Abstract
Objective: To explore the possible influence of painless delivery on the maternal and neonatal outcomes under the guidance of new concept of labor. Methods: Primiparas who received painless delivery in our hospital were selected for this retrospective clinical study. They were divided into two groups, the experimental group and the control group. The experimental group received painless delivery with the application of new labor management, while the control group received painless delivery with the application of routine labor management. The maternal and neonatal outcomes (postpartum hemorrhage, postpartum urinary retention, fetal distress and neonatal asphyxia), the duration of first and second stages of labor, the total duration of labor, medical intervention during first stage of labor such as artificial rupture of membranes or the use of oxytocin, visual analog scale (VAS) scores upon complete cervical dilation, delivery method and maternal satisfaction rate were compared between the two groups. Results: Among the 208 primiparas, 112 cases were enrolled in the control group and 96 cases in the experimental group. There were no significant differences in the incidences of postpartum hemorrhage, postpartum urinary retention, fetal distress and neonatal asphyxia between the two groups (all P>0.05). The duration of first and second stages of labor and the total duration of labor in the control group were shorter than those in the experimental group (all P<0.001). The rates of artificial rupture of membranes and intravenous use of oxytocin in the control group were higher than those in the experimental group (both P<0.05). The VAS scores upon complete cervical dilation in the control group were significantly higher than those in the experimental group (P<0.05). The vaginal delivery and maternal satisfaction rates were significantly lower in the control group than in the experimental group (both P<0.05). Conclusion: Painless delivery under the guidance of new concept of labor has no significant influence on the maternal and neonatal outcomes. Instead, it can prolong the labor process, provide more delivery time for pregnant women, reduce the intervention measures during delivery, decrease the delivery pain and finally increase the natural delivery rate and their satisfaction with delivery, which is worth wide promotion in clinical practice.
Keywords: New concept of labor, painless delivery, maternal and neonatal outcomes
Introduction
In the process of natural labor, the failure of childbirth may occur because of excessive mental tension, anxiety or extreme pain, which can even endanger lives of the mother and the fetus [1,2]. Painless delivery uses the epidural continuous injection of low-dose drugs, which greatly reduces the pain in the process of delivery and increases the success rate of natural delivery [3,4].
Labor management is an important part of the painless delivery strategy. In the past, labor was divided into latent period, active period, second stage, and third stage. With the clinical promotion and application, the old classification method increases the probability of maternal medical intervention and decreases the rate of vaginal delivery. However, the cervical dilation trend of modern pregnant women is a slow increase, and the labor progresses slowly. Therefore, it is no longer suitable for the present delivery process [5,6]. To ensure the safety, effectiveness and rationality of the delivery process and reduce maternal medical intervention, the new concept of labor was proposed [7-9]. It redefines the latent period and the active period. Cervical dilation <6 cm is the latent period; cervical dilation >6 cm to complete dilation is the active period. Dilation stopping >4 h is regarded as active period stagnation; when the uterine contraction is not good, dilation stopping >6 h is also considered as stagnation of active period. Moreover, “no progress” refers to cervical dilation <4 cm and no improvement for more than 8 h after treatment; cervical dilation of 4-8 cm and no improvement for more than 6 h after treatment; cervical dilation >8 cm and no improvement for more than 2 h after treatment. The application of the new concept of labor in vaginal delivery has been studied, which confirmed that the vaginal delivery rate was higher under the new labor management and it did not affect the maternal and neonatal outcomes [7]. However, few studies have confirmed its safety and effectiveness in painless delivery. This study not only compared the vaginal delivery rate but also provided effective clinical evidence for the application of new labor management in painless delivery to prove the safety of new labor management.
Materials and methods
General information
Primiparas who underwent painless delivery in our hospital from January 1st, 2020 to December 31th, 2020 were selected for this retrospective clinical study. The primiparas were divided into two groups, a control group and an experimental group. The control group received painless delivery with the application of routine labor management. The experimental group received new labor management on the basis of painless delivery. The inclusion criteria were: primiparas with a full-term, head-presentation singleton; primiparas who were willing to accept painless delivery; primiparas who could tolerate vaginal delivery. The exclusion criteria were: primiparas with abnormal fetal position and fetal condition; primiparas with severely damaged function of important organs; primiparas who had a history of uterine-related surgery; primiparas who were not suitable for epidural puncture; primiparas with pregnancy-related complications; primiparas who had mental illness and could not cooperate with researchers. This study was approved by the Ethics Committee of our hospital (Approval No. 2020KY235).
Labor analgesia methods
When the cervix dilated to 3 cm, primiparas in both groups underwent epidural puncture in the space between L2 and L3, and the drug solution was continuously pumped with a catheter. The drug solution was 0.1% ropivacaine solution (AstraZeneca AB, H20140763, 100 mg) [including 50 ug of sufentanil (Yichang Renfu Pharmaceutical Co., Ltd., China, H20054171, 50 ug)]. The first dose was 10 mL, and the pumping speed was 10 mL/h. The pump was injected until the end of delivery.
Labor management
The control group adopted routine labor management during the painless delivery. In the first stage of labor, the cervical dilation <3 cm was the latent period. The extension of this period to >16 h was called the extension of the latent period. The cervical dilation >3 cm to complete dilation was the active period, and the stagnation of the active period meant the cervical dilation at a certain stage of the active period remained unchanged for 4 h. In the second stage of labor, the delivery time exceeding 2 h was defined as prolonged labor. The speed of the fetal head descending lowering below 1 cm/h was defined as slow descent, and the fetal head not descending for more than 2 h was defined as descending stagnation. The indications of cesarean section were prolonged latent period and active period stagnation [5].
The experimental group adopted new labor management during the painless delivery. The cervical dilation <6 cm was the latent period. The cervical dilation >6 cm to complete dilation was the active period. Dilation stopping >4 h during the active period was considered as active period stagnation. When the uterine contraction was not good, dilation stopping >6 h was defined as active period stagnation. If a primipara had second stage of labor over 4 h during painless labor, it can be seen as prolonged second stage of labor [7].
Outcome measures
Primary outcome measures
This study intended to compare the maternal and neonatal outcomes of the control group and the experimental group, including the cases of postpartum hemorrhage, postpartum urinary retention, fetal distress and neonatal asphyxia.
Secondary outcome measures
Secondary outcome measures included the duration of labor (first stage, second stage and total labor time); the maternal medical intervention during the first stage of labor; the visual analog scale (VAS) scores upon complete cervical dilation; the final delivery method of the mother, including vaginal delivery (natural delivery, forceps assisted delivery) and halfway transfer to cesarean section; maternal satisfaction rate. The VAS scores were evaluated by drawing a 10 cm horizontal line on the paper. One end of the horizontal line was 0, indicating no pain. The other end was 10, indicating severe pain. The middle part indicated different degrees of pain.
The satisfaction rate was evaluated by the self-designed hospital satisfaction scale before the primiparas were discharged from the hospital. The total score was 100 points. The satisfaction was divided into three levels: unsatisfied (<70), generally satisfied (70~89) and very satisfied (90~100). Generally satisfied and very satisfied belonged to the category of satisfaction. Satisfaction rate of treatment = satisfied cases/total cases *100%.
Statistical analysis
Data in this study were analyzed by SPSS 22.0 software. The measurement data were exhibited by mean ± standard deviation (x̅±sd). Comparison between the two groups was performed by the independent-samples t-test. The count data were exhibited by cases/rate (n/%). Comparison of the count data between the two groups was performed by the chi-square test or the Fisher exact probability method. P<0.05 was considered significantly different.
Results
Comparison of general information between the two groups
There were no uncontrollable accidents and withdrawal during the trial period, and the trial was completed successfully, as shown in Figure 1. Moreover, there was no significant difference in the general data between the two groups (all P>0.05). See Table 1.
Figure 1.
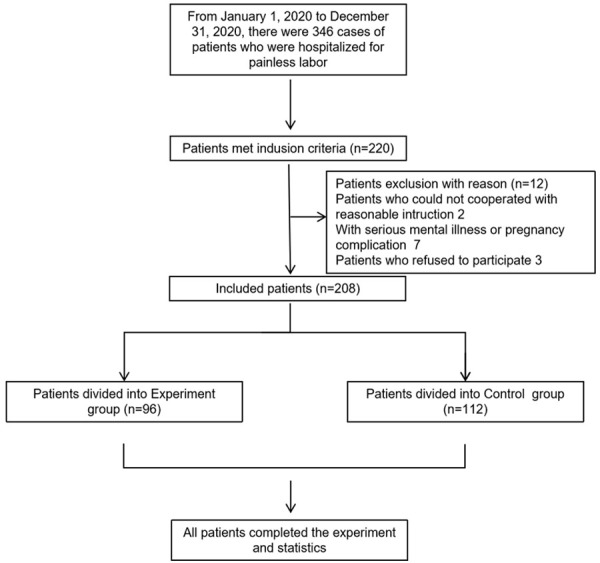
CONSORT flow chart.
Table 1.
Comparison of general information between the two groups
| Control group | Experimental group | t/χ2 | P | |
|---|---|---|---|---|
| n | 112 | 96 | ||
| Age (year) | 25.2±3.3 | 24.9±2.3 | 4.738 | 0.935 |
| BMI (kg/m2) | 29.38±3.62 | 30.11±4.06 | -0.421 | 0.674 |
| Gestational week (week) | 38.84±4.83 | 39.22±4.90 | -2.785 | 0.632 |
Note: BMI: body mass index.
Comparison of maternal and neonatal outcomes between the two groups
There were 3 cases of postpartum hemorrhage, 4 cases of postpartum urinary retention, 4 cases of fetal distress and 2 cases of neonatal asphyxia in the experimental group. No significant difference was identified in maternal and neonatal outcomes between the two groups (all P>0.05). See Table 2.
Table 2.
Comparison of maternal and neonatal outcomes between the two groups
| Control group (n=112) | Experimental group (n=96) | χ2 | P | |
|---|---|---|---|---|
| Postpartum hemorrhage (n, %) | 4 (3.57) | 3 (3.13) | 6.286 | 0.312 |
| Postpartum urinary retention (n, %) | 6 (5.36) | 4 (4.17) | 4.990 | 0.226 |
| Fetal distress (n, %) | 3 (2.68) | 4 (4.17) | 1.073 | 0.300 |
| Neonatal asphyxia (n, %) | 2 (1.79) | 2 (2.08) | 7.580 | 0.202 |
Comparison of labor duration between the two groups
In the experimental group, the first stage of labor was 600.87±113.91 min; the second stage of labor was 97.11±30.06 min; the total time of labor was 702.22±114.90 min. The durations of labor were markedly longer in the experimental group than those in the control group (all P<0.001). See Table 3.
Table 3.
Comparison of labor duration between the two groups (x̅±sd)
| Control group (n=112) | Experimental group (n=96) | t | P | |
|---|---|---|---|---|
| First stage of labor (min) | 484.82±111.23 | 600.87±113.91 | -5.738 | 0.000 |
| Second stage of labor (min) | 66.38±22.62 | 97.11±30.06 | -6.421 | 0.000 |
| Total duration of labor (min) | 556.84±113.83 | 702.22±114.90 | -2.785 | 0.000 |
Comparison of medical intervention during first stage of labor between the two groups
In the experimental group, there were 4 cases of artificial rupture of membranes and 8 cases of intravenous use of oxytocin during the first stage of labor. The cases needed medical interventions in the experimental group were significantly fewer than those in the control group (both P<0.05). See Table 4.
Table 4.
Comparison of medical intervention during first stage of labor between the two groups
| Control group (n=112) | Experimental group (n=96) | χ2 | P | |
|---|---|---|---|---|
| Artificial rupture of membranes (n, %) | 12 (10.71) | 4 (4.17) | 4.627 | 0.032 |
| Intravenous use of oxytocin (n, %) | 21 (18.75) | 8 (8.33) | 7.726 | 0.005 |
Comparison of VAS scores between the two groups
Compared with the control group, the VAS score upon complete cervical dilation in the experimental group was significantly decreased (P<0.05). See Figure 2.
Figure 2.
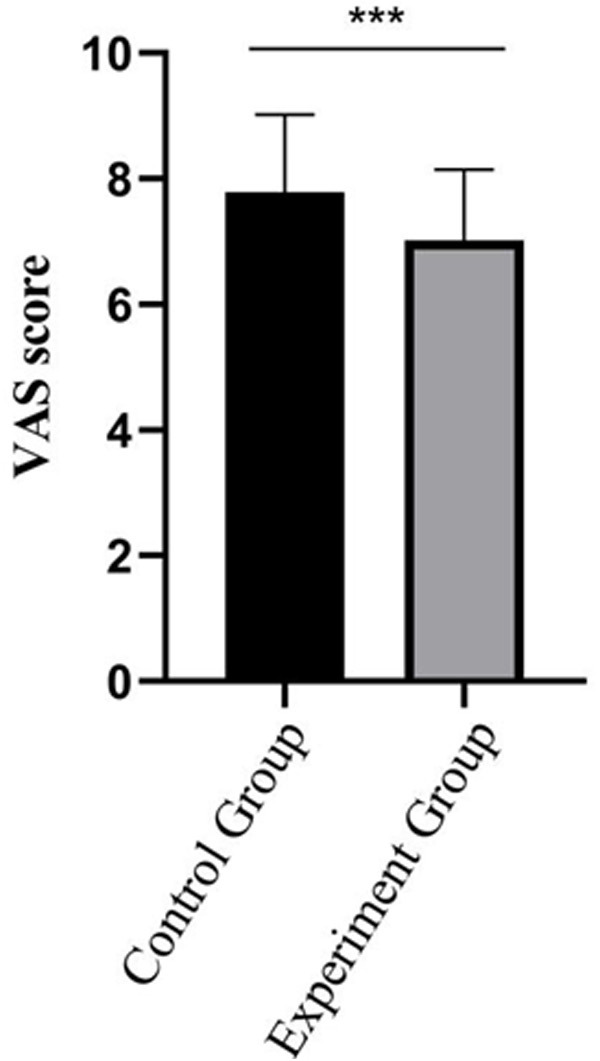
Comparison of VAS score between the control group and experiment group. Compared with the control group, ***P<0.001.
Comparison of vaginal delivery rate between the two groups
The vaginal delivery rate of primiparas in the experimental group was 84.38%, which was significantly higher than 68.75% in the control group (P<0.05). See Table 5.
Table 5.
Comparison of vaginal delivery rate between the two groups
| Control group (n=112) | Experimental group (n=96) | χ2 | P | |
|---|---|---|---|---|
| Natural delivery (n) | 70 | 73 | 6.940 | 0.031 |
| Forceps assisted delivery (n) | 7 | 8 | ||
| Halfway transfer to cesarean section (n) | 35 | 15 | ||
| Vaginal delivery rate (%) | 68.75 | 84.38 | 7.515 | 0.006 |
Comparison of satisfaction rate between the two groups
The maternal satisfaction rate of the experimental group was 86.46%, which was higher than 72.32% in the control group (P<0.05). See Table 6.
Table 6.
Comparison of satisfaction rate between the two groups
| Control group (n=112) | Experimental group (n=96) | χ2 | P | |
|---|---|---|---|---|
| Very satisfied (n) | 52 | 58 | 6.797 | 0.030 |
| Generally satisfied (n) | 29 | 25 | ||
| Unsatisfied (n) | 31 | 13 | ||
| Satisfaction rate (%) | 72.32 | 86.46 | 6.110 | 0.013 |
Discussion
Nowadays, painless delivery not only improves the quality of maternal labor but also provides effective protection for the safety of pregnant women and newborns [10-12]. With the increase of painless delivery rate, the labor management during delivery has been paid more attention. The old concept of labor management lags behind, which may increase the probability of cesarean section and the risk of newborn delivery. The new concept of labor, redefining the time of each stage of labor, may provide a better theoretical guarantee for painless delivery [13,14].
In this study, we found that compared with the old labor management, the new labor management did not increase the incidence of postpartum hemorrhage, urinary retention and fetal distress and neonatal asphyxia, which proved that the new labor management did not affect the safety of painless delivery. Some studies have pointed out that the labor duration under the new labor management is longer than that under the conventional labor management, and the longer labor time may increase the anxiety of pregnant women [15,16]. However, the prolongation of labor makes the pregnant women have more time to adjust their mentality. Also, the improvement of nursing quality further alleviated the anxiety of the pregnant women. So, the adverse maternal and neonatal outcomes caused by the negative emotions of pregnant women can be further reduced [17,18]. Moreover, this study showed that under the new labor management, the duration of labor was prolonged; the probability of using oxytocin or artificial rupture of membranes in the first stage of labor was reduced; the natural delivery rate was significantly increased; the probability of natural delivery transferring to caesarean section was significantly reduced, obviously reducing the anxiety and pain caused by the change of delivery method. In addition, this study found that under the guidance of the new labor strategy, the maternal pain score further decreased, and the quality of painless delivery was increased, which may be related to the reduction of maternal psychological stress [19,20]. This study identified that the satisfaction rate of primiparas who received new labor management was significantly improved, which may be related to the lack of intervention in the first stage of labor and the decrease of VAS scores during delivery [21,22].
However, the sample size of this trial is relatively small, and the investigation time of maternal and infant outcomes and maternal satisfaction rate is relatively short, which may lead to relative errors in the test results. Therefore, a prospective trial with a larger sample size to verify the above test results is needs.
Painless delivery under the guidance of new concept of labor has no influence on the maternal and neonatal outcomes. However, it can prolong labor duration, and provide sufficient delivery time for primiparas. Meanwhile, it can reduce the intervention measures in the process of labor and reduce the pain of delivery. It can also increase the success rate of natural delivery and improve maternal satisfaction, which should be applied more in clinical nursing practice.
Acknowledgements
This work was supported by the Major Clinical Research Project for the Second Round of Shanghai Shenkang Three-year Action Plan to Promote Clinical Skills and Innovation in Municipal Hospitals (SHDC2020CR2060B).
Disclosure of conflict of interest
None.
References
- 1.Klomp T, Witteveen AB, de Jonge A, Hutton EK, Lagro-Janssen AL. A qualitative interview study into experiences of management of labor pain among women in midwife-led care in the Netherlands. J Psychosom Obstet Gynaecol. 2017;38:94–102. doi: 10.1080/0167482X.2016.1244522. [DOI] [PubMed] [Google Scholar]
- 2.Kohn JR, Rao V, Sellner AA, Sharhan D, Espinoza J, Shamshirsaz AA, Whitehead WE, Belfort MA, Sanz Cortes M. Management of labor and delivery after fetoscopic repair of an open neural tube defect. Obstet Gynecol. 2018;131:1062–1068. doi: 10.1097/AOG.0000000000002577. [DOI] [PubMed] [Google Scholar]
- 3.Santana VGD, Santos Neto PMD. Modelos de gestão pública da Secretaria de Saúde de Pernambuco: implicações na gestão do trabalho. Saúde em Debate. 2017;41:122–132. [Google Scholar]
- 4.Micaglio M, Sorbello M, Di Filippo A. The painful search of a painless labour. Trends Anaesth Crit Care. 2018;20:32–33. [Google Scholar]
- 5.Wang Y, Ying H, Zhang W, He R, Lin J. Application of ultrasound-guided epidural catheter indwelling in painless labour. J Pak Med Assoc. 2020;70:45–50. [PubMed] [Google Scholar]
- 6.Wang J, Huang J, Yang S, Cui C, Ye L, Wang SY, Yang GP, Pei Q. Pharmacokinetics and safety of esketamine in Chinese patients undergoing painless gastroscopy in comparison with ketamine: a randomized, open-label clinical study. Drug Des Devel Ther. 2019;13:4135–4144. doi: 10.2147/DDDT.S224553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ali L. Barriers to effective painless labor in developing countries and the remedial measures. Anaesth Pain Intensiv Care. 2020;24:586–587. [Google Scholar]
- 8.Smith CA, Collins CT, Levett KM, Armour M, Dahlen HG, Tan AL, Mesgarpour B. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2:CD009232. doi: 10.1002/14651858.CD009232.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fesenko O, Lysyuk V, Sakharova Z. Risk-oriented approach to labor protection at grain process enterprises. Grain Prod Mixed Fodder. 2019;19:4–10. [Google Scholar]
- 10.Lee K, Kulviwat S, Al-Shuridah O. Key antecedents and outcomes of korean workers’ perceived labor-management relations. J Asia-Pac Bus. 2019;20:1–20. [Google Scholar]
- 11.Pan K. Clinical experience of painless labor under epidural block. J Xiang Yang Vocat Tech College. 2018;17:62–64. [Google Scholar]
- 12.Shokouh N, Ghanbari Z, Saedi N. Successful management of cervical elongation during pregnancy and labor: a case report. Case Rep Clin Pract. 2020;5:98–100. [Google Scholar]
- 13.Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. The expert consensus of new standard and management of labor (2014): interpretation and statement. Zhonghua Fu Chan Ke Za Zhi. 2018;53:143–144. doi: 10.3760/cma.j.issn.0529-567X.2018.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Lee NJ, Neal J, Lowe NK, Kildea SV. Comparing different partograph designs for use in standard labor care: a pilot randomized trial. Matern Child Health J. 2018;22:355–363. doi: 10.1007/s10995-017-2366-0. [DOI] [PubMed] [Google Scholar]
- 15.Distelhorst G, Hainmueller J, Locke RM. Does lean improve labor standards? Management and social performance in the nike supply chain. Manag Sci. 2017;63:707–728. [Google Scholar]
- 16.Ross S, Eisenhardt R. Clear statement rules and the integrity of labor arbitration. Arbitration Law Rev. 2018:10. [Google Scholar]
- 17.Ashcraft K. ‘Submission’ to the rule of excellence: ordinary affect and precarious resistance in the labor of organization and management studies. Organ. 2017;24:36–58. [Google Scholar]
- 18.Niu B, Li M. The effect of epidural anesthesia for labor analgesia on the outcome of labor under the new standard of labor. Trauma Crit Care Med. 2019;7:178–183. [Google Scholar]
- 19.Jia M, Chen M, Peng J. Influence of promoting new production process standard in prognosis of newborns. Mod Hosp. 2018;18:1325–1327. [Google Scholar]
- 20.Aswitami N, Septiani N. Antenatal clinical hypnosis and birth ball exercise as adjunct therapy for management of labor and delivery pain: a summary of its empirical findings. Jurnal Midpro. 2020;12:233. [Google Scholar]
- 21.Schekoldin V, Bogatyreva I, Ilyukhina L. Digitalization of labor regulation management: new forms and content. Digit Age: Chances, Chall Future. 2020:137–143. [Google Scholar]
- 22.Tsurane K, Tanabe S, Miyasaka N, Matsuda M, Takahara M, Ida T, Kohyama A. Management of labor and delivery in myasthenia gravis: a new protocol. J Obstet Gynaecol Res. 2019;45:974–980. doi: 10.1111/jog.13922. [DOI] [PubMed] [Google Scholar]


