Abstract
Objective: The incidence of gastric cancer is declining in parts of Asia including China. This study was designed to investigate the incidence and mortality trend of gastric cancer in different regions and ethnic groups in Xining of Qinghai-Tibet Plateau. Methods: Data of gastric cancer from January 2009 to December 2016 were collected from Disease Control Center in Xining for repeated cross-sectional study. Primary outcome measures: Gastric cancer. Participants: Xining resident population with pathological diagnosis of gastric cancer. Main outcome measure: Age, gender composition ratio, morbidity, mortality and trends. Results: There were 4822 new cases of gastric cancer from 2009 to 2016, including 3583 males and 1239 females; 2290 cases were in villages and 2532 in towns. Male incidence rate (38.37/100,000) was higher than female (13.35/100,000). The incidence in rural areas (39.29/100,000) was higher than in urban areas (20.59/100,000). During 2009-2016, there were 2109 gastric cancer deaths in Xining, 1543 in males and 566 in females. There were 1185 cases in villages and 924 in cities. Male mortality (16.64/100,000) was higher than female (6.42/100,000). The mortality rate in rural areas (20.40/100,000) was higher than in urban areas (7.62/100,000). Conclusion: Overall morbidity and mortality rates of gastric cancer are on the rise in Xining. Male morbidity and mortality rates are higher than female ones, and rural areas are higher than urban areas.
Keywords: Gastric-cancer, morbidity, mortality, trend, Xining
Introduction
The burden of cancer is a universal public health challenge that afflicts every country in the world, with cases distributed across all age groups and genders. With the rapid economic development, urbanization, acceleration of population aging, and changes in traditional lifestyle in China, malignant tumors have become the fifth leading cause of death along with cerebrovascular diseases, respiratory diseases and heart disease.
Gastric cancer is a common gastrointestinal tumor that occurs worldwide. Its incidence in China is 36.21/100,000 and the standard-population rate is 17.85/100,000, while the mortality rate is 25.88/100,000 [1]. According to tumor registration data in China, incidence rates of gastric cancer differ between the eastern and western areas [2]. Of the 31 urban tumor registration regions in China in 2009, Xining had the seventh-highest incidence rate of gastric cancer, being a high-incidence area with a serious disease burden [1]. Although the monitoring, intervention and publicity of the disease have been strengthened in high-risk groups of gastric cancer, there is no systematic data analysis of the local incidence of and trends in gastric cancer in western China due to the late start of tumor registration. Based on data from the 2009-2016 tumor registration, this study analyzed the prevalence, status, and changes in gastric-cancer trends in Xining. Based on the actual situation of the gastric cancer population, it is anticipated to formulate corresponding prevention and control strategies and to pay special attention to high-risk group.
Materials and methods
Patient and public involvement
Patients or the public were not involved in the design of the study.
Data collection
Taking the permanent residents of Xining as the research object, we collected incidence and mortality data on malignant tumors from the Tumor Registration Office of the Xining Center for Disease Control and Prevention and four hospitals in Xining, which are qualified to diagnose such tumors (Qinghai University Hospital, the Red Cross Hospital, Qinghai Provincial People’s Hospital and the Fifth People’s Hospital). This data of gastric-cancer were based the 10th edition of the International Classification of Diseases (ICD-10). The Xining Municipal Public Security Bureau provided population data for Xining, as well as population numbers (by gender and age group) in the registered area for the years studied. The study was approved by Qinghai University Hospital Ethics Committee. We referred to (1) the Chinese Cancer Registry; (2) the tumor registration work instruction manual of the People’s Republic of China; (3) The quality of the registration requirements of the Cancer Incidence in Five Continents series. We reviewed and sorted the pathogenesis information of patients with gastric cancer in Xining from 2009 to 2016, including name, gender, date of birth, residential area, nature of tumor, pathological stage, diagnosis date, basis of diagnosis, surgical treatment and other original data. Finally, we obtained data for incidence, mortality and standard population of gastric cancer (gender, age, urban vs. rural) in this region. The reliability of the overall research data is relatively high.
Statistical analysis
All statistical analysis was performed using SPSS software, version 23.0 for Windows (SPSS, Chicago, Illinois, USA). Morbidity and mortality were calculated based on the permanent population of Xining. The specific morbidity and mortality of gastric cancer according to different regions and genders were calculated. the morbidity and mortality for different age cohorts in different years was compared using the chi-square test. P<0.05 was considered statistically significant.
Ethical approval
This study was approved by the ethical review committee of the Affiliated Hospital of Qinghai University (Qinghai, China). (AF-RHEC-007-01, AF-RHEC-0034-01).
Results
Gastric-cancer incidence rate and trends
From 2009 to 2016, a total of 4822 new cases of gastric cancer were registered in Xining, including 3583 males and 1239 females. In 2009, the incidence of gastric cancer in Xining was 6/100,000, while in 2016, it was 36.63/100,000, showing an obvious upward trend from previous years. In 2009, the incidence of gastric cancer was 8.5/100,000 in men and 3.7/100,000 in women; by 2016, the incidence in men was 52.48/100,000 and in women 19.85/100,000. The incidence of gastric cancer is on the rise for both men and women, but the trend was higher for men than for women (Table 1; Figure 1).
Table 1.
New cases of and deaths from gastric cancer in men vs. women from 2009 to 2016
| Year | Total population (n) | New cases (n) | Deaths (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Total | Men | Women | Total | Men | Women | Total | Men | Women | |
| 2009 | 220.50 | 111.09 | 109.41 | 130 | 93 | 37 | 45 | 32 | 13 |
| 2010 | 220.87 | 113.68 | 107.19 | 404 | 307 | 97 | 163 | 118 | 45 |
| 2011 | 222.80 | 114.50 | 108.30 | 559 | 423 | 136 | 253 | 194 | 59 |
| 2012 | 224.74 | 115.30 | 109.44 | 804 | 582 | 222 | 412 | 294 | 118 |
| 2013 | 226.76 | 116.50 | 110.26 | 659 | 482 | 177 | 316 | 237 | 79 |
| 2014 | 229.07 | 117.88 | 111.19 | 639 | 485 | 154 | 290 | 221 | 69 |
| 2015 | 231.00 | 118.80 | 112.20 | 772 | 581 | 191 | 331 | 214 | 90 |
| 2016 | 233.37 | 120.03 | 113.34 | 855 | 630 | 225 | 299 | 206 | 93 |
| Total | 1809.11 | 927.78 | 881.33 | 4822 | 3583 | 1239 | 2109 | 1543 | 566 |
Figure 1.
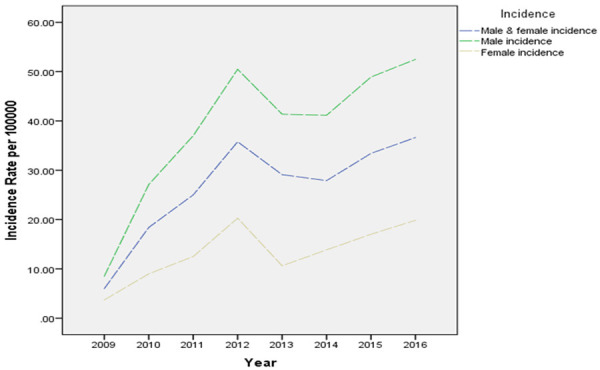
Trends of gastric cancer in Xining.
Number of cases and trends by age group
In 2016, the number of gastric-cancer patients of different ages in Xining varied by age range. Gastric cancer occurs at a lower rate in patients <40 years old, but the incidence rate increases rapidly in those 40-64 years old, slows down in the age cohort of 65-74 years and gradually decreases with age after 75 years. From 2009 to 2015, the incidence trend of gastric cancer in Xining by age cohort differed slightly from that in 2016, peaking at 74 years of age (P=0.140). The difference was not statistically significant. Incidence was generally higher in men than in women and in villages than in towns within the same age groups (Table 2; Figures 2, 3).
Table 2.
New cases of gastric cancer in different age groups from 2009 to 2016
| 2009 (n) | 2010 (n) | 2011 (n) | 2012 (n) | 2013 (n) | 2014 (n) | 2015 (n) | 2016 (n) | χ2 | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| New cases | 131.30 | 0.140 | ||||||||
| 0-4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 5-9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 10-14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 15-19 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | ||
| 20-24 | 0 | 8 | 2 | 6 | 3 | 1 | 1 | 3 | ||
| 25-29 | 0 | 2 | 2 | 3 | 5 | 2 | 3 | 5 | ||
| 30-34 | 5 | 1 | 8 | 6 | 5 | 5 | 8 | 5 | ||
| 35-39 | 2 | 10 | 15 | 14 | 13 | 18 | 15 | 14 | ||
| 40-44 | 8 | 18 | 25 | 31 | 35 | 36 | 39 | 39 | ||
| 45-49 | 16 | 29 | 42 | 57 | 45 | 50 | 76 | 67 | ||
| 50-54 | 8 | 39 | 53 | 65 | 43 | 51 | 69 | 92 | ||
| 55-59 | 21 | 48 | 84 | 98 | 95 | 79 | 82 | 109 | ||
| 60-64 | 19 | 66 | 79 | 123 | 109 | 95 | 117 | 144 | ||
| 65-69 | 18 | 50 | 88 | 136 | 116 | 88 | 119 | 132 | ||
| 70-74 | 18 | 68 | 85 | 122 | 101 | 109 | 121 | 95 | ||
| 75-79 | 12 | 39 | 49 | 78 | 55 | 60 | 72 | 87 | ||
| 80-84 | 3 | 21 | 21 | 49 | 27 | 27 | 38 | 50 | ||
| 85+ | 0 | 5 | 4 | 15 | 7 | 17 | 12 | 13 | ||
| Total | 130 | 404 | 559 | 804 | 659 | 639 | 772 | 855 |
Figure 2.
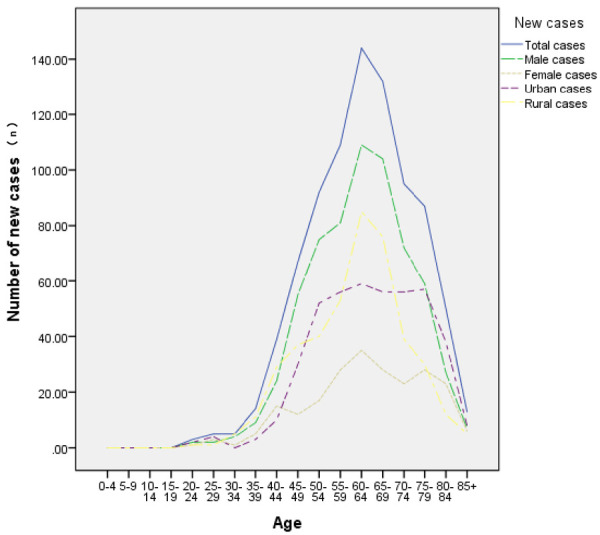
New cases of gastric cancer in different age groups.
Figure 3.
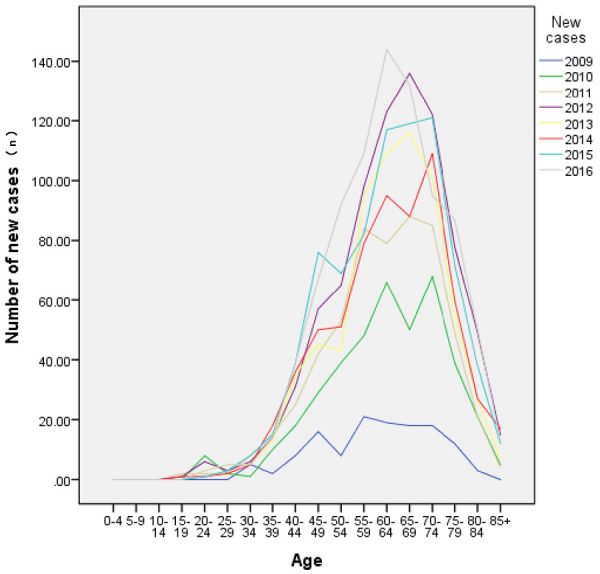
Trends of new cases of gastric cancer in different age groups.
Urban and rural morbidity and changes in trends
According to the data, we found that in Xining, gastric-cancer incidence differed significantly between urban and rural areas. With the present state of sustained growth, rural incidence of gastric cancer since 2011 has been significantly higher than urban incidence, as high as 60.60/100,000 in 2016. The incidence of gastric cancer in Xining is rising steadily; the incidence rate is higher in rural areas than in urban areas, in which morbidity exceeded 26.37/100,000 by the end of 2016 (Table 3; Figure 4).
Table 3.
New cases of and deaths from gastric cancer in different areas from 2009 to 2016
| Year | Total population | New cases | Deaths | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Total (n) | Urban (n) | Rural (n) | Total (n) | Urban (n) | Rural (n) | Total (n) | Urban (n) | Rural (n) | |
| 2009 | 220.50 | 135.28 | 85.22 | 130 | 83 | 47 | 45 | 35 | 10 |
| 2010 | 220.87 | 140.69 | 80.18 | 404 | 284 | 120 | 163 | 135 | 28 |
| 2011 | 222.80 | 145.80 | 77.00 | 559 | 348 | 211 | 253 | 146 | 107 |
| 2012 | 224.74 | 152.20 | 72.54 | 804 | 411 | 393 | 412 | 167 | 245 |
| 2013 | 226.76 | 153.74 | 73.02 | 659 | 292 | 367 | 316 | 108 | 208 |
| 2014 | 229.07 | 157.15 | 71.92 | 639 | 324 | 315 | 290 | 93 | 197 |
| 2015 | 231.00 | 159.50 | 71.50 | 772 | 359 | 413 | 331 | 111 | 220 |
| 2016 | 233.37 | 163.41 | 69.96 | 855 | 431 | 424 | 299 | 129 | 170 |
| Total | 1809.11 | 1207.77 | 601.34 | 4822 | 2532 | 2290 | 2109 | 924 | 1185 |
Figure 4.
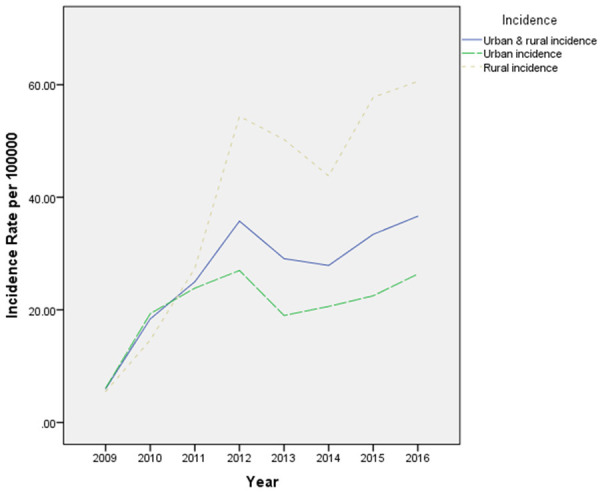
New cases and trends of gastric cancer in different areas.
Mortality rate of gastric cancer and its trends
From 2009 to 2016, there were 2109 deaths from gastric cancer in Xining, of which 1543 cases were male and 566 were female. Thus, the data showed that the death rate of gastric cancer was higher in men than in women. Mortality was 2.04/100,000 in 2009 and 12.81/100,000 in 2016, showing an overall upward trend. However, if we take 2012 as a cut-off point, the mortality rate of gastric cancer had previously showed a trend of rapid growth but began a slow decline starting from 2012 (Figure 5).
Figure 5.
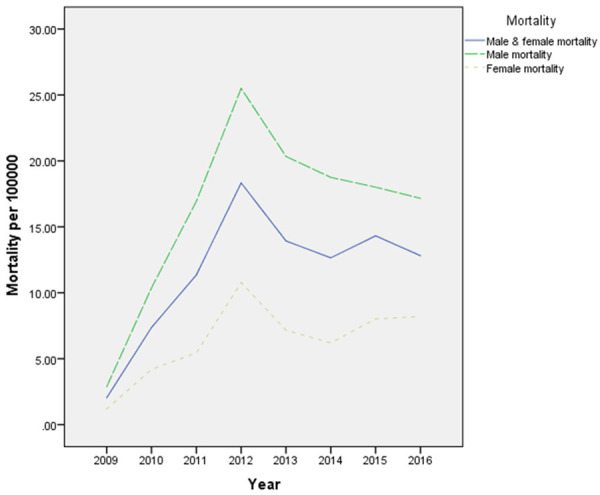
Mortality and trends in gastric cancer in different gender.
Age-specific mortality rate of gastric cancer and its trends
In 2016, there were significant differences in gastric-cancer mortality among different age groups in Xining. This study found that patients >40 years old had the lowest mortality rate from gastric cancer, that of patients in 40-64 years old was the highest, that of patients in 65-74 years old was lower, and that of patients >75 years old was significantly decreased. From 2009 to 2016, the difference was not statistically significant (P=0.346). The overall trend of gastric-cancer mortality was higher in men than in women and higher in rural areas than in towns within different age groups (Table 4; Figure 6).
Table 4.
Deaths from gastric cancer in different age groups from 2009 to 2016
| 2009 (n) | 2010 (n) | 2011 (n) | 2012 (n) | 2013 (n) | 2014 (n) | 2015 (n) | 2016 (n) | χ2 | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Deaths | 102.949 | 0.346 | ||||||||
| 0-4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 5-9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 10-14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 15-19 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 20-24 | 0 | 2 | 1 | 3 | 2 | 0 | 0 | 0 | ||
| 25-29 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | ||
| 30-34 | 2 | 1 | 1 | 1 | 1 | 0 | 1 | 3 | ||
| 35-39 | 0 | 5 | 8 | 8 | 5 | 4 | 5 | 6 | ||
| 40-44 | 2 | 2 | 11 | 12 | 12 | 14 | 10 | 11 | ||
| 45-49 | 5 | 10 | 14 | 23 | 17 | 18 | 19 | 19 | ||
| 50-54 | 4 | 9 | 18 | 31 | 16 | 17 | 22 | 20 | ||
| 55-59 | 6 | 20 | 36 | 42 | 39 | 37 | 43 | 27 | ||
| 60-64 | 7 | 20 | 27 | 52 | 55 | 42 | 45 | 49 | ||
| 65-69 | 6 | 23 | 47 | 61 | 60 | 42 | 48 | 43 | ||
| 70-74 | 6 | 32 | 37 | 77 | 56 | 56 | 61 | 39 | ||
| 75-79 | 5 | 22 | 34 | 49 | 32 | 30 | 47 | 41 | ||
| 80-84 | 2 | 12 | 18 | 41 | 19 | 19 | 20 | 32 | ||
| 85+ | 0 | 4 | 2 | 12 | 2 | 10 | 10 | 8 | ||
| Total | 45 | 163 | 254 | 412 | 316 | 290 | 331 | 299 |
Figure 6.
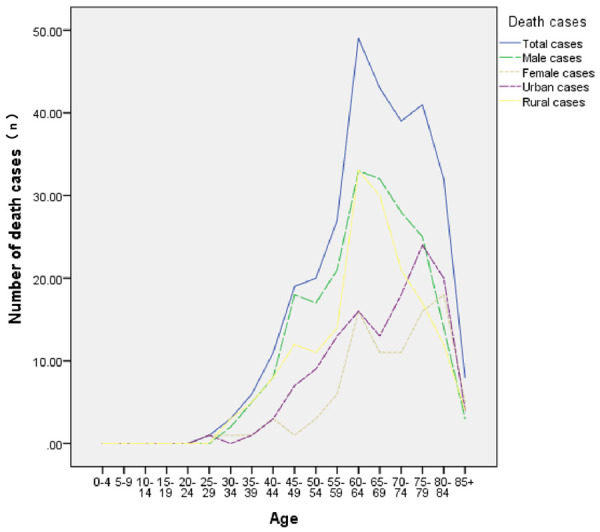
Deaths from gastric cancer in different age groups.
Mortality rate in urban and rural areas and its trends
There were 2109 deaths from gastric cancer in Xining, including 924 cases in cities and 1185 cases in villages, from 2009 to 2016. In 2009, the urban mortality rate was 0.16/100,000, which was significantly higher than the rural mortality rate of 0.05/100,000. In 2016, the urban mortality rate was 7.89/100,000, while the rural mortality rate was significantly higher, 24.30/100,000. Both urban and rural mortality rates showed an increasing trend from 2009 to 2016 (Figure 7).
Figure 7.
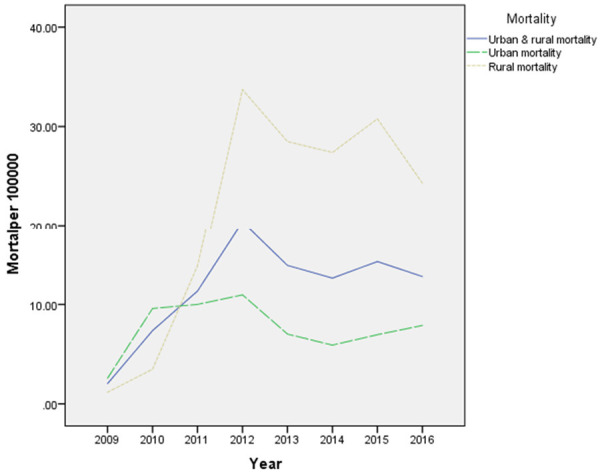
Mortality and trends of gastric cancer in different areas.
Discussion
In recent years, with the improvement of global socio-economic status, environmental factors, and health conditions, the morbidity and mortality rates of gastric cancer in most regions of China and in many other countries with high incidences have been decreasing [3]. The main reasons may be as follows: (1) the decrease rate of the Helicobacter pylori infection [4,5]. (2) changes in people’s dietary habits, such as less salt and animal fat intake and more fresh-vegetable and -fruit intake. However, in this study, we found that the incidence of gastric cancer in Xining showed a trend of increasing from 2009 to 2016.
This high incidence rate in Xining may partially due to the following facts: (1) With the improvement of tumor diagnostic technology, the detection rate for gastric cancer has increased significantly. (2) Medical insurance coverage has expanded, and the quality of tumor registration data has been continuously improving. (3) Xining, where multiple ethnic groups reside, has unique dietary habits. For example, the Hui ethnicity tend to eat a great deal of fried food. High-temperature cooking such as frying is likely to produce the carcinogen acrylamide; exposure to this chemical leads to an increase of DNA synthesis and acceleration of cell growth, and the higher the temperature, the greater the amount of acrylamide. Tibetans like to eat raw, hard foods, such as red meat. Their animal-fat intake is high, while their fresh-fruit and -vegetable intake is low. Studies have proven that fresh vegetables are protective factors against gastric cancer. All of the above habits cause damage to the gastric mucosa. Eating fresh vegetables, however, protects against the occurrence of gastric cancer [6]. (4) Xining is located on the Qinghai-Tibet Plateau, which has a cold climate and low oxygen. One study shows that a plateau hypoxia environment tends to cause ischemic hypoxia in body mucosa, increased cell apoptosis, physiological-function changes to the gastric cavity, damage to the gastric mucosal barrier and decreased ability to repair it [7].
We have shown that the incidence of gastric cancer in Xining was significantly higher in rural areas than in urban areas, which was consistent with the results of previous study [1]. This is because: (1) The living standard of the rural population has improved, meaning that the disease is valued and can be detected early. (2) Rural residents’ drinking water is mostly cellar water. Studies have found that cellar water contains nitrite, which is a risk factor for gastric cancer if drinking over long period [8]. (3) Rural areas usually lag behind in transportation infrastructures and economies, so residents in rural area may eat less fresh fruits and vegetables and may rely more on pickled foods. High sodium levels and osmotic pressure can damage gastric mucosa and increase the risk of gastric cancer, and in the mean time, high sodium plus H. pylori infection synergistically increase the occurrence of gastric cancer [9,10]. We also found that the incidence of gastric cancer in Xining was significantly higher in men than in women in recent years, which was similar to the results of the national study [1,11]. The reasons could be that: (1) Smoking is positively correlated with the incidence of gastric cancer. Men smoke at a much higher rate than women, which is one of the important risk factors leading to the difference between male and female morbidity [12]. (2) Alcohol intake increases the risk of primary gastric cancer [13,14]. (3) Estrogen has a protective effect against gastric cancer, and estradiol can prevent the development of stromal stem cells into gastric cancer [15]. (4) Men work in jobs that are riskier and more labor-intensive, meaning they have greater mental stress and more-irregular lifestyles than women [16]. (5) The higher incidence of gastric cancer in men than in women is also related to heredity. Dnmt-3a and rs36012910, genes or polymorphism that are unique to men, which increase the risk of gastric cancer [17,18]. While the incidence of gastric cancer is decreasing globally, there has been no change in the proportion of men to women with this disease, which also suggests that the gender difference may be a blind spot in its prevention and control and in the screening of high-risk groups.
From 2009 to 2016, the death rate for gastric cancer in Xining showed an overall upward trend. Before 2012, it was trending rapidly upward, but this trend reversed after 2012, which was consistent with a decline in gastric-cancer deaths in much of the world [19-21].
To sum up, in most of the world today, gastric cancer shows a trend of decline, but its incidence and mortality in Xining continue to increase and in a younger trend. Exploring the Xining region’s gastric-cancer epidemiology in view of its high-risk population, popularizing health education and screening and improving the early detection of cancer are especially important.
Strengths and limitations of this study
This is the first observational study on the trend of incidence and mortality of gastric cancer in Xining.
We collected gastric cancer data from 2009 to 2016 from Disease Control Center in Xining, and repeated cross-sectional study observations were done. Gastric cancer is on the decline in some parts of Asia including China, but the increased incidence in this study may be related to the special geographical location and living habits of The Qinghai-Tibet Plateau. Gender and age are other two factors that may affect the incidence of gastric cancer in Xining’s urban and rural area, which should take into consideration so as to develop effective and feasible prevention and control strategies.
Acknowledgements
We acknowledge Qinghai and Xining Center for Disease Control for their data. This work was supported by the Ministry of Education “Chunhui Program”, and Science and Technology Department of Qinghai Province (2018-HZ-814 and 2018-ZJ-702).
Disclosure of conflict of interest
None.
References
- 1.Zheng ZX, Zheng RS, Chen WQ. Analysis of gastric cancer incidence and death in China in 2009. Chin Oncol. 2013;22:327–332. [Google Scholar]
- 2.Gong YX, Tang YP, Guo L, Chen TM, Kang LL, Niu W, Wang ZF, Chen Y, Zhang T. Influence of regional differences on characteristics of gastric cancer. World Chin Dig. 2016;24:1092–1097. [Google Scholar]
- 3.Katanoda K, Matsuda T, Matsuda A, Shibata A, Nishino Y, Fujita M, Soda M, Ioka A, Sobue T, Nishimoto H. An updated report of the trends in cancer incidence and mortality in Japan. Jpn J Clin Oncol. 2013;43:492–507. doi: 10.1093/jjco/hyt038. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe M, Ito H, Hosono S, Oze I, Ashida C, Tajima K, Katoh H, Matsuo K, Tanaka H. Declining trends in prevalence of helicobacter pylori infection by birth-year in a Japanese population. Cancer Sci. 2015;106:1738–1743. doi: 10.1111/cas.12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Martel C, Ferlay J, Franceschi S, Vignat J, Bray F, Forman D, Plummer M. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13:607–615. doi: 10.1016/S1470-2045(12)70137-7. [DOI] [PubMed] [Google Scholar]
- 6.Wang Q, Hao J, Guan Q, Yuan W. The mediterranean diet and gastrointestinal cancers risk. Recent Pat Food Nutr Agric. 2014;6:23–26. doi: 10.2174/2212798406666141024111945. [DOI] [PubMed] [Google Scholar]
- 7.Xiong YZ. Clinical study on gastric mucosal lesion of chronic plateau disease. Chin Dig endoscopy. 2008;2:20–22. [Google Scholar]
- 8.Zhou Y, Xiao JR, Ying MG, Chen ZC, Chen BY, Chen HY. Investigation on the quantity of chemical elements, nitrate and nitrite in the drinking water in the high and low gastric cancer incidence area. Chin J Dis Control Prev. 2009;13:619–620. [Google Scholar]
- 9.Fang X, Wei J, He X, An P, Wang H, Jiang L, Shao D, Liang H, Li Y, Wang F, Min J. Landscape of dietary factors associated with risk of gastric cancer: a systematic review and dose-response meta-analysis of prospective cohort studies. Eur J Cancer. 2015;51:2820–2832. doi: 10.1016/j.ejca.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Raei N, Behrouz B, Zahri S, Latifi-Navid S. Helicobacter pylori infection and dietary factors act synergistically to promote gastric cancer. Asian Pac J Cancer Prev. 2016;17:917–921. doi: 10.7314/apjcp.2016.17.3.917. [DOI] [PubMed] [Google Scholar]
- 11.Wang WW, Liu WB, Cao GW. Risk factors related to gender differences in the incidence of gastric cancer. Shanghai Prev Med. 2017;29:257–260. [Google Scholar]
- 12.Marqués-Lespier JM, González-Pons M, Cruz-Correa M. Current perspectives on gastric cancer. Clin Gastroenterol North Am. 2016;45:413–428. doi: 10.1016/j.gtc.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou WB, Wu H, Cai QC, Li ZS. Research progress on risk factors of gastric cancer. Chin J Pract Med. 2014:415–420. [Google Scholar]
- 14.Ma K, Baloch Z, He TT, Xia X. Alcohol consumption and gastric cancer risk: a meta-analysis. Med Sci Monit. 2017;23:238–246. doi: 10.12659/MSM.899423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gan L, He J, Zhang X, Zhang YJ, Yu GZ, Chen Y, Pan J, Wang JJ, Wang X. Expression profile and prognostic role of sex hormone receptors in gastric cancer. BMC Cancer. 2012;12:566. doi: 10.1186/1471-2407-12-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li J. Work stress and cancer risk: a meta-analysis of 5,700 accidental cancer events in 116,000 European men and women. Br Med J. 2013;6:369–370. [Google Scholar]
- 17.Ibbs M, Miller M, Hadjipanayis A, Bass AJ, Pedamallu AC. Comprehensive molecular characterization of gastric adenocarcinoma. Nat. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu Q, Lu S, Wang L, Hu J, Qiao F, Qiu X, Zhao C, Lao Y, Song Y, Fan H. DNMT3A rs36012910 A>G polymorphism and gastric cancer susceptibility in a Chinese population. Mol Biol Rep. 2012;39:10949–10955. doi: 10.1007/s11033-012-1996-y. [DOI] [PubMed] [Google Scholar]
- 19.Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, Valkov M, Johnson CJ, Estève J, Ogunbiyi OJ, Azevedo ESG, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37513025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 21.GBD 2017 Causes of Death Collaborators. Global, Regional, and National Age-Sex-Specific Mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


