Abstract
Dengue virus and severe acute respiratory syndrome coronavirus 2 coexist in dengue‐endemic countries; therefore, the adoption of preventive measures is essential to control the spread of both viruses. We conducted an ecological study to compare the temporal patterns of the incidence of dengue before and during the Coronavirus disease 2019 (COVID‐19) pandemic in Peru. A time‐series analysis comparing the incidence of dengue using a Student's t test with variance correction was performed. Poisson regression was applied to determine the incidence rate ratio (IRR) of dengue before and during the COVID‐19 pandemic. The incidence of dengue was found to be increased in all endemic regions of Peru during the COVID‐19 pandemic, with the highest incidences registered in Ica (IRR = 90.14), Huánuco (IRR = 38.6), and Ucayali (IRR = 23.78), with the exception of Piura (IRR = 0.83). The highest increases in the number of dengue cases per million inhabitants were in Ucayali (393.38), Tumbes (233.19), Ica (166.08), and Loreto (129.93). The gradient of dengue cases was positive in all endemic regions during the COVID‐19 pandemic. The number of dengue cases per million increased during the COVID‐19 pandemic throughout Peru and in several endemic regions, with the exception of Piura.
Keywords: COVID‐19; dengue; interrupted time series analysis, Peru; SARS‐CoV‐2
1. INTRODUCTION
Dengue is the most important mosquito‐borne viral infection. It causes 400 million cases of dengue fever worldwide every year. In the word, most cases are mild or asymptomatic, and only 100 million cases are clinically symptomatic, of which half a million require hospitalization. 1 Dengue can be misdiagnosed as other febrile illnesses, resulting in an underestimation of the actual number of cases. 2 As there is no specific treatment for this disease, only early diagnosis and access to immediate medical attention allow for the timely management of the disease, thereby preventing its progression to a serious stage and/or death. 1
Due to epidemics, other public health issues such as dengue have been neglected in Peru due to the excessive prioritization of the prevention and control of these new diseases. 3 , 4 In March 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID‐19) a pandemic caused by the severe acute respiratory syndrome coronavirus type 2 (SARS‐CoV‐2). 5 The Americas have reported the highest number of cases to date. 6 However, Latin America and the Caribbean continue to experience dengue epidemics that cause a large medical, human, and economic burden, which is why they should not be ignored. 7
Currently, both viruses coexist in dengue‐endemic countries, and it may be difficult to differentiate one from the other because both diseases share identical clinical symptoms, 8 and laboratory results. 9 The trends of COVID‐19 and dengue analyzed in other countries have allowed us to reflect upon the relevance of adopting preventive measures necessary to control the spread of both diseases 8 , 10 , 11 , 12 The purpose of this study was to compare the temporal pattern of dengue incidences before and during the COVID‐19 pandemic in Peru.
2. METHODS
2.1. Study design
An ecological study was conducted using secondary data sources.
2.2. Geographical area of the study
Data on dengue and COVID‐19 cases were assessed in 23 regions of Peru that have reported dengue cases in the past 3 years as an analysis unit, of which only the regions defined as endemic by the Ministerio de Salud del Perú (Ministry of Health of Peru)—such as Loreto, Amazonas, Ucayali, Junín, Tumbes, Huánuco, Piura, and Lambayeque—and not endemic as Ica were considered (see Supporting Information Figure).
2.3. Data sources
Data on the number of dengue cases were obtained from the virtual Health Situation Room of the Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, CDC, Peru (National Center for Epidemiology, Prevention and Disease Control, CDC, Peru) (available at https://www.dge.gob.pe/salasituacional/). This database contains the updated epidemiological information necessary to understand the healthcare situation and trends of diseases subject to epidemiological surveillance to guide, prioritize, and focus healthcare interventions by national, regional, and local authorities for the control of the health problems identified.
2.4. Procedures
Several databases were constructed using Microsoft Excel for each of the studied regions, as well as a database containing data from all Peruvian territories. The date of notification of cases was taken into account to determine the epidemiological weeks of COVID‐19, and each was estimated using STATA® 16.0 and Microsoft® Excel. The COVID variable was regarded as a variable consisting of two values, which allowed for the division of time into two stages: before and during the COVID‐19 pandemic. The population variable was determined based on population data estimated for each year in Peru and in each region, according to the Instituto Nacional de Estadística e Informática (National Institute of Statistics and Informatics or INEI, Spanish acronym). The variable “number of dengue cases per epidemiological week” in each region and in Peru was calculated as the annual number of dengue cases registered in the virtual Health Situation Room of the Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, CDC, Peru, expressed as a real number for each epidemiological week from 2015 to 2020. Cases per million were calculated based on the variable “dengue cases per epidemiological week” and taking into account the estimated population in Peru and in each region. The temperature and humidity variables were determined based on the data available for each region, calculating the mean temperature and humidity of each station by epidemiological week, according to the Servicio Nacional de Meteorología e Hidrología del Perú (National Service of Meteorology and Hydrology or SENAMHI, Spanish acronym). The data are available on the website: https://www.senamhi.gob.pe/?%26p=estaciones
2.5. Statistical analysis
Epidemiological weeks were converted into time series to analyze the time series of Peru and of each endemic region. A white noise test was performed to assess the randomness of the time series. The Kendall Tau test was performed to determine whether the series is stationary. The partial autocorrelation function was used to determine the existence of any temporal dependence of the number of dengue cases at a given time as opposed to previous periods. To estimate the average incidence of dengue (cases per million) before and during the COVID‐19 pandemic, Student's t test was used with correction of variances, and Poisson regression was applied to compare the incidence of dengue before and during the COVID‐19 pandemic, obtaining an incidence rate ratio (IRR) crude and IRR adjusted for temperature and humidity. Moreover, 95% confidence intervals (CIs) and p values were calculated.
2.6. Ethical aspects
This study did not require the approval of an ethics committee as it was an analysis of secondary aggregate data obtained from an open‐access public domain that does not allow for the identification of the cases assessed.
3. RESULTS
In 2020, the total number of dengue cases was 895 in the department of Amazonas, 1776 in Huánuco, 4256 in Junín, 10 829 in Loreto, 208 in Piura, 3104 in Tumbes, 10 934 in Ucayali, 577 in Lambayeque, 7126 in Ica, and 38 879 nationwide. The number of dengue cases per million increased during the COVID‐19 pandemic throughout Peru as well as in several endemic regions, with the exception of Piura, where it decreased. The incidence of dengue has increased during the COVID‐19 pandemic in all dengue‐endemic regions of Peru, showing a greater increase in Huánuco (IRR = 58.3, 95% CI: 46.26–73.47), Ica (IRR = 53.93, 95% CI: 48.27–60.25), and Ucayali (IRR = 30.66, 95% CI: 28.56–32.92). However, adjusting for temperature and humidity, Ica is the region with the highest increase (adjusted IRR = 90.14, 95% CI: 80.60–100.81). Piura showed the lowest increase in incidence (IRR = 0.7, 95% CI: 0.59–0.83) and adjusting for temperature and humidity, (adjusted IRR = 0.83, 95% CI: 0.70−0.98). These results are statistically significant (p < 0.001, except el IRR adjusted of Ica: p = 0.029), suggesting that the incidence of dengue has changed between the pre‐pandemic era and the pandemic era in Peru (Table 1).
Table 1.
Incidence of dengue and cases per million inhabitants during the COVID‐19 pandemic in endemic regions of Peru
| Region | Pre‐COVID‐19a | COVID‐19a | IRR crude | 95% CI crude | IRR adjustedb | 95% CI adjusted |
|---|---|---|---|---|---|---|
| Amazonas | 7.84 | 41.25 | 5.25* | 4.64−5.94 | 5.39* | 4.75–6.12 |
| Huánuco | 0.87 | 50.99 | 58.3* | 46.26−73.47 | 38.6* | 30.47–48.90 |
| Junín | 7.39 | 61.12 | 8.2* | 7.67−8.77 | 10.15* | 9.43–10.93 |
| Loreto | 59.16 | 129.93 | 2.18* | 2.10−2.25 | 2.17* | 2.10−2.25 |
| Piura | 2.8 | 1.94 | 0.7* | 0.59−0.83 | 0.83** | 0.70−0.98 |
| Tumbes | 33.18 | 233.19 | 6.91* | 6.42−7.46 | 6.25* | 5.75–6.80 |
| Ucayali | 12.68 | 393.38 | 30.66* | 28.56−32.92 | 23.78* | 21.66–26.10 |
| Lambayeque | 6.21 | 7.86 | 1.26* | 1.12−1.41 | 2.17* | 1.89–2.50 |
| Ica | 3.04 | 166.08 | 53.93* | 48.27−60.25 | 90.14* | 80.60–100.81 |
| Peru | 8.22 | 32.60 | 3.93* | 3.87–3.99 | ‐ |
Abbreviations: 95% CI, 95% confidence interval; IRR, incidence rate ratio.
Dengue cases per million inhabitants.
Adjusted for temperature and humidity.
p < 0.001
p = 0.029.
Figure 1 shows that the time series of Peru and its nine endemic regions evidenced a generally increasing trend. Additionally, the values were not random, there were no seasonal influences on the variability of data before or during the COVID‐19 pandemic, and there was no autocorrelation between epidemiological weeks in any region. In most endemic regions, a positive gradient of total dengue cases has been observed since the beginning of the COVID‐19 pandemic in Peru, especially in the regions of Amazonas, Huánuco, Ucayali, Junín, Tumbes, and Ica. The national graph shows a decrease in the number of dengue cases reported as from the first case of COVID‐19 reported in Peru, which increased again over time. As shown in Figure 2, there was a general increase in the number of dengue cases reported in Peru during 2020 relative to that in 2018 and 2019.
Figure 1.
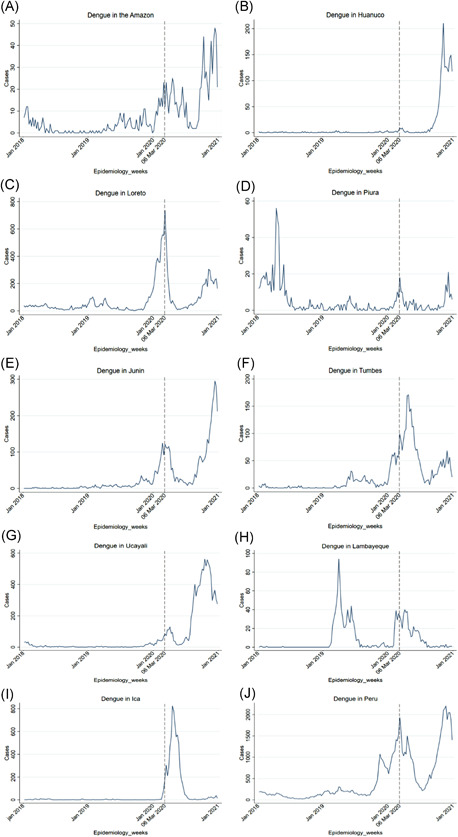
Number of dengue cases per epidemiological week from January 2018 to December 2020 in nine endemic regions of Peru and nationwide. (A) Amazon. (B) Huanuco. (C) Loreto. (D) Piura. (E) Junin. (F) Tumbes. (G) Ucayali. (H) Lambayeque. (I) Ica. (J) Peru. The vertical black dotted line corresponds to the first case of COVID‐19 reported in Peru, dividing the time into two periods: before and during the COVID‐19 pandemic
Figure 2.
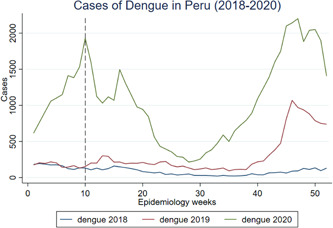
Number of dengue cases per epidemiological week in 2018, 2019, and 2020 in Peru. The vertical black dotted line corresponds to the first case of COVID‐19 reported in Peru, dividing the time into two periods: before and during the COVID‐19 pandemic
4. DISCUSSION
The results of this study suggest that the variability in the number of dengue cases in Peru and its endemic regions during the years 2018–2020 was influenced by seasonal drivers. The upward trend coincides with the rainy season in the Amazon regions and with the summer on the coast. 13 There was no autocorrelation between the number of cases in a given epidemiological week and that in any previous week. This is consistent with previous findings in China, where the majority of cases increase in the epidemiological weeks of summer and where the number of dengue cases in a certain month is related to that in the previous month. 14
We observed that since the first case of COVID‐19 was reported in Peru, there has been a decrease in the number of dengue cases reported in several endemic regions of Peru. This temporal pattern is consistent with findings in Brazil. 15 This could be due to the fact that the epidemiological alert triggered by an increase in the number of COVID‐19 cases in Peru has affected the epidemiological surveillance of dengue, resulting in an underreporting of dengue cases, as has also occurred in recent epidemics, where the excessive prioritization of the prevention and control of emerging diseases has led to the unintentional neglect of endemic diseases. 4 Dengue virus is transported mainly by infected travelers. 1 Therefore, social isolation, quarantine, and other preventive measures that were implemented in Peru to counteract the progression of COVID‐19 could have generated a real decrease in the incidence of dengue. 11 , 15 In contrast, difficulty in access to timely diagnosis together with the population's concern about the risk of being infected with COVID‐19 in healthcare facilities may be another reason for the decrease in the number of dengue cases reported at the beginning of the COVID‐19 pandemic. 16
Similarly, until July 2020, in the West Pacific region, countries such as China, Malaysia, Vietnam, and Australia registered fewer cases of dengue compared with that in the same period in 2019. 17 Moreover, in the Americas, data registered up to epidemiological week 21, 2020, show a reduction by approximately 10% compared with that in 2019. 18 Countries such as Bolivia, Honduras, Mexico, Paraguay, and Brazil reported a large increase in the number of dengue cases during the first weeks of 2020, 11 , 15 , 19 which abruptly decreased subsequently, coinciding with the exponential increase in the number of COVID 19 cases. 11 , 15
The findings of our study also demonstrate that the number of dengue cases per million inhabitants during the COVID‐19 pandemic has exceeded the number of cases reported in the years before the pandemic. This is in line with findings in other geographical areas such as Brazil, the Southwest Indian Ocean Islands, 16 and Asia. 20 Paradoxically, this could also be explained because of the prevention measures established to prevent COVID‐19 transmission because, during the quarantine, populations have lived in close contact with each other for a long time, which promotes the reproduction of arthropods/mosquitoes in and around the houses. 21
Aedes aegypti is found in 22 of the 24 regions of Peru, due to population migration from endemic areas and social determinants such as unplanned urban growth, deficient provision of basic services such as drinking water, housing development, and poverty conditions that make vector control increasingly difficult. 13 The reduction of vector control measures, the suspension of preventive campaigns, and fumigations 16 may have resulted in an increase in the number of cases during the COVID‐19 pandemic. Moreover, some populations believe that fumigation can favor the spread of COVID‐19, and for fear of contagion, do not allow health authorities to apply this vector control measure, resulting in a higher risk for dengue. 22
Previous studies found difficulties in the correct diagnosis of dengue and COVID‐19 cases because both diseases share similar clinical symptoms, which is why coinfection in endemic areas is very likely to occur. 9 , 23 An increase in the incidence of dengue and other arboviral diseases poses a real threat during the COVID‐19 pandemic 24 because it could lead to the overburdening of health systems.
During the Phenomenon Niño Costero 2017 in Peru, Piura was the region that reported 64% of all dengue cases nationwide, being the region with the highest incidence rate in the country. 25 This generated a high natural immunization of its population, which could explain the decrease in the incidence of dengue in the following years, even during the COVID‐19 era. In addition, Piura is the only region where DENV‐2 and DENV‐3 are circulating, although all four dengue serotypes are currently circulating throughout the country, with DENV‐1 and DENV‐2 circulating in the regions of Loreto, Ucayali, Tumbes, and Lambayeque, and only DENV‐2 in Junin and Huánuco. 13
The limitations of this study mainly relate to Peru having a passive surveillance system, and therefore, the results could have a selection bias, which could result in their underestimation. Furthermore, being an ecological study, no inferences can be made at the individual level (ecological fallacy).
In conclusion, the number of dengue cases per million has increased during the COVID‐19 pandemic throughout Peru and in several endemic regions, with the exception of Piura, where it has decreased. The entire country has experienced an increased incidence during the COVID‐19 pandemic compared with the incidence before the COVID‐19 pandemic. However, Huánuco, Ica, and Ucayali are the regions with the highest increase. Coepidemics of COVID‐19 and dengue in endemic areas, especially in Latin America and Southeast Asia, constitute a health, economic, and social burden. Therefore, it is important to apply vector control measures in conjunction with those established to prevent COVID‐19, as well as measures that allow for the timely and adequate deployment of health personnel.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information.
Plasencia‐Dueñas R, Failoc‐Rojas VE, Rodriguez‐Morales AJ. Impact of the COVID‐19 pandemic on the incidence of dengue fever in Peru. J Med Virol. 2021;94:393‐398. 10.1002/jmv.27298
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the public domain in the National Center for Epidemiology, Prevention and Disease Control, CDC, Peru (available at https://www.dge.gob.pe/salasituacional/) and Servicio Nacional de Meteorología e Hidrología del Perú (National Service of Meteorology and Hydrology or SENAMHI, Spanish acronym) available on the website https://www.senamhi.gob.pe/?%26p=estaciones
REFERENCES
- 1. WHO Dengue and severe dengue [sede Web]. Washington D.C. USA; 2020. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue. Accessed August 18, 2020.
- 2. Waggoner JJ, Gresh L, Vargas MJ, et al. Viremia and clinical presentation in Nicaraguan patients infected with zika virus, chikungunya virus, and dengue virus. Clin Infect Dis. 2016;63(12):1584‐1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ledermann DW. El hombre y sus epidemias a través de la historia. Revista chilena de infectología. 2003;20:13‐17. [Google Scholar]
- 4. Caylà JA. Epidemias mediáticas: una reflexión para la salud pública. Gac Sanit. 2009;23:362‐364. [DOI] [PubMed] [Google Scholar]
- 5. Organización Mundial de la Salud . COVID‐19: cronología de la actuación de la OMS. [sede Web]. Washington. [Última actualización: 29 de enero de 2021; acceso: 10 de febrero de 2021]. Disponible en: https://www.who.int/es/news/item/29-06-2020-covidtimeline
- 6. WHO . Coronavirus Disease (COVID‐19) Dashboard. [sede Web]. Washington, DC; 2021. Accessed February 10, 2021. https://covid19.who.int/
- 7. Esparza J. Epidemias y pandemias virales emergentes: ¿Cuál será la próxima? Invest Clin. 2016;57:231‐235. [PubMed] [Google Scholar]
- 8. Dash N, Rose W, Nallasamy K. India's lockdown exit: are we prepared to lock horns with COVID‐19 and dengue in the rainy season? Pediatr Res. 2020;89:1047‐1048. [DOI] [PubMed] [Google Scholar]
- 9. Miah MA, Husna A. Coinfection, coepidemics of COVID‐19, and dengue in dengue‐endemic countries: a serious health concern. J Med Virol. 2020;93:161‐162. 10.1002/jmv.26269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Din M, Asghar M, Ali M. COVID‐19 and dengue coepidemics: a double trouble for overburdened health systems in developing countries. J Med Virol. 2020;93:601‐602. 10.1002/jmv.26348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mascarenhas MDM, Batista FMA, Rodrigues MTP, Barbosa OAA, Barros VC. Simultaneous occurrence of COVID‐19 and dengue: what do the data show? Cad Saude Publica. 2020;36(6):e00126520. [DOI] [PubMed] [Google Scholar]
- 12. Cardona‐Ospina JA, Arteaga‐Livias K, Villamil‐Gómez WE, et al. Dengue and COVID‐19, overlapping epidemics? An analysis from Colombia. J Med Virol. 2020;93:522‐527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Valderrama B. Situación de dengue en el Perú a la semana 53. 2020. 29(53):753–761.
- 14. Lu L, Lin H, Tian L, Yang W, Sun J, Liu Q. Time series analysis of dengue fever and weather in Guangzhou, China. BMC Public Health. 2009;9:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lorenz C, Dias Bocewicz AC, Corrêa de Azevedo Marques C, et al. Have measures against COVID‐19 helped to reduce dengue cases in Brazil? Travel Med Infect Dis. 2020;37:101827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Olive MM, Baldet T, Devillers J, et al. The COVID‐19 pandemic should not jeopardize dengue control. PLOS Neglected Trop Dis. 2020;14(9):e0008716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. WHO . Update on the Dengue situation in the Western Pacific Region [sede Web]; 2020 [UpDate el 13 August 2020; acceso el 18 de August 16, 2020]. https://www.who.int/docs/default-source/wpro---documents/emergency/surveillance/dengue/dengue-20200813.pdf?sfvrsn=fc80101d_38
- 18. Organización Panamericana de la Salud/Organización Mundial de la Salud . Actualización Epidemiológica: Dengue [sede Web]. Washington, D.C.: OPS/OMS; 2020 [actualizada el 10 de junio de 2020; acceso 18 de agosto de 2020]. https://iris.paho.org/bitstream/handle/10665.2/52289/EpiUpdate10June20202_spa.pdf?sequence=2%26isAllowed=y
- 19. PAHO Epidemiological update dengue [sede Web] . 2020; [Update 7 February 2020; access 18 August 2020]. https://www.paho.org/hq/index.php?option=com_docman%26view=download%26category_slug=dengue-2217%26alias=51690-7-february-2020-dengue-epidemiological-update-1%26Itemid=270%26lang=es
- 20. Harapan H, Ryan M, Yohan B, et al. Covid-19 and dengue: double punches for dengue‐endemic countries in Asia. Rev Med Virol. 2020;31:e2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Awan UA, Zahoor S, Ayub A, Ahmed H, Aftab N, Afzal MS. COVID‐19 and arboviral diseases: another challenge for Pakistan's dilapidated healthcare system. J Med Virol. 2020;93:4065‐4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cruz JPS, Tovilla‐Zárate CA, González‐Morales DL, González‐Castro TB. Risk of a syndemic between COVID‐19 and dengue fever in southern Mexico. Gac Med Mex. 2020;156(5):460‐464. [DOI] [PubMed] [Google Scholar]
- 23. Mejía‐Parra JL, Aguilar‐Martinez S, Fernández‐Mogollón JL, et al. Characteristics of patients coinfected with severe acute respiratory syndrome coronavirus 2 and dengue virus, lambayeque, Peru, May‐August 2020: a retrospective analysis. Travel Med Infect Dis. 2021;43:102132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilder‐Smith A, Tissera H, Ooi EE, Coloma J, Scott TW, Gubler DJ. Preventing dengue epidemics during the COVID‐19 pandemic. Am J Trop Med Hyg. 2020;103(2):570‐571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guzmán J. Situación Epidemiológica de dengue en el Perú, a la SE 52. 2017;26(52): 1628–1630.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available in the public domain in the National Center for Epidemiology, Prevention and Disease Control, CDC, Peru (available at https://www.dge.gob.pe/salasituacional/) and Servicio Nacional de Meteorología e Hidrología del Perú (National Service of Meteorology and Hydrology or SENAMHI, Spanish acronym) available on the website https://www.senamhi.gob.pe/?%26p=estaciones


