Abstract
Stressful experiences commonly increase among health workers during the coronavirus disease 2019 (COVID‐19) pandemic. From this perspective, this study primarily aimed to examine the mediating role of resilience in the effect of perceived social support on work stress among health workers. The sample of the study consisted of 402 health workers. In the research, the “General Work Stress Scale,” “Brief Resiliency Scale,” and “Multidimensional Scale of Perceived Social Support” were used. There was a statistically significant negative correlation between work stress and social support (r = −0.223, p = 0.00) and resilience (r = −0.432, p = 0.00), and a statistically significant positive correlation between social support and resilience (r = 0.226, p = 0.00). Resilience mediates the relationship between perception of social support and work stress. When planning effective intervention strategies, it will be critical to reduce the risk of adverse mental health outcomes in health workers, who are fighting against the COVID‐19 pandemic, by increasing social support and resilience and reducing work stress.
Keywords: health worker, resilience, social support, work stress
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has become an urgent health problem worldwide and, in this period, health workers have been in the front lines against the pandemic. It has become more important to investigate the psychological impact of the outbreak on health workers as the number of cases continues to increase and health workers have become more vulnerable to trauma and psychological risks (Carmassi et al., 2020; Salazar de Pablo et al., 2020). Factors such as the rapid increase in the number of critically ill patients, high daily mortality rates, changes in hospital procedures, inadequate personal equipment, physical fatigue, risk of infection and transmission, stigma, and loss of social support can have significant impacts on the physical and mental health of health workers (De Kock et al., 2021; Papoutsi et al., 2020).
Available studies revealed that health workers who are in the front lines of the fight against COVID‐19 have not recovered from the psychological and mental health consequences of the pandemic and that the stress level is high among health workers (Alnazly et al., 2021; Saladino et al., 2020; Serrano‐Ripoll et al., 2020). Stress is a factor that affects the psychosocial life of a person and damages the current balance. Although health workers encounter many stressful conditions during the pandemic, personal, familial, social, and work‐related protective factors increase their resilience (Carmassi et al., 2020; Labrague, 2021). It is emphasized that social support can increase resilience to stress and help protect from the development of trauma‐related psychopathology. It was demonstrated that individuals are more likely to be exposed to negative mental and psychological consequences when they do not have adequate resilience and coping skills during stressful events (including disasters and disease outbreaks) (Conti et al., 2021; Labrague, 2021). Resilience is a process that enables adaptation when faced with major stresses such as disturbance and trauma. Individuals with high resilience engage in a restructuring process when faced with sources of stress and difficulties, go through a more positive experience, and consequently, they actively respond to the results, which are shown as more flexible and stronger self‐efficacy (Duncan, 2020; Xiao et al., 2020). A study on COVID‐19 reported that health workers are facing intense pressure due to stress, depression, and anxiety and that resilience and social support play a role as mediating variables (Bohlken et al., 2020).
In Turkey, the first COVID‐19 case was reported on March 11. The number of infected cases in Turkey exceeded 5 million at the time of the research (30.05.2021–05.06.2021). Although the number of patients who require hospitalization is decreasing, the heavy burden on the health system remains (WHO Turkey Internet, 2021). Health workers have been the most affected population during the pandemic. Immediate interventions are of great importance to reduce work stress, increase resilience, improve the well‐being of health workers, and the capacity of health‐care systems (Lou et al., 2021). Evaluating the effect of social support perceived by health workers on work stress and the variables that may play a mediating role in this process can help alleviate the negative effects and ensure the quality and maintenance of health‐care services during the pandemic period. Therefore, the present study aimed to evaluate the mediating role of resilience in the effect of perceived social support on work stress in health workers working in Turkey during the COVID‐19 pandemic.
1.1. Research hypotheses
Two hypotheses were proposed based on the above literature information regarding relevant theoretical and empirical research:
Hypothesis 1
There is a significant relationship between work stress, perception of social support, and resilience.
Hypothesis 2
Resilience mediates the relationship between work stress and social support.
2. METHODS
2.1. Design and sample
This descriptive and cross‐sectional study was conducted with 402 health workers between May and June 2021, during the period when the number of COVID‐19 cases was high. Health workers who worked in public, private, and university hospitals and who were voluntary to participate in the research were included in the sample. An online questionnaire was used to minimize face‐to‐face interactions with all participants and facilitate the participation of health workers who worked intensively during this emergency period. The form created via Google Forms was sent to health workers electronically (Facebook, Instagram, and Whatsapp). The form, which had informed consent at the beginning, was completed online by those who gave consent. Of the participants, 72.1% were women; 48.5% were nurses; 16.2% were physicians; 10.4% were midwives; 7.2% were emergency medicine technicians; 5.5% were paramedics; 12.2% were other health workers (physiotherapists, dietitians, etc.). Of the health workers, 56.2% had a bachelor's degree and 78.4% worked in a state health institution. A total of 35.8% of health workers worked in the emergency department and 55% had 0–5 years of working experience.
2.2. Data gathering tools
2.2.1. Personal Information Form
The form was prepared by the researchers in line with the literature (Arıkan, 2021; Labrague, 2021) and consists of nine questions regarding information such as age, gender, profession, education level, department of work, and years of work.
2.2.2. General Work Stress Scale
The scale was developed by De Bruin (2006 and is a 5‐point Likert‐type scale consisting of nine items. High scores indicate high work stress whereas low scores indicate low work stress. The Turkish validity and reliability study was performed by Teles and the Cronbach α value of the scale was found 0.91 (Teles, 2021). In this study, the Cronbach α value was determined as 0.93.
2.2.3. Brief Resiliency Scale (BRS)
The scale was developed by Smith et al. (2008). The one‐dimensional version consisting of six items, of which the Turkish validity and reliability study was conducted by Dogan (2015), was used. Participants ranked the statements on a 5‐point Likert‐type scale (Dogan, 2015). In this study, the Cronbach α value of BRS was found to be 0.80.
2.2.4. Multidimensional Scale of Perceived Social Support (MSPSS)
The scale of perceived social support was developed by Zimet et al. (1990) and adapted to Turkish by Eker et al. (2001). The scale consists of three dimensions, family support, friend support, and significant other support, and 12 items and is ranked in 7‐point Likert‐type scale (Eker et al., 2001). In this study, the Cronbach α value was found as 0.94.
2.3. Data analysis
The data were analyzed in the SPSS 25 (IBM Corp.) package program. The significance level of all results was taken as α = 0.05. The assumption of normality of the data was tested with normality tests (Kolmogorov–Smirnov and Shapiro–Wilk) and the data showed normal distribution with 95% confidence interval. The sociodemographic characteristics of the participants were determined using descriptive statistics (number, percentage, mean, and standard deviation). The data were analyzed using mean scores and regression analysis PROCESS model 4.
As seen in the “Conceptual Model of Mediation Effect” presented in Figure 1, the mediating variable was psychological resilience; the predictor variable was the perception of social support; the predicted variable was work stress. The results of the correlation analysis showed that there was a significant relationship between the predictor variable, perception of social support, and the predicted variable, work stress, and the mediating variable, resilience. This result demonstrated that the mediating role of resilience in the effect of social support on work stress could be examined. For this purpose, the analysis was carried out with the PROCESS Multiple Mediation Model 4, which was developed by Hayes (2018) to obtain more valid and reliable results for the analysis of mediation models (Hayes, 2018).
Figure 1.
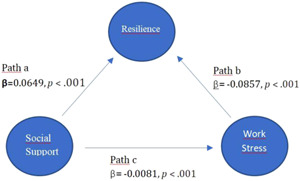
Conceptual model of mediation effect
2.4. Ethical considerations
To carry out the study, approval was taken from the Clinical Research Ethics Committee (2021/114) and permission was taken from the Ministry of Health.
3. RESULTS
Table 1 shows the mean scores of the participants on the scales. The mean Work Stress Scale score of health workers was 3.14 ± 1.05; the mean BRS score was 18.17 ± 4.94; the mean MSPSS score was 65.27 ± 17.23. The mean MSPSS family subdimension score was 23.19 ± 5.84; the mean friend subdimension score was 22.20 ± 5.95; the mean significant other subdimension score was 19.87 ± 8.49.
Table 1.
Mean perceived social support, work stress, and resilience scores of health workers (n = 402)
| Scales | Mean ± SD | Min–Max | Range |
|---|---|---|---|
| Work stress | 3.14 ± 1.05 | 1–5 | 1–5 |
| Resilience | 18.17 ± 4.94 | 6–30 | |
| Social support | 65.27 ± 17.23 | 12–84 | |
| Family | 23.19 ± 5.84 | 4–28 | |
| Friend | 22.20 ± 5.95 | 4–28 | |
| Significant other | 19.87 ± 8.49 | 4–28 |
Abbreviation: SD, standard deviation
3.1. Correlations between social support, work stress, and resilience levels
Table 2 shows correlations between social support, work stress, and resilience levels. A statistically significant negative correlation was found between work stress and social support (r = −0.223, p = 0.00); a significant negative correlation was found between work stress and resilience (r = −0.432, p = 0.00). A statistically significant positive correlation was found between social support and resilience (r = 0.226, p = 0.00). Accordingly, the H1 hypothesis was supported.
Table 2.
Correlations between work stress, resilience, and social support levels
| Scales | Work stress | Social support | Resilience |
|---|---|---|---|
|
– | −0.223* | −0.432* |
|
−0.223* | – | 0.226* |
p ≤ 0.001.
3.2. Regression analysis results regarding the mediating role of resilience in the relationship between social support and work stress
Table 3 shows the results of the regression analysis to determine the mediating role of resilience in the effect of social support on work stress. According to the analysis results, social support significantly and positively affected resilience (b = 0.0649, SE = 0.14, 95% bias‐corrected and accelerated bootstrap (BCa) CI = [0.0374, 0.0923], p < 0.001). Social support explained 22% of the variance in the resilience variable (F = 21.60, p < 0.001). This result shows that resilience increases as the social support score increases (path a).
Table 3.
Regression analysis results regarding the role of social support mediator in the relationship between work stress and resilience
| Resulting variables | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilience (mediator) | Work stress (variable Y) | ||||||||||
| β | SE | 95% BCa confidence interval | β | SE | 95% BCa confidence interval | ||||||
| LLCI | ULCI | LLCI | ULCI | ||||||||
| Social support (Variable X) | Path a | 0.0649 * | 0.140 | 0.0374 | 0.0923 | Path c' | −0.0081 * | 0.0028 | −0.0136 | −0.0025 | |
| Resilience (Mediator) | – | – | – | – | Path b | −0.0857 * | 0.0098 | −0.1049 | −0.0664 | ||
| Constant | |||||||||||
| R 2 = 0.22, F = 21.60, p = <0.001 | R 2 = 0.45, F = 50.72, p = <0.001 | ||||||||||
| Total effect X on Y | Path c | −0.0136 | 0.0030 | −0.0195 | −0.0078 | ||||||
| Direct effect X on Y | Path c' | −0.0081 | 0.0028 | −0.0136 | −0.0025 | ||||||
| Indirect effect X on Y | a.b | −0.0056 | 0.0013 | −0.0084 | −0.0031 | ||||||
Abbreviations: R 2, adjusted R 2; B, partial regression coefficient; β, standard partial regression coefficient; 95% CI, 95% BCa (bias corrected and accelerated bootstrap) confidence interval.
p ≤ 0.001.
Regression analysis showed that resilience had a significant negative effect on work stress (b = −0.0857, SE = 0.098, 95% BCa CI = [0.1049, 0.0664], p < 0.01). Accordingly, work stress decreases as resilience increases (path b). When resilience was checked, it was determined that the direct effect of social support on work stress (path c') was significant (b = −0.0081, SH = 0.0028, 95% BCa CI = [−0.0136, 0.0025], p = 0.1892).
At the final stage, the indirect effect of social support on work stress through resilience was examined (a.b) with a boostrapping method and the indirect effect of social support on work stress was determined to be significant (b = −0.0056, SE = 0.0013, 95% BCa CI = [−0.0084, −0.0031]). Because according to boostrapping analysis, a corrected and accelerated confidence interval of 95% (95% BCa CI) does not include 0 (zero). Social support and resilience together explained approximately 45% of work stress (F = 50.72, p < 0.001). According to these results, resilience mediates the relationship between social support and work stress. In line with these results, the H2 hypothesis was supported.
4. DISCUSSION
Work stress is an important factor that affects the quality of life, life satisfaction, and physical and mental well‐being of individuals (Charkhat Gorgich et al., 2017). It is necessary to determine the positive and negative factors that can affect work stress to prevent its negative consequences. In this study, it was investigated whether resilience has a mediating role in the effect of social support on work stress in health workers during the pandemic. Within this framework, primarily, the relationships between the variables were examined in the research. As a result of the correlation analysis, it was determined that there were negative significant relationships between work stress, social support, and resilience. According to this finding, work stress decreases as the social support level and resilience increase.
Specifically, our findings conclude that social support is negatively associated with work stress, confirming our first hypothesis. This result is consistent with previous studies associating work stress with social support in health workers (Nowicki et al., 2020; Woon et al., 2020). It was stated that how a person adapts to stress is shaped by the social support one receives, that social support has a protective role in work stress, and that it increases the quality of life by reducing the negative effects of work stress (Arıkan, 2021). Another study showed that social support from colleagues increased nurses' job satisfaction (Orgambídez‐Ramos & de Almeida, 2017). A study conducted with nurses reported a direct relationship between administrator support and job satisfaction (Bagheri Hossein Abadi et al., 2020). In a study conducted with health workers in China, it was determined that work‐related social support from family partially mediates the relationship between occupational stress and attitudes toward evidence‐based practices (Qiao et al., 2018). It was stated that supportive professional relationships help employees cope with work stress (Waddimba et al., 2016). It is suggested that it is necessary to improve the social support sources of health workers in this period when the increased workload during the pandemic is more critically important for work stress.
In this study, resilience was found to be negatively associated with work stress and this finding is consistent with previous empirical studies (Kreh et al., 2021; Maiorano et al., 2020). These findings are important for understanding how resilience affects work stress among health workers. In a study, health workers with high resilience reported less stress, fatigue, and anxiety (Huffman et al., 2021). Bahadır Yılmaz (2017) stated that resilience enables nurses to cope with their work environment and maintain healthy and stable psychological functioning. In this sense, it is thought that studies that will increase resilience in health workers will reduce work stress. Rogers (2016) determined that educational interventions such as resilience workshops, problem‐solving activities in small groups, reflection, cognitive‐behavioral training, mindfulness and relaxation training, and mentoring can be provided to improve resilience. A systematic review examining methods used to increase resilience in physicians determined that the most frequently used interventional strategies are psychosocial skills training and mindfulness training (Fox et al., 2018). Considering the positive outcomes of interventions to increase resilience in the literature, interventions to increase resilience are recommended to be urgently planned and implemented especially for the increased workload, stress, and anxiety during the pandemic period.
The mediating role of resilience in the relationship between social support and work stress was confirmed in this study. It can be said that a higher level of social support leads to stronger resilience, which in turn reduces work stress. A study conducted with medical doctors determined that social support has a role among the factors affecting resilience (McKinley et al., 2019). Resilience mediated the association between COVID‐19 stressors and psychological distress in Chinese HIV health‐care providers during the COVID‐19 pandemic (Tam et al., 2021). Another study reported that resilience level differentiated the direct and indirect effects of stress on depression (Havnen et al., 2020). A study among Chinese rural elderly individuals in nursing homes confirmed the mediating role of resilience in the relationship between social support and quality of life (Wu et al., 2018). In a study conducted with nurses, it was found that friend support had an indirect effect on nurses' resilience (Wang et al., 2018). Based on this finding, it is thought that studies to increase resilience and social support should be supported. In employees, perceived stress and low social support are among the predictive factors of negative psychological outcomes. Even people get back to their routine life when the pandemic period is over, the mental effects of the pandemic may persist for months or even years (Arıcı Ozcan, 2019). Research findings will contribute to the planning of individual and organizational interventions that will contribute to the increase of resilience and perceived social support in employees and reduction of the level of stress they perceive for their jobs.
This study provided an excellent basis for evaluating the mediating role of resilience in the effect of social support on work stress in health workers in Turkey. This study has some limitations. The generalizability of the results is limited because a convenience sample was used in this study. In addition, the findings are based on individuals' self‐reports. Therefore, the generalizability of the results obtained represents a limitation of this study.
5. CONCLUSION
In this study, it was determined that social support and resilience have an effect on work stress in health workers. This study showed that the work stress of health workers can be reduced by increasing social support and resilience. Resilience fully mediates the impact of social support on work stress in health workers. This study provides important and instructive information to administrators in the workplace about strategies that can increase resilience in health workers. It is important for hospital administrators to understand how to develop effective counseling programs to reduce the factors that contribute to work stress. Coping skills should be developed to increase resilience among health workers and alternative ways should be determined to provide social support.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions as follows: (1) Ayşe Karadaş and Songül Duran conceived and designed the study; (2) Songül Duran and Ayşe Karadaş acquired, analyzed, and interpreted the data; (3) Ayşe Karadaş drafted the article and Songül Duran critically revised it to add important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibilityfor its accuracy and integrity.
1. PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/jcop.22742
ACKNOWLEDGMENTS
The authors are thankful to the health workers who participated to this study.
Karadaş, A. , Duran, S. (2022). The effect of social support on work stress in health workers during the pandemic: The mediation role of resilience. J Community Psychol, 50, 1640–1649. 10.1002/jcop.22742
REFERENCES
- Alnazly, E. , Khraisat, O. M. , Al‐Bashaireh, A. M. , & Bryant, C. L. (2021). Anxiety, depression, stress, fear and social support during COVID‐19 pandemic among Jordanian healthcare workers. PLOS One, 12(163), e0247679. 10.1371/journal.pone.0247679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arıcı Ozcan N. (2019). Yetişkinlerde Travma Sonrası Stres ve Öz Duyarlılığın Travma Sonrası Büyüme Üzerindeki Yordayıcı Rolü. OPUS Uluslararası Toplum Araştırmaları Dergisi, 14(20), 621–642. 10.26466/opus.594006 [DOI] [Google Scholar]
- Arıkan, G. (2021). Stress in COVID‐19 pandemic: Negative and positive outcomes, and the possible role of preventive interventions. Current Approaches in Psychiatry, 13, 135–145. [in Turkish]. [Google Scholar]
- Bagheri Hossein Abadi, M. , Taban, E. , Khanjani, N. , Naghavi Konjin, Z. , Khajehnasiri, F. , & Samaei, S. E. (2020). Relationships between job satisfaction and job demand, job control, social support, and depression in Iranian nurses. The Journal of Nursing Research, 29, e143. 10.1097/jnr.0000000000000410 [DOI] [PubMed] [Google Scholar]
- Bahadır Yılmaz, E. (2017). Resilience as a strategy for struggling against challenges related to the nursing profession. Chinese Nursing Research, 4, 9–13. [Google Scholar]
- Bohlken, J. , Schömig, F. , Lemke, M. R. , Pumberger, M. , & Riedel‐Heller, S. G. (2020). COVID‐19 pandemic: stress experience of healthcare workers: A short current review. Psychiatrische Praxis, 47, 190–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi, C. , Foghi, C. , Dell'Oste, V. , Cordone, A. , Bertelloni, C. A. , Bui, E. , & Dell'Osso, L. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID‐19 pandemic. Psychiatry Research, 292, 113312. 10.1016/j.psychres.2020.113312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charkhat Gorgich E. A., Zare S., Ghoreishinia G., Barfroshan S., Arbabisarjou A., Yoosefian N. (2017). Job stress and mental health among nursing staff of educational hospitals in South East Iran. Thrita, Advance online publication. 10.5812/thrita.45421 [DOI] [Google Scholar]
- Conti, C. , Fontanesi, L. , Lanzara, R. , Rosa, I. , Doyle, R. L. , & Porcelli, P. (2021). Burnout status of Italian healthcare workers during the first COVID‐19 pandemic peak period. Healthcare, 9(5):510. 10.3390/healthcare9050510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bruin G. P. (2006). The dimensionality of the general work stress scale: A hierarchical exploratory factor analysis. SA Journal of Industrial Psychology, 32, (4), 68–75. 10.4102/sajip.v32i4.250 [DOI] [Google Scholar]
- De Kock, J. H. , Latham, H. A. , Leslie, S. J. , Grindle, M. , Munoz, S. A. , Ellis, L. , Polson, R. , & O'Malley, C. M. (2021). A rapid review of the impact of COVID‐19 on the mental health of healthcare workers: Implications for supporting psychological well‐being. BMC Public Health, 21, 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogan, T. (2015). Adaptation of the Brief Resilience Scale into Turkish: A validity and reliability study. The Journal of Happiness & Well‐Being, 3, 93–102. [in Turkish]. [Google Scholar]
- Duncan, D. L. (2020). What the COVID‐19 pandemic tells us about the need to develop resilience in the nursing workforce. Nursing Management, 27, 22–27. [DOI] [PubMed] [Google Scholar]
- Eker, D. , Arkar, H. , & Yaldız, H. (2001). Factorial structure, validity, and reliability of revised form of the Multidimensional Scale of Perceived Social Support. Turkish Journal of Psychiatry, 12(1), 17–25. [in Turkish]. https://app.trdizin.gov.tr/publication/paper/detail/TVRVNU9ESXk [Google Scholar]
- Fox, S. , Lydon, S. , Byrne, D. , Madden, C. , Connolly, F. , & O'Connor, P. (2018). A systematic review of interventions to foster physician resilience. Postgraduate Medical Journal, 94, 162–170. [DOI] [PubMed] [Google Scholar]
- Havnen, A. , Anyan, F. , Hjemdal, O. , Solem, S. , Riksfjord, M. G. , & Hagen, K. (2020). Resilience moderates negative outcome from stress during the COVID‐19 pandemic: A moderated mediation approach. International Journal of Environmental Research and Public Health, 17, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach (2nd ed., pp. 91‐95). The Guilford Press. [Google Scholar]
- Huffman, E. M. , Athanasiadis, D. I. , Anton, N. E. , Haskett, L. A. , Doster, D. L. , Stefanidis, D. , & Lee, N. K. (2021). How resilient is your team? Exploring healthcare providers' well‐being during the COVID‐19 pandemic. The American Journal of Surgery, 221, 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreh, A. , Brancaleoni, R. , Magalini, S. C. , Chieffo, D. , Flad, B. , Ellebrecht, N. , & Juen, B. (2021). Ethical and psychosocial considerations for hospital personnel in the Covid‐19 crisis: Moral injury and resilience. PLOS One, 16, e0249609. 10.1371/journal.pone.0249609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. (2021). Psychological resilience, coping behaviours and social support among health care workers during the COVID‐19 pandemic: A systematic review of quantitative studies. Journal of Nursing Managemet, Apr, 29, 12–1905. 10.1111/jonm.13336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou, N. M. , Montreuil, T. , Feldman, L. S. , Fried, G. M. , Lavoie‐Tremblay, M. , Bhanji, F. , Kennedy, H. , Kaneva, P. , Drouin, S. , & Harley, J. M. (2021). Evaluations of healthcare providers' perceived support from personal, hospital, and system resources: Implications for well‐being and management in healthcare in Montreal, Quebec, during COVID‐19. Evaluation & the Health Professionals, 27, 319–322 1632787211012742. 10.1177/01632787211012742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiorano, T. , Vagni, M. , Giostra, V. , & Pajardi, D. (2020). COVID‐19: Risk factors and protective role of resilience and coping strategies for emergency stress and secondary trauma in medical staff and emergency workers‐an online‐based inquiry. Sustainability, 12(21), 9004. 10.3390/su12219004 [DOI] [Google Scholar]
- McKinley, N. , Karayiannis, P. N. , Convie, L. , Clarke, M. , Kirk, S. J. , & Campbell, W. J. (2019). Resilience in medical doctors: A systematic review. Postgraduate Medical Journal, 95, 140–147. [DOI] [PubMed] [Google Scholar]
- Nowicki, G. J. , Ślusarska, B. , Tucholska, K. , Naylor, K. , Chrzan‐Rodak, A. , & Niedorys, B. (2020). The severity of traumatic stress associated with COVID‐19 pandemic, perception of support, sense of security, and sense of meaning in life among nurses: Research protocol and preliminary results from Poland. International Journal of Environmental Research and Public Health, 17, 6491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgambídez‐Ramos, A. , & de Almeida, H. (2017). Work engagement, social support, and job satisfaction in Portuguese nursing staff: A winning combination. Applied Nursing Research, 36, 37–41. [DOI] [PubMed] [Google Scholar]
- Papoutsi, E. , Giannakoulis, V. , Ntella, V. , Pappa, S. , & Katsaounou, P. (2020). Global burden of COVID‐19 pandemic on healthcare workers. ERJ Open Research, 6, 00195–02020. 10.1183/23120541.00195-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiao, S. , Li, X. , Zhou, Y. , Shen, Z. , & Stanton, B. (2018). Attitudes toward evidence‐based practices, occupational stress and work‐related social support among health care providers in China: A SEM analysis. PLOS One, 13, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers, D. (2016). Which educational interventions improve healthcare professionals' resilience? Medical Teacher, 38, 1236–1241. [DOI] [PubMed] [Google Scholar]
- Saladino, V. , Algeri, D. , & Auriemma, V. (2020). The psychological and social impact of Covid‐19: New perspectives of well‐being. Frontiers in Psychology, 11, 2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo, G. , Vaquerizo‐Serrano, J. , Catalan, A. , Arango, C. , Moreno, C. , Ferre, F. , Shin, J. I. , Sullivan, S. , Brondino, N. , Solmi, M. , & Fusar‐Poli, P. (2020). Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta‐analysis. Journal of Affective Disorders, 275, 48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano‐Ripoll, M. J. , Meneses‐Echavez, J. F. , Ricci‐Cabello, I. , Fraile‐Navarro, D. , Fiol‐Deroque, M. A. , Pastor‐Moreno, G. , Castro, A. , Ruiz‐Pérez, I. , Zamanillo Campos, R. , & Gonçalves‐Bradley, D. C. (2020). Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta‐analysis. Journal of Affective Disorders, 277, 347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B. W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, (3), 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Tam, C. C. , Sun, S. , Yang, X. , Li, X. , Zhou, Y. , & Shen, Z. (2021). Psychological distress among HIV healthcare providers during the COVID‐19 pandemic in China: Mediating roles of ınstitutional support and resilience. AIDS and Behavior, 25(1), 9–17. 10.1007/s10461-020-03068-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleş Mesut (2021). Validity and reliability of the Turkish version of the General Work Stress Scale. Journal of Nursing Management, 29, (4), 710–720. 10.1111/jonm.13211 [DOI] [PubMed] [Google Scholar]
- Waddimba, A. C. , Scribani, M. , Hasbrouck, M. A. , Krupa, N. , Jenkins, P. , & May, J. J. (2016). Resilience among employed physicians and mid‐level practitioners in Upstate New York. Health Services Research, 51, 1706–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L. , Tao, H. , Bowers, B. J. , Brown, R. , & Zhang, Y. (2018). Influence of social support and self‐efficacy on resilience of early career registered nurses. Western Journal of Nursing Research, 40, 648–664. [DOI] [PubMed] [Google Scholar]
- WHO Turkey The current COVID‐19 situation. 2021. Accessed June 3, 2021. https://www.who.int/countries/tur/
- Woon, L. S. , Sidi, H. , Nik Jaafar, N. R. , & Leong Bin Abdullah, M. F. I. (2020). Mental health status of University Healthcare workers during the COVID‐19 pandemic: A post‐movement lockdown assessment. International Journal of Environmental Research and Public Health, 8(17), 9155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, M. , Yang, Y. , Zhang, D. , Zhao, X. , Sun, Y. , Xie, H. , Jia, J. , Su, Y. , & Li, Y. (2018). Association between social support and health‐related quality of life among Chinese rural elders in nursing homes: The mediating role of resilience. Quality of Life Research, 27, 783–792. [DOI] [PubMed] [Google Scholar]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID‐19) in January and February 2020 in China. Medical Science Monitor, 26, e923549‐1–e923549‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G. D., Powell S. S., Farley G. K., Werkman S., Berkoff K. A. (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55, (3‐4), 610–617. 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]


