17.3) | 137 (4.3) |
Abbreviations: DVT, deep vein thrombosis; PE, pulmonary embolism.
Results of univariate analysis regarding postingestion mortality risk factors are shown in Table 3. Correlation matrix between variables are shown in the eFigure in the Supplement. On multivariate analysis, independent predictors of mortality included older age (OR, 1.06; 95% CI, 1.05-1.07; P < .001), higher comorbidity score (OR, 1.14; 95% CI, 1.08-1.20; P < .001), suicidal ingestion (OR, 3.45; 9%% CI, 1.85-7.14; P < .001), ICU admission (OR, 4.42; 95% CI, 3.17-6.21; P < .001), emergency surgery for digestive necrosis (OR, 3.44; 95% CI, 2.47-4.78; P < .001), and treatment in low-volume centers (OR, 1.45; 95% CI, 1.01-2.08; P = .04).
Table 3. In-Hospital Factors Associated With Risk of Mortality Among 3544 Patients Treated for Caustic Ingestion.
| Factor | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| No. (%) | P value | OR (95% CI) | P value | ||
| Alive | Dead | ||||
| No. | 3250 | 294 | |||
| Age, median (IQR), y | 47 (32-61) | 65 (55-78) | <.001 | 1.06 (1.05-1.07) | <.001 |
| Female | 1537 (47.3) | 148 (50.3) | .35 | NA | NA |
| Male | 1,713 (52.7) | 146 (49.7) | .35 | NA | NA |
| Charlson comorbidity index, mean (SD) | 0.8 (1.9) | 1.5 (2.6) | <.001 | 1.14 (1.08-1.20) | <.001 |
| Unintentional ingestion | 371 (11.4) | 10 (3.4) | <.001 | 0.29 (0.14-0.54) | <.001 |
| Intensive care unit admission | 992 (30.5) | 181 (61.6) | <.001 | 4.42 (3.17-6.21) | <.001 |
| Emergency resection for necrosis | 292 (9.0) | 96 (32.7) | <.001 | 3.44 (2.47-4.78) | <.001 |
| Center volume | |||||
| High (>9 patients/y) | 1114 (34.3) | 82 (27.9) | NA | [Reference] | |
| Middle (2-9 patients/y) | 1111 (34.2) | 113 (38.4) | .08 | 1.21 (0.87-1.69) | .26 |
| Low (<2 patients/y) | 1025 (31.5) | 99 (33.7) | NA | 1.45 (1.01-2.08) | .04 |
Abbreviations: NA, not applicable; OR, odds ratio.
Results of univariate analysis regarding postingestion morbidity risk factors are shown in Table 4. On multivariate analysis, independent predictors of morbidity included older age (OR, 1.02; 95% CI, 1.02-1.03; P < .001), higher comorbidity score (OR, 1.07; 95% CI, 1.03-1.11; P < .001), ICU admission (OR, 8.07; 95% CI, 6.72-9.70; P < .001), and emergency surgery for digestive necrosis (OR, 2.82; 95% CI, 2.16-3.71; P < .001).
Table 4. In-Hospital Factors Associated With Risk of Morbidity Among 3544 Patients Treated for Caustic Ingestion.
| Factor | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Morbidity, No. (%) | P value | OR (95% CI) | P value | ||
| No | Yes | ||||
| No. | 2346 | 1198 | NA | NA | NA |
| Age, median (IQR), y | 46 (31-61) | 53 (41-66) | <.001 | 1.02 (1.02-1.03) | <.001 |
| Female | 1118 (47.7) | 567 (47.3) | .88 | NA | NA |
| Male | 1228 (52.3) | 631 (52.7) | .88 | NA | NA |
| Charlson comorbidity index, mean (SD) | 0.8 (2.0) | 0.9 (2.1) | .20 | 1.07 (1.03-1.11) | <.001 |
| Unintentional ingestion | 280 (11.9) | 101 (8.4) | .002 | 0.79 (0.59-1.04) | .08 |
| Intensive care unit admission | 544 (23.2) | 874 (73.0) | <.001 | 8.07 (6.72-9.70) | <.001 |
| Emergency resection for necrosis | 94 (4.0) | 294 (24.5) | <.001 | 2.82 (2.16-3.71) | <.001 |
| Center volume | <.001 | ||||
| High (>9 patients/y) | 748 (31.9) | 448 (37.4) | [Reference] | NA | |
| Middle (2-9 patients/y) | 787 (33.5) | 437 (36.5) | 0.82 (0.67-1.01) | .06 | |
| Low (<2 patients/y) | 811 (34.6) | 313 (26.1) | 0.98 (0.79-1.21) | .83 | |
Abbreviations: NA, not applicable; OR, odds ratio.
Mortality and morbidity analyses were performed using center categorization according to the number of oncological esophageal resections per year and yielded similar results (eTables 4 and 5 in the Supplement). The management of caustic ingestion in centers performing fewer than 5 esophageal resections per year was an independent predictor of mortality. Morbidity and mortality rates were not different between patients who ingested acids vs those who ingested alkalis (eTable 6 in the Supplement).
Therapeutic Endoscopy and Esophageal Reconstruction
Therapeutic endoscopy was used for stricture management in 409 patients (12%); of these, 323 patients underwent dilation alone, 19 underwent stenting alone, and 67 underwent both dilation and stenting. Patients underwent a median (IQR) of 3 (1-5) endoscopic procedures.
Reconstructive surgery was undertaken in 456 patients (13%) (eTable 7 in the Supplement). The median (IQR) delay in reconstruction was 6 (3- 10) months. Esophageal reconstruction was performed using the stomach in 113 patients, including 39 Ivor Lewis operations, 58 McKeown procedures, and 16 retrosternal gastroplasties. Esophageal reconstruction with the colon was performed in 343 patients, and esophagocolonic anastomoses were located in the neck in all patients. Esophageal reconstruction was undertaken in high-, middle-, and low-volume centers in 223 patients (49%), 204 patients (45%) and 29 patients (6%), respectively. Following esophageal reconstruction, 323 patients (71%) experienced in-hospital complications, and 22 patients (5%) died. In-hospital morbidity and mortality rates were similar after esophageal reconstruction with the stomach and the colon (eTables 4 and 5 in the Supplement).
Hospital Readmissions
During follow-up, 2577 patients (73%) required at least 1 hospital readmission. The median (IQR) number of hospital readmissions in these patients was 4 (2-9).
Discussion
This nationwide study reports early management of and outcomes associated with caustic ingestion in a cohort of 3544 patients admitted in hospitals in France from 2010 to 2019. These patients represented 0.016% of all emergency outpatient admissions in France during the same period. There is a general consensus in France that caustic ingestion requires hospital admission.19 Thus, it is highly probable that the percentage of patients lost (ie, dead before admission or receiving no medical consultation) is minimal and that those figures reliably mirror the clinical reality in the country. Our data highlight interesting modifications in ingestion patterns and emergency management of caustic injuries over time. First, we found a constant increase of unintentional ingestion incidents during a period when the overall annual caseload was globally stable. There is no clear explanation for this finding; no specific education programs have been implemented and no effective measures limiting access to strong caustic agents were taken in France during the study period. Second, we found a constant increase of CT use in the emergency evaluation of caustic injuries. This finding underscores the clinical impact of recent publications, which showed that CT outperformed endoscopy in detecting transmural caustic necrosis,1,4,20,21 leading to an endorsement of CT-based management algorithms by specialized teams.22,23,24 The lack of examinations (CT and/or endoscopy) in more than one-fourth of patients was surprising. It can be postulated that the ingested amount was minimal in some patients, who would have then not required investigation or specific therapy and their inclusion in the study may be questioned. However, systematic investigation of caustic ingestion incidents is recommended, as ingested amounts are usually unknown or unreliable, and symptoms are poorly associated with the severity of digestive injuries. Absence of emergency investigation was most likely owing to lack of availability—that is, a number of small hospitals do not have 24-hour CT or endoscopy access—combined with misinterpretation of the emergency degree by the medical team. High mortality (8.3%) and morbidity (28%) rates in this specific population support this hypothesis.
Even though most ingestion incidents in this study (89%) were intentional and more severe outcomes might be expected, most patients (89%) were treated nonsurgically. Several factors may explain this finding. In many cases, the reason for suicide attempt is not a real desire to die; pain and last-minute changes of mind may limit ingested amounts. Oxidants induce less severe damage than acids and alkalis, even if ingested intentionally. Of note, these figures are in accordance with recent reports showing constant decline of surgical approaches in the emergency setting.
We reported postingestion mortality and morbidity rates of 8% and 34%, respectively. Mortality and morbidity increased in patients who required surgery for digestive necrosis; mortality rates were associated with the extent of digestive involvement. Multivariate analysis showed that outcomes were associated with patient factors (ie, age, comorbidity score, and suicide) and the severity of caustic injuries (ie, the need for surgery or ICU management). These results are in accordance with published data regarding outcomes of emergency surgery for caustic injuries.1
A major finding was the significant improvement of in-hospital survival in patients treated in high-volume centers. During the last 20 years, a large number of publications have shown major benefits associated with increased hospital and surgeon volumes on perioperative outcomes among patients undergoing high-risk elective25,26 and emergency operations.27,28 Worldwide, there is a current trend toward centralization of high-risk procedures, and minimal surgeon and hospital thresholds are regularly defined for esophageal,29 pancreatic,30 liver,31 and rectal32 resections. To our knowledge, the present study is the first to suggest that emergency treatment in high-volume centers might benefit patients with adverse outcomes associated with caustic ingestion. Such survival benefits may be associated with a better selection of patients for surgery, improved intraoperative and postoperative management strategies, and wide access to multidisciplinary management. In view of these findings, the very low emergency referral rate of caustic injuries to larger centers in France is of concern; it may also represent a lever that can be operated to improve patient outcomes.
In contrast, only 6% of esophageal reconstruction procedures were done in low-volume centers. This may suggest that esophageal reconstructions are perceived as difficult procedures by surgeons who spontaneously refer them to expert teams; it could also explain why early results after esophageal reconstruction in this national study are comparable with those reported by highly specialized centers.1 Although the study design did not allow for specific analysis of long-term results, performing esophageal reconstruction in highly specialized units may also benefit nutritional outcomes. The high readmission rate in this study may indicate the long-term impact of caustic ingestion on patients’ lives. Although the study design did not allow for measurement of direct correlation between hospital readmission and caustic ingestion episode, the use of health resources was unexpectedly high compared with population age and comorbidities.
Limitations
This study has limitations. First, we used an administrative database used for financial rather than research purposes; this may render questionable the accuracy and completeness of data coding. Nevertheless, the PMSI database used for hospital budget allocation undergoes regular controls to limit the risk of overcoding and has proven accurate with internal and external quality control.25 Second, the PMSI-based study design did not allow for patient follow-up and thus we could not provide long-term nutritional and survival analysis. This is a major drawback, as it has been previously shown that survival and functional results in patients with severe caustic injuries tend to deteriorate over time.3 Moreover, as PMSI only codes in-hospital mortality, the analysis could be biased by exclusion of out-of-hospital fatalities. The PMSI database does not calculate ICU severity scores at admission (eg, the Acute Physiology and Chronic Health Evaluation [APACHEII] or the Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity [POSSUM]) that could help identify patients who are most likely to benefit from early-stage referral to a high-volume center. Further, the registry-based study design did not allow for a patient-tailored management algorithm. In addition to patients from low-volume centers, some patients from middle-volume centers might benefit from transfer to high-volume facilities; presence of extensive damage (eg, pancreatic and duodenal necrosis or airway involvement) should be considered for transfer or at least discussed with a high-volume center staff. Increasing incidents of unintentional ingestion over time cannot be explained by the present study; cultural or familial factors may be involved but could not be assessed as the PMSI database does not include this kind of information.
Conclusions
In this study, rates of hospital mortality and morbidity after caustic ingestion were high and were associated with patient characteristics and the severity of initial injuries. Over the last decade, caustic ingestion patterns have changed, with a progressive increase of unintentional ingestion incidents. In parallel, computed tomography evaluation is progressively replacing endoscopy in emergency management protocols. In this study, referral to expert centers was associated with early survival after caustic ingestion. If feasible, low-volume hospitals should transfer patients to larger centers instead of attempting on-site management.
eTable 1. Charlson comorbidity score calculation and codes used for description of other comorbidities
eTable 2. CCAM codes used for definition of variables
eTable 3. ICD-10 codes used to define complication during the management
eTable 4. In-hospital mortality risk factors of 3544 patients managed for caustic ingestion. Centers were categorized according to the number of oncologic esophageal resections per year in low (0-5 esophagectomies/year), middle (5-55 esophagectomies/year) and high (>55 esophagectomies/year) volume
eTable 5. In-hospital morbidity risk factors of 3544 patients managed for caustic ingestion. Centers were categorized according to the number of oncologic esophageal resections per year in low (0-5 esophagectomies/year), middle (5-55 esophagectomies/year) and high (>55 esophagectomies/year) volume
eTable 6. Early outcomes according to the nature of the ingested agent. Data were available for 1185 patients (33%) of whom 221 have ingested acids and 604 alkalis and 260 other agents
eTable 7. Characteristics and outcomes of 456 patients who underwent esophageal reconstruction after caustic ingestion with the colon (n=343) and the stomach (n=113)
eFigure. Correlation matrix of variables included in the logistic regression model
References
- 1.Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. Lancet. 2017;389(10083):2041-2052. doi: 10.1016/S0140-6736(16)30313-0 [DOI] [PubMed] [Google Scholar]
- 2.Chirica M, Resche-Rigon M, Zagdanski AM, et al. Computed tomography evaluation of esophagogastric necrosis after caustic ingestion. Ann Surg. 2016;264(1):107-113. doi: 10.1097/SLA.0000000000001459 [DOI] [PubMed] [Google Scholar]
- 3.Chirica M, Resche-Rigon M, Bongrand NM, et al. Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg. 2012;256(6):994-1001. doi: 10.1097/SLA.0b013e3182583fb2 [DOI] [PubMed] [Google Scholar]
- 4.Bruzzi M, Chirica M, Resche-Rigon M, et al. Emergency computed tomography predicts caustic esophageal stricture formation. Ann Surg. 2019;270(1):109-114. doi: 10.1097/SLA.0000000000002732 [DOI] [PubMed] [Google Scholar]
- 5.Cheng HT, Cheng CL, Lin CH, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008;8:31. doi: 10.1186/1471-230X-8-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chirica M, Veyrie N, Munoz-Bongrand N, et al. Late morbidity after colon interposition for corrosive esophageal injury: risk factors, management, and outcome. a 20-years experience. Ann Surg. 2010;252(2):271-280. doi: 10.1097/SLA.0b013e3181e8fd40 [DOI] [PubMed] [Google Scholar]
- 7.Abbas A, Brar TS, Zori A, Estores DS. Role of early endoscopic evaluation in decreasing morbidity, mortality, and cost after caustic ingestion: a retrospective nationwide database analysis. Dis Esophagus. 2017;30(6):1-11. doi: 10.1093/dote/dox010 [DOI] [PubMed] [Google Scholar]
- 8.Li Y, Langworthy J, Xu L, et al. Nationwide estimate of emergency department visits in the United States related to caustic ingestion. Dis Esophagus. 2020;33(6):doaa012. doi: 10.1093/dote/doaa012 [DOI] [PubMed] [Google Scholar]
- 9.Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th annual report. Clin Toxicol (Phila). 2020;58(12):1360-1541. doi: 10.1080/15563650.2020.1834219 [DOI] [PubMed] [Google Scholar]
- 10.Hoffman RS, Burns MM, Gosselin S. Ingestion of caustic substances. N Engl J Med. 2020;382(18):1739-1748. doi: 10.1056/NEJMra1810769 [DOI] [PubMed] [Google Scholar]
- 11.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee . The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Domin J-P. Le Programme de médicalisation des systèmes d’information (PMSI). Histoire, médecine et santé. 2013;4:69-87. doi: 10.4000/hms.355 [DOI] [Google Scholar]
- 13.Assurance Maladie. Classification Commune des Actes Médicaux (CCAM). Assurance Maladie. Accessed February 12, 2021. http://www.ameli.fr/accueil-de-la-ccam/telechargement/version-actuelle/index.php
- 14.Quantin C, Cottenet J, Vuagnat A, et al. Quality of perinatal statistics from hospital discharge data: comparison with civil registration and the 2010 National Perinatal Survey. Qualité des données périnatales issues du PMSI: comparaison avec l’état civil et l’enquête nationale périnatale 2010. J Gynecol Obstet Biol Reprod (Paris). 2014;43(9):680-690. doi: 10.1016/j.jgyn.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 15.Quantin C, Benzenine E, Hägi M, et al. Estimation of national colorectal-cancer incidence using claims databases. J Cancer Epidemiol. 2012;2012:298369. doi: 10.1155/2012/298369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pierron A, Revert M, Goueslard K, et al. Evaluation of the metrological quality of the medico-administrative data for perinatal indicators: A pilot study in 3 university hospitals. Évaluation de la qualité métrologique des données du programme de médicalisation du système d’information (PMSI) en périnatalité : étude pilote réalisée dans 3 CHU. Rev Epidemiol Sante Publique. 2015;63(4):237-246. doi: 10.1016/j.respe.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 17.Charlson M, Wells MT, Ullman R, King F, Shmukler C. The Charlson comorbidity index can be used prospectively to identify patients who will incur high future costs. PLoS One. 2014;9(12):e112479. doi: 10.1371/journal.pone.0112479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 19.Fieux F, Chirica M, Villa A, Losser MR, Cattan P. Ingestion de produits caustiques chez l’adulte. Réanimation. 2009;18(7):606-616. doi: 10.1016/j.reaurg.2009.08.003 [DOI] [Google Scholar]
- 20.Chirica M, Resche-Rigon M, Pariente B, et al. Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg Endosc. 2015;29(6):1452-1461. doi: 10.1007/s00464-014-3823-0 [DOI] [PubMed] [Google Scholar]
- 21.Chirica M, Bonavina L, Cattan P. Ingestion of caustic substances. N Engl J Med. 2020;383(6):600. doi: 10.1056/NEJMc2019467 [DOI] [PubMed] [Google Scholar]
- 22.Bonavina L, Chirica M, Skrobic O, et al. Foregut caustic injuries: results of the world society of emergency surgery consensus conference. World J Emerg Surg. 2015;10:44. doi: 10.1186/s13017-015-0039-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gill M, Tee D, Chinnaratha MA. Caustic ingestion: has the role of the gastroenterologist burnt out? Emerg Med Australas. 2019;31(3):479-482. doi: 10.1111/1742-6723.13278 [DOI] [PubMed] [Google Scholar]
- 24.Kalayarasan R, Ananthakrishnan N, Kate V. Corrosive ingestion. Indian J Crit Care Med. 2019;23(suppl 4):S282-S286. doi: 10.5005/jp-journals-10071-23305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Amrani M, Lenne X, Clement G, et al. Specificity of procedure volume and its association with postoperative mortality in digestive cancer surgery: a nationwide study of 225 752 patients. Ann Surg. 2019;270(5):775-782. doi: 10.1097/SLA.0000000000003532 [DOI] [PubMed] [Google Scholar]
- 26.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128-1137. doi: 10.1056/NEJMsa012337 [DOI] [PubMed] [Google Scholar]
- 27.Brown JB, Rosengart MR, Kahn JM, et al. Impact of volume change over time on trauma mortality in the United States. Ann Surg. 2017;266(1):173-178. doi: 10.1097/SLA.0000000000001838 [DOI] [PubMed] [Google Scholar]
- 28.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285(9):1164-1171. doi: 10.1001/jama.285.9.1164 [DOI] [PubMed] [Google Scholar]
- 29.Clark JM, Cooke DT, Hashimi H, et al. Do the 2018 Leapfrog Group minimal hospital and surgeon volume thresholds for esophagectomy favor specific patient demographics? Ann Surg. 2019. doi: 10.1097/SLA.0000000000003553 [DOI] [PubMed] [Google Scholar]
- 30.El Amrani M, Clement G, Lenne X, et al. Failure-to-rescue in patients undergoing pancreatectomy: is hospital volume a standard for quality improvement programs? nationwide analysis of 12 333 patients. Ann Surg. 2018;268(5):799-807. doi: 10.1097/SLA.0000000000002945 [DOI] [PubMed] [Google Scholar]
- 31.Ardito F, Famularo S, Aldrighetti L, et al. ; HERCOLES group . The impact of hospital volume on failure to rescue after liver resection for hepatocellular carcinoma: analysis from the HERCOLES Italian registry. Ann Surg. 2020;272(5):840-846. doi: 10.1097/SLA.0000000000004327 [DOI] [PubMed] [Google Scholar]
- 32.El Amrani M, Clement G, Lenne X, et al. The impact of hospital volume and charlson score on postoperative mortality of proctectomy for rectal cancer: a nationwide study of 45 569 patients. Ann Surg. 2018;268(5):854-860. doi: 10.1097/SLA.0000000000002898 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Charlson comorbidity score calculation and codes used for description of other comorbidities
eTable 2. CCAM codes used for definition of variables
eTable 3. ICD-10 codes used to define complication during the management
eTable 4. In-hospital mortality risk factors of 3544 patients managed for caustic ingestion. Centers were categorized according to the number of oncologic esophageal resections per year in low (0-5 esophagectomies/year), middle (5-55 esophagectomies/year) and high (>55 esophagectomies/year) volume
eTable 5. In-hospital morbidity risk factors of 3544 patients managed for caustic ingestion. Centers were categorized according to the number of oncologic esophageal resections per year in low (0-5 esophagectomies/year), middle (5-55 esophagectomies/year) and high (>55 esophagectomies/year) volume
eTable 6. Early outcomes according to the nature of the ingested agent. Data were available for 1185 patients (33%) of whom 221 have ingested acids and 604 alkalis and 260 other agents
eTable 7. Characteristics and outcomes of 456 patients who underwent esophageal reconstruction after caustic ingestion with the colon (n=343) and the stomach (n=113)
eFigure. Correlation matrix of variables included in the logistic regression model