Abstract
Social determinants of health, including neighborhood factors, play a key role in the health of diverse older adults. However, few longitudinal studies have examined the role of neighborhood racial/ethnic segregation on cognitive decline in diverse samples. We examined older non-Hispanic White (NHW), Black, and Latino participants evaluated at an Alzheimer’s Disease Research Center. Neighborhood racial/ethnic segregation was measured using the Getis-Ord Gi* statistic, a spatial measure of clustering that was created for Latino and Black clustering separately. Cognitive outcomes included episodic memory, semantic memory, and executive function. We used mixed effects multivariable regression models to evaluate associations between segregation and cognitive function and decline. We had 452 individuals: 46% NHW, 26% Black, and 21% Latino in 309 census tracts with an average of 5.2 years of follow-up data (range 0.6–15.0). In analyses that adjusted for a variety of covariates (including neighborhood SES), individuals in neighborhoods with a higher clustering of Latino residents (higher Gi* statistic) had slower declines over time on semantic memory and those in neighborhoods with a higher clustering of Black residents had slower declines over time on episodic memory. In race-stratified adjusted analyses: for Black participants, the association between clustering and cognition was present for episodic memory and executive function, showing lower baseline scores in highly clustered Black and Latino neighborhoods, respectively. There was no association with cognitive change. Among Latino participants, highly clustered Latino neighborhoods were associated with lower baseline scores in semantic memory, but slower declines in episodic memory; Latinos living in neighborhoods with a greater clustering of Black residents also had slower declines in episodic memory. Among NHWs, residing in neighborhoods with a higher clustering of Latino residents was associated with slower declines over time on semantic memory. Segregated neighborhoods may be differentially associated with cognitive outcomes depending on individual race/ethnicity.
Keywords: Residential segregation, Race/ethnicity, Cognition, Neighborhoods, Disparities
INTRODUCTION
The increase of both ethnically diverse and older adult populations is predicted to be significant over the coming years. Moreover, the Hispanic/Latino and Black/African American populations (henceforth Latino and Black) have been projected to grow significantly (114.8% and 63.6% respectively, between 2014–2060).1 Given this growth in the older adult population in general, and Black and Latino adults specifically, it is imperative that we understand the risks for cognitive impairment in these populations given their higher prevalence of Alzheimer’s disease (AD).2 Many studies have denoted the individual characteristics associated with cognitive impairment related to dementia including age, education, genetics, and medical conditions such as cardiovascular disease.3,4 However, a growing body of research has demonstrated the important role of social determinants of health, including neighborhood racial/ethnic characteristics on older adults’ general health,5 depression,6 mortality,7 and more recently- cognition.8,9 Contextual factors play an important role in health disparities but up until only recently, have been understudied in cognition. Given that some contextual factors may be modified by public health policy and intervention, it is important that their role be elucidated in AD research.
Williams and Collins (2001)10 posited that racial segregation, or the spatial separation of groups, is a fundamental cause of health disparities among Black populations. Segregation, one form of structural racism that existed prior to the 1960’s, was pervasive and enforced by social and public policies such as the Jim Crow laws and the historical act of redlining, which directly played a role in the segregation of neighborhoods by race and socioeconomic status (SES) through involvement of the national mortgage market.11,12 Neighborhoods that are segregated and thus disenfranchised experience higher levels of poverty and policing/crime. When certain groups of people are systematically placed into environments that are exposed to higher levels of policing/crime, individuals tend to socially isolate from each other which limits their interactions. 13 The limitation on diverse social interactions, in turn, inhibits potential for cognitive growth and stimulation. Segregation has created distinct social environments in that most poor Black adults reside in neighborhoods of concentrated poverty.10 Similarly, Latinos are disproportionately exposed to neighborhood disadvantage, which may have detrimental consequences for their health.14,15 Oftentimes, concentrated poverty is linked to poor cognitive functioning due to the lack of resources like higher quality education, access to health care, better job opportunities, healthy grocery stores (including fresh produce), and safe recreational and greenspace areas, all of which can impact health and cognition.16
On the other hand, residential segregation may lead to ethnically clustered neighborhoods, or ethnic enclaves, characterized by high social capital or cohesion.17,18 This theoretical perspective assumes a positive effect of living within a neighborhood characterized by a high concentration of individuals from similar backgrounds through the creation of social networks and the diffusion of positive cultural practices.19–22 At the neighborhood level, social capital is composed of collective resources accessible to groups of people within a social structure that allows for achieving common goals.23 Ethnically homogeneous Latino neighborhoods are associated with higher self-rated health,22 lower risk of mortality,24–26 fewer depressive symptoms,17,20 and healthier dietary habits.27 In Philadelphia, Black mortality was lower among residents of predominantly Black neighborhoods with high neighborhood social capital in comparison to Black residents living in predominantly White neighborhoods.28 It may be that residents in ethnically homogeneous neighborhoods benefit from shared psychosocial resources, social organization and control, preservation of culture, common language, and healthful traditional behavioral norms,17,22,24,27 as well as high rates of labor force participation, intact family structures, home ownership, and residential stability.29 Latino and Black residents living in homogeneous neighborhoods were more likely to use health care services than those living in heterogeneous communities.30 This collective capital may contribute to better cognitive health.31
These two theoretical perspectives and subsequent predicted outcomes may vary because of the different ways that segregation has been measured. There are formal measures of segregation, namely evenness, exposure, concentration, centralization, and clustering.32 Evenness captures the level of differential spatial distribution of groups: racial/ethnic minorities are overrepresented in some areas and underrepresented in others. Exposure refers to the probability of interacting with other groups. Concentration measures the physical space inhabited by certain groups. Centralization indicates the degree to which a group is located at the center of an area. Finally, clustering refers to the level that groups might form one large contiguous enclave, or be scattered widely around the urban area. Then, there are proxies of segregation, such as racial/ethnic composition of neighborhoods. Segregation and composition are conceptually different.33 The former relates to how two or more groups distribute spatially across neighborhoods within a large area (e.g., a metropolitan area), whereas the latter refers to the relative size of racial/ethnic groups in an area (i.e., racial composition). It is important to distinguish these categorizations in empirical studies of residential segregation. We highlight the different ways that segregation has been assessed to provide a context for understanding studies on segregation and health outcomes.
Using data from the Health and Retirement Study (HRS), Aneshensel and colleagues (2011)34 showed that late middle-aged adults living in highly segregated Black communities had poor cognitive function at baseline; however, this was the case only if they had low education. In contrast, the highest level of cognitive functioning was among highly educated persons who lived in predominantly Black neighborhoods. In that study, racial/ethnic segregation was operationalized as the proportion of residents who were Black and proportion of residents who were Latino. Kovalchik and colleagues (2015)9 expanded on this work by using multiple waves of HRS data and by examining both informal (census tract racial/ethnic composition) and formal (county-level isolation index) measures of segregation. They found that both Latino composition and segregation were positively correlated with cognitive function (cognition at baseline) and negatively correlated with cognitive decline (cognition over time) for all older adults- NHW, Black, and Latino. The cross-sectional finding suggested that there may be higher levels of social integration and cultural resources that protect people, regardless of their race/ethnicity, in Latino communities.35 The longitudinal finding, however, showed a steeper rate of decline (over time) in these neighborhoods. Recently, Caunca and colleagues (2020)8 examined life-course or long-term residential segregation of Black participants in CARDIA. They found that the longer Black participants were segregated in young adulthood, the worse their processing speed was in midlife.
Given the paucity of longitudinal studies on cognition, it is unclear how residential segregation is associated with cognitive trajectories of its diverse residents. The goal of this study is to examine the association of neighborhood segregation on cognitive function (cross-sectionally as measured at study baseline) and cognitive decline over time in a diverse cohort of older NHWs, Latinos, and Blacks. We add to the literature on neighborhood and cognition by considering the impact of racial/ethnic segregation and contrasting the potential effects of segregation and ethnic enclaves. Moreover, the cognitive outcomes of living in distinct neighborhoods may impact residents differently, as posited by the ecological framework principle- that the same environment has systematically different effects on people depending upon their personal characteristics.36 Given these unique individual-environment interactions, we additionally stratify our analyses based on individual race/ethnicity. Thus, we hypothesized that greater neighborhood segregation would be associated with baseline cognition and change in cognition over time and that the associations would vary by race/ethnicity. However, relevant prior studies and theoretical underpinnings are currently insufficient to hypothesize specific directions for the associations.
METHODS
Sample
The sample comprised 452 participants in an ongoing longitudinal study with complete address data at the University of California, Davis (UCD) Alzheimer’s Disease Center (ADC). All participants were followed approximately annually (Mean: 1.35 years; SD=0.57) and had at least two evaluations with a mean of 5.4 visits (SD: 2.9) and a range of 2–10 visits. Participants were recruited into the UCD ADRC through two routes: 1) memory clinic referrals and 2) community outreach. Approximately 81% of participants were recruited through community-based recruitment protocols designed to enhance racial/ethnic diversity as well as the spectrum of cognitive dysfunction (normal cognition, mild cognitive impairment: MCI, and dementia). Recruiters utilized various outreach methods such as soliciting in a community hospital lobby, a community survey, health fairs or word of mouth. The other 19% of the sample initially sought a clinical evaluation at the UCD ADC and subsequently were recruited for this study; these individuals predominantly had a clinical diagnosis of MCI. Further details regarding our recruitment methods have been articulated by Hinton et al. (2010).37
Inclusion criterion was ability to speak English or Spanish. Exclusion criteria included unstable major medical illness, such as severe heart disease, major psychiatric disorders (history of schizophrenia, bipolar disorder, or recurrent major depression), active cancer with chemotherapy, and active substance abuse and dependence disorders, all assessed in a clinical exam by a physician. This study was approved by the institutional review board at UCD and all participants provided informed consent.
Clinical evaluations.
All participants received multidisciplinary diagnostic evaluations at baseline and at approximately annual intervals. All evaluations followed the same protocol and included a detailed medical history and a physical and neurological exam. A bilingual physician examined participants who only spoke Spanish. Family members or other close informants were interviewed to obtain information about levels of independent functioning for the participants. Clinical neuropsychological evaluation using standard neuropsychological tests (distinct from the outcome measures used in this study) was performed at each visit. Routine dementia work-up laboratory tests were obtained at the baseline evaluation for all participants and when clinically indicated at the time of follow-up evaluations. Diagnosis of cognitive syndrome included normal cognition, MCI, and dementia based on standard diagnostic criteria. Each case at baseline was initially diagnosed at a consensus conference by the clinical team evaluating the participant. Those appearing likely to be eligible for this study were then reviewed at a second, multidisciplinary case adjudication conference. Follow-up cases were diagnosed at a case conference of the clinical team examining the participant, and in addition, were reviewed at a case adjudication conference when the examining team identified a change in the diagnosis. All diagnoses were made blind to research neuropsychological testing.
The Clinical Dementia Rating 38 was completed on the basis of a standardized interview with the identified participant and an informant; the sum of individual items or boxes (CDRSum) was used as a continuous measure of clinical status. The CDR was completed blind to other evaluation results including clinical and research neuropsychological test results, the physical and neurological exam, and the clinical diagnosis.39
Cognitive outcomes.
The cognitive outcomes in this study were from the Spanish and English Neuropsychological Assessment Scales (SENAS) and were administered at all evaluations. The SENAS has undergone extensive development as a battery of cognitive tests relevant to diseases of aging.40–43 Modern psychometric methods based on item response theory were used to create psychometrically matched measures across different scales, across English and Spanish versions, and that were appropriate for individuals with diverse education levels. This study used a subset of SENAS tests to measure three cognitive domains affected by diseases of aging: executive function, semantic memory, and episodic memory. Executive function is a composite measure constructed from component tasks of category fluency (number of animals named in 60 seconds), phonemic (letter) fluency (words beginning with the/f/sound, words beginning with the/l/sound), and working memory (digit-span backward, visual-span backward, list sorting). Semantic memory is a composite of highly correlated verbal (object-naming) and nonverbal (picture- association) tasks. Episodic memory is a composite score derived from a multi-trial word- list-learning test (Word List Learning 1).40 There were three alternate forms of the word list learning task used; these forms were alternated in the longitudinal evaluations to control for practice effects. SENAS scores are presented in z- score like units (derived from a larger sample) where a score of zero corresponds to the mean and differences from the mean are expressed in standard deviation units. Measure development and psychometric characteristics are described in more detail elsewhere.40,42,44
Neighborhood variables.
Similar to prior research, neighborhoods were categorized by census tracts, an administrative boundary designated by the U.S. Census Bureau.45 There were 309 census tracts in the present sample of 452 participants. We used QGIS and the MMQGIS plug-in to geocode participant addresses (at baseline) along the US Census Bureau’s road network for the relevant counties to merge with the data from the 2010 U.S. Census Tract.46,47 Geocoding was checked for quality assurance.
Measures of residential segregation have traditionally focused on numerical indices that capture various dimensions of the distribution of population groups across metropolitan areas such as evenness (dissimilarity), exposure, isolation, centralization, and concentration.48,49 While these measures accurately represent the overall pattern of population distribution in a particular area, they do not account for spatial dependence or patterns of localized clustering. Recently, the focus of residential segregation studies has shifted to various applications of geospatial statistical methods to characterize and map those patterns.50,51 In this study, neighborhood-level residential segregation was assessed using both global and local spatial clustering measures. Spatial clustering diagnostics of the data on race/ethnicity was performed using global spatial autocorrelation measures including the Getis-Ord General G52 and global Moran’s I.53,54 Diagnostic tests resulted in high positive z-score values for both Black (G = 0.000615, p < 0.000; Moran’s I = 0.385, p < 0.000) and Latino participants (G = 0.000632, p < 0.000; Moran’s I = 0.237, p < 0.000), indicating significant spatial clustering of high percentage values for both groups. The local Getis-Ord Gi* statistic is a widely accepted measure of spatial clustering, also known as hotspot analysis.52,55 The measure was computed in ArcGIS® using the Hot Spot Analysis Tool.
The Gi* statistic was calculated using data on Black composition (e.g., percentage of Blacks in tract) and Latino composition separately. The proportion of Black or Latino residents in a census tract was compared with the mean proportion of Black or Latino residents in the surrounding area, with a spatial weight included to account for composition of each tract compared with neighboring tracts. The Gi* statistic produces a z score representing the number of standard deviations that racial/ethnic composition of one’s tract is from the greater surrounding area. The more positive the Gi* statistic, the greater the clustering of Black or Latino residents in the census tract and surrounding neighborhoods (i.e., within a search threshold of 12.4 mi/20 km) compared with the larger surrounding area. The more negative the Gi* statistic, the lower the clustering of Black or Latino residents compared to the surrounding area. Gi* statistics near the null indicate no racial/ethnic clustering in tracts compared to the larger surrounding area.
Given that any cognitive consequence of residential segregation may be offset by accompanying socioeconomic advantage or disadvantage, it is important to control for neighborhood SES (NSES). From U.S. Census Tract 2010 data,47 we extracted variables that cohere conceptually and correlate empirically to capture the construct of NSES, including percentage of individuals with a high school diploma, percentage who owned their own home, percentage not on public assistance, percentage employed, median household income, and median number of rooms in home. Similar to prior research,56,57 these variables were z-score standardized and then averaged together to create the NSES variable (range: −2.2 to 1.8, where a larger positive value indicates a higher SES).
Covariates.
We included covariates that might confound the relation between residential segregation and cognitive outcomes, including NSES (described above), race/ethnicity (Black, Latino, or NHW), sex, age and education in years, and diagnosis (normal, MCI, or dementia). In our sample, more non-Latino Whites were recruited from the memory clinic than Black and Latino participants; thus, we controlled for recruitment source (clinic or community). Other covariates included clinic site (East Bay versus Sacramento), language of interview (only for models focused on Latinos, who was the only group that did not speak English), neighborhood population density (people/mi2), and a vascular risk/disease score assessed through medical histories and medical records which included the presence of diabetes, hypertension, hypercholesterolemia, stroke, transient ischemic attack, heart attack, atrial fibrillation, angioplasty, coronary artery bypass surgery, pacemaker, and congestive heart failure (where 0: no conditions and 1:all conditions; e.g., value for persons with 4 of these conditions=0.36). ApoE genotype was coded as presence of at least one ε4 allele versus none. Time was calculated as years from baseline evaluation and captures annualized rate of change.
Data Analysis
Descriptive statistics and mixed-effects multivariable regression models examining the association between neighborhood segregation and cognition were estimated using SAS v9.4. This sample was recruited from a large region that included urban as well as rural areas; thus, very few census tracts were represented by more than a single individual Therefore, similar to previous research,58,59 we treated the NSES and Gi* statistic variables as person-level factors in a contextual analysis rather than modeling their effects in a multilevel model. Random intercepts were included to account for between-person variability in level of cognitive outcomes at the baseline evaluation. Random slopes accounted for variation in rate of change between individuals. Main regression analyses focused on associations between Gi* statistic for Black and Latino participants and longitudinal change in the three cognitive domains over time. Segregation may affect individuals differently, and thus, the main models were also stratified by participant race/ethnicity.
As a sensitivity analysis, in our race/ethnicity stratified models, we used inverse probability weighting (IPW) to account for potential attrition/selection bias due to our exclusion of participants with only one visit and those who were missing addresses. Weights were based on propensity scores calculated from logistic regression, where the outcome was defined as 1=in analytic sample or 0=not in analytic sample. The participant’s age at baseline, sex, education level, race/ethnicity, site, and diagnosis at baseline were used to construct the inverse probability weights, which were then applied in the mixed effects regression models using the SAS Proc MIXED weight statement. We performed two other sensitivity analyses: in minimally adjusted models, we excluded NSES, population density, and vascular risk score as covariates, as they may be partial mediators of the association between neighborhood segregation and cognition. In a final sensitivity analysis, we controlled for practice effects by using an indicator variable (0 = first assessment; 1 = all subsequent assessments). This was entered as a time-varying fixed effect in all models.
Results
Sample Characteristics
Table 1 shows characteristics of the sample by race/ethnicity. Mean age was 75 years (SD: 7); 46% were White, 26% were Black, and 21% were Latino. A majority of the sample were women (64%), had normal cognitive functioning at baseline (66%), were recruited from the community (81%), and had their assessments conducted in English (89%). The sample was highly educated on average (mean years of education: 14, SD: 4).
Table 1.
Demographics, Neighborhood, and Clinical Characteristics of the Sample by Race/Ethnicity
| Characteristica | Totale N=452 | Black n=118 | White n=209 | Latino n=96 |
|---|---|---|---|---|
|
| ||||
| Age (years), n (%) | 74.8 (7.1) | 75.0 (6.9) | 75.1 (7.2) | 73.1 (6.8) |
| Male, n (%) | 163 (36.1%) | 27 (22.9%) | 91 (43.5%) | 36 (37.5%) |
| Education (years), mean (SD) | 14.3 (4.0) | 14.5 (3.0) | 15.7 (3.1) | 10.6 (5.0) |
| Cognitive status at IV, n (%) | ||||
| Normal | 297 (65.7%) | 81 (71.7%) | 118 (57.0%) | 79 (86.8%) |
| Mild cognitive impairment | 111 (25.3%) | 25 (22.1%) | 73 (35.3%) | 7 (7.7%) |
| Dementia | 31 (7.1%) | 7 (6.2%) | 16 (7.7%) | 5 (5.5%) |
| APOE e4 carrier, n(%) | 171 (41.0%) | 52 (52.0%) | 94 (46.3%) | 20 (21.5%) |
| Clinic sample (vs community), n(%) | 79 (18.9%) | 11 (10.4%) | 58 (29.9%) | 4 (4.6%) |
| Tested in English (vs. Spanish),n (%) | 360 (88.9%) | − | − | 46 (50.6%) |
| Number of visits, mean (SD) | 5.4 (2.9) | 5.5 (2.9) | 5.0 (2.8) | 6.4 (3.0) |
| Years of follow-up, mean (SD) | 5.2 (3.7) | 5.9 (4.0) | 4.8 (3.3) | 7.0 (3.9) |
| Vascular risk/disease score,b mean (SD) | 0.17 (0.14) | 0.19 (0.15) | 0.15 (0.13) | 0.20 (0.15) |
| Population densityc | 4710 (1979) | 4463 (1642) | 4716 (1649) | 5136 (2844) |
| Neighborhood SESd | 0.10 (0.73) | −0.11 (0.66) | 0.35 (0.63) | −0.20 (0.86) |
| Neighborhood composition | ||||
| % Black | 13.3 (14.2) | 26.4 (18.0) | 7.0 (8.6) | 11.1 (7.1) |
| % Latino | 20.7 (14.5) | 22.9 (14.6) | 16.6 (12.6) | 28.5 (16.0) |
| Neighborhood segregation Gi* statistic | ||||
| Black (versus others) | 8.1 (6.6) | 10.5 (4.6) | 7.6 (7.6) | 5.9 (5.6) |
| Latino (versus others) | −3.6 (5.1) | −5.5 (4.9) | −3.4 (4.4) | −1.5 (6.1) |
| Cognitive z-score, initial visit, mean (SD) | ||||
| Semantic memory | 0.35 (0.78) | 0.19 (0.66) | 0.69 (0.66) | −0.16 (0.85) |
| Episodic memory | −0.07 (0.92) | 0.07 (0.78) | −0.08 (1.02) | −0.18 (0.85) |
| Executive function | 0.04 (0.61) | 0.01 (0.57) | 0.19 (0.62) | −0.20 (0.53) |
Abbreviations: APOE = apolipoprotein E; TIA = transient ischemic attack; vs = versus; mi = mile; SES =socioeconomic status; IV = initial visit
Missing data: cognitive status, n=13; vascular risk/disease index, n=20; test language, n=47; recruitment source, n=35; semantic memory, n=48; APOE, n=35
Vascular risk/disease index on scale of 0 (none) to 1 (all present): heart attack, atrial fibrillation, angioplasty, coronary artery bypass surgery, pacemaker, congestive heart failure, stroke, TIA, hypertension, hypercholesterolemia, diabetes
people/mi2
Mean of z-scores for % not on public assistance, % employed, % high school diploma, %median household income, median number of rooms, % own home
29 participants were classified as “Other.”
On average, the included census tracts were composed of 13% blacks (SD: 14, range: 0.4–69.8%) and 21% Latinos (SD: 15, range: 1.1–78.7%) (Table 1, Supplemental Table 1). In contrast to composition, on average, neighborhoods had a higher clustering of Black residents (Gi* statistic mean: 8.1, SD: 6.6, range: −6.4 to 22.3) and a lower clustering of Latino residents (Gi* statistic mean:−3.6, SD: 5.1, range: −10.6 to 15.4). Categorizing the Gi* statistic based on low clustering (z-score<−1.645), no clustering (−1.645 ≤ z-score ≤1.645), or high clustering (z-score>1.645) showed that 86% of the sample lived in neighborhoods with significantly higher clustering of Blacks and 11% lived in neighborhoods with significantly high clustering of Latinos (Supplemental Table 2). Black participants lived in neighborhoods with higher clustering of Black residents and lower clustering of Latinos, compared to NHW and Latino participants (Table 1, Supplemental Table 3). Figures 1 and 2 illustrate that our study’s Black clustered neighborhoods were primarily in the East Bay (Oakland) areas and Latino clustered neighborhoods in the San Joaquin/Central Valley areas respectively.
Figure 1.
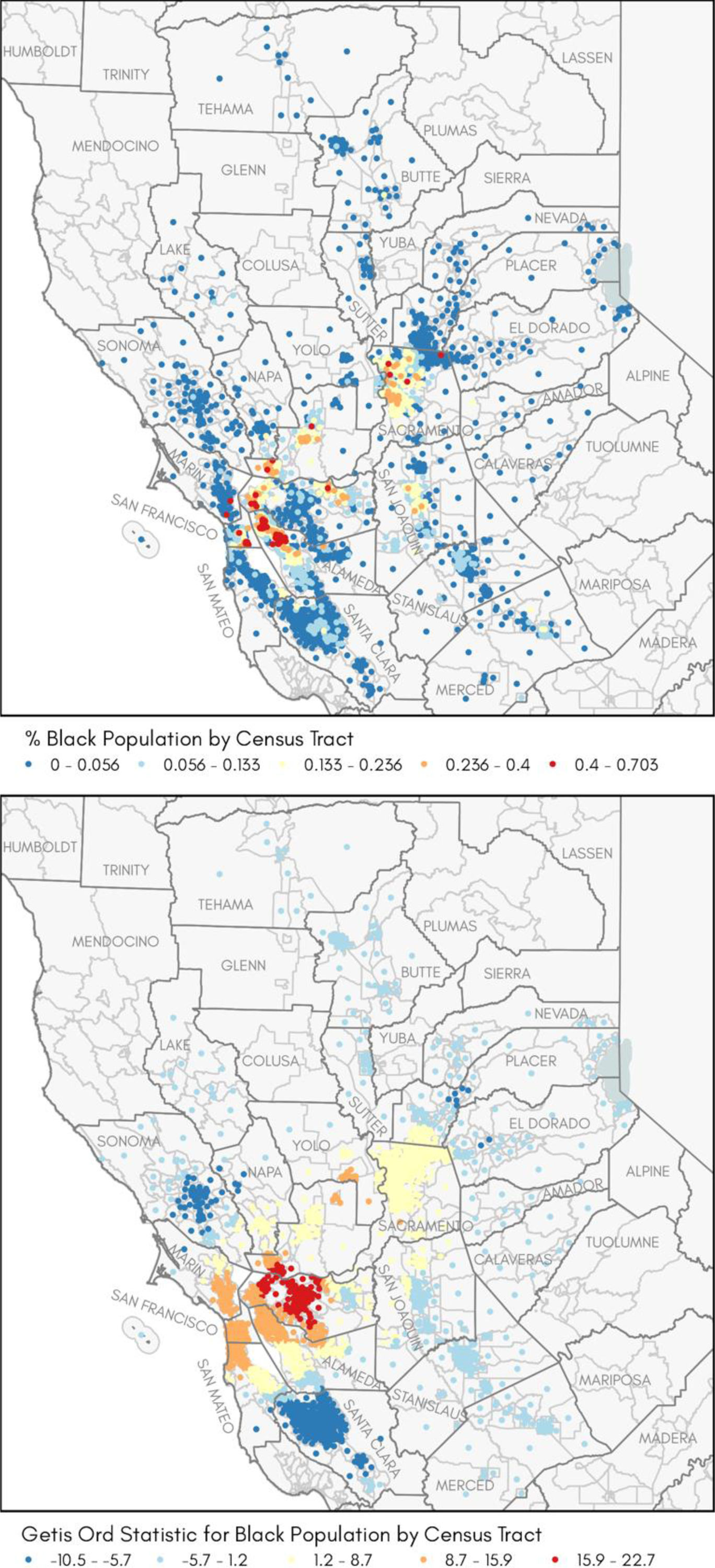
Observed distribution of Black/African American population by census tract: (a) Each census tract is represented by its centroid (geometric center), where blue dots represent tracts with the lowest percent, and red dots represent tracts with the highest percent of Black/African American population; (b) Calculated Getis-Ord Gi* statistic where red represents tracts with z-scores > 1.645 (high clustering, ɑ = 90%; 95%; 99%); blue represents tracts with z-score < 1.645 (low clustering); yellow dots indicate a random pattern (no evidence of clustering).
Figure 2.
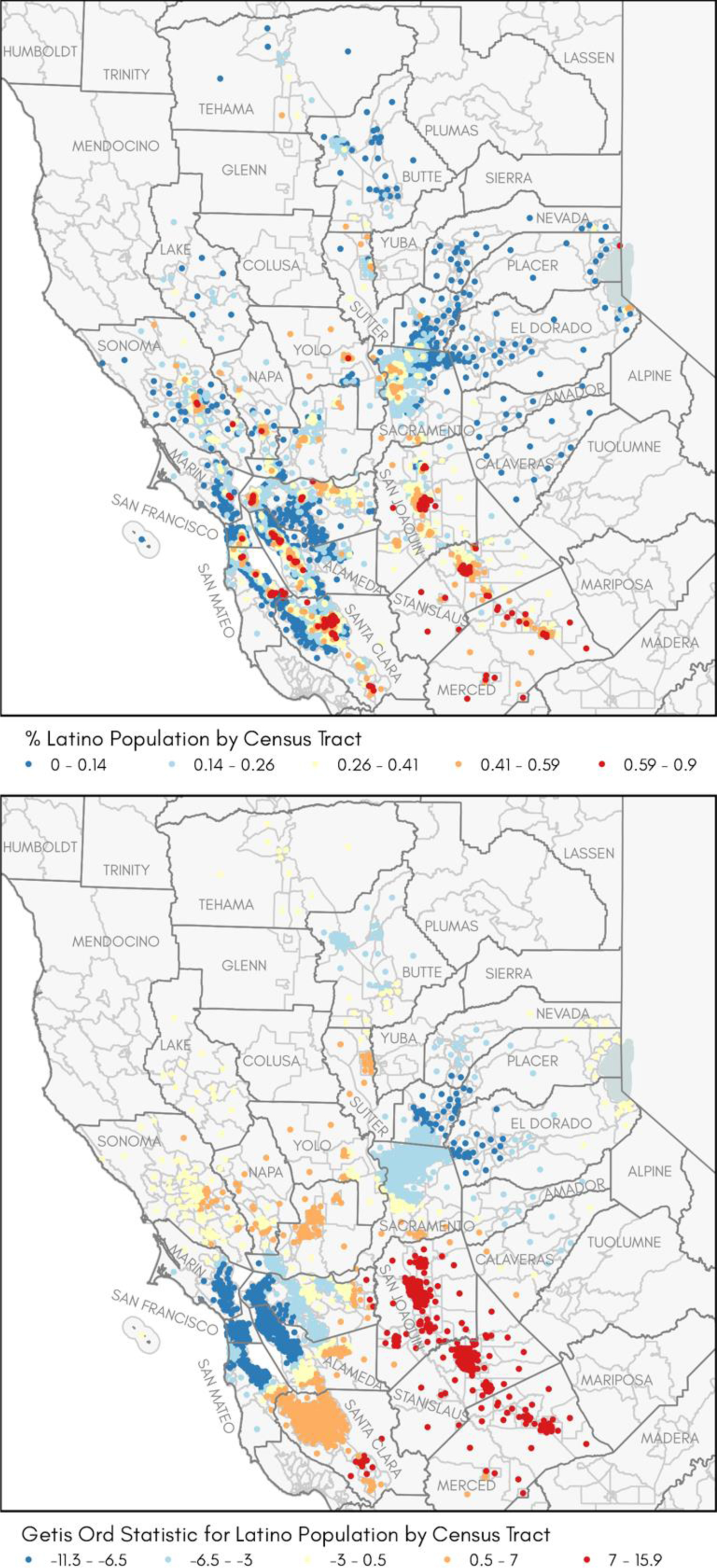
Observed distribution of Latino population by census tract: (a) Each census tract is represented by its centroid (geometric center), where blue dots represent tracts with the lowest percent, and red dots represent tracts with the highest percent of Latino population; (b) Calculated Getis-Ord Gi* statistic where red represents tracts with z-scores > 1.645 indicating high degree of clustering (ɑ = 90%; 95%; 99%); blue represents tracts with z-score < 1.645 indicating low degree of clustering; yellow dots indicate a random pattern (no evidence of clustering).
Residential Segregation and Cognitive Outcomes
Prior to conducting the regression analyses, we ensured that the Gi* statistic for Black and Latino participants were not highly correlated (Supplemental Table 4). In adjusted analyses (controlling for age, sex, race/ethnicity, education, cognitive status at initial visit, clinic versus community recruited, vascular risk score, number of visits, neighborhood SES, neighborhood population density, and site), individuals in neighborhoods with a higher clustering of Latino residents (i.e., higher Gi* statistic) had slower declines over time on semantic memory and those in neighborhoods with a higher clustering of Black residents had slower declines over time on episodic memory (Table 2). We did not find an association with baseline cognitive scores. Supplemental Table 5 provides the full results including estimates for the covariates for the regression analyses presented in Table 2.
Table 2.
Adjusted Associations between Neighborhood Segregation and Cognition at Baseline and Change Over Time in Full Sample
| Variables in model | Semantic memory |
Episodic memory |
Executive function |
|||
|---|---|---|---|---|---|---|
| Adjusted estimatea | 95% CI | Adjusted estimatea | 95% CI | Adjusted estimatea | 95% CI | |
|
| ||||||
| Years since initial visit | −0.02 | −0.04, 0.00 | −0.05**** | −0.06, −0.03 | −0.03 ** | −0.04, −0.01 |
| Gi* score-Black | 0.001 | −0.014, 0.016 | −0.001 | −0.016, 0.013 | −0.005 | −0.015, 0.006 |
| Gi* score-Black x Years | 0.001 | −0.001, 0.003 | 0.002 * | 0.000, 0.004 | 0.002 | −0.000, 0.004 |
| Gi* score-Latino | −0.004 | −0.017, 0.009 | −0.003 | −0.016, 0.009 | −0.001 | −0.011, 0.008 |
| Gi* score-Latino x Years | 0.002 * | 0.000, 0.004 | 0.001 | −0.000, 0.003 | 0.001 | −0.000, 0.003 |
Controlling for age, sex, race/ethnicity, education, cognitive status at initial visit, clinic versus community recruited, vascular risk score, number of visits neighborhood socioeconomic status, neighborhood population density, site; Full model results in Supplemental Table 5
p<0.05
p<0.01
p<0.001
p<0.0001
After stratifying the adjusted models by race/ethnicity, for Black participants, greater neighborhood clustering of Black residents was associated with lower baseline scores in episodic memory while greater clustering of Latino residents was associated with lower baseline scores in executive function (Table 3). There was no effect of neighborhood clustering on longitudinal change in cognition. Among Latino participants, those living in neighborhoods with greater clustering of Black residents had slower declines in episodic memory. Those with higher neighborhood clustering of Latinos had worse baseline semantic memory and slower declines over time on episodic memory. Among NHWs, there was no effect of neighborhood clustering on baseline cognition, but residing in neighborhoods with a greater clustering of Latinos was associated with slower decline over time on semantic memory. Supplemental Figures 1–4 show the average trajectory of cognitive change over time for the sample overall and stratified by race/ethnicity.
Table 3.
Adjusted Associations Between Neighborhood Segregation and Cognition at Baseline and Change Over Time by Individual Race/Ethnicity
| Participant’s Race/ethnicity | Variable in model | Semantic memory |
Episodic memory |
Executive function |
|||
|---|---|---|---|---|---|---|---|
| Adjusted estimatea | 95% CI | Adjusted estimatea | 95% CI | Adjusted estimatea | 95% CI | ||
|
| |||||||
| Black | Years since initial visit | 0.00 | −0.03, 0.04 | −0.04 | −0.08, 0.00 | −0.03 * | −0.05, −0.00 |
| Gi* score-Black | −0.012 | −0.050, 0.026 | −0.046 ** | −0.075, −0.016 | −0.025 | −0.051, 0.001 | |
| Gi* score-Black x Years | 0.001 | −0.002, 0.004 | 0.001 | −0.004, 0.006 | 0.001 | −0.001, 0.003 | |
| Gi* score-Latino | −0.014 | −0.043, 0.015 | −0.012 | −0.036, 0.011 | −0.025 ** | −0.042, −0.008 | |
| Gi* score-Latino x Years | 0.001 | −0.001, 0.003 | −0.001 | −0.005, 0.002 | −0.002 | −0.004, 0.000 | |
| Latino | Years since initial visit | 0.00 | −0.04, 0.04 | −0.05** | −0.08, −0.02 | −0.01 | −0.03, 0.02 |
| Gi* score-Black | −0.014 | −0.047, 0.020 | −0.024 | −0.056, 0.009 | −0.002 | −0.023, 0.019 | |
| Gi* score-Black x Years | 0.001 | −0.005, 0.006 | 0.008 **** | 0.004, 0.011 | 0.001 | −0.002, 0.004 | |
| Gi* score-Latino | −0.034 ** | −0.056, −0.011 | −0.007 | −0.026, 0.013 | −0.008 | −0.022, 0.008 | |
| Gi* score-Latino x Years | 0.002 | −0.000, 0.004 | 0.003 ** | 0.001, 0.005 | 0.001 | −0.000, 0.003 | |
| White | Years since initial visit | −0.02 | −0.05, 0.01 | −0.05** | −0.08, −0.01 | −0.04 ** | −0.07, −0.01 |
| Gi* score-Black | 0.005 | −0.015, 0.025 | 0.011 | −0.006, 0.028 | −0.005 | −0.018, 0.007 | |
| Gi* score-Black x Years | 0.001 | −0.003, 0.004 | 0.001 | −0.002, 0.004 | 0.002 | −0.002, 0.005 | |
| Gi* score-Latino | 0.009 | −0.009, 0.027 | −0.013 | −0.034, 0.008 | 0.009 | −0.009, 0.026 | |
| Gi* score-Latino x Years | 0.005 * | 0.001, 0.008 | 0.003 | −0.001, 0.006 | 0.003 | −0.001, 0.007 | |
Controlling for age, sex, education, cognitive status at initial visit, clinic versus community recruited, vascular risk score, number of visits neighborhood socioeconomic status, neighborhood population density, and site (Latino models also controlled for test language).
p<0.05
p<0.01
p<0.001
p<0.0001
Sensitivity Analyses
In the sensitivity analysis employing IPW, the estimates remained comparable to the analyses without IPW with two exceptions (Supplemental Table 6). Among Latinos, the association between a higher clustering of Latinos and a slower decline in episodic memory was no longer significant. Additionally, a new association was found for NHWs in which a higher clustering of Latinos was associated with a slower annual decline in executive function. Compared to the minimally adjusted models that did not control for NSES, population density, and vascular risk score, the fully adjusted models controlling for those variables resulted in no/minimal reductions in estimates (Supplemental Tables 7 and 8). This suggests that NSES, population density, and vascular risk factors are confounders and not mediators of the segregation-cognition associations. Finally, in the full sample model, estimates were unchanged after controlling for practice effects. In stratified models, estimates changed very little or not at all and were in the same direction. Significance of variables remain unchanged.
Discussion
We found that in the full sample, residential clustering of Black and Latino participants was associated with slower declines in episodic memory and semantic memory, respectively. These findings partially mirror those of Kovalchik et al., who found that Latino segregated neighborhoods were associated with better cognitive outcomes at baseline for all of its residents, regardless of individual level race/ethnicity. However, our study differed in that associations were found for cognitive decline (cognition over time).
Our race/ethnicity stratified models indicated that only Latinos and NHWs benefited from living in neighborhoods with higher clustering of Black and Latino residents. Although living in highly clustered Latino neighborhoods was associated with worse semantic memory for Latinos- this was only at baseline; yet highly clustered Black and Latino neighborhoods were associated with slower declines in episodic memory over time for Latinos. This may be related to the test characteristics of the cohort shown in a previous study,60 in which baseline cognitive scores were lower for Latinos, but there were no strong ethnic differences in cognitive change over time. This is likely because sociodemographic (e.g., race/ethnicity, NSES) differences in educational and life experiences may directly influence test performance but do not indicate greater disease effects on cognition. That is, cross-sectional effects reflect accumulated life experiences and exposures (e.g., educational quality) and health disparities that exert their effects on baseline cognition so that Latinos are impacted. However, the slower declines over time for Latinos, as well as NHWs, may reflect the ethnic enclave effect and the density hypothesis- that these neighborhoods provide their residents with social capital and support and resources that may be associated with certain protective features for cognition.61,62
Ethnic communities have been theorized to protect its members from social isolation, marginalization, discrimination and prejudice, as well as put its residents in a better position to access social support and community resources, therefore protecting its members against poor health outcomes, and potentially reducing potentially negative effects of low SES on cognition. The ethnic enclave theory helps us better understand the findings for Latinos, but it is unclear how NHWs benefit from living in Latino segregated neighborhoods. Further research is needed to clarify and confirm these results.
We found that Black residents living in highly clustered Black and Latino neighborhoods had lower baseline scores in episodic memory and executive function, respectively. Again, this may reflect lifelong differences in cognitive function that reflect the effects of educational and occupational quality/access and poorer health care access inherent in systemic racism and discrimination. However, similar to the results for Latinos, highly clustered Black and Latino neighborhoods were not associated with worse cognition over time among Black participants.
Overall, study findings indicate residential segregation may have negative associations with baseline cognitive scores, but a neutral or positive association with cognitive trajectories, at least for Latinos and NHWs. This contributes to the literature on the nuanced findings of racially/ethnically clustered neighborhoods. In particular, the impact of residential segregation may depend on individual race/ethnicity (as in the current study) or educational level (as in the case of Kovalchik et al.). Some research suggests that older adults may benefit from living areas that are racially/ethnically diverse (e.g., where residents’ individual backgrounds differ from their neighbors). Living in diverse environments and interacting with individuals from a variety of backgrounds and life experiences can be cognitively and socially stimulating for older adults. Research has found that socially diverse environments characterized by complex networks and patterns of socialization as well as multiple contexts contribute to improved cognitive functioning in older adults due to their cognitively challenging nature.63,64 Older adults exposed to more complex environments have been found to be at lower risk of cognitive impairment than their counterparts reporting less diverse interactions.64 Additionally, population-based studies have shown that older adults living in socially mixed neighborhoods (greater mix of housing prices) had lower risk for depression,65 and those in racially/ethnically diverse neighborhoods had lower risks for metabolic syndrome,66 both of which are linked to cognitive outcomes and may serve as underlying mechanisms. Although racial/ethnic segregation often connotes poor access to resources, a growing literature points to resilient features of segregated neighborhoods. Hutchinson and colleagues (2009) found that Black mortality was lower among residents of predominantly Black neighborhoods in Philadelphia with high neighborhood social capital in comparison to Black residents living in predominantly White neighborhoods. However, more research is needed to understand and replicate the results found in this study.
Study limitations include the possible lack of generalizability to other US regions and to those who would not be reached via clinic or community recruitment methods, and potential lack of power to detect race/ethnicity-stratified associations given the smaller sample of Black and Latino older adults. Moreover, it is possible that our findings are affected by self-selection, in which individuals with a certain level of cognition choose to live in a particular area (e.g., if cognitively healthy individuals choose to live in areas with high clusters of Latino or Black residents). Moreover, we were unable to compare those who enrolled in the study versus those who did not, given the rolling enrollment of our cohort. Although we accounted for participant education and NSES in the models, it is possible that our findings for differences in baseline cognition are due to residual confounding by individual and NSES including early-life SES or place of birth, variables not measured in this study but that would be a logical next step in future research. We had addresses from one point in time and therefore could not account for residential tenure or longer-term exposures to residential segregation. Our three cognitive composites are at least moderately correlated and it is unclear whether the differences we found regarding the impact of residential segregation on specific cognitive outcomes will be replicated in future work. Lastly, we did not have data on neighborhood factors that could help explain our observed associations, including access to resources, social cohesion, crime, and safety, and these factors will be important to explore as potential mediators in future studies.
Despite the relatively consistent pattern in which racial/ethnic segregation is associated with worse cognition at baseline but a positive or neutral impact on cognitive change across groups, the reason for the different impacts on cognitive domains both in cross-sectional and longitudinal modeling is unclear at this time. Further work is needed to determine if these findings are replicable. Studies with larger samples and that define neighborhoods using alternate boundaries (e.g., ½-mile around residence) might be able to further characterize segregation (partly by categorizing neighborhoods based on low, medium, and high Gi* scores) and its impact on incident MCI and dementia. Moreover, qualitative data assessing residents’ perceptions of and experiences with segregation, discrimination, and social cohesion would add to the current literature.
Our study advances prior work in this area by including neighborhood level data (e.g., geocoding addresses and linking to U.S. Census data) on a well-characterized cohort of English and Spanish-speaking older Latino and Black adults followed up over a long period of time, using a psychometrically robust neuropsychological battery (with similar reliability/validity indicators across racial/ethnic groups and Spanish/English speakers) that encompasses several domains of cognition, and by incorporating a well-established, formal measure of racial/ethnic segregation. Additionally, we control for a number of important potential confounders, including individual-level education and neighborhood SES. Given that certain neighborhoods, particularly in certain parts of the state and country are segregated, it is imperative that we understand the impacts it has on cognition for our growing older population.
Supplementary Material
Highlights.
Social determinants of health affect cognition in ethnically diverse older adults
Residential segregation is a manifestation of historical racism
Segregation is complexly related to cognition at baseline and cognitive decline
More research is needed on complex associations of segregation with cognition
References
- 1.Colby SLOJ. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. 2014:13, 2020. [Google Scholar]
- 2.Tang M-X, Stern Y, Marder K, et al. The APOE-∊ 4 allele and the risk of Alzheimer disease among African Americans, whites, and Hispanics. Jama. 1998;279(10):751–755. [DOI] [PubMed] [Google Scholar]
- 3.Hu C, Yu D, Sun X, Zhang M, Wang L, Qin H. The prevalence and progression of mild cognitive impairment among clinic and community populations: a systematic review and meta-analysis. International psychogeriatrics. 2017;29(10):1595. [DOI] [PubMed] [Google Scholar]
- 4.Tilvis RS, Kähönen-Väre MH, Jolkkonen J, Valvanne J, Pitkala KH, Strandberg TE. Predictors of cognitive decline and mortality of aged people over a 10-year period. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59(3):M268–M274. [DOI] [PubMed] [Google Scholar]
- 5.White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & place. 2011;17(2):438–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mair C, Roux AVD, Osypuk TL, Rapp SR, Seeman T, Watson KE. Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Social science & medicine. 2010;71(3):541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warner ET, Gomez SL. Impact of neighborhood racial composition and metropolitan residential segregation on disparities in breast cancer stage at diagnosis and survival between black and white women in California. Journal of community health. 2010;35(4):398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caunca MR, Odden MC, Glymour MM, et al. Association of Racial Residential Segregation Throughout Young Adulthood and Cognitive Performance in Middle-aged Participants in the CARDIA Study. JAMA Neurol. 2020;77(8):1000–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kovalchik SA, Slaughter ME, Miles J, Friedman EM, Shih RA. Neighbourhood racial/ethnic composition and segregation and trajectories of cognitive decline among US older adults. J Epidemiol Community Health. 2015;69(10):978–984. [DOI] [PubMed] [Google Scholar]
- 10.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports. 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kimble J Insuring inequality: The role of the Federal Housing Administration in the urban ghettoization of African Americans. Law & Social Inquiry. 2007;32(2):399–434. [Google Scholar]
- 12.Kushner J Apartheid in America: A historical and legal analysis of contemporary racial segregation in the United States. Howard Law Journal. 1979;22:559–560. [Google Scholar]
- 13.Massey D, Denton NA. American apartheid: Segregation and the making of the underclass. Harvard university press; 1993. [Google Scholar]
- 14.Firebaugh G, Farrell CR. Still large, but narrowing: The sizable decline in racial neighborhood inequality in Metropolitan America, 1980–2010. Demography. 2016;53:139–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Do D, Frank R, Zheng C, Iceland J. Hispanic segregation and poor health. It’s just not Black and White. Am J Epidemiol. 2017;186:990–999. [DOI] [PubMed] [Google Scholar]
- 16.Ertel KA, Glymour MM, Berkman LF. Effects of social integration on preserving memory function in a nationally representative US elderly population. American journal of public health. 2008;98(7):1215–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostir GV, Eschbach K, Markides KS, Goodwin JS. Neighbourhood composition and depressive symptoms among older Mexican Americans. Journal of Epidemiology & Community Health. 2003;57(12):987–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw CR, McKay HD. Juvenile delinquency and urban areas. 1942.
- 19.Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? American journal of public health. 2004;94(10):1807–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37(4):293–310. [PubMed] [Google Scholar]
- 21.Lee M-A, Ferraro KF. Neighborhood residential segregation and physical health among Hispanic Americans: Good, bad, or benign? Journal of health and social behavior. 2007;48(2):131–148. [DOI] [PubMed] [Google Scholar]
- 22.Patel KV, Eschbach K, Rudkin LL, Peek MK, Markides KS. Neighborhood context and self-rated health in older Mexican Americans. Annals of epidemiology. 2003;13(9):620–628. [DOI] [PubMed] [Google Scholar]
- 23.Rostila M The facets of social capital. Journal for the Theory of Social Behaviour. 2011;41(3):308–326. [Google Scholar]
- 24.Eschbach K, Ostir G, Patel K, Markides K, Goodwin J. Neighborhood context and mortality among older Mexican Americans: evidence from the Hispanic EPESE. Am J Public Health. 2004;94:1807–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Social Forces. 1997;76(1):169–198. [Google Scholar]
- 26.Bond Huie SA, Krueger PM, Rogers RG, Hummer RA. Wealth, race, and mortality. Social Science Quarterly. 2003;84(3):667–684. [Google Scholar]
- 27.Lee RE, Cubbin C. Neighborhood context and youth cardiovascular health behaviors. American journal of public health. 2002;92(3):428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hutchinson R, Putt M, Dean L, Long J, Montagnet C, Armstrong K. Neighborhood racial composition, social capital and black all-cause mortality in Philadelphia. Soc Sci Med. 2009;68:1859–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moore MG. Three types of interaction. In: Taylor & Francis; 1989. [Google Scholar]
- 30.Haas JS, Phillips KA, Sonneborn D, et al. Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical care. 2004:707–714. [DOI] [PubMed] [Google Scholar]
- 31.Glymour MM, Manly JJ. Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology review. 2008;18(3):223–254. [DOI] [PubMed] [Google Scholar]
- 32.Massey DS, Denton NA. The dimensions of residential segregation. Social forces. 1988;67(2):281–315. [Google Scholar]
- 33.Lee BA, Iceland J, Farrell CR. Is ethnoracial residential integration on the rise? Evidence from metropolitan and micropolitan America since 1980. In: Diversity and disparities: America enters a new century. Russell Sage Foundation; 2014:415–456. [Google Scholar]
- 34.Aneshensel CSKM, Chodosh J, Wight RG. The Urban Neighborhood and Cognitive Functioning in Late Middle Age. J Health Soc Behav. 2011;52(2):163–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scarmeas N, Stern Y. Cognitive reserve and lifestyle. Journal of clinical and experimental neuropsychology. 2003;25(5):625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bronfenbrenner U The ecology of human development: Experiments by nature and design. Harvard university press; 1979. [Google Scholar]
- 37.Hinton L, Carter K, Reed BR, et al. Recruitment of a community-based cohort for research on diversity and risk of dementia. Alzheimer disease and associated disorders. 2010;24(3):234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morris J Current vision and scoring rules The Clinical Dementia Rating (CDR). Neurology. 1993;43:2412–2414. [DOI] [PubMed] [Google Scholar]
- 39.DeCarli C, Reed BR, Jagust W, Martinez O, Ortega M, Mungas D. Brain behavior relationships amongst African Americans, caucasians and Hispanics. Alzheimer disease and associated disorders. 2008;22(4):382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mungas D, Reed BR, Crane PK, Haan MN, González H. Spanish and English Neuropsychological Assessment Scales (SENAS): further development and psychometric characteristics. Psychological assessment. 2004;16(4):347. [DOI] [PubMed] [Google Scholar]
- 41.Mungas D, Reed BR, Farias ST, Decarli C. Criterion-referenced validity of a neuropsychological test battery: equivalent performance in elderly Hispanics and non-Hispanic Whites. Journal of the International Neuropsychological Society: JINS. 2005;11(5):620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mungas D, Reed BR, Haan MN, González H. Spanish and English neuropsychological assessment scales: relationship to demographics, language, cognition, and independent function. Neuropsychology. 2005;19(4):466. [DOI] [PubMed] [Google Scholar]
- 43.Mungas D, Reed BR, Marshall SC, González HM. Development of psychometrically matched English and Spanish language neuropsychological tests for older persons. Neuropsychology. 2000;14(2):209. [DOI] [PubMed] [Google Scholar]
- 44.Crane A, McWilliams A, Matten D, Moon J, Siegel DS. The Oxford handbook of corporate social responsibility. Oxford University Press on Demand; 2008. [Google Scholar]
- 45.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian S. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. American journal of public health. 2003;93(10):1655–1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.QGIS Geographic Information System [computer program]. QGIS Association; 2021. [Google Scholar]
- 47.US Census Bureau. American Community Survey, Table DP04. In:2010.
- 48.Massey DS, White MJ, Phua V-C. The dimensions of segregation revisited. Sociological methods & research. 1996;25(2):172–206. [Google Scholar]
- 49.Logan JR, Stults BJ, Farley R. Segregation of minorities in the metropolis: Two decades of change. Demography. 2004;41(1):1–22. [DOI] [PubMed] [Google Scholar]
- 50.Allen JP, Turner E. Ethnic differentiation by blocks within census tracts. Urban Geography. 1995;16(4):344–364. [Google Scholar]
- 51.Kaplan DH, Woodhouse K. Research in ethnic segregation II: Measurements, categories and meanings. Urban Geography. 2005;26(8):737–745. [Google Scholar]
- 52.Anselin L, Getis A. Spatial statistical analysis and geographic information systems. The Annals of Regional Science. 1992;26(1):19–33. [Google Scholar]
- 53.Moran PA. Notes on continuous stochastic phenomena. Biometrika. 1950;37(1/2):17–23. [PubMed] [Google Scholar]
- 54.Li H, Calder CA, Cressie N. Beyond Moran’s I: testing for spatial dependence based on the spatial autoregressive model. Geographical Analysis. 2007;39(4):357–375. [Google Scholar]
- 55.Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geographical analysis. 1995;27(4):286–306. [Google Scholar]
- 56.Zeki Al Hazzouri A, Haan MN, Osypuk T, Abdou C, Hinton L, Aiello AE. Neighborhood socioeconomic context and cognitive decline among older Mexican Americans: results from the Sacramento Area Latino Study on Aging. American journal of epidemiology. 2011;174(4):423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Clarke G, McGlinchey EL, Hein K, et al. Cognitive-behavioral treatment of insomnia and depression in adolescents: A pilot randomized trial. Behav Res Ther. 2015;69:111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meyer OL, Mungas D, King J, et al. Neighborhood socioeconomic status and cognitive trajectories in a diverse longitudinal cohort. Clinical gerontologist. 2018;41(1):82–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sisco SM, Marsiske M. Neighborhood influences on late life cognition in the ACTIVE study. Journal of Aging Research. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Early DR, Widaman KF, Harvey D, et al. Demographic predictors of cognitive change in ethnically diverse older persons. Psychol Aging. 2013;28(3):633–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sheffield KM, Peek MK. Neighborhood context and cognitive decline in older Mexican Americans: results from the Hispanic Established Populations for Epidemiologic Studies of the Elderly. American journal of epidemiology. 2009;169(9):1092–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Halpern D Minorities and mental health. Social Science & Medicine. 1993;36(5):597–607. [DOI] [PubMed] [Google Scholar]
- 63.Schooler C Psychological effects of complex environments during the life span: A review and theory. Intelligence. 1984;8(4):259–281. [Google Scholar]
- 64.Ellwardt L, Van Tilburg TG, Aartsen MJ. The mix matters: Complex personal networks relate to higher cognitive functioning in old age. Social science & medicine. 2015;125:107–115. [DOI] [PubMed] [Google Scholar]
- 65.Marshall A, Jivraj S, Nazroo J, Tampubolon G, Vanhoutte B. Does the level of wealth inequality within an area influence the prevalence of depression amongst older people? Health & place. 2014;27:194–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li K, Wen M, Fan JX. Neighborhood Racial Diversity and Metabolic Syndrome: 2003–2008 National Health and Nutrition Examination Survey. Journal of immigrant and minority health. 2019;21(1):151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


