Objective
Many women reported changing or considering changing the location where they planned to give birth because of COVID-19, despite community births (births in birth centers and home births) in the United States being associated with increased patient-risk profiles, neonatal injury, and death.1 This study aimed to evaluate changes of place of births and risk profiles before (2019) and during (2020) the COVID-19 pandemic.
Study Design
This was a retrospective descriptive population-based cohort study that used the Centers for Disease Control and Prevention WONDER online natality online database for the years 2019 (before the pandemic) and 2020 (during the pandemic).2 We compared births in birth centers and home births with those in hospitals (births by midwives and births by others, such as doctors).
Results
The study population included 3,747,540 births in 2019 and 3,613,647 in 2020. Hospital births performed by other professionals except midwives dropped by 4.3% from 3,330,141 in 2020 to 3,185,997 in 2020, whereas hospital births performed by midwives dropped by 0.2% from 355,615 in 2019 to 354,997 in 2020 (Table ).
Table.
Risk profiles of out-of-hospital births
| Variable | Hospital (no MW) Percentage change (2020 vs 2019) |
Hospital (MW) Percentage change (2020 vs 2019) |
Home births intended Percentage change (2020 vs 2019) |
Home births not intended Percentage change (2020 vs 2019) |
Freestanding birth center Percentage change (2020 vs 2019) |
|---|---|---|---|---|---|
| Total | −4.3 (3,185,997 vs 3,330,141) | −0.2 (354,887 vs 355,615) | 20.2 (35,513 vs 29,550) | 9.0 (5508 vs 5053) | 9.2 (21,884 vs 20,043) |
| AMA (>35 y) | −2.1 (622,542 vs 635,636) | 3.6 (56,469 vs 54,522) | 22.4 (8896 vs 7270) | 12.8 (1025 vs 909) | 13.1 (4338 vs 3836) |
| Para 1 | −3.1 (1,223,034 vs 1,262,263) | 1.6 (137,790 vs 135,560) | 24.3 (6209 vs 4997) | 7.3 (936 vs 872) | 9.3 (7024 vs 6427) |
| Multiple pregnancy | −6.8 (113,560 vs 121,882) | −4.9 (1184 vs 1245) | 22.7 (281 vs 229) | 21.6 (124 vs 102) | 19.0 (50 vs 42) |
| Breech | −2.5 (145,266 vs 148,966) | −8.5 (804 vs 879) | 37.3 (324 vs 236) | 20.4 (112 vs 93) | −4.3 (67 vs 70) |
| Weight<2500 g | −4.6 (278,070 vs 291,610) | 0.7 (12,494 vs 12,403) | 21.0 (443 vs 366) | 7.8 (978 vs 907) | 3.9 (215 vs 207) |
| Apgar score of 0–3 | −3.9 (19,706 vs 20,514) | 1.7 (841 vs 827) | 35.9 (125 vs 92) | 3.6 (145 vs 140) | −19.6 (45 vs 56) |
| Apgar score of <7 | −2.5 (70,321 vs 72,132) | 2.5 (3906 vs 3810) | 18.5 (609 vs 514) | 4.0 (261 vs 251) | 16.5 (310 vs 266) |
| Previous cesarean delivery | −4.0 (545,010 vs 567,900) | −4.6 (11,532 vs 12,087) | 27.6 (1633 vs 1280) | 15.4 (270 vs 234) | 15.5 (498 vs 431) |
| Gestational age at <37 wk | −5.1 (345,298 vs 363,666) | −2.0 (15,728 vs 16,055) | 39.3 (351 vs 252) | 1.6 (1026 vs 1010) | 26.4 (134 vs 106) |
| Gestational age at >41 wk | −12.2 (139,112 vs 158,376) | −4.1 (32,274 vs 33,643) | 20.3 (7770 vs 6461) | 21.1 (298 vs 246) | 12.1 (4312 vs 3845) |
| Abnormal neonatal conditions | −3.2 (388,964 vs 401,946) | 0.6 (21,208 vs 21,091) | 24.4 (1279 vs 1028) | 6.26 (1103 vs 1038) | 6.9 (856 vs 801) |
| Range | −12.2 to −2.1 | −8.5 to 3.6 | 18.5–39.3 | 1.6–1.6 | −4.3 to 26.4 |
AMA, advanced maternal age; MW, Midwife.
Grünebaum. Worsening risk profiles of out-of-hospital births. Am J Obstet Gynecol 2022.
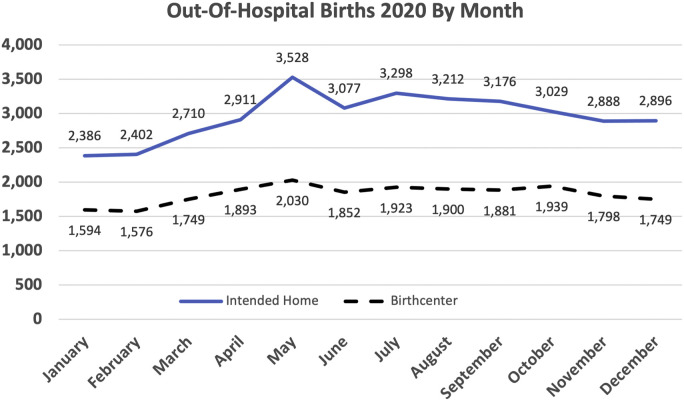
Overall, planned home births and births from freestanding birth centers increased by 20.2% and 9.2%, respectively, from 2019 to 2020. Out-of-hospital births peaked in May 2020, plateaued, and then dropped in October 2020 (Figure ). Risk profiles for hospital births decreased corresponding to the overall drop in births, but risk profiles of community births increased beyond their overall increase. Breech births among home births increased by 37.3%, preterm births increased by 39.3%, and 5-minute Apgar scores of 0 to 3 increased by 35.9% from 2019 to 2020.
Figure.
Monthly out-of-hospital births in 2020
Grünebaum. Worsening risk profiles of out-of-hospital births. Am J Obstet Gynecol 2022.
Conclusion
Our study showed that community births increased during the COVID-19 pandemic, consistent with the belief that community births seem more appealing to some women who view being in a hospital as more dangerous. However, our data showed a different result. Although intended home births increased by 20.2% during the COVID-19 pandemic, Apgar scores of 0 to 3 and preterm births increased by 35.9% and 39.3%, respectively, showing a worsening trend of an increase in many of the risk profiles at community births and confirming that risks in out-of-hospital births are even higher than previously reported.1 , 3
In our study, during the COVID-19 pandemic, 1 in 126 home births was twins, an increase from 1 in 156 home births; 1 in 110 home births was breech, an increase from 1 in 135 home births; 1 in 21 women had a previous cesarean delivery, an increase from 1 in 23 women4; and the 5-minute Apgar score of 0 to 3 (which according to the American College of Obstetricians and Gynecologists may be one of the first indications of encephalopathy and confers an increased relative risk of cerebral palsy) was 35.2 per 10,000 births, an increase from 29.7 per 10,000 births in 2016.2
During the COVID-19 pandemic, it was argued that community births offered improved safety compared with hospital births. However, our data showed a different result. In community births, safety was decreased and risks were increased.
In conclusion, neonatal morbidity and mortality and infection control were clinically superior in planned hospital births compared with out-of-hospital births as previously reported.5 Therefore, all healthcare providers should discourage planned out-of-hospital births and should recommend planned hospital births.5
Footnotes
The authors report no conflict of interest.
Supplementary Data
References
- 1.Grünebaum A., McCullough L.B., Orosz B., Chervenak F.A. Neonatal mortality in the United States is related to location of birth (hospital versus home) rather than the type of birth attendant. Am J Obstet Gynecol. 2020;223:254.e1–254.e8. doi: 10.1016/j.ajog.2020.01.045. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention About natality, 2016-2019 expanded. 2021. http://wonder.cdc.gov/natality-expanded-current.html Available at:
- 3.Grünebaum A., McCullough L.B., Chervenak F.A. Most intended home births in the United States are not low risk: 2016-2018. Am J Obstet Gynecol. 2020;222:384–385. doi: 10.1016/j.ajog.2019.11.1245. [DOI] [PubMed] [Google Scholar]
- 4.Grünebaum A., McCullough L.B., Brent R.L., Arabin B., Levene M.I., Chervenak F.A. Perinatal risks of planned home births in the United States. Am J Obstet Gynecol. 2015;212:350.e1–350.e6. doi: 10.1016/j.ajog.2014.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Grünebaum A., McCullough L.B., Bornstein E., Klein R., Dudenhausen J.W., Chervenak F.A. Professionally responsible counseling about birth location during the COVID-19 pandemic. J Perinat Med. 2020;48:450–452. doi: 10.1515/jpm-2020-0183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.