Abstract
Background
Limited COVID‐19 vaccination acceptance among healthcare assistants (HCAs) may adversely impact older adults, who are at increased risk for severe COVID‐19 infections. Our study objective was to evaluate the perceptions of COVID‐19 vaccine safety and efficacy in a sample of frontline HCAs, overall and by race and ethnicity.
Methods
An online survey was conducted from December 2020 to January 2021 through national e‐mail listserv and private Facebook page for the National Association of Health Care Assistants. Responses from 155 HCAs, including certified nursing assistants, home health aides, certified medical assistants, and certified medication technicians, were included. A 27‐item survey asked questions about experiences and perceptions of COVID‐19 vaccines, including how confident they were that COVID‐19 vaccines are safe, effective, and adequately tested in people of color. Multivariable regression was used to identify associations with confidence in COVID‐19 vaccines.
Results
We analyzed data from 155 completed responses. Among respondents, 23.9% were black and 8.4% Latino/a. Most respondents worked in the nursing home setting (53.5%), followed by hospitals (12.9%), assisted living (11.6%), and home care (10.3%). Respondents expressed low levels of confidence in COVID‐19 vaccines, with fewer than 40% expressing at least moderate confidence in safety (38.1%), effectiveness (31.0%), or adequate testing in people of color (27.1%). Non‐white respondents reported lower levels of confidence in adequate testing of vaccines compared to white respondents. In bivariate and adjusted models, respondents who gave more favorable scores of organizational leadership at their workplace expressed greater confidence in COVID‐19 vaccines.
Conclusion
Frontline HCAs reported low confidence in COVID‐19 vaccines. Stronger organizational leadership in the workplace appears to be an important factor in influencing HCA's willingness to be vaccinated. Action is needed to enhance COVID‐19 vaccine uptake in this important population with employers playing an important role to build vaccine confidence and trust among employees.
Keywords: COVID‐19, frontline healthcare workers, healthcare assistants, staff, vaccines
Key Points
Confidence in the safety and effectiveness of COVID‐19 vaccines was low among frontline healthcare assistants, who provide the majority of direct patient care to older adults.
Perceptions of organizational leadership exhibited a consistent and positive correlation with confidence in COVID‐19 vaccines, suggesting that employers play an important role to build vaccine confidence and trust among employees.
Why Does this Paper Matter?
Healthcare assistants expressed low levels of confidence in COVID‐19 vaccines, which has serious health implications for older adults who rely on their care. Employers may plan an important role to build vaccine confidence and trust among employees to enhance COVID‐19 vaccine uptake.
INTRODUCTION
The novel coronavirus disease 2019 (COVID‐19) pandemic has had devastating effects on frail and chronically ill older adults, and on the frontline healthcare workers who support them. In the United States, more than 460,000 older adults have died from COVID‐19 infections. 1 In the long‐term care setting, there have been more than 133,000 resident deaths and 1900 staff deaths as of May 2021. 2 The need for social distancing and other restrictions to prevent the transmission of COVID‐19 have also contributed to worsening mental health and quality of life in older adults. 3 , 4 The COVID‐19 pandemic has created an unprecedented demand for front‐line healthcare workers to provide care under more hazardous conditions with infected patients, putting their own health and safety at risk. This is particularly true of healthcare assistants (HCAs), who provide the majority of direct patient care to functionally impaired older adults residing in both congregate settings and in the community. 5 , 6 These include certified nursing assistants, home health aides, certified medical assistants, and certified medication technicians.
Although the rollout of COVID‐19 vaccines has provided a sense of hope, the health benefits of vaccination programs are entirely dependent on sufficient uptake in the community. 7 Vaccine uptake has been high for older adults, particularly those in nursing homes and other congregate living settings. 8 However, willingness to be vaccinated among the general population is variable and may be lower than 50% in certain areas. 9 , 10 , 11 , 12 , 13 , 14 In the United States, black and Latino/a respondents report more vaccine hesitancy than white correspondents. 15 , 16 Early investigation suggests that hesitancy is multifactorial, including safety and efficacy concerns, given the rapid approval process. 17
Vaccine hesitancy among frontline HCAs may have serious consequences for older adults. Despite the critical role of HCAs, rates of vaccination have lagged behind other disciplines. 14 HCAs are predominantly female (90%), and more than 30% and 20% are black and Latino/a, respectively. 18 , 19 , 20 In addition, HCAs are underpaid and overworked, and have been left with scarce resources to deal with surging COVID‐19 cases during the pandemic. 21 Given that vaccine distribution and education for healthcare workers has primarily been orchestrated through healthcare organizations and employers, leadership and support in the workplace may be an important factor in influencing the likelihood that HCAs will be vaccinated. Hesitancy may also be driven by historical failures of the healthcare system to inspire trust among minority and disenfranchised groups. 22 , 23
To date, there are no studies evaluating COVID‐19 vaccine hesitancy among HCAs. Understanding potential drivers of vaccine hesitancy in HCAs is critical for their safety and the safety of older adults who are dependent on their care. Therefore, our objective was to evaluate perceptions of COVID‐19 vaccine safety and efficacy in a sample of HCAs, and to examine whether these perceptions differ by race, ethnicity, or work environment.
METHODS
This study was deemed exempt by the Institutional Review Board, Advarra.
Survey distribution and respondents
The target population for this study was HCAs aged 18 years and older. We partnered with the National Association of Health Care Assistants (NAHCA), the primary professional association representing HCAs, who distributed an anonymous Qualtrics survey link on December 20, 2020 to their email listserv and private Facebook page to their members and partners. NAHCA re‐promoted the survey using the same channels on January 7, 2021. Data collection was completed on January 15, 2021.
A total of 442 individuals participated in the survey, with 366 (82.8%) of those being responses from HCAs (certified nursing assistants, home health aides, certified medication technicians), the focus of this study. We excluded responses with any missing data (n = 211, 57.6%), resulting in a final sample of 155 completed responses from HCAs used in the main analysis.
Survey items
We developed a 27‐item survey to evaluate experiences and perceptions of COVID‐19, testing, vaccines, and communication preferences based on an environmental scan of the literature and expert opinion of our study team (see Supplementary Materials S1 in Appendix S1). For this study, we focused on questions related to perceptions of COVID‐19 vaccine safety and efficacy.
The following demographic information was collected: census region, age (18–24, 25–34, 35–44, 45–54, 55+), race (white, black, other), and ethnicity (Latino/a, non‐Latino/a). Respondents were asked to select their job category (i.e., certified nursing assistant, certified medication assistant, nurse, etc.). We categorized job setting into four categories based on the type of the work environment and hierarchy: (1) nursing home or hospital, (2) assisted living or continuing care retirement community (CCRC), (3) home care, or (4) other.
Respondents were asked to rate how confident (1 = not confident, 2 = somewhat confident, 3 = moderately confident, 4 = very confident) they were that COVID‐19 vaccines are safe, effective, and adequately tested in people of color. Two additional items asked respondents to rate the importance of different factors in decision‐making for being vaccinated using a sliding scale (1 = not important, 2 = somewhat important, 3 = moderately important, 4 = very important). These included characteristics of the vaccine (safety, effectiveness, cost, pain, convenience) and social/environmental factors (recommendation from a healthcare provider, seeing public figures, coworkers, or other trusted individuals get the vaccine, getting paid time off ).
We also asked respondents to indicate any trusted sources of information to learn more about COVID‐19 (e.g., government, local news, employer, colleagues) and to select any preferred channels of communication to receive further information about COVID‐19 (e.g., TV news, newspapers, websites, social media).
Finally, to assess the contribution of employer characteristics to employee perceptions about vaccines, we included the nursing leadership subscale of the Practice Environment Scale of the Nursing Work Index, a validated National Quality Forum endorsed measure of the nurse work environment. 24 This 5‐item scale contains questions on nurse manager ability, leadership, and support of nurses and aides. We made minor modifications to be applicable for long‐term care and community work settings. Responses to the five questions were averaged to create a composite measure of nursing leadership and characterized as poor (lowest 25th), average (25th–75th), and good (top 75th). 25
Analysis
Demographic characteristics and item responses for the full sample were summarized for all completed surveys. For descriptive purposes, we reported slider scale responses as the proportion of respondents rating each item as a score of 3 or more (i.e., at least moderate importance or moderate confidence). We compared responses related to vaccine confidence across race, ethnicity, job setting, and nursing leadership using Pearson's chi‐squared tests. We used generalized linear regression models to evaluate the association of respondent characteristics with confidence in COVID‐19 vaccine safety and effectiveness in univariable and multivariable adjusted models including race, ethnicity, age, care setting, region, and organizational leadership.
As a sensitivity analysis, for questions related to vaccine confidence, we compared the proportion of missing versus non‐missing responses across racial and ethnic groups to determine the potential for nonresponse bias. We also conducted the same comparisons of slider scale responses to determine whether including partial responders resulted in substantive changes to our findings.
RESULTS
Demographic characteristics for the 155 respondents are presented in Table 1. Over half of the respondents aged 45 years or older (53.5%) and were predominantly white (63.9%; black 23.9%), and 8.4% were identified as Latino/a. Most respondents (53.5%) worked in nursing homes, followed by hospitals (12.9%), assisted living (11.6%), and home care (10.3%). Respondents were more likely to live in the South (40.6%) or the Midwest (32.9%) and most received the flu vaccine in the prior year (78.1%).
TABLE 1.
Respondent characteristics (n = 155)
| Variable | n (%) |
|---|---|
| Age | |
| 18–24 | 11 (7.1) |
| 25–34 | 22 (14.2) |
| 35–44 | 38 (25.2) |
| 45–54 | 52 (33.4) |
| 55+ | 31 (20.0) |
| Race | |
| White | 99 (63.9) |
| Black | 37 (23.9) |
| Asian | 6 (3.9) |
| American Indian/Alaskan Native | 3 (1.9) |
| Native Hawaiian/Pacific Islander | 1 (0.6) |
| Multiracial | 4 (2.6) |
| Other | 5 (3.2) |
| Ethnicity | |
| Latino/a | 13 (8.4) |
| Job setting | |
| Nursing home | 83 (53.5) |
| Hospital | 20 (12.9) |
| Assisted living | 18 (11.6) |
| Home care | 16 (10.3) |
| Other | 18 (11.6) |
| Geographic region | |
| Northeast | 21 (13.5) |
| Midwest | 51 (32.9) |
| South | 63 (40.6) |
| West | 20 (12.9) |
| Organizational leadership | |
| Poor | 33 (21.3) |
| Average | 81 (52.3) |
| Good | 41 (26.5) |
| Vaccine history | |
| Flu vaccine in last 12 months | 121 (78.1%) |
Overall COVID‐19 vaccine perceptions
Overall, HCAs expressed low levels of confidence in COVID‐19 vaccines (Figure 1). Just 38.1% and 31.0% of respondents expressed at least moderate confidence in the safety and effectiveness of COVID‐19 vaccines, respectively. In addition, only 27.1% of HCAs expressed at least moderate confidence that COVID‐19 vaccines have been adequately tested in people of color.
FIGURE 1.
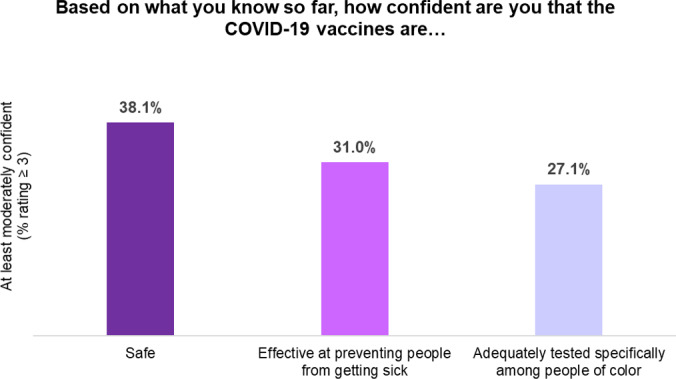
Overall confidence in COVID‐19 vaccines
Large majority of respondents expressed that safety (91%) and effectiveness (89%) were important in deciding whether to receive a vaccine for COVID‐19 (Figure 2). Factors that appeared to be less important, with fewer than half of the respondents indicating at least moderate importance, were whether the vaccine is painful (38.7%), seeing coworkers get vaccinated (41.3%), and seeing public figures get vaccinated (29.7%).
FIGURE 2.
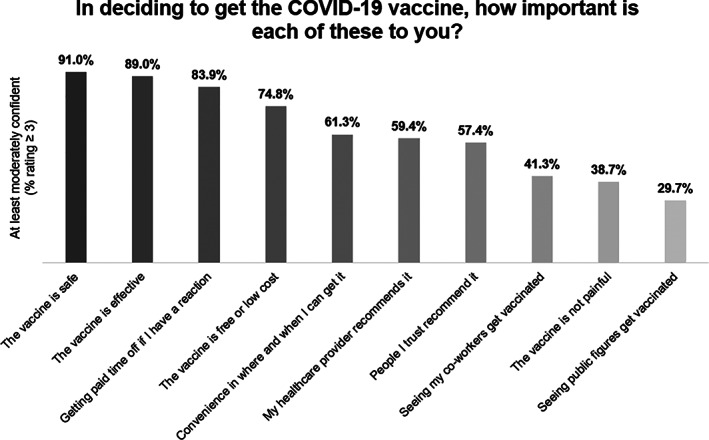
Important decision‐making factors for COVID‐19 vaccines
COVID‐19 vaccine perceptions by race and ethnicity
Black and other race respondents were less confident that COVID‐19 vaccines have been adequately tested in people of color, with just 16.2% and 10.5% reporting at least moderate confidence compared to 34.3% of white respondents (p = 0.02) (Table 2). Fewer black respondents reported safety and effectiveness of vaccines as important in decision‐making (safety: 81.1%; effectiveness: 78.4%) compared to white (safety: 93.9%; effectiveness 91.9%) or other race respondents (safety: 94.7%; effectiveness: 94.7%). However, these differences failed to reach statistical significance (safety: p = 0.06; effectiveness: p = 0.06). No differences were noted across ethnicity. Additional stratified analyses are presented in Tables S1 and S2.
TABLE 2.
Confidence in COVID‐19 vaccines by Key Strata (n = 155)
| Confidence in COVID‐19 Vaccines | |||
|---|---|---|---|
| Based on what you know so far, how confident are you that the COVID‐19 vaccines are… (% rating ≥ 3—at least moderately confident) | |||
| Safe | Effective at preventing people from getting sick | Adequately tested for safety and effectiveness specifically among people of color. | |
| By race | |||
| White | 40.4% | 35.4% | 34.3% |
| Black | 27.0% | 18.9% | 16.2% |
| Other | 34.3% | 16.2% | 10.5% |
| p‐value | 0.24 | 0.18 | 0.02* |
| By ethnicity | |||
| Latino/a | 53.8% | 38.5% | 46.2% |
| Non‐Latino/a | 36.6% | 30.3% | 25.4% |
| p‐value | 0.22 | 0.54 | 0.11 |
| By job setting | |||
| Nursing home/hospital | 27.2% | 33.0% | 27.2% |
| AL/CCRC | 44.4% | 22.2% | 22.2% |
| Home care | 43.8% | 37.5% | 43.8% |
| Other | 33.3% | 22.2% | 16.7% |
| p‐value | 0.86 | 0.61 | 0.33 |
| By organizational leadership | |||
| Poor | 27.3% | 15.2% | 15.2% |
| Average | 35.8% | 29.6% | 25.9% |
| Good | 51.2% | 46.3% | 39.0% |
| p‐value | 0.09 | 0.02* | 0.07 |
p < 0.05.
COVID‐19 vaccine perceptions by job setting and organizational leadership
We observed no statistically significant differences in perceptions of vaccine safety and efficacy across work settings.
Respondents who rated their organization's leadership as good or average were more likely to report at least moderate confidence in the effectiveness of COVID‐19 vaccines: For example, among respondents who rated their organization's leadership as poor, only 15.2% reported moderate or high confidence in the effectiveness of the vaccine, compared with 29.6% and 46.3% among those who rated their organization's leadership as moderate or good, respectively; p = 0.02 (Table 2). We observed a similar nonsignificant trend for respondents' confidence in whether COVID‐19 vaccines are safe and whether they have been adequately tested in people of color.
Communication preferences
Healthcare providers were most often selected as a trusted source of information (60.9%) (Table S3). This was consistent across racial and ethnic groups as well as job setting and organizational leadership categories. Less common trusted sources of information indicated by respondents were state/local (33.5%) or federal government (31.0%), and employer (28.4%). Communication preferences related to COVID‐19 were equally divided between TV news (40.6%), in person education (40.0%), and websites (39.4%).
Association of respondent characteristics with confidence in COVID‐19 vaccines
The results from univariable and multivariable regression models are presented in Table 3. In multivariable regression models, the only factor to be significantly associated with the questions of vaccine confidence (safety or efficacy) was perceived organizational leadership. These associations remained statistically significant after adjusting for race, ethnicity, age, job setting, and geographic region. In adjusted univariable models, a good rating for perceived organizational leadership was associated with greater confidence in COVID‐19 vaccine efficacy (good rating: +0.65 [0.09–0.91], p = 0.02). A rating of moderate or good leadership confidence was associated with greater belief that the COVID‐19 vaccines were adequately tested in people of color (moderate rating: +0.43 [0.05, 0.81], p = 0.03; good rating: +0.68 [0.26–1.11], p = 0.002).
TABLE 3.
Association of respondent characteristics with confidence in COVID‐19 vaccines
| Based on what you know so far, how confident are you that the COVID‐19 vaccines are… | Estimate (unadjusted) | p‐value | Estimate (adjusted) | p‐value |
|---|---|---|---|---|
| Safe? | ||||
| Race | ||||
| White (ref) | ‐ | ‐ | ‐ | ‐ |
| Black | −0.28 [−0.63, 0.08] | 0.12 | −0.150 [−0.540, 0.239] | 0.447 |
| Other | 0.20 [−0.26, 0.66] | 0.38 | 0.199 [−0.316, 0.714] | 0.446 |
| Ethnicity | ||||
| Non‐Latino/a (ref) | ‐ | ‐ | ‐ | ‐ |
| Latino/a | 0.32 [−0.21, 0.86] | 0.234 [−0.340, 0.817] | 0.416 | |
| Setting | ||||
| NH/Hospital (ref) | ‐ | ‐ | ‐ | ‐ |
| Assisted living/CCRC | −0.03 [−0.51, 0.44] | 0.89 | 0.03 [−0.47, 0.52] | 0.92 |
| Home care | 0.048 [−0.45, 0.55] | 0.85 | 0.04 [−0.47, 0.56] | 0.87 |
| Other | −0.06 [−0.54, 0.42] | 0.81 | −0.09 [−0.57, 0.40] | 0.73 |
| Organizational leadership | ||||
| Poor (ref) | ‐ | ‐ | ‐ | ‐ |
| Average | 0.20 [−0.18, 0.59] | 0.29 | 0.268 [−0.13, 0.67] | 0.19 |
| Good | 0.37 [−0.06, 0.80] | 0.09 | 0.371 [−0.08, 0.82] | 0.10 |
| Effective? | ||||
| Race | ||||
| White (ref) | ‐ | ‐ | ‐ | ‐ |
| Black | −0.25 [−0.58, 0.08] | 0.13 | −0.11 [−0.46, 0.25] | 0.55 |
| Other | 0.15 [−0.28, 0.57] | 0.50 | 0.08 [−0.39, 0.55] | 0.73 |
| Ethnicity | ||||
| Non‐Latino/a (ref) | ‐ | ‐ | ‐ | ‐ |
| Latino/a | 0.38 [−0.13, 0.87] | 0.13 | 0.27 [−0.25, 0.80] | 0.30 |
| Setting | ||||
| NH/Hospital (ref) | ‐ | ‐ | ‐ | ‐ |
| Assisted living/CCRC | −0.17 [−0.61, 0.27] | 0.44 | −0.16 [−0.61, 0.29] | 0.48 |
| Home care | −0.06 [−0.52, 0.40] | 0.81 | −0.05 [−0.52, 0.42] | 0.84 |
| Other | −0.13 [−0.57, 0.30] | 0.55 | −0.17 [−0.604, 0.27] | 0.46 |
| Organizational leadership | ||||
| Poor (ref) | ‐ | ‐ | ‐ | ‐ |
| Average | 0.21 [−0.14, 0.56] | 0.24 | 0.26 [−0.10, 0.63] | 0.15 |
| Good | 0.48 [0.09, 0.88] | 0.02* | 0.65 [0.09, 0.91] | 0.02* |
| Adequately tested for safety and effectiveness specifically among people of color? | ||||
| Race | ||||
| White (ref) | ‐ | ‐ | ‐ | ‐ |
| Black | −0.21 [−0.56, 0.10] | 0.24 | −0.17 [−0.49, 0.25] | 0.54 |
| Other | 0.031 [−0.42, 0.48] | 0.89 | 0.07 [−0.42, 0.55] | 0.79 |
| Ethnicity | ||||
| Non‐Latino/a (ref) | ‐ | ‐ | ‐ | ‐ |
| Latino/a | 0.25 [−0.28, 0.78] | 0.35 | 0.24 [−0.31, 0.78] | 0.39 |
| Setting | ||||
| NH/Hospital (ref) | ‐ | ‐ | ‐ | ‐ |
| Assisted living/CCRC | −0.11 [−0.57, 0.36] | 0.65 | −0.03 [−0.49, 0.43] | 0.91 |
| Home care | 0.26 [−0.23, 0.74] | 0.30 | 0.19 [−0.30, 0.67] | 0.45 |
| Other | −0.25 [−0.71, 0.21] | 0.28 | −0.29 [−0.75, 0.17] | 0.21 |
| Organizational leadership | ||||
| Poor (ref) | ‐ | ‐ | ‐ | ‐ |
| Average | 0.37 [0.01, 0.71] | 0.04* | 0.43 [0.05, 0.81] | 0.03* |
| Good | 0.67 [0.26, 1.08] | 0.002* | 0.68 [0.26, 1.11] | 0.002* |
p < 0.05.
Sensitivity analyses
We noted no consistent patterns in missing responses for questions related to confidence in COVID‐19 vaccines across racial or ethnic groups. Across racial categories, missing responses were higher among black respondents, compared to white or other race respondents, but there are no statistically significant differences that were consistent across responses. No statistically significant differences were noted across ethnicities. When examining comparisons across groups for all completed responses, we noted no substantive changes in our findings. There were a few instances where the statistical significance of comparisons fluctuated, but this was likely driven by changes in sample size across groups (Table S4).
DISCUSSION
In a national survey of HCAs, we found a low level of confidence in the safety, effectiveness, and adequate testing of COVID‐19 vaccines in people of color. Fewer than 40% of respondents expressed at least a moderate level of confidence in COVID‐19 vaccines. Black respondents tended to express lower levels of confidence in COVID‐19 vaccines compared to white or other race respondents. We also observed a notable dose–response relationship between perceived organizational leadership and confidence in vaccine efficacy, which remained significant in multivariable regression models.
To our knowledge, the present study is the first survey to evaluate COVID‐19 vaccine hesitancy among HCAs working in nursing homes, assisted living communities, hospitals, and homecare. Although our sample was limited to NAHCA members, the demographic makeup of our sample was comparable to national data on HCAs, with approximately 15%–25% being black and 10%–20% being Latino/a. 19 , 20 Several prior studies have evaluated the acceptance of COVID‐19 vaccines among other groups of healthcare workers. A recent single‐state survey 14 conducted among nursing home and assisted living staff with varied clinical roles found that just 45% were willing to receive a vaccine for COVID‐19. Increased willingness to be vaccinated was observed among white respondents and those who were older. Another survey of hospital employees from several states 26 reported just 36% reporting willingness to be vaccinated and lower rates of willingness among black and Latino/a respondents. A slightly higher rate of COVID‐19 vaccine acceptance (55%) was reported in another survey of U.S. hospital system employees, 27 but did not examine differences across subgroups. Our study affirms concerns about vaccine hesitancy by adding data on HCAs, arguably the healthcare workers in the closest contact with the highest risk patient population.
Our results suggested that health professionals may remain even more influential in their decision‐making than peers and members of the community. We observed that seeing others get vaccinated (e.g., public figures) was less frequently reported as important for decision‐making among HCAs. Numerous efforts have been made to increase the visibility of public figures and community leaders being vaccinated against COVID‐19 to influence those who may be hesitant. However, our results suggest that healthcare providers may be more influential in addressing vaccine hesitancy. Taken together, these findings are informative for future targeted efforts to increase vaccine uptake.
When examining results across key subgroups, we noted no significant differences across ethnicities or job setting in terms of confidence in COVID‐19 vaccines. Generally speaking, black respondents expressed lower levels of confidence in COVID‐19 vaccine effectiveness, safety, and adequate testing. However, most of these trends failed to reach statistical significance in our analyses. Lower confidence in COVID‐19 vaccines among racial minorities is not surprising, given the historical underrepresentation of people of color in clinical trials. Enrollment data suggest that although COVID‐19 vaccine trials 28 , 29 have achieved greater representation than what has been achieved in most clinical trials, people of color are still underrepresented, despite the higher burden of severe illness in these populations. A lack of trust in government and structural racism may also play a role in confidence in COVID‐19 vaccines in people of color. In a recent qualitative study conducted by the members of our research team, 17 respondents expressed that low willingness to be vaccinated among black individuals may be driven by the skepticism of government and organizational leaders, who tend to be white men. Trust in government to make decisions in their best interest also emerged as a strong predictor of vaccine hesitancy among racial and ethnic minorities in another national survey. 30 Thus, it is particularly important that educational efforts to increase confidence in the safety and efficacy of COVID‐19 vaccines also seek to establish trust with black HCAs.
One important finding was a dose–response relationship of perceived organizational leadership and confidence in COVID‐19 vaccines, which has not been previously reported. Respondents who perceived their organization's leadership as good had higher levels of confidence in COVID‐19 vaccine effectiveness and adequate testing among people of color. Many HCAs may have mistrust in leadership as the initial response to COVID‐19 was often suboptimal and personal protective equipment, testing, and paid time off for illness symptoms or exposures were inadequate. An effective response to COVID‐19 outbreaks may have been pivotal in earning the trust necessary for vaccination campaigns. However, further research is needed to better understand specific factors that may contribute to poor perceived organizational leadership and how to address issues of trust between healthcare organizations and staff. Prior literature suggests a relationship between the perceived work environment and organizational leadership on staff and patient outcomes. Specifically, adequate staffing, support from management, and engagement in organizational affairs have been associated with less nursing burnout and improved patient outcomes, including hospitalizations and pressure ulcers. 31 , 32 , 33 In addition, a handful of studies have reported that more favorable work environments were associated with greater rates of influenza vaccine uptake among healthcare workers. 34 , 35 , 36 Future vaccine campaigns should seek to improve organizational culture and perceptions of leadership through a participatory approach that considers the preferences and concerns of all stakeholders, including frontline nursing staff. 31 , 32 , 33
Several findings from our study regarding communication preferences may be informative for developing interventions to address COVID‐19 vaccine hesitancy or misinformation. Medical directors and other healthcare providers have been largely absent from campaigns to promote COVID‐19 vaccinations, with most campaigns being led by governmental officials or agencies. Yet, healthcare providers were overwhelmingly selected as a trusted source of information across all groups. Leveraging the established level of trust between individuals and their healthcare providers may be more effective in overcoming issues of trust in organizational leadership or government than using generic educational messaging. In addition, given that in‐person education was listed as one of the more preferred communication channels overall among HCAs, opportunities that facilitate a one‐on‐one conversation between HCAs and healthcare providers may be a desirable avenue to improve COVID‐19 vaccine uptake.
Several limitations to our analysis should be acknowledged. The survey was distributed through a listserv and online forum for NAHCA, the primary professional organization representing HCAs. The members of this organization may not be the representative of all HCAs in the United States, and survey respondents may not be the representative of all NAHCA members. However, our sample reflects racial, ethnic, and geographic representation from across the United States, and is comparable to that of national data with just slightly lower representation from black and Latino/a respondents. 19 , 20 , 37 We also had a large proportion of missing responses for questions related to perceptions of COVID‐19 vaccines. Although we observed no statistically significant differences in missingness across racial and ethnic groups, it is possible that other unmeasured factors may have contributed to missing data. There are a number of unmeasured psychosocial factors that contribute to vaccine hesitancy, including personal experiences with COVID‐19, that were not considered in this analysis. We also did not assess the influence of staff turnover or whether staff perceptions of work environment differ between agency and non‐agency staff. Finally, it is highly likely that perceptions of vaccines have changed. Given that these data were collected over December 2020 to January 2021, our findings should be interpreted in the context of data collected in the early months of vaccine approval and rollout. Despite these limitations, we believe that our findings still provide original and meaningful insight into vaccine hesitancy for frontline healthcare workers and have the potential to increase vaccine uptake in this essential and vulnerable segment of the healthcare workforce.
CONCLUSIONS
Frontline HCAs reported low confidence in COVID‐19 vaccines. Stronger organizational leadership in the workplace appears to be an important factor in influencing HCA's willingness to be vaccinated. Efforts are needed to further understand and develop targeted strategies to address reasons for the lack of confidence in COVID‐19 vaccines among HCAs, despite data from well‐designed trials demonstrating high levels of effectiveness and safety. Action is needed to enhance COVID‐19 uptake in this important population with employers playing an important role to build vaccine confidence and trust among employees.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Joshua D. Niznik, Jill Harrison, Elizabeth White, and Sarah D. Berry contributed to the study concept and survey design. Joshua D. Niznik and Casey J. Kelley helped with data management and cleaning. Joshua D. Niznik, C.Kelley, and Sarah D. Berry performed statistical analysis and interpretation. Joshua D. Niznik, Elizabeth White, Maggie Syme, Laura C. Hanson, and Sarah D. Berry helped with clinical perspectives. Joshua D. Niznik, Jill Harrison, Elizabeth White, Maggie Syme, Laura C. Hanson, Casey J. Kelley, and Sarah D. Berry contribute to the preparation of the manuscript. Joshua D. Niznik, Jill Harrison, Elizabeth White, Maggie Syme, Laura C. Hanson, Casey J. Kelley, Lori Porter, and Sarah D. Berry helped with critical revision and feedback.
SPONSOR'S ROLE
The funding sources had no role in the study design, data collection and analysis, manuscript preparation, or the decision to submit the manuscript for publication.
Supporting information
Appendix S1. Supporting Information.
Supplementary Materials S1. Survey distributed to the National Association of Health Care Assistants (NAHCA) Membership.
Supplementary Materials 2
Table S1. Respondent perceptions of COVID‐19 vaccines by race.
Table S2. Respondent perceptions of COVID‐19 vaccines by ethnicity.
Table S3. Overall information and communication preferences.
Table S4. Confidence in COVID‐19 vaccines by Key Strata (all completed responses).
Niznik JD, Harrison J, White EM, et al. Perceptions of COVID‐19 vaccines among healthcare assistants: A national survey. J Am Geriatr Soc. 2022;70(1):8‐18. doi: 10.1111/jgs.17437
Funding information This work was supported through a supplemental award by the National Institute on Aging (NIA) of the National Institutes of Health under Award Number 3U54AG063546‐02S2 to the NIA Imbedded Pragmatic Alzheimer's Disease and AD‐Related Dementias Clinical Trials Collaboratory (NIA IMPACT Collaboratory, U54AG063546) as part of the RADx Underserved Populations (RADx‐UP) program, which supports 32 institutions across the United States to focus on populations disproportionately affected by the pandemic. Dr. Berry receives funds to mentor through a grant from the NIA (K24 AG070106). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Centers for Disease Control and Prevention . COVID‐19 Mortality Overview. Published 2021. Accessed April 24, 2021. https://www.cdc.gov/nchs/covid19/mortality-overview.htm
- 2. Centers for Medicare and Medicaid Services . COVID‐19 Nursing Home Data. Published 2021. Updated May 30, 2021. Accessed June 14, 2021. https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/
- 3. O'Caoimh R, O'Donovan MR, Monahan MP, et al. Psychosocial impact of COVID‐19 nursing home restrictions on visitors of residents with cognitive impairment: a cross‐sectional study as part of the engaging remotely in care (ERiC) project. Front Psychiatry. 2020;11:585373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wammes JD, Kolk MD, van den Besselaar MD, MacNeil‐Vroomen JL, Buurman‐van Es BM, van Rijn M. Evaluating perspectives of relatives of nursing home residents on the nursing home visiting restrictions during the COVID‐19 crisis: a Dutch Cross‐Sectional Survey Study. J Am Med Dir Assoc. 2020;21(12):1746‐1750.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xu H, Intrator O, Bowblis JR. Shortages of staff in nursing homes during the COVID‐19 pandemic: what are the driving factors? J Am Med Dir Assoc. 2020;21(10):1371‐1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Institute of Medicine (US) Committee on Nursing Home Regulation . Improving the Quality of Care in Nursing Homes. National Academies Press; 1986. [PubMed] [Google Scholar]
- 7. Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS‐CoV‐2 infection by mass vaccination. Lancet. 2020;396(10263):1614‐1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gharpure R, Guo A, Bishnoi CK, et al. Early COVID‐19 first‐dose vaccination coverage among residents and staff members of skilled nursing facilities participating in the pharmacy partnership for long‐term care program ‐ United States, December 2020‐January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(5):178‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goldman RD, Yan TD, Seiler M, et al. Caregiver willingness to vaccinate their children against COVID‐19: cross sectional survey. Vaccine. 2020;38(48):7668‐7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kourlaba G, Kourkouni E, Maistreli S, et al. Willingness of Greek general population to get a COVID‐19 vaccine. Glob Health Res Policy. 2021;6(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Neumann‐Bohme S, Varghese NE, Sabat I, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID‐19. Eur J Health Econ. 2020;21(7):977‐982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prati G. Intention to receive a vaccine against SARS‐CoV‐2 in Italy and its association with trust, worry and beliefs about the origin of the virus. Health Educ Res. 2020;35(6):505‐511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID‐19 vaccine hesitancy in a representative working‐age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210‐e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Unroe KT, Evans R, Weaver L, Rusyniak D, Blackburn J. Willingness of long‐term care staff to receive a COVID‐19 vaccine: a single state survey. J Am Geriatr Soc. 2020;69(3):593‐599. [DOI] [PubMed] [Google Scholar]
- 15. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID‐19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500‐6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kreps S, Prasad S, Brownstein JS, et al. Factors associated with US adults' likelihood of accepting COVID‐19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harrison J, Berry S, Mor V, Gifford D. "Somebody Like Me": understanding COVID‐19 vaccine hesitancy among staff in skilled nursing facilities. J Am Med Dir Assoc. 2021;22(6):1133‐1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. Vital Health Stat 13. 2009;(167):1‐155. [PubMed] [Google Scholar]
- 19. Artiga S, Rae M, Claxton G, Garfield R. Key Characteristics of Health Care Workers and Implications for COVID‐19 Vaccination. Published 2021. Accessed January 29. 2021. https://www.kff.org/coronavirus‐covid‐19/issue‐brief/key‐characteristics‐of‐health‐care‐workers‐and‐implications‐for‐covid‐19‐vaccination/
- 20. US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, National Center for Health Workforce Analysis . Sex, Race, and Ethnic Diversity of U.S. Health Occupations (2011‐2015). Vol 2017. https://bhw.hrsa.gov/sites/default/files/bureau‐health‐workforce/data‐research/diversity‐us‐health‐occupations.pdf. [Google Scholar]
- 21. Muench U, Jura M, Spetz J, Mathison R, Herrington C. Financial vulnerability and worker well‐being: a comparison of long‐term services and supports workers with other health workers. Med Care Res Rev. 2020;1077558720930131. 10.1177/1077558720930131. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 22. Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97(7):1283‐1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99(7):1293‐1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176‐188. [DOI] [PubMed] [Google Scholar]
- 25. Lake ET. The nursing practice environment: measurement and evidence. Med Care Res Rev. 2007;64(2 Suppl):104S‐122S. [DOI] [PubMed] [Google Scholar]
- 26. Shekhar R, Sheikh AB, Upadhyay S, et al. COVID‐19 vaccine acceptance among health care workers in the United States. Vaccines (Basel). 2021;9(2):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Meyer MN, Gjorgjieva T, Rosica D. Trends in health care worker intentions to receive a COVID‐19 vaccine and reasons for hesitancy. JAMA Netw Open. 2021;4(3):e215344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA‐1273 SARS‐CoV‐2 vaccine. N Engl J Med. 2021;384(5):403‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid‐19 vaccine. N Engl J Med. 2020;383(27):2603‐2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Langer Research Associates . COVID Collaborative Survey: Coronavirus Vaccination Hesitancy in the Black and Latinx Communities. COVID Collaborative. 2020. https://www.covidcollaborative.us/content/vaccine-treatments/coronavirus-vaccine-hesitancy-in-black-and-latinx-communities [Google Scholar]
- 31. White EM, Aiken LH, McHugh MD. Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. J Am Geriatr Soc. 2019;67(10):2065‐2071. 10.1111/jgs.16051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. White EM, Aiken LH, Sloane DM, McHugh MD. Nursing home work environment, care quality, registered nurse burnout and job dissatisfaction. Geriatr Nurs. 2020;41(2):158‐164. 10.1016/j.gerinurse.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Flynn L, Liang Y, Dickson GL, Aiken LH. Effects of nursing practice environments on quality outcomes in nursing homes. J Am Geriatr Soc. 2010;58(12):2401‐2406. 10.1111/j.1532-5415.2010.03162.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hogan V, Lenehan M, Hogan M, Natin DP. Influenza vaccine uptake and attitudes of healthcare workers in Ireland. Occup Med (Lond). 2019;69(7):494‐499. [DOI] [PubMed] [Google Scholar]
- 35. Pless A, McLennan SR, Nicca D, Shaw DM, Elger BS. Reasons why nurses decline influenza vaccination: a qualitative study. BMC Nurs. 2017;16:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mignot A, Wilhelm MC, Valette A, Gavard‐Perret ML, Abord‐De‐Chatillon E, Epaulard O. Behavior of nurses and nurse aides toward influenza vaccine: the impact of the perception of occupational working conditions. Hum Vaccin Immunother. 2020;16(5):1125‐1131. 10.1080/21645515.2019.1694328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sengupta M, Harris‐Kojetin LD, Ejaz FK. A national overview of the training received by certified nursing assistants working in U.S. nursing homes. Gerontol Geriatr Educ. 2010;31(3):201‐219. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information.
Supplementary Materials S1. Survey distributed to the National Association of Health Care Assistants (NAHCA) Membership.
Supplementary Materials 2
Table S1. Respondent perceptions of COVID‐19 vaccines by race.
Table S2. Respondent perceptions of COVID‐19 vaccines by ethnicity.
Table S3. Overall information and communication preferences.
Table S4. Confidence in COVID‐19 vaccines by Key Strata (all completed responses).


