Abstract
To frame the substantial prevalence of type 2 diabetes (T2D) as a ‘Modern Preventable Pandemic’ (MPP) and present certain replicable policy lessons from the COVID-19 crisis to address it. A literature and policy review was performed to analyze data about the COVID-19 and T2D pandemics to establish their multi-factorial health, social, and economic impacts. With the global prevalence of T2D tripling in the last two decades, T2D has become an MPP largely due to modifiable human behaviors. Certain successful elements of the response to the COVID-19 pandemic provide important lessons that can be adapted for the growing T2D MPP. With proper education and access to resources, it is possible to mitigate the T2D MPP through focused government policies as illustrated by many of the lessons of the COVID-19 pandemic response. Without such government intervention, the T2D MPP will continue to grow at an unsustainable pace with enormous health, social and economic implications. Immediate action is necessary. The scale of the T2D pandemic warrants a robust response in health policy as outlined through eight coordinated efforts; the lessons of the COVID-19 crisis should be studied and applied to the T2D MPP.
Abbreviations: CVD, Cardiovascular disease; DPP, Diabetes Prevention Program; HIC, High income countries; LMIC, Low- and middle-income countries; MPP, Modern Preventable Pandemic; PCP, Primary care physician; T2D, Type 2 Diabetes; T1D, Type 1 Diabetes
Keywords: Public health, Prevention, Type 2 diabetes, Pandemic, Preventable Pandemic, Diabetes
1. The ‘pandemic’ awareness impact of COVID-19
Historically, pandemics have led to major advances in public health policy and healthcare. The COVID-19 pandemic beginning in 2019 did the same. While fraught with levels of failure and controversy, this crisis has led to an unprecedented coordinated global sprint among government, academia, and industry for diagnostics, therapeutics, and vaccines for COVID-19. Indeed, the onset of COVID-19 prompted historic urgent action at federal and state levels to waive regulations to increase hospital capacity, provide payment for remote care, remove barriers to testing and to regulatory approval of new drugs and diagnostics, and to greatly accelerate the testing approval of vaccines – to name a few.
As cases of COVID-19 surged in dramatic fashion, the dull roar of a global chronic disease pandemic - type 2 diabetes (T2D) – has continued in the background. Over 34 million Americans have diabetes, 90–95% of whom have T2D, and 88 million American adults - about 1 in 3 - have prediabetes (Centers for Disease Control and Prevention, 2020). Globally, 1 in 10 adults have diabetes (IDF Diabetes Atlas, 2021).
This article examines the multi-factorial public health T2D pandemic, framing it as a Modern Preventable Pandemic (MPP), and outlines eight key steps to address it, gleaned from recent lessons related to COVID-19.
2. The vast global scope of T2D
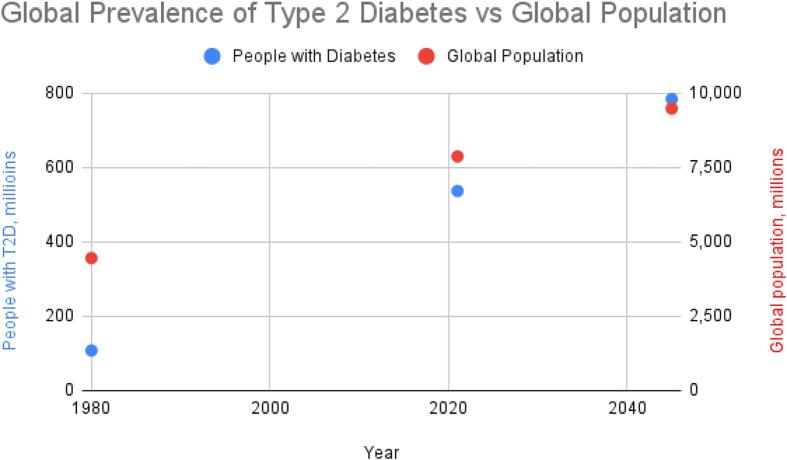
Globally, according to the International Diabetes Federation, an estimated 537 million adults were living with diabetes in 2021, compared to 108 million in 1980 (IDF Diabetes Atlas, 2021). Overall, the number of adults globally living with diabetes has more than tripled over the past 20 years, predicted to increase to 784 million by 2045 (Fig. 1) (IDF Diabetes Atlas, 2021).
Fig. 1.
Estimated future global prevalence of T2D using a statistical model (IDF Diabetes Atlas, 2021).
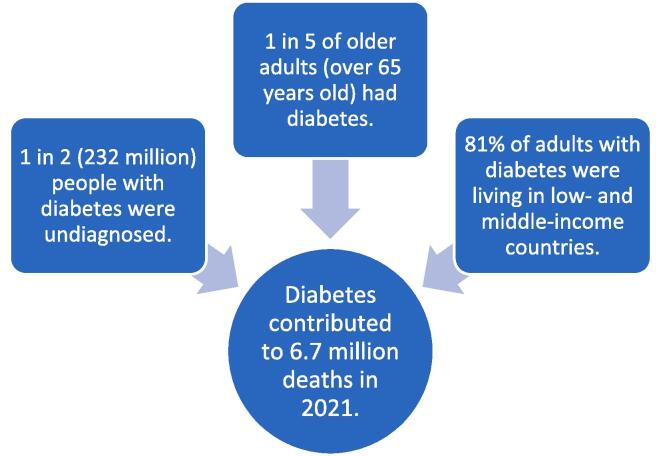
T2D was long regarded as a disease state associated with high income country (HIC) affluence. However, over the last several decades, profound changes in the quality, quantity, and source of food consumed in many low- and middle-income countries (LMICs) have led to a substantial prevalence of diabetes across all socio-economic levels of the population worldwide (Fig. 2).
Fig. 2.
Snapshot global impact of T2D (IDF Diabetes Atlas, 2021).
Moreover, the estimated number of people with T2D is proportional to population size, with the largest absolute numbers residing in China, India, and the U.S. Another 541 million people worldwide have impaired glucose tolerance and are considered pre-diabetic, an increased risk of developing T2D (IDF Diabetes Atlas, 2021).
3. Pandemic defined
The term “pandemic” has been fraught with definitional issues. The classical definition is the widespread occurrence of disease that crosses international boundaries and affects a significant number of people in excess of what normally might be expected in a geographical region (Kelly, 2011). The most impactful pandemics in human history are attributable to infectious disease outbreaks. Throughout history, infectious diseases have been the major cause of death. The rapid spread of infectious diseases required an urgent response and provided an effective exhortation to mobilize prevention and eradication. Antimicrobial therapies, immunizations, and public health measures in the 20th century reduced mortality from these infectious diseases by 99 percent (Fries, 1983).
4. The ‘Modern Preventable Pandemic’ (MPP)
How might we apply the traditional and new responses to a contagious, transmissible pandemic to this – what we call the T2D Modern Preventable Pandemic? With improvements in public health, prevention, and treatment of infectious diseases, mortality has been increasingly concentrated in older individuals with chronic conditions. The aging of the population has led to a dramatic increase in diseases of lifestyle, and the leading causes of death now are cardiovascular disease, cerebrovascular disease (Dal Canto et al., 2019), chronic lung disease, and neoplasms (Leading causes of death). Even while multiple kinds of therapy are reducing cardiovascular risk, adults with T2D are at 2–4 times increased risk for cardiovascular disease and have a 75% increase in mortality rate, of which cardiovascular disease accounts for the majority of the excess mortality (Dal Canto et al., 2019).
Applying the classical definition of a pandemic to modern diseases of lifestyle – recognizing that all pandemics have global health, social, and economic implications that vary in severity and duration - K.M. Venkat Narayan, a CDC epidemiologist, coined the term the “diabetes pandemic” (Narayan, 2005). T2D is a prime example of a growing pandemic, impacting more than 10% of the global population and costing hundreds of billions of dollars each year globally. Yet T2D is rarely regarded, let alone termed, as a “pandemic,” even though the health, social, and economic consequences are staggering. Indeed, it is important to set the context of T2D for purposes of discussion: the combination of increased consumption of ultra-processed foods and the convenience of modern life have greatly contributed to the increasing prevalence of T2D globally. Distinct from type one diabetes (T1D), an autoimmune disease unrelated to behaviors, lifestyle interventions form the basis for prevention of T2D (Srour et al., 2020). Further, T2D is often associated with major long-term complications including cardiovascular disease, end stage renal disease, and an increased risk, if not a potential etiology, for dementia and Alzheimer’s disease (Kuehn, 2020). The impact is broader than individual health: public health and the international economy are deeply affected by the global prevalence of T2D.
Ironically, while a devastating pandemic such as COVID-19 can only be considered “preventable” to the extent that virulent disease spread can be mitigated, T2D does not face this specific contagious hurdle.
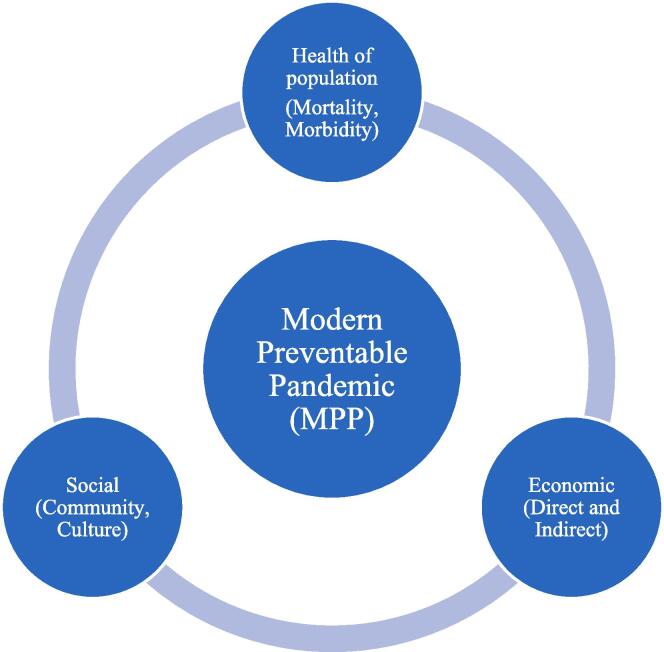
5. Diabetes as a global health, social, and economic MPP
The impact of interrelated health, social, and economic elements necessitate rapid mobilization of resources, as it becomes a matter of common interest to end a pandemic. This type of response is only possible when multiple sectors agree to prioritize a response, which is often necessary due to the multifactorial impact of a pandemic (Fig. 3). The growing global burden of T2D as an MPP warrants a proportional call to action.
Fig. 3.
Multi-factorial impact of modern preventable pandemics.
6. T2D is heavily underrated, underestimated, and preventable
Despite the alarming data surrounding T2D, diabetes often does not make major global disease state reports. For example, in the Kaiser Family Foundation’s 2019 primer for US global health policy, non-communicable diseases ranked tenth among the top 10 global health initiatives; diabetes was listed at the bottom of the non-communicable diseases category while diseases with fewer patients ranked higher (The US Government Engagement in Global Health, 2019). This report is yet another example of the vast global underestimation and lack of acknowledgement of the magnitude of the diabetes pandemic.
In an article in the peer-reviewed journal Clinical Diabetes and Endocrinology, Dr. Paul Z. Zimmet wrote:
The ‘Diabesity’ epidemic (obesity and type 2 diabetes) is likely to be the biggest epidemic in human history. Diabetes has been seriously underrated as a global public health issue and the world can no longer ignore ‘the rise and rise’ of type 2 diabetes (Zimmet, 2017).
While genetics play a role in the development of T2D and the potentially stigmatizing nature of the descriptor “preventable” is to be considered, such language aptly describes conditions that may not have developed if addressed through prevention. For example, few would argue today that the eradication of smoking would not dramatically help to reduce the incidence rates of lung cancer or cardiovascular disease, both of which also have genetic and behavioral risk factors.
With systemic change at the broader community level, there is the potential to prevent the development and associated risks of conditions like T2D, dramatically reducing the broad societal impact, thus making this modern pandemic largely ‘preventable.’
7. The economic burden of T2D
There is further substantial evidence specifically documenting the large and accelerated economic burden of T2D from both direct and indirect costs to HICs and LMICs. Bommer et al. defined the absolute economic burden of diabetes as “the sum of excess health expenditure (direct costs) and the value of foregone production (indirect costs) due to diabetes and its complications” (Bommer et al., 2018). This study showed current absolute costs at $1.3 trillion, rising to well over $2 trillion under any scenario (and as high as nearly $2.5 trillion) in less than ten years (2030). The authors further assert that the global economic burden of diabetes in 2030 will exceed 2015 levels by over 85%, reaching over 2.2% of global GDP (compared with only 1.8% in 2015) (Bommer et al., 2018).
The COVID cost example is instructive. As Cutler and Summers illustrate, the COVID-19 pandemic has been estimated to cost over $16 trillion from lost GDP and health loss and is considered to be “the greatest threat to prosperity and well-being the U.S. has encountered since the Great Depression” (Cutler and Summers, 2020). The authors assume a relatively modest duration of the COVID-19 pandemic to less than two years globally, as economic cost “aggregates mortality, morbidity, mental health conditions, and direct economic losses” (Cutler and Summers, 2020).
While the annual direct and indirect costs of diabetes and its complications to the U.S. economy are estimated at a much lower, though still substantial, $327 billion (Complications), this amount represents a growing, long-term economic burden. Existing and forecasted consistent growth of T2D should create great concern about the long-term economic impact.
8. The uniquely underestimated ‘diabetes multiplier effect’
While costs associated with diabetes, cancer, and cardiovascular disease are all substantial, diabetes has a unique multiplier effect with an unparalleled propensity to lead to other serious, costly diseases. While these are traditionally referred to as “complications,” diabetes predisposes patients to these high morbidity and mortality diseases that are also costly to treat. For example, while the annual economic impact of cardiovascular disease (CVD) is $555 billion (American Stroke Association, 2017) – over $200 billion more than that of diabetes – diabetes significantly increases the risk of developing CVD (American Heart Association, 2021). Moreover, not only are adults with diabetes two to four times more likely to die from CVD than those without diabetes (Dal Canto et al., 2019), the type of CVD present in people with diabetes is more likely to be severe, and thus more costly, than in people without diabetes (American Heart Association, 2021).
Beyond CVD, a host of other secondary conditions are commonly attributed to diabetes (Tolman et al., 2007), prompting a rapid cascade of additional healthcare costs. With increasing links between diabetes and Alzheimer’s disease, which costs $290 billion per year alone (and growing) (Fact sheet, 2019), diabetes likely acts as a precursor to yet another costly and debilitating disease (Lee et al., 2018).
Furthermore, people with diabetes who contract COVID-19 experience markedly higher mortality than people without diabetes or uncontrolled hyperglycemia, including greater risk for death and longer hospital stays (Bode et al., 2020).
9. Current T2D prevention efforts are insufficient
There is compelling evidence that government intervention programs, primarily those related to lifestyle (food, nutrition, exercise), are effective in reducing the risk of T2D (Galaviz et al., 2015). The Diabetes Prevention Program (DPP) demonstrated that lifestyle changes alone, focusing on diet and exercise, could lower the incidence of T2D by 58% in high-risk patients (71% for people over 60 years old) (About the National DPP, 2018). DPP, which is covered under Medicare since 2018 (Medicare Diabetes Prevention Program, 2020), saves Medicare an average of $2,650 per person with diabetes enrolled in the program for fifteen months (Medicare to cover Diabetes Prevention Program, 2016). Such prevention measures are powerful, as they are far more cost-effective to prevent diabetes – or to at least prevent its complications – than to treat it.
Despite strong evidence for the effectiveness of diabetes prevention programs, primary care physicians (PCPs) have been reluctant to focus on prevention; as frontline providers, PCPs can proactively address medical issues before they develop into conditions to be managed by endocrinologists. Proactive care for people with diabetes is an effective tool in the management of T2D and its complications, yet today the preventive, potentially T2D-mitigating role of the PCP is still heavily underutilized. Telemedicine for prevention, diagnosis, and disease management of T2D by PCPs is also still at a nascent stage.
The high prevalence of obesity in the U.S. has also contributed substantially to this MPP. There is strong correlation between obesity and diabetes – 85% of people with T2D are also overweight or obese (Bhupathiraju and Hu, 2016). Nearly 40% of American adults were considered obese in 2015–2016, up from 34 percent in 2007–2008 (Hales et al., 2018), with child and adult obesity rates increasing by as much as 85% since the 1980s (The State of Obesity: Better Policies for a Healthier America). With obesity rates increasing in children, educational programs aimed at younger populations are assuredly even more important. The CDC sponsors several community programs aimed toward reducing obesity, including improving early care and education systems to address nutrition and physical activity, promoting healthy food environments in supermarkets, and advancing worksite wellness programs (Overweight and Obesity: Community Efforts, 2020). Social, cultural, educational, and socioeconomic factors in combination, however, greatly complicate the implementation of successful programs targeted at lifestyle modification despite their importance as part of a comprehensive prevention strategy. Hence, while prevention programs for T2D and its frequent precursor of obesity exist – and some are proven effective – they are vastly underused, and their implementation is modest at best (Bowen et al., 2018). The lessons are instructive for diabetes management programs, which similarly can be efficacious when strongly advocated by healthcare leaders.
As a counterexample, despite the controversy associated with many of the COVID-19 prevention programs, they do starkly demonstrate the ability of government-academia programmatic activity targeted to inhibit disease spread with a substantial level of urgency (Brooks and Butler, 2021). To address the T2D pandemic properly, cultural behavior change must be a societal focus with a clear sense of individual responsibility and societal understanding and resolve. Such cultural adaptation should be fostered through educational programs that effectively change those norms that have exacerbated the T2D MPP. As a successful example, tobacco campaigns were targeted at education and ultimately made smoking less socially acceptable.
10. Lack of T2D therapeutic awareness and adherence
The rationale for T2D therapeutic non-adherence varies from patient to patient, but major sources of this problem include lack of access to adequate care, lack of awareness of the consequences of noncompliance, and cost (Morello and Hirsch, 2017). Stigma further reduces therapeutic adherence and proper use of insulin (Liu et al., 2017). Insulin is necessary for glycemic management in over 29% of people with T2D (Selvin et al., 2016), with far more who would likely benefit from insulin therapy. While global T2D insulin use is expected to increase from 516 million 1,000-unit vials to 633.7 million vials per year between 2018 and 2030 (Basu et al., 2018), studies have shown that over 40% percent of patients with T2D decline insulin therapy when recommended.
11. The relatively modest U.S. Government and private research funding for diabetes
The underestimation of the diabetes MPP is further illustrated by the lack of attention from three groups that would naturally step in and tackle such a large societal problem: the government, foundations, and non-governmental organizations, along with industry in public–private partnership. Yet, while this long-standing public health problem warrants a large, multi-sectoral group of organizations to fight it, it is met with relatively modest investment from these core groups.
Current public investment in research on treatment and prevention of diabetes is small relative to the prevalence of the disease. In 2021, $1.214 billion of NIH funding will be allocated for diabetes research (Estimates of Funding for Various Research, 2021), a small component of the $41.7 billion NIH research budget (National Institutes of Health, 2014). This estimate might not perfectly represent the government investment in diabetes research, but it is indicative of the lack of government research focus on diabetes and is consistent with the historic lack of growth in diabetes research funding, which was a modestly lower $1.1 billion dating back to 2008 (Estimates of Funding for Various Research, 2021).
As an MPP, diabetes is a global public health crisis that has continued to grow unabated and should be addressed with the same intensity, focus, and collaboration as any other pandemic such as COVID-19.
12. Eight key replicable actions in the COVID-19 crisis to address the diabetes MPP
The COVID-19 pandemic response, as flawed or controversial as it may be or has been, provides important lessons that can be heavily replicated to address the diabetes pandemic. Below are eight replicable actions from the COVID-19 crisis to address the diabetes MPP.
-
1.
Focus on diagnostics/testing led by the federal government.
Of the 34 million Americans with diabetes, 7.3 million (over 20%) remain undiagnosed (Centers for Disease Control and Prevention, 2020). Early identification of prediabetes, followed by appropriate education and resources, can halt the progression to T2D and prevent or delay years of costly complications (Complications). While this will be led by the federal government, solutions will also come from state- and community-level interventions and involvement.
-
2.
Concentrate on direct prevention measure programs led by the federal government (e.g., obesity, lifestyle management).
Programs like the DPP have produced promising results, including lowering the incidence of T2D by 58% in high-risk patients (About the National DPP, 2018). By increasing the emphasis on how to make prevention programs more accessible with greater retention and sustained results, the U.S. can reverse the trends of T2D. Similar to diagnostics, the prevention efforts will draw on multiple tiers of the community, from local to state to federal government programming.
-
3.
Instill the PCP as the key healthcare provider with broad use of telemedicine tools and institute payment reform for appropriate reimbursement for prevention, diagnosis, and disease management of T2D.
T2D is best managed by PCPs with dedicated multidisciplinary teams trained in diabetes management and armed with enabling technology. Effective diabetes management programs that support the individual needs of each patient are critical to preventing or delaying complications and improving quality of life.
-
4.
Improve awareness, access, and coverage of current safe and efficacious T2D therapeutics led by industry (including payors), supported by federal policy and funding.
Insulin and other T2D therapeutics such as metformin, GLP-1, SGLT2s, and others can substantially reduce the impacts of the disease, particularly those that occur longer-term and induce the “diabetes multiplier effect.” Providing awareness, access, and comprehensive coverage of these therapeutics can substantially reduce T2D morbidity and co-morbidities.
-
5.
Increase insulin adherence for insulin-dependent T2D patients substantially through economic means.
Many more people with T2D would likely benefit if insulin was widely acknowledged as a core therapeutic, accessible and prescribed to achieve optimal glucose control (The State of Obesity: Better Policies). In particular, the ability to manage T2D more effectively with insulin could sharply reduce complications and the longer-term costs of diabetes, which far exceed the near-term costs of accessible and affordable insulin. Methods of achieving this outcome could include insulin affordability programs.
-
6.
Foster substantial, rapid industry-academia-government collaboration for not only diabetes diagnostics and therapeutics but management and prevention.
-
The expedited and highly public COVID-19 vaccine example of government-industry collaboration (as flawed or controversial as it has been) clearly illustrates that such partnerships can yield dramatic results in a very short time. As Cutler and Summers state with respect to the economic cost of COVID-19, “… the immense financial loss from COVID-19 suggests a fundamental rethinking of government’s role in pandemic preparation… investments that are made in testing, contact tracing and isolation should be established permanently and not dismantled when the concerns about COVID-19 begin to recede” (Cutler and Summers, 2020).
Similarly, the United States must not only bolster its development of diabetes therapeutics and technology but also approach the diabetes MPP by investing in testing, education, and prevention programs.
-
7.
Increase public awareness of the T2D MPP substantially, including awareness of its immense health, social, and economic impacts.
Though diabetes has a significant impact on the economy and the healthcare infrastructure of the United States, it has not received the collective action from the public like other diseases, such as COVID-19. To reduce the incidence of diabetes at the population-level, greater public awareness and education are crucial. By destigmatizing T2D through education, the public could be encouraged to get tested and maintain healthy lifestyle behaviors (Nazar et al., 2015).
-
8.
Undertake U.S. global leadership to address and defeat the diabetes MPP.
-
The U.S. has the resources, the authority, and the global standing to lead the way on diabetes prevention and management. In an important publication from the Institute of Medicine a decade ago, the authors presciently wrote about the importance of the global health leadership role the U.S. should play:At this historic moment, the United States has the opportunity to advance the welfare and prosperity of people around the globe through intensified and sustained attention to better health… U.S. leadership in global health reflects many motives: the national interest of protecting U.S. residents from threats to their health; the humanitarian obligation to enable healthy individuals, families, and communities everywhere to live more productive and fulfilling lives; and the broader mission of U.S. foreign policy to reduce poverty, build stronger economies, promote peace, and enhance the U.S. image in the world (The US Commitment to Global Health, 2009).
Given the substantial global prevalence and economic impact of diabetes, United States foreign economic and health policy is inextricably intertwined with domestic policies. The alignment of these policies allows for benefits that span across the globe and give way to improved economic, and humanitarian standings. The U.S. can lead the way toward a healthier future for all communities affected by the T2D MPP.
13. Conclusion
As the COVID-19 pandemic has demonstrated, a coordinated national effort can reduce substantial disease spread to the level of pandemic. Mobilization of similar focus, speed, and coordination is needed for the T2D MPP. Despite the physical, emotional, and financial costs of the diabetes MPP, the current efforts are grossly insufficient. As the number of diagnoses of T2D swells, diabetes’ economic footprint has also significantly increased and will continue to rise in the long-term.
This problem can be successfully addressed; the global response to COVID-19, as flawed and controversial as it may be and has been, provides important lessons of what can be done. An appropriate T2D MPP response requires robust health policy action, strong accompanying political leadership, significant public investment, and expanded media campaigns.
By decreasing the burden of the T2D MPP, the multifactorial benefit to the economy, the healthcare system, national security and, most importantly, the national and global health can lead to reduced mortality and morbidity along with a substantial reduction in T2D-associated healthcare costs.
CRediT authorship contribution statement
Michael E. Singer: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. Kevin A. Dorrance: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Monica M. Oxenreiter: Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. Karena R. Yan: Investigation, Writing – original draft. Kelly L. Close: Conceptualization, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors would like to thank the diaTribe Foundation for funding this paper. The authors would like to thank Benjamin Pallant for initial research contributions. Additionally, the authors would like to thank James Hirsch, John MacAulay M.D., Leslie Prichep Ph.D., Michael Schneider Ph.D., Scott Singer, Richard Thomas MD, David Van Slyke Ph.D., and Terry Vance for their helpful commentary on drafts of this paper.
Funding
Michael Singer is an unpaid advisor to the diaTribe Foundation, an advocacy and information 501(c)(3) organization for people with diabetes, prediabetes, and obesity.
Kevin Dorrance is an unpaid advisor to the diaTribe Foundation.
Monica Oxenreiter was a paid associate at the diaTribe Foundation.
Karena Yan was a paid associate at the diaTribe Foundation.
Kelly Close is the Founder of the diaTribe Foundation; all her work for the diaTribe Foundation has been as an unpaid volunteer.
References
- National Diabetes Statistics Report 2020: Estimates of Diabetes and Its Burden in the US. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.
- IDF Diabetes Atlas. International Diabetes Federation. Published 2021. https://diabetesatlas.org/.
- Kelly H. The classical definition of a pandemic is not elusive. Bull. World Health Organ. 2011;89(7):540–541. doi: 10.2471/BLT.11.088815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries J. The compression of morbidity. Milbank Mem. Fund Q. 1983;61(3):397–419. [PubMed] [Google Scholar]
- Dal Canto E., Ceriello A., Ryden L., et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur. J. Prev. Cardiol. 2019;26(2):25–32. doi: 10.1177/2047487319878371. [DOI] [PubMed] [Google Scholar]
- Leading causes of death. National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
- Narayan K. The diabetes pandemic: looking for the silver lining. Clin. Diabetes. 2005;23(2):51–52. doi: 10.2337/diaclin.23.2.51. [DOI] [Google Scholar]
- Srour B., Fezeu L.K., Kesse-Guyot E., Allès B., Debras C., Druesne-Pecollo N., Chazelas E., Deschasaux M., Hercberg S., Galan P., Monteiro C.A., Julia C., Touvier M. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Santé Prospective Cohort. JAMA Intern. Med. 2020;180(2):283. doi: 10.1001/jamainternmed.2019.5942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehn B. In Alzheimer research, glucose metabolism moves to center stage. JAMA. 2020;323(4):297–299. doi: 10.1001/jama.2019.20939. [DOI] [PubMed] [Google Scholar]
- The US Government Engagement in Global Health: A Primer. Henry J Kaiser Family Foundation; 2019. http://files.kff.org/attachment/Report-The-US-Government-Engagement-in-Global-Health-A-Primer.
- Zimmet P. Diabetes and its drivers: The largest epidemic in human history? Clin. Diabetes Endocrinol. 2017;3(1) doi: 10.1186/s40842-016-0039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bommer C., Sagalova V., Heesemann E., Manne-Goehler J., Atun R., Bärnighausen T., Davies J., Vollmer S. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–970. doi: 10.2337/dc17-1962. [DOI] [PubMed] [Google Scholar]
- Cutler D, Summers L. The COVID-19 pandemic and the $16 trillion virus. JAMA 324(15), 1495-1496. [DOI] [PMC free article] [PubMed]
- Cardiovascular disease: A costly burden to America. American Stroke Association. Published 2017. https://www.heart.org/-/media/files/get-involved/advocacy/burden-report-consumer-report.pdf?la=en.
- Complications. American Diabetes Association. https://www.diabetes.org/diabetes/complications.
- Cardiovascular disease and diabetes. American Heart Association. Published 2021. https://www.heart.org/en/health-topics/diabetes/diabetes-complications-and-risks/cardiovascular-disease--diabetes.
- Tolman K.G., Fonseca V., Dalpiaz A., Tan M.H. Spectrum of liver disease in type 2 diabetes and management of patients with diabetes and liver disease. Diabetes Care. 2007;30(3):734–743. doi: 10.2337/dc06-1539. [DOI] [PubMed] [Google Scholar]
- Fact sheet. Alzheimer’s Impact Movement. Published 2019. https://act.alz.org/site/DocServer/2012_Costs_Fact_Sheet_version_2.pdf?docID=7161.
- Lee H.J., Seo H.I., Cha H.Y., Yang Y.J., Kwon S.H., Yang S.J. Diabetes and Alzheimer’s disease: mechanisms and nutritional aspects. Clin. Nutr. Res. 2018;7(4):229–240. doi: 10.7762/cnr.2018.7.4.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bode B., Garrett V., Messler J., McFarland R., Crowe J., Booth R., Klonoff D.C. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J. Diabetes Sci. Technol. 2020;14(4):813–821. doi: 10.1177/1932296820924469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galaviz K.I., Narayan K.M.V., Lobelo F., Weber M.B. Lifestyle and the prevention of type 2 diabetes: a status report. Am. J. Lifestyle Med. 2015;12(1):4–20. doi: 10.1177/1559827615619159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- About the National DPP. Centers for Disease Control and Prevention; 2018. https://www.cdc.gov/diabetes/prevention/about.htm.
- Medicare Diabetes Prevention Program. National Association of Chronic Disease Directors; 2020. https://coveragetoolkit.org/medicare-advantage/mdpp-final-rule/.
- Medicare to cover Diabetes Prevention Program. diaTribe Learn. Published 2016. https://diatribe.org/medicare-cover-diabetes-prevention-program.
- Bhupathiraju S.N., Hu F.B. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ. Res. 2016;118(11):1723–1735. doi: 10.1161/CIRCRESAHA.115.306825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Ogden C.L. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723. doi: 10.1001/jama.2018.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The State of Obesity: Better Policies for a Healthier America. Trust for America’s Health; 2019. https://www.tfah.org/wp-content/uploads/2019/09/2019ObesityReportFINAL-1.pdf.
- Overweight and Obesity: Community Efforts. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/obesity/strategies/community.html.
- Bowen M.E., Schmittdiel J.A., Kullgren J.T., Ackermann R.T., O’Brien M.J. Building toward a population-based approach to diabetes screening and prevention for US adults. Curr. Diab. Rep. 2018;18(11):104. doi: 10.1007/s11892-018-1090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks J., Butler J. Effectiveness of mask wearing to control community spread of SARS-CoV-2. JAMA. 2021;325(10):998–999. doi: 10.1001/jama.2021.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello C., Hirsch J. Strategies for addressing the cost of nonadherence in diabetes. Am. J. Manag. Care. 2017;23(13) [PubMed] [Google Scholar]
- Liu N, Brown A, Folias A, et al. 2017. Stigma in people with type 1 or type 2 diabetes. Clin. Diabet. 35(1), 27-34. doi:https://doi.org/10.2337/cd16-0020. [DOI] [PMC free article] [PubMed]
- Selvin, E., Parrinello, C., Daya, N., Bergenstal, R. 2016. Trends in insulin use and diabetes control in the US: 1988-1994 and 1999-2012. Diabetes Care 39(3), e33-e35. doi:10.2447dc15-2229. [DOI] [PMC free article] [PubMed]
- Basu S., Yudkin J., Kehlenbrink S., et al. Estimation of global insulin use for type 2 diabetes mellitus, 2018–2030. Lancet Diabetes Endocrinol. 2018;7(1):25–33. doi: 10.1016/S2213-8587(18)30303-6. [DOI] [PubMed] [Google Scholar]
- Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). National Institute of Health; 2021. Accessed November 7, 2021. https://report.nih.gov/funding/categorical-spending#/.
- National Institutes of Health. Budget. National Institutes of Health (NIH). Published October 31, 2014. Accessed November 7, 2021. https://www.nih.gov/about-nih/what-we-do/budget.
- Nazar C.M.J., Bojerenu M.M., Safdar M., Marwat J. Effectiveness of diabetes education and awareness of diabetes mellitus in combating diabetes in the United Kigdom; a literature review. J. Nephropharmacol. 2015;5(2):110–115. [PMC free article] [PubMed] [Google Scholar]
- The US Commitment to Global Health: Recommendations for the Public and Private Sectors. Institute of Medicine (US) Committee on the US Commitment to Global Health; 2009. [PubMed]