Abstract
The gut metabolite trimethylamine N-oxide (TMAO) at admission has a prognostic value in ST-elevation myocardial infarction (STEMI) patients. However, its sequential changes and relationship with long-term infarct-related outcomes after primary percutaneous coronary intervention (PCI) remain elusive. We delineated the temporal course of TMAO and its relationship with infarct size and left ventricular ejection fraction (LVEF) post-PCI, adjusting for the estimated glomerular filtration rate (eGFR). We measured TMAO levels at admission, 24 h and 4 months post-PCI in 379 STEMI patients. Infarct size and LVEF were determined by cardiac magnetic resonance 4 months after PCI. TMAO levels decreased from admission (4.13 ± 4.37 μM) to 24 h (3.41 ± 5.84 μM, p = 0.001) and increased from 24 h to 4 months (3.70 ± 3.86 μM, p = 0.026). Higher TMAO values at 24 h were correlated to smaller infarct sizes (rho = −0.16, p = 0.024). Larger declines between admission and 4 months suggestively correlated with smaller infarct size, and larger TMAO increases between 24 h and 4 months were associated with larger infarct size (rho = −0.19, p = 0.008 and rho = −0.18, p = 0.019, respectively). Upon eGFR stratification using 90 mL/min/1.73 m2 as a cut-off, significant associations between TMAO and infarct size were only noted in subjects with impaired renal function. In conclusion, TMAO levels in post-PCI STEMI patients are prone to fluctuations, and these fluctuations could be prognostic for infarct size, particularly in patients with impaired renal function.
Keywords: trimethylamine N-oxide (TMAO), ST-elevation myocardial infarction (STEMI), infarct size, left ventricular ejection fraction (LVEF), estimated glomerular filtration rate (eGFR)
1. Introduction
Preventative and therapeutic efforts have contributed to the decline of coronary heart disease (CHD)-related mortality in the past decades. Nevertheless, CHD remains the main global cause of death with rates exceeding 9 million deaths per year, thereby underscoring the importance of furthering our current understanding of this disease [1,2,3].
Atherosclerosis hallmarks CHD, and efforts are currently being directed at better understanding the manner through which this inflammatory process contributes to the development of CHD. Trimethylamine N-oxide (TMAO), a gut microbial product derived from L-carnitine and choline-rich foods, has gained substantial attention due to its atherogenic potential and its impact on CHD prognosis and all-cause mortality [4,5,6,7,8,9]. Indeed, recent endeavors have suggested that higher admission plasma TMAO values reflect a larger atherosclerotic burden and a higher risk of plaque rupture in patients presenting with ST-segment elevation myocardial infarction (STEMI) prior to undergoing percutaneous coronary intervention (PCI) [10,11]. Furthermore, higher systemic TMAO levels exhibited a dose-dependent relationship with increased risk of incident major adverse cardiac events (MACE) in patients presenting with acute coronary syndrome (ACS) [6].
While these aforementioned efforts have certainly delineated the value of pre-PCI TMAO levels in STEMI patients, the relevance of circulating TMAO in the post-PCI context remains elusive. Furthermore, data on the relationship between TMAO and infarct-related outcomes in STEMI patients, which could potentially explain the current established prognostic value of TMAO, is scant. For these reasons, the aim of the current study is to (i) delineate the temporal course of TMAO levels in STEMI patients who underwent primary PCI, and (ii) to outline the link between TMAO levels and infarct-related outcomes 4 months after the occurrence of STEMI.
2. Materials and Methods
2.1. Study Population and Design
Our study included all patients enrolled in the ‘Glycometabolic Intervention as Adjunct to Primary Coronary Intervention in ST Elevation Myocardial Infarction‘(GIPS-III) trial. This clinical trial aimed to delineate whether metformin treatment preserved left-ventricular ejection fraction (LVEF) in STEMI patients without diabetes [12]. In short, all patients admitted to the University Medical Center Groningen (UMCG) via the STEMI protocol between 1 January 2011 and 26 May 2013 were eligible for inclusion. Further inclusion criteria included an age of older than 18 years, presence of STEMI, and percutaneous coronary intervention (PCI) utilizing a minimum of one stent with a diameter of at least 3 mm which resulted in a post–intervention TIMI flow grade of 2 or 3 [12]. Major exclusion criteria included previous myocardial infarction, known diabetes, the need for coronary artery bypass graft surgery, severe renal dysfunction (creatinine > 177 μmol/L or eGFR < 30 mL/min/1.73 m2), and standard contraindications for magnetic resonance imaging (MRI) [12]. The GIPS-III trial showed that the use of metformin had no effect on infarct-related outcomes in STEMI patients after 4 months [12]. Further detail regarding the design and rationale of the GIPS-III trial can be found elsewhere [13]. Patients were treated according to the standard protocol of the UMCG for PCI. Periprocedural medications included heparin, acetylsalicylic acid, and P2Y12 receptor inhibitor. The GIPS-III trial was carried out in agreement with the declaration of Helsinki and approved by the UMCG Medical Ethical Committee (Groningen, the Netherlands, nr: 2010.077); informed consent was obtained from all participating subjects prior to their inclusion [12].
Out of the 1473 STEMI patients admitted to the UMCG between January 2011 and May 2013, 379 subjects befitted the inclusion criteria and were included in our analysis.
2.2. Data Collection
Standard physical examination parameters and routine laboratory values were measured at admission as per protocol. Patients returned to the outpatient clinic for follow-up at 2 weeks, 7 weeks, 4 months, and 1 year after discharge. Blood was sampled at these timepoints according to protocol to allow for the routine measurement of common laboratory parameters (i.e., cardiac enzymes) [12,13,14]. Additional blood samples for metabolic profiling (i.e., TMAO) were collected at admission, 24 h after PCI, and at 4 months after PCI and at follow-up points beyond the 4-month mark [12,13]. Samples of sufficient quality for TMAO measurement were only available at admission, 24 h and 4 months after PCI. eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration study equation [15]. The total number of subjects after eGFR stratification differs from the total cohort because of missing eGFR data at baseline from some subjects. The methods utilized for MRI measurement of LVEF and infarct size are described elsewhere [13].
Plasma TMAO was quantified using NMR by 1H-nuclear magnetic resonance (NMR) spectroscopy employing a Vantera® Clinical Analyzer (LabCorp, Raleigh, NC, USA) as previously reported [16]. To separate TMAO from other trimethylamine-containing species on the NMR spectrum, the pH was lowered to 5.3 by mixing TMAO specimens with a citrate buffer (3:1 v/v). The Carr-Purcell-Meiboom-Gill (CPMG) acquisition technique was used to obtain NMR spectra, after which TMAO was quantified from TMAO peaks using a non-negative least squares fitting algorithm and subsequently converted to concentration units (μM) through an empirically determined conversion factor. The TMAO assay has intra- and inter-assay coefficients of variation (CV%) that range from 4.3–10.3% and 9.8–14.5%, respectively [17].
2.3. Statistical Analysis
Baseline characteristics were expressed as means ± standard deviation when normally distributed, as medians with interquartile ranges when non-normally distributed, or as frequencies and percentages for categorical variables. Differences between groups were determined by Student t test, Mann–Whitney U test, Chi-square or Fisher’s exact test.
The temporal course of TMAO at admission and in the post-PCI context was studied using a mixed model with random intercepts followed by a pairwise comparison with a Bonferroni correction to delineate differences between specific timepoints. Additionally, we calculated Spearman rank correlation coefficients between TMAO values and infarct-related outcomes at and across the different time points. This analysis was reiterated twice after stratification of subjects based on their admission eGFR values (with 90 and 60 mL/min/1.73 m2 as two different cut-off values), seeing that renal impairment has been reported to confound the associations between TMAO and cardiovascular disease [18].
In line with Benjamin et al., a 2-sided p-value < 0.005 was considered to be statistically significant, whereas a p-value between 0.05 and 0.005 was considered to be suggestive [19]. All analyses were carried out using STATA version 16.0 (StataCorp LLC, College Station, TX, USA). All figures were generated using GraphPad Prism version 9.0.1 (GraphPad Software, LLC, San Diego, CA, USA).
3. Results
3.1. Study Cohort
Baseline characteristics are presented in Table 1. The median age at presentation was 59 years (interquartile range [IQR] 50.6–66.6 years), and 75% of all subjects were male. The median ischemic time was 161 min (IQR 109–250 min), and the median eGFR was 93 (IQR 80–106 mL/min/1.73 m2). Baseline characteristics stratified according to eGFR values at admission with 90 mL/min/1.73 m2 as cut-offs are presented in Table 1. The baseline characteristics of groups stratified by eGFR with cut-off point 60 mL/min/1.73 m2 can be found in Supplemental Table S1.
Table 1.
Baseline characteristics of GIPS-III subjects.
| Total | eGFR Groups | |||||
|---|---|---|---|---|---|---|
| Reduced | Normal | p-Value | ||||
| eGFR < 90 | eGFR≥90 | |||||
| n = 379 | n = 144 * | n = 188 * | ||||
| Age | 59.1 (50.6–66.5) | 63.7 (54.6–71.1) | 54.9 (48.4–62.7) | <0.001 | ||
| Female sex | 95 (25.1%) | 43 (29.9%) | 39 (20.7%) | 0.056 | ||
| BMI (kg/m2) | 26.6 (24.2–29.3) | 27.1 (25.1–29.6) | 26.2 (24.1–29.1) | 0.050 | ||
| Cardiovascular related history | ||||||
| Hypertension | 112 (29.6%) | 60 (41.7%) | 42 (22.3%) | <0.001 | ||
| Current smoking | 209 (55.1%) | 64 (44.4%) | 123 (65.4%) | <0.001 | ||
| Hypercholesterolemia | 239 (63.1%) | 83 (57.6%) | 126 (67.0%) | 0.079 | ||
| Stroke | 3 (0.8%) | 2 (1.4%) | 1 (0.5%) | 0.580 | ||
| Peripheral artery disease | 0 | 0 | 0 | - | ||
| Previous PCI | 4 (1.1%) | 2 (1.4%) | 2 (1.1%) | 1.00 | ||
| Blood Pressure | ||||||
| Systolic (mmHg) | 133 (120–147) | 133 (120–149) | 132 (120–146) | 0.750 | ||
| Diastolic (mmHg) | 83 (74–94) | 84 (72–93) | 83 (76–95) | 0.440 | ||
| Heart rate (beats/min) | 74.0 (64.0–85.0) | 72.0 (61.0–84.5) | 73.0 (65.0–84.0) | 0.460 | ||
| Ischemia time (min) | 161 (109–250) | 144 (107–203) | 170 (113–273) | 0.030 | ||
| Single vessel disease | 258 (68.1%) | 96 (66.7%) | 128 (68.1%) | 0.780 | ||
| Culprit vessel | ||||||
| LAD | 146 (38.5%) | 52 (36.1%) | 72 (38.3%) | |||
| LCX | 64 (16.9%) | 27 (18.8%) | 26 (13.8%) | |||
| RCA | 169 (44.6%) | 65 (45.1%) | 90 (47.9%) | |||
| Laboratory measures | ||||||
| CK-MB (U/L) | 16 (13–25) | 15 (13–22) | 17 (13–27) | 0.130 | ||
| Troponin (ng/L) | 50 (23–136) | 49 (26–136) | 50 (23–136) | 0.970 | ||
| NT-proBNP (ng/L) | 81 (40–200) | 90 (45–218) | 77 (37–172) | 0.120 | ||
| eGFR (mL/min/1.73 m2) | 93 (80–106) | 79 (68–85) | 104 (96–117) | <0.001 | ||
| TMAO (μM) | 3.10 (1.80–5.10) | 4.10 (2.50–6.10) | 2.80 (1.55–4.00) | <0.001 | ||
| Cholesterol (mmol/L) | 5.3 (4.7–6.0) | 5.2 (4.6–5.9) | 5.4 (4.8–6.2) | 0.026 | ||
| HDL cholesterol (mmol/L) | 1.1 (0.9–1.3) | 1.1 (0.9–1.3) | 1.1 (0.9–1.4) | 0.570 | ||
| LDL cholesterol (mmol/L) | 3.8 (3.2–4.4) | 3.6 (3.0–4.3) | 3.8 (3.3–4.6) | 0.006 | ||
| Triglycerides (mmol/L) | 0.9 (0.6–1.5) | 1.0 (0.7–1.4) | 0.9 (0.6–1.6) | 0.059 | ||
Data are expressed as median (interquartile range [IQR]) or as number (%). p-values were based on Student t test, Mann–Whitney U test, Chi-square, or Fisher’s exact test when appropriate. * The total number of subjects after eGFR stratification differs from the total cohort because of missing eGFR data at baseline from some subjects. Abbreviations: BMI—body mass index; CK-MB—myocardial band of creatine kinase; eGFR—estimated glomerular filtration rate; PCI—percutaneous coronary intervention; NT-proBNP—N-terminal pro-brain natriuretic peptide; TMAO—trimethylamine N-oxide; LAD—left anterior descending; LCX—left circumflex artery; RCA—right coronary artery; LDL—low-density lipoprotein; HDL—high-density lipoprotein.
3.2. Temporal Changes in TMAO
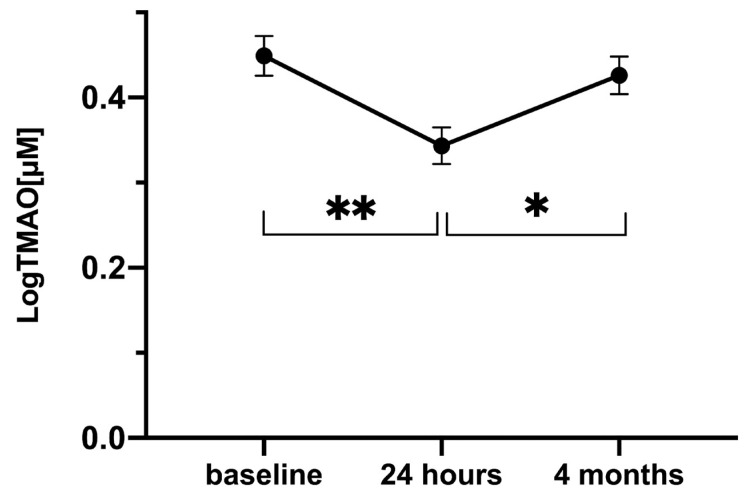
Figure 1 depicts the levels of TMAO at admission, 24 h, and at 4 months after PCI after logarithmic transformation. Mixed model analysis revealed that the mean TMAO concentration differed significantly between the three time points (p = 0.001). Post hoc pairwise comparison with an applied Bonferroni correction outlined that the reductions in TMAO levels between admission and 24 h and subsequent increase between 24 h and 4 months were statistically significant (from 0.45 ± 0.02 μM to 0.34 ± 0.02 μM, p = 0.001, and from 0.34 ± 0.02 μM to 0.43 ± 0.02 μM, p = 0.026, respectively).
Figure 1.
LogTMAO levels across time in subjects admitted via the STEMI protocol (n = 379). Mixed model analysis was utilized to contrast the temporal course of logTMAO between categorical groups. Data are presented as mean and standard error of the mean (SEM). * = p ≤ 0.05; ** = p ≤ 0.001 Abbreviations: TMAO—trimethylamine N-oxide, STEMI—ST-elevated myocardial infarction.
3.3. TMAO and Infarct-Related Outcomes
Spearman correlation analysis revealed that TMAO levels at the three timepoints, as well as their changes across such timepoints were not associated with LVEF. The gut metabolite did, however, exhibit suggestive associations with infarct size (Table 2). Specifically, higher TMAO levels at 24 h were associated with smaller infarct sizes, whereas larger TMAO declines between admission and 4 months were associated with smaller infarct sizes (rho = −0.16, p = 0.024 and rho = −0.19, p = 0.008, respectively). Furthermore, larger TMAO increases between 24 h and 4 months were correlated with larger infarct sizes (rho = −0.18, p = 0.019) (see Supplementary Table S3 for delta values). The baseline Spearman correlations between TMAO and MRI indices 4 months post-STEMI stratified by eGFR with cut-off point 60 mL/min/1.73 m2 can be found in Table S2.
Table 2.
Spearman correlations between TMAO and MRI indices 4 months post-STEMI.
| Infarct Size * | LVEF | |||
|---|---|---|---|---|
| Rho | p-Value | Rho | p-Value | |
| TMAO at admission | −0.12 | 0.064 | 0.04 | 0.583 |
| TMAO at 24 h | −0.16 | 0.024 | 0.06 | 0.353 |
| TMAO at 4 months | 0.05 | 0.437 | −0.02 | 0.729 |
| Delta TMAO (admission–24 h) | 0.01 | 0.861 | −0.02 | 0.770 |
| Delta TMAO (24 h–4 months) | −0.18 | 0.019 | 0.10 | 0.163 |
| Delta TMAO (admission–4 months) | −0.19 | 0.008 | 0.02 | 0.726 |
* Infarct size as % of left ventricular thickness. Abbreviations: TMAO—trimethylamine N-oxide; LVEF—left ventricular ejection fraction.
Some of these suggestive findings persisted and became significant after eGFR stratification with 90 mL/min/1.73 m2 as a cut-off value, but only in patients with an eGFR < 90 mL/min/1.73 m2 (Table 3). To illustrate, in the <90 mL/min/1.73 m2 eGFR group, the TMAO decline between admission and 4 months became significantly associated with infarct size (rho = −0.49, p < 0.001), and the TMAO increase between 24 h and 4 months became significantly associated with infarct size (rho = −0.35, p = 0.004). Additionally, these patients exhibited a positive suggestive correlation between larger increases in TMAO values between admission and 4 months and LVEF (rho = 0.25, p = 0.030). Comparing the correlations of the two different groups using a regression model with an interaction term (eGFR × TMAO) showed that the correlations for infarct size suggestively, and significantly, differed for the decline in TMAO levels between admission and 4 months, and the TMAO increase between 24 h and 4 months, respectively (p = 0.010; p < 0.001), and that the correlations for LVEF suggestively differed for delta TMAO levels between 24 h and 4 months (p = 0.013). Lastly, no significant correlations were observed between TMAO values and infarct-related outcomes when subjects were stratified using 60 mL/min/1.73 m2 as a cut-off value for eGFR.
Table 3.
Spearman correlations between TMAO and MRI indices 4 months post-STEMI stratified by eGFR.
| Reduced eGFR (eGFR < 90 mL/min/1.73 m2) n = 144 |
Normal eGFR (eGFR ≥ 90 mL/min/1.73 m2) n = 188 |
|||||||
|---|---|---|---|---|---|---|---|---|
| Infarct Size * | LVEF | Infarct Size * | LVEF | |||||
| Rho | p -Value | Rho | p -Value | Rho | p -Value | Rho | p -Value | |
| TMAO at admission | −0.28 | 0.016 | 0.20 | 0.068 | −0.03 | 0.779 | −0.004 | 0.968 |
| TMAO at 24 h | −0.20 | 0.107 | 0.13 | 0.244 | −0.17 | 0.081 | 0.008 | 0.935 |
| TMAO at 4 months | 0.24 | 0.031 | −0.10 | 0.352 | −0.12 | 0.221 | 0.09 | 0.351 |
| Delta TMAO (admission–24 h) | −0.11 | 0.421 | 0.08 | 0.537 | 0.10 | 0.312 | −0.05 | 0.638 |
| Delta TMAO (24 h–4 months) | −0.35 | 0.004 | 0.19 | 0.100 | 0.01 | 0.914 | −0.06 | 0.575 |
| Delta TMAO (admission–4 months) | −0.49 | <0.001 | 0.25 | 0.030 | 0.15 | 0.122 | −0.18 | 0.059 |
* Infarct size as % of left ventricular thickness. Abbreviations: TMAO = trimethylamine N-oxide; LVEF = left ventricular ejection fraction; eGFR = estimated glomerular filtration rate.
4. Discussion
We investigated the sequential changes of TMAO and its relationship to infarct-related outcomes before and after adjusting for kidney function in STEMI patients. The major findings of the present study were as follows: (i) TMAO levels significantly decreased within the first 24 h after PCI and returned to baseline values after 4 months, (ii) TMAO exhibited suggestive associations with infarct size but not with LVEF, and (iii) eGFR stratification with 90 mL/min/1.73 m2 as a cut-off value accentuated the association between TMAO and infarct size in subjects with eGFR < 90 mL/min/1.73 m2.
4.1. Admission TMAO Levels and Its Temporal Course
Plasma TMAO levels are prone to influence by an array of factors, including but not limited to gut microbiome composition, dietary choline and L-carnitine intake, and genetic heterogeneity of the hepatic flavin monooxygenase 3 enzyme responsible for the generation of TMAO from trimethylamine [4,20]. Indeed, previous investigations not only showed variation in TMAO levels across different cardiovascular disease cohorts but also across cohorts sharing the same cardiovascular disease pathology [6,21,22]. To illustrate, while investigating the prognostic potential of admission TMAO levels across two ACS cohorts, Xinmin and colleagues observed higher TMAO levels in the Cleveland cohort (median: 4.28 uM) compared to the Swiss cohort (2.87 μM) [6]. Interestingly, our current Dutch cohort (median: 3.1 μM) demonstrated closer affinity to the Swiss cohort admission TMAO level relative to the US cohort. While this observation could be attributed to genetic and/or dietary similarities between our cohort and the Swiss cohort as a result of their geographic proximity relative to the US cohort, we cannot draw such a definitive conclusion since both our study and that of Xinmin et al. lacked information regarding the dietary habits and genetic background of the subjects involved. In terms of studies exclusive to STEMI patients, admission median TMAO levels ranged from 2 μM to 6 μM, a range to which our present STEMI cohort conforms [11,23,24].
Our analysis is the first in (i) delineating changes in TMAO levels across three different timepoints and (ii) reporting such temporal patterns within the first 4 months in STEMI patients who underwent PCI. The drop in TMAO values within the first 24 h of admission in the present cohort indicates that TMAO is prone to acute changes in the post-PCI setting. We could not, however, pinpoint the precise reason behind such variation as subjects were not necessarily fasted, nor were they expected to follow a prespecified dietary regimen upon admission. Analyzing such dietary parameters is of central importance as TMAO has been shown to exhibit volatile changes in response to acute changes in dietary patterns. In a pilot study including healthy participants randomized to a 24 h water-only fast or a 24 h ad libitum fed diet, Washburn et al. reported a significant decrease of TMAO levels at the end of a fasted day, which subsequently returned to admission values within 24 h from the start of the refeeding phase [25].
The only other report describing the sequential change of TMAO after PCI in STEMI patients is that of Matsuzawa et al. In their cohort, TMAO significantly increased between admission (median: 5.63 μM) and 10 months (6.76 μM) [23]. While our present investigation found no significant difference between admission and 4 months, it is important to note that the TMAO change observed by Matsuzawa et al. was borderline significant (or rather suggestive when maintaining our definition of significance; p = 0.048). Furthermore, the difference in the temporal period used to measure changes in TMAO levels between their investigation (10 months) and ours (4 months) could also be a reason behind this discrepancy.
4.2. TMAO, Long-Term Infarct-Related Outcomes and Renal Function
In addition to the state of post-PCI perfusion, we analyzed the relationship between TMAO and infarct size, as well as LVEF, as both are important predictors of STEMI prognosis [26]. Studies conducted on murine models analyzed the relationship between TMAO and these infarct-related outcomes, but such investigations yielded conflicting results [27,28]. In humans, previous reports showed that TMAO levels were not associated with infarct size as determined by peak admission CK-MB and creatine phosphate values [20,29]. These findings are supported by the recent work of Zhou et al., in which it was shown that baseline TMAO levels did not significantly correlate with infarct size nor with LVEF at 30 days in patients presenting with a first anterior STEMI [30]. Our work extends these findings as it includes all STEMI patients irrespective of the culprit vessel involved and reports the relationship between TMAO (at and across three distinct timepoints) and infarct-related outcomes (at 4 months).
In our study, greater TMAO declines between admission and 4 months reflected smaller infarcts, and greater TMAO elevations between 24 h and 4 months were suggestively correlated to larger infarcts. It is established that the extent of inflammation—a process to which TMAO is linked—in the reperfusion phase is pivotal in determining the size of the infarct [28,31,32]. Such a process ensures the removal of necrotic debris, yet excessive inflammation in itself could expand the area of damage and, subsequently, the size of the infarct [31,32,33]. We hypothesize that greater elevations in TMAO levels between 24 h and 4 months could reflect the persistence of an overactive inflammatory response that spills into, and after, the reparative phase, thereby exacerbating the size of the infarct [33,34].
eGFR stratification showed that such associations became no longer suggestive in patients with normal kidney function (eGFR ≥ 90 mL/min/1.73 m2). In the impaired kidney function group (eGFR < 90 mL/min/1.73 m2), however, such stratification accentuated some of the suggestive associations into becoming significant, where greater TMAO declines between admission and 4 months became significantly associated with smaller infarcts and greater TMAO elevations between 24 h and 4 months became significantly correlated to larger infarcts. These findings are of relevance in as much as the relationship between TMAO and kidney function is a current topic of discussion. Not only is plasma TMAO mostly cleared by the kidney, but a “uremic environment”—characteristic of CKD patients—may also elevate plasma TMAO levels through promoting dysbiosis of the gut microbiome [35,36]. On the other end of the spectrum, TMAO has been shown to increase tubulointerstitial fibrosis and collagen deposition in murine models [35]. Thus, the question that remains in light of our findings and the nature of our post hoc analysis is whether TMAO’s association with infarct-related outcomes is simply confounded by low eGFR. This possibility is supported by the findings of the aforementioned works of Zhou et al., in which TMAO was not shown to be associated with infarct outcomes, and the work of Sonmez and colleagues, in which decreased eGFR (eGFR < 60 mL/min/1.73 m2) was shown to be associated with lower LVEF and greater infarct sizes [30,37]. The lack of significant relationships between TMAO and infarct-related outcomes in our <60 mL/min/1.73 m2 eGFR group does not necessarily refute the confounding possibility, seeing that such group comprised of only 14 subjects. In terms of LVEF and its association to TMAO (or changes thereof), we hypothesize that the lack of significant associations between the two variables to be the result of our study population, as well as the limitations associated with using LVEF to represent the myocardial function. GIPS-III subjects underwent rapid PCI, thereby limiting the extent of myocardial infarction and subsequent deterioration of LV function. In doing so, this rapid PCI approach could have limited the variation in LVEF amongst these patients, which could explain the lack of an association between LVEF and TMAO [12,13,14]. Furthermore, inherent to the use of LVEF as a marker of cardiac function and remodeling are physiological, technical, and clinical limitations [38]. In contrast to LVEF, infarct size measurement using MRI allows for a more accurate representation of the functional state of the myocardium and has been shown to be a superior prognostic predictor [39,40]. This could potentially explain why TMAO levels were significantly associated with infarct size but not with LVEF.
4.3. Limitations
Several limitations warrant consideration. First, the post hoc nature of our investigation limits our conclusion to being correlative rather than causative. Second, the GIPS-III trial was designed to test metformin in non-diabetic subjects presenting with a first STEMI. In the Dutch system, STEMI patients undergo rapid primary PCI, thereby limiting infarct size and preserving LVEF. Moreover, subjects with severe renal dysfunction at presentation were excluded from the GIPS-III trial. Therefore, our analysis is not free from selection bias, and conclusions should be drawn with caution in light of other STEMI cohorts. Furthermore, we did not prospectively collect information regarding the dietary patterns nor antibiotic use prior to or after PCI, both of which are key in influencing TMAO concentrations [4,41]. However, dietary intake at the coronary care unit (CCU) was standardized according to clinical protocol, and a retrospective review of medical charts revealed that no antibiotics were used by the patients included.
4.4. Future Perspectives
The fluctuations in TMAO levels after PCI urge future endeavors to investigate the reasons behind such changes in a controlled environment, taking into account the influence of diet, genetics, and antibiotic use on the gut metabolite. Additionally, more investigations are needed to clarify the relationship between TMAO, eGFR, and infarct-related outcomes.
5. Conclusions
In this investigation, we outlined the temporal course of TMAO in the post-PCI context of STEMI patients and associations between TMAO levels and infarct sizes. These associations were accentuated in terms of significance in patients with impaired renal function (eGFR < 90 mL/min/1.73 m2), thereby implying an interplay between renal dysfunction, higher TMAO values, and infarct sizes. The baseline Descriptive statistics of post-PCI medication stratified by eGFR with cut-off point 60 mL/min/1.73 m2 can be found in Table S4.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10235677/s1, Table S1: Baseline characteristics of 332 GIPS-III subjects stratified by eGFR (cut-off: 60 mL/min/1.73 m2). Table S2: Spearman correlations between TMAO and MRI indices 4 months post-STEMI stratified by eGFR (cut-off: 60 mL/min/1.73 m2). Table S3: Descriptive statistics of delta TMAO values across all eGFR strata. Table S4: Descriptive statistics of postPCI medication stratified by eGFR (cutoff: 90 mL/min/1.73 m2).
Author Contributions
Conceptualization, M.A.A. and H.E.G.; data curation, M.A.C. and E.G.; analysis and interpretation of data, M.A.A., F.M.P. and H.E.G.; writing—original draft preparation, M.A.A.; writing—review and editing, M.A.A., F.M.P., H.E.G., R.P.F.D., E.L. and P.v.d.H.; supervision, E.L., R.P.F.D. and P.v.d.H. All authors have read and agreed to the published version of the manuscript.
Funding
The GIPS-III trial was supported by a grant from ZonMw (The Netherlands Organization for Health Research and Development, The Hague), grant number 95103007. TMAO was measured at LabCorp, Morrisville, USA, at no cost.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Medical Ethical Committee of the University Medical Center Groningen (UMCG) (protocol code 2010.077 (13 August 2010)).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nowbar A.N., Gitto M., Howard J.P., Francis D.P., Al-Lamee R. Mortality From Ischemic Heart Disease. Circ. Cardiovasc. Qual. Outcomes. 2019;12:e005375. doi: 10.1161/CIRCOUTCOMES.118.005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herrington W., Lacey B., Sherliker P., Armitage J., Lewington S. Epidemiology of Atherosclerosis and the Potential to Reduce the Global Burden of Atherothrombotic Disease. Circ. Res. 2016;118:535–546. doi: 10.1161/CIRCRESAHA.115.307611. [DOI] [PubMed] [Google Scholar]
- 3.Nichols M., Townsend N., Scarborough P., Rayner M. Cardiovascular disease in Europe 2014: Epidemiological update. Eur. Heart J. 2014;35:2950–2959. doi: 10.1093/eurheartj/ehu299. [DOI] [PubMed] [Google Scholar]
- 4.Wang Z., Klipfell E., Bennett B.J., Koeth R., Levison B.S., Dugar B., Feldstein A.E., Britt E.B., Fu X., Chung Y.M., et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63. doi: 10.1038/nature09922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Senthong V., Wang Z., Li X.S., Fan Y., Wu Y., Tang W.H.W., Hazen S.L. Intestinal microbiota-generated metabolite Trimethylamine-N-oxide and 5-year mortality risk in stable coronary artery disease: The contributory role of intestinal microbiota in a COURAGE-like patient cohort. J. Am. Heart Assoc. 2016;5:e002816. doi: 10.1161/JAHA.115.002816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X.S., Obeid S., Klingenberg R., Gencer B., Mach F., Räber L., Windecker S., Rodondi N., Nanchen D., Muller O., et al. Gutmicrobiota-dependent trimethylamine N-oxide in acute coronary syndromes: A prognostic marker for incident cardiovascular events beyond traditional risk factors. Eur. Heart J. 2017;38:814–824. doi: 10.1093/eurheartj/ehw582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gruppen E.G., Garcia E., Connelly M.A., Jeyarajah E.J., Otvos J.D., Bakker S.J.L., Dullaart R.P.F. TMAO is Associated with Mortality: Impact of Modestly Impaired Renal Function. Sci. Rep. 2017;7:13781. doi: 10.1038/s41598-017-13739-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flores-Guerrero J.L., van Dijk P.R., Connelly M.A., Garcia E., Bilo H.J.G., Navis G., Bakker S.J.L., Dullaart R.P.F. Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59) J. Clin. Med. 2021;10:2269. doi: 10.3390/jcm10112269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flores-Guerrero J.L., Post A., van Dijk P.R., Connelly M.A., Garcia E., Navis G., Bakker S.J.L., Dullaart R.P.F. Circulating trimethylamine-N-oxide is associated with all-cause mortality in subjects with nonalcoholic fatty liver disease. Liver Int. 2021;41:2371–2382. doi: 10.1111/liv.14963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhaoxue S., Hongbing Y. Association of Circulating Trimethylamine N-Oxide With Coronary Atherosclerotic Burden in Patients With St-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2019;73:6. doi: 10.1016/S0735-1097(19)30615-1. [DOI] [PubMed] [Google Scholar]
- 11.Tan Y., Sheng Z., Zhou P., Liu C., Zhao H., Song L., Li J., Zhou J., Chen Y., Wang L., et al. Plasma trimethylamine N-oxide as a novel biomarker for plaque rupture in patients with ST-segment-elevation myocardial infarction. Circ. Cardiovasc. Interv. 2019;12:e007281. doi: 10.1161/CIRCINTERVENTIONS.118.007281. [DOI] [PubMed] [Google Scholar]
- 12.Lexis C.P.H., Van Der Horst I.C.C., Lipsic E., Wieringa W.G., De Boer R.A., Van Den Heuvel A.F.M., Van Der Werf H.W., Schurer R.A.J., Pundziute G., Tan E.S., et al. Effect of metformin on left ventricular function after acute myocardial infarction in patients without diabetes: The GIPS-III randomized clinical trial. JAMA J. Am. Med. Assoc. 2014;311:1526–1535. doi: 10.1001/jama.2014.3315. [DOI] [PubMed] [Google Scholar]
- 13.Lexis C.P.H., Van Der Horst I.C.C., Lipsic E., Van Der Harst P., Van Der Horst-Schrivers A.N.A., Wolffenbuttel B.H.R., De Boer R.A., Van Rossum A.C., Van Veldhuisen D.J., De Smet B.J.G.L. Metformin in non-diabetic patients presenting with st elevation myocardial infarction: Rationale and design of the glycometabolic intervention as adjunct to primary percutaneous intervention in st elevation myocardial infarction (gips)-iii trial. Cardiovasc. Drugs Ther. 2012;26:417–426. doi: 10.1007/s10557-012-6413-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Groot H.E., Karper J.C., Lipsic E., van Veldhuisen D.J., van der Horst I.C.C., van der Harst P. High-sensitivity C-reactive protein and long term reperfusion success of primary percutaneous intervention in ST-elevation myocardial infarction. Int. J. Cardiol. 2017;248:51–56. doi: 10.1016/j.ijcard.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 15.Posma R.A., Lexis C.P.H., Lipsic E., Nijsten M.W.N., Damman K., Touw D.J., van Veldhuisen D.J., van der Harst P., van der Horst I.C.C. Effect of Metformin on Renal Function After Primary Percutaneous Coronary Intervention in Patients Without Diabetes Presenting with ST-elevation Myocardial Infarction: Data from the GIPS-III Trial. Cardiovasc. Drugs Ther. 2015;29:451–459. doi: 10.1007/s10557-015-6618-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia E., Wolak-Dinsmore J., Wang Z., Li X.S., Bennett D.W., Connelly M.A., Otvos J.D., Hazen S.L., Jeyarajah E.J. NMR quantification of trimethylamine-N-oxide in human serum and plasma in the clinical laboratory setting. Clin. Biochem. 2017;50:947–955. doi: 10.1016/j.clinbiochem.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flores-Guerrero J.L., Osté M.C.J., Baraldi P.B., Connelly M.A., Garcia E., Navis G., Bakker S.J.L., Dullaart R.P.F. Association of circulating trimethylamine n-oxide and its dietary determinants with the risk of kidney graft failure: Results of the transplantlines cohort study. Nutrients. 2021;13:262. doi: 10.3390/nu13010262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jia J., Dou P., Gao M., Kong X., Li C., Liu Z., Huang T. Assessment of Causal Direction Between Gut Microbiota—Dependent Metabolites and Cardiometabolic Health: A Bidirectional Mendelian Randomization Analysis. Diabetes. 2019;68:1747–1755. doi: 10.2337/db19-0153. [DOI] [PubMed] [Google Scholar]
- 19.Benjamin D.J., Berger J.O., Johannesson M., Nosek B.A., Wagenmakers E.-J., Berk R., Bollen K.A., Brembs B., Brown L., Camerer C., et al. Redefine statistical significance. Nat. Hum. Behav. 2018;2:6–10. doi: 10.1038/s41562-017-0189-z. [DOI] [PubMed] [Google Scholar]
- 20.Bennett B.J., Vallim T.Q.D.A., Wang Z., Shih D.M., Meng Y., Gregory J., Allayee H., Lee R., Graham M., Crooke R., et al. Trimethylamine-N-Oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013;17:49–60. doi: 10.1016/j.cmet.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schiattarella G.G., Sannino A., Toscano E., Giugliano G., Gargiulo G., Franzone A., Trimarco B., Esposito G., Perrino C. Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: A systematic review and dose-response meta-analysis. Eur. Heart J. 2017;38:2948–2956. doi: 10.1093/eurheartj/ehx342. [DOI] [PubMed] [Google Scholar]
- 22.Heianza Y., Ma W., Manson J.A.E., Rexrode K.M., Qi L. Gut microbiota metabolites and risk of major adverse cardiovascular disease events and death: A systematic review and meta-analysis of prospective studies. J. Am. Heart Assoc. 2017;6:e004947. doi: 10.1161/JAHA.116.004947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsuzawa Y., Nakahashi H., Konishi M., Sato R., Kawashima C., Kikuchi S., Akiyama E., Iwahashi N., Maejima N., Okada K., et al. Microbiota-derived Trimethylamine N-oxide Predicts Cardiovascular Risk After STEMI. Sci. Rep. 2019;9:11647. doi: 10.1038/s41598-019-48246-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gencer B., Li X.S., Gurmu Y., Bonaca M.P., Morrow D.A., Cohen M., Bhatt D.L., Steg P.G., Storey R.F., Johanson P., et al. Gut Microbiota-Dependent Trimethylamine N-oxide and Cardiovascular Outcomes in Patients With Prior Myocardial Infarction: A Nested Case Control Study From the PEGASUS-TIMI 54 Trial. J. Am. Heart Assoc. 2020;9:e015331. doi: 10.1161/JAHA.119.015331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Washburn R.L., Cox J.E., Muhlestein J.B., May H.T., Carlquist J.F., Le V.T., Anderson J.L., Horne B.D. Pilot study of novel intermittent fasting effects on metabolomic and trimethylamine N-oxide changes during 24-hour water-only fasting in the FEELGOOD trial. Nutrients. 2019;11:246. doi: 10.3390/nu11020246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu E., Ortiz J.T., Tejedor P., Lee D.C., Bucciarelli-Ducci C., Kansal P., Carr J.C., Holly T.A., Lloyd-Jones D., Klocke F.J., et al. Infarct size by contrast enhanced cardiac magnetic resonance is a stronger predictor of outcomes than left ventricular ejection fraction or end-systolic volume index: Prospective cohort study. Heart. 2008;94:730–736. doi: 10.1136/hrt.2007.122622. [DOI] [PubMed] [Google Scholar]
- 27.Huc T., Drapala A., Gawrys M., Konop M., Bielinska K., Zaorska E., Samborowska E., Wyczalkowska-Tomasik A., Pączek L., Dadlez M., et al. Chronic, low-dose TMAO treatment reduces diastolic dysfunction and heart fibrosis in hypertensive rats. Am. J. Physiol.-Heart. Circ. Physiol. 2018;315:H1805–H1820. doi: 10.1152/ajpheart.00536.2018. [DOI] [PubMed] [Google Scholar]
- 28.Li X., Geng J., Zhao J., Ni Q., Zhao C., Zheng Y., Chen X., Wang L. Trimethylamine N-oxide exacerbates cardiac fibrosis via activating the NLRP3 inflammasome. Front. Physiol. 2019;10:866. doi: 10.3389/fphys.2019.00866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okamura A., Ito H., Iwakura K., Kurotobi T., Koyama Y., Date M., Higuchi Y., Inoue K., Fujii K. Clinical Implications of Distal Embolization During Coronary Interventional Procedures in Patients With Acute Myocardial Infarction. Quantitative Study With Doppler Guidewire. JACC Cardiovasc. Interv. 2008;1:268–276. doi: 10.1016/j.jcin.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 30.Zhou J., Yu S., Tan Y., Zhou P., Liu C., Sheng Z., Li J., Chen R., Zhao S., Yan H. Trimethylamine N-Oxide Was Not Associated With 30-Day Left Ventricular Systolic Dysfunction in Patients With a First Anterior ST-Segment Elevation Myocardial Infarction After Primary Revascularization: A Sub-analysis From an Optical Coherence Tomography R. Front. Cardiovasc. Med. 2020;7:613684. doi: 10.3389/fcvm.2020.613684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leoni G., Soehnlein O. (Re) solving repair after myocardial infarction. Front. Pharmacol. 2018;9:1342. doi: 10.3389/fphar.2018.01342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Puhl S.L., Steffens S. Neutrophils in Post-myocardial Infarction Inflammation: Damage vs. Resolution? Front. Cardiovasc. Med. 2019;6:25. doi: 10.3389/fcvm.2019.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu J., Wang H., Li J. Inflammation and inflammatory cells in myocardial infarction and reperfusion injury: A double-edged sword. Clin. Med. Insights Cardiol. 2016;10:79–84. doi: 10.4137/CMC.S33164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prabhu S.D., Frangogiannis N.G. The Biological Basis for Cardiac Repair After Myocardial Infarction: From Inflammation to Fibrosis. Physiol. Behav. 2017;176:139–148. doi: 10.1161/CIRCRESAHA.116.303577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang W.H.W., Wang Z., Kennedy D.J., Wu Y., Buffa J.A., Agatisa-boyle B., Li X.S., Levison B.S., Hazen S.L. Clinical Track (TMAO) Pathway Contributes to Both Development of Renal Insufficiency and Mortality Risk in Chronic Kidney Disease. Circ. Res. 2015;116:448–455. doi: 10.1161/CIRCRESAHA.116.305360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramezani A., Raj D.S. The Gut Microbiome, Kidney Disease, and Targeted Interventions. J. Am. Soc. Nephrol. 2014;25:657–670. doi: 10.1681/ASN.2013080905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sonmez O., Vatankulu M.A., Tasal A., Bacaksiz A., Ayhan S., Yazici H.U., Karakaya E., Ozdogru I., Aygul N., Ozdemir K., et al. Does estimated glomerular filtration rate have an effect on left ventricular function after ST-elevation myocardial infarction? Echocardiography. 2014;31:318–324. doi: 10.1111/echo.12359. [DOI] [PubMed] [Google Scholar]
- 38.Marwick T.H. Ejection Fraction Pros and Cons: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018;72:2360–2379. doi: 10.1016/j.jacc.2018.08.2162. [DOI] [PubMed] [Google Scholar]
- 39.Yan A.T., Shayne A.J., Brown K.A., Gupta S.N., Chan C.W., Luu T.M., Di Carli M.F., Reynolds H.G., Stevenson W.G., Kwong R.Y. Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality. Circulation. 2006;114:32–39. doi: 10.1161/CIRCULATIONAHA.106.613414. [DOI] [PubMed] [Google Scholar]
- 40.Roes S.D., Kelle S., Kaandorp T.A.M., Kokocinski T., Poldermans D., Lamb H.J., Boersma E., van der Wall E.E., Fleck E., de Roos A., et al. Comparison of Myocardial Infarct Size Assessed with Contrast-Enhanced Magnetic Resonance Imaging and Left Ventricular Function and Volumes to Predict Mortality in Patients With Healed Myocardial Infarction. Am. J. Cardiol. 2007;100:930–936. doi: 10.1016/j.amjcard.2007.04.029. [DOI] [PubMed] [Google Scholar]
- 41.Tang W.H.W., Wang Z., Levison B.S., Koeth R.A., Britt E.B., Fu X., Wu Y., Hazen S.L. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N. Engl. J. Med. 2013;368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.