ABSTRACT
Leprosy is an infectious and contagious disease affecting skin and nerves. The number of cases in individuals under 15 years old is one of the parameters used in Brazil as an indicator of endemic permanence of the disease and its continuous transmission. Rio Grande do Sul State, in Southern Brazil, is low-endemic to leprosy. However, the disease remains a public health problem. This is a retrospective, observational and analytical study of a historical series of new cases of leprosy in children under 15 years old diagnosed in the period from 2000 to 2019, in all health units in Rio Grande do Sul State. Seventy-seven new cases were notified. The male gender was predominant in 53.2% of the cases (n=41). The average age was 10.4 years (standard deviation of 2.9), with predominance of the age group between 10 and 15 incomplete years old. The most frequent operational classification was multibacillary, in 62.3% of cases (n=48), and the most common clinical form was borderline, in 38.9% of cases (n=28). The predominant disability degree in the sample was grade zero, in 80.0% of the cases (n=60), but in 4.0% (n=3) the grade assessed was 2. In 54.0% of cases (n=27), bacilloscopy was performed, with positive results in 36.0% (n=9) of the exams. Multibacillary cases, with physical disability and/or positive bacilloscopy, draws attention that that the diagnosis is frequently not made in early stages.
KEYWORDS: Leprosy, Public health, Children, Adolescents, Epidemiology
INTRODUCTION
Leprosy is an infectious disease mainly affecting skin and nerves, it has high infectivity and low pathogenicity 1 . The transmission occurs through the upper airways and contact between an untreated patient and a person with a predisposition to the disease 2 . The etiological agent of leprosy is the bacillus Mycobacterium leprae, which has slow growth, making the incubation period long, with an average of three to five years. However, in children, this period can be reduced to weeks 1 .
The late diagnosis of the disease is a potential factor for the generation of physical disability and emotional damage, affecting the patient’s quality of life 3 . Thus, the early diagnosis is essential, especially in individuals under 15 years old.
In Brazil, the World Health Organization guidelines are followed for operational treatment purposes. Thus, leprosy cases are classified as paucibacillary (PB) when they present up to five skin lesions, and as multibacillary (MB) when they present six or more skin lesions and/or there is a positive intradermal bacilloscopy (if it is possible to performthis exam) 4 . However, for patients who do not have visible skin lesions, such as the cases of primarily neural leprosy, and also in cases in which skin lesions only appear during treatment, the Ministry of Health indicates the use of the Madrid classification (1953): indeterminate (PB), tuberculoid (PB), borderline (MB) and lepromatous (MB) 5 leprosy.
For operational purposes, patients classified as indeterminate or tuberculoid are paucibacillary and must receive six doses of multidrug therapy within a maximum of nine months, while those classified as borderline or lepromatous are multibacillary and must receive 12 doses of multidrug therapy within a maximum of 18 months 5 . As a fundamental complementary exam for verifying neural integrity, a simplified neurological assessment is performed, which evaluates the face, upper and lower limbs, assigning a degree for the verified physical disabilities. Grade zero is characterized by the total preservation of sensitivity and strength in the regions evaluated, grade 1 is characterized by loss or decrease of sensitivity or strength in one of the evaluated regions, and grade 2 is characterized by visible deficiencies caused by leprosy, such as lagophthalmos, claws, bone resorptionand wounds 5 .
The number of cases in individuals under 15 years old is one of the parameters chosen in Brazil as an indicator of endemic permanence of the disease and its continuous transmission 6,7 . Between 2008 and 2016, the country recorded 301,322 cases of leprosy, of which 21,666 (7.2%) were in children under 15 years old. In this group, there was the presence of grade 2 physical disability in 2.7% of the cases. In the period from 2009 to 2018, Rio Grande do Sul State had an average detection rate of 1.20 cases per 100,000 inhabitants. Among children under 15 years old, the average rate of detection of the disease was 0.33 cases per 100,000 inhabitants in the same period, with 1.68 new cases diagnosed with grade 2 physical disability per 1 million inhabitants 8 .
Rio Grande do Sul State, over time, remains classified as a low-endemic region for new cases of leprosy 8 . However, the disease is still a public health problem in the State, mainly due to the late diagnosis in all age groups, a fact observed by the expressive number of new cases with physical disabilities at the time of diagnosis, which also suggests the occurrence of hidden cases 9-11 .
This study aims to present the trend of leprosy diagnosis, socioeconomic, clinical and epidemiological characteristics in individuals under 15 years old in Rio Grande do Sul State, Southern Brazil, in the period from 2000 to 2019.
MATERIALS AND METHODS
Retrospective, observational and analytical study of a historical series of new cases of leprosy in children under 15 years old, from 2000 to 2019, in all health units in Rio Grande do Sul State (32°1’60’’ South, 52°5’55’’ West). The research project was submitted to the Research Ethics Committee of the Hospital de Clinicas de Porto Alegre, and the Ethics Committee of the School of Public Health of Rio Grande do Sul (CAAE: 31959120.6.0000.5327/3195120.6.5312), being approved according to the process 4.075.445/4.121.621, respecting the resolutions 466/2012 and 510/2016 of the National Health Council that regulates research with human beings.
The data were obtained through the Notifiable Diseases Information System (SINAN), stored at the State Health Surveillance Center (CEVS) in Rio Grande do Sul State. The selection was carried out by the CEVS database, including all individuals under 15 years old diagnosed with leprosy in the period from 2000 to 2019. The variables of interest were sex, age, clinical form, operational classification, mode of entry of the new case, disability degree and bacilloscopy results.
Data were grouped by variables in an Excel 365 spreadsheet, distributed in columns, and the database was individually entered in the rows. The descriptive statistical measures used were frequencies, percentages, means and standard deviations. Bivariate analyses were made using the Fisher’s Exact Test for categorical variables, assuming a statistical significance level of 5% (bilateral). Analyses were conducted using the SPSS program Statistical Package for the Social Sciences 26 (SPSS) software (IBM, Armonk, NY, USA).
RESULTS
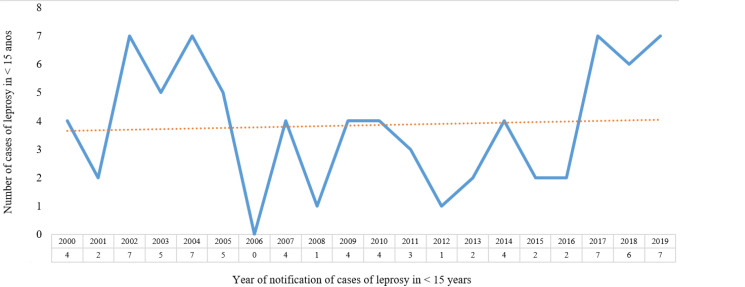
From 2000 to 2019, 4,233 new leprosy cases were reported, with 1.88% (n=77) of cases in individuals under 15 years old. In the surveyed period, the average was 3.8 cases/year. However, in the period from 2002 to 2005, the average was 6 cases/year, from 2006 to 2016 it was reduced to 2 cases/year, and from 2017 to 2019, it has increased again to 6.6 cases/year (Figure 1), suggesting a return to the 2000s level.
Figure 1. Number of notified leprosy cases in children under 15 years old in the period 2000 to 2019, Rio Grande do Sul, Brazil.
The predominance of the sample regarding gender was male for 53.2% of the cases (n=41), and the average age was 10.4 years (standard deviation=2.9). The predominant age group was between 10 and 15 years old at the time of diagnosis, in 63.6% (n=49) of the cases. The majority (77.4%) of the patients lived in urban areas of Rio Grande do Sul (Table 1). The predominant operational classification was multibacillary, in 62.3% of cases (n=48), and the most common clinical form was borderline, in 38.9% of cases (n=28). In four cases, there was no classification of the clinical form. Twenty percent of the sample already had a degree of physical disability at the time of diagnosis, and 18.0% (n=9) of the cases had positive bacilloscopy (Table 2).
Table 1. Socioeconomic characteristics of individuals under 15 years old diagnosed with leprosy from 2000 to 2019 in Rio Grande do Sul, Brazil.
| Characteristic | number (total = 77*) | Percentage | |
|---|---|---|---|
| Sex | |||
| Male | 41 | 53.2 | |
| Female | 36 | 46.8 | |
| Age group (years) | |||
| 0 – 4 | 3 | 3.9 | |
| 5 – 9 | 25 | 32.5 | |
| 10 – 15 | 49 | 63.6 | |
| Ethnicity/skin color | |||
| White | 41 | 59.4 | |
| Black | 5 | 7.3 | |
| Mixed (black and white) | 23 | 33.3 | |
| Residence | |||
| Urban | 58 | 77.4 | |
| Rural | 16 | 21.3 | |
| Periurban | 1 | 1.3 | |
Total data may vary depending on the possibility of absent information.
Table 2. Clinical and epidemiological characteristics of individuals under the age of 15, diagnosed with leprosy in the period from 2000 to 2019, in Rio Grande do Sul, Brazil.
| Characteristic | number (total= 77*) | Percentage | |
|---|---|---|---|
| Operational classification | |||
| Paucibacillary | 29 | 37.7 | |
| Multibacillary | 48 | 62.3 | |
| Clinical form | |||
| Indeterminate | 16 | 22.2 | |
| Tuberculoid | 16 | 22.2 | |
| Borderline | 28 | 38.9 | |
| Lepromatous | 8 | 11.1 | |
| Unclassified | 4 | 5.6 | |
| Therapeutic scheme | |||
| Paucibacillary multidrug therapy | 30 | 39.5 | |
| Multibacillary multidrug therapy | 38 | 50.0 | |
| Substitute regimes | 8 | 10.5 | |
| Case entry mode | |||
| New case | 62 | 81.6 | |
| Transfer from another municipality | 8 | 10.5 | |
| Transfer from another State | 5 | 6.6 | |
| Transfer from another country | 1 | 1.3 | |
| Case detection mode | |||
| Forwarding | 17 | 27.0 | |
| Spontaneous demand | 14 | 22.2 | |
| Contact exams | 32 | 50.8 | |
| Degree of physical disability at the time of diagnosis | |||
| Zero degree | 60 | 80.0 | |
| Grade 1 | 12 | 16.0 | |
| Grade 2 | 3 | 4.0 | |
| Bacilloscopy | |||
| Positive | 9 | 18.0 | |
| Negative | 18 | 36.0 | |
| Not performed | 23 | 46.0 | |
Total data may vary depending on the possibility of missing information.
In the bivariate analysis, an association was found between the operational classification and the clinical form with the degree of physical disability (p <0.001). For bacilloscopy, no association was found (p = 1.000) (Table 3).
Table 3. Quantitative cross distribution with respect to the following characteristics: operational classification, clinical forms and bacilloscopy with degree of physical disability caused by leprosy, in the period 2000-2019, in Rio Grande do Sul, Brazil.
| Characteristic* | Degree of physical disability | p -value1 | ||
|---|---|---|---|---|
| Grade 0 n = 60 | Grade 1-2 n = 15 | |||
| Operational Classification | <0.001 | |||
| Paucibacillary | 29 (100) | 0 (0) | ||
| Multibacillary | 31 (67.4) | 15 (32.6) | ||
| Clinical Form | <0.001 | |||
| Indeterminate | 16 (100) | 0 (0) | ||
| Tuberculoid | 0 (0) | 0 (0) | ||
| Borderline | 28 (100) | 0 (0) | ||
| Lepromatous | 0 (0) | 8 (0) | ||
| Baciloscopy | 1.000 | |||
| Negative | 18 (100) | 0 (0) | ||
| Positive | 9 (100) | 0 (0) | ||
Fisher’s exact test;
Total data may vary depending on the possibility of missing information.
DISCUSSION
This study showed that, even in low-endemic regions for leprosy, occurrences in children under 15 years old are present and suggest the permanence of the disease as a public health problem in Brazil 8,9,12 . Some authors consider that it is essential to monitor cases in this population, as they reflect the spreading force of Mycobacterium leprae. In addition, this age group is the most vulnerable due to a continuous exposure to the etiological agent 13-15 .
The trend and intensity of the disease in the population under 15 years old is used as one of the main parameters for monitoring and determining the level of the bacterium circulation 13-15 to assess the endemic level in each region. In low endemic regions, this parameter is associated with the clinical form of the disease and the degree of physical disability and may also suggest undiagnosed cases in adults 10,11 . In previous studies, the authors have presented a rate between 2.9 up to 9 of hidden cases for each diagnosis made in children under 15 years old 9-11 .
In other studies carried out in Brazil, the average age at diagnosis was similar to that found here 16 . There was variation regarding sex and clinical forms, with some studies showing a predominance of females and multibacillary patients 16-18 , and others with a predominance of males and paucibacillary forms, especially the tuberculoid clinical form 19,20 .
The number of cases with physical disability and positive bacilloscopy found in our study suggests a late diagnosis. In other studies, there is a fluctuation in the percentage of cases with physical disability ranging from 9% to 23% and, in most of them, there is no report of bacilloscopy results 20-24 . When performed, its percentage varied from 10.3% to 23% of the total sample 20,22,25 . In our sample, this examination was performed in 54.0% (n=27) of the cases. If only this number is considered, the percentage with a positive result increases to approximately 33%, which is in accordance with other studies 26-28 . In Rio Grande do Sul State, bacilloscopy is performed only at the Leprosy Reference Center in Porto Alegre, the State capital. Due to the invasive nature of bacilloscopy, this exam is not performed frequently in the analyzed age group. Ruiz-Fuentes et al. 29 , in their study, showed that less than 4% of the cases had a degree of physical disability at the time of diagnosis, even though most cases were multibacillary.
In order to facilitate the diagnosis and treatment of leprosy, the Ministry of Health has determined the following guidelines: paucibacillary patients are those who have indeterminate or tuberculoid clinical forms and are treated with the paucibacillary therapeutic scheme. In contrast, multibacillary patients present the borderline or lepromatous clinical forms and are treated with the multibacillary therapeutic scheme 5 . In certain situations, it is possible to notice that the notifications inserted in SINAN do not allow the logical sequence indicated by the Ministry of Health to happen. Records with ignored fields or the excess of missing data are frequent and confuse or preclude the correct analysis according to the reality of each case 20 .
In the present study, a significant number of missing data was observed, in addition to inconsistent data with the treatment guidelines recommended by the Ministry of Health. For example, while 29 cases had the paucibacillary operational classification, the therapeutic scheme of these forms of leprosy was applied in at least 30 cases (Table 2). In the literature review, several studies were found with data in accordance with the diagnostic and treatment guidelines 20,22,23,25 . However, it is also possible to find studies in which diagnostic and treatment are not suitable 21,24 . Inadequate treatment deserves attention due to their potential to generate relapses.
About 81% (n=62) of the analyzed data were classified as “new cases”, and the examination of “household/social contacts” was the most frequent detection mode. Leprosy cases in individuals under 15 years old demonstrate that the disease remains latent and contaminating, indicating that it will continue to be a public health problem if more effective measures are not taken 14,16,17,19,20,25 .
Regarding the association of the operational classification with the degree of physical disability, there was a significant relationship (p < 0.001) for the presence of physical disability at the time of diagnosis in cases classified as multibacillary. In more robust studies in which the odds ratio was available, a ratio of 1.3 to 2.7 times was more likely to have grade 1 or 2 in multibacillary cases 26,27 . The sample of the present study indicates that, in order to avoid the presence of a degree of physical disability at the time of diagnosis, it is necessary to diagnose leprosy earlier to avoid cases classified as multibacillary 5 .
In the association of the clinical form with the degree of physical disability, it was found that the most severe cases of leprosy, the lepromatous forms, are also those with the greatest impairment (p < 0.001). Although it was not observed in the present study, the occurrence of physical disability in patients with borderline leprosy is also expected, as this is a group with the highest number of reactional outbreaks 30 . However, in low endemic regions and in cases in which late diagnosis occurs, it is possible to expect that these reactional outbreaks will not be noticed. This leads to the evolution of the disease to the most severe form and to the presence of physical disability. In addition, the occurrence of silent neuritis, which is not common in the age group studied, but which causes the appearance of physical disability, must also be considered 31,32 . The lack of perception of family members and health professionals regarding the early diagnosis of leprosy can also contribute to the significant result found in the studied sample.
Regarding bacilloscopy, no statistically significant association was found with the degree of physical disability in the sample (p = 1.000). Bacilloscopy is not routinely performed in the studied age group, in addition to being a complementary diagnostic test that often becomes unnecessary in view of the clinical manifestations present in cases of leprosy in children and adolescents 5 .
The present study showed that, despite Rio Grande do Sul State being historically a low endemic region, diagnoses of new cases in individuals under 15 years old that are multibacillary and present with a high average of physical disability continues to occur. These data are also found in studies in other regions of Brazil, showing that it is necessary to maintain active care and disease control measures, such as: promote training/updates on leprosy to health workers, so that they will think about the diagnosis of leprosy, especially in the early stages of the disease, and continue the annual monitoring of leprosy cases in all Brazilian States 16,19,20,33 . Especially in the studied age group, physical disabilities produce social isolation, discrimination and will negatively impact the adult life of these individuals. The early-stage disease diagnosis is essential to avoid these physical and psychological sequelae 23,34 . It is the government’s responsibility to deploy in its territory services capable of receiving, identifying, diagnosing, treating, and rehabilitating people affected by leprosy. In this scenario, those under 15 years old stand out since they are a source of infection and a confounding factor in terms of operational classification and clinical form, which may in the future become cases of recurrence.
CONCLUSION
We conclude that the occurrence of cases in individuals under 15 years old in multibacillary clinical forms with a degree of physical disability t and/or positive bacilloscopy, even if in small numbers, is enough reason to speculate that leprosy will continue to be present in Rio Grande do Sul State and even though, as it is a low-endemic region it will not be possible to avoid new cases in this age group.
Footnotes
FUNDING
None to declare.
REFERENCES
- 1.Bhat RM, Prakash C. Leprosy: an overview of pathophysiology. Interdiscip Perspect Infect Dis. 2012;2012:181089–181089. doi: 10.1155/2012/181089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kerr-Pontes LR, Barreto ML, Evangelista CM, Rodrigues LC, Heukelbach J, Feldmeier H. Socioeconomic, environmental, and behavioral risk factors for leprosy in North-east Brazil: results of a case-control study. Int J Epidemiol. 2006;35:994–1000. doi: 10.1093/ije/dyl072. [DOI] [PubMed] [Google Scholar]
- 3.Eidt LM. Ser hanseniano: sentimentos e vivências. Hansen Int. 2004;29:21–27. [Google Scholar]
- 4.World Health Organization . A Guide to eliminating leprosy as a public health problem. 2nd ed. Geneva: WHO; 1997. [cited 2021 Sep 20]. Action Programme for the Elimination of Leprosy. Available from: https://apps.who.int/iris/handle/10665/65311 . [Google Scholar]
- 5.Brasil . Departamento de Vigilância e Doenças Transmissíveis. Guia prático sobre a hanseníase. Brasília: Ministério da Saúde; 2017. [cited 2021 Sep 20]. Ministério da Saúde. Secretaria de Vigilância em Saúde. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/guia_pratico_hanseniase.pdf . [Google Scholar]
- 6.Lastória JC, Abreu MA. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects - Part 1. An Bras Dermatol. 2014;89:205–218. doi: 10.1590/abd1806-4841.20142450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodrigues LC, Lockwood DN. Leprosy now: epidemiology, progress, challenges, and research gaps. Lancet Infect Dis. 2011;11:464–470. doi: 10.1016/S1473-3099(11)70006-8. [DOI] [PubMed] [Google Scholar]
- 8.Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde Hanseníase 2020. [cited 2021 Sep 20];Bol Epidemiol. 2020 Esp:1–51. Available from: http://www.aids.gov.br/pt-br/pub/2020/boletim-epidemiologico-de-hanseniase-2020 . [Google Scholar]
- 9.Santos AS, Castro DS, Falqueto A. Fatores de risco para transmissão da hanseníase. Rev Bras Enferm. 2008;61:738–743. doi: 10.1590/s0034-71672008000700014. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues TS, Gomes LC, Cortela DC, Silva EA, Silva CA, Ferreira SM. Factors associated with leprosy in children contacts of notified adults in an endemic region of Midwest Brazil. J Pediatr (Rio J) 2020;96:593–599. doi: 10.1016/j.jped.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moet FJ, Pahan D, Schuring RP, Oskam L, Richardus JH. Physical distance, genetic relationship, age, and leprosy classification are independent risk factors for leprosy in contacts of patients with leprosy. J Infect Dis. 2006;193:346–353. doi: 10.1086/499278. [DOI] [PubMed] [Google Scholar]
- 12.Oliveira MB, Diniz LM. Leprosy among children under 15 years of age: literature review. An Bras Dermatol. 2016;91:196–203. doi: 10.1590/abd1806-4841.20163661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freitas LR, Duarte EC, Garcia LP. Trends of main indicators of leprosy in Brazilian municipalities with high risk of leprosy transmission, 2001-2012. BMC Infect Dis. 2016;16:472–472. doi: 10.1186/s12879-016-1798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos SD, Penna GO, Costa MC, Natividade MS, Teixeira MG. Leprosy in children and adolescents under 15 years old in an urban centre in Brazil. Mem Inst Oswaldo Cruz. 2016;111:359–364. doi: 10.1590/0074-02760160002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde [cited 2021 Sep 20];Situação epidemiológica e estratégias de prevenção, controle e eliminação das doenças tropicais negligenciadas no Brasil, 1995 a 2016 Bol Epidemiol. 2018 49:1–15. Available from: https://portalarquivos2.saude.gov.br/images/pdf/2018/novembro/19/2018-032.pdf . [Google Scholar]
- 16.Oppermann K, Salvi CS, Casali HM, Moraes PC, Cattani CA, Eidt LM. Aspectos epidemiológicos da hanseníase em menores de 15 anos, diagnosticados em um Centro de referência do sul do Brasil, entre 2007 e 2017: uma tendência à mudança na detecção de casos novos? Hansen Int. 2018;43:2366–2366. [Google Scholar]
- 17.Pinto AC, Wachholz PA, Silva GV, Masuda PY. Profile of leprosy in children under 15 years of age monitored in a Brazilian referral center (2004-2012) An Bras Dermatol. 2017;92:580–582. doi: 10.1590/abd1806-4841.20175676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreira SC, Batos CJ, Tawil L. Epidemiological situation of leprosy in Salvador from 2001 to 2009. An Bras Dermatol. 2014;89:107–117. doi: 10.1590/abd1806-4841.20142175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lima PM, Neto, Silva AR, Santos LH, Lima RJ, Tauil PL. Gonçalves EG. Leprosy in children under 15 years of age in a municipality in northeastern Brazil: evolutionary aspects from 2003 to 2015. Rev Soc Bras Med Trop. 2020;53:e20200515. doi: 10.1590/0037-8682-0515-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freitas BH, Cortela DC, Ferreira SM. Perfil sociodemográfico, clínico e epidemiológico da hanseníase em menores de quinze anos, Mato Grosso, Brasil. Hansen Int. 2017;42:12–18. [Google Scholar]
- 21.Monteiro LD, Mello FR, Miranda TP, Heukelbach J. Hansen’s disease in children under 15 years old in the state of Tocantins, Brazil, 2001-2012: epidemiological patterns and temporal trends. Rev Bras Epidemiol. 2019;22:e190047. doi: 10.1590/1980-549720190047. [DOI] [PubMed] [Google Scholar]
- 22.Lana FC, Fabri AC, Lopes FN, Carvalho AP, Lanza FM. Deformities due to leprosy in children under fifteen years old as an indicator of quality of the leprosy control programme in Brazilian municipalities. J Trop Med. 2013;2013:812793–812793. doi: 10.1155/2013/812793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ferreira IN, Alvarez RR. Hanseníase em menores de quinze anos no município de Paracatu, MG (1994 a 2001) Rev Bras Epidemiol. 2005;8:41–49. [Google Scholar]
- 24.Loiola HA, Aquino DM, Cardoso LS, Paiva MF, Coutinho NP, Dias RS. Perfil epidemiológico, clínico e qualidade de vida de crianças com hanseníase em um município hiperendêmico. Rev Enferm UERJ. 2018;26:e32251 [Google Scholar]
- 25.Franco MC, Macedo GM, Menezes BQ, Jucá FO, Neto, Franco AC, Xavier MB. Perfil de casos e fatores de risco para hanseníase, em menores de quinze anos, em município hiperendêmico da região norte do Brasil. Rev Paraense Med. 2014;28:29–40. [Google Scholar]
- 26.Santos AN, Costa AK, Souza JE, Alves KA, Oliveira KP, Pereira ZB. Epidemiological profile and tendency of leprosy in people younger than 15 years. Rev Esc Enferm USP. 2020;54:e03659. doi: 10.1590/S1980-220X2019016803659. [DOI] [PubMed] [Google Scholar]
- 27.Guerrero MI, Muvdi S, León CI. Retraso en el diagnóstico de lepra como factor pronóstico de discapacidad en una cohorte de pacientes en Colombia, 2000-2010. Rev Panam Salud Publica. 2013;33:137–143. doi: 10.1590/s1020-49892013000200009. [DOI] [PubMed] [Google Scholar]
- 28.Shumet T, Demissie M, Bekele Y. Prevalence of disability and associated factors among registered leprosy patients in all Africa Tb and Leprosy Rehabilitation and Training Centre (ALERT), Addis Ababa, Ethiopia. Ethiop J Health Sci. 2015;25:313–320. doi: 10.4314/ejhs.v25i4.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruiz-Fuentes JL, Castillo RR, Gascón LC, Pastrana F. Leprosy in children: a Cuban experience on leprosy control. BMJ Paediatr Open. 2019;3:e000500. doi: 10.1136/bmjpo-2019-000500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alves CJ, Barreto JA, Fogagnolo L, Contin LA, Nassif PW. Avaliação do grau de incapacidade dos pacientes com diagnóstico de hanseníase em serviço de dermatologia do estado de São Paulo. Rev Soc Bras Med Trop. 2010;43:460–461. doi: 10.1590/s0037-86822010000400025. [DOI] [PubMed] [Google Scholar]
- 31.Carneiro M, Possuelo LG, Valim AR. Neuropatia por hanseníase: atraso no diagnóstico ou um diagnóstico difícil? Cad Saude Publica. 2011;27:2069–2069. doi: 10.1590/s0102-311x2011001000020. [DOI] [PubMed] [Google Scholar]
- 32.Leite VM, Lima JW. Gonçalves HS. Neuropatia silenciosa em portadores de hanseníase na cidade de Fortaleza, Ceará, Brasil. Cad Saude Publica. 2011;27:659–665. doi: 10.1590/s0102-311x2011000400005. [DOI] [PubMed] [Google Scholar]
- 33.Dogra S, Narang T, Khullar G, Kumar R, Saikia UN. Childhood leprosy through the post-leprosy-elimination era: a retrospective analysis of epidemiological and clinical characteristics of disease over eleven years from a tertiary care hospital in North India. Lepr Rev. 2014;85:296–310. [PubMed] [Google Scholar]
- 34.Schneider PB, Freitas BH. Tendência da hanseníase em menores de 15 anos no Brasil, 2001-2016. Cad Saude Publica. 2018;34:e00101817. doi: 10.1590/0102-311X00101817. [DOI] [PubMed] [Google Scholar]