Abstract
Purpose
Despite widespread promotion of breast and cervical cancer (BCC) screening, uptake remains low in rural communities. Barriers to healthcare, which often result in poorer health outcomes, differentially impact residents of rural communities. Effective interventions addressing the unique needs of rural women may target these barriers and increase BCC screening participation. Our objective is to review and assess the published literature on interventions to increase BCC screening in rural communities.
Methods
A systematic scoping review of PubMed/Medline was performed to identify BCC screening interventions conducted in rural settings. English language articles from peer-reviewed journals published from January 2006 to October 2019 were included if they reported results for BCC screening interventions in rural communities in the United States.
Results
We reviewed 228 articles and identified eight articles consistent with our inclusion criteria. Studies varied in sample population characteristics, geographic location, design, and mode of intervention delivery. Interventions included patient navigation strategies, educational outreach programs, peer counseling, and small media initiatives. Interventions focused on promoting uptake of initial or one-time screening rather than targeted repeat screening, and few studies detailed the cost-effectiveness of the interventions.
Conclusion
This review may inform efforts to develop strategies to increase BCC screening among rural women. Additional cancer prevention and control research gaps in rural communities include the examination of the theoretical foundations, design, delivery, and cost-effectiveness of BCC screening interventions for rural communities. Future research might focus on methods to promote repeat BCC screening and effective translation of these interventions for other rural populations.
Keywords: breast cancer screening, cervical cancer screening, rural health, mammography, Pap test
Introduction
Despite widespread promotion of breast and cervical cancer (BCC) screening, uptake of these strategies remains consistently low in rural communities.[1] A recent study found rates of incident cancers that can be prevented by screening and associated deaths were higher in rural areas compared to non-rural areas.[2] Timely initial and regular screening is critical to cancer prevention and control efforts for detecting precancerous lesions and early stage cancer.[2] Women who are not routinely screened for BCC are at increased risk of later stage diagnosis compared to women who receive these screenings at the appropriate intervals,[3] and disease risk may be compounded for women in rural communities. Many barriers to quality health care—often resulting in poor health outcomes—impact residents of rural communities, and these barriers may be exacerbated by geography. Residents of rural areas report limited access to quality health care and may be restricted in obtaining recommended care by travel distance, transportation difficulties, provider shortages, and access to specialty care.[4–6] Furthermore, some women experience emotional and physical discomfort during BCC screening tests, and the anticipation of pain and or stigma during screening has been identified as a notable barrier to care in some rural communities. [7] Improving uptake of routine BCC screening is critical for earlier disease detection and, potentially, better outcomes in these medically underserved communities.[8]
Barriers to quality health care faced by rural populations suggest interventions designed to address the specific needs of rural women, such as access to routine and specialty care, are necessary. [9] However, limited information is available about the types of BCC screening interventions being implemented in rural settings. Previous reviews have examined interventions used in the general population as well as some traditionally medically underserved populations including African American, Asian, and Hispanic women. [10,11] Yet, few have examined BCC interventions implemented in rural settings, and to date, no review has summarized these activities. Furthermore, there are several barriers to healthcare that are more prevalent among racial/ethnic minorities in rural communities including lack of economic and educational resources, limited healthcare coverage, and physician shortages. [12] These barriers may compound racial/ethnic minorities’ access to BCC screening services and warrants further investigation of interventions designed to address their needs.
To address this gap, we conducted a review of the literature to identify existing interventions designed to increase BCC screening among residents of rural areas. We were interested in identifying characteristics of BCC interventions in rural settings and providing an overview of the interventions’ characteristics, which may inform future systematic reviews in this topic. The limited number of BCC interventions implemented in rural setting and heterogenous nature of the rural target populations made a scoping review appropriate for our objective.
The definition of rurality varies across the literature, which makes it difficult to determine whether a particular region is considered urban or rural. The nuances in what makes a region rural are marked by indicators including, but not limited to, population density, land use, and distance to an urban center.[13] Given the complexities in defining rurality, our review did not explicitly define “rural” in our inclusion criteria. Rather, we included any literature that described intervention implementation in a rural community as defined by study authors. Definitions of rural varied by individual studies. We used Community Preventive Services Task Force (CPSTF) recommendations on effective intervention strategies to increase BCC screening as a framework to classify interventions included in the review. Review findings can provide guidance about opportunities for research and practice to address BCC prevention and control in rural communities.
Methods
We conducted a scoping review [14,15] of the literature to synthesize the research on existing BCC interventions in rural communities by identifying and categorizing key characteristics of the interventions. We used the PRISMA extension for scoping review (PRISMA-ScR) as the methodological guideline for our review.[16]
Search Strategy
The literature search was conducted using a multi-step strategy. First, one researcher conducted an initial search for literature reviews on breast and/or cervical cancer screening interventions in rural settings. No US-based literature reviews were found, however, confirming the need for a review of this literature. Second, in January 2017, we identified relevant peer-reviewed articles through a PubMed/MEDLINE search of the literature published in English between January 2006 and January 2017. Interventions included in publications prior to January 2006 would likely have outdated intervention strategies that would no longer be relevant to current day rural settings. Additionally, future studies would likely not adapt interventions implemented beyond 10 years given the technologic advances in BCC screening tools. PubMed/MEDLINE was the most appropriate database given that it is the most widely accessible biomedical resource nationally and covers a large number of indexed peer-reviewed literature. The PubMED/MEDLINE search was supplemented by scanning the reference lists of relevant manuscripts.
The search terms included: cancer AND breast OR cervical AND intervention OR program(s) OR prevention AND rural OR rural communities OR rural areas OR rural populations OR rurality AND screening OR mammography OR Pap smear OR Pap OR Pap test OR HPV test, OR human papillomavirus test. Third, an additional literature search was conducted in October 2019 to identify any literature meeting our inclusion criteria newly published between January 2017 and October 2019. The same search strategy from January 2017 was used in the October 2019 search. This search did not yield additional articles.
Eligibility Criteria
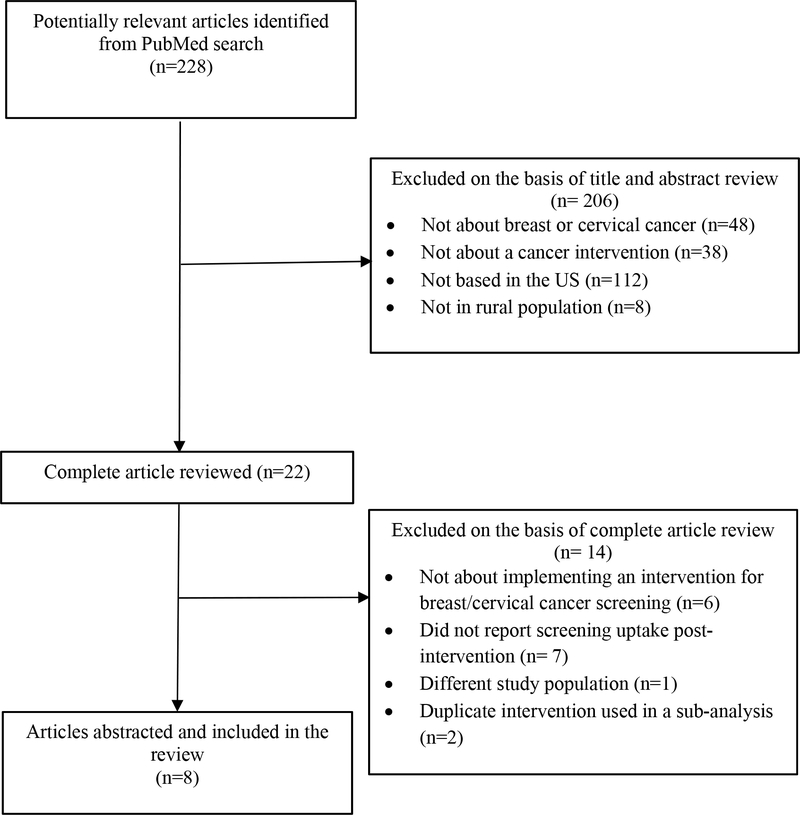
We developed inclusion/exclusion criteria to determine articles appropriate for full-article review. Selections for full review would meet the following criteria:1) published in a peer-reviewed journal, 2) written in English, 3) published between January 1, 2006 and October 1, 2019, 4) provided a description of a cancer screening intervention for breast and/or cervical cancer, 5) reported screening outcome data, 6) included participants in rural communities, 7) reported on outcomes of rural participants independently (if sample included participants not residing in rural locations) and 8) conducted in the United States. Given the complexities in defining rurality, our review did not explicitly define “rural” in our inclusion criteria. Rather, we included any literature described as implementing the intervention in a rural community as defined by the individual studies. Given the variation in healthcare systems and insurance coverage worldwide, we only included studies conducted in the United States. Furthermore, definitions of rurality vary domestically and even more so in a global context. Articles were excluded if they only reported screening antecedents or intermediate outcomes including scheduling appointments, intentions to screen, and knowledge/awareness about cancer screening. Our search was not limited to a specific age range due to the variance in BCC screening guidelines or recommendations. Figure I depicts the PRISMA diagram of the number of articles identified, included, excluded, and the reasoning for exclusion.
Figure I.
PRISMA Diagram
Data Abstraction
One researcher reviewed titles and abstracts for all articles and classified abstracts as “relevant”, “additional information needed”, or “not relevant. Any questions or concerns about relevance were discussed among the three researchers. For papers marked as “relevant” or “additional information needed”, three researchers independently conducted a full text review of each article. All three researchers reviewed all the full text publications to confirm inclusion criteria were met and confirm relevant data items for abstraction. We resolved disagreements on study inclusion and data item extraction with discussion until consensus was reached.
One researcher carried out the data item abstraction. Study exclusion and inclusion criteria are provided in Figure I. Data for the title and abstract review and the full article review were stored and managed in Microsoft Excel. We abstracted data on the intervention characteristics (i.e. intervention name, geographic location), study design, cancer focus of intervention (i.e. breast, cervical, or both), characteristics of the target population (i.e. age, race/ethnicity), reported BCC screening guidelines (yes or no; specified organizational guideline), theoretical framework(s) (yes/no; specified theory), cost-effectiveness analyses (yes/no), screening target (i.e. one-time screening or repeated screening), and the CPSTF intervention type (one-on-one, group, or multicomponent).
CPSTF Intervention Strategies
The CPSTF was established by the U.S Department of Health and Human Services and tasked with identifying scientifically sound population-based health interventions proven to improve population health, increase lifespans, and improve quality of life. Scientists and subject matter experts from the Centers for Disease Control and Prevention (CDC) make recommendations and identify knowledge gaps to inform decision making based on rigorous and replicable systemic reviews of scientific literature (https://www.thecommunityguide.org/task-force/about-community-preventive-services-task-force). The CPSTF identified client-oriented, multicomponent, and provider-oriented intervention strategies that are effective in increasing breast and/or cervical cancer screening (https://www.thecommunityguide.org/content/task-force-findings-cancer-prevention-and-control). We used these CPSTF intervention strategies as a framework to assign studies included in our review to an “intervention type” based on the aforementioned CPSTF recommendations for effective BCC screening interventions. Table I provides intervention type definitions as defined by the CPSTF.
Table I.
Community Preventive Services Task Force (CPSTF) Intervention Definitions[17]
| Intervention type | CPSTF Definition |
|---|---|
| One-on-One Education | One-on-one education is provided in person or by telephone to encourage individuals to be screened for cancer. Healthcare providers can deliver one-on-one education in clinical settings, at home, or in local gathering places. Brochures, informational letters, or reminders may also be used. The information can be general or tailored to the needs of each person. |
| Group Education | Group education sessions are usually conducted by health educators or trained laypeople, using slide presentations or other teaching aids in a lecture or interactive setting. These sessions convey information on indications for, benefits of, and ways to overcome barriers to screening, with the goal of informing, encouraging, and motivating participants to seek recommended screenings. |
| Multicomponent | Multicomponent interventions to promote cancer screening combine two or more intervention approaches reviewed by the CSPTF. Combinations may include the following. • Two or more intervention approaches from the following strategies: ◦ Interventions to increase community demand: client reminders, client incentives, small media, mass media, group education, one-on-one education ◦ Interventions to increase community access: reducing structural barriers, reducing client out-of-pocket costs (reducing administrative barriers, appointment scheduling assistance, providing transportation, providing translation, providing childcare) ◦ Interventions to increase provider delivery of screening services: provider assessment and feedback, provider incentives, provider reminders • Two or more intervention approaches to reduce different structural barriers Multicomponent interventions to increase cancer screening may be coordinated through healthcare systems, delivered in community settings, or both. |
Results
The literature search initially identified 228 potential articles on breast and/or cervical screening interventions implemented in rural communities. Of the 228 potentially relevant articles, 206 were excluded after an abstract review. As summarized in Figure I, 22 articles were selected for a full-text review, of which eight fulfilled criteria for inclusion and were included in the final review. Additionally, we scanned the references of the 22 articles included in the full-text review, but we did not identify additional articles to be included in the scoping review. Many articles were excluded because they did not report screening outcomes or only reported cancer screening antecedents such as intention to seek cancer screening and knowledge about cancer screening. Of the 8 articles included, two studies reported outcomes exclusively on increasing breast cancer screening,[18,19] three examined only cervical cancer screening,[20–22] and three focused on both breast and cervical cancer screening.[23–25] Four articles were published in the early 2000s and four were published in 2010 or later. We identified 3 randomized control trials, 2 cross-sectional studies, 1 cohort study, 1 case-control study, and 1 community case study. The findings and descriptive characteristics of the eight abstracted articles are found in Table II.
Table II.
Study characteristics of breast and cervical cancer screening interventions in rural settings
| First Author, Year | Intervention Name | Breast, Cervical, or Combined | Community Guide Intervention Approach | Target Population (Sample size) | Location | Intervention Description | Significant Findings |
|---|---|---|---|---|---|---|---|
| BENCIVENGA, 2008 | Adaptation of "Tell a Friend" | Breast | One-on-One Education | Women aged 40 and older (302) | Pennsylvania, US | One-on-one peer counseling to encourage women to get a regular mammogram. Intervention also included small media, appointment scheduling, patient reminders, and incentives. | Of the 158 women in need of a mammogram, 138 (87.3%) received a mammogram as a result of the intervention. |
| FALK, 2016 | Friend to Friend plus Patient Navigation | Combined | Group Education | African American, Latina, and Non-Hispanic White women aged 18 and older (2689) | Texas, US | Community based small-group education conducted by patient navigators to educate women on need for mammograms and Pap tests in an effort to increase screening at follow-up visit. | PN* intervention participants had increased odds of getting screened for both breast (OR: 2.64 (1.93–3.60) and cervical (OR: 2.72 (2.00–3.69) cancer compared to non-PN participants. |
| GELLERT, 2006 | Ohana Day | Breast | One-on-One Education | Hawaiian women aged 40 and older (38) | Hawaii, US | Community day project designed to educate underserved Hawaiians about breast cancer screening and incorporates native Hawaiian cultural styles and values. | Breast cancer screening increased from 66% to 86% (p=0.02) as a result of the intervention. |
| KATZ, 2007 | The Rose Project | Cervical | One-on-One Education | Native American, non-Hispanic White and African American women aged 40 and older (775) | North Carolina, US | Study examined cervical cancer screening uptake among women participating in a mammography program. Intervention group received an individual health education program on mammography and control group received physician letter/brochure on Pap tests. | Intervention participants significantly increased Pap test uptake; (OR: 1.70, p > .001) |
| LUQUE, 2016 | Salud es Vida | Cervical | Group Education | Immigrant Latina women aged 21–65 years from farmworker backgrounds (90) | Georgia, US | Lay health worker-led, Spanish language group education on Pap tests, self-efficacy, and knowledge. Intervention group received materials including curriculum guide, brochure, flipchart, short animated video, and in-class activities during the group sessions. | Twelve (32%) intervention group participants received cervical cancer screening compared to 10 (19%) control group participants (p=0.178). There were no significant differences in Pap test uptake between groups. |
| NUNO, 2011 | Entre Amigas/Between Friends | Combined | Group Education | Hispanic women aged 50 and older (381) | Arizona, US | Women were randomly assigned to the promotora-led education intervention or usual care. The intervention group received general BCC information, explanations of cancer screening, and information on community resources for health care and screening. | Intervention group was significantly more likely to be screened for breast cancer compared to the usual care group (OR: 2.0, 95% CI= 1.3–3.1). Intervention group was more likely to be screened for cervical cancer (OR: 1.5, CI= 0.9–2.6), although the result was not statically significant. |
| THOMPSON, 2006 | Celebremos la salud! | Combined | Multicomponent | Hispanic and non-Hispanic White women aged 18 and older (1083) | Washington, US | Multicomponent intervention that includes community group education conducted in schools, religious organizations, and worksites; outreach materials; health fair events; free/subsidized screening services; and mobile screening services. | Among both Hispanics and Whites, there were no significant differences in use of screening services for cervical or breast cancer. |
| THOMPSON, 2017 | N/A | Cervical | One-on-One Education | Latinas aged 21–64 years (443) | Washington, US | RCT examining the effects of a low-intensity intervention (video) and high-intensity (video and home-base education session with promotora) intervention to increase cervical cancer screening uptake. | Significantly more women in the high intensity arm [78 (53.4%)] were screened for cervical compared to the usual care [50 (34%), p<.001] arm or low-intensity arm [58 (38.7%), p<.01]. |
PN – patient navigation
Study Demographics
Age
Participant age in the studies varied by type of screening intervention. Both breast cancer screening interventions reported outcomes for women 40 and older. All cervical cancer screening interventions included women aged 21–65 years. The age range for the combined interventions varied. Two of the combined interventions included participants aged 18 to 99 years, [23,25] while the other focused on women 50 and older.[24]
Race/ethnicity
The majority of articles included study populations comprised of multiple racial/ethnic groups in rural settings including African American, Hispanic/Latina, and non-Hispanic White women (n=4). Some articles focused solely on specific racial/ethnic groups including Hispanic/Latina (n=3) and Native Hawaiian (n=1) women in rural communities.
Geographic location
Study authors characterized the regions served by the intervention as rural. Limited information was provided about specific characteristics of the regions, although a few articles did describe the locations as agricultural. The interventions were implemented in the following states: Arizona, Georgia, Hawaii, North Carolina, Pennsylvania, Texas and Washington. We used the US Census Bureau Region and Divisions to categorize the states as West (i.e. AZ, WA, HI), South (i.e. TX, GA, NC) and Northeast (i.e. PA). [26]
Screening guidelines or recommendations
Six of the studies described the screening guidelines or recommendations used to inform the intervention materials and messages The United States Preventive Services Task Force[27,28] and the American Cancer Society.[29,30] were the most commonly cited BCC screening guidelines or recommendations.
Theoretical framework
Five of the eight articles included a mention of the theoretical framework(s) that informed the intervention design. Of these, four articles named multiple theoretical frameworks including but not limited to social learning theory [31], PRECEDE-PROCEED [32], the Transtheoretical Model [33], the communication-behavior change model [34], and the community organization model for health promotion. [35] The most prevalent theoretical framework mentioned across all the studies was social cognitive theory. [36]
One-time versus repeat screening
All of the studies detailed interventions focused on one-time breast and/or cervical cancer screening. No intervention described promotion of repeat screening for either cancer.
Outcomes by Intervention Strategy
Group Education Strategies
Friend to Friend + PN.
The Friend to Friend plus patient navigation (FTF + PN) program is designed to increase BCC screening uptake in underserved, uninsured, older women residing in rural Texas aged 18 to 99 years from March 2012 to February 2015.[23] The FTF intervention consists of “pink parties” organized by cancer prevention specialists to educate women about BCC screening. The “pink parties” had three components 1) an oral presentation from clinical staff on the benefits of mammography, 2) a facilitator-led small groups to encourage seeking mammography and discuss concerns and 3) a session with the facilitator to help the participant prompt their provider to offer mammography. The intervention also covered the cost of clinical services and transportation for participants with financial needs.[37] Participants in the FTF + PN program also receive active support to obtain BCC screening from a patient navigator. The findings suggest the effects of the FTF + PN intervention varied by race/ethnicity and primary language spoken. English-speaking Latina women had decreased odds of receiving a mammogram [OR: 0.60 (0.43–0.83)] and Pap test [OR: 0.66 (0.47–0.92)] compared to non-Hispanic White control group. However, Spanish-speaking Latina women had increased odds [OR: 1.64 (1.22–2.20)] of receiving a Pap test compared with non-Hispanic White controls.
Salud es Vida.
Salud es Vida is an intervention designed to increase cervical cancer screening for rural immigrant Latina women led by promotoras in a group setting.[20] The intervention was implemented in four rural counties in Southeast Georgia in 2014–2015 among women aged 21–65 years. The intervention consisted of education materials developed and administered by promotoras including a curriculum guide, a brochure, a flipchart, an animated video and in-class activities. There were no statistically significant differences in Pap test uptake between the intervention and control groups. The results of the study found 32% of intervention participants were screened for cervical cancer at the 3-month follow-up compared to 19% of control participants (p=0.178).
Entre Amigas.
Entre Amigas (Between Friends) is a promotora-led intervention developed to reduce the risk of breast, cervical, and diet-related cancers among medically underserved Hispanic women.[24] The study was conducted among Hispanic women aged 50 or older living a in a rural U.S Mexico border community in Texas. Women were randomly assigned to the educational intervention or usual care arms. The intervention group received group education on general BCC information, explanations of cancer screening, and information on community resources for health care and screening. Women in the intervention group were more likely to receive breast cancer screening at one-year follow up compared to the usual care group (OR: 2.0, 95% CI= 1.3–3). At one-year post-intervention, no significant differences in cervical cancer screening were seen between women in the intervention group versus controls (OR: 1.5, 95% CI= 0.9–2.6).
One-on-One Education Strategies
Ohana Day Project.
The Ohana Day Project is designed to educate underserved Hawaiians on breast cancer screening and incorporates native Hawaiian cultural styles and values in the educational sessions. The intervention is a one-day program and was implemented in a small, rural Hawaiian community. BCC screening was assessed among Hawaiian women aged 40 and older. The program included one-on-one physician visits for screening and cancer education including culturally appropriate brochures. The results demonstrated improvements in breast cancer screening with 84% of the women aged 40 or older receiving a mammogram at 6 month follow up compared to the 66% pre-intervention comparison group (p= 0 .002).[18]
Tell a Friend.
The Tell a Friend intervention was originally designed to reach eligible women less likely to take advantage of early detection. In the adaptation of the intervention deployed from February to June 2015, investigators used one-on one peer counseling to increase breast cancer screening among low-income, rural women in Pennsylvania. The site for the educational sessions was a food pantry and all participants were aged 40 years and older.[19] The intervention focused on one-on-one contact by volunteers to encourage friends and family to get a routine mammogram. The intervention also included small media, appointment scheduling, patient reminders, and incentives. The results of the cross-sectional study found 52.3% of age-eligible women were non-adherent to breast cancer screening guidelines at baseline. Of these women, 87% received a mammogram as a result of the intervention.
Individualized lay health advisor education intervention.
A 2007 study assessed cervical cancer screening uptake among women participating in an intervention designed to increase mammography uptake among medically underserved women aged 40 and older in rural southeastern North Carolina.[21] Authors sought to determine if prior exposure to an earlier breast cancer screening intervention would improve uptake of cervical cancer screening. The intervention group received an individual health education program on mammography, which was customized to the needs of each participant and administered by a lay health worker. The control group received a physician letter/brochure on Pap tests. Findings demonstrated that women in the intervention (OR: 1.70;1.31, 2.21) and control (OR: 1.38; 1.04, 1.82) groups had significantly increased Pap test completion rates. Additionally, women in the high-risk groups for cervical cancer (>2 sexual partners, age at first sexual intercourse <18 years, current smoker, treated for STD or partner treated for STD) significantly increased cervical cancer screening uptake (OR:1.88, p < 0.001) compared to women in the low-risk group.
Individual video and community health worker intervention.
The effects of a low-intensity and high-intensity intervention for cervical cancer screening were compared to usual care among Latina women aged 21 to 64 years who were not up-to-date with cervical cancer screening in rural Washington.[22] The intervention included assistance in scheduling appointments and improving knowledge about cancer screening. In the low intensity arm, a video on cervical cancer screening was presented in the participant’s home. The high intensity arm included the video plus a home-based education session with a community health worker. The results of this randomized controlled trial (RCT) suggested significantly more women in the high intensity arm (53%) received a Pap test compared to women in the low-intensity (39%, p <.001) and usual care (34%, p <.01) arms.
Multicomponent Intervention Strategies
Celebremos la Salud!.
Celebremos la Salud is a community-based RCT aimed at increasing colorectal, breast, and cervical cancer screening in rural communities specifically among Latinas 18 years and older in Washington.[25] This multicomponent intervention incorporated multiple intervention strategies as defined by the CPSTF including group education, reducing structural barriers, and reducing out-of-pocket costs. The trial was conducted in the 20 small communities located in the Lower Yakima Valley of Washington state with communities ranging in size from 300 to 7,000 residents. Using baseline survey data on size, proportion Hispanic, and presence of community clinic, communities were placed into matched pairs where one community was randomized to receive the intervention and the other served as the control. The 30-month intervention was implemented in community, small groups, and individuals. Community sites included health fairs, fun runs, and other events which included bicultural and bilingual interventionists delivering educational presentations about cancer screening and distributing screening promotion materials. A wellness van provided free screening, and local clinics provided free or reduced cost screening as part of the intervention. The results of this RCT found no significant changes in the use of screening services between the intervention and control groups for breast and cervical cancer.[25]
Discussion
This review of eight studies describes the published literature on the effectiveness of existing BCC screening interventions targeting women in rural settings. Of these studies, six increased BCC screening uptake in rural communities following intervention implementation. We compared our findings with the CPSTF recommendations for interventions to increase screening for BCC. Intervention strategies used in the reviewed studies were consistent with the CPSTF recommended approach of increasing community demand. One-on-one educational programs[19,21,22,18] and group education[23,24] were found to increase BCC screening in these rural populations. None of the reviewed single-component interventions applied the CPSTF strategies of increasing community access or increasing provider delivery.
The CPSTF recommends use of one-on-one education to increase community demand for BCC screening, and our review demonstrated the effectiveness of this approach. [17] The design of one-on-one educational outreach allows for messages on the benefits of cancer screening to be delivered by a lay health worker or health care professional. The effectiveness of this approach is likely due to its ability to directly interact with intervention participants and address questions immediately in a personal setting.[38] Our review also found one-on-one education interventions were often tailored to cater to the unique needs of specific populations. For example, some interventions were adapted to specific cultural components using native language materials or communication messages. The tailored design of these one-on-one education interventions support the theory that tailored materials can improve effectiveness of screening interventions in reaching specific groups.[39,40]
For multicomponent interventions, the CPSTF recommends the use of a combination of intervention approaches that increase community demand, increase community access, or increase provider delivery. The multicomponent intervention in our review incorporated approaches to increase community demand and increase community access. However, this intervention did not effectively increase BCC screening in the study reviewed.[25] This finding may be the result of no intervention approach consistent with increasing provider delivery of services.[39]
The cervical cancer screening intervention in our review that employed a group education approach did not increase screening.[20] The CPSTF has found insufficient evidence that group education alone increases cervical cancer screening.[41] The results of this study support the need for more well-designed studies to examine this intervention strategy for cervical cancer screening.
Rural communities, in particular, have a number of barriers to obtaining care such as travel distance, transportation difficulties, and access to specialty care. There is a need to mitigate the structural barriers in these communities that may depress screening uptake. For breast cancer screening, the CPSTF recommends increasing community access through reducing client out-of-pocket costs and structural barriers. The one intervention in this review that included free or reduced cost BCC screening was not successful in increasing screening uptake. [25] Currently, there is insufficient evidence for strategies associated with increasing community access for cervical cancer screening.[42] Importantly, many of the interventions that included components designed to reduce structural barriers [25,23,19] employed system and policy enhancements such as reducing administrative costs and assistance with appointment scheduling.[43]
Our review identified several notable gaps in BCC interventions in rural communities. None of the studies detailed interventions focused on repeat BCC screening. While is it is important to develop interventions for women who are never or rarely screened, current guidelines and recommendations support routine screening for BCC.[27,28] There may be opportunities to build additional components into existing interventions to encourage women to be screened regularly, consistent with recommended guidelines or recommendations. As new technologies emerge and guidelines or recommendations are revised, the potential for increasing disparities in BCC screening uptake may occur and interventions for rural women may be developed to mitigate this increase. Future research to identify or develop effective interventions that promote on-time repeat BCC screening could address cancer disparities in rural areas.
Several distinct challenges exist for translation of interventions to promote BCC and wider implementation in rural settings. Few studies reported how rurality was defined. In order to fully examine interventions in rural settings and assess opportunities for adaptation to other rural and medically underserved populations, it will be important to have a systematic definition of rurality applied across intervention activities. Very few of the articles included in this review explicitly identified the metrics employed to identify the region as rural. Some definitions were based on the Health Resources and Services Administration (HRSA) list of rural counties and census tracts or population density of the region.[44] Most studies simply used the word ‘rural’ or “agricultural” to define the setting of interest without further explanation. The lack of consistency in defining rurality may be due to the colloquial use of “rural” that has become commonplace in the literature. Future interventions to increase BCC screening may include explicit information about the rural setting to aid in implementation and adaptation of effective methods.[45] At minimum, we recommend interventions could convey the population density of the setting of interest. Other indicators of rurality including land use and distance to urbanized regions could also be considered. Most importantly, interventions should provide a clear explanation of the indicators used to define the rural community.
Further, heterogeneity in population demographics and geographic locations exists in the rural regions of the United States. For example, the residents of rural Appalachia[46–48] have different demographic characteristics compared to the residents in the rural Mississippi Delta.[49,50] Despite both areas being largely rural, there may be important differences in the needs and barriers of both communities. These differences may require varied intervention design or delivery to improve screening uptake. The demographic and geographic characteristics of the populations covered in this review were very heterogeneous. Despite several interventions targeting racial and ethnic minority populations, there are several other medically underserved populations that were not represented in the review. Notably, we found no studies reporting on interventions focused on Native Americans or Alaska Natives. Importantly, the results also highlighted a lack of geographic diversity. We found no studies reporting BCC interventions in rural areas located in Midwestern states. Given our results, additional research on rural women in areas not included in existing BCC screening interventions could elucidate similarities and differences between those mentioned in this paper.
Our search also identified variability in the reporting of outcomes with some studies using absolute differences while others used relative differences. This difference in reporting outcomes may be important for those searching for viable interventions for their populations of interest. While some studies demonstrated the effectiveness of the intervention strategy, only one study reported the costs associated with intervention development or implementation. The inclusion of cost data can support development of novel interventions, adoption and/or modification of existing approaches, and subsequent implementation and scaling of proven interventions. An understanding of the financial and resource requirements of these interventions can effectively inform considerations for translating the programs to other settings and/or audiences.
We found multiple studies included a mention of the theoretical framework(s) that informed the interventions. However, few studies engaged deeply to describe which theories informed the different components of the interventions. A detailed description of how the theories were incorporated is especially necessary for the interventions that mentioned multiple theoretical frameworks and interventions with multiple components. We argue that a thorough discussion of how the theories were incorporated to inform their BCC screening program is critical to determine whether that intervention can be translated to other rural settings.
While this review provides important knowledge on the types of cancer screening interventions being implemented in rural communities, some limitations must be noted including restricting the search to PubMed/Medline database and publication bias. We limited our search to published studies and have not included findings that may be successful in practice, but not part of the peer-reviewed literature. Further, we were strict in our inclusion criteria and some studies that have examined BCC screening in the population of interest - but did not explicitly identify rurality as a characteristic of their study population - may have been missed. The variability in the study designs, geographic locations, data collection time points, and sample demographics of the interventions make cross-study comparison difficult.
Despite the noted limitations, our review has several strengths. This study provides a review of published literature relative to study design, demographic characteristics, cost-effectiveness analysis, and outcomes of BCC screening interventions in rural settings. This review is the first to focus on interventions designed to increase breast and/or cervical cancer screening uptake in rural populations.
In 2017, an estimated 23 million women aged 18 and older were living in rural areas and accounted for 14.3% of all women in the US.[42] The findings of our review suggest these women may be underserved by health efforts to increase BCC screening relative to the general population. Efforts have been made to implement interventions for BCC in the general population, however, our review revealed few interventions targeting rural women according to our inclusion and exclusion criteria. Our review adds to the previous literature documenting the dearth of targeted interventions to increase BCC screening in rural communities.[51] In addition, we have utilized the CPSTF recommended strategies as a framework to articulate the types of interventions being developed for these communities. Since there is existing evidence to support effective intervention approaches, future research and intervention development might focus on strategies endorsed and gaps identified by the CPSTF, specifically, interventions to increase community access and provider delivery of BCC screening in rural settings, as well as multicomponent interventions. Further, additional gaps documented in this review (limited geographic diversity, limited descriptions of theoretical frameworks, no interventions focused on repeat screening, and a dearth of cost data) can be addressed. Public health agencies, researchers, and partners have multiple opportunities to improve the design and implementation of effective BCC screening interventions in these often under resourced communities and reduce the attendant disparities.
Acknowledgements of Funding
All authors have read and approved the abstract. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC) or Oak Ridge Institute for Science and Education (ORISE). Ms. Atere-Roberts’ role as an author of this manuscript was initially supported by her appointment to the Research Participation Program at the CDC administered by ORISE through an interagency agreement between the U.S. Department of Energy and CDC. Ms. Atere-Roberts is currently affiliated with the University of North Carolina at Chapel Hill.
References
- 1.Doescher MP, Jackson JE (2009) Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. Journal of Public Health Management and Practice 15 (3):200–209. doi: 10.1097/PHH.0b013e3181a117da [DOI] [PubMed] [Google Scholar]
- 2.Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC (2017) Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties—United States. MMWR Surveillance Summaries 66 (14):1–13. doi: 10.15585/mmwr.ss6614a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mille JW, Royalty J, Henley J, White A, Richardson LC (2015) Breast and cervical cancers diagnosed and stage at diagnosis among women served through the National Breast and Cervical Cancer Early Detection Program. Cancer causes & control : CCC 26 (5):741–747. doi: 10.1007/s10552-015-0543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T (2005) Perceived barriers to health care access among rural older adults: A qualitative study. The Journal of Rural Health 21 (3):206–213. doi:doi: 10.1111/j.1748-0361.2005.tb00084.x [DOI] [PubMed] [Google Scholar]
- 5.Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P Challenges of rural cancer care in the United States. Oncology 29 (9):633–640 [PubMed] [Google Scholar]
- 6.Chan L, Hart LG, Goodman DC (2006) Geographic access to health care for rural Medicare beneficiaries. The Journal of Rural Health 22 (2):140–146. doi:doi: 10.1111/j.1748-0361.2006.00022.x [DOI] [PubMed] [Google Scholar]
- 7.Schoenberg NE, Studts CR, Hatcher-Keller J, Buelt E, Adams E (2013) Patterns and determinants of breast and cervical cancer non-screening among Appalachian women. Women Health 53 (6):552–571. doi: 10.1080/03630242.2013.809400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu L, Sabatino S, White M (2019. (In press)) Rural-urban and racial disparities in invasive cervical cancer incidence in the United States, 2010–2014. Preventing Chronic Disease; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Advisory Committee on Rural Health and Human Services (2019) Examining Rural Cancer Prevention and Control Efforts: Policy Brief and Recomendations to the Secretary doi:https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2019-Cancer-Control.pdf
- 10.Meissner HI, Breen N, Coyne C, Legler JM, Green DT, Edwards BK (1998) Breast and cervical cancer screening interventions: an assessment of the literature. Cancer Epidemiology Biomarkers & Prevention 7 (10):951–961 [PubMed] [Google Scholar]
- 11.Chan DNS, So WKW (2015) A systematic review of randomised controlled trials examining the effectiveness of breast and cervical cancer screening interventions for ethnic minority women. European Journal of Oncology Nursing 19 (5):536–553. doi: 10.1016/j.ejon.2015.02.015 [DOI] [PubMed] [Google Scholar]
- 12.Probst JC, Moore CG, Glover SH, Samuels ME (2004) Person and Place: The Compounding Effects of Race/Ethnicity and Rurality on Health. 94 (10):1695–1703. doi: 10.2105/ajph.94.10.1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ratcliffe M, Burd C, Holder K, Fields A (2016) Defining rural at the US Census Bureau. American community survey and geography brief:1–8 [Google Scholar]
- 14.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E (2018) Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology 18 (1):143. doi: 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CBJIjoe-bh (2015) Guidance for conducting systematic scoping reviews. 13 (3):141–146 [DOI] [PubMed] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine 169 (7):467–473. doi: 10.7326/M18-0850 %J Annals of Internal Medicine [DOI] [PubMed] [Google Scholar]
- 17.Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, Melillo S, Carvalho M, Taplin S, Bastani R, Rimer BK, Vernon SW, Melvin CL, Taylor V, Fernandez M, Glanz K (2012) Effectiveness of Interventions to Increase Screening for Breast, Cervical, and Colorectal Cancers: Nine Updated Systematic Reviews for the Guide to Community Preventive Services. American Journal of Preventive Medicine 43 (1):97–118. doi: 10.1016/j.amepre.2012.04.009 [DOI] [PubMed] [Google Scholar]
- 18.Gellert K, Braun KL, Morris R, Starkey V (2006) The Òhana Day Project: A community approach to increasing cancer screening. Preventing Chronic Disease 3 (3):A99. [PMC free article] [PubMed] [Google Scholar]
- 19.Bencivenga M, DeRubis S, Leach P, Lotito L, Shoemaker C, Lengerich EJ (2008) Community partnerships, food pantries, and an evidence-based intervention to increase mammography among rural women. The Journal of Rural Health 24 (1):91–95. doi: 10.1111/j.1748-0361.2008.00142.x [DOI] [PubMed] [Google Scholar]
- 20.Luque JS, Tarasenko YN, Reyes-Garcia C, Alfonso ML, Suazo N, Rebing L, Ferris DG (2017) Salud es Vida: A cervical cancer screening intervention for rural Latina immigrant women. Journal of Cancer Education 32 (4):690–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz ML, Tatum CM, Degraffinreid CR, Dickinson S, Paskett ED (2007) Do cervical cancer screening rates increase in association with an intervention designed to increase mammography usage? Journal of Women’s Health 16 (1):24–35. doi: 10.1089/jwh.2006.0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson B, Carosso EA, Jhingan E, Wang L, Holte SE, Byrd TL, Benavides MC, Lopez C, Martinez-Gutierrez J, Ibarra G, Gonzalez VJ, Gonzalez NE, Duggan CR (2016) Results of a randomized controlled trial to increase cervical cancer screening among rural Latinas. Cancer 123 (4):666–674. doi: 10.1002/cncr.30399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Falk D, Cubbin C, Jones B, Carrillo-Kappus K, Crocker A, Rice C (2016) Increasing breast and cervical cancer screening in rural and border Texas with friend to friend plus patient navigation. Journal of Cancer Education:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nuño T, Martinez ME, Harris R, García F (2011) A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.–Mexico border: a randomized controlled trial. Cancer Causes & Control 22 (3):367–374. doi: 10.1007/s10552-010-9705-4 [DOI] [PubMed] [Google Scholar]
- 25.Thompson B, Coronado G, Chen L, Islas I (2006) Celebremos la salud! a community randomized trial of cancer prevention (United States). Cancer Causes Control 17 (5):733–746 [DOI] [PubMed] [Google Scholar]
- 26.US Census Bureau (2010) Census regions and divisions of the United States. doi:https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf
- 27.U.S. Preventive Services Task Force (April 2018) Final Update Summary: Breast Cancer: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1?ds=1&s=breast. Accessed September 24, 2018 [Google Scholar]
- 28.U.S. Preventive Services Task Force (April 2018) Final update summary: Cervical cancer: Screening. U.S. Preventive Services Task Force. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1?ds=1&s=breast. Accessed September 24, 2018 [Google Scholar]
- 29.Oeffinger KC, Fontham EH, Etzioni R, et al. (2015) Breast cancer screening for women at average risk: 2015 guideline update from American Cancer Society. JAMA 314 (15):1599–1614. doi: 10.1001/jama.2015.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, Garcia FAR, Moriarty AT, Waxman AG, Wilbur DC, Wentzensen N, Downs LS, Spitzer M, Moscicki A-B, Franco EL, Stoler MH, Schiffman M, Castle PE, Myers ER (2012) American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA: A Cancer Journal for Clinicians 62 (3):147–172. doi: 10.3322/caac.21139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glanz K, Rimer BK, Viswanath K (2008) Health behavior and health education: theory, research, and practice. John Wiley & Sons. [Google Scholar]
- 32.Green LW, Kreuter MW (1993) Health promotion planning: An educational and ecological approach. New York: McGraw-Hill. [Google Scholar]
- 33.Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, Fiore C, Harlow LL, Redding CA, Rosenbloom D (1994) Stages of change and decisional balance for 12 problem behaviors. Health Psychology 13 (1):39. [DOI] [PubMed] [Google Scholar]
- 34.McGuire WJ (1984) Public communication as a stratey for inducing health-promoting behaviorial change. Preventive medicine. [DOI] [PubMed] [Google Scholar]
- 35.Bracht NF (1999) Health promotion at the community level: new advances, vol 15. Sage Publications. [Google Scholar]
- 36.Sheeran P, Orbell S (2000) Using implementation intentions to increase attendance for cervical cancer screening. Health Psychology 19 (3):283. [DOI] [PubMed] [Google Scholar]
- 37.Slater JS, Nim Ha C, Malone ME, McGovern P, Madigan SD, Finnegan JR, Casey-Paal AL, Margolis KL, Lurie N (1998) A Randomized Community Trial to Increase Mammography Utilization among Low-Income Women Living in Public Housing. Preventive Medicine 27 (6):862–870. doi: 10.1006/pmed.1998.0370 [DOI] [PubMed] [Google Scholar]
- 38.Community Preventive Services Task Force (2013) Increasing Cancer Screening: One-on-One Education for Clients. Guide to Community Preventive Services. https://www.thecommunityguide.org/sites/default/files/assets/Cancer-Screening-One-on-One-Education.pdf. Accessed September 24, 2018 [Google Scholar]
- 39.Sohl SJ, Moyer A (2007) Tailored interventions to promote mammography screening: A meta-analytic review. Preventive medicine 45 (4):252–261. doi: 10.1016/j.ypmed.2007.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.MR E, Randa S, Terry H, Michael R, VS W, James C, Thomas W, Jocelyn A, Richard W (2007) A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer 110 (9):2083–2091. doi:doi: 10.1002/cncr.23022 [DOI] [PubMed] [Google Scholar]
- 41.Baron RC, Rimer BK, Breslow RA, Coates RJ, Kerner J, Melillo S, Habarta N, Kalra GP, Chattopadhyay S, Wilson KM, Lee NC, Mullen PD, Coughlin SS, Briss PA (2008) Client-Directed Interventions to Increase Community Demand for Breast, Cervical, and Colorectal Cancer Screening: A Systematic Review. American Journal of Preventive Medicine 35 (1, Supplement):S34–S55. doi: 10.1016/j.amepre.2008.04.002 [DOI] [PubMed] [Google Scholar]
- 42.U.S. Department of Health and Human Services HRSA, Maternal and Child Health Bureau. (2013) Rural and Urban Women. Women’s Health USA 2013. [Google Scholar]
- 43.Community Preventive Services Task Force (2017) Multicomponent Interventions to Increase Cancer Screening – Breast Cancer. Accessed April 1, 2019
- 44.Administration HRaS Defining Rural Population. Health Resources and Services Administration (HRSA). https://www.hrsa.gov/rural-health/about-us/definition/index.html. Accessed September 24, 2018 [Google Scholar]
- 45.Wheeler SB, Davis MM (2017) “Taking the bull by the horns”: four principles to align public health, primary care, and community efforts to improve rural cancer control. The Journal of Rural Health 33 (4):345–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pollard K, Jacobsen LA (2012) The Appalachian Region: A data overview from the 2006–2010 American Community Survey Chartbook. Washington, DC. Appalachian Regional Commission, [Google Scholar]
- 47.The Appalachian Region. Appalachian Regional Commission. http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp. Accessed March 29, 2019 [Google Scholar]
- 48.Maps by topic: economic status. Appalachian Regional Commission. http://www.arc.gov/research/MapsofAppalachia.asp?F_CATEGORY_ID=1. Accessed March 29, 2019 [Google Scholar]
- 49.Zahnd WE, Jenkins WD, Mueller-Luckey GS (2017) Cancer mortality in the Mississippi Delta region: descriptive epidemiology and needed future research and interventions. 28 (1):315–328 [DOI] [PubMed] [Google Scholar]
- 50.Authority DR (2015) Today’s Delta 2.0. Clarksdale, MS: Delta Regional Authority. https://www.dra.gov/images/uploads/content_files/Todays_Delta_FINAL_print-w-borders.pdf. Accessed March 29, 2019 [Google Scholar]
- 51.Falk D (2018) A Mixed Methods Review of Education and Patient Navigation Interventions to Increase Breast and Cervical Cancer Screening for Rural Women. Social Work in Public Health 33 (3):173–186 [DOI] [PubMed] [Google Scholar]