Abstract
Objective
This study explored risk and resilience factors of mental health functioning during the coronavirus disease (COVID‐19) pandemic.
Methods
A sample of 467 adults (M age = 33.14, 63.6% female) reported on mental health (depression, anxiety, posttraumatic stress disorder [PTSD], and somatic symptoms), demands and impacts of COVID‐19, resources (e.g., social support, health care access), demographics, and psychosocial resilience factors.
Results
Depression, anxiety, and PTSD rates were 44%, 36%, and 23%, respectively. Supervised machine learning models identified psychosocial factors as the primary significant predictors across outcomes. Greater trauma coping self‐efficacy and forward‐focused coping, but not trauma‐focused coping, were associated with better mental health. When accounting for psychosocial resilience factors, few external resources and demographic variables emerged as significant predictors.
Conclusion
With ongoing stressors and traumas, employing coping strategies that emphasize distraction over trauma processing may be warranted. Clinical and community outreach efforts should target trauma coping self‐efficacy to bolster resilience during a pandemic.
Keywords: anxiety, coping self‐efficacy, COVID‐19, depression, PTSD, trauma
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic has seen devastating physical, mental, and economic impacts. The chronic, ongoing nature of a pandemic that is a threat to life, coupled with economic repercussions, forced social isolation, and widespread uncertainties are inducing a wide range of psychological responses, including fear, anxiety, traumatic stress, and depression. The toll of pandemics on mental health over the last few decades is well‐established (Taylor, 2019), but the psychological response to COVID‐19 appears highly varied (Gao et al., 2020; Huang & Zhao, 2020; Liu, Zhang, et al., 2020; Taylor et al., 2020), partly due to individual differences in level of risk, exposure, and impact. For some, the pandemic represents a major stressor that impacts financial, educational, and social functioning. For others, it represents a trauma, in which the individual may be experiencing life‐threatening issues due to the virus or bearing witness to the sudden and unexpected death of a loved one. And for others, it may represent a more minor annoyance, where life is disrupted but not severely impacted. As compared to other potentially traumatic events (PTEs), the ongoing nature and prolonged duration of COVID‐19 presents a unique temporal window with confluence of posttraumatic, peritraumatic, and future‐oriented catalytic factors for psychopathology. Additionally, COVID‐19's global reach has distinguished it from more regionally‐specific pandemics described in pandemic literature, such as MERS and SARS. As COVID‐19 presents a novel collective psychosocial experience, cross‐disciplinary researchers are attempting to understand the heterogeneity of psychological responses for both vulnerable and general populations, and to identify risk and protective factors associated with better or worse adaptation.
A plethora of research has emerged documenting rates of psychological disorders and exploring possible predictors of poor mental health response. Meta‐analyses have shown that individuals who are struggling with COVID‐19 experience a diffuse set of symptoms crossing a number of diagnoses; rates of depression range from 14.6% to 48.3%, rates of anxiety range from 6.3% to 50.9%, and rates of posttraumatic stress disorder (PTSD) range from 7.0% to 53.8% (Xiong et al., 2020). While somatic symptoms have been comparatively less studied as an outcome measure of distress during COVID‐19, it is not uncommon for individuals to manifest distress somatically and the prevalence of somatic symptoms appear elevated in the general population (16.6%) in one recent COVID‐19 study (Ran et al., 2020).
Researchers attempting to identify predictors of mental health outcomes related to COVID‐19 have primarily applied traditional statistical methods that examine group differences or relationships between discrete variables. These studies have identified female gender (González‐Sanguino et al., 2020; Mazza et al., 2020; Özdin & Bayrak Özdin, 2020; Wang et al., 2020), younger age (Elbay et al., 2020; González‐Sanguino et al., 2020; Huang & Zhao, 2020), pre‐existing mental health conditions (Asmundson et al., 2020; González‐Sanguino et al., 2020; French et al., 2020; Özdin & Bayrak Özdin, 2020; Usher et al., 2020), poorer physical health (Zhou et al., 2020; Wang et al., 2020), financial instability (Sinawi et al., 2021), financial loss due to COVID‐19 (Hyland et al., 2020), and social isolation or loneliness (Asmundson et al., 2020; Brooks et al., 2020; González‐Sanguino et al., 2020; Liu, Zhang, et al., 2020) as risk factors for COVID‐related distress. Research on the influence of psychological resources has identified an array of psychosocial risk factors of psychological distress during the pandemic, including high fear and exaggerated beliefs about the dangerousness of COVID (Taylor et al., 2020; Zacher & Rudolph, 2020), maladaptive coping strategies including denial, self‐blame, and substance use (Rettie & Daniels, 2020), intolerance of uncertainty (Glowacz & Schmits, 2020; Rettie & Daniels, 2020), low openness to experience (Kroska et al., 2020), avoidant coping (Dawson & Golijani‐Moghaddam, 2020; Mariani et al., 2020), hopelessness (Shanahan et al., 2020), and high levels of rumination (Zhou et al., 2020). Additionally, studies examining predictors of healthy COVID‐19 adaptation have shown distress tolerance (Liu, Zhang, et al., 2020), social support (Liu, Zhang et al., 2020; Ye et al., 2020), positive individual well‐being in domain‐specific functioning (Kimhi et al., 2020), positive reappraisal/reframing (Shanahan et al., 2020; Zacher & Rudolph, 2020), religiosity (Marzo et al., 2020; Thomas & Barbato, 2020), mindfulness (Conversano et al., 2020; Wielgus et al., 2020). and psychological flexibility (Arslan et al., 2020; Dawson & Golijani‐Moghaddam, 2020; McCracken et al., 2021; Pakenham et al., 2020) to be significant predictors. However, despite the influx of new research concerning predictors of distress, many gaps remain. Extant studies have primarily relied on correlations and/or univariate and multivariate regression techniques that assume linearity between variables to predict outcomes, and often only examine a small number of variables in a single model. Furthermore, while many of these studies provide a theoretical rationale for their primary predictor of interest, they lack an overarching framework through which to unify constructs and describe how variables examined in concert are likely to influence each other.
Research modeling psychological responses and predictors of adaptation is critical to understanding the mental health ramifications of a global pandemic and developing resilience‐building interventions. Machine learning (ML) is a dynamic, robust statistical approach that allows for the identification of complex (i.e., nonlinear) relationships and interactions between a large number of predictors that lead to a given outcome. Although ML is often used in an exploratory and atheoretical manner, using theory and prior research on stress, coping, and trauma adaptation to guide variable selection serves to reduce Type I error and spurious findings and increase generalizability (Elhai & Montag, 2020). A handful of COVID‐19 mental health studies have adopted an ML approach. In an international sample assessing predictors of specific mental health outcomes (anxiety, depression, and PTSD), somatization and emotion regulation were robust predictors of all outcomes (Prout et al., 2020). In a sample of Chinese adults, stress and rumination were strong predictors of COVID‐related anxiety, whereas demographic variables like sex and age were not predictive. An ML study examining Korean immigrants residing in the United States found that lower psychological distress related to COVID‐19 was most strongly predicted by resilience (Choi et al., 2020). As resilience is often conceptualized as lack of distress, this finding is unsurprising and a finer‐tuned understanding of what aspects of resilience assist individuals during a pandemic is needed. A unique finding from the Choi et al. study involved the experience and perception of racial discrimination toward Asians specifically related to COVID‐19 as a significant predictor of distress. While their results present an innovative approach to examining distinctive predictors among Asian immigrants during a global pandemic, findings are limited in their inability to generalize and confer implications for the broader general population.
An ML approach allows for the examination of demographic, environmental, and psychosocial factors concurrently as potential predictors of COVID‐related distress and adaptation. Theories on stress, coping, and trauma adaptation as well as prior research documenting risk and protective factors frequently associated with PTEs drove our variable selection decisions. These theories emphasize the dynamic interplay between socio‐contextual factors and person‐centered variables in human capacity for adaptation (Benight & Bandura, 2004; Bonanno, 2005; Lazarus & Folkman, 1984). Socio‐contextual factors include the demands of the stressor and available external resources, which vary depending on the person's degree of exposure, risk, and impact from COVID‐19.
In assessing environmental demands, we examined variables related to the COVID‐19 experience itself, including those associated with increased risk of exposure and mortality as well as PTEs including being diagnosed with COVID‐19 or having a loved one diagnosed with or die from COVID‐19. Pandemic response is also associated with availability and loss of resources. Similar in some ways to a natural disaster, in which resource losses like the loss of shelter are salient predictors of poorer adjustment (Hobfoll & Lilly, 1993), COVID‐19 may involve loss of income or social support for some. We examined four primary types of resources based on Hobfoll's (1989) conservation of resources (COR) theory of trauma adaptation: (1) material resources (e.g., income and income loss); (2) energy resources (e.g., availability of health insurance and food assistance); (3) interpersonal resources (availability of social support); and (4) work resources (employment).
Person‐centered variables in adaptation to trauma include coping strategies, styles, and appraisals (e.g., Benight & Bandura, 2004; Bonanno & Mancini, 2008; Carver et al., 1989). Individual differences across these domains of person‐centered functioning are differentially predictive of resilient adaptation to stress and trauma, with certain responses conferring adaptive or maladaptive value specific to context, while other styles and strategies are more broadly adaptive (Mancini & Bonanno, 2009). Prominent trauma theories place importance on trauma‐focused coping, emphasizing effortful focus and processing of the thoughts, images, and worries surrounding the traumatic event (e.g., Ehlers & Clark, 2003; Foa & Rothbaum, 1998). However, others have argued that types of forward‐focused coping, namely avoidance, distraction, and minimization, have their place in coping scenarios (Bonanno et al., 2011). Forward‐focused coping, which refers to the ability to distract oneself from the traumatic event, generate positive thoughts, and sublimate distressing feelings, may foster adjustment to trauma as it helps people maintain focus on goals and plans (Carver & Scheier, 2001). Typically, the flexible use of both styles, assessed with the Perceived Ability to Cope Scale (PACT, Bonanno et al., 2011) is most adaptive (Galatzer‐Levy et al., 2012). However, thus far, to our knowledge only one study has investigated the efficacy of each coping style during the COVID‐19 pandemic via the PACT, and found forward‐focused coping to be predictive of lower levels of depression across three time points, while trauma‐focused coping was predictive of higher levels of depression at time point 1, suggesting that effortful processing of the pandemic during its most novel stage may be overwhelming (Zhou et al., 2020). As this finding conflicts with a preponderance of trauma research asserting the adaptive use of both trauma‐focused and forward‐focused coping following a past trauma (e.g., Galatzer‐Levy et al., 2012; Knowles & O'Connor, 2015; Pinciotti et al., 2017; Rodin et al., 2017), more research is needed to understand their roles during COVID‐19. As the pandemic is an ongoing stressor, it may necessitate the implementation of styles unique from those utilized to cope with a past traumatic event. In addition to trauma‐related coping styles, in recognition that some pragmatic coping strategies may involve behaviors that are maladaptive or ineffective (Bonanno, 2005), we also assessed coping strategies associated with poorer adaptation (e.g., avoiding through substance use) and a strategy with mixed findings regarding its role in adaptation (turning to religion).
Social cognitive theory (SCT) emphasizes the importance of self‐appraisals in the stress response (Benight & Bandura, 2004). In coping with trauma specifically, trauma coping self‐efficacy (CSE‐T; Benight & Cieslak, 2011), defined as one's perceived ability to manage the challenges of a traumatic event, distress‐related symptoms, and recovery, is one of the strongest predictors of trauma adaptation (for a review, see Luszczynska et al., 2009). Self‐efficacy varies and changes according to the task at hand as well as changes in environmental conditions (Benight & Cieslak, 2011). For example, a person may have positive self‐efficacy beliefs around coping with some specific demands but not others. As such, SCT theorists emphasize the importance of measuring coping self‐efficacy specific to the traumatic event or stressor, in this case, one's self‐efficacy to cope with an ongoing pandemic. Several studies have examined self‐efficacy during COVID‐19, and found it to be a significant predictor of positive mental health outcomes (Hou et al., 2020; Shahrour & Dardas, 2020; Vagni et al., 2020; Wang et al., 2020; Xiong et al., 2020; Yıldırım & Güler, 2020). However, most have utilized general measures of self‐efficacy rather than coping self‐efficacy to a trauma, and more specifically to a pandemic. Additionally, almost all have been conducted in populations of healthcare workers. To date, no studies have assessed a person's self‐efficacy in his or her ability to cope with the challenges of COVID‐19 and evaluate its protective value against psychological distress.
Similar to yet distinct from coping self‐efficacy (CSE) is the construct of hope, which often serves as a protective factor in the face of adversity (Valle et al., 2006). Whereas CSE is an appraisal about the self, hope is often conceptualized as an appraisal or outlook about the world and the likelihood of good things happening (Magaletta & Oliver, 1999). During such an unprecedented and prolonged period of stress for many, having the capacity to maintain a hopeful outlook may be instrumental in predicting psychological well‐being.
Finally, in addition to assessing socio‐contextual and person‐centered psychosocial factors, understanding mental health response to COVID‐19 should take into account the impact of notable demographic factors (age, gender, employment, income, and education) and history variables (prior trauma exposure, mental health history) that have been documented in prior research on adaptation to PTEs, including COVID‐19 and severe acute respiratory syndrome (SARS; Bonanno, 2005; Bonanno et al., 2007, 2008; Elbay et al., 2020; Liu, Stevens, et al., 2020; Ozer et al., 2003; Wu et al., 2005).
A call to action by Holmes et al. (2020) identified immediate COVID‐19 mental health research priorities: to document rates of anxiety, depression, and other mental health issues across both the general population and vulnerable groups and to determine risk and resilience factors associated with mental health response. The present study addresses these research priorities. Expanding upon early COVID‐19 research that has primarily reported on mental health prevalence rates and used regression analyses to model discrete sets of predictors, we used ML to identify predictors of mental health outcomes (depression, PTSD, anxiety, and somatic symptoms). We chose to examine somatic symptoms as an additional, important outcome variable as some individuals manifest psychological distress through a broad set of somatic symptoms, which might be associated with a unique set of predictors. Although ML is often used in an exploratory and atheoretical manner, we based selection on prior research and resilience theories, therefore limiting the number of variables tested. Following coping theories that emphasize the interplay between person‐centered variables and environmental demands and resources, we assessed the relative importance of variables associated with demands and impacts of COVID‐19 (variables associated with increased risk of exposure and mortality and PTEs including being diagnosed with COVID‐19 or having a loved one diagnosed with or die from COVID‐19); resources (e.g., SES, social support, access to health care); and coping appraisals, styles, and strategies. We drew from the traumatic stress literature to examine specific coping constructs found to be highly predictive of resilience in trauma survivors: coping self‐efficacy and trauma‐focused and forward‐focused coping. In contrast to prior COVID‐19 research efforts, trauma‐focused measures were specifically targeted with symptoms and coping to the pandemic rather than more broadly. Based on the substantial literature identifying CSE as a prominent predictor of trauma adaptation, we hypothesized that CSE‐T would be more highly associated with COVID‐19 adaptation than other coping variables and that person‐centered variables would emerge as more powerful predictors than environmental variables.
2. METHODS
2.1. Participants
We created an online baseline survey on Qualtrics and shorter follow‐up surveys to be administered monthly for a year. This paper reports the cross‐sectional data from the baseline survey of American participants (N = 467 completers). The survey was administered via social media over a 12‐week period from May 1 to July 29, 2020. Inclusion criteria required participants to be over the age of 18 and able to read and comprehend English. Study procedures were approved by the University of Colorado—Colorado Springs Institutional Review Board.
2.2. Measures
2.2.1. Demographic variables
Demographic information collected included age, gender, ethnicity, race, education, occupation, income, marital status, household size, food assistance, and health insurance. Socioeconomic status (SES) was determined using Index 3 of the National Crime Victimization Survey (NCVS; Berzofsky et al., 2014). This index calculates SES using household income (percent above or below the US poverty line based on household size), individual education level, and employment status.
2.2.2. Medical risk variables
We collected self‐reported history of medical conditions, including conditions associated with risk of COVID‐19 mortality. These conditions were grouped as: (1) heart‐related conditions (angina, congestive heart failure, high blood pressure, heart attack history), (2) lung‐related conditions (COPD, emphysema, moderate or severe asthma, and current or past smoking), (3) immune deficiencies and factors related to immunocompromised health (Type 1 and 2 diabetes, lupus, rheumatoid arthritis, cystic fibrosis, multiple sclerosis, cancer, bone marrow transplant, and chronic treatment with corticosteroids), and (4) severe obesity.
2.2.3. Mental health history
Self‐reported history of mental health conditions was collected and grouped into four categories for descriptive purposes: (1) depressive disorders, (2) anxiety disorders, (3) PTSD, and (4) all other mental health disorders. Participants were asked, “Have you been previously diagnosed with a psychiatric disorder? Click all that apply” and all DSM‐5 disorders were included. Previous trauma history was assessed with the Brief Trauma Questionnaire (BTQ; Schnurr et al., 1999).
2.2.4. COVID‐19 risk and exposure
Questions that assessed exposure to COVID‐19 included: (1) diagnosis of COVID‐19, (2) experiencing symptoms of COVID‐19 (e.g., fever, respiratory problems), (3) suspected COVID‐19 without confirmed diagnosis, (4) direct exposure to someone with diagnosed COVID‐19, and (5) direct exposure to someone with suspected COVID‐19. Two questions from the Pandemic Stress Index (Harkness et al., 2020) assessed engagement in remote work and social distancing.
2.2.5. COVID‐19 impact measures
The COVID Impacts Questionnaire—Shortened Version (Conway et al., 2020), financial status subscale, is a 2‐item scale that assesses personal financial impact of COVID‐19 on a scale of 0 (no impact) to 2 (high impact). Cronbach's α was α = 0.76. Three items assessed COVID‐related events that would potentially fulfill Criterion A of the DSM‐5 diagnosis of PTSD and were summed. These items, labeled “COVID experiences” involved (a) a loved one's diagnosis of COVID‐19, (b) a loved one's death from COVID‐19, and (c) personal diagnosis of COVID‐19.
2.2.6. Psychological measures: Resilience and risk factors
The two subscales of the Perceived Ability to Cope with Trauma Scale (PACT; Bonanno et al., 2011) assessed forward‐focused coping (α = 0.91) and trauma‐focused coping (α = 0.80) to COVID‐19. We administered two subscales of the Brief COPE Scale (Carver, 1997), a widely used measure of effective and ineffective coping skills. Asking specifically about coping strategies used during the pandemic in the past month, the subscales assessed turning to religion (α = 0.83) and substance use (α = 0.91) as means of coping. The Perceived Hope Scale (α = 0.94) is a brief and broad measure of “how people perceive hope in everyday life” (Krafft et al., 2019, p. 4) in a manner that distinguishes the construct from self‐efficacy and optimism. The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., 1988) is a measure of subjectively assessed social support. We administered four items related broadly to any “special person” in the participant's life that is relied upon for support (α = 0.97).
The 5‐item Pandemic Self‐Efficacy Scale was developed to assess participants' perceived capability to successfully cope with COVID‐19 specific stressors (e.g., “manage distressing dreams or images about the pandemic”). It was based on the well‐established Trauma Coping Self‐Efficacy Scale (CSE‐T; Benight et al., 2015) with participant ratings ranging from 1 (I'm not capable at all) to 7 (I'm totally capable) and summed. Cronbach's α for this sample was 0.85.
2.2.7. Mental health symptoms and functioning
Self‐reports of symptoms and functioning included the Patient Health Questionnaire (PHQ‐9; Kroenke et al., 2001) to measure depression (α = 0.90), the Generalized Anxiety Disorder—7 (GAD‐7; Spitzer et al., 2006) to measure anxiety (α = 0.93), the Somatic Symptom Scale (SSS‐8; Gierk et al., 2014) to measure somatic symptom burden (α = 0.83), and the PTSD Checklist for DSM‐5 (PCL‐5; Weathers et al., 2013) to measure symptoms of PTSD (α = 0.92). For the PCL‐5, we directed participants to respond to questions referencing the COVID‐19 pandemic as the index trauma.
2.3. Analysis
Descriptive statistics were calculated for the whole sample. To identify the most salient predictors of mental health outcomes (depression, PTSD, anxiety, and somatic symptoms), we employed four well‐established supervised ML algorithms: the ensemble methods Random Forest (RF) and eXtreme Gradient Boosting (XGBoost), a Support Vector Machine with Radial Basis Function Kernel (SVM‐RBF), and an Elastic Net regularized regression. The RF and XGBoost implement decision trees to predict an outcome; both approaches iteratively build stronger predictive algorithms from weaker algorithms that are derived from random subsets of the data and random subsets of predictor variables. The SVM‐RBF examines relationships between predictor variables and an outcome in three‐dimensional space, while the Elastic Net is an algorithm that imposes a “shrinkage” term on a linear regression that emphasizes out‐of‐sample predictions and allows for multicollinearity between predictors. All ML algorithms were trained to optimize model . The data were randomly split into a training (75%) and hold‐out sample (25%); repeated k‐fold cross‐validation was applied to the training data, with five repeats of 10‐fold cross‐validation (i.e., data was trained using 50 resamples of the data). Each fold tested 20 different combinations of algorithm hyperparameters. A random‐number seed was set before each analysis to ensure consistent replication. Models were evaluated based on their performance in the hold‐out sample based on the optimized hyperparameters identified in the training sample. Code for the ML models can be found at https://bit.ly/3so30bJ. Comparison of model performance was evaluated by bootstrapping the hold‐out sample , with 5000 replications of the data using the bias‐corrected and accelerated method (BCa). Models were considered to be significantly different from one another if there was no overlap in the 95% BCa confidence intervals. Missing data among predictors were imputed before all ML analyses using RF imputation, which has been shown to outperform other types of imputation commonly used in ML (Waljee et al., 2013). The RF imputation used 1000 trees and k = 5 nearest neighbors with one imputation. The same imputed data set was used across all ML analyses.
The RF imputation and ML algorithms were conducted in R (R Core Team, 2017) using the “missRanger” (Mayer, 2019) and “caret” (Kuhn, 2008; with all dependencies) packages. All other analyses were in IBM SPSS Statistics (version 26).
3. RESULTS
A total of 621 participants started the survey and 467 completed the demographic questionnaire and other measures and were included in analyses. Among the 467 participants, 351 (75%) had complete data. Data were assumed to be missing at random, as there were no evident patterns of missing data (all patterns of missingness among predictor and outcome variables were <5%), which suggests that estimates of imputed variables were relatively unbiased.
3.1. Descriptive statistics: Demographic, background, health disparities, and COVID‐specific variables
Descriptive characteristics of the sample can be found in Table 1. There was a range of education levels, but the majority (62.5%) held a bachelor's degree or higher. Age ranged from 18 to 85, with a mean age of 33.14 years (SD = 12.96), and 63.6% were female. Of note, 4.9% of the sample identified as transgender or nonbinary. The sample was racially and ethnically diverse with the majority being White and non‐Hispanic (65.8%). To address possible health disparities related to race and ethnicity for the ML algorithms, we created a binary variable based on race/ethnicities documented to be at higher risk for COVID‐19 infection and mortality (Bibbins‐Domingo, 2020). The two groups consisted of (a) White/non‐Hispanic and Asian (83.1%) and (b) Black, Latinx, Native American, Pacific Islander, and biracial (16.9%). Sample SES varied widely but skewed in the higher NCVS categories. Resources variables included unemployment (15.4%), lack of health insurance (4.1%), and receiving food assistance (8.4%). Finally, mental health history, trauma exposure history, and prior medical diagnoses are also included in Table 1.
Table 1.
Participant descriptives
| Variable | M (SD) or % (N = 467) |
|---|---|
| Demographics | |
| Age (years) | 33.14 (12.95) |
| Gender identity | |
| Female | 63.6 |
| Male | 31.5 |
| Gender non‐conforming | 4.9 |
| Race/ethnicitya | |
| White/Asian | 83.1 |
| Black, Latinx, Pacific | 16.9 |
| Islander, Native American | |
| Highest education level | |
| Less than high school | 1.5 |
| High school graduate | 4.9 |
| Partial college | 20.8 |
| 2‐year college or | 10.3 |
| specialized training | |
| 4‐year college | 34.0 |
| Master's degree | 19.1 |
| Doctoral degree | 9.4 |
| Income ($) | |
| <10k | 6.6 |
| 10k–50k | 25.3 |
| 50k–75k | 18.0 |
| 75k–100k | 12.8 |
| 100k–125k | 10.7 |
| 125k–150k | 7.3 |
| 150k–175k | 2.6 |
| 175k–200k | 2.8 |
| >200k | 7.3 |
| Sexual orientation | |
| Straight | 72.2 |
| Gay/Lesbian | 6.9 |
| Bisexual | 15.6 |
| Other | 5.4 |
| Marital status | |
| Single, never married | 43.7 |
| Married | 45.8 |
| Other | 10.3 |
| Married | 45.8 |
| Religion | |
| Judaism | 3.9 |
| Islam | 1.3 |
| Christianity | 38.1 |
| Hinduism | 0.9 |
| Buddhism | 1.3 |
| Nonreligious | 49.7 |
| Other | 3.6 |
| Religious | 49.0 |
| Medical risk variables | |
| Heart‐related conditions | 16.3 |
| Lung‐related conditionsb | 43.7 |
| Immunocompromised | 15.8 |
| Severe Obesity | 4.9 |
| Mental health history | |
| Trauma exposure history | 64.9 |
| BTQ total trauma exposure | 2.02 (1.96) |
| Depression history | 27.4 |
| Anxiety history | 29.3 |
| PTSD history | 11.3 |
| Other MH history | 31.7 |
| Any mental health diagnosis | 46.9 |
| COVID risk | |
| Thought had COVIDc | 25.3 |
| COVID exposedd | 9.0 |
| Working from homee | 51.8 |
| Social distancingf | 94.6 |
| Resources | |
| Employment status | |
| Employed full time | 50.7 |
| Employed part time | 13.1 |
| Out of work | 15.4 |
| Retired | 3.9 |
| Student | 16.9 |
| Employed | 63.8 |
| SES: NCVS3 total | |
| 0 | 0.4 |
| 1 | 4.7 |
| 2 | 7.5 |
| 3 | 13.9 |
| 4 | 14.8 |
| 5 | 16.9 |
| 6 | 19.1 |
| 7 | 15.6 |
| Any health insurance | 95.9 |
| Receive food assistance | 8.4 |
| Resilience factors/predictors | |
| Perceived Hope Scale | 24.30 (6.90) |
| PACT Forward‐Focused | 58.15 (12.65) |
| PACT Trauma‐Focused | 39.49 (8.18) |
| Brief COPE Substances subscale | 3.52 (1.88) |
| Brief COPE Religion subscale | 3.75 (1.94) |
| Social supportg | 21.61 (6.83) |
| Pandemic Coping Self‐Efficacy Scale | 24.18 (6.35) |
| COVID‐19 Experiences and Impacts | |
| COVID financial impactsh | 0.95 (0.90) |
| Loved one diagnosed with COVID‐19 | 23.1 |
| Loved one who died due to COVID‐19 | 6.4 |
| Diagnosed with COVID‐19 | 1.7 |
| COVID‐19 cumulative traumai | 0.57 (0.76) |
Abbreviations: MH, mental health; NCVS, National Crime Victimization Survey Index 3 socioeconomic status; PACT, Perceived Ability to Cope with Trauma scale; PTSD, posttraumatic stress disorder; BTQ, Brief Trauma Questionnaire.
Lower risk: White, Asian; Higher Risk: Black, Latino/a, Pacific Islander, Native American.
Includes current or former smokers.
Have
Have you been directly exposed to someone who has a confirmed COVID‐19 diagnosis?"
During COVID‐19, are you working from home?"
During COVID‐19, are you practicing social distancing?"
Multidimensional Scale of Perceived Social Support—Special Person.
COVID Impacts Questionnaire—Financial Impacts Subscale (2 item) Total.
Sum of three COVID‐related events that would potentially fulfill Criterion A of the DSM‐5 diagnosis of PTSD (knowing a loved one who had been diagnosed with COVID‐19, having a loved one die from COVID‐19, and being personally diagnosed with COVID‐19).
Table 1 provides information on COVID‐related demands, labeled “experiences” (probable Criterion A events) and “impacts.” Many participants (57.2%) reported negative financial impacts of COVID‐19, such as loss of job‐related income. Approximately 23% of participants reported having a loved one who was diagnosed with COVID‐19, 6.4% endorsed having a loved one who died due to COVID‐19, 25% thought they had COVID‐19 but did not have a confirmed diagnosis, and 1.7% had received a diagnosis of COVID‐19.
3.2. Mental health outcomes
Mental health outcomes, presented in Table 2, include the PHQ‐9, the GAD‐7, the PCL‐5 (addressing COVID‐19 specifically), and somatization. On the PHQ‐9, 44.1% of participants endorsed scores ≥10, indicating probable clinical depression (Manea et al., 2012). On the GAD‐7, 36.2% had a score >10, indicative of probable clinical anxiety (Spitzer et al., 2006). On the PCL‐5, 22.5% of the sample had a score ≥31, which is indicative of probable PTSD (Bovin et al., 2016). On the SSS‐8, the mean score was 9.60 (SD = 6.36); well above the normative mean population score of 3.23 (Gierk et al., 2014). The four mental health outcomes were highly associated with one another (PHQ‐9 and GAD‐7: r = 0.77, PHQ‐9 and PCL‐5: r = 0.71, PHQ‐9 and SSS‐8: r = 0.71, GAD‐7 and PCL‐5: r = 0.69, GAD‐7 and SSS‐8: r = 0.65, PCL‐5 and SSS‐8: r = 0.62) but we chose to examine each outcome separately in ML models to determine if specific predictors convey risk differently for different outcomes.
Table 2.
Mental Health Outcomes
| Variable | M (SD) or %N = 467 |
|---|---|
| PHQ‐9 total | 9.90 (6.48) |
| Probable depression (PHQ‐9 total > 10.00) | 44.1% |
| GAD‐7 total | 8.09 (5.67) |
| Probable anxiety (GAD‐7 total > 10.00) | 36.2% |
| COVID PCL‐5 total | 19.93 (14.95) |
| Probable PTSD (PCL total > 31.00) | 22.5% |
| Somatization: SSS‐8 total | 9.60 (6.36) |
Abbreviations. GAD‐7, General anxiety disorder‐ 7; PCL, PTSD checklist for DSM‐5; PHQ‐9, Patient health questionnaire; SSS‐8, Somatic symptom scale.
3.3. Bivariate relationships with mental health outcomes
Table 3, 4 presents a series of Pearson's and Point‐Biserial correlations that were first conducted to examine bivariate relationships between distinct mental health outcomes and all predictors (demographic, health disparities, COVID‐specific variables, and psychological factors). Higher levels of coping self‐efficacy, forward‐focused coping, and perceived hope were highly negatively associated (r's ranging from −0.39 to −0.65) with all four mental health outcomes (depression, anxiety, PTSD, and somatic symptoms). Smaller associations were seen between demographic variables (r's < 0.20), COVID risk variables (r's < 0.16), resources (r's < 0.26), and COVID‐19 impacts (r's < 0.20) and mental health outcomes. Some minor differences between patterns of relationships emerged between each of the mental health outcomes. History of medical conditions and higher risk of COVID mortality was associated with depression and somatic symptoms, but not anxiety or PTSD. Moderate associations were observed between previous mental health disorder diagnoses and mental health outcomes.
Table 3.
Bivariate relationships between predictors and mental health outcomes
| Variable | PHQ‐9 | GAD‐7 | PCL‐COVID | SSS‐8 |
|---|---|---|---|---|
| Demographics | ||||
| Age | −0.135** | −0.150** | −0.111* | −0.060 |
| Male | −0.137** | −0.196*** | 0.000 | −0.154*** |
| Gender non‐conforming | 0.202*** | 0.198*** | 0.172*** | 0.169*** |
| White/Asian | −0.040 | −0.021 | −0.147** | −0.081 |
| Married | −0.117* | −0.087 | −0.063 | −0.013 |
| Religious | 0.012 | 0.041 | 0.137** | 0.020 |
| Medical risk variables | ||||
| Heart‐related conditions | 0.101* | 0.041 | 0.044 | 0.147** |
| Lung‐related conditions | 0.152** | 0.080 | 0.092 | 0.167*** |
| Immunocompromised | 0.102* | 0.064 | 0.073 | 0.119* |
| Obesity | 0.167*** | 0.099* | 0.102* | 0.065 |
| Mental health variables | ||||
| BTQ total trauma exposure | 0.195*** | 0.159** | 0.195*** | 0.263*** |
| Anxiety disorder (self‐reported) | 0.352*** | 0.342*** | 0.187*** | 0.334*** |
| Depressive disorder (self‐reported) | 0.367*** | 0.284*** | 0.154** | 0.266*** |
| PTSD diagnosis (self‐reported) | 0.241*** | 0.239*** | 0.211*** | 0.219*** |
| Other mental health diagnosis (self‐reported) | 0.370*** | 0.328*** | 0.197*** | 0.328*** |
| COVID risk | ||||
| Thought had COVID | 0.141** | 0.072 | 0.078 | 0.157*** |
| COVID exposed | −0.071 | −0.111* | −0.117 | −0.092* |
| Working from home | −0.143** | −0.018 | 0.105* | −0.066 |
| Social distancing | −0.053 | 0.019 | −0.055 | −0.021 |
| Resources | ||||
| Employed | −0.196*** | −0.081 | −0.082 | −0.068 |
| Socioeconomic status (NCVS3) | −0.259*** | −0.110* | −0.129** | −0.129** |
| Any health insurance | 0.043 | 0.095* | 0.086 | −0.129** |
| Receive food assistance | 0.172*** | 0.078 | 0.149** | −0.000 |
| Resilience factors/predictors | ||||
| Perceived Hope Scale | −0.528*** | −0.390*** | −0.368*** | −0.362*** |
| PACT Forward‐Focused | −0.569*** | −0.467*** | −0.546*** | −0.393*** |
| PACT Trauma‐Focused | −0.248*** | −0.169*** | −0.252*** | −0.168*** |
| Brief COPE Substances subscale | 0.299*** | 0.259*** | 0.275*** | 0.241*** |
| COPE Religion subscale | 0.046 | 0.072 | 0.195*** | 0.053 |
| Social support | −0.136** | −0.056 | −0.155** | −0.052 |
| Pandemic Coping Self‐Efficacy Scale | −0.651*** | −0.600*** | −0.619*** | −0.475*** |
| COVID‐19 Experiences and Impacts | ||||
| COVID financial impacts | 0.151** | 0.116* | 0.190*** | 0.141** |
| COVID cumulative trauma | 0.136** | 0.093* | 0.195*** | 0.159*** |
Note: For continuous variables, Pearson's correlations were used; for binary variables, point‐biserial correlations were used.
p < 0.05
p < 0.01
p < 0.001.
Table 4.
Out‐of‐sample performance for all machine learning algorithms
| PHQ‐9 | GAD‐7 | PCL‐COVID | SSS‐8 | |
|---|---|---|---|---|
| Model | R 2 (95% BCa CIa) | R 2 (95% BCa CIa) | R 2 (95% BCa CIa) | R 2 (95% BCa CIa) |
| Random Forest | 0.526 (0.406, 0.634) | 0.376 (0.243, 0.512) | 0.322 (0.149, 0.480) | 0.309 (0.176, 0.430) |
| XGBoost | 0.501 (0.375, 0.615) | 0.353 (0.215, 0.489) | 0.313 (0.121, 0.475) | 0.298 (0.174, 0.415) |
| SVM‐RBF | 0.550 (0.408, 0.663) | 0.354 (0.229, 0.484) | 0.278 (0.116, 0.432) | 0.293 (0.154, 0.420) |
| Elastic Net | 0.537 (0.411, 0.650) | 0.402 (0.270, 0.529) | 0.336 (0.140, 0.498) | 0.298 (0.164, 0.426) |
Abbreviations: BCa CI, Bias‐Corrected and Accelerated bootstrapped Confidence Intervals; SVM‐RBF, Support Vector Machine with Radial Basis Function; XGBoost, eXtreme Gradient Boosting.
Based on 5000 bootstrapped replications of the out‐of‐sample model R 2.
3.4. Predictors of mental health outcomes
Four ML models assessed for each mental health outcome (depression, PTSD, anxiety, and somatic symptoms) were conducted, allowing for examination of each predictor while accounting for the predictive value of all other predictors simultaneously. All four supervised ML algorithms had good out‐of‐sample performance (all out‐of‐sample ≥ 0.503 for PHQ‐9, ≥ 0.389 for GAD‐7, ≥ 0.274 for PCL‐COVID, and ≥ 0.303 for SSS‐8). There were no differences between algorithms in predicting mental health outcomes based on BCa 95% Confidence Intervals (see Table 2). Variable importance was evaluated by RF, as it allows nonlinear relationships between the predictor variables and dependent variables and has a well‐established test of statistical significance for predictors through the bias‐correcting permutation importance (PIMP) algorithm. The PIMP algorithm examines the importance for every predictor variable assuming a “null importance” for each variable, here with 100 permutations of the outcome variable (Altmann et al., 2010). Because there were four outcome variables, statistical significance for predictors was evaluated at a conservative p < 0.05/4 = 0.0125. The relationship between significant predictors and each of the mental health outcomes were then examined through partial dependence plots (PDPs).
Variable importance plots can be found in Figures 1, 2, 3, 4. PDPs for significant predictors can be found in Figures 5, 6, 7, 8. Results were largely similar for the depression and anxiety models (i.e., the same variables emerged as significant predictors across models) with a few notable differences for the somatic symptom and PTSD models. The strongest predictor across all outcomes was pandemic CSE; individuals with lower levels of CSE reported higher PTSD, depression, anxiety, and somatic symptoms. Other significant predictors included forward‐focused coping (individuals with lower levels of forward‐focused coping reported higher for PTSD, anxiety, and depression), perceived hope (individuals with lower levels of hope reported higher anxiety and depression), coping through substance use (individuals who reported coping by using substances reported higher anxiety and depression). Notably, with the exception of pandemic CSE, coping variables did not predict somatic symptoms as they had for depression, anxiety, and PTSD.
Figure 1.
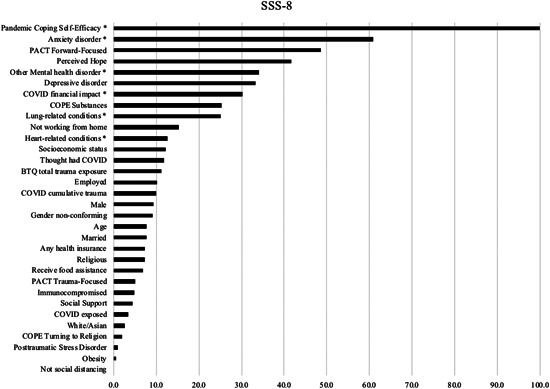
Variable importance in predicting somatic symptoms
Figure 2.
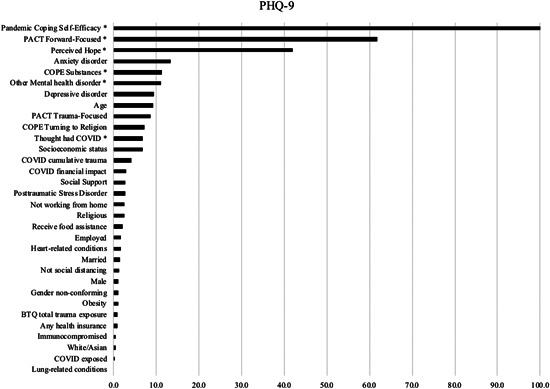
Variable importance in predicting depression symptoms
Figure 3.
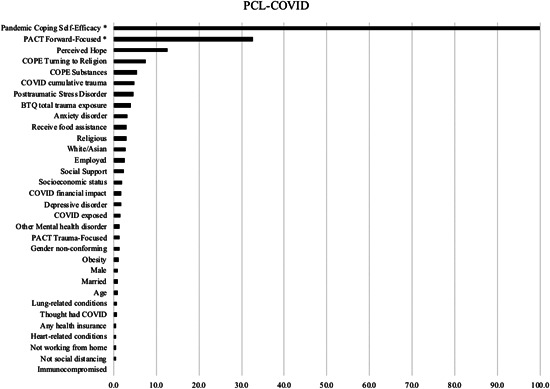
Variable importance in predicting posttraumatic stress disorder symptoms
Figure 4.
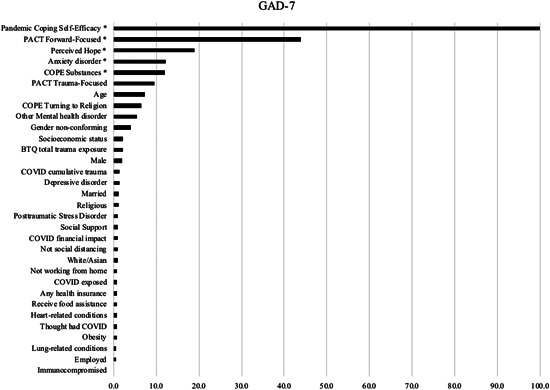
Variable importance in predicting anxiety symptoms
Figure 5.
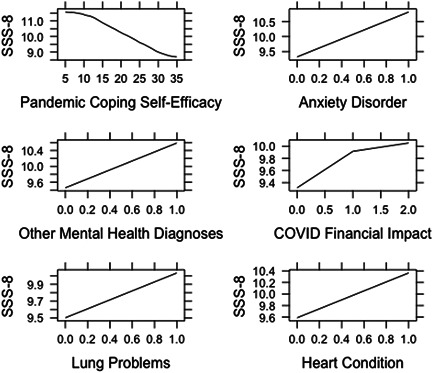
Relationships between significant predictors and somatic symptoms
Figure 6.
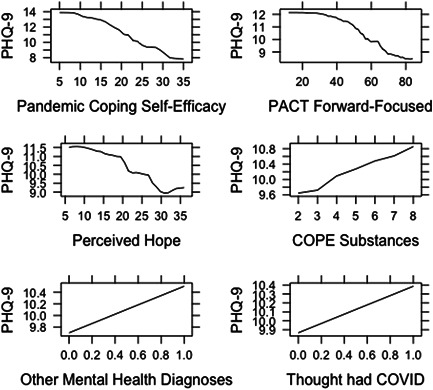
Relationships between significant predictors and depression symptoms
Figure 7.
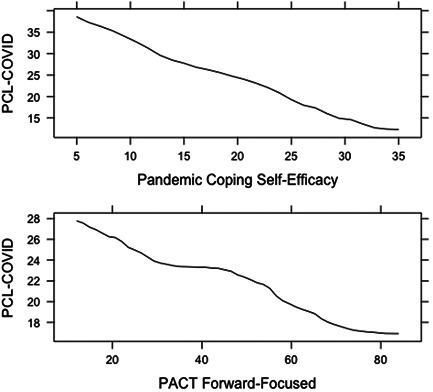
Relationships between significant predictors and PTSD symptoms
Figure 8.
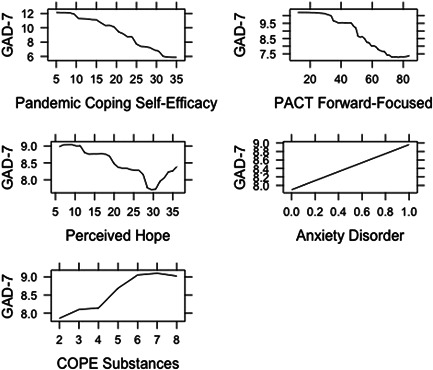
Relationships between significant predictors and anxiety symptoms
Reporting a prior mental health diagnosis was predictive of mental health outcomes, although different diagnoses predicted different outcomes. Individuals with a history of an anxiety diagnosis reported higher anxiety and somatic symptoms; individuals with a history of an “other” psychiatric diagnosis reported higher depression and somatic symptoms.
Only a few demographic, resource‐related, and COVID‐related variables emerged as statistically significant predictors of mental health outcomes. Thinking one had COVID‐19 (but not actually receiving the diagnosis) was associated with higher levels of depression symptoms. Report of negative financial impacts due to COVID‐19 was associated with higher levels of somatic symptoms. For PTSD, no demographic, history, resources, or risk variables emerged as predictors; only pandemic CSE and forward focused‐coping were predictive.
Because mental health variables were highly associated with one another, we conducted a sensitivity analysis with an empirically‐derived composite score of “psychological distress” using the aforementioned mental health variables. Results from these analyses were consistent with individual mental health variables, as person‐centered variables rather than demographic or external resources were most predictive of psychological distress. Additional details can be found in the Supporting Information.
4. DISCUSSION
In a sample of 467 adults, we administered a comprehensive online survey with the aims of identifying mental health outcomes and their prevalence rates and modeling risk and resilience predictors of adaptation or distress during the COVID‐19 pandemic. Similar to prior studies documenting probable mental health disorder prevalence rates (e.g., Xiong et al., 2020), we observed rates of probable depression (44.1%), anxiety (36.2%), and PTSD (22.5%) that are much higher than typical population rates (e.g., 2%–7%; American Psychiatric Association DSM‐5 Task Force, 2013). Additionally, participants reported significant levels of somatic symptom burden, with the group mean falling in the moderately severe range (Gierk et al., 2014). Notably and in contrast to prior studies, we assessed PTSD symptoms specifically to COVID‐19 rather than broadly assessing symptoms to any trauma. The prevalence of self‐reported PTSD specifically to COVID‐19 is noteworthy, and suggests that the pandemic, although not a past trauma that induces distressing memories, serves for many as a continuous trauma that may induce distressing intrusive thoughts of future harm.
Supervised ML models revealed that the primary predictors of adaptation to COVID‐19 are person‐centered variables rather than COVID‐related demands and resources, with pandemic coping self‐efficacy being the strongest predictor by far across mental health outcomes. Prior mental health history was also a significant predictor across models. Surprisingly, when accounting for psychosocial factors, few demographic, environmental, and resource variables emerged as significant predictors of mental health outcomes. Report of suspected (but not confirmed) COVID‐19 diagnosis was associated with depression and somatic symptoms; negative COVID‐related financial impacts was associated with somatic symptoms; and nonbinary status was associated with anxiety. Although statistically significant, these variables showed less importance compared to psychological resources. Overall, our findings extend prior research by examining established risk and resilience variables in concert with one another to determine their relative importance. From a clinical and public policy perspective, findings are encouraging. Regardless of a person's background, degree of exposure and risk to COVID‐19, or external resources, when these variables are considered concurrently with psychological resilience variables, inner resources (which are potentially modifiable) are more powerful predictors of mental health functioning.
As a PTE, the COVID‐19 pandemic is unique in that it represents both a chronic, ongoing threat and a collective trauma. In conceptualizing COVID‐19 as a PTE, we sought to understand the role of trauma coping processes in adaptation. The most robust predictor of adaptation to COVID‐19 across mental health outcomes was the pandemic CSE‐T, the self‐appraisal that one can cope with the ongoing stress of pandemic and the negative feelings surrounding it. CSE has repeatedly played a substantive role in adaptation to trauma (e.g., Luszczynska et al., 2009), and our findings highlight the importance of bolstering CSE‐T in prevention and intervention efforts. Interestingly, compared to the self‐appraisal of CSE, hope, which could be considered an outward appraisal about the world and expectation that something desired will happen in the face of threat (Roth & Hammelstein, 2007), had a smaller effect and only on depression and anxiety. This finding underscores the importance of efficacious appraisals about the self, rather than optimistic appraisals about the world in general, in adjusting to a pandemic.
When participants were asked to reflect on the coping strategies they employ during the COVID‐19 pandemic, the use of forward‐focused coping (utilizing distraction, generating positive thoughts while sublimating distressing feelings) was associated with better mental health outcomes whereas the use of trauma‐focused coping (effortful focus on the thoughts, images, and worries surrounding the traumatic event) was not a significant predictor of distress. Though these findings run contrary to the body of literature concerning efficacious coping in response to past traumatic events, research conducted in contexts of ongoing traumatic stress has suggested that trauma‐focused coping to an ongoing stressor may be implausible because individuals are less likely to identify discrete traumatic events to process (Diamond et al., 2010). Further explanation may be found in Hobfoll's COR theory (Hobfoll, 1989): during an ongoing trauma, it may be impractical to attempt to cope with feelings or emotions related to an event that is continuing to impact the individual as it has the potential to deplete one's psychological resources (Diamond et al., 2010; Gelkopf et al., 2013). This is important information from a clinical perspective, and suggests that when a trauma is ongoing, individuals who utilize adaptive avoidance coping strategies have better mental health outcomes than individuals who cope by confronting it head on. Additionally, it is possible that trauma‐focused coping strategies that do not appear to confer benefit in the acute phase will actually emerge as predictors of positive adaptation longitudinally. One 4‐year study of college undergraduates who had experienced a PTE showed that students who utilized high levels of trauma‐focused coping and low forward‐focused coping were more likely to belong to the distressed‐recovered trajectory group (Galatzer‐Levy et al., 2012). Longitudinal studies of coping and distress trajectories during COVID‐19 are needed to parse out relationships between coping and psychological outcomes as a function of time.
Coping through substance use was associated with higher levels of depression and should be a target for clinical interventions during the pandemic and other long‐lasting stressors. This finding is consistent with a plethora of research supporting the self‐medication hypothesis, which links substance use to mental health problems (Khantzian, 1987) but extends that research by directly asking about the use of substances as a coping strategy (e.g., Poindexter et al., 2015; Ullman et al., 2013).
As noted, only a select few demographics, COVID‐specific demands, and external resources variables emerged as significant predictors when accounting for the strong contribution of psychological resources. This is in contrast to prior COVID‐19 studies that have identified age (e.g., Elbay et al., 2020), gender (e.g., González‐Sanguino et al., 2020), SES (e.g., Sinawi et al., 2021), and social support (e.g., Liu, Zhang, et al., 2020) as predictors of distress or adaptation. This discrepancy is likely due to prior studies' reliance on regression or group comparison models that do not account for the examination of a large number of variables simultaneously. Indeed, in the present study, bivariate correlations revealed small effect sizes associated with SES, gender, age, social support, and mental health outcomes that were similar magnitude as other studies (e.g., Flesia et al., 2020), yet no longer significant when included in our ML model with psychological resilience variables. Similarly, in their ML investigation of with Chinese adults, Elhai et al. (2021) did not find age or sex to be predictors or anxiety whereas psychosocial variables were. These are important findings from a public health perspective that need to be replicated in larger, more diverse samples and ideally using ML. The one background variable that emerged as a significant predictor across mental health outcomes during COVID‐19 was prior mental health history, a finding consistent with prior research (Asmundson et al., 2020; French et al., 2020; González‐Sanguino et al., 2020; Özdin & Bayrak Özdin, 2020; Usher et al., 2020).
Prout et al. (2020) also examined predictors of anxiety, depression, and PTSD in an international sample of 2787 adults utilizing similar demographic and COVID‐specific variables but psychosocial variables that focused on implicit and explicit emotion regulation strategies. The strongest predictor of psychological distress was somatization, which was conceptualized as a defense mechanism by the authors. Here, we conceptualize somatic symptom burden as a psychological distress outcome, in which some individuals may experience psychological distress through somatic symptoms rather than emotional expression. Similar to the other mental health outcomes, pandemic CSE was the strongest predictor of somatic symptom burden, whereas other psychological resource variables (forward‐focused coping, coping styles, hope) that were predictive of depression, anxiety, and/or PTSD were not predictive of somatization. In contrast, COVID‐related variables (negative financial impacts and suspected diagnosis of COVID‐19) emerged as unique predictors of somatic symptom burden. Individuals who suspect they have COVID‐19 in the absence of a confirmed diagnosis may be more likely to experience and misinterpret somatic symptoms. Clinicians and researchers are often focused on the “traditional” mental health outcomes of depression, anxiety, and PTSD but may be less attuned to somatic symptoms as a negative outcome related to COVID‐19. Manifesting psychological distress via a broad array of somatic symptoms may be particularly salient when the stressor involves a threat to physical health, as COVID‐19 has been. The cross‐sectional nature of this study, and most of the COVID‐19 research literature, prevents any inferences around causality. Longitudinal research could assist in determining directionality in the relationships between somatization and depression, anxiety, and PTSD, to help determine the temporal role of somatization in adaptation to a chronic stressor.
Several limitations and directions for future research should be noted. First, the sample size is relatively small, especially in comparison to recent COVID‐19 papers utilizing much larger samples. This limits confidence in the generalizability of conclusions. In addition, participants were recruited via social media, which does not guarantee representativeness or fully allow for generalization to other samples. There may be selection bias for participants who volunteer to participate in COVID‐related mental health research. The recruitment approach may be partially responsible for the discrepancy in findings regarding demographic and resource variables. It is also important to acknowledge that some important sociocultural variables raised analytic challenges. For example, because low numbers of participants formed various racial and ethnic minority groups, we created a binary variable based on COVID‐19 risk to meet statistical assumptions. The limitations of our sampling do not allow for a nuanced examination and appreciation of cultural differences. Future research would benefit from larger samples with sufficient numbers of participants of diverse racial and ethnic backgrounds. The sole use of self‐report questionnaires limits reliability and validity; the high correlations observed between the mental health outcomes, and the consistent patterns of predictors across mental health outcomes, may be indicative of a “distressed” response bias. Finally, our data is cross‐sectional, making it impossible to determine causality or directionality. It will be imperative to continue to study the effects of pandemic (and varying degrees of lockdown and social isolation) over time. Longitudinal modeling of adaptation can assist in informing interventions during pandemic conditions. We are continuing to collect longitudinal data with this sample, which will allow for examination of trajectories of resilience, recovery, nonlinear shifts in functioning, and chronic difficulties. In addition, further research is needed to better understand COVID‐19 as a trauma and how PTSD symptoms, typically conceptualized as pertaining to a past trauma, are experienced when the event involves a chronic, uncertain, current and future life threat.
Overall, this ML approach identified a set of specific factors that was highly effective in predicting mental health outcomes during the COVID‐19 pandemic. Compared to environmental factors, psychological resources were the most salient predictors of mental health functioning, with pandemic coping self‐efficacy emerging as the most robust predictor. Contrary to prior trauma research, forward‐focused coping, but not trauma‐focused coping, was associated with better adaptation. These findings can assist in the development of targeted intervention and prevention programs. As COVID‐19 represents an ongoing and uncertain “trauma,” individuals may need to employ a specific set of coping strategies that emphasize distraction over processing. This is an important delineation for practitioners accustomed to trauma‐focused approaches and aligns with some prior research that suggests in the acute phase following a trauma, processing may not be beneficial. Finally, coping self‐efficacy should be directly targeted in psychotherapy (e.g., Luszczynska & Schwarzer, 2005), online self‐help (e.g., Benight et al., 2018), and community outreach efforts.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supplemental Figure 1.
Supplemental Figure 2.
Supporting information.
ACKNOWLEDGMENTS
We would like to acknowledge Julie Hurd, Jocelyn Walker, Lauren Siegel, Nicholas Wood, and Megha Patel for their assistance in data collection and Dr. Charles Benight for developing and providing the Pandemic Coping Self‐Efficacy Scale.
Samuelson, K. W. , Dixon, K. , Jordan, J. T. , Powers, T. , Sonderman, S. , & Brickman, S. (2022). Mental health and resilience during the coronavirus pandemic: A machine learning approach. Journal of Clinical Psychology, 78, 821–846. 10.1002/jclp.23254
REFERENCES
- Altmann, A. , Tolosi, L. , Sander, O. , & Lengauer, T. (2010). Permutation importance: A corrected feature importance measure. Bioinformatics, 26(10), 1340–1347. 10.1093/bioinformatics/btq134 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, DSM‐5 Task Force . (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM‐5 (5th ed). American Psychiatric Publishing, Inc. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Arslan, G. , Yıldırım, M. , Tanhan, A. , Buluş, M. , & Allen, K. A. (2020). Coronavirus stress, optimism‐pessimism, psychological inflexibility, and psychological health: Psychometric properties of the coronavirus stress measure. International Journal of Mental Health and Addiction. Advance online publication, 1–17. 10.1007/s11469-020-00337-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson, G. J. , Paluszek, M. M. , Landry, C. A. , Rachor, G. S. , McKay, D. , & Taylor, S. (2020). Do pre‐existing anxiety‐related and mood disorders differentially impact COVID‐19 stress responses and coping? Journal of Anxiety Disorders, 74, 02271. 10.1016/j.janxdis.2020.102271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benight, C. , & Cieslak, R. (2011). Cognitive factors and resilience: How self‐efficacy contributes to coping with adversities. In Southwick S., Litz B., Charney D., & Friedman M. (Eds.), Resilience and mental health: Challenges across the lifespan (pp. 45–55). Cambridge University Press. 10.1017/CBO9780511994791.005 [DOI] [Google Scholar]
- Benight, C. C. , & Bandura, A. (2004). Social cognitive theory of posttraumatic recovery: The role of perceived self‐efficacy. Behaviour Research and Therapy, 42(10), 1129–1148. 10.1016/j.brat.2003.08.008 [DOI] [PubMed] [Google Scholar]
- Benight, C. C. , Shoji, K. , James, L. E. , Waldrep, E. E. , Delahanty, D. L. , & Cieslak, R. (2015). Trauma coping self‐efficacy: A context‐specific self‐efficacy measure for traumatic stress. Psychological Trauma: Theory, Research, Practice, and Policy, 7(6), 591–599. 10.1037/tra000004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benight, C. C. , Shoji, K. , Yeager, C. M. , Weisman, P. , & Boult, T. E. (2018). Predicting change in posttraumatic distress through change in coping self‐efficacy after using the My Trauma Recovery eHealth intervention: Laboratory investigation. JMIR Mental Health, 5(4), e10309. 10.2196/10309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzofsky, M. , Smiley‐McDonald, H. , Moore, A. , & Krebs, C. (2014). Measuring socioeconomic status (SES) in the NCVS: Background, options, and recommendations. Bureau of Justice Statistics. [Google Scholar]
- Bibbins‐Domingo, K. (2020). This time must be different: Disparities during the COVID‐19 pandemic. Annals of Internal Medicine, 173, 233–234. 10.7326/m20-2247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno, G. A. (2005). Resilience in the face of potential trauma. Current Directions in Psychological Science, 14(3), 135–138. 10.1111/j.0963-7214.2005.00347.x [DOI] [Google Scholar]
- Bonanno, G. A. , Galea, S. , Bucciarelli, A. , & Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5), 671–682. 10.1037/0022-006X.75.5.671 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Ho, S. M. , Chan, J. C. , Kwong, R. S. , Cheung, C. K. , Wong, C. P. , & Wong, V. C. (2008). Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology, 27(5), 659–667. 10.1037/0278-6133.27.5.659 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , & Mancini, A. D. (2008). The human capacity to thrive in the face of potential trauma. Pediatrics, 121(2), 369–375. 10.1542/peds.2007-1648 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Pat‐Horenczyk, R. , & Noll, J. (2011). Coping flexibility and trauma: The Perceived Ability to Cope with Trauma (PACT) scale. Psychological Trauma: Theory, Research, Practice, and Policy, 3(2), 117–129. 10.1037/a0020921 [DOI] [Google Scholar]
- Bovin, M. J. , Marx, B. P. , Weathers, F. W. , Gallagher, M. W. , Rodriguez, P. , Schnurr, P. P. , & Keane, T. M. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth edition (PCL‐5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C. S. (1997). You want to measure coping but your protocol's too long: Consider the Brief Cope. International Journal of Behavioral Medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. , & Scheier, M. F. (2001). On the self‐regulation of behavior. Cambridge University Press. [Google Scholar]
- Carver, C. S. , Scheier, M. F. , & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267. 10.1037/0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- Choi, S. , Hong, J. Y. , Kim, Y. J. , & Park, H. (2020). Predicting psychological distress amid the COVID‐19 pandemic by Machine Learning: Discrimination and coping mechanisms of Korean immigrants in the US. International Journal of Environmental Research and Public Health, 17(17), 6057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conversano, C. , Di Giuseppe, M. , Miccoli, M. , Ciacchini, R. , Gemignani, A. , & Orru, G. (2020). Mindfulness, age and gender as protective factors against psychological distress during COVID‐19 pandemic. Frontiers in Psychology, 11, 1900. 10.3389/fpsyg.2020.01900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway, L. G., III , Woodard, S. R. , & Zubrod, A. (2020). Social psychological measurements of COVID‐19: Coronavirus perceived threat, government response, impacts, and experiences questionnaires. Preprint. 10.31234/osf.io/z2x9a [DOI]
- Dawson, D. L. , & Golijani‐Moghaddam, N. (2020). COVID‐19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science, 17, 126–134. 10.1016/j.jcbs.2020.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond, G. M. , Lipsitz, J. D. , Fajerman, Z. , & Rozenblat, O. (2010). Ongoing traumatic stress response (OTSR) in Sderot, Israel. Professional Psychology: Research and Practice, 41(1), 19–25. 10.1037/a0017098 [DOI] [Google Scholar]
- Ehlers, A. , & Clark, D. (2003). Early psychological interventions for adult survivors of trauma: A review. Biological Psychiatry (1969), 53(9), 817–826. 10.1016/S0006-3223(02)01812-7 [DOI] [PubMed] [Google Scholar]
- Elbay, R. Y. , Kurtulmuş, A. , Arpacıoğlu, S. , & Karadere, E. (2020). Depression, anxiety, stress levels of physicians and associated factors in Covid‐19 pandemics. Psychiatry Research, 290, 113130. 10.1016/j.psychres.2020.113130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai, J. D. , & Montag, C. (2020). The compatibility of theoretical frameworks with machine learning analyses in psychological research. Current Opinion in Psychology, 36, 83–88. 10.1016/j.copsyc.2020.05.002 [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Yang, H. , McKay, D. , Asmundson, G. J. , & Montag, C. (2021). Modeling anxiety and fear of COVID‐19 using machine learning in a sample of Chinese adults: associations with psychopathology, sociodemographic, and exposure variables. Anxiety, Stress, & Coping, 34(2), 130–144. 10.1080/10615806.2021.18781 [DOI] [PubMed] [Google Scholar]
- Flesia, L. , Monaro, M. , Mazza, C. , Fietta, V. , Colicino, E. , Segatto, B. , & Roma, P. (2020). Predicting perceived stress related to the Covid‐19 outbreak through stable psychological traits and machine learning models. Journal of Clinical Medicine, 9(10), 3350. 10.3390/jcm9103350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa, E. B. , & Rothbaum, B. 0 (1998). Treating the trauma of rape. Guilford. [Google Scholar]
- French, M. T. , Mortensen, K. , & Timming, A. R. (2020). Psychological distress and Coronavirus fears during the initial phase of the COVID‐19 pandemic in the United States. The Journal of Mental Health Policy and Economics, 23(3), 93–100. [PubMed] [Google Scholar]
- Galatzer‐Levy, I. R. , Burton, C. L. , & Bonanno, G. A. (2012). Coping flexibility, potentially traumatic life events, and resilience: A prospective study of college student adjustment. Journal of Social and Clinical Psychology, 31(6), 542–567. 10.1521/jscp.2012.31.6.542 [DOI] [Google Scholar]
- Gao, J. , Zheng, P. , Jia, Y. , Chen, H. , Mao, Y. , Chen, S. , Wang, Y. , Fu, H. , & Dai, J. (2020). Mental health problems and social media exposure during COVID‐19 outbreak. PLoS One, 15(4), e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelkopf, M. , Solomon, Z. , & Bleich, A. (2013). A longitudinal study of changes in psychological responses to continuous terrorism. Israel Journal of Psychiatry and Related Sciences, 50(2), 100–109. [PubMed] [Google Scholar]
- Gierk, B. , Kohlmann, S. , Kroenke, K. , Spangenberg, L. , Zenger, M. , Brähler, E. , & Löwe, B. (2014). The Somatic Symptom Scale–8 (SSS‐8): A brief measure of somatic symptom burden. JAMA Internal Medicine, 174(3), 399–407. 10.1001/jamainternmed.2013.12179 [DOI] [PubMed] [Google Scholar]
- Glowacz, F. , & Schmits, E. (2020). Psychological distress during the COVID‐19 lockdown: The young adults most at risk. Psychiatry Research, 293, 113486. 10.1016/j.psychres.2020.113486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González‐Sanguino, C. , Ausín, B. , Castellanos, M. Á. , Saiz, J. , López‐Gómez, A. , Ugidos, C. , & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID‐19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness, A. , Behar‐Zusman, V. , & Safren, S. A. (2020). Understanding the impact of COVID‐19 on Latino sexual minority men in a US HIV hot spot. AIDS and Behavior, 1–7. 10.1007/s10461-020-02862-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. 10.1037/0003-066X.44.3.513 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. , & Lilly, R. S. (1993). Resource conservation as a strategy for community psychology. Journal of Community Psychology, 21(2), 128–148. [DOI] [Google Scholar]
- Holmes, E. A. , O'connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, Christensen, H. , Cohen Silver, R. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou, T. , Zhang, R. , Song, X. , Zhang, F. , Cai, W. , Liu, Y. , Dong, W. , & Deng, G. (2020). Self‐efficacy and fatigue among non‐frontline health care workers during COVID‐19 outbreak: A moderated mediation model of posttraumatic stress disorder symptoms and negative coping. PLoS One, 15(12), e0243884. 10.1371/journal.pone.0243884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Mental health burden for the public affected by the COVID‐19 outbreak in China: Who will be the high‐risk group? Psychology, Health & Medicine, 26, 1–12. 10.1080/13548506.2020.1754438 [DOI] [PubMed] [Google Scholar]
- Khantzian, E. J. (1987). The self‐medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 65–74. [DOI] [PubMed] [Google Scholar]
- Kimhi, S. , Marciano, H. , Eshel, Y. , & Adini, B. (2020). Resilience and demographic characteristics predicting distress during the COVID‐19 crisis. Social Science & Medicine (1982), 265, 113389. 10.1016/j.socscimed.2020.113389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles L. M., O'Connor M.‐F. (2015). Coping flexibility, forward focus and trauma focus in older widows and widowers. Bereavement Care, 34(1), 17–23. 10.1080/02682621.2015.1028200 [DOI] [Google Scholar]
- Krafft, A. M. , Martin‐Krumm, C. , & Fenouillet, F. (2019). Adaptation, further elaboration, and validation of a scale to measure hope as perceived by people: Discriminant value and predictive utility vis‐à‐vis dispositional hope. Assessment, 26(8), 1594–1609. 10.1177/1073191117700724 [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. W. (2001). The PHQ‐9. Journal of General Internal Medicine, 16(9), 606–661. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroska, E. B. , Roche, A. I. , Adamowicz, J. L. , & Stegall, M. S. (2020). Psychological flexibility in the context of COVID‐19 adversity: Associations with distress. Journal of Contextual Behavioral Science, 18, 28–33. 10.1016/j.jcbs.2020.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn, M. (2008). Building predictive models in R using the caret package. Journal of Statistical Software, 28, 1–26. 10.18637/jss.v028.i05 27774042 [DOI] [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress, appraisal, and coping. Springer. [Google Scholar]
- Liu, C. H. , Stevens, C. , Conrad, R. C. , & Hahm, H. C. (2020). Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID‐19 pandemic among U.S. young adults with suspected and reported psychiatric diagnoses. Psychiatry Research, 292, 113345. Advance online publication. 10.1016/j.psychres.2020.113345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. H. , Zhang, E. , Wong, G. T. F. , & Hyun, S. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: Clinical implications for US young adult mental health. Psychiatry Research, 290, 113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska, A. , Benight, C. C. , & Cieslak, R. (2009). Self‐efficacy and health‐related outcomes of collective trauma: A systematic review. European Psychologist, 14(1), 51–62. 10.1027/1016-9040.14.1.51 [DOI] [Google Scholar]
- Luszczynska, A. , & Schwarzer, R. (2005). Social cognitive theory. Predicting Health Behaviour, 2, 127–169. [Google Scholar]
- Magaletta, P. R. , & Oliver, J. M. (1999). The hope construct, will, and ways: Their relations with self‐efficacy, optimism, and general well‐being. Journal of Clinical Psychology, 55(5), 539–551. [DOI] [PubMed] [Google Scholar]
- Mancini, A. D. , & Bonanno, G. A. (2009). Predictors and parameters of resilience to loss: Toward an individual differences model. Journal of Personality, 77(6), 1805–1832. 10.1111/j.1467-6494.2009.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manea, L. , Gilbody, S. , & McMillan, D. (2012). Optimal cut‐off score for diagnosing depression with the Patient Health Questionnaire (PHQ‐9): A meta‐analysis. Canadian Medical Association Journal, 184(3), E191–E196. 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani, R. , Renzi, A. , Di Trani, M. , Trabucchi, G. , Danskin, K. , & Tambelli, R. (2020). The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the Coronavirus Pandemic (COVID‐19) lockdown. Frontiers in Psychiatry, 11, 1195. 10.3389/fpsyt.2020.587724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzo, R. R. , Villanueva, III, E. Q. , Faller, E. M. , & Baldonado, A. M. (2020). Factors associated with psychological distress among Filipinos during Coronavirus Disease‐19 Pandemic crisis. Open Access Macedonian Journal of Medical Sciences, 8(T1), 309–313. 10.3889/oamjms.2020.5146 [DOI] [Google Scholar]
- Mayer, M. (2019). missRanger: Fast Imputation of Missing Values. R package version 2.1.0. https://CRAN.R-project.org/package=missRanger
- Mazza, C. , Ricci, E. , Biondi, S. , Colasanti, M. , Ferracuti, S. , Napoli, C. , & Roma, P. (2020). A nationwide survey of psychological distress among Italian people during the COVID‐19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health, 17(9), 3165. 10.3390/ijerph17093165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken, L. M. , Badinlou, F. , Buhrman, M. , & Brocki, K. C. (2021). The role of psychological flexibility in the context of COVID‐19: Associations with depression, anxiety, and insomnia. Journal of Contextual Behavioral Science, 19, 28–35. 10.1016/j.jcbs.2020.11.003 [DOI] [Google Scholar]
- Özdin, S. , & Bayrak Özdin, Ş. (2020). Levels and predictors of anxiety, depression and health anxiety during COVID‐19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry, 66(5), 504–511. 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer, E. J. , Best, S. R. , Lipsey, T. L. , & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: a meta‐analysis. Psychological Bulletin, 129(1), 52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Pakenham, K. I. , Landi, G. , Boccolini, G. , Furlani, A. , Grandi, S. , & Tossani, E. (2020). The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID‐19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science, 17, 109–118. 10.1016/j.jcbs.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinciotti, C. M. , Seligowski, A. V. , & Orcutt, H. K. (2017). Psychometric properties of the PACT Scale and relations with symptoms of PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 9(3), 362–369. [DOI] [PubMed] [Google Scholar]
- Poindexter, E. K. , Mitchell, S. M. , Jahn, D. R. , Smith, P. N. , Hirsch, J. K. , & Cukrowicz, K. C. (2015). PTSD symptoms and suicide ideation: Testing the conditional indirect effects of thwarted interpersonal needs and using substances to cope. Personality and Individual Differences, 77, 167–172. [Google Scholar]
- Prout, T. A. , Zilcha‐Mano, S. , Aafjes‐van Doorn, K. , Aafjes‐van Doorn, V. , Békés, I. , Christman‐Cohen, K. , Whistler, Kui, T. , & Di Giuseppe, M. (2020). Identifying predictors of psychological distress during COVID‐19: A machine learning approach. Frontiers in Psychology, 11, 586202. 10.3389/fpsyg.2020.586202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran, L. , Chen, X. , Wang, Y. , Wu, W. , Zhang, L. , & Tan, X. (2020). Risk factors of healthcare workers with Coronavirus Disease 2019: A retrospective cohort study in a designated hospital of Wuhan in China. Clinical Infectious Diseases, 71(16), 2218–2221. 10.1093/cid/ciaa287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/ [Google Scholar]
- Rettie, H. , & Daniels, J. (2020). Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID‐19 pandemic. The American Psychologist, 76, 427–437. 10.1037/amp0000710 [DOI] [PubMed] [Google Scholar]
- Rodin, R. , Bonanno, G. A. , Knuckey, S. , Satterthwaite, M. L. , Hart, R. , Joscelyne, A. , Bryant, R. A. , & Brown, A. D. (2017). Coping flexibility predicts post‐traumatic stress disorder and depression in human rights advocates. International Journal of Mental Health, 46(4), 327–338. [Google Scholar]
- Roth, M. , & Hammelstein, P. (2007). Hope as an emotion of expectancy: First assessment results. GMS Psycho‐Social Medicine, 4, 1–9. [PMC free article] [PubMed] [Google Scholar]
- Schnurr, P. , Vielhauer, M. , Weathers, F. , & Findler, M. (1999). Brief Trauma Questionnaire (BTQ) [Database record]. APA PsycTests. 10.1037/t07488-000 [DOI] [Google Scholar]
- Shahrour, G. , & Dardas, L. A. (2020). Acute stress disorder, coping self‐efficacy and subsequent psychological distress among nurses amid COVID‐19. Journal of Nursing Management, 28(7), 1686–1695. 10.1111/jonm.13124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan, L. , Steinhoff, A. , Bechtiger, L. , Murray, A. L. , Nivette, A. , Hepp, U. , Ribeaud, D. , & Eisner, M. (2020). Emotional distress in young adults during the COVID‐19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine, 1–10. 10.1017/S003329172000241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinawi, H. A. , Al Balushi, N. , Al‐Mahrouqi, T. , Al Ghailani, A. , McCall, R. K. , Sultan, A. , & Al‐Alawi, M. (2021). Predictors of psychological distress among the public in Oman amid coronavirus disease 2019 pandemic: A cross‐sectional analytical study. Psychology, Health & Medicine, 26(1), 131–144. 10.1080/13548506.2020.1842473 [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. W. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Taylor, S. (2019). The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Cambridge Scholars Publishing. [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. (2020). COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety, 37(8), 706–714. 10.1002/da.23071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, J. , & Barbato, M. (2020). Positive religious coping and mental health among Christians and Muslims in response to the COVID‐19 pandemic. Religions (Basel, Switzerland), 11(10), 498. 10.3390/rel11100498 [DOI] [Google Scholar]
- Ullman, S. E. , Relyea, M. , Peter‐Hagene, L. , & Vasquez, A. L. (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive Behaviors, 38(6), 2219–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K. , Bhullar, N. , & Jackson, D. (2020). Life in the pandemic: Social isolation and mental health. Journal of Clinical Nursing, 29, 2756–2757. 10.1111/jocn.15290 [DOI] [PubMed] [Google Scholar]
- Vagni, M. , Maiorano, T. , Giostra, V. , & Pajardi, D. (2020). Coping with COVID‐19: Emergency stress, secondary trauma and self‐efficacy in healthcare and emergency workers in Italy. Frontiers in Psychology, 11, 566912. 10.3389/fpsyg.2020.566912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valle, M. F. , Huebner, E. S. , & Suldo, S. M. (2006). An analysis of hope as a psychological strength. Journal of School Psychology, 44(5), 393–406. [Google Scholar]
- Waljee, A. K. , Mukherjee, A. , Singal, A. G. , Zhang, Y. , Warren, J. , Balis, U. , … Higgins, P. D. (2013). Comparison of imputation methods for missing laboratory data in medicine. British Medical Journal Open, 3(8). 10.1136/bmjopen-2013-002847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , McIntyre, R. S. , … Ho, C. (2020). A longitudinal study on the mental health of general population during the COVID‐19 epidemic in China. Brain, Behavior, and Immunity, 87, 40‐48. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The PTSD Checklist for DSM–5 (PCL‐5). Scale available from the National Center for PTSD at: www.ptsd.va.gov
- Wielgus, B. , Urban, W. , Patriak, A. , & Cichocki, Ł. (2020). Examining the associations between psychological flexibility, mindfulness, psychosomatic functioning, and anxiety during the COVID‐19 pandemic: A path analysis. International Journal of Environmental Research and Public Health, 17(23), 8764. 10.3390/ijerph17238764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, K. C. , Chan, S. K. , & Ma, T. M. (2005). Post‐traumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). Journal of Traumatic Stress, 18, 39–42. 10.1002/jts.20004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong, J. , Lipsitz, O. , Nasri, F. , Lui, L. M. W. , Gill, H. , Phan, L. , Chen‐Li, D. , Iacobucci, M. , Ho, R. , Majeed, A. , & McIntyre, R. S. (2020). Impact of COVID‐19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye, Z. , Yang, X. , Zeng, C. , Wang, Y. , Shen, Z. , Li, X. , & Lin, D. (2020). Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Applied Psychology: Health and Well‐Being, 12(4), 1074–1094. 10.1111/aphw.12211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildirim, M. , & Guler, A. (2020). COVID‐19 severity, self‐efficacy, knowledge, preventive behaviors, and mental health in turkey. Death Studies, 1‐8. 10.1080/07481187.2020.1793434 [DOI] [PubMed] [Google Scholar]
- Zacher, H. , & Rudolph, C. W. (2021). Individual differences and changes in subjective wellbeing during the early stages of the COVID‐19 pandemic. American Psychologist, 76(1), 50. [DOI] [PubMed] [Google Scholar]
- Zhou, Y. , MacGeorge, E. L. , & Myrick, J. G. (2020). Mental health and its predictors during the early months of the COVID‐19 pandemic experience in the United States. International Journal of Environmental Research and Public Health, 17(17), 6315. 10.3390/ijerph17176315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet, G. D. , Dahlem, N. W. , Zimet, S. G. , & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1.
Supplemental Figure 2.
Supporting information.


