Abstract
Background
The diagnostic accuracy of the ISTH’s disseminated intravascular coagulation (DIC) score remains to be investigated in contemporary patient populations.
Objective
To examine the positive predictive value (PPV) of an ISTH DIC score ≥5 for identifying patients with overt DIC in a Danish hospital laboratory information system database.
Materials and Methods
A population‐based cross‐sectional validation study in the Central Denmark Region (2015‐2018). Patients with a DIC score ≥5 were identified from the hospital laboratory information system database. Only patients with a potential underlying cause of DIC were included in the analyses. Cases were adjudicated by the authors as the gold standard for DIC diagnosis. The diagnosis of overt DIC was assigned on the basis of clinical signs of microthrombosis and/or bleeding and available laboratory records. PPVs with 95% confidence intervals (CIs) were computed.
Results
Medical records of 225 patients were included. The overall PPV for overt DIC was 68% (95% CI, 61‐74) and for overt + subclinical DIC, 83% (95% CI, 77%‐88%) and increased with higher scores from 47% (95% CI, 35‐59) for DIC score 5 to 88 (95% CI, 79‐94) for DIC score ≥7. PPV was higher among intensive care patients and patient with sepsis, low antithrombin activity, prolonged activated partial thromboplastin time, or high Sequential Organ Failure Assessment score.
Conclusion
The accuracy of ISTH DIC score ≥5 was moderate for overt DIC but increased with increasing scores and depended on the underlying cause of DIC. This new knowledge provides guidance to physicians and enables DIC research using laboratory‐based data.
Keywords: blood coagulation tests, critical care, diagnosis, disseminated intravascular coagulation, predictive value of tests, validation study as topic
Essentials.
The blood clot disorder disseminated intravascular coagulation (DIC) is difficult to diagnose.
We evaluated the positive predictive value (PPV) of the diagnostic ISTH DIC score.
Overall PPV was moderate and was influenced by patient characteristics and comorbidities.
Physicians and researchers must be aware of limitations to laboratory‐based scores for DIC diagnosis.
1. INTRODUCTION
Disseminated intravascular coagulation (DIC) is characterized by systemic coagulation and platelet activation that results in global microthrombus formation and organ dysfunction. Further, concomitant consumption of platelets and coagulation factors can lead to life‐threatening bleeding. 1 , 2 The diagnosis of DIC encompasses findings of coagulopathy or disturbed fibrinolysis in the presence of an underlying cause of DIC (eg, sepsis or malignancy); 3 , 4 however, the clinical diagnosis of DIC is difficult, and therefore laboratory tests are vital for the diagnosis. 5 As no single laboratory test can accurately confirm or eliminate the diagnosis of DIC, international guidelines recommend the use of DIC scoring systems to support the diagnosis of DIC. 6 , 7 The existing scoring systems are based on laboratory tests available in most hospital laboratories. One of the most widely employed scoring systems was developed by the ISTH. The score is based on the patient’s platelet count, international normalized ratio (INR), fibrinogen, and fibrin D‐dimer. A score of ≥5 indicates overt DIC. 5 Other scoring systems, such as the Japanese Association for Acute Medicine (JAAM) DIC score, include antithrombin but may exclude fibrinogen, and the JAAM DIC score also uses change in platelet count as a supplement to absolute platelet count. 8 In the present study, we focused on the ISTH DIC score, as this scoring system is one of the most used in the clinical setting in the Western part of the world and because it can be calculated solely on the basis of laboratory database records, which represented our main data source.
DIC scoring systems are reported to have a sensitivity of ≈90% and a specificity of ≈97%. 9 , 10 However, the positive predictive value (PPV) of different DIC scoring systems will depend on the prevalence of DIC in the source population. Furthermore, as the score is laboratory based, it is sensitive to the presence of factors that can influence the laboratory parameters comprising the DIC score, for example, liver disease, which can cause prolonged prothrombin time and in advanced stages, thrombocytopenia or hematological disease, which can affect platelet count either directly or through antineoplastic treatment. Thus, the PPV of the DIC score must be expected to vary depending on the underlying cause of DIC, the clinical setting (internal medicine ward/intensive care unit [ICU]), the severity of coagulopathy (DIC score 5 vs 8), and the presence of coexisting conditions and medications that influence routine coagulation analyses (eg, liver dysfunction or vitamin K antagonist treatment). 11 Furthermore, the ISTH DIC score was introduced 20 years ago this year, and the demography and clinical characteristics of patients with DIC may have changed during this time span. Estimating the PPV for the ISTH DIC score in a hospital‐based setting is important for two reasons: First, it will assist clinicians in the evaluation of the patient with suspected DIC, ensuring timely diagnosis and interventions; second, valid identification of patients with DIC from laboratory information system databases will enable research on DIC epidemiology. The present study therefore examined the PPV of the ISTH DIC score for overt DIC in an adult Danish in‐hospital population.
2. MATERIALS AND METHODS
2.1. Setting and design
This validation study was conducted in the Central Denmark Region from January 1, 2015, through December 31, 2018, within a source population of 1.2 million residents. Denmark has a tax‐supported health care system that guarantees unfettered access to medical care for all residents. 12
2.2. Study population
Patients were eligible for inclusion if (i) laboratory results for all ISTH DIC score components (platelet count, INR, fibrinogen, fibrin D‐dimer) were available from the same date, (ii) they had a first‐time ISTH DIC score ≥5, and (iii) the main indication for ordering the laboratory tests was a clinical suspicion of DIC and no other causes (eg, surgical bleeding).
We searched the hospital laboratory information system in the Central Denmark Region to sample adult patients (≥18 years old) with potential DIC diagnoses using a predefined algorithm. We identified patients from Aarhus University Hospital and two regional hospitals (Regional Hospital West Jutland and Regional Hospital Central Jutland). All biomarkers used at the hospital departments are tracked in the electronic hospital laboratory information system using the International System of Nomenclature, Properties, and Units. 13 Given the homogeneity of the Danish health care system, these hospitals are considered representative for similar‐sized hospitals in other Danish regions. 14
First, we identified all patients with laboratory records of platelet count, INR, fibrin D‐dimer, and fibrinogen levels during the study period (Figure 1 and Table S1). Then, we restricted to patients who had all components of the ISTH DIC scoring system measured on the same date. After this, we calculated all their ISTH DIC scores during the study period using the algorithms provided in Table 1. For patients with more measurements (eg, platelet count measures) on the same day, we used the most abnormal values, that is, the lowest value for measurements of platelet counts and fibrinogen and the highest value for fibrin D‐dimer and INR. Patients were included only once, according to their first record of a given DIC score ≥5. Records from general practitioners, emergency room departments, and outpatients (likely not requested on DIC indication) were excluded from the analyses, but they were included if they were later admitted to a hospital department. We subsequently divided the study population into three groups with ISTH DIC scores of 5, 6, or ≥7.
FIGURE 1.
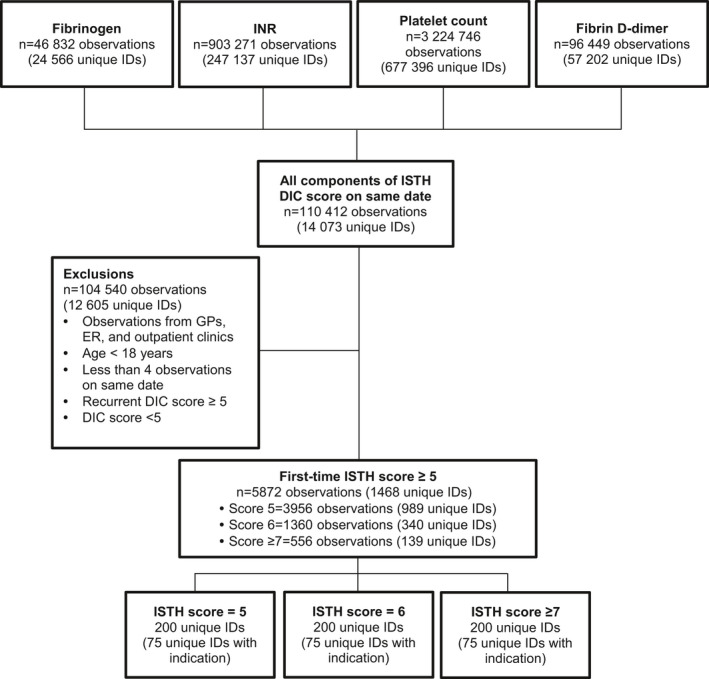
Flowchart showing selection of patients from the laboratory database and the random samples from each DIC score category. DIC, disseminated intravascular coagulation; ER, emergency room; GPs, general practitioners; INR, international normalized ratio
TABLE 1.
ISTH DIC score algorithms used in the study
| ISTH‐DIC score | ||
|---|---|---|
| Value | Score | |
|
International normalized ratio Reference range <1.2 |
<1.3 | 0 |
| 1.3‐1.6 | 1 | |
| >1.6 | 2 | |
|
Fibrin D‐dimer (mg/L) Reference range: age‐specific a |
<0.8 | 0 |
| ≥0.8‐8.0 | 2 | |
| >8.0 | 3 | |
|
Platelet count (109/L) Reference range 145–400 |
>100 | 0 |
| 50–100 | 1 | |
| <50 | 2 | |
|
Fibrinogen (µmol/L) Reference range: 5.5‐12 |
≥2.94 (equivalent to ≥1 g/L) | 0 |
| <2.94 (equivalent to <1 g/L) | 1 | |
Abbreviation: DIC, disseminated intravascular coagulation.
18‐55 years:<0.50, 55‐65 years:<0.60, 65‐75 years:<0.70, 75‐85 years:<0.80, 85‐95 years: <0.90.
Some patients may have had testing performed on other indications than suspicion of DIC. To estimate the proportion of patients with DIC as an indication for testing, in a pilot project, we randomly selected 10 patients from each ISTH DIC score group and reviewed their medical records to determine the indication for DIC score testing. In patients with a DIC score of 5, a relevant indication was present in only 50% of patients. Based on these preliminary results, we decided to include a sample size of up to 200 patients in each ISTH DIC score group to obtain 75 patients with a relevant indication for DIC testing in each group. The sample size of 75 has shown to yield relatively precise effect estimates in prior validation studies. 15 , 16
2.3. Adjudication of the DIC diagnosis
A true gold standard for the clinical diagnosis of DIC does not exist. Therefore, the patients were classified as having overt (symptomatic) DIC, subclinical DIC, or no DIC through expert consensus, based on available information in the electronic medical record during a window of ±2 days within the time of blood sampling for DIC score. The diagnosis of overt DIC was based on the presence or strong suspicion of bleeding and/or microthrombus formation (acute organ dysfunction, blue extremities, necrosis/gangrene) in combination with relevant laboratory results not included in the ISTH DIC score (eg, activated partial thromboplastin time [aPTT], antithrombin, increment or decrement in platelet count), microbiology results, imaging results, information on medication, and the absence of other conditions that could clearly explain abnormal laboratory results (eg, liver cirrhosis in a patient with moderate thrombocytopenia and and prolonged INR). The diagnosis of subclinical DIC was based on clear biochemical signs of DIC and, as for overt DIC, an absence of other conditions that could clearly explain abnormal laboratory results, but no suspicion of bleeding or microthrombus formation. To ensure consensus on data collection and assignment of a clinical diagnosis of DIC, five medical records first were reviewed and discussed by all authors. Subsequently, one of three authors (JBL, MAA, or KA) reviewed each medical record and judged whether a definite diagnosis of overt DIC should be made. In case of doubt, cases were discussed among the three authors to reach consensus, and if the diagnosis remained uncertain, a secondary review was performed together with an expert in thrombosis and hemostasis (AMH) to reach consensus.
2.4. Medical record data collection
Data were systematically extracted from the medical records using the form provided in Table S2 and entered into REDCap (Research Electronic Data Capture; Vanderbilt University, Nashville, TN, USA) hosted by Central Denmark Region. 17
Data items included (i) baseline characteristics (age and sex); (ii) indication for DIC testing; (iii) presence or suspicion of relevant DIC etiology; (iv) presence or suspicion of possible differential diagnosis to DIC; (v) all‐cause mortality; (vi) presence or suspicion of venous or arterial thrombotic disease; (vii) presence or suspicion of thrombotic microangiopathy, bleeding, and circulatory instability; (viii) Simplified Acute Physiology Score at ICU admission, if available, and Sequential Organ Failure Assessment (SOFA) score; (ix) laboratory records; (x) microbiology results; (11) relevant treatments (Table S2). A time window of ±2 days was set for the classical clinical manifestations of DIC thrombotic microangiopathy and bleeding to allow for potential reporting delay in the medical record. Bleeding was defined and categorized according to the modified World Health Organization (WHO) bleeding score 18 (Table S2). The final decision on presence/absence of overt DIC also took into account presence/absence of circulatory instability, presence of other conditions, which could influence the laboratory parameters included in the DIC score, and other laboratory results (eg, aPTT and antithrombin).
2.5. Statistical analysis
Only patients with a relevant indication for DIC testing were included in the analysis. For all patients in total and for each subscore (ie, ISTH DIC scores 5, 6, or 7‐8), we computed the PPVs with 95% confidence intervals (CIs). The PPVs were computed as the proportion of DIC diagnoses retrieved from the laboratory database (ISTH DIC score ≥5) that could be confirmed in the discharge summary or medical record (“gold standard positive”). In additional analyses, we calculated the PPVs excluding patients with a history of cancer (solid tumors and hematological cancers) and liver disease, as these conditions often are associated with coagulation abnormalities.
To examine any disparities in PPV across subgroup of patients, analyses were stratified by age (≤60 years vs >60 years), sex, year of diagnosis (2015‐2016 vs 2017‐2018), department (ICU vs non‐ICU), etiology (eg, sepsis or malignancy), platelet count levels (<50 vs ≥50 × 109/L), fibrinogen level (<2.94 and ≥2.94 µmol/L), INR (>1.6 and ≤1.6), fibrin D‐dimer (>8 and ≤8 mg/L), antithrombin activity (≤0.60 and >0.60 IU/L), aPTT (>1.5 × upper reference limit and ≤1.5 × upper reference limit), and SOFA score (0–12 and >12). In addition, we tabulated descriptive data on the patients with DIC overall, and according to ISTH score and biochemical DIC. We calculated 30‐day mortality using the Kaplan‐Meier method.
Data management and sampling of patients was performed using Stata version 16.0 (StataCorp, College Station, TX, USA). PPV with 95% CI was calculated using the “ci prop” function. The study was approved as a quality assurance project by all hospital directors and heads of relevant departments in accordance with the Danish Health Care Act.
3. RESULTS
An overview of the patient record selection process is provided in Figure 1. We identified the following test results from the laboratory information system database: fibrinogen, 46 832 (24 566 unique individuals); INR, 903 271 (24 566 unique individuals); platelet count, 3 224 746 (677 396 unique individuals); and fibrin D‐dimer: 96 449 (57 202 unique individuals). Overall, 14 073 patients had all laboratory components of the DIC score measured on the same date. After exclusions (Figure 1) and following restriction to first‐time ISTH scores, 1590 patients with an ISTH score ≥5 were eligible for inclusion. It was necessary to adjudicate 356 medical records (retrieval rate = 100%), which were selected based on a random sample, to identify the desired 225 (63.2%) patients (or 75 in each DIC score group) who had an underlying etiology potentially consistent with DIC. These 225 records were subject to further detailed medical record review. The patients were mainly hospitalized in the ICU (79%).
3.1. PPV for overt DIC
The overall PPV for an ISTH score ≥5 was 68% (95% CI, 61%‐74%) for overt DIC with symptoms of bleeding and/or microthrombus formation and 83% (95% CI, 77%‐87%) for overt and subclinical DIC combined (Table 2). Increasing DIC score was associated with higher PPV: 47% (95% CI, 35%‐59%) for a score of 5, 68% (95% CI, 56%‐78%) for a score of 6, and 88% (95% CI, 79%‐94%) for a score ≥7. Further, the PPV was higher among patients admitted to an ICU than among patients at non‐ICU departments (PPV = 74% vs PPV = 44%; Table 3). The PPV was also higher among patients with sepsis than among patients with malignancy (PPV = 70% vs PPV = 40%), antithrombin activity below ≤0.60 IU/L (PPV = 81% vs PPV = 49%), prolonged activated partial thromboplastin time >1.5 × upper reference limit (PPV = 80% vs PPV = 50%), and in patients with a SOFA score >12 (PPV = 81% vs PPV = 49%; Table 3). The PPVs were largely similar across age groups, sex, and calendar period. A detailed overview stratified after DIC score is showed in Table S3. The PPVs remained unchanged when excluding 83 patients with a history of cancer or liver disease (PPV overall = 67% (95% CI, 59%‐75%); PPV for score 5 = 45% (95% CI, 32%‐60%); PPV for score 6 = 67% (95% CI, 51%‐80%); and PPV for score ≥7 = 92% (95% CI, 80%‐98%).
TABLE 2.
Positive predictive values for ISTH DIC score ≥5
|
DIC‐positive cases (overt DIC) |
DIC‐positive cases (overt and subclinical DIC) |
DIC‐negative cases b | |||
|---|---|---|---|---|---|
| DIC score | Ratio a |
PPV, % (95% CI) |
Ratio a |
PPV, % (95% CI) |
No. of cases (%) |
| Overall | 152/225 | 68 (61‐74) | 186/225 | 83 (77‐87) | 39 (17) |
| 5 | 35/75 | 47 (35‐59) | 56/75 | 75 (63‐84) | 19 (25) |
| 6 | 51/75 | 68 (56‐78) | 60/75 | 80 (69‐88) | 15 (20) |
| ≥7 | 66/75 | 88 (78‐94) | 70/75 | 93 (85‐98) | 5 (8) |
Abbreviations: CI, confidence interval; DIC, disseminated intravascular coagulation; PPV, positive predictive value.
Number of patients classified correct/total number of medical record reviews.
These included liver disease, hematological disease, congestive heart failure, medical treatments (eg, warfarin, chemotherapy), immune thrombocytopenia, or thrombotic thrombocytopenia purpura/hemolytic uremic syndrome.
TABLE 3.
Positive predictive values of ISTH DIC score for overt DIC, by patient subgroups
| Ratio | PPV, % (95% CI) | Ratio | PPV, % (95% CI) | |
|---|---|---|---|---|
| Age | ≤60 years | >60 years | ||
| 63/89 | 71 (60‐80) | 89/136 | 65 (57‐73) | |
| Sex | Male | Female | ||
| 87/129 | 67 (59‐75) | 65/96 | 68 (57‐77) | |
| Time period | 2015‐2016 | 2017‐2018 | ||
| 79/120 | 66 (57‐74) | 73/105 | 70 (60‐78) | |
| Admission type | ICU | Non‐ICU | ||
| 131/177 | 74 (67‐80) | 21/48 | 44 (30‐59) | |
| DIC etiology | Sepsis | Malignancy | ||
| 96/138 | 70 (61‐77) | 4/10 | 40 (12‐74) | |
| Platelet count | <50 × 109/L | ≥50 × 109/L | ||
| 93/128 | 73 (64‐80) | 59/97 | 61 (50‐71) | |
| Fibrinogen | <2.94 µmol/L | ≥2.94 µmol/L | ||
| 28/33 | 85 (68‐95) | 124/192 | 65 (57‐71) | |
| INR | >1.6 | ≤1.6 | ||
| 131/175 | 75 (68‐81) | 21/50 | 42 (28‐57) | |
| Fibrin D‐dimer | >8.0 mg/L | ≤8.0 mg/L | ||
| 121/173 | 70 (63‐77) | 31/52 | 60 (45‐73) | |
| Antithrombin | ≤0.60 IU/L | >0.60 IU/L | ||
| 104/128 | 81 (73‐88) | 48/97 | 49 (39‐60) | |
| aPTT | >1.5 × upper reference limit a | ≤1.5 × upper reference limit | ||
| 55/64 | 86 (75‐93) | 37/74 | 50 (38‐62) | |
| SOFA score | ≤12 | >12 | ||
| 46/94 | 49 (38–59) | 105/129 | 81 (74–88) | |
Abbreviations: aPTT, activated partial thromboplastin time; CI, confidence interval; DIC disseminated intravascular coagulation; INR, international normalized ratio; PPV, positive predictive value; SOFA, Sequential Organ Failure Assessment.
Restricted to individuals after July 1, 2016, due to changes in the reference interval for the analysis.
In total, 39 patients were classified as DIC negative, that is, they had a DIC score ≥5 but were judged to (i) have neither overt nor subclinical DIC based on the absence of microthrombus or bleeding symptoms described in the medical record and (ii) have one or more concurrent conditions or treatments that could explain the abnormal laboratory tests and influence the DIC score. The most prevalent conditions in the DIC negative cases were liver dysfunction (21%), hematological malignancy (33%), and medications that influenced one or more DIC score parameters (chemotherapy or vitamin K antagonists) (31%). The 39 patients who were DIC negative were similar to the patients who were overtly DIC positive regarding mean age (65 years vs 64 years), the prevalence of sepsis (85% vs 87%), and platelet count (46 × 109/L vs 42 × 109/L), but they had lower median SOFA scores (10 vs 15), higher prevalence of malignancy (41% vs 26%), higher fibrinogen (12.4 µmol/L vs 7.5 µmol/L) and higher antithrombin (0.70 IU/L vs 0.47 IU/L), lower fibrin D‐dimer (9.1 mg/L vs 16.5 mg/L), and slightly lower INR (1.7 vs 2.0), and their 30‐day mortality was 41% as compared to 63% in patients with overt DIC.
3.2. Characteristics of DIC patients
Among the 152 patients with overt DIC, the median age was 64 years (25th‐75th percentile, 52‐73 years) and 65 (43%) were women (Table 4). The most common DIC etiology was infection/sepsis (87%). Virtually all patients had confirmed or suspected thrombotic microangiopathy with a majority of the patients having signs of cold extremities, blue skin, and acute kidney injury. Venous thromboembolism was diagnosed in 14 patients (9%), while 36 (24%) experienced an arterial cardiovascular event. Overall, 115 (76%) patients experienced any bleeding, most often equivalent to WHO grade 2. The overall 30‐day mortality was 63%. On the date of DIC score, patients generally had moderate to severe thrombocytopenia (median platelet count = 42 × 109/L), pronounced INR prolongation (median = 2.0), and high fibrin D‐dimer (median = 16.5 mg/L); however, median fibrinogen was within the reference interval, and only 28 of the 152 overt DIC patients had fibrinogen below the cutoff <2.94 μmol/L. Low antithrombin activity was prevalent, with median (25th‐75th percentile) antithrombin activity 0.47 (0.35‐0.64) IU/L. The median SOFA score was 15. A positive blood culture was observed among 57 (38%) of the patients. The most frequent treatment modalities received on the day of the DIC score and on the 2 days after included inotropes (74%), blood transfusion (45%), fresh frozen plasma (51%), platelet transfusion (51%), dialysis (46%), and prophylactic low‐molecular‐weight heparin (42%). The use of antithrombin, surgery, fibrinogen concentrate, and tranexamic acid was less common (Table 4). A detailed overview of demographic and clinical characteristics stratified after DIC score is displayed in Table S4.
TABLE 4.
Characteristics of patients with overt (n = 152) and subclinical (n = 34) DIC
|
Overt DIC n = 152 |
Subclinical DIC n = 34 |
|
|---|---|---|
| Demographic data | ||
| Age, y (median, IQR) | 64 (52‐73) | 67 (48‐77) |
| Female sex, n (%) | 65 (43) | 19 (56) |
| 30‐day all‐cause mortality, n (%) | 95 (63) | 0 (0) |
| DIC etiology, n (%) | ||
| Infection/sepsis | 132 (87) | 30 (88) |
| Malignancy | 40 (26) | 10 (29) |
| Other a | 44 (29) | 6 (18) |
| Thrombosis, n (%) | ||
| Microthrombus formation | ||
| No | ≤5 | 11 (32) |
| Suspected | 46 (30) | 23 (68) |
| Yes | 101 (66) | 0 (0) |
| Venous thrombosis | 14 (9) | ≤5 |
| Arterial thrombosis | 36 (24) | 7 (21) |
| Bleeding | ||
| No | 28 (18) | 25 (74) |
| Suspected | 9 (6) | 2 (6) |
| Yes (any) | 115 (76) | 7 (21) |
| WHO grade 2 | 111 (73) | 7 (21) |
| WHO grade 3‐4 | 47 (31) | 2 (6) |
| Laboratory results | ||
|
Platelet count, ×109/L (ref: 150‐400) |
42 (26‐76) | 66 (36‐100) |
|
Fibrinogen, μmol/L (ref: 5.5‐12.0) |
7.5 (4.0‐12.2) | 12.6 (9.5‐15.5) |
| INR (ref: <1.2) | 2.0 (1.7‐2.5) | 1.8 (1.3‐2.0) |
| Fibrin D‐dimer, mg/L b | 16.5 (8.6‐21.0) | 12.6 (7.5‐21.0) |
|
Antithrombin activity, IU/L (ref: 0.80‐1.20) |
0.47 (0.35‐0.64) | 0.70 (0.57‐0.82) |
| aPTT, s c (ref: 20‐29) | 49 (36‐65) | 33 (29‐35) |
| SAPS III score | 70 (60‐87) | 76 (65‐84) |
| SOFA score | 15 (12‐18) | 8 (5‐14) |
| Treatment received | ||
| LMWH (prophylactic) | 64 (42) | 15 (44) |
| LMWH (treatment) | 13 (9) | 6 (18) |
| UFH | 26 (17) | ≤5 |
| Red blood cell transfusion | 69 (45) | 6 (18) |
| Platelet transfusion | 78 (51) | 6 (18) |
| Fresh frozen plasma | 77 (51) | ≤5 |
| Fibrinogen concentrate | 16 (11) | 0 (0) |
| Tranexamic acid | 11 (7) | ≤5 |
| Antithrombin | 28 (18) | ≤5 |
| Surgery d | 26 (17) | ≤5 |
| Dialysis | 70 (46) | ≤5 |
| ECMO | 27 (18) | ≤5 |
| Inotropes | 112 (74) | 15 (44) |
Abbreviations: ALAT, alanine transaminase; aPTT, activated partial thromboplastin time; DIC, disseminated intravascular coagulation; ECMO, extracorporeal membrane oxygenation; INR, international normalized ratio; IQR, interquartile range; LMWH, low‐molecular‐weight heparin; ref, reference interval; SAPS, Simplified Acute Physiology Score; SOFA, Sequential Organ Failure Assessment; UFH, unfractionated heparin.
Other conditions include obstetric complications, cardiac arrest, acute pancreatitis.
Reference intervals are age specific: <55 years, <0.50 mg/L; 55‐64 years, <0.60 mg/L; 65‐74 years, <0.70 mg/L; 75‐84 years, <0.80 mg/L; 85‐94 years, <0.90 mg/L; ≥95 years, <1.0 mg/L.
Restricted to individuals after July 1, 2016, due to changes in the reference interval for the analysis.
Amputation or bowel resection.
4. DISCUSSION
Our study investigated PPV of an ISTH DIC score ≥5 for overt DIC using Danish hospital laboratory data. Overall PPV for overt (symptomatic) DIC was moderate but increased with increasing DIC score in a dose‐response manner and when subclinical DIC was included. Furthermore, PPV was higher among patients with sepsis, patients with low antithrombin activity or prolonged aPTT, and patients with a high SOFA score. The main reasons for a false‐positive ISTH DIC score were the presence of liver dysfunction, hematological malignancy, or pharmacological treatment that could influence either platelet count or INR (eg, vitamin K antagonist or chemotherapy).
Our study adds considerably to the sparse literature on the diagnostic accuracy of the ISTH DIC score. One study from 2004 by Bakhtiari et al 9 investigated the sensitivity and specificity of the ISTH DIC score in an ICU population. The gold‐standard diagnosis of DIC was assigned by an expert panel based on clinical and laboratory data, similarly to our study. The authors found a sensitivity and specificity of 91% and 97% and a PPV of 96%, which is higher than our findings. An explanation for this discrepancy may be that we included patients from both internal medicine wards and ICU wards, as we found that PPV increased when restricting the analysis to ICU patients. Studies have also validated the ISTH DIC score using other DIC scoring systems as gold standard, such as the Japanese Ministry of Health and Welfare (JMHW) DIC score 19 , 20 and the JAAM DIC score. 21 Wada and colleagues found a concordance between the ISTH and JMHW scoring systems of 0.63, 19 which increased when patients with malignancy were excluded, 20 while the JAAM DIC score appeared more sensitive for DIC in a setting of sepsis. 21 , 22 Very recently, Helms et al 23 investigated concordance between ISTH DIC score, the 2016 JAAM DIC score and the sepsis‐induced coagulopathy (SIC) score in a large septic shock population. 24 The authors found concordance between JAAM and ISTH DIC scores of 0.67. 23 The study did not use a clinical diagnosis of DIC as gold standard, but notably, the authors reported that only 20% of patients with positive ISTH and/or JAAM DIC score had clinically significant signs of bleeding or thrombosis on the day of DIC score, while ≈50% developed these signs during the days after the DIC score. This is similar to our estimated overall PPV of 68% for symptomatic DIC.
The clinical significance of our findings is that while the ISTH DIC score remains a sensitive and easy‐to‐use diagnostic tool for DIC, PPV may vary widely depending on the type and severity of the underlying condition. The physician should be aware of other conditions that can influence the laboratory parameters comprising the DIC score, the most prominent being liver dysfunction and thrombocytopenia from other causes. Our findings also underline the value of other laboratory parameters to support the diagnosis, including antithrombin, and aPTT. Our findings also have important implications for DIC research. The use of a laboratory record‐based DIC score to identify DIC patients poses obvious benefits for research using large data sets. However, the moderate PPV indicates limitations to this approach. Our results underline that, depending on the source population, the diagnosis of DIC may need additional verification from clinical data and laboratory records to avoid misclassification.
A strength of the present study was that our data set was based on a large source population representative for contemporary hospitalized patients in Denmark. Medical records and laboratory data were available for all patients through their unique Danish personal identification number. Data were extracted systematically from medical records using a prespecified form, and the diagnosis of DIC was settled by consensus in a panel of physicians with clinical and laboratory experience. However, some limitations must be mentioned. We included a heterogeneous group of patients from both internal medicine and ICU wards with multiple concurrent conditions. However, in our opinion, this approach more accurately reflects the population of patients with suspected DIC that meets the clinicians and researchers in their daily work. Furthermore, the lack of a gold standard for DIC diagnosis is a challenge in all DIC research, including the present study. The diagnosis of DIC was based on medical record entries, and we cannot exclude underregistration of bleeding or thrombotic events, especially for patients with short follow‐up times due to death. The sample size of 75 patients in each DIC score group yielded good overall effect estimates but limited the options for stratification into subgroups. Finally, as the purpose of the study was to investigate positive predictive value of an ISTH DIC score ≥5, we included only patient records with a positive DIC score and thus could not calculate sensitivity, specificity, or negative predictive value.
4.1. Conclusions
The overall PPV of ISTH DIC score ≥5 was moderate for overt DIC in a contemporary Danish hospital setting but increased with increasing scores in a dose‐response manner and was higher in ICU patients than non‐ICU patients. PPV was dependent on the underlying cause of DIC and was highest in patients with sepsis, presence of other signs of coagulation disturbances or high SOFA scores. Highlighting strengths and pitfalls of DIC scoring systems, our findings enable research on patients with DIC using laboratory‐based data.
RELATIONSHIP DISCLOSURE
The authors have no conflicts of interest pertaining to the present study.
AUTHOR CONTRIBUTIONS
All authors were involved in the design of the study. JBL, MAA, KA, and A‐MH reviewed the medical records and performed data extraction. KA performed the data management and the statistical analyses. JBL and KA wrote the first manuscript draft, which was reviewed for intellectual content by all authors. All authors approved the manuscript prior to submission.
Supporting information
Supplementary Material
Larsen JB, Aggerbeck MA, Granfeldt A, Schmidt M, Hvas A‐M, Adelborg K. Disseminated intravascular coagulation diagnosis: Positive predictive value of the ISTH score in a Danish population. Res Pract Thromb Haemost. 2021;5:e12636. doi: 10.1002/rth2.12636
Handling Editor: Pantep Angchaisuksiri
Funding information
The study was supported by the Aarhus University Research Foundation.
REFERENCES
- 1. Levi M, de Jonge E, van der Poll T. New treatment strategies for disseminated intravascular coagulation based on current understanding of the pathophysiology. Ann Med. 2004;36(1):41‐49. [DOI] [PubMed] [Google Scholar]
- 2. Papageorgiou C, Jourdi G, Adjambri E, et al. Disseminated intravascular coagulation: an update on pathogenesis, diagnosis, and therapeutic strategies. Clin Appl Thromb Hemost. 2018;24(9_suppl):8S‐28S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levi M, Sivapalaratnam S. Disseminated intravascular coagulation: an update on pathogenesis and diagnosis. Expert Rev Hematol. 2018;11(8):663‐672. [DOI] [PubMed] [Google Scholar]
- 4. Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2:16037. [DOI] [PubMed] [Google Scholar]
- 5. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327‐1330. [PubMed] [Google Scholar]
- 6. Wada H, Takahashi H, Uchiyama T, et al. The approval of revised diagnostic criteria for DIC from the Japanese Society on Thrombosis and Hemostasis. Thromb J. 2017;15:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145(1):24‐33. [DOI] [PubMed] [Google Scholar]
- 8. Iba T, Di Nisio M, Thachil J, et al. Revision of the Japanese Association for Acute Medicine (JAAM) disseminated intravascular coagulation (DIC) diagnostic criteria using antithrombin activity. Crit Care. 2016;20:287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bakhtiari K, Meijers JC, de Jonge E, Levi M. Prospective validation of the International Society of Thrombosis and Haemostasis scoring system for disseminated intravascular coagulation. Crit Care Med. 2004;32(12):2416‐2421. [DOI] [PubMed] [Google Scholar]
- 10. Toh CH, Hoots WK. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5‐year overview. J Thromb Haemost. 2007;5(3):604‐606. [DOI] [PubMed] [Google Scholar]
- 11. Adelborg K, Larsen JB, Hvas AM. Disseminated intravascular coagulation: epidemiology, biomarkers, and management. Br J Haematol. 2021;192(5):803‐818. [DOI] [PubMed] [Google Scholar]
- 12. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563‐591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Arendt JFH, Hansen AT, Ladefoged SA, Sørensen HT, Pedersen L, Adelborg K. Existing data sources in clinical epidemiology: laboratory information system databases in Denmark. Clin Epidemiol. 2020;12:469‐475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Henriksen DP, Rasmussen L, Hansen MR, Hallas J, Pottegård A. Comparison of the five Danish regions regarding demographic characteristics, healthcare utilization, and medication use–a descriptive cross‐sectional study. PLoS One. 2015;10(10):e0140197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sundbøll J, Adelborg K, Munch T, et al. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6(11):e012832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adelborg K, Sundbøll J, Munch T, et al. Positive predictive value of cardiac examination, procedure and surgery codes in the Danish National Patient Registry: a population‐based validation study. BMJ Open. 2016;6(12):e012817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaufman R, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205‐213. [DOI] [PubMed] [Google Scholar]
- 19. Wada H, Gabazza EC, Asakura H, et al. Comparison of diagnostic criteria for disseminated intravascular coagulation (DIC): diagnostic criteria of the International Society of Thrombosis and Hemostasis and of the Japanese Ministry of Health and Welfare for overt DIC. Am J Hematol. 2003;74(1):17‐22. [DOI] [PubMed] [Google Scholar]
- 20. Matsumoto T, Wada H, Nishioka Y, et al. Frequency of abnormal biphasic aPTT clot waveforms in patients with underlying disorders associated with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2006;12(2):185‐192. [DOI] [PubMed] [Google Scholar]
- 21. Takemitsu T, Wada H, Hatada T, et al. Prospective evaluation of three different diagnostic criteria for disseminated intravascular coagulation. Thromb Haemost. 2011;105(1):40‐44. [DOI] [PubMed] [Google Scholar]
- 22. Gando S, Saitoh D, Ogura H, et al. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013;17(3):R111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Helms J, Severac F, Merdji H, et al. Performances of disseminated intravascular coagulation scoring systems in septic shock patients. Ann Intensive Care. 2020;10(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Iba T, Nisio MD, Levy JH, Kitamura N, Thachil J. New criteria for sepsis‐induced coagulopathy (SIC) following the revised sepsis definition: a retrospective analysis of a nationwide survey. BMJ Open. 2017;7(9):e017046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


