Abstract
Introduction
Burnout syndrome is a major cause of decreased life quality, mental health, and productivity for physicians. It is strongly related to work overload and has been a scarcely studied topic in pediatric urology. During the COVID-19 pandemic, authorities’ recommendations have led to big changes in pediatric urology practice worldwide. This study aimed to evaluate the level of burnout in Ibero-American pediatric urologists (IPUs) during this pandemic.
Material and methods
A cross-sectional study was conducted by applying an electronic survey during the COVID-19 pandemic peak to members of the two major associations of pediatric urology in Ibero-America (the Ibero-American Society of Pediatric Urology [SIUP] and the Brazilian School of Pediatric Urology [BSPU]) to evaluate demographic, pre-pandemic, and pandemic data. Burnout levels were assessed using the Copenhagen Burnout Inventory (CBI) questionnaire.
Results
A response rate of 40% was obtained (182 out of 455 IPU respondents). Participants were from 14 different countries in Ibero-America and 75.4% were male. Data showed that during the pandemic there was a significant decrease in weekly workload, that is: > 40 h per week (h/w) (91.4%–44.6%, p < 0.001); and >6 h/w (94.9%–45.1%%, p < 0.001) in operating room time (ORT). Personal (Pe-BO), work-related (W-BO), and patient-related (Pa-BO) burnout levels among IPUs were 26.3%, 22.3%, and 7.4%, respectively (Summary table). An important difference by gender was seen, with women suffering more from the syndrome (odds ratio of 2.67 [95% confidence interval, 1.285.58; p = 0.013] for Pe-BO and OR of 3.26 [95% CI, 1.52–7.01; p = 0.004] for W-BO).
Conclusion
A significant decrease in workload for IPU during the pandemic was observed, as well as a low level of burnout syndrome during this time. However, the predominance of burnout in women found in this study is notable.
Summary table.
∗ = by Copenhagen Burnout Inventory questionnaire (CBI).
| Burnout Prevalence∗ | % | |
|---|---|---|
| Personal- related | 26.3 | |
| Work-related | 22.3 | |
| Patient-related | 7.4 | |
| Daily activities during COVID-19 pandemic | Pre pandemic | Pandemic |
| Working time >40 h by week | 91.4% | 44.6% |
| Surgical time >6 h by week | 94.9% | 45.1% |
∗= by Copenhagen Burnout Inventory questionnaire (CBI).
Burnout syndrome in pediatric urology: a perspective during the COVID-19 pandemic — Ibero-American Survey
Keywords: COVID-19, Pandemic, Pediatric urology, Mental health, Professional burnout
Abbreviations: pediatric urologists, (PU); Ibero-American pediatric urologists, (IPU); Sociedad Iberoamericana de Urología Pediátrica, (SIUP); the Brazilian School of Pediatric Urology, BSPU); Copenhagen Burnout Inventory questionnaire, (CBI); personal burnout, (Pe-BO); work-related burnout, (W-BO); patient-related burnout, (Pa-BO); hours/week, (h/w); operating room time, (ORT); emotional exhaustion, (EE); depersonalization, (DP); personal achievement, (PA); Maslach Burnout Inventory, (MBI); World Health Organization, (WHO)
Introduction
The term “burnout” has been used since 1970s to describe fatigue and loss of idealism and passion for a job, especially among human service workers [1]. Later, it was conceptualized as a psychological syndrome in response to chronic interpersonal stressors on the job. In 1981, three key dimensions were described according to the Maslach Burnout Inventory (MBI) [2]: 1) overwhelming emotional exhaustion (EE), which represents an individual stress dimension; 2) detachment from the job or depersonalization (DP), which represents an interpersonal context; and 3) a sense of ineffectiveness or personal achievement (PA), which represents self-evaluation [1].
Currently, the MBI has been highly criticized, mainly because the DP domain is considered a coping strategy and not a component of burnout itself. Moreover, low PA may develop independently from the others and could have other causes, such as long-term stress [3]. Therefore, EE is considered the most accurate domain to correctly evaluate burnout levels. Since 2005, the Copenhagen Burnout Inventory (CBI) questionnaire has better evaluated the syndrome [3], as it recognizes the core of burnout as physical and emotional exhaustion caused by long-term involvement in emotionally demanding situations, being referred to as personal burnout (Pe-BO). Furthermore, there are additional key features which are attributed to fatigue and exhaustion to specific domains or spheres in a person's life, such as work-related burnout (W-BO) and patient-related burnout (Pa-BO) [[3], [4], [5]].
It is recognized that physicians have a higher risk of burnout. A survey carried out in 2017 by the Mayo Clinic demonstrated that 45% of physicians had the syndrome, while in the general population this rate was 28% (odds ratio [OR] of 1.39 [95% CI, 1.26–1.54; P < 0.001] for burnout risk in physicians) [6].
Burnout syndrome is linked to important outcomes like job performance, productivity, and effectiveness. Considering the mental health aspect, it is related to anxiety and depression. Moreover, it could have a negative impact on colleagues, causing greater personal conflict and the spillover effect [1]. A strong relationship has been described between physicians with burnout and a higher risk of medical errors (OR 3.33, 95% CI, 2.35–3.25), worst safety, poorer quality of life, fatigue, depressive symptoms, or suicidal ideation [7]. Studies have also described an increased risk of patient safety incidents, poorer quality of care due to low professionalism, and reduced patient satisfaction [8].
By medical specialty, urologist's burnout reports are between 37% and 78% [6,9,10]. According to the study carried out by the Mayo Clinic, urology presented the seventh-highest rate among physicians and the second among surgical specialties [6]. Regarding pediatric surgery, moderate EE (75.3%) was reported [11] and associated with the lack of balance with little time available for family [12].
Weekly workload is a factor strongly related to burnout. It has been demonstrated that general workers who work >40 h/w and >60 h/w and have ORs of 1.58 and 2.29 (p < 0.01) were considered positive for burnout [13].
During the COVID-19 pandemic, declared by the World Health Organization (WHO) at the beginning of March 2020 [14], authorities worldwide made recommendations for the general public and medical practice to reduce the chance of infection or spreading. In pediatric urology, this meant big changes [[15], [16], [17]], with a significant reduction in the normal working practice, such as the number of surgeries and outpatient clinic visits, especially early in the coronavirus pandemic.
There is little evidence available in the literature for the burnout levels in pediatric urology practice, in particular considering the Ibero-American population and COVID-19 pandemic. Based on the hypothesis that the workload of IPUs decreased during the pandemic, this study aimed to assess their burnout levels during the pandemic.
Material and methods
A descriptive, cross-sectional study was conducted. A web survey was created using Google Forms® with restrictions to ensure that the questionnaire could be answered only once per participant, and distributed to a convenience sample of the members of the two largest pediatric urology associations in Ibero-America, the Ibero-American Society of Pediatric Urology (SIUP) and the Brazilian School of Pediatric Urology (BSPU). The survey was carried out for one month (epidemiological week 28–32/2020) during the first COVID-19 pandemic peak in the American continent. Participants signed an informed consent form before proceeding with the survey, which required answering all questions. Anonymous answers were preserved. Two versions of the questionnaire were prepared, one in Spanish (https://adobe.ly/3q5TDN1) and another in Brazilian Portuguese (https://adobe.ly/2Jdi3mD), using the respectively validated versions of the scales. Those respondents that declared to be inactive before the start of the pandemic, such as retirees, were asked not to answer the questionnaire and excluded.
The survey contained three domains: demographic and working data, mental health data (stress perception and sleep quality questionnaires), and burnout evaluation.
For this study, demographic data like age, country of residence, gender, medical specialty (considering that pediatric urology can be practiced by adult urologists or pediatric surgeons in Ibero-America), workplace (academic, non-academic hospitals, or both), and work team characteristics (alone, 1 to 3, or more than 3 pediatric urologists) were collected.
Daily pre-pandemic and pandemic practice information was acquired. Considering the standard workload to be 40 h a week, as established by the International Labour Organization Convention in 1935, participants were divided into three groups. These were <20 h/week (h/w), 20–40 h/w, and >40 h/w, being half, the standard, and more than the standard weekly working hours, respectively. Operation room time (ORT), the standard being 6 h, was also organized into three groups, i.e., <6 h/w, 6–12 h/w, and >12 h/w.
Respondents filled out the CBI questionnaire [4,5]. It works in three levels to measure Pe-BO, W-BO, and Pa-BO during the month of lockdown previous to the answering of the survey. Each item is weighted on a 1–5 interval scale, which means scores of 0, 25, 50, 75, and 100, respectively. A score greater than 50 for each level is considered positive for burnout [3]. That questionnaire was selected in response to the perceived limitations of the MBI, as it allows for a better evaluation of fatigue and exhaustion, symptoms considered to be the core of burnout [3]. Despite being used in 85.7% of the papers, only 50% used and interpreted the MBI questionnaire in a standard way [18].
Descriptive statistics were used for the qualitative variables, which are described as proportions. To compare the frequency distribution among the qualitative variables at two different moments, the McNemar test was used. A non-normal distribution was found in the quantitative variables, using the Shapiro–Wilk test, for which they were described in corresponding terms of median and confidence intervals. To evaluate associations, the OR was used. To assess the association among qualitative variables, the Chi-squared was calculated using Fisher's exact test. To determine the association with quantitative variables, the Kruskal–Wallis test was used and, when necessary, the Mann–Whitney U test was used as a posthoc test. Calculations were performed using the SPSS software (IBM SPSS Statistics for Windows, version 25.0. Armonk, NY: IBM Corp). This study was approved by the local Internal Review Board of the Porto Alegre Clinical Hospital (HCPA) under the number CAAE: 31645020.5.0000.5327.
Results
Out of 455 IPUs, 182 responded to the survey, meaning a response rate of 40%, and five (1.1%) were excluded due to work inactivity before the pandemic. Respondents were from 14 countries (Brazil 45.7%, Argentina 11.4%, Chile 10.9%, Mexico 9.7%, Colombia 8.6%, and others 13.7%) and mostly male (75.4%). The median age was 44 years old (32–56), with a 1:1 ratio between adult urologists and pediatric surgeons who practice pediatric urology. Eight participants (4.6%) were in training fellowship programs. Most of the respondents (62.3%) worked at both academic and non-academic hospitals, and 85.1% worked in a team with other PUs (Table 1 ).
Table 1.
Frequency distribution of demographics variables, total number of participants = 177; express in proportions = %; + = median (interquartile Q1-interquartile Q3); ∗ = Nicaragua 2.3%, US 1.7%, Ecuador 1.7%, Panama 1.1%, Republica Dominicana 0.6%, Paraguay 0.6%, Qatar 0.6%.
| N | % | ||
|---|---|---|---|
| Gender | Male | 132 | 75.4 |
| Age (years-old) + | 44 | (32–56) | |
| In training program | Fellowship | 8 | 4.6 |
| Country | Brazil | 80 | 45.7 |
| Argentina | 20 | 11.4 | |
| Chile | 19 | 10.9 | |
| Mexico | 17 | 9.7 | |
| Colombia | 15 | 8.6 | |
| Spain | 4 | 2.3 | |
| Other∗ | 20 | 11.4 | |
| Clinical Practice | Academic | 16 | 9.1 |
| Non-academic | 50 | 28.6 | |
| Combined | 109 | 62.3 | |
| Surgical specialty | Urology | 85 | 48.6 |
| Pediatric surgery | 90 | 51.4 | |
| Team group | Alone | 26 | 14.9 |
| Team 1–3 PU | 74 | 42.3 | |
| Team > 3 PU | 75 | 42.9 |
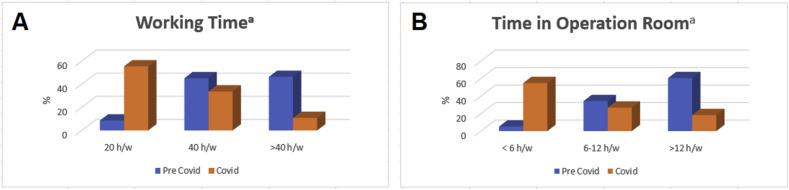
Exploring the working aspects, IPUs that, until March, had a workload of 20–40 h/w were 45%; >40 h/w, 46%; and <20 h/w, 8.6%. During the pandemic, their workload decreased significantly, with 55.4% of the participants working <20 h/w and just 10.9% working >40 h/w (p < 0.001) (Fig. 1 a).
Figure 1.
Distribution of hours spent by Iberoamerican pediatric urologists by activity. A) Number of hours at hospital by week. B) Number of hours at surgery by week. a = statistical significance p < 0.001 by the McNemar test.
The time spent in the ORT also decreased significantly. Comparing pre-pandemic times, until March, 5.1% of the participants spent <6 h/w in the ORT; 34.3%, 6–12 h/w; and 60.6%, >12 h/w. After the pandemic, this percentage was 54.9%, 26.9%, and 18.3%, respectively (p < 0.001) (Fig. 1b).
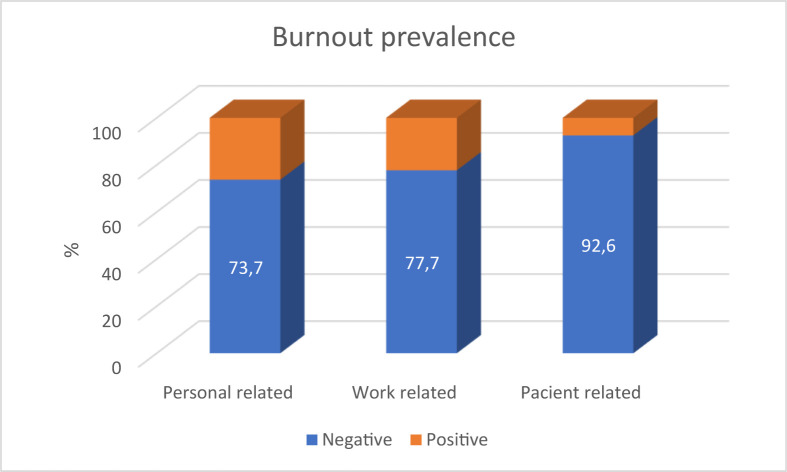
Burnout levels during the pandemic presented a non-normal distribution with a median of 33.33 (95% CI, 33.23–40.06) for the Pe-BO; 35.71 (95% CI, 36.56–42.22) for W-BO; and 20.83 (95% CI, 20.30–25.66) for Pa-BO levels. With a burnout prevalence of 26.3%, 22.3%, and 7.4% for Pe-BO, W-BO, and Pa-BO, respectively (Fig. 2 ). The respondents without burnout were 66.9%, while 15.4% were considered positive for one domain, 12.6% for two domains, and 5.1% for three domains.
Figure 2.
Distribution of burnout levels by CBI questionnaire in Ibero-American pediatric urologists during the pandemic.
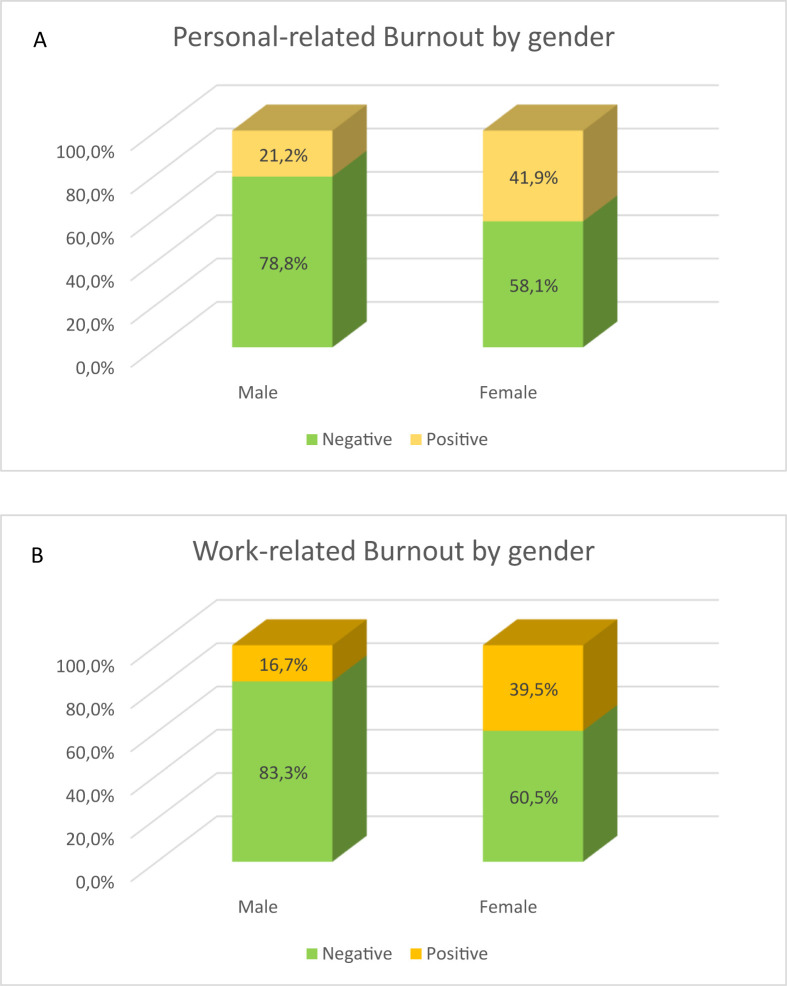
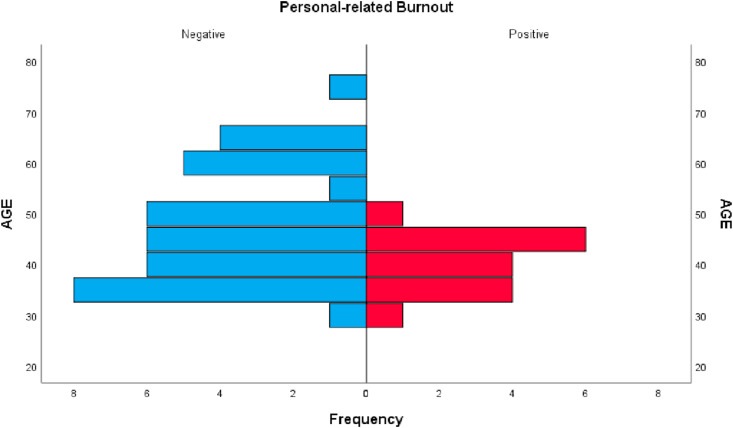
In the bivariate analysis of Pe-BO, a significant difference between genders was found: 21.2% (n = 22) of males vs. 41.9% (n = 17) of females were positive, with OR of 2.67 (95% CI, 1.28–5.58; p = 0.013) (Fig. 3 a). Considering age, despite not being a statistically significant difference, a tendency for positive Pe-BO was seen more frequently in the middle-age group (35–65 years old, p = 0.078) (Fig. 4 ). No differences were found regarding demographic and other working variables.
Figure 3.
Burnout levels by gender, using the CBI questionnaire. A) personal-related level, B) work-related level. ∗ = significant difference p < 0.05 by Chi squared correlation test.
Figure 4.
Personal-related burnout by the CBI questionnaire by age, with a tendency of p = 0.07 by Mann–Whitney U test.
For the W-BO domain, a significant difference between genders was also seen: 16.7% (n = 28) of males vs. 39.5% (n = 18) of females were positive, with an OR of 3.26 (95% CI, 1.52–7.01; p = 0.004) (Fig. 3b). Similar to the Pe-BO, no differences regarding other demographic and working variables were found. For the Pa-BO domain, no differences were identified for any of the variables. When applying the findings to a multivariate model, none of the variables proved to be significant in predicting burnout.
Discussion
There is little information in the literature regarding burnout in pediatric urology. It is important to note that the information available used the old questionnaire, the MBI; however, because of its limitations, the CBI questionnaire was applied following the trends on the subject. According to this questionnaire, results showed that 66.9% of respondents did not have burnout during the pandemic.
Data showed that 15.4% of the respondents had positive results for at least one domain, 12.6% for two, and 5.1% for three. A recent study on French PU, using the MBI questionnaire, found a burnout level as high as 48.6%, 21.4%, and 8.6% for one domain, two, and three domains, respectively [19]. Nevertheless, as previously explained, the EE component of the MBI questionnaire is used exclusively to try to approximate the findings of this work to those of previous reports.
This study found low levels of burnout in IPUs during the pandemic regarding all three domains evaluated, that is, 26.3% of respondents presented Pe-BO; 22.3%, W-BO; and 7.4%, Pa-BO. Considering the emotional exhaustion domain found in another work which used the MBI questionnaire, the risk of burnout prevalence was low, moderate, and high for 30%, 15%, and 20–30% of the participants, respectively [19]. A study carried out with the members of the American Academy of Pediatrics Urology, regarding the same domain, found that 15% of the subjects had moderate risk and 15%, high risk of burnout [20]. Finally, the 2016 American Urological Association (AUA) annual census reported approximately 25.5% of high-level burnout in pediatric urology, according to the EE domain [9]. The findings from this research could suggest a reduction in burnout levels during pandemic; however, further studies using the CBI questionnaire are required.
A significant reduction in the number of working and ORT hours of IPUs during the pandemic was demonstrated in this study. Previous works have shown that a higher risk of burnout is related to a workload of >60 h per week (h/w) [6]. Moreover, urologists who work >50 h/w had more burnout than those working <50 h/w (41.8% vs. 32.8%, respectively, p < 0.001). Even when comparing those who work more or less than 40 h/w, the difference was significant (42.3% vs. 32.4%, p < 0.001) [9]. These findings could probably explain why there has been a low burnout level since March 2020, supporting the theory that sees work overload as a strong predictor of burnout. Nonetheless, further studies are needed to test this theory.
At the beginning of the pandemic, before the epidemiological peak, a study considering the EE domain showed how the burnout level was significantly lower in frontline workers (13%) compared with non-frontline workers (39%) (p < 0.001) [21]. This changed during the pandemic peak, with the highest burnout level in the EE scale associated with frontline physicians, compared to non-frontline professionals (50% and 36%, respectively [p = 0.01]) [22]. Considering these data and taking into account that pediatric urology is a non-frontline specialty, the prevalence of burnout could seem even lower for this population. However, the questionnaire and population are different since a modified version of the MBI questionnaire was used and resident physicians, who are usually more susceptible to burnout, were also included. Another study, developed on this topic during the pandemic period among otolaryngologists, found rates similar to ours (burnout rate of 21.8% during the pandemic regarding the EE domain) [23], Despite using another questionnaire, theirs also included graduate specialists, non-frontline, so it is a population with greater similarities to the one studied in this research.
In contrast to other studies on burnout in pediatric urology [19,20], a significant difference between genders was found in this study, with females having a higher risk of burnout regarding Pe-Bo and W-BO levels. The female sample in this study was larger than in previous investigations, which probably allowed for the identification of the differences between genders. Other studies also found differences by gender in health workers during the pandemic [23,24].
Female Burnout is a topic that has been widely studied because it is constantly present in the general working population. A pre-pandemic meta-analysis taking into account the EE scale reported an 8% difference by gender (54% of women vs. 46% of men), suggesting that women are more likely to report the EE burnout component than men [25]. Some authors propose that this difference may be related to the occupation; however, it is not the only determining factor for the existence of the gap, as it can be found not only among physicians.
The analysis according to the place of origin has also shown differences. In the United States (US), a 12% difference in the EE of women and men was reported (56% and 44%, respectively). In contrast, there was a 4% difference in the EE of women and men from the European Union (EU) (52% and 48%, respectively) [25]. These data mean that the number of women suffering from EE in relation to men is more than double in the US compared to the EU. The author proposes that such differences should be due to work organizations, policy-making institutions, and governing bodies [25].
In this regard, there is no clear data in Latin America, but it has been shown that general workers women work 25 h/w more than men, and only half of them are paid for or otherwise profit from their work, with weak protection of rights and more gender inequality [26]; therefore, it is not a surprise that the gender gap in this study is higher (20.7%). Cultural and economic differences are believed to also influence these results; thus, for future assessments of the subject, other variables that allow for a thorough evaluation of these aspects should be studied.
For physicians, it was previously described in the literature that female gender is a risk factor for burnout syndrome (OR 1.329; 95% CI, 1.15–1.52; p < 0.001) [6]. For urologists, some studies revealed a significant difference between genders, with 24% of women reporting severe burnout in contrast to 10% of men (p < 0.001), with the strongest association resulting in females being four times more likely than males to report severe burnout (p = 0.02; 95% CI, 1.30–14.72) [10].
While European and North American studies did not find differences by age, a weak tendency for burnout to be more frequent in the middle age group (35–65 years old) was seen in this research. This has been described previously for physicians [6] and adult urologists, who present a 5–30% increased risk of burnout under 65 years of age [9]. Moreover, social and economic pressures of this middle-aged group generate more concerns about job performance, factors which may justify why the syndrome is more commonly diagnosed in this group than in extreme ages.
This survey did not find significant differences related to country, practice characteristics, specialty (urology vs. pediatric surgery), or the number of hours respondents spent working or in the operating room. The North American study reported no significant differences related to academic position, practice characteristics, workload, age, gender, or years in practice [20], while the European research did not find a clear association between age, gender, or being a trainee and the presence of burnout. Nevertheless, the European research found that working in university hospitals was associated with a higher risk of burnout in all three domains (EE, DP, and PA) than working in a non-teaching environment [19]. This association also was described for adult urologists [9].
Even though the EE domain is the most used to predict burnout, DP and PA were related to moderate and low levels of burnout, respectively, in PUs; however, as mentioned, it is still a debate if these domains actually evaluate correctly the burnout level. It is interesting to note, nonetheless, that as many as 34.6% of respondents who did not believe themselves to have signs of burnout tested positive for at least one domain [19].
Although this study had a good representative population sample of Ibero-Americans and was the largest research carried out regarding pediatric urology burnout syndrome in the world, some limitations were encountered, such as a smaller sample of females, probably an example of gender disparity in urology specialty and pediatric urology subspecialty.
Other potential limitations are the different questionnaires used and the interpretation made by each group in the burnout evaluation. To correct this, the EE scale was used to make the comparisons, as previously explained. However, the limitation in the use of questionnaires goes beyond pediatric urology, being an already identified problem. Currently, fewer studies use the full MBI questionnaire or mainly opt for modified versions [18]. Moreover, the CBI questionnaire is also an alternative that is not considered the gold standard, but when trying to overcome the difficulties, we decided to venture to apply this widely validated CBI questionnaire to our area.
Finally, the little information available for pediatric urology made it necessary the use of a wide range of studies to compare and discuss the findings of this work, allowing for a broad context. It is necessary to evaluate the policies applied to pediatric urology to prevent burnout and improve mental health, mainly in women.
Conclusions
The prevalence of burnout is a scarcely studied topic in pediatric urology. These are the results of the first study available on this topic during the COVID-19 pandemic. The findings regarding IPUs show a huge decrease in workload and hours in the operating room during the coronavirus pandemic, as well as low burnout levels during this period. A female predominance of the syndrome was demonstrated, with levels worse than those reported by European and North American studies, probably due to sociocultural characteristics.
Conflict of interest/funding
None.
Ethical approval
This study was submitted and approved by the local Internal Review Board at Hospital de Clínicas de Porto Alegre (HCPA) under the number CAAE: 31645020.5.0000.5327.
References
- 1.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.Maslach C., Jackson S.E. The measurement of experienced burnout. J Organ Behav. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 3.Kristensen T.S., Borritz M., Villadsen E., Christensen K.B. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19:192–207. doi: 10.1080/02678370500297720. [DOI] [Google Scholar]
- 4.Fonte CMS da. Universidade de Coimbra; 2011. Adaptação E validação para português do questionário de copenhagen burnout inventory (CBI) [Google Scholar]
- 5.Molinero-Ruiz E., Basart-Gómez Quintero H., Moncada-Lluis S. Validation OF the Spanish version OF the copenhagen burnout inventory questionnaire. Rev Esp Salud Publica. 2013;87:165–179. doi: 10.4321/S1135-57272013000200006. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt T.D., West C.P., Sinsky C., Trockel M., Tutty M., Satele D.V., et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94:1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Tawfik D.S., Profit J., Morgenthaler T.I., Satele D.V., Sinsky C.A., Dyrbye L.N., et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018;93:1571–1580. doi: 10.1016/j.mayocp.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panagioti M., Geraghty K., Johnson J., Zhou A., Panagopoulou E., Chew-Graham C., et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:1317–1330. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.North A.C., McKenna P.H., Fang R., Sener A., McNeil B.K., Franc-Guimond J., et al. Burnout in urology: findings from the 2016 AUA annual census. Urol Pract. 2018;5:489–494. doi: 10.1016/j.urpr.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Chouhan J.D., Anwar T., Jones A., Murray K.S. Burnout in the urology workforce: voluntary survey results in the United States. Urol Pract. 2020;7:566–570. doi: 10.1097/upj.0000000000000156. In press. [DOI] [PubMed] [Google Scholar]
- 11.Ja C., Mt J.L., Mm C. Study of “burnout” syndrome in Spanish pediatric surgeons. Cir Pediatr. 2002;15(2):73–78. [PubMed] [Google Scholar]
- 12.Katz A., Mallory B., Gilbert J.C., Bethel C., Hayes-Jordan A.A., Saito J.M., et al. State of the practice for pediatric surgery-career satisfaction and concerns. A report from the American pediatric surgical association task force on family issues. J Pediatr Surg. 2010;45 doi: 10.1016/j.jpedsurg.2010.05.011. 1975–82. [DOI] [PubMed] [Google Scholar]
- 13.Hu N.C., Chen J.D., Cheng T.J. The associations between long working hours, physical inactivity, and burnout. J Occup Environ Med. 2016;58:514–518. doi: 10.1097/JOM.0000000000000715. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO) 2020. Novel coronavirus (2019-nCoV) SITUATION REPORT - 1. [Google Scholar]
- 15.McCarthy L. 2020. Recommendations for paediatric urology practice during covid-19 epidemic. [Google Scholar]
- 16.Ribal M.J., Cornford P., Briganti A., Knoll T., Gravas S., Babjuk M., et al. vol. 12. Oliver W. Hakenberg; 2020. (EAU Guidelines Office Rapid Reaction Group: an organisation-wide collaborative effort to adapt the EAU guidelines recommendations to the COVID-19 era). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tur A.B., Prieto J.C., Gómez-Fraile A., Corbetta J.P. The effect of the Covid-19 Pandemic on pediatric urology. Int Braz J Urol. 2020;46:133–144. doi: 10.1590/S1677-5538.IBJU.2020.S112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rotenstein L.S., Torre M., Ramos M.A., Rosales R.C., Guille C., Sen S., et al. Prevalence of burnout among physicians a systematic review. JAMA, J Am Med Assoc. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harper L., Alshammari D., Ferdynus C., Kalfa N. Burnout amongst members of the French-speaking Society of Pediatric and Adolescent Urology (SFUPA). Are there specific risk factors? J Pediatr Urol. 2020 doi: 10.1016/j.jpurol.2020.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Au J., Elizondo R.A., Roth D.R. Surgeon burnout among American pediatric urologists. Urol Pract. 2017;4:264–268. doi: 10.1016/j.urpr.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Wu Y., Wang J., Luo C., Hu S., Lin X., Anderson A.E., et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in wuhan, China. J Pain Symptom Manag. 2020;60 doi: 10.1016/j.jpainsymman.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dimitriu M.C.T., Pantea-Stoian A., Smaranda A.C., Nica A.A., Carap A.C., Constantin V.D., et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.109972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Civantos Ba A.C., Yasmeen Ba, Changgee B., Aman C., et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck. 2020:1–13. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barello S., Palamenghi L., Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatr Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Purvanova R.K. Gender differences in burnout: a meta-analysis. J Vocat Behav. 2010;77:168–185. doi: 10.1016/j.jvb.2010.04.006. [DOI] [Google Scholar]
- 26.Bando R. Evidence-based gender equality policy and pay in Latin America and the Caribbean: progress and challenges. Lat Am Econ Rev. 2019;28 doi: 10.1186/s40503-019-0075-3. [DOI] [Google Scholar]