Abstract
Empirical data on the association between diet and incident hypertension in Southwest China is lacking. We examined the associations between various dietary patterns and the risk of incident hypertension in this prospective population cohort of Southwest China. A total of 5442 eligible adults were included from Guizhou Province, China, since 2010. Dietary information was obtained using face-to-face interviews with a semi-quantitative food frequency questionnaire, and dietary patterns were characterized using factor analysis. The hazard ratios (HRs) and 95% confidence intervals (95% CIs) were estimated for the associations between various dietary patterns and incident hypertension risk using a Cox proportional hazard model. Until 2020, a total of 1177 new hypertension cases were identified during an average follow-up of 6.97 years. In the multivariable-adjusted analysis, a low intake of the junk food pattern was significantly associated with the reducing risk of incident hypertension (HR: 0.772, 95% CI: 0.671, 0.887) and a high intake of the vegetable–grain pattern statistically lowered the risk of incident hypertension (HR: 0.774, 95% CI: 0.669, 0.894) compared with the medium intake of such patterns. Higher adherence to the vegetable–grain pattern and lower adherence to the junk food pattern significantly lowered the hypertension incidence among the population in Southwest China. Those findings suggested healthy diet guidelines should be developed for the prevention of hypertension.
Keywords: dietary patterns, factor analysis, cohort study, hypertension, China
1. Introduction
Hypertension (HTN) is a global public health issue, especially in low- and middle-income countries [1], and the prevalence has been increasing in recent decades in China [2]. The disease burden of HTN is generally complicated by possibly developing cardiovascular disease (CVD), stroke, heart failure, and kidney disease, which affect both the quality and expectancy of life [3,4]. Thus, there is a key unmet need to investigate the complex and multifaceted causes and develop more specific preventive strategies.
An imbalanced diet was highlighted as a major contributor to hypertension development [5]. However, different approaches for constructing dietary patterns and differences in their composition varied the conclusions regarding healthy patterns for HTN prevention. The Dietary Approaches to Stop Hypertension diet (DASH, characterized by a high intake of fruits, vegetables, low-fat dairy foods, and reduced saturated and total fat) was shown to be an effective dietary approach for substantially reducing blood pressure and preventing cardiovascular disease [6], and the Mediterranean dietary pattern (characterized by a high intake of fruits, vegetables, nuts, and whole grains) can decrease major clinical endpoints, including blood pressure [7]. However, since many differences exist between typical diets in Chinese and Western populations, existing diet patterns are not wholly appropriate for multiethnic Chinese with different genetic characteristics and food cultures [8].
Recently published studies paid greater attention to factor analysis [9], which takes account of the complex interactions between the different categories of dietary intake and forms dietary patterns that are targeted for local ethnic groups [10]. To our knowledge, cohort studies on specific dietary patterns in relation to the incidence risk of hypertension in China are sparse. Several cross-sectional studies have observed relationships between various dietary patterns and hypertension and called for further prospective studies [11,12,13]. Based on a cohort study of adults from Southwest China, we aimed to evaluate the associations with various dietary patterns and the risk of developing hypertension using factor analysis and to provide evidence for dietary recommendations in HTN prevention.
2. Materials and Methods
2.1. Recruitment and Study Population
The Guizhou Population Health Cohort Study (GPHCS) is an ongoing multiethnic epidemiological study of incident chronic diseases and potential risk factors in Guizhou province, China. Briefly, a total of 9280 adult residents from 48 townships of 12 districts were recruited into this prospective cohort using the multistage proportional stratified cluster sampling method. The eligibility criteria of subjects included those who (1) were aged 18 years or above, (2) lived in the study region and had no plan to move out, (3) completed survey questionnaire and blood sampling, and (4) signed the written informed consent form. Based on the intent-to-treat criteria, participants were followed up from the date of entry until death, loss to follow-up, time of a request for no further contact, or until the planned completion date in 2016–2020. During the follow-up until 2020, we updated information on the status of major chronic diseases and vital status, with a response rate of 88%. All deaths were confirmed by the unified criteria through the Death Registration Information System and Basic Public Health Service System. In this study, exclusions for participants were loss to follow-up (n = 1117), incomplete dietary data (n = 277), a history of hypertension (n = 2056) at baseline, and missing hypertension status (n = 388) during follow-up. The final analysis involved 5442 participants in this cohort (Figure S1). All participants provided written informed consent at enrollment. The study was approved by the Institutional Review Board of Guizhou Centre for Disease Control and Prevention (no. S2017-02).
2.2. Assessment of Dietary Patterns
Food consumption was obtained using a semi-quantitative food frequency questionnaire (FFQ) that covered 22 food and beverage items that are commonly consumed by the multiethnic residents of Southwest China at the baseline. The questionnaire was designed by the Chinese Center for Disease Control and Prevention [14] and applied in China’s chronic disease surveillance (2010). The categories included main dishes, desserts and cereals, fruits, vegetables, beverages, and dairy in this FFQ to obtain more reliable information on the dietary intake of participants in the last year. Using the food list, subjects were asked to grade their frequency of consumption of each food item using either of the four responses “times per day,” “times per week,” “times per month,” and “times per year” and their average intake per time, with the unit “50 g per day.” Food intakes were computed by multiplying the frequency of food consumption by a single intake unit of each item.
2.3. Assessment of Outcome and Covariates
Baseline information on socio-demographic characteristics, lifestyles, and health conditions was obtained using a structured questionnaire with a face-to-face interview. Using a standard protocol that is recommended by the World Health Organization (WHO), height and weight were measured with participants wearing lightweight clothing without shoes and recorded to the nearest 0.1 kg (or cm) [10]. The body mass index (BMI) was calculated by dividing the weight in kilograms by the square of the height in meters and categorized as recommended by the Guidelines for Prevention and Control of Overweight and Obesity in Chinese Adults [15]. All measurements were performed with quality control procedures in place. Field-measured hypertension was carried out three times per participant by trained investigators and the average of three blood pressure measurements was calculated. The Chinese Guidelines for Hypertension Prevention and Treatment (2019) were used, where hypertension was defined as an average systolic blood pressure of 140 mmHg or higher, and/or an average diastolic blood pressure of 90 mmHg or higher, and/or reporting physician-diagnosed hypertension or receiving hypertension treatment. Several variables were adjusted in the multivariable models: gender, age (<35, 35–49, ≥50 years), Han Chinese (yes, no), education years (≤9, >9 years), married (yes, no), BMI (<18.5, 18.5–23.9, 24–27.9, ≥28 kg/m2), farmers (yes, no), hypertension family history (yes, no), smoking (yes, no), drinking (yes, no), and regular physical activity (yes, no).
2.4. Statistical Analysis
Factor analysis was conducted with varimax rotation using the 16 aggregated food items, and four factors were determined according to the eigenvalue (>1), a scree plot, and the explained variation ratio. Specific food items were aggregated on the basis of the degree to which food items in the dataset were correlated with one another. Those with larger absolute factor loadings were considered to significantly contribute to the pattern. A summary score for each pattern was then derived [16] and categorized into low, medium, and high tertiles in further analysis. The factor loading matrix for the two retained dietary patterns is shown in Table S1. Factor 1, named the junk food pattern, was dominated by a high factor load of fried food, soft drinks, and desserts (0.28–0.54). The second factor was characterized by a high factor load of vegetables and grains (0.55 and 0.38) and named the vegetable–grain pattern. Common food items in the junk food pattern are partly presented in Table S2.
Person time in years was calculated for each participant from the date of enrolling the cohort to the date of diagnosis of hypertension, death, or follow-up, whichever came first. Pearson’s chi-squared test was used to compare the characteristics between subjects with different hypertension statuses at follow-up and various dietary patterns. The association between the various dietary patterns and hypertension incidence was assessed using a Cox proportional hazards regression model. The assumption of hazard proportionality in Cox regression models was tested and shown using the Schoenfeld residuals. Sensitivity analysis was conducted to investigate the potential errors and their impacts on conclusions to be drawn from the models. All statistical tests were two-sided. The data were performed using R software (Version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Baseline Characteristics of Subjects
Table 1 shows the distribution of the baseline characteristics according to the follow-up hypertension status. Of the 5442 participants, three-fifths were at the age of 18–34 years and more than half were women. Newly diagnosed hypertension cases significantly tended to be older, married, farmers, having shorter education years, smokers, and fat. There were no significant differences over other variables (Table 1).
Table 1.
Baseline characteristics among the community population in Southwest China.
| Characteristics | Total | Non-HTN | New HTN | p-Value |
|---|---|---|---|---|
| Participants, n | 5442 | 4265 | 1177 | |
| Age, years | <0.001 | |||
| 18.0–34.9 | 3267 (60.0) | 2739 (64.2) | 528 (44.9) | |
| 35.0–49.9 | 1542 (28.3) | 1119 (26.2) | 423 (35.9) | |
| ≥50.0 | 633 (11.6) | 407 (9.5) | 226 (19.2) | |
| Women, % | 2970 (54.6) | 2357 (55.3) | 613 (52.1) | 0.056 |
| Han Chinese, % | 3096 (56.9) | 2397 (56.2) | 699 (59.4) | 0.055 |
| Education > 9 years, % | 2453 (45.1) | 2020 (47.4) | 433 (36.8) | <0.001 |
| Married, % | 4380 (80.5) | 3404 (79.8) | 976 (82.9) | 0.019 |
| Farmer, % | 3111 (57.2) | 2373 (55.6) | 738 (62.7) | <0.001 |
| Current smoker, % | 1484 (27.3) | 1128 (26.4) | 356 (30.2) | 0.011 |
| Alcohol use, % | 1691 (31.1) | 1324 (31.0) | 367 (31.2) | 0.956 |
| Physical activity, % | 4717 (86.7) | 3695 (86.6) | 1022 (86.8) | 0.899 |
| HTN family history, % | 522 (9.6) | 421 (9.9) | 101 (8.6) | 0.203 |
| BMI, kg/m2 | 0.001 | |||
| <22.0 | 357 (6.6) | 290 (6.8) | 67 (5.7) | |
| 22.0–23.9 | 3585 (66.0) | 2844 (66.8) | 741 (63.1) | |
| 24.0–27.9 | 1233 (22.7) | 942 (22.1) | 291 (24.8) | |
| ≥28.0 | 257 (4.7) | 181 (4.3) | 76 (6.5) |
Abbreviations: HTN, hypertension; BMI, body mass index.
3.2. Distribution of Dietary Patterns
As shown in Table 2, subjects who were over 50 years old (39.2%), non-Han Chinese (41.9%), had shorter education years (40.3%), married (33.8%), farmers (39.7%), non-smokers (34.8%), non-alcohol users (34.5%), without regular physical activity (41.5%) or hypertension family history (34.7%), and normal weight (35.0%) tended to have low junk food pattern scores. Comparatively, those who were aged from 18 to 34 years (34.9%), men (37.2%), non-Han Chinese (40.3%), had longer education years (36.0%), farmers (33.6%), smokers (36.6%), and alcohol users (36.9%) tended to have high vegetable–grain food pattern scores.
Table 2.
Tertiles of dietary patterns over subjects with different baseline characteristics in Southwest China (%).
| Characteristics | Junk Food Pattern | Vegetable–Grain Pattern | ||||||
|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | p-Value | Low | Medium | High | p-Value | |
| Participants, n | 1814 | 1814 | 1814 | 1814 | 1814 | 1814 | ||
| Age, years | <0.001 | <0.001 | ||||||
| 18.0–34.9 | 1013 (31.0) | 1032 (31.6) | 1222 (37.4) | 985 (30.1) | 1141 (34.9) | 1141 (34.9) | ||
| 35.0–49.9 | 553 (35.9) | 551 (35.7) | 438 (28.4) | 537 (34.8) | 500 (32.4) | 505 (32.7) | ||
| ≥50.0 | 248 (39.2) | 231 (36.5) | 154 (24.3) | 292 (46.1) | 173 (27.3) | 168 (26.5) | ||
| Gender | 0.101 | <0.001 | ||||||
| Women | 953 (32.1) | 1011 (34.0) | 1006 (33.9) | 1096 (36.9) | 980 (33.0) | 894 (30.1) | ||
| Men | 861 (34.8) | 803 (32.5) | 808 (32.7) | 718 (29.0) | 834 (33.7) | 920 (37.2) | ||
| Han Chinese | <0.001 | <0.001 | ||||||
| Yes | 832 (26.9) | 982 (31.7) | 1282 (41.4) | 1206 (39.0) | 1021 (33.0) | 869 (28.1) | ||
| No | 982 (41.9) | 832 (35.5) | 532 (22.7) | 608 (25.9) | 793 (33.8) | 945 (40.3) | ||
| Education years | <0.001 | 0.001 | ||||||
| >9 | 608 (24.8) | 729 (29.7) | 1116 (45.5) | 772 (31.5) | 799 (32.6) | 882 (36.0) | ||
| ≤9 | 1206 (40.3) | 1085 (36.3) | 698 (23.4) | 1042 (34.9) | 1015 (34.0) | 932 (31.2) | ||
| Married | <0.001 | 0.677 | ||||||
| Yes | 1480 (33.8) | 1512 (34.5) | 1388 (31.7) | 1449 (33.1) | 1470 (33.6) | 1461 (33.4) | ||
| No | 334 (31.5) | 302 (28.4) | 426 (40.1) | 365 (34.4) | 344 (32.4) | 353 (33.2) | ||
| Farmers | <0.001 | <0.001 | ||||||
| Yes | 1236 (39.7) | 1082 (34.8) | 793 (25.5) | 974 (31.3) | 1093 (35.1) | 1044 (33.6) | ||
| No | 578 (24.8) | 732 (31.4) | 1021 (43.8) | 840 (36.0) | 721 (30.9) | 770 (33.0) | ||
| Current smoker | <0.001 | <0.001 | ||||||
| Yes | 437 (29.4) | 493 (33.2) | 554 (37.3) | 439 (29.6) | 502 (33.8) | 543 (36.6) | ||
| No | 1377 (34.8) | 1321 (33.4) | 1260 (31.8) | 1375 (34.7) | 1312 (33.1) | 1271 (32.1) | ||
| Alcohol use | <0.001 | <0.001 | ||||||
| Yes | 519 (30.7) | 530 (31.3) | 642 (38.0) | 472 (27.9) | 595 (35.2) | 624 (36.9) | ||
| No | 1295 (34.5) | 1284 (34.2) | 1172 (31.2) | 1342 (35.8) | 1219 (32.5) | 1190 (31.7) | ||
| Physical activity | <0.001 | 0.267 | ||||||
| Yes | 1513 (32.1) | 1552 (32.9) | 1652 (35.0) | 1570 (33.3) | 1557 (33.0) | 1590 (33.7) | ||
| No | 301 (41.5) | 262 (36.1) | 162 (22.3) | 244 (33.7) | 257 (35.4) | 224 (30.9) | ||
| HTN family history, % | <0.001 | 0.629 | ||||||
| Yes | 107 (20.5) | 158 (30.3) | 257 (49.2) | 166 (31.8) | 183 (35.1) | 173 (33.1) | ||
| No | 1707 (34.7) | 1656 (33.7) | 1557 (31.6) | 1648 (33.5) | 1631 (33.2) | 1641 (33.4) | ||
| BMI, kg/m2 | 0.013 | 0.444 | ||||||
| <22.0 | 117 (32.8) | 124 (34.7) | 116 (32.5) | 123 (34.5) | 134 (37.5) | 100 (28.0) | ||
| 22.0–23.9 | 1254 (35.0) | 1169 (32.6) | 1162 (32.4) | 1190 (33.2) | 1181 (32.9) | 1214 (33.9) | ||
| 24.0–27.9 | 370 (30.0) | 428 (34.7) | 435 (35.3) | 410 (33.3) | 414 (33.6) | 409 (33.2) | ||
| ≥28.0 | 70 (27.2) | 87 (33.9) | 100 (38.9) | 87 (33.9) | 82 (31.9) | 88 (34.2) | ||
Abbreviations: HTN, hypertension; BMI, body mass index.
3.3. Associations between Dietary Patterns and Hypertension Incidence
During the 37,932.5 PYs of follow-up, 1177 incident hypertension cases were documented. The junk food pattern was significantly associated with an HTN incidence risk (Table 3). Participants in the low score category of junk food pattern had a 23% lower risk of hypertension (HR: 0.783, 95% CI: 0.682, 0.899) than those in the medium intake category. After the adjustment for covariates, including lifestyles and other demographic characteristics, this association became a little stronger (HR: 0.772, 95% CI: 0.671, 0.887). Furthermore, an inverse association was observed between the vegetable–grain pattern and incident hypertension. Compared with subjects in the medium score category, those with the high scores had a lower risk of incident hypertension (HR: 0.762, 95% CI: 0.660, 0.880). Such a protective effect persisted after further adjusting these covariates (HR: 0.774, 95% CI: 0.669, 0.894).
Table 3.
The incidence risk of hypertension according to tertiles of dietary patterns among participants in Southwest China.
| Cases, n | Incident Density/1000 PYs |
HR (95% CI) | |||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||
| Junk food pattern | |||||
| Low | 376 | 29.52 | 0.783 (0.682, 0.899) *** | 0.771 (0.671, 0.886) *** | 0.772 (0.671, 0.887) *** |
| Medium | 435 | 34.60 | 1.000 | 1.000 | 1.000 |
| High | 366 | 34.00 | 0.865 (0.752, 0.994) * | 0.917 (0.794, 1.060) | 0.895 (0.775, 1.030) |
| Vegetable and grain pattern |
|||||
| Low | 416 | 33.11 | 0.964 (0.842, 1.100) | 0.986 (0.860, 1.130) | 0.990 (0.864, 1.140) |
| Medium | 438 | 34.26 | 1.000 | 1.000 | 1.000 |
| High | 323 | 25.67 | 0.762 (0.660, 0.880) *** | 0.775 (0.670, 0.895) *** | 0.774 (0.669, 0.894) *** |
Note: Model 1—adjusted for age, gender; model 2—model 1 plus nationality, education, marriage, occupation, hypertension family history, and baseline BMI value; model 3—model 2 plus smoking status, alcohol use, and regular physical exercise. ***: p < 0.001, *: p < 0.05. Abbreviations: PY, person-years; HR, hazard ratio; 95% CI, 95% confidence interval.
3.4. Sensitivity Analysis
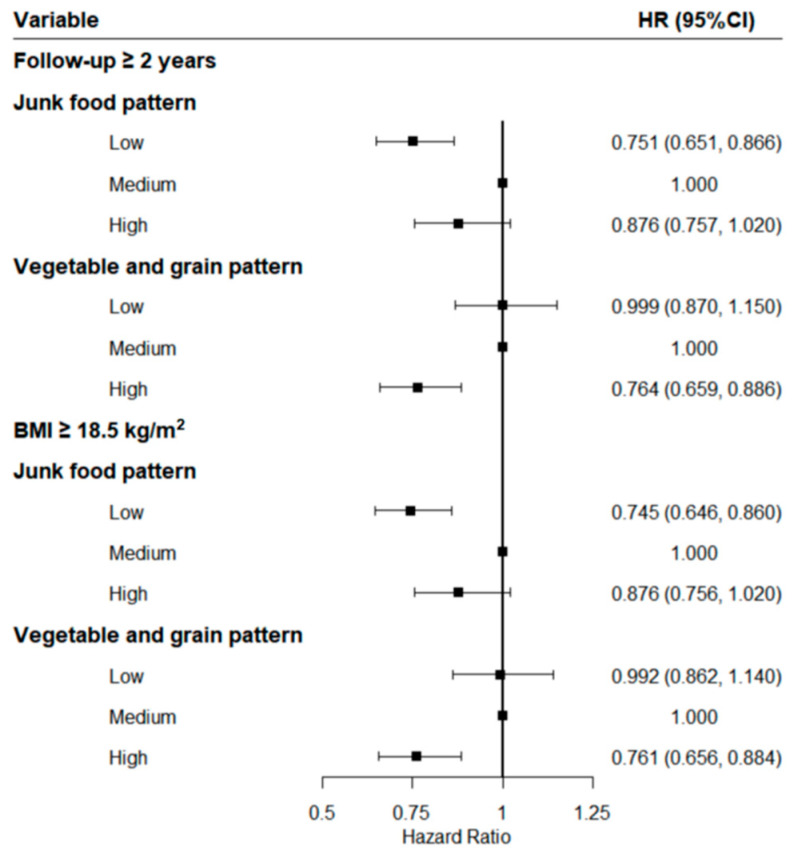
In the sensitivity analysis with participants who entered the cohort for two years or longer or those with a baseline BMI of no less than 18.5 kg/m2 (Figure 1), the results remained robust. Compared with the results presented above, the protective effects of the highest scores of the vegetable–grain pattern and the lowest scores of the junk food pattern did not change substantially after the adjustment for covariates.
Figure 1.
Sensitivity analysis after excluding those who entered the cohort for less than two years or were lean.
4. Discussion
The risk of incident hypertension was as high as 31.03/1000 person-years among this study population in Southwest China, indicating that hypertension was an imminent health crisis for local populations. Two main dietary patterns were prominent in this community-based prospective cohort study. We found that both low adherence to the junk food pattern and high adherence to the vegetable–grain pattern were associated with significant risk reductions of incident hypertension. Those associations were independent of BMI and other HTN risk factors, and the results were virtually unchanged in the sensitivity analysis upon further restriction of participant categories. These findings suggested that offering an attractive dietary strategy may be useful in the prevention of hypertension.
Previous cohort studies or meta-analyses demonstrated that the DASH diet reduces blood pressure and is recommended for preventing cardiovascular disease [6,17]. The DASH diet emphasizes the intake of fruits, vegetables, low-fat dairy foods, and reduced saturated and total fat. However, Southwest China is a multi-minority community with different genetic characteristics [18], and different ethnic groups have specialized food preferences and food cultures for geographical and economic reasons [19]. The habit that features beef, mutton, and pickles as the main component still exists among residents. Vegetables are commonly eaten steamed or boiled and mixed with seasonings rather than eaten raw. Therefore, the DASH is not very appropriate for evaluating the dietary quality of people in China. Factor analysis was conducted in this study to characterize dietary patterns based on the main food types that are consumed locally and evaluate the dietary quality among the population in Southwest China.
In China, the traditional diet greatly changed from low to high in fat and energy density with the rapid growth of the economy [20], and this remarkable nutrition transition may be a better explanation of the high rates of diet-related non-communicable disease in the past few decades [21]. In the current analysis, low adherence to the junk food pattern was associated with a 23% lower risk of incident HTN compared with the medium category after an adjustment for potential covariates. The underlying biological mechanisms may be explained as a high-fat-diet-induced sensitization of angiotensin-II-elicited hypertension is mediated by leptin through the upregulation of the central renin–angiotensin system and proinflammatory cytokines [22]. The association between avoiding excessive consumption of carbohydrates and sodium and promoted prevention of hypertension was further supported by a study based on 14,338 South Korean women [23]. Moreover, high saturated fat and sugar intake was found to be associated with accelerated development of cardiac pathology and dysfunction in hypertensive subjects [24,25]. However, the increased risk was not observed to be significant in the high level of such a pattern. One possible reason was that the intake did not reach the dangerous thresholds in the study population. Another was that the sample size was not enough for such an association in this study.
Moreover, it was observed that high adherence to the vegetable–grain pattern was associated with a 23% decreased risk of HTN, which was consistent with previous studies [5,26]. A 6-year follow-up study based on the Korean Genome and Epidemiology Study cohort demonstrated that women in the highest tertile of the whole grains and legumes pattern scores had a lower risk of incident hypertension [5]. Similar dietary patterns were reported by a randomized clinical trial involving Swedish women [26]. Grains and vegetables contain various nutrients and food components, which contribute to a synergistic and favorable effect on hypertension [27,28]. Vitamins and minerals that are included in vegetables and dietary fiber in whole grains have antihypertensive effects [29], and magnesium in diets directly moderates blood pressure by controlling the contraction or vasodilation of vascular cells [30]. Furthermore, a higher intake of whole grains and legumes was inversely related to specific cellular adhesion molecules and the reactive hyperemia index, which serve as surrogates of endothelial dysfunction and peripheral vascular function, respectively [31,32]. In addition, the components of whole grains and legumes may induce an increase in insulin sensitivity and anti-inflammatory markers, further lowering blood pressure levels [26,33].
Nevertheless, the finding remains controversial. No association was observed between vegetable consumption and risk of incident hypertension in middle-aged and older Korean adults [34]. This pattern only shared vegetables of food items in the vegetable-grain pattern, but no grain category was included. This may partly be attributed to the fact that a combination of vitamins, minerals, and bio-active compounds contributes to a lower hypertension risk than the intake of a single nutrient alone. Moreover, different effects in various studies may be caused by the inconsistency of study designs, demography characteristics, duration of follow-up time, and methods of measurement. In this study, the per capita daily intake of vegetables (355.35 g) in the second tertile of the vegetable–grain pattern met the amount (300–500 g) that is recommended by the Dietary Guidelines for Chinese Residents (2016 Edition) [35] and, therefore, was used as the reference group.
Except for a high-salt diet as a well-established detrimental factor for hypertension, divergent effects among different food groups on hypertension risk remain unclear. Furthermore, evidence from cohort studies that focus on the effects of various dietary patterns on incident hypertension in Southwest China is lacking. The strengths of this study should be noted. First, the longitudinal study and long duration assisted in making causal inferences between dietary patterns and new-onset hypertension. Second, the analysis of food consumption in the form of dietary patterns offered a comprehensive approach to disease prevention by addressing the collective health benefit of the whole diet and enhancing the applicability and sustainability in practice. Several diet patterns that were unique to the local customs were identified using factor analysis. Further strengths also included the genetic and socioeconomic variation with a considerable proportion of Chinese minorities, as well as a high follow-up rate (88%). Of course, some limitations should be discussed. One of the important limitations of this study was the possibility of measurement error from the self-reported diet assessment. Despite the adjustment for potential confounders, residual confounding cannot be ruled out. Moreover, the subjectivity in factor analysis modeling might have slight impacts on the results, but the dietary patterns were generally consistent in this cohort and the findings remained robust in the subgroups. In addition, diet may change during the 7-year follow-up period but we could not evaluate such change in those diet patterns and its possible impact on the risk of incident hypertension.
5. Conclusions
In conclusion, the junk food pattern was associated with a higher risk of incident hypertension and the vegetable–grain pattern was associated with a lower risk of incident hypertension in Southwest China. The diverse cohort offered some insights into the etiology of the association between dietary patterns and incident hypertension, and these findings provide additional support for dietary intervention strategies to improve population diet patterns, such as shifting from a junk food pattern to a vegetable–grain pattern in order to combat the growing disease burden among multi-ethnic Chinese populations.
Acknowledgments
We would like to thank all participants that were enrolled in this cohort study and all the health workers of the Guizhou Center for Disease Control and Prevention for contributing to the study.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182312378/s1, Figure S1: The flow chart, Table S1: Factor loading matrix after the dietary pattern rotation and average daily intake of each food group (g), Table S2: Common food list of the junk food pattern.
Author Contributions
Conceptualization, Y.Z., Y.W., C.F. and T.L.; methodology, Y.Z., Y.W. and C.F.; software, Y.C.; formal analysis, Y.Z. and Y.W.; investigation, J.Z. and L.X.; resources, T.L.; data curation, K.X. and Y.W.; writing—original draft preparation, Y.Z. and Y.W.; writing—review and editing, N.W., C.F. and T.L.; project administration, C.F. and T.L.; funding acquisition, T.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Guizhou Province Science and Technology Support Program (Qiankehe [2018]2819).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the Guizhou Center for Disease Control and Prevention (no. S2017-02).
Informed Consent Statement
Informed consent was obtained from all subjects that were involved in the study.
Data Availability Statement
The datasets that were generated for this study are available on request to the corresponding author.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou B., Bentham J., Di Cesare M., Bixby H., Danaei G., Cowan M.J., Paciorele C.J., Singh G., Hajifathalian K., Benett J.E., et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang J., Zhang L., Wang F., Liu L., Wang H. Prevalence, awareness, treatment, and control of hypertension in China: Results from a national survey. Am. J. Hypertens. 2014;27:1355–1361. doi: 10.1093/ajh/hpu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shim J.S., Oh K., Jung S.J., Kim H.C. Self-reported diet management and adherence to dietary guidelines in Korean adults with hypertension. Korean Circ J. 2020;50:432–440. doi: 10.4070/kcj.2019.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mozaffarian D., Benjamin E.J., Go A.S., Arnett D.K., Blaha M.J., Cushman M., de Ferranti S., Despres J.-P., Fullerton H.J., Howard V.J., et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 5.Song S., Kim J., Kim J. Gender differences in the association between dietary pattern and the incidence of hypertension in middle-aged and older adults. Nutrients. 2018;10:252. doi: 10.3390/nu10020252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sacks F.M., Campos H. Dietary therapy in hypertension. N. Engl. J. Med. 2010;362:2102–2112. doi: 10.1056/NEJMct0911013. [DOI] [PubMed] [Google Scholar]
- 7.Choi H.K., Curhan G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation. 2007;116:894–900. doi: 10.1161/CIRCULATIONAHA.107.703389. [DOI] [PubMed] [Google Scholar]
- 8.Sacks F.M., Svetkey L.P., Vollmer W.M., Appel L.J., Bray G.A., Harsha D., Obarzanek E., Conlin P.R., Miller E.R., Simons-Morton D.G., et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N. Engl. J. Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 9.Shen X.M., Huang Y.Q., Zhang X.Y., Tong X.Q., Zheng P.F., Shu L. Association between dietary patterns and prediabetes risk in a middle-aged Chinese population. Nutr. J. 2020;19:77. doi: 10.1186/s12937-020-00593-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park S.Y., Murphy S.P., Wilkens L.R., Yamamoto J.F., Sharma S., Hankin J.H., Henderson B.E., Kolonel L.N. Dietary patterns using the Food Guide Pyramid groups are associated with sociodemographic and lifestyle factors: The multiethnic cohort study. J. Nutr. 2005;135:843–849. doi: 10.1093/jn/135.4.843. [DOI] [PubMed] [Google Scholar]
- 11.Zheng P.F., Shu L., Zhang X.Y., Si C.J., Yu X.L., Gao W., Tong X.-Q., Zhang L. Association between dietary patterns and the risk of hypertension among Chinese: A cross-sectional study. Nutrients. 2016;8:239. doi: 10.3390/nu8040239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D., He Y., Li Y., Luan D., Yang X., Zhai F., Ma G. Dietary patterns and hypertension among Chinese adults: A nationally representative cross-sectional study. BMC Public Health. 2011;11:925. doi: 10.1186/1471-2458-11-925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruan Y., Huang Y., Zhang Q., Qin S., Du X., Sun Y. Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health. 2018;18:1106. doi: 10.1186/s12889-018-6003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao W.H., Ning G. Contents and methods of chronic disease surveillance project in China in 2010. Chin. J. Prev. Med. 2012;46:477–479. [Google Scholar]
- 15.China Obesity Working Group Prevention and control of overweight and obesity in Chinese adults. Preparation guide (excerpt) J. Nutr. 2004;26:1–4. [Google Scholar]
- 16.Hu F.B., Rimm E., Smith-Warner S.A., Feskanich D., Stampfer M.J., Ascherio A., Sampson L., Willett W.C. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am. J. Clin. Nutr. 1999;69:243–249. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 17.Chiavaroli L., Viguiliouk E., Nishi S.K., Blanco Mejia S., Rahelić D., Kahleová H., Salas-Salvado J., Kendall C.W., Sievenpiper J.L. DASH dietary pattern and cardiometabolic outcomes: An umbrella review of systematic reviews and meta-analyses. Nutrients. 2019;11:338. doi: 10.3390/nu11020338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen P., He G., Zou X., Zhang X., Li J., Wang Z., Gao H., Luo L., Zhang Z., Yu J., et al. Genetic diversities and phylogenetic analyses of three Chinese main ethnic groups in southwest China: A Y-Chromosomal STR study. Sci. Rep. 2018;8 doi: 10.1038/s41598-018-33751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X., Liu A., Du M., Wu J., Wang W., Qian Y., Zheng H., Liu D., Nan X., Jia L., et al. Diet quality is associated with reduced risk of hypertension among Inner Mongolia adults in northern China. Public Health Nutr. 2020;23:1543–1554. doi: 10.1017/S136898001900301X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du S.F., Wang H.J., Zhang B., Zhai F.Y., Popkin B.M. China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes. Rev. 2014;15:8–15. doi: 10.1111/obr.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhai F., Fu D., Du S., Ge K., Chen C., Popkin B.M. What is China doing in policy-making to push back the negative aspects of the nutrition transition? Public Health Nutr. 2002;5:269–273. doi: 10.1079/PHN2001303. [DOI] [PubMed] [Google Scholar]
- 22.Xue B., Yu Y., Zhang Z., Guo F., Beltz T.G., Thunhorst R.L., Felder R.B., Johnson A.K. Leptin mediates high-fat diet sensitization of angiotensin II-elicited hypertension by upregulating the brain renin-angiotensin system and inflammation. Hypertension. 2016;67:970–976. doi: 10.1161/HYPERTENSIONAHA.115.06736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oh H.Y., Kim M.K., Lee M., Kim Y.O. Macronutrient composition and sodium intake of diet are associated with risk of metabolic syndrome and hypertension in Korean women. PLoS ONE. 2013;8:e78088. doi: 10.1371/journal.pone.0078088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Majane O.H., Vengethasamy L., du Toit E.F., Makaula S., Woodiwiss A.J., Norton G.R. Dietary-induced obesity hastens the progression from concentric cardiac hypertrophy to pump dysfunction in spontaneously hypertensive rats. Hypertension. 2009;54:1376–1383. doi: 10.1161/HYPERTENSIONAHA.108.127514. [DOI] [PubMed] [Google Scholar]
- 25.Stanley W.C., Shah K.B., Essop M.F. Does junk food lead to heart failure? Importance of dietary macronutrient composition in hypertension. Hypertension. 2009;54:1209–1210. doi: 10.1161/HYPERTENSIONAHA.109.128660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tovar J., Nilsson A., Johansson M., Björck I. Combining functional features of whole-grain barley and legumes for dietary reduction of cardiometabolic risk: A randomised cross-over intervention in mature women. Br. J. Nutr. 2014;111:706–714. doi: 10.1017/S000711451300305X. [DOI] [PubMed] [Google Scholar]
- 27.Borneo R., León A.E. Whole grain cereals: Functional components and health benefits. Food Funct. 2012;3:110–119. doi: 10.1039/C1FO10165J. [DOI] [PubMed] [Google Scholar]
- 28.Villegas R., Gao Y.T., Yang G., Li H.L., Elasy T.A., Zheng W., Shu X.O. Legume and soy food intake and the incidence of type 2 diabetes in the Shanghai Women’s Health Study. Am. J. Clin. Nutr. 2008;87:162–167. doi: 10.1093/ajcn/87.1.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aleixandre A., Miguel M. Dietary fiber and blood pressure control. Food Funct. 2016;7:1864–1871. doi: 10.1039/C5FO00950B. [DOI] [PubMed] [Google Scholar]
- 30.Bain L.K., Myint P.K., Jennings A., Lentjes M.A., Luben R.N., Khaw K.T., Wareham N.J., Welch A.A. The relationship between dietary magnesium intake, stroke and its major risk factors, blood pressure and cholesterol, in the EPIC-Norfolk cohort. Int. J. Cardiol. 2015;196:108–114. doi: 10.1016/j.ijcard.2015.05.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jenkins D.J., Kendall C.W., Vuksan V., Faulkner D., Augustin L.S., Mitchell S., Ireland C., Srichaikul K., Mirrahimi A., Chiavaroli L., et al. Effect of lowering the glycemic load with canola oil on glycemic control and cardiovascular risk factors: A randomized controlled trial. Diabetes Care. 2014;37:1806–1814. doi: 10.2337/dc13-2990. [DOI] [PubMed] [Google Scholar]
- 32.Sijtsma F.P., Meyer K.A., Steffen L.M., Van Horn L., Shikany J.M., Odegaard A.O., Gross M.D., Kromhout D., Jacobs D.R., Jr. Diet quality and markers of endothelial function: The CARDIA study. Nutr. Metab. Cardiovasc. Dis. 2014;24:632–638. doi: 10.1016/j.numecd.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steffen L.M., Jacobs D.R., Jr., Murtaugh M.A., Moran A., Steinberger J., Hong C.P., Sinaiko A.R. Whole grain intake is associated with lower body mass and greater insulin sensitivity among adolescents. Am. J. Epidemiol. 2003;158:243–250. doi: 10.1093/aje/kwg146. [DOI] [PubMed] [Google Scholar]
- 34.Kim J., Kim J. Association between fruit and vegetable consumption and risk of hypertension in middle-aged and older Korean adults. J. Acad. Nutr. Diet. 2018;118:1438–1449.e5. doi: 10.1016/j.jand.2017.08.122. [DOI] [PubMed] [Google Scholar]
- 35.Tang O., Miller E.R., Gelber A.C., Choi H.K., Appel L.J., Juraschek S.P. DASH diet and change in serum uric acid over time. Clin. Rheumatol. 2017;36:1413–1417. doi: 10.1007/s10067-017-3613-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets that were generated for this study are available on request to the corresponding author.