Abstract
Complement receptor of immunoglobulin superfamily (CRIg) is expressed on liver macrophages and directly binds complement component C3b or Gram-positive bacteria to mediate phagocytosis. CRIg plays important roles in several immune-mediated diseases, but it is not clear how its pathogen recognition and phagocytic functions maintain homeostasis and prevent disease. We previously associated cytolysin-positive Enterococcus faecalis with severity of alcohol-related liver disease. Here, we demonstrate that CRIg is reduced in liver tissues from patients with alcohol-related liver disease. CRIg-deficient mice developed more severe ethanol-induced liver disease than wild-type mice; disease severity was reduced with loss of toll-like receptor 2. CRIg-deficient mice were less efficient than wild-type mice at clearing Gram-positive bacteria such as Enterococcus faecalis that had translocated from gut to liver. Administration of the soluble extracellular domain CRIg–Ig protein protected mice from ethanol-induced steatohepatitis. Our findings indicate that ethanol impairs hepatic clearance of translocated pathobionts, via decreased hepatic CRIg, which facilitates progression of liver disease.
Subject terms: Alcoholic liver disease, Translational research, Monocytes and macrophages
CRIg is expressed on liver macrophages and binds Gram-positive bacteria to mediate phagocytosis, but it is not clear how its phagocytic functions contribute to liver homeostasis or disease. Here the authors report that ethanol impairs hepatic clearance of translocated pathobionts, via decreased hepatic CRIg, which facilitates progression of alcoholic liver disease.
Introduction
Alcohol-related liver disease is the most prevalent liver disease worldwide1–3 and is the leading cause of liver transplantation in the United States4. Within this disease spectrum, alcoholic hepatitis is a severe acute-on-chronic liver failure, which is associated with 90-day mortality rates of 20–50%5–8. Early liver transplantation is the only curative therapy, but is solely available at select centers, to a limited group of patients9–11.
Chronic alcohol consumption leads to intestinal microbial dysbiosis12–14, which contributes to the development and progression of alcohol-associated liver disease15–18. Gut dysbiosis induces gut barrier dysfunction and allows viable bacteria to translocate from the gut to the liver19,20. We recently found that the presence of cytolysin-positive (cytolytic) Enterococcus faecalis (E. faecalis) in the intestine correlated with the severity of liver disease and with mortality in patients with alcoholic hepatitis. Translocated E. faecalis contribute to liver disease by producing cytolysin that can directly cause hepatocyte death17.
Bacteria that breach the intestinal barrier translocate into the blood stream and enter the liver, which serves as a second firewall to prevent their further spread21. Kupffer cells (KC) are the largest population of macrophages in the liver, where they phagocytose bacteria that escaped from the gut and arrived via the portal vein21. Phagocytosis of pathogens depends on opsonins, including antibodies and complement components22. The complement receptor of immunoglobulin superfamily (V-set and immunoglobulin domain containing 4, VSIG4, also called CRIg) is expressed primarily by KC23. CRIg binds to complement component C3b, iC3b and C3c, and mediates the clearance of C3b-opsonized bacteria23,24. CRIg can also directly, and independent of complement, bind to lipoteichoic acid—one of the cell wall components of Gram-positive bacteria—to support hepatic capture of circulating bacteria25. Independent from its phagocytic function, CRIg is able to reverse inflammation in experimental models of arthritis through inhibition of the alternative complement pathway, and has immunomodulatory functions in a mouse model of autoimmune type 1 diabetes26,27. Here, we investigated whether absence of CRIg or administration of a soluble CRIg-Ig protein affects progression of ethanol-induced liver disease via alteration in hepatic clearance of pathobionts.
Results
Liver tissue from patients with alcohol-related liver disease has lower levels of CRIg
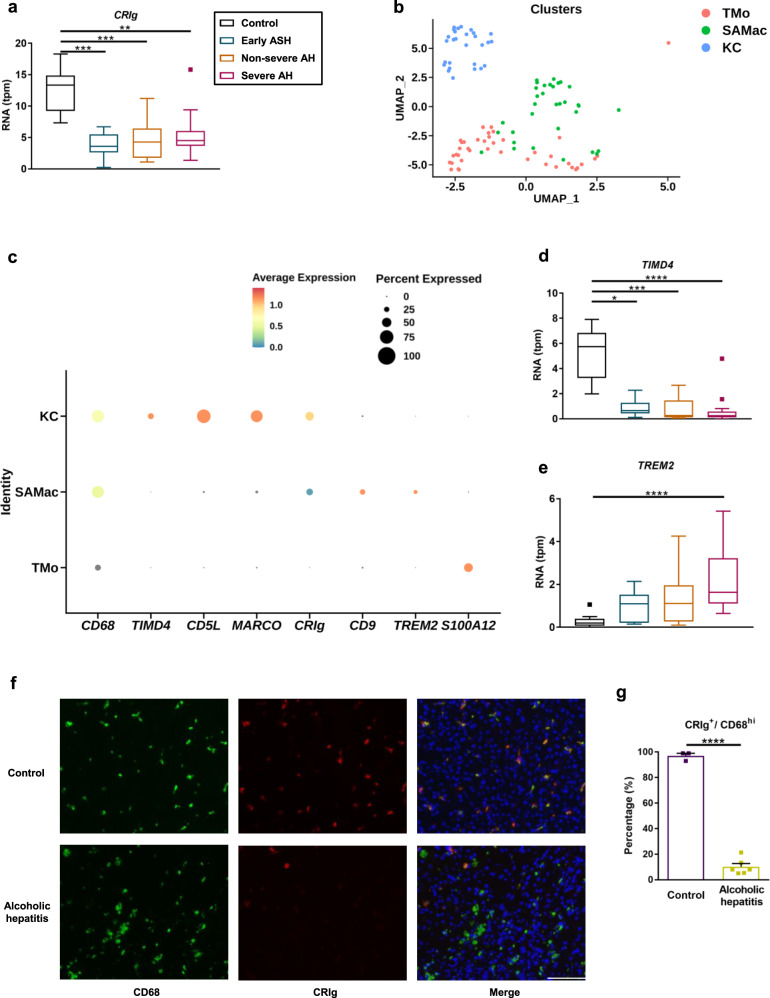
To determine whether patients with alcohol-related liver disease have different hepatic CRIg expression levels, we analyzed RNA sequencing data of liver tissues from subjects without liver disease (controls) and patients with alcohol-related liver disease28. Compared with controls, liver tissues from patients with early alcohol-related steatohepatitis, severe and non-severe alcoholic hepatitis had a lower CRIg mRNA expression (Fig. 1a).
Fig. 1. Patients with alcohol-related liver disease have less CRIg expression on liver macrophages.
a, d, e RNA sequencing data of liver tissues from subjects without liver disease (Control; n = 10), patients with early alcoholic steatohepatitis (Early ASH; n = 12), non-severe alcoholic hepatitis (Non-severe AH; n = 11) and severe alcoholic hepatitis (Severe AH; n = 18). b and c Single-cell RNA sequencing data of liver tissues from subjects without liver disease (uninjured; n = 5) and alcohol-related cirrhotic patients (cirrhotic; n = 2). a mRNA level of CRIg. b UMAP annotating different macrophage cell types as KC (Kupffer cell), TMo (tissue monocyte) and SAMac (scar-associated macrophage). c Dot plot showing expression of CRIg and other stated marker genes in human liver macrophage subpopulations. d mRNA level of TIMD4 (marker for Kupffer cells). e mRNA level of TREM2 (marker for scar-associated macrophages). f Representative liver sections of CD68 and CRIg immunofluorescence staining. g Quantification of the stained liver sections. Scale bar = 100 μm. Results are expressed as median with interquartile range (a, d, e), or mean ± s.e.m. (g). P value is determined by two-sided Kruskal–Wallis test with Dunn’s post-hoc test (a, d, e), or two-sided Student t-test (g). *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Recent single-cell RNA-seq (scRNAseq) studies of healthy and diseased human liver have defined heterogeneity in hepatic macrophages29,30, distinguishing transcriptionally distinct populations of tissue-resident KC, TMo, and scar-associated macrophages (SAMac) which expand in patients with chronic liver disease30. To assess which subpopulations of hepatic macrophages express CRIg in alcohol-related liver disease, we reanalyzed scRNAseq data from healthy and patients with alcohol-related liver disease30. Single cells were annotated as KC, TMo, and SAMac according to the original publication30 (Fig. 1b). CRIg is expressed primarily by KC (Fig. 1c), alongside other previously defined Kupffer cell markers including TIMD4, CD5L and MARCO30. In contrast, SAMac (distinguished by expression of TREM2 and CD9) and TMo (distinguished by expression of S100A12) demonstrate lower expression of CRIg (Fig. 1c). Fewer KC were present in patients with alcohol-related cirrhosis (Fig. 1b and Supplementary Fig. 1a), whilst assessment of marker expression in whole liver tissue demonstrated that patients with alcohol-related liver disease also had reduced expression of other Kupffer cell marker genes (TIMD4, CD5L and MARCO) and increased expression of scar-associated macrophage marker genes (TREM2 and CD9) (Fig. 1d, e and Supplementary Fig. 1b–d). Overall, these data indicate that altered hepatic macrophage composition with a reduction in KC contributes to the lower CRIg expression observed in alcohol-related liver disease.
Consistent with this, patients with alcoholic hepatitis showed a lower percentage of CRIg+/CD68hi cells by immunofluorescence staining, indicating a reduced number of CRIg+ liver macrophages in patients with alcoholic hepatitis (Fig. 1f, g).
To determine regulation of CRIg expression on KC, primary mouse KC were treated with the TLR4 ligand LPS, heat-killed E. faecalis as TLR2 ligand, or inflammatory cytokines TNF and IL1B. All treatment groups showed reduced CRIg mRNA expression relative to control cells (Supplementary Fig. 1e). Taken together, our results indicate that reduced hepatic levels of CRIg in patients with alcohol-related liver disease is likely caused by a combination of inflammation-associated downregulation of CRIg and a reduced number of KC.
We also assessed T cell and neutrophil infiltration in liver tissues of patients with alcoholic hepatitis by H&E staining. Compared to control subjects, the sections of the six explanted livers showed advanced cirrhosis with thick fibrous bands containing mild lymphocytic inflammation and few neutrophils (Supplementary Fig. 1f). Occasional Mallory hyaline is noted which is related to oxidative injury and collapse of the cytoskeleton in the hepatocytes (Supplementary Fig. 1g).
CRIg-deficient mice develop more severe ethanol-induced liver disease
We confirmed previous findings that CRIg is most highly expressed in liver in mice23—expression levels are low in other tissues (Supplementary Fig. 2a). Wild-type mice fed a chronic plus binge ethanol diet31 had significantly lower levels of hepatic CRIg than mice fed an isocaloric (control) diet (Supplementary Fig. 2b).
To study whether CRIg is involved in ethanol-induced liver disease, we fed CRIg-deficient mice and their wild-type littermates a chronic plus binge ethanol diet31. Compared with wild-type mice, CRIg−/− mice developed more severe ethanol-induced liver injury, indicated by a significantly higher level of serum alanine aminotransferase (ALT) (Supplementary Fig. 2c) and increased hepatic steatosis (Supplementary Fig. 2d, e). CRIg−/− mice fed the ethanol diet also had more liver inflammation, expressing significantly higher levels of mRNAs encoding inflammatory cytokines and chemokines (Il1b, Cxcl1, and Cxcl2) (Supplementary Fig. 2f).
To determine whether increased liver damage in CRIg−/− mice was due to less-efficient bacterial clearance and possibly increased signaling from Gram-positive bacteria, we created double mutant-mice, with disruptions in the CRIg gene and toll-like receptor 2 gene (Tlr2). TLR2 is a pattern recognition receptor that binds components of Gram-positive bacteria and activates the inflammatory response, but does not function as phagocytosis receptor32,33. Compared with CRIg−/− mice, mice with disruptions in both CRIg and Tlr2 had less liver injury, steatosis, and inflammation—similar to ethanol-fed wild-type mice (Supplementary Fig. 2c–f). Disruption of CRIg or Tlr2 did not affect intestinal absorption or hepatic metabolism of ethanol, based on serum levels of ethanol and hepatic levels of Adh1 and Cyp2e1 mRNAs, which encode the enzymes that metabolize ethanol in the liver (Supplementary Fig. 2g, h).
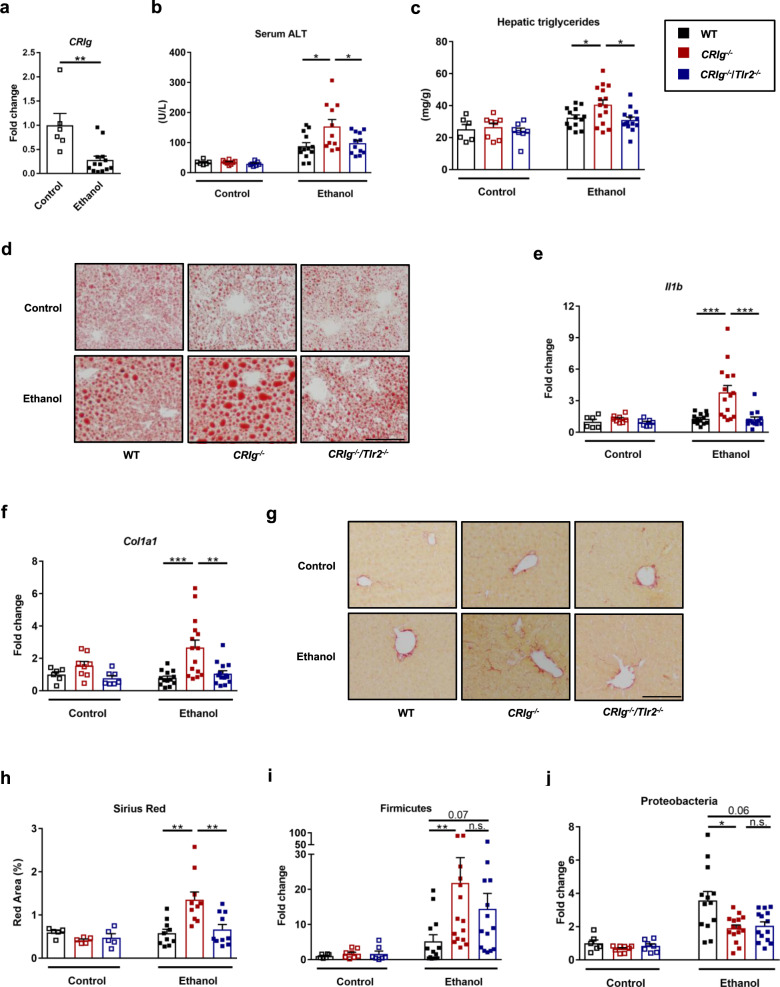
We then studied the effects of CRIg loss in a model of more chronic liver disease, placing mice on an ethanol-containing Lieber DeCarli diet for 8 weeks34. Wild-type mice had reduced hepatic CRIg expression following ethanol feeding (Fig. 2a and Supplementary Fig. 3a, b). Ethanol-fed CRIg−/− mice developed more severe liver injury, steatosis, and inflammation than wild-type mice; the increase in severity was not observed in CRIg−/−/Tlr2−/− mice (Fig. 2b–e, Supplementary Fig. 3c, d). In addition, livers from ethanol-fed CRIg−/− mice had increased expression of genes involved in fibrosis—namely collagen a1(I) (Col1a1) (Fig. 2f) and smooth muscle α-actin (Acta2) (Supplementary Fig. 3e), a marker of activated myofibroblasts and stellate cells, which contribute to the development of fibrosis. Livers from ethanol-fed CRIg−/− mice also had elevated expression of transforming growth factor b1 (Tgfb1) (Supplementary Fig. 3f) and increased fibrosis staining (Fig. 2g, h). To assess whether CRIg deficiency affects liver bacteria, we determined the relative proportion of the Gram-positive phylum Firmicutes, and of the Gram-negative phyla Proteobacteria and Bacteriodetes in the liver. Compared with wild-type mice, CRIg−/− mice had higher proportions of Gram-positive Firmicutes, but lower proportions of Gram-negative Proteobacteria (Fig. 2i, j) and Bacteriodetes (Supplementary Fig. 3g). Wild-type, CRIg−/−, and CRIg−/−/Tlr2−/− mice had similar intestinal absorption and hepatic metabolism of ethanol (Supplementary Fig. 3h, i). We also assessed T cell and neutrophil infiltration in all groups of ethanol-fed mice and did not observe significant differences (Supplementary Fig. 4). Taken together, our results indicate that CRIg deficiency results in more severe ethanol-induced liver damage, and this exacerbation of disease is reduced in the absence of TLR2.
Fig. 2. Deficiency of CRIg causes progression of ethanol-induced liver disease in mice.
Wild-type (WT), CRIg−/−, and CRIg−/−/Tlr2−/− mice were fed the Lieber DeCarli ethanol diet for 8 weeks. a Hepatic level of mRNA encoding CRIg in WT mice. b Serum levels of ALT. c Hepatic triglyceride content. d Representative oil red O-stained liver sections. e and f Hepatic levels of Il1b and Col1a1 mRNAs. g Representative sirius red-stained liver sections. h Quantification of the sirius red-stained liver sections. i and j Hepatic DNA levels of Firmicutes and Proteobacteria, normalized to total amount of bacteria using universal 16S primers. Scale bar = 100 μm. Results are expressed as mean ± s.e.m. (a–c, e, f, h–j). P values among groups of mice fed with control diet or ethanol diet are determined by two-sided Student t-test (a) or one-way ANOVA with Tukey´s post-hoc test (b, c, e, f, h–j). *P < 0.05, **P < 0.01, ***P < 0.001.
CRIg protects from E. faecalis-exacerbated ethanol-induced liver disease
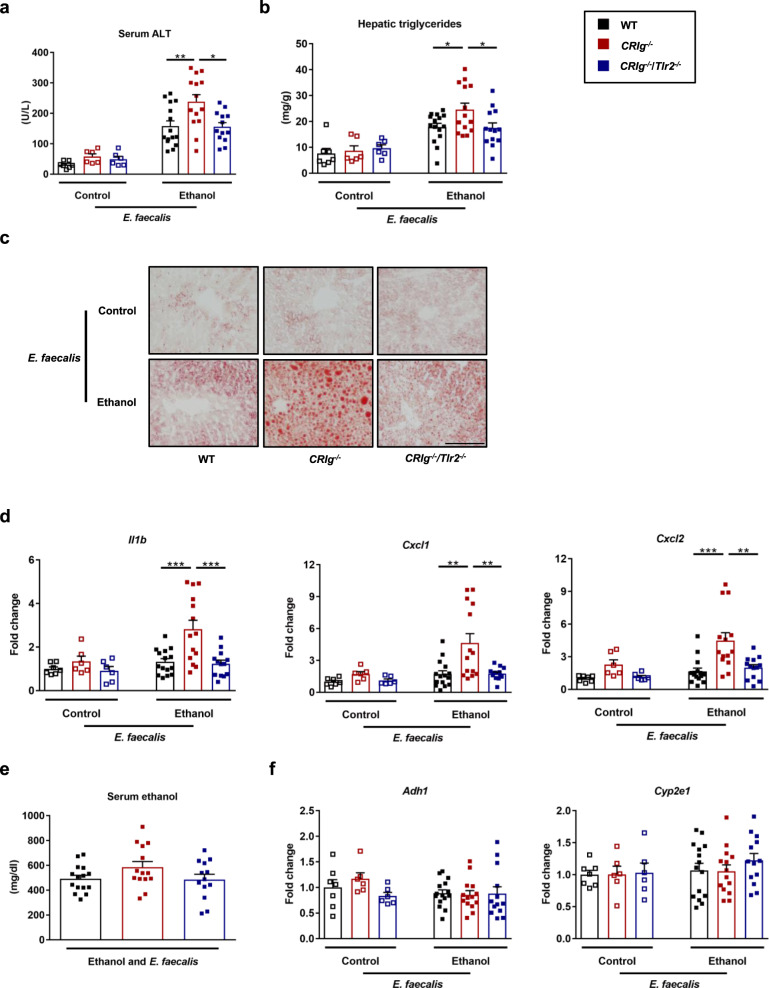
Oral administration of cytolytic E. faecalis promotes ethanol-induced liver disease in wild-type mice17,35. To determine whether CRIg−/− mice are more susceptible to E. faecalis-exacerbated ethanol-induced liver disease, we gavaged mice with a cytolytic strain of E. faecalis35 and placed them on the chronic–binge ethanol diet. CRIg−/− mice developed more severe liver injury, steatosis, and inflammation; this effect was reduced in CRIg−/−/Tlr2−/− mice (Fig. 3a–d). CRIg−/− mice also had more systemic inflammation as indicated by higher levels of circulating cytokines compared with their wild-type littermates and CRIg−/−/Tlr2−/− mice (Supplementary Fig. 5a, b). No significant differences were observed in intestinal absorption and hepatic metabolism of ethanol among the three groups (Fig. 3e, f). These findings provide evidence that CRIg protects against E. faecalis-exacerbation of ethanol-induced liver damage.
Fig. 3. CRIg−/− mice are more susceptible to E. faecalis- and ethanol-induced liver disease.
WT, CRIg−/− and CRIg−/−/Tlr2−/− mice were placed on the chronic–binge ethanol diet and gavaged with a cytolytic E. faecalis strain (5 × 108 colony forming units (CFUs)) every third day. a Serum levels of ALT. b Hepatic triglyceride content. c Representative oil red O-stained liver sections. d Hepatic levels of mRNAs encoding inflammatory cytokines and chemokines IL1B, CXCL1, and CXCL2. e Serum levels of ethanol in ethanol-fed mice. f Hepatic levels of Adh1 and Cyp2e1 mRNAs. Scale bar = 100 μm. Results are expressed as mean ± s.e.m. (a, b, d–f). P values among groups of mice fed with control diet or ethanol diet are determined by one-way ANOVA with Tukey´s post-hoc test (a, b, d–f). *P < 0.05, **P < 0.01, ***P < 0.001.
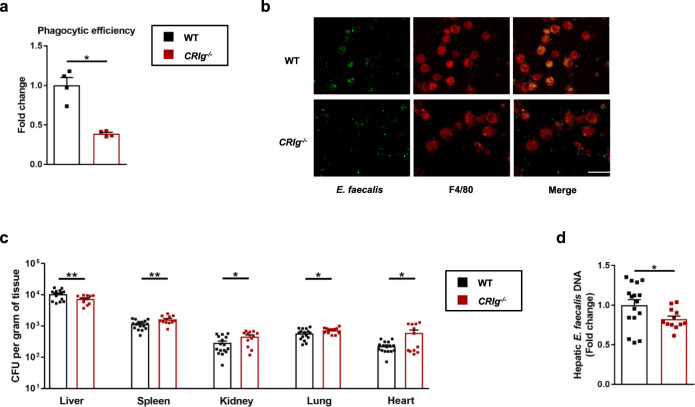
CRIg is required for capturing E. faecalis translocated from gut to the liver
CRIg is important for capturing Gram-positive bacteria Staphylococcus aureus and Listeria monocytogenes that are circulating in the blood23,25. Therefore, ethanol-fed CRIg−/− mice and their wild-type littermates were injected with fluorescently labeled E. faecalis and then KC were isolated. CRIg-deficient KC phagocytosed E. faecalis much less efficiently than KC isolated from wild-type mice (Fig. 4a, b), indicating that CRIg is important for phagocytosis of systemic E. faecalis.
Fig. 4. CRIg is required for capturing of E. faecalis translocated from gut to the liver.
a and b CRIg−/− mice and their WT littermates were placed on a chronic–binge ethanol diet and GFP-E. faecalis (2 × 107 CFUs) was intravenously injected 1 h after ethanol-binge. Mice were sacrificed 1 h after injection and Kupffer cells were isolated. a Quantification of the stained cells. b Representative microscopy pictures. c and d CRIg−/− mice and their WT littermates were fed the chronic-binge ethanol diet. One hour after the ethanol binge, mice were gavaged with E. faecalis (5 × 109 CFUs). Bacterial load (c) and DNA levels (d) were determined 20 min after bacterial gavage. Scale bar = 10 μm. Results are expressed as mean ± s.e.m. (a, c, d). P values determined by two-sided Mann–Whitney test (a, c, d). *P < 0.05, **P < 0.01.
To further characterize the phenotype of CRIg-deficient KC, primary KC were isolated from CRIg−/− mice and their wild-type littermates, and stimulated with LPS. There was no difference in baseline or LPS-induced Il1b, Tnf and Il10 mRNA expression, or in cell viability between wild-type and CRIg-deficient KC (Supplementary Fig. 6a–d).
To determine whether CRIg+ KC are also capable of capturing E. faecalis translocated from gut to the liver, we gavaged ethanol-fed CRIg−/− mice and their wild-type littermates with fluorescently labeled E. faecalis. Due to deficiency in phagocytosis of KC, the number of translocated E. faecalis recovered from ethanol-fed CRIg−/− mice were significantly lower in the liver but significantly higher in the spleen, kidney, lung, and heart shortly after ethanol binge (Fig. 4c, d). These data indicate that fewer translocated bacteria are captured in CRIg−/− livers, resulting in increased numbers in the circulation and other organs. CRIg therefore captures E. faecalis that translocated from gut to liver.
Extracellular domain of CRIg protects mice from ethanol-induced liver disease
muCRIg contains two regions—an extracellular region consisting of one immunoglobulin-like domain (CRIg-Ig) and an intracellular region with the transmembrane domain23. CRIg-Ig binds Gram-positive bacteria such as S. aureus, L. monocytogenes, Bacillus cereus, and Enterococcus faecium25. We confirmed that CRIg-Ig binds to Gram-positive E. faecalis, but not Gram-negative E. coli in vitro (Supplementary Fig. 7a). To determine whether CRIg-Ig is capable of binding to E. faecalis translocated from gut to the liver, ethanol-fed wild-type mice were injected with CRIg-Ig or control-Ig, and gavaged with fluorescently labeled E. faecalis. The number of translocated E. faecalis recovered from mice with CRIg-Ig were significantly lower in the liver but higher in other organs (Fig. 5a), indicating that translocated E. faecalis bound to CRIg-Ig escape Kupffer cell phagocytosis. We next determined whether E. faecalis bound to CRIg are recognized by TLR2. E. faecalis were incubated with CRIg-Ig or control-Ig, and used to stimulate primary mouse KC. E. faecalis incubated with control-Ig induced a stronger inflammatory response as compared with E. faecalis incubated and bound to CRIg-Ig (Supplementary Fig. 7b), indicating that E. faecalis binding to CRIg-Ig interferes with their ability to bind pattern recognition receptors such as TLR2.
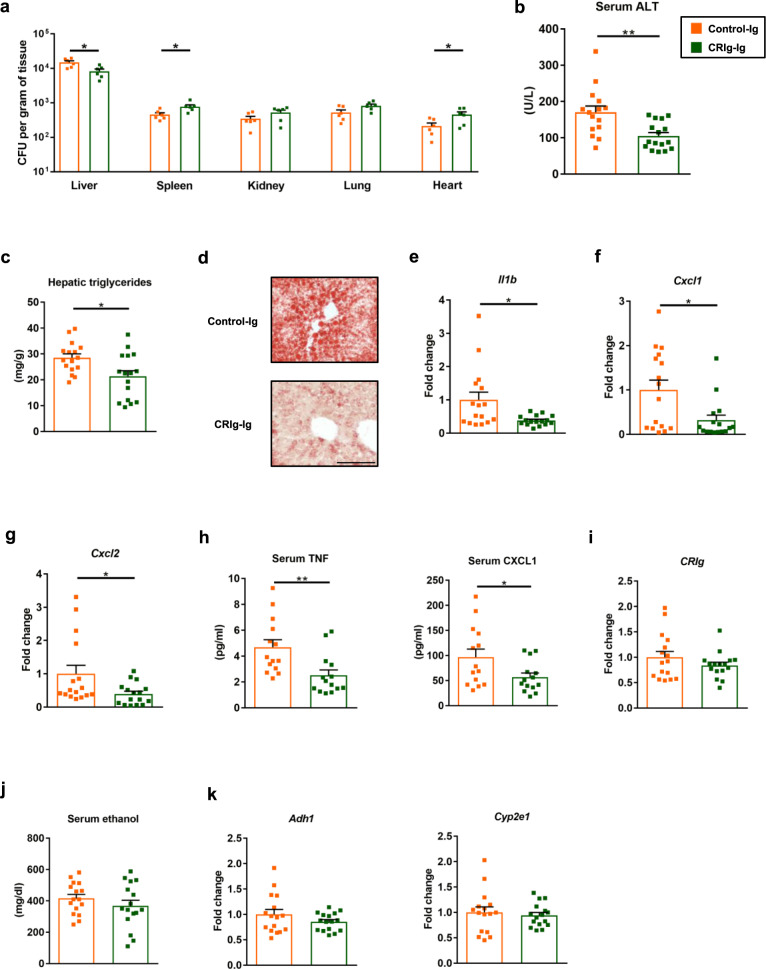
Fig. 5. Extracellular region of CRIg protects mice from ethanol-induced liver disease.
WT mice were fed the chronic–binge ethanol diet. a One hour after the ethanol binge, mice were given intravenous injections of control-Ig or CRIg-Ig (12 mg/kg body weight [BW]) and gavaged with E. faecalis (5 × 109 CFUs). Bacterial load was determined 20 min after bacterial gavage. b–k One day before the ethanol binge, mice were given intravenous injections of control-Ig or CRIg-Ig (12 mg/kg body weight [BW]). b Serum levels of ALT. c Hepatic triglyceride content. d Representative oil red O-stained liver sections. e–g Hepatic levels of mRNAs encoding inflammatory cytokines and chemokines IL1B, CXCL1, and CXCL2. h Serum levels of inflammatory cytokines and chemokines TNF and CXCL1. i Hepatic level of mRNA encoding CRIg. j Serum levels of ethanol. k Hepatic levels of Adh1 and Cyp2e1 mRNAs. Scale bar = 100 μm. Results are expressed as mean ± s.e.m (a–c, e–k). P values determined by two-sided Student’s t-test (a–c, e–k). *P < 0.05, **P < 0.01.
We then investigated whether CRIg-Ig protects mice from ethanol-induced liver disease. Wild-type mice were fed a chronic-binge ethanol diet and then given intravenous injections of CRIg-Ig or control-Ig. Mice injected with CRIg-Ig developed less-severe liver injury (Fig. 5b), steatosis (Fig. 5c, d), hepatic inflammation (Fig. 5e–g) and systemic inflammation (Fig. 5h) than mice given the control-Ig but had no change in hepatic levels of CRIg or intestinal absorption or hepatic metabolism of ethanol (Fig. 5i–k). Together, our results indicate that CRIg protects against ethanol-related liver disease and might be developed as a therapeutic agent for alcohol-induced liver injury.
Discussion
CRIg serves not only as a complement receptor, but is also important for pathogen recognition and clearance23,25. We recently showed that cytolysin-positive E. faecalis are increased in the intestine of patients with severe alcoholic hepatitis and their abundance correlates with mortality. These pathobionts escape the intestinal firewall21 and translocate to the liver, where they produce cytolysin, which damages hepatocytes17. In this study, we demonstrate that alcohol has detrimental effects on the liver as second firewall. Alcohol-related liver injury results in altered hepatic macrophage composition and phenotype, with a reduced number of CRIg+ KC ultimately attenuating the clearance of pathogenic bacteria. Mice deficient in CRIg developed more severe ethanol-induced liver disease than wild-type mice and had greater exacerbation of liver disease following oral administration of E. faecalis and ethanol feeding. Circulating E. faecalis are recognized by TLR2, a pattern recognition receptor that binds molecular patterns of Gram-positive bacteria, resulting in hepatic inflammation and chronic liver damage (Fig. 6). Ethanol therefore contributes to liver disease not only via its direct toxic effects on liver cells, but also by increasing intestinal passage of microbes into the blood stream and reducing liver CRIg expression, preventing clearance of bacteria from the liver.
Fig. 6. Alcohol reduces the clearance of pathobionts by Kupffer cells and contributes to liver disease.
Left panel: During homeostasis, translocation of pathobionts from the gut to the liver is a rare event. Translocated E. faecalis are cleared and phagocytosed by CRIg on Kupffer cells. Right panel: Chronic alcohol consumption results in intestinal expansion of E. faecalis. These pathobionts escape the intestinal barrier and translocate to the liver. Alcohol changes hepatic macrophage composition and phenotype, and downregulates CRIg on Kupffer cells, thus contributing to reduced CRIg expression in the liver and reducing clearance of translocated E. faecalis. Hepatic and circulating E. faecalis are recognized by TLR2, a pattern recognition receptor that binds Gram-positive bacteria, resulting in hepatic inflammation and progression of alcoholic liver disease.
We also showed that the effects of ethanol-mediated downregulation of CRIg on KC can be overcome by administration of soluble CRIg-Ig, which protects mice from ethanol-induced liver disease. As a complement receptor, CRIg modulates the immune system via different mechanisms. It binds to the activated complement component C3b and inhibits the alternative pathway of complement24. Soluble CRIg-Ig protein has been shown to have beneficial effects in models of autoimmune disease. The extracellular domain of CRIg prevents inflammation and bone loss in a mouse model of arthritis26. Administration of CRIg-Ig protein inhibits development of type I diabetes36, by attenuating proliferation of effector T cells and promoting differentiation and stability of T-regulatory cells27,37. CRIg helps maintain endogenous liver T- and natural killer T-cell tolerance to prevent concanavalin A-induced hepatitis38.
Little is known about the mechanisms by which CRIg modulates T-cell activity39. Although we cannot rule out that CRIg-Ig has beneficial T-cell modulatory effects, alcohol-associated liver disease is not considered to be mediated by a T-cell immune response. Furthermore, CRIg was shown to upregulate pyruvate dehydrogenase kinase-2 (PDK2) and reduce secretion of mitochondrial reactive oxygen species by macrophages, which inhibits their activation and inflammation in murine hepatitis virus strain-3 (MHV-3)-induced fulminant hepatitis40. We did not find a significant difference in expression of Pdk2 among the groups of mice in all of our models, indicating that the exacerbation of ethanol-induced liver injury in CRIg−/− mice was not due to a lower level of PDK2. In our model, CRIg-Ig acts as decoy receptor for Gram-positive pathobionts—it obscures their pathogen-associated molecular pattern and prevents activation of pathogen recognition receptors such as TLR2. Soluble CRIg-Ig protein might therefore be developed as a therapeutic agent for patients with alcoholic hepatitis, which has limited treatment options.
In summary, we describe a novel mechanism by which alcohol causes failure of the hepatic firewall, by changing hepatic macrophage composition and phenotype, thus contributing to reduced CRIg expression in the liver. Reduced CRIg results in decreased removal of translocating pathobionts, which might not only contribute to more severe liver disease, but also to an increased rate of systemic infections in patients with end-stage liver disease (cirrhosis) or alcoholic hepatitis. CRIg is therefore an attractive target for treatment of alcohol-associated liver diseases.
Methods
Human study
Liver explants from six patients with severe alcoholic hepatitis, who underwent liver transplantation, and three liver tissues from donors (control) were obtained from Clinical Resource for Alcoholic Hepatitis Investigations (NIH R24 AA025017) at Johns Hopkins University (Baltimore, MD). Tissues were excised from explanted livers in patients with severe alcoholic hepatitis during liver transplantation, or wedge biopsies from the donor livers. The protocol was approved by the Johns Hopkins Medicine Institutional Review Boards (IRB00107893) and patients were enrolled after written informed consent was obtained.
Mice
C57BL/6 mice were purchased from Charles River and used in Fig. 5 and Supplementary Fig. 2a. All mice used in other figures were bred in the animal facility at University of California, San Diego (La Jolla, CA). CRIg−/− mice on a C57BL/6 background have been described (Genentech)23,27). Heterozygous female (+/−) and wild-type (y/+) or knock-out (y/−) male mice were used for breeding. CRIg−/−/Tlr2−/− mice on a C57BL/6 background were generated by crossing CRIg−/− mice with Tlr2−/− mice.
Male mice (age, 9–12 weeks) were placed on a chronic–binge ethanol diet (NIAAA model) as described17. Mice were fed with the Lieber–DeCarli diet and the caloric intake from ethanol was 0% on days 1–5 and 36% from day 6 until the end of the study period. At day 16, mice were gavaged with a single dose of ethanol (5 g/kg body weight) in the early morning and sacrificed 9 h later. Pair-fed control mice received a diet with an isocaloric substitution of dextrose.
Female mice (age, 9–12 weeks) were placed on Lieber DeCarli diet for 8 weeks as previously described34. The caloric intake from ethanol was 0% on day 1, 10% on days 2 and 3, 20% on days 4 and 5, 30% from day 6 until the end of 6 weeks, and 36% for the last 2 weeks. On the last day, mice were gavaged with a single dose of ethanol (5 g/kg body weight) in the early morning and sacrificed 9 h later. Pair-fed control mice received a diet with an isocaloric substitution of dextrose.
To study the effect of E. faecalis on CRIg−/− and CRIg−/−/Tlr2−/− mice, E. faecalis (5 × 108 colony forming units (CFUs)) were gavaged every third day, starting from day 6 through day 15 of ethanol feeding (see above). Administration every third day was necessary, given that E. faecalis does not colonize mice17.
In studies using CRIg-Ig, wild-type male mice were placed on a chronic–binge ethanol feeding model. CRIg-Ig or control-Ig (12 mg/kg BW) were injected intravenously 1 day before ethanol binge. CRIg-Ig was obtained from Genentech and was generated by fusing the extracellular domain of CRIg to the Fc portion of murine IgG123. Murine anti-gp120 IgG1 (Bio X Cell) was used as control Ig as described23,27.
Mice were housed with a light cycle of 12 h of light (6 a.m.–6 p.m.) and a dark cycle of 12 h of darkness (6 p.m.–6 a.m.) at a temperature between 20 and 22 °C and a relative humidity between 40% and 70%. All animal studies were reviewed and approved by the Institutional Animal Care and Use Committee of the University of California, San Diego. The studies were performed in accordance with all relevant ethical regulations regarding the use of research animals.
RNA sequencing
Previously published high-throughput transcriptome profiling by RNA sequencing with liver samples was used as described28. 41 patients with different phenotypes were selected: 12 patients with early alcoholic steatohepatitis, 11 patients with non-severe alcoholic hepatitis (with Maddrey discriminant function (MDF ≤ 32), and 18 patients with severe alcoholic hepatitis (MDF > 32). Controls (n = 10) were non-diseased livers obtained from biopsied single nodules, whose histology was without significant alterations. Transcripts were quantified using RSEM package41. Data was normalized and expressed as Transcripts Per Kilobase Million or TPM. The raw and phenotypic data are available through the Database of Genotypes And Phenotypes (dbGAP) of the National Center for Biotechnology Information (NCBI) under the Study Accession Id phs001807.v1.p1.
Single cell RNA sequencing analysis
Previously published scRNAseq data following QC and annotation30 was downloaded from a publicly available server42. All analysis was performed in the Seurat R package (version 3.2.3). Data was initially subsetted only for cells from the 5 healthy and 2 alcohol-related cirrhotic livers (patient IDs cirrhotic 2 and cirrhotic 3)30. Cells from these patients which were annotated as mononuclear phagocytes (MP) based on the original published analyses were isolated for re-analysis, using the built-in functions of Seurat to normalize the cells per 10,000 transcripts and then log(x + 1) transformed allowing the resulting values to be scaled. Finally, the uniform Approximation and Projection Method (UMAP) was used to construct a data visualization graph using 1 to 10 principal components as determined by the dataset variability shown in principal component analysis (PCA). For this analysis, the genes of interest included “CD68”, “TIMD4”, “CD5L”, “MARCO”, “CRIg”, “CD9”, “TREM2” and “S100A12”. To identify how the expression of these genes differ between cells previously annotated as tissue monocytes (TMo), scar-associated macrophages (SAMac) and Kupffer cells (KC) in healthy and alcohol-related liver disease liver tissue, UMAP visualizations, violin plots and dot plots were generated using Seurat functions in conjunction with the ggplot2 package.
Immunofluorescence staining
Liver sections were embedded in OCT compound. 5 μm frozen sections were then cut. To determine CRIg expression levels in controls and patients with alcoholic hepatitis, liver sections were stained with anti-huCRIg (1:500) (Genentech) and anti-CD68 (1:200) (Agilent Dako) primary antibodies. To determine CRIg expression levels in control- and ethanol-fed mice, liver sections were stained with anti-muCRIg (1:5,000) (Genentech) and anti-F4/80 (1:50) (Biolegend) primary antibodies. To determine T cell and neutrophil infiltration in all groups of ethanol-fed mice, liver sections were stained with anti-CD3e (1:300) (Biolegend) and anti-Ly6G (1:200) (Biolegend) primary antibodies. Representative pictures from both groups are shown. Five high-power fields of each sample were randomly selected for quantification using ImageJ and Qupath43.
Real-time quantitative PCR
RNA was extracted from mouse tissues and cDNA was generated17. Primer sequences for mouse genes were obtained from the NIH qPrimerDepot. All primers used in this study are listed in Supplementary Table 1. Gene expression was determined with Sybr Green (Bio-Rad Laboratories) using ABI StepOnePlus real-time PCR system. The qPCR value was normalized to 18S.
Bacterial culture
To make GFP producing E. faecalis, 1 μg of the plasmid pBSU10144 was transformed into a cytolytic E. faecalis strain35. All E. faecalis strains were grown statically in brain heart infusion (BHI) broth or on BHI agar plate at 37 °C. 125 μg/ml spectinomycin was added when GFP-produced E. faecalis strain was grown.
Kupffer cell isolation and cell culture experiments
Primary mouse Kupffer cells were isolated by two-step collagenase-pronase perfusion followed by three-layer discontinuous density gradient centrifugation with 8.2% (w/v) and 14.5% (w/v) Nycodenz (Accurate Chemical and Scientific Corporation) to obtain Kupffer-cell fraction. 5 × 105 Kupffer cells were plated on six-well plates and cultured with RPMI 1640 medium (Fisher Scientific) containing 10% (v/v) FBS. RNA was extracted and used for qPCR. Cell culture medium was replaced to be RPMI 1640 without serum, before the stimulation started. Kupffer cells from CRIg−/− mice and their wild-type littermates were isolated and treated with PBS as vehicle, LPS (ENZO Life Sciences; 10 ng/ml), heat-killed E. faecalis (MOI 10:1), TNF (R&D Systems; 2 ng/ml), or IL1B (R&D Systems; 2 ng/ml) for 8 h. To check whether CRIg-bound E. faecalis can activate pathogen recognition receptor signaling, CRIg-Ig (100 μg/ml) or control-Ig (100 μg/ml) was incubated with 105 E. faecalis at room temperature for 2 h and fixed by 1% paraformaldehyde. Bacteria were washed three times with PBS, and Kupffer cells were stimulated for 8 h.
To determine cell viability, Kupffer cells from CRIg−/− mice and their wild-type littermates were isolated and plated on 96-well plates, cultured with RPMI 1640 medium (Fisher Scientific) containing 10% (v/v) FBS overnight. Fresh medium was then changed, and lactate dehydrogenase was measured 4 h following medium change in the supernatant (Fisher Scientific).
Confocal microscopy
CRIg−/− mice and their wild-type littermates were subjected to the chronic–binge ethanol feeding model. One hour after ethanol-binge, GFP-E. faecalis (2 × 107 CFUs) was injected intravenously. Animals were sacrificed 1 h after bacterial injection and hepatic Kupffer cells were isolated. Cells were then stained with APC anti-F4/80 antibody (BioLegend) and sorted using anti-APC microbeads (Miltenyi Biotec). Before microscopy, cells were put on poly-l-lysine-coated slides. Pictures were taken with ×630 magnification. For quantification, five high-power fields of each sample were randomly selected and the number of internalized GFP-E. faecalis was counted. The phagocytic index was then calculated.
Bacterial load
To determine bacterial load from different tissues, mice were placed on the chronic–binge ethanol diet. One hour after the ethanol binge, E. faecalis (5 × 109 CFUs) were gavaged to each mouse. Animals were sacrificed 20 min after bacteria gavage and tissues were harvested. Each tissue was weighed and resuspended into 500 μl PBS. 100 μl of each homogenized tissue sample was then plated onto a BHI agar plate with 125 μg/ml spectinomycin; the plates were then incubated at 37 °C overnight. Colony numbers of each sample were then counted and CFUs were calculated.
Flow cytometry of CRIg binding to bacteria
CRIg-Ig protein was labeled with Alexa Fluor 647 using a protein labeling kit (Fisher Scientific). Labeled CRIg-Ig was incubated with E. faecalis (2 × 105 CFUs) or E. coli (2 × 105 CFUs) at room temperature for 2 h. Bacteria were washed three times with PBS, resuspended in 1% paraformaldehyde, fixed on ice for 30 min, and subjected to flow cytometry, using the software SpectroFlo 2.2.0.
Biochemical analysis
Serum levels of ALT were determined using Infinity ALT kit (Thermo Scientific). Hepatic triglyceride levels were measured using Triglyceride Liquid Reagents kit (Pointe Scientific). Serum levels of ethanol were measured using Ethanol Assay kit (BioVision). Serum levels of cytokines were measured using Proinflammatory Panel 1 (mouse) kit (Meso Scale Diagnostics). All results were measured using the software SoftMax Pro 7.0.3.
Staining procedures
To determine lipid accumulation, liver sections were embedded in OCT compound. 8 μm frozen sections were then cut and stained with Oil Red O (Sigma-Aldrich). To check liver fibrosis, formalin-fixed tissue samples were embedded in paraffin and stained with Sirius red. Five high-power fields were randomly selected for quantification.
Statistical analysis
Results are expressed as mean ± s.e.m. (except when stated otherwise). Significance of two groups or multiple groups were evaluated using two-sided unpaired Student’s t-test, two-sided unpaired Mann–Whitney test, one-way analysis of variance (ANOVA) with Tukey’s post-hoc test, Kruskal–Wallis test with Dunn’s post-hoc test, or two-way ANOVA, respectively. Exact P values for all comparisons, together with group size for each group, were listed in Supplementary Data 1. All results were generated from at least two independent technical replicates. Statistical analyses were performed using GraphPad Prism v7.04. A P < 0.05 was considered to be statistically significant (adjusted for multiple comparison when performing multiple tests).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
We thank Dr. M. van Lookeren Campagne (Genentech) for insightful discussions and for kindly providing CRIg-deficient mice and CRIg-Ig protein. This study was supported in part by a Biocodex Microbiota Foundation Grant, NIH grants R01 AA024726, R37 AA020703, U01 AA026939, U01 AA026939-S1, by Award Number BX004594 from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development (to B.S.), NIH grant U01AA026972 (to R.B.), NIH grant U01 AA027681 and R37AI043477 (to M.K.) and services provided by P30 DK120515 and P50 AA011999. Human liver biopsies were obtained from Johns Hopkins University supported by NIH grant R24 AA025017. H.C. was supported by Science Research Foundation from Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (02.03.2018-239), Natural Science Foundation of Hubei Province (02.07.19040037.03) and National Natural Science Foundation of China (grant number 82000561). P.R. was supported by UK MRC Clinician Scientist Fellowship (MR/N008340/1).
Source data
Author contributions
Y.D. was responsible for acquisition, analysis and interpretation of data, and drafting of the manuscript; H.C. was responsible for acquisition, analysis and interpretation of data; K.B., L.J., S.Z., N.M., E.P., J.A., B.G.M., Y.W., H.S., W.S., C.L., T.H., X.L. and M.H. provided assistance on data acquisition; T.K., D.A.B., R.B., P.R., M.K. and W.F. provided materials and technical support; B.S. was responsible for the study concept and design, study supervision and editing the manuscript.
Peer review information
Nature Communications thanks Claudia Kemper, Cynthia Ju and the other anonymous reviewer(s) for their contribution to the peer review this work.
Data availability
The data that support the findings of this study are available from the author (B.S.) upon reasonable request. Source data are provided as a Source Data file. Original raw single-cell RNA-seq data have been deposited in the Gene Expression Omnibus (GEO) under accession GSE136103 and processed/annotated data available from https://datashare.ed.ac.uk/handle/10283/343342. Original raw and phenotypic data from liver RNA sequencing are available through the Database of Genotypes And Phenotypes (dbGAP) of the National Center for Biotechnology Information (NCBI) under the Study Accession ID phs001807.v1.p128. Source data are provided with this paper.
Competing interests
B.S. has been consulting for Ferring Research Institute, Intercept Pharmaceuticals, HOST Therabiomics, Mabwell Therapeutics, Patara Pharmaceuticals and Takeda. B.S.’s institution UC San Diego has received grant support from BiomX, NGM Biopharmaceuticals, CymaBay Therapeutics, Synlogic Operating Company, Prodigy Biotech and Axial Biotherapeutics. B.S. is founder of Nterica Bio. UC San Diego has filed several patents with B.S. as inventor related to this work. The remaining authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yi Duan, Huikuan Chu.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-021-27385-3.
References
- 1.Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J. Hepatol. 2013;59:160–168. doi: 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Rehm J, et al. Burden of disease associated with alcohol use disorders in the United States. Alcohol.: Clin. Exp. Res. 2014;38:1068–1077. doi: 10.1111/acer.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee BP, Vittinghoff E, Dodge JL, Cullaro G, Terrault NA. National trends and long-term outcomes of liver transplant for alcohol-associated liver disease in the United States. JAMA Intern. Med. 2019;179:340–348. doi: 10.1001/jamainternmed.2018.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maddrey WC, et al. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–199. [PubMed] [Google Scholar]
- 6.Mathurin P, et al. Early change in bilirubin levels is an important prognostic factor in severe alcoholic hepatitis treated with prednisolone. Hepatology. 2003;38:1363–1369. doi: 10.1016/j.hep.2003.09.038. [DOI] [PubMed] [Google Scholar]
- 7.Forrest EH, et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut. 2005;54:1174. doi: 10.1136/gut.2004.050781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dominguez M, et al. A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am. J. Gastroenterol. 2008;103:2747–2756. doi: 10.1111/j.1572-0241.2008.02104.x. [DOI] [PubMed] [Google Scholar]
- 9.Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N. Engl. J. Med. 2009;360:2758–2769. doi: 10.1056/NEJMra0805786. [DOI] [PubMed] [Google Scholar]
- 10.Mathurin P, Lucey MR. Management of alcoholic hepatitis. J. Hepatol. 2012;56:S39–S45. doi: 10.1016/S0168-8278(12)60005-1. [DOI] [PubMed] [Google Scholar]
- 11.Thursz MR, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N. Engl. J. Med. 2015;372:1619–1628. doi: 10.1056/NEJMoa1412278. [DOI] [PubMed] [Google Scholar]
- 12.Gao B, et al. Functional microbiomics reveals alterations of the gut microbiome and host co-metabolism in patients with alcoholic hepatitis. Hepatol. Commun. 2020;4:1168–1182. doi: 10.1002/hep4.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang L, et al. Intestinal virome in patients with alcoholic hepatitis. Hepatology. 2020;72:2182–2196. doi: 10.1002/hep.31459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lang S, et al. Intestinal fungal dysbiosis and systemic immune response to fungi in patients with alcoholic hepatitis. Hepatology. 2020;71:522–538. doi: 10.1002/hep.30832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lang S, et al. Changes in the fecal bacterial microbiota associated with disease severity in alcoholic hepatitis patients. Gut Microbes. 2020;12:1785251. doi: 10.1080/19490976.2020.1785251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu H, et al. The Candida albicans exotoxin candidalysin promotes alcohol-associated liver disease. J. Hepatol. 2020;72:391–400. doi: 10.1016/j.jhep.2019.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duan Y, et al. Bacteriophage targeting of gut bacterium attenuates alcoholic liver disease. Nature. 2019;575:505–511. doi: 10.1038/s41586-019-1742-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong W, et al. Paneth cell dysfunction mediates alcohol-related steatohepatitis through promoting bacterial translocation in mice: role of zinc deficiency. Hepatology. 2020;71:1575–1591. doi: 10.1002/hep.30945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stärkel P, Schnabl B. Bidirectional communication between liver and gut during alcoholic liver disease. Semin. Liver Dis. 2016;36:331–339. doi: 10.1055/s-0036-1593882. [DOI] [PubMed] [Google Scholar]
- 20.Lang S, Schnabl B. Microbiota and fatty liver disease—the known, the unknown, and the future. Cell Host Microbe. 2020;28:233–244. doi: 10.1016/j.chom.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balmer ML, et al. The liver may act as a firewall mediating mutualism between the host and its gut commensal microbiota. Sci. Transl. Med. 2014;6:237ra266. doi: 10.1126/scitranslmed.3008618. [DOI] [PubMed] [Google Scholar]
- 22.Flannagan RS, Jaumouillé V, Grinstein S. The cell biology of phagocytosis. Annu. Rev. Pathol. 2012;7:61–98. doi: 10.1146/annurev-pathol-011811-132445. [DOI] [PubMed] [Google Scholar]
- 23.Helmy KY, et al. CRIg: a macrophage complement receptor required for phagocytosis of circulating pathogens. Cell. 2006;124:915–927. doi: 10.1016/j.cell.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 24.Wiesmann C, et al. Structure of C3b in complex with CRIg gives insights into regulation of complement activation. Nature. 2006;444:217–220. doi: 10.1038/nature05263. [DOI] [PubMed] [Google Scholar]
- 25.Zeng Z, et al. CRIg functions as a macrophage pattern recognition receptor to directly bind and capture blood-borne Gram-positive bacteria. Cell Host Microbe. 2016;20:99–106. doi: 10.1016/j.chom.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Katschke KJ, Jr., et al. A novel inhibitor of the alternative pathway of complement reverses inflammation and bone destruction in experimental arthritis. J. Exp. Med. 2007;204:1319–1325. doi: 10.1084/jem.20070432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yuan X, Yang B-H, Dong Y, Yamamura A, Fu W. CRIg, a tissue-resident macrophage specific immune checkpoint molecule, promotes immunological tolerance in NOD mice, via a dual role in effector and regulatory T cells. Elife. 2017;6:e29540. doi: 10.7554/eLife.29540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Argemi J, et al. Defective HNF4alpha-dependent gene expression as a driver of hepatocellular failure in alcoholic hepatitis. Nat. Commun. 2019;10:3126. doi: 10.1038/s41467-019-11004-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacParland SA, et al. Single cell RNA sequencing of human liver reveals distinct intrahepatic macrophage populations. Nat. Commun. 2018;9:4383. doi: 10.1038/s41467-018-06318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramachandran P, et al. Resolving the fibrotic niche of human liver cirrhosis at single-cell level. Nature. 2019;575:512–518. doi: 10.1038/s41586-019-1631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bertola A, Mathews S, Ki SH, Wang H, Gao B. Mouse model of chronic and binge ethanol feeding (the NIAAA model) Nat. Protoc. 2013;8:627–637. doi: 10.1038/nprot.2013.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moresco EMY, LaVine D, Beutler B. Toll-like receptors. Curr. Biol. 2011;21:R488–R493. doi: 10.1016/j.cub.2011.05.039. [DOI] [PubMed] [Google Scholar]
- 33.Yimin, et al. Contribution of toll-like receptor 2 to the innate response against Staphylococcus aureus infection in mice. PLoS ONE. 2013;8:e74287. doi: 10.1371/journal.pone.0074287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chu H, et al. The selective PPAR-delta agonist seladelpar reduces ethanol-induced liver disease by restoring gut barrier function and bile acid homeostasis in mice. Transl. Res. 2021;227:1–14. doi: 10.1016/j.trsl.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Llorente C, et al. Gastric acid suppression promotes alcoholic liver disease by inducing overgrowth of intestinal Enterococcus. Nat. Commun. 2017;8:837. doi: 10.1038/s41467-017-00796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fu W, Wojtkiewicz G, Weissleder R, Benoist C, Mathis D. Early window of diabetes determinism in NOD mice, dependent on the complement receptor CRIg, identified by noninvasive imaging. Nat. Immunol. 2012;13:361–368. doi: 10.1038/ni.2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vogt L, et al. VSIG4, a B7 family-related protein, is a negative regulator of T cell activation. J. Clin. Investig. 2006;116:2817–2826. doi: 10.1172/JCI25673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jung K, et al. Protective role of V-set and immunoglobulin domain-containing 4 expressed on kupffer cells during immune-mediated liver injury by inducing tolerance of liver T- and natural killer T-cells. Hepatology. 2012;56:1838–1848. doi: 10.1002/hep.25906. [DOI] [PubMed] [Google Scholar]
- 39.van Lookeren Campagne M, Verschoor A. Pathogen clearance and immune adherence “revisited”: immuno-regulatory roles for CRIg. Semin. Immunol. 2018;37:4–11. doi: 10.1016/j.smim.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Li J, et al. VSIG4 inhibits proinflammatory macrophage activation by reprogramming mitochondrial pyruvate metabolism. Nat. Commun. 2017;8:1322. doi: 10.1038/s41467-017-01327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li B, Dewey CN. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinforma. 2011;12:323. doi: 10.1186/1471-2105-12-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramachandran, P., Henderson, N. & Wilson-Kanamori, J. R. Resolving the fibrotic niche of human liver cirrhosis at single-cell level - Seurat RData object. (University of Edinburgh Centre for Inflammation Research, 2019). [DOI] [PMC free article] [PubMed]
- 43.Bankhead P, et al. QuPath: open source software for digital pathology image analysis. Sci. Rep. 2017;7:16878. doi: 10.1038/s41598-017-17204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aymanns S, Mauerer S, van Zandbergen G, Wolz C, Spellerberg B. High-level fluorescence labeling of Gram-positive pathogens. PLoS ONE. 2011;6:e19822. doi: 10.1371/journal.pone.0019822. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The data that support the findings of this study are available from the author (B.S.) upon reasonable request. Source data are provided as a Source Data file. Original raw single-cell RNA-seq data have been deposited in the Gene Expression Omnibus (GEO) under accession GSE136103 and processed/annotated data available from https://datashare.ed.ac.uk/handle/10283/343342. Original raw and phenotypic data from liver RNA sequencing are available through the Database of Genotypes And Phenotypes (dbGAP) of the National Center for Biotechnology Information (NCBI) under the Study Accession ID phs001807.v1.p128. Source data are provided with this paper.