Abstract
Objective: To evaluate the effect of crisis intervention nursing on perioperative psychological state and self-efficacy of patients with laparoscopic radical hysterectomy. Method: A total of 151 cervical cancer patients that underwent laparoscopic radical surgery during January 2018 to March 2020 in our hospital were selected as the research objects. The patients were divided into control group (n=73) and observation group (n=78) according to treatment regimen. The control group received conventional nursing measures, and the observation group was treated with crisis intervention nursing in addition to the traditional measures. The changes of psychological state, self-efficacy, psychological crisis, hope degree before and after intervention, and the satisfaction of the two groups with nursing care were compared. Results: The scores of HAMA, HAMD, self-efficacy, psychological crisis and hope degree in the two groups were remarkably improved after intervention compared with before intervention (all P<0.05), and the improvement of each index in observation group was obviously superior to that in control group (P<0.05). After intervention, the satisfaction to nursing care in observation group was dramatically higher than that in control group (P<0.05). Conclusion: The application of crisis intervention nursing on patients with laparoscopic radical hysterectomy is conductive to alleviating the adverse emotions such as anxiety and depression, reducing their sense of psychological crisis, improving the self-efficacy and hope degree of curing disease, as well as the satisfaction rate with the nursing care, which is worthy of clinical application.
Keywords: Crisis intervention nursing, laparoscopy, radical resection of cervical cancer, psychological state, self-efficacy
Introduction
Cervical cancer is a common malignant tumor in gynecology. China is one of the countries with high incidence of cervical cancer in the world, and patients’ physical and mental health and life are seriously threatened [1]. Epidemiological data in recent years have shown that the incidence of cervical cancer in China has been increasing year by year, and the age of onset tends to be younger. At present, the surgeries and radiotherapies are the primary ways that effectively treat cervical cancer [2]. With the continuous improvement of screening technology, an increasingly number of patients is being detected at an early stage. Laparoscopic surgery, at the same time, is one of the growing trends for the surgical treatment of cervical cancer. Compared with traditional ones, it has the advantages of less surgical trauma and pain, as well as shorter hospital stay [3]. Studies have indicated that most patients undergoing cervical cancer surgery suffer severe psychological stress such as anxiety, depression, and fear. And the surgical trauma, postoperative reproductive organ changes, and possible complications would aggravate such stress responses and induce psychological crisis, thus seriously affecting their living quality [4]. The crisis intervention nursing refers to the use of emergency responses to resolve imminent psychological crisis of patients, helping them restore the psychological stability, and mastering effective coping skills to prevent the recurrence of psychological crises [5]. At present, domestic and foreign scholars have applied the crisis intervention nursing to patients with different malignant tumors, including colon cancer, lung cancer, stomach cancer, breast cancer, etc. This intervention is conductive to improving the psychological state of patients, reducing their fear of disease, improving the quality of life of patients, and enhancing their confidence in overcoming the disease [6]. This study investigated the impact of crisis intervention nursing on perioperative psychological state and self-efficacy of patients with laparoscopic radical hysterectomy.
Materials and methods
Research subjects
A total of 151 cervical cancer patients that underwent laparoscopic radical surgery during January 2018 to March 2020 were selected as the research objects, and their clinical data were retrospectively analyzed. They were divided into control group (n=73) and observation group (n=78) according to the therapeutic regimen. The study was conducted under approval of hospital ethics committee (No. 2017080101).
The inclusive criteria
(1) Patients who met the diagnostic criteria for cervical cancer and diagnosed by pathology before surgery. The diagnostic criteria of cervical cancer referred to the relevant standards in the “Guidelines for the Standardized Diagnosis and Treatment of Cervical Cancer and Precancerous Lesions (Trial)” [7]; (2) Patients that suitable to the laparoscopic radical hysterectomy; (3) Patients with normal cognitive functions and full behavioral ability; (4) The patients had no contraindications to laparoscopic surgery; (5) The clinical stage of the patients was Ia-IIa (according to the FIGO standard of the International Association of Gynecology and Obstetrics); (6) Patients that voluntarily to sign the informed consent forms.
The exclusive criteria
(1) Patients with dysfunctions in vital organs such as kidney, heart, liver or lung; (2) Those accompanied by other primary malignant tumors; (3) Patients who received radiotherapy or chemotherapy before surgery; or (4) Patients with paracervical invasion or lymph node metastasis by imaging examination.
Methods
The control group was given conventional nursing intervention, including health training, basic nursing care, psychological nursing care, functional exercise and prevention of complications.
Patients in observation group were treated with crisis intervention nursing in addition to the conventional therapy, and the. Specifics are as follows: (1) Establishment of a crisis intervention team: the team members included surgeons, responsible nurses, and psychological counselors, etc. They were organized to learn the knowledge of laparoscopic radical resection of cervical cancer, the crisis intervention theory, study the scales, and develop corresponding crisis intervention countermeasures in line with the study object. (2) Admission assessment: after admission, the responsible nurse communicated with the patient one-on-one to assess his crisis state, and analyzed the impact of the psychological crisis degree from the perspective of the patient’s age, clinical stage, education degree, and family economic status. The most concerned problems of the patient were clarified from the perspective of patient, so that the personalized crisis intervention plan for the patient could be developed. The assessment could be conducted by multiple times according to the patient’s condition. (3) Crisis intervention countermeasures: In this study, we primarily conducted the intervention from four aspects below: cognition, psychology, behavior and society. ① Cognition: the medical staff explained to patients on knowledge of disease-related information of cervical cancer, laparoscopic radical surgery, perioperative complications, postoperative functional exercise, etc., and introduced the team members and their previous experience to the patients to correct their negative cognition, and help them treat the disease correctly and relieve fear and tension. ② Psychology: the intervention team used positive psychological suggestion and guidance to encourage patients to express their demands and mental pain. The team showed respect and understanding to the patients, and helped analyzing the causes of psychological crisis from the perspective of patients; guided patients to accept the current state, and applied psychological supports such as empathy and companionship to help patients alleviate their negative emotions; corrected the patient’s negative self-denial state, strengthened the positive coping approaches, and enhanced their confidence to cooperate with surgery and postoperative rehabilitation. ③ Behaviors: The intervention team informed the patients of possible perioperative complications, and instructed them of deep breathing training, gastrointestinal function training, pelvic floor muscle and abdominal muscle training, urination training, diet guidance, etc., in order to improve their disease managing ability. ④ Social support: The intervention team communicated with the family members and relatives of patients, provided psychological counseling for the direct caregivers, and gave more emotional supports to the patients, so as to improve their self-efficacy. (4) Intervention measures: the intervention measures contained one-to-one communication by nursing staff, video materials, lectures, set up of WeChat public account, and information of health education and communication via WeChat, etc. The follow-up and intervention after operation lasted for 6 months.
Index observation
① Evaluation of mental state [8]: The Hamilton Anxiety Scale (HAMA) and Hamilton Depression Scale (HAMD) were applied to evaluate the psychological status of the two groups before and after intervention. The Hamilton Scale >18 points is positive for anxiety. The higher score indicates the severer anxiety and depression in patient. ② Self-efficacy [9]: The cancer self-efficacy scale (SUPPH) was used to score patients’ self-efficacy before and after intervention. The scale covered self-decision-making (3 items), positive attitudes (15 items), and self-decompression (10 items), and each item was scored on a scale of 1 to 5. The higher score represents better self-efficacy of patients. ③ Psychological crisis [10]: The psychological crisis degree of the two groups before and after intervention was evaluated by the psychological crisis level assessment scale. The scale consists of 6 items in 3 dimensions, including emotion, cognition and behavior, and each item has a scale of 1 to 10 points. The higher score reflects stronger psychological crisis of patients. ④ Hope degree [11]: The Herth Hope Index was used before and after intervention to evaluate the hope degree of the two groups. There are three dimensions in the index, including attitudes towards reality and the future, positive actions and intimate relationships with others, with a total score of 12 to 48. A score of 12-23 points indicates low hope degree, 24-35 points indicates medium degree and 36-48 points indicates high degree of hope. ⑤ The satisfaction questionnaire designed by the hospital was used for investigation and analysis after completion of intervention. The scale has been tested with a Cronbach’s α=0.792. The questionnaire contains a total of 20 items and measured by 1-5 scoring method. The total score is 100 points. 90-100 points indicate very satisfied, 80-89 points indicate satisfied, and <80 points indicates dissatisfied. The satisfaction rate = (very satisfied + satisfied)/total number of cases ×100%.
Statistical analysis
SPSS 25.0 was applied for data processing and analysis. The measurement data were represented by (x̅±s), and the enumeration data were represented by percentage. The comparison of measurement data and enumeration data were conducted respectively with t-test and χ2 test, and Paired T test was used for intra-group comparison. The statistical significance was positive with P<0.05. The graphic software was Graphpad prism9.
Results
Clinical data
The difference of clinical data between two groups of patients was insignificant (P>0.05), as shown in Table 1.
Table 1.
Comparison of clinical data between the two groups
| Clinical data | Observation group (n=78) | Control group (n=73) | t/χ2 | P |
|---|---|---|---|---|
| Age (years old, x̅±s) | 42.37±10.39 | 41.98±11.01 | 0.228 | 0.820 |
| Pathological Type | ||||
| Squamous carcinoma | 68 | 61 | 0.397 | 0.529 |
| Adenocarcinoma | 10 | 12 | ||
| FIGO Staging | ||||
| Stage Ia | 17 | 21 | 0.335 | 0.737 |
| Stage Ib | 39 | 32 | ||
| Stage IIa | 22 | 29 | ||
| Educational degree | ||||
| Senior high school or below | 41 | 43 | 0.614 | 0.433 |
| College or above | 37 | 30 |
Perioperative indicators
There were no significant differences between the two groups in operation time, intraoperative bleeding volume, postoperative anal exhaust and postoperative hospital stay between the two groups (P>0.05), as shown in Table 2.
Table 2.
Perioperative indicators of the two groups of patients (x̅±s)
| Indicator | Observation group (n=78) | Control group (n=73) | t | P |
|---|---|---|---|---|
| Operation time (min) | 238.49±37.49 | 240.21±42.52 | 0.264 | 0.792 |
| Intraoperative bleeding volume (ml) | 459.38±67.42 | 468.53±70.13 | 0.817 | 0.415 |
| Postoperative anal exhaust (h) | 61.23±19.50 | 63.21±21.09 | 0.599 | 0.550 |
| Postoperative hospital stay (d) | 6.02±1.29 | 6.32±1.44 | 1.350 | 0.179 |
Evaluation of psychological state before and after intervention
HAMA and HAMD scores in two groups of patients after intervention were evidently lower than those before intervention (P<0.05), and the observation group had lower scores after intervention scores than the control group (P<0.05), as indicated in Table 3 and Figure 1.
Table 3.
Evaluation of psychological state before and after intervention (points, x̅±s)
| Group | Time | HAMA | HAMD |
|---|---|---|---|
| Observation group (n=78) | Before intervention | 24.01±5.29 | 22.19±3.47 |
| After intervention | 12.03±3.10* | 10.37±2.16* | |
| t | 17.256 | 25.540 | |
| P | <0.001 | <0.001 | |
| Control group (n=73) | Before intervention | 23.79±4.77 | 22.75±4.08 |
| After intervention | 15.64±2.93 | 13.29±2.76 | |
| t | 12.439 | 16.409 | |
| P | <0.001 | <0.001 |
Note: Compared with the control group in the same period;
P<0.05.
Figure 1.
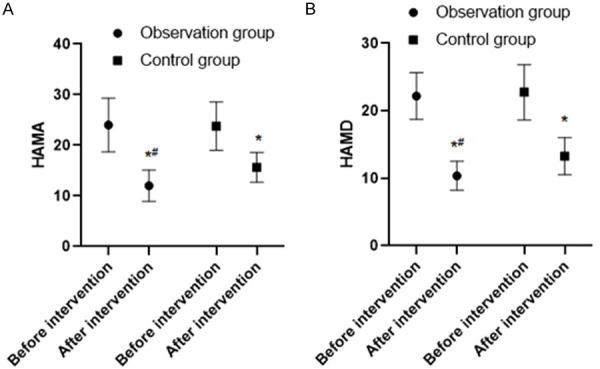
Evaluation of psychological state before and after intervention. Note: Compared with before intervention, *P<0.05; compared with the control group, #P<0.05. A: HAMA; B: HAMD.
Comparison of self-efficacy scores before and after intervention
The self-decision-making, positive attitude and self-decompression in both groups of patients after intervention were critically higher than before intervention (P<0.05), and the observation group had lower after intervention scores in each dimension of self-efficacy than the control group (P<0.05), as shown in Table 4.
Table 4.
Comparison of self-efficacy scores before and after intervention (points, x̅±s)
| Group | Time | Self-decision-making | Positive attitude | Self-decompression |
|---|---|---|---|---|
| Observation group (n=78) | Before intervention | 8.68±1.26 | 36.84±5.20 | 51.86±7.21 |
| After intervention | 13.52±1.78* | 44.52±6.12* | 64.72±7.08* | |
| t | 19.601 | 8.446 | 11.240 | |
| P | <0.001 | <0.001 | <0.001 | |
| Control group (n=73) | Before intervention | 8.49±1.44 | 36.19±4.93 | 51.07±8.15 |
| After intervention | 11.04±1.39 | 41.05±4.97 | 57.38±6.94 | |
| t | 10.886 | 5.932 | 5.037 | |
| P | <0.001 | <0.001 | <0.001 |
Note: Compared with the control group in the same period;
P<0.05.
Comparison of psychological crisis before and after intervention
The emotional, cognitive, and behavioral scores in Psychological Crisis Scale of the two groups after intervention were notably lower than those before intervention (P<0.05), and the observation group had remarkably lower scores of psychological crisis in each dimension than the control group (P<0.05), as listed in Table 5.
Table 5.
Comparison of psychological crisis before and after intervention
| Group | Time | Emotional score | Cognitive score | Behavioral scores |
|---|---|---|---|---|
| Observation group (n=78) | Before intervention | 6.08±0.95 | 6.85±1.25 | 5.49±0.83 |
| After intervention | 4.16±0.54* | 3.22±0.49* | 3.27±0.31* | |
| t | 15.518 | 23.878 | 22.129 | |
| P | <0.001 | <0.001 | <0.001 | |
| Control group (n=73) | Before intervention | 6.17±1.02 | 6.97±1.20 | 5.58±0.94 |
| After intervention | 4.83±0.60 | 4.38±0.75 | 4.10±0.62 | |
| t | 9.675 | 15.638 | 11.230 | |
| P | <0.001 | <0.001 | <0.001 |
Note: Compared with the control group in the same period;
P<0.05.
Comparison of hope degree before and after intervention
Score of each dimension and total score of hope degree in the two groups after intervention increased remarkably than those before intervention (P<0.05), and the scores in observation group after intervention were obviously higher than those before intervention (P<0.05), as shown in Table 6.
Table 6.
Comparison of hope level before and after intervention (points, x̅±s)
| Group | Time | Attitudes towards reality and the future | Take positive action | Keep close relationships with others | Total score |
|---|---|---|---|---|---|
| Observation group (n=78) | Before intervention | 6.85±2.17 | 6.17±1.82 | 5.21±1.83 | 17.96±4.28 |
| After intervention | 11.27±2.96* | 10.97±2.11* | 9.95±2.28* | 31.04±7.30* | |
| t | 10.636 | 15.214 | 14.319 | 13.651 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | |
| Control group (n=73) | Before intervention | 6.98±2.05 | 6.23±1.77 | 5.15±1.96 | 18.21±3.12 |
| After intervention | 9.07±2.10 | 8.52±1.93 | 7.48±2.31 | 24.59±6.06 | |
| t | 6.085 | 7.471 | 6.841 | 7.998 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 |
Note: Compared with the control group in the same period;
P<0.05.
Comparison of nursing satisfaction
The satisfaction to nursing care after intervention in observation group was dramatically higher than that of control group (P<0.05), as shown in Table 7.
Table 7.
Comparison of nursing satisfaction between two groups of patients [n (%)]
| Group | Number of cases | Very satisfied | Satisfied | Dissatisfied | Satisfaction rate (%) |
|---|---|---|---|---|---|
| Observation group (n=78) | 48 | 49 (62.82) | 25 (32.05) | 4 (5.13) | 94.87 |
| Control group (n=73) | 48 | 32 (43.84) | 30 (41.10) | 11 (15.07) | 84.93 |
| χ2 | - | - | - | - | 4.165 |
| P | - | - | - | - | 0.041 |
Discussion
Psychological research has shown that when people suffer severe traumas or changes, their psychological status will be disturbed, and they are prone to a great sense of psychological crisis, tension, anxiety, and depression, causing serious impact to physical and mental health [12]. For patients undergoing cervical cancer surgery, due to the fear to disease and surgical trauma, their normal organ function and estrogen secretion will be affected. Such effects will further affect body function and produce a series of stress reactions. In turn, the patients will enter a state of crisis, which imposes adverse effect to the recovery [13,14].
Crisis intervention is an effective intervening model in psychological nursing care. The intervention, via a series of physical and psychological interventions, helps patients recover from the crisis as soon as possible, thereby helping them to restore mental stability. This study analyzed the effect of crisis intervention nursing on perioperative psychological state and self-efficacy of patients with laparoscopic radical hysterectomy. The results have shown that HAMA and HAMD scores in observation group were remarkably lower than those in control group after intervention, the observation group had lower post-intervention scores in each dimension of self-efficacy than the control group, the observation group had remarkably lower scores of psychological crises in each dimension than the control group, and the scores of hope degree in observation group after intervention were obviously higher than those before intervention. Compared with conventional perioperative nursing care, crisis nursing intervention can effectively promote the improvement of patients’ negative psychological emotions, as well as their self-management efficiency and hope degree, and this consequence is consisted with those reported by scholars [15,16].
Based on the literature reports [17,18] and analysis of the possible causes, this study implemented the crisis intervention nursing from four aspects: cognitive intervention, psychological intervention, behavior intervention, and social support. Among them, health education in terms of cognitive intervention was implemented for patients to keep a scientific and reasonable understanding of cervical cancer, thus to alleviate their tension and anxiety on disease and surgery [19,20]. Psychological intervention targeted the negative emotions of patients, helped them relieve the negative psychological pressure by empathy, companionship and other psychological support, and encouraged them to release their negative emotions, thereby adjusting mental state and improving clinical treatment compliance [21,22]. Through scientific and reasonable guidance on patients’ rehabilitation, exercise, diet, etc., behavioral intervention helped to improve the disease managing ability of patients, promoted the postoperative rehabilitation, and helped them to adapt to the postoperative living status as soon as possible [23]. Social support, through the sense of social support brought by family members and relatives, enabled the patients to feel the goodwill from the society. By participating in social activities, they could transfer the attention from disease and avoid the impact of negative psychological emotions [24,25].
In addition, the nursing satisfaction of patients in observation group was significantly higher than that of the control group. This suggested that through effective nursing countermeasures, the negative psychological mood of patients and the satisfaction degree to nursing care could be both improved, which is conductive to improving nurse-patient relationship. The results reported in this study are consistent with those reported by previous scholars [26], indicating that effective nursing intervention can effectively alleviate the adverse psychological state of patients during perioperative period. The crisis intervention nursing which covers aforementioned four interventions, helps patients understand disease treatment and strengthen their compliance behavior, thereby promoting postoperative recovery and helping to adapt to postoperative life. However, due to the limited time and sample size in this study, the results may be biased. Meanwhile, only the patients undergoing laparoscopic radical cervical cancer surgery were analyzed. In the follow-up study, we’ll further expand the sample size and analyze the impact of crisis intervention nursing on different malignant tumors, so that more reliable clinical basis for improving the quality of life in patients with malignant tumors can be provided.
In conclusion, crisis intervention nursing on patients with laparoscopic radical hysterectomy is conductive to alleviating the anxiety, depression and other adverse emotions of patients, reducing their sense of psychological crisis, improving the self-efficacy and hope degree of curing disease, and greatly improving the satisfaction with nursing care.
Disclosure of conflict of interest
None.
References
- 1.Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, Buda A, Yan X, Shuzhong Y, Chetty N, Isla D, Tamura M, Zhu T, Robledo KP, Gebski V, Asher R, Behan V, Nicklin JL, Coleman RL, Obermair A. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379:1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- 2.Lairson DR, Fu S, Chan W, Xu L, Shelal Z, Ramondetta L. Mean direct medical care costs associated with cervical cancer for commercially insured patients in Texas. Gynecol Oncol. 2017;145:108–113. doi: 10.1016/j.ygyno.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Rauh LA, Saks EJ, Nakad-Rodriguez D, Showalter TN, Duska LR. Cervical cancer care in rural Virginia: the impact of distance from an academic medical center on outcomes & the role of non-specialized radiation centers. Gynecol Oncol. 2018;150:338–342. doi: 10.1016/j.ygyno.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 4.Zhang S, Wang S, Lv A, Huang S. Laparoscopically assisted radical vaginal hysterectomy for early-stage cervical cancer: a systemic review and meta-analysis. Int J Gynecol Cancer. 2016;26:1497–502. doi: 10.1097/IGC.0000000000000794. [DOI] [PubMed] [Google Scholar]
- 5.Tapera O, Kadzatsa W, Nyakabau AM, Mavhu W, Dreyer G, Stray-Pedersen B, Sjh H. Sociodemographic inequities in cervical cancer screening, treatment and care amongst women aged at least 25 years: evidence from surveys in Harare, Zimbabwe. BMC Public Health. 2019;19:428. doi: 10.1186/s12889-019-6749-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melamed A, Margul DJ, Chen L, Keating NL, Del Carmen MG, Yang J, Seagle BL, Alexander A, Barber EL, Rice LW, Wright JD, Kocherginsky M, Shahabi S, Rauh-Hain JA. Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med. 2018;379:1905–1914. doi: 10.1056/NEJMoa1804923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Health and Family Planning Commission of the People’s Republic of China. Guidelines for the standardized diagnosis and treatment of cervical cancer and precancerous lesions (for trial implementation) Chinese Journal of Medical Frontiers (Electronic Edition) 2013;8:40–49. [Google Scholar]
- 8.Brandt B, Sioulas V, Basaran D, Kuhn T, LaVigne K, Gardner GJ, Sonoda Y, Chi DS, Long Roche KC, Mueller JJ, Jewell EL, Broach VA, Zivanovic O, Abu-Rustum NR, Leitao MM Jr. Minimally invasive surgery versus laparotomy for radical hysterectomy in the management of early-stage cervical cancer: survival outcomes. Gynecol Oncol. 2020;156:591–597. doi: 10.1016/j.ygyno.2019.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leath CA, Monk BJ. Twenty-first century cervical cancer management: a historical perspective of the gynecologic oncology group/NRG oncology over the past twenty years. Gynecol Oncol. 2018;150:391–397. doi: 10.1016/j.ygyno.2018.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanao H, Matsuo K, Aoki Y, Tanigawa T, Nomura H, Okamoto S, Takeshima N. Feasibility and outcome of total laparoscopic radical hysterectomy with no-look no-touch technique for FIGO IB1 cervical cancer. J Gynecol Oncol. 2019;30:e71. doi: 10.3802/jgo.2019.30.e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JJ, Burger EA, Regan C, Sy S. Screening for cervical cancer in primary care: a decision analysis for the US preventive services task force. JAMA. 2018;320:706–714. doi: 10.1001/jama.2017.19872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasamatsu T, Ishikawa M, Murakami N, Okada S, Ikeda SI, Kato T, Itami J. Identifying selection criteria for non-radical hysterectomy in FIGO stage IB cervical cancer. J Obstet Gynaecol Res. 2019;45:882–891. doi: 10.1111/jog.13902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim AW, Hamilton W, Hollingworth A, Stapley S, Sasieni P. Performance characteristics of visualising the cervix in symptomatic young females: a review of primary care records in females with and without cervical cancer. Br J Gen Pract. 2016;66:e189–e192. doi: 10.3399/bjgp16X683833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matanes E, Abitbol J, Kessous R, Kogan L, Octeau D, Lau S, Salvador S, Gotlieb WH. Oncologic and surgical outcomes of robotic versus open radical hysterectomy for cervical cancer. J Obstet Gynaecol Can. 2019;41:450–458. doi: 10.1016/j.jogc.2018.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Bernard L, Fearon D, McFaul S, Faught W. Role of primary care enrolment in advanced cervical cancer diagnosis: a population-based case-control study. Int J Gynecol Cancer. 2020;30:29–34. doi: 10.1136/ijgc-2019-000713. [DOI] [PubMed] [Google Scholar]
- 16.Li F, Guo H, Qiu H, Liu S, Wang K, Yang C, Tang C, Zheng Q, Hou Y. Urological complications after radical hysterectomy with postoperative radiotherapy and radiotherapy alone for cervical cancer. Medicine (Baltimore) 2018;97:e0173. doi: 10.1097/MD.0000000000010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piedimonte S, Czuzoj-Shulman N, Gotlieb W, Abenhaim HA. Robotic radical hysterectomy for cervical cancer: a population-based study of adoption and immediate postoperative outcomes in the United States. J Minim Invasive Gynecol. 2019;26:551–557. doi: 10.1016/j.jmig.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Bianchi FP, Gallone MS, Fortunato F, Boccalini S, Martinelli D, Prato R, Tafuri S. Epidemiology and cost of cervical cancer care and prevention in Apulia (Italy), 2007/2016. Ann Ig. 2018;30:490–501. doi: 10.7416/ai.2018.2249. [DOI] [PubMed] [Google Scholar]
- 19.Ladd IG, Gogoi RP, Bogaczyk TL, Larson SL. Cervical cancer patients’ willingness and ability to serve as health care educators to advocate for human papillomavirus vaccine uptake. J Cancer Educ. 2019;34:608–613. doi: 10.1007/s13187-018-1348-2. [DOI] [PubMed] [Google Scholar]
- 20.Melamed A, Rauh-Hain JA, Ramirez PT. Minimally invasive radical hysterectomy for cervical cancer: when adoption of a novel treatment precedes prospective, randomized evidence. J. Clin. Oncol. 2019;37:3069–3074. doi: 10.1200/JCO.19.01164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Musselwhite LW, Oliveira CM, Kwaramba T, de Paula Pantano N, Smith JS, Fregnani JH, Reis RM, Mauad E, Vazquez FL, Longatto-Filho A. Racial/ethnic disparities in cervical cancer screening and outcomes. Acta Cytol. 2016;60:518–526. doi: 10.1159/000452240. [DOI] [PubMed] [Google Scholar]
- 22.Pankaj S, Nazneen S, Kumari S, Kumari A, Kumari A, Kumari J, Choudhary V, Kumar S. Comparison of conventional Pap smear and liquid-based cytology: a study of cervical cancer screening at a tertiary care center in Bihar. Indian J Cancer. 2018;55:80–83. doi: 10.4103/ijc.IJC_352_17. [DOI] [PubMed] [Google Scholar]
- 23.Ito F, Sugiura A, Toyoda S, Itani Y, Iwai K, Yamada Y, Tanase Y, Kawaguchi R, Kobayashi H, Kita T. Search for conditions to avoid parametrectomy during radical hysterectomy for cervical cancer. J Obstet Gynaecol Res. 2019;45:1371–1375. doi: 10.1111/jog.13986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pimple SA, Mishra GA. Global strategies for cervical cancer prevention and screening. Minerva Ginecol. 2019;71:313–320. doi: 10.23736/S0026-4784.19.04397-1. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Kim K, Park SJ, Lee JY, Kim K, Lim MC, Kim JW. Comparative effectiveness of abdominal versus laparoscopic radical hysterectomy for cervical cancer in the postdissemination era. Cancer Res Treat. 2019;51:788–796. doi: 10.4143/crt.2018.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bateman LB, Blakemore S, Koneru A, Mtesigwa T, McCree R, Lisovicz NF, Aris EA, Yuma S, Mwaiselage JD, Jolly PE. Barriers and facilitators to cervical cancer screening, diagnosis, follow-up care and treatment: perspectives of human immunodeficiency virus-positive women and health care practitioners in Tanzania. Oncologist. 2019;24:69–75. doi: 10.1634/theoncologist.2017-0444. [DOI] [PMC free article] [PubMed] [Google Scholar]


