Abstract
Background
Telemedicine has spread rapidly during the coronavirus disease 2019 (COVID‐19) pandemic and shown its usefulness, particularly for patients with epilepsy, compared to face‐to‐face visits. We sought to evaluate the clinical features of patients with childhood onset epilepsy associated with consultations by telephone call during the COVID‐19 pandemic.
Methods
We retrospectively investigated the medical records of patients with childhood onset epilepsy who visited an outpatient clinic in Saitama Children's Medical Center, Saitama, Japan, from 1 March 2020 to 30 September 2020. To find the clinical features of patients who utilized telemedicine consultation (by telephone call), we divided the patients into the telemedicine group and the face‐to‐face group. We then reviewed the clinical features. Telemedicine consultation was not implemented for new patients.
Results
We enrolled 776 outpatients in total, and 294 patients (37.9%) utilized telemedicine consultations. The total number of visits was 2,299 and the total number of telemedicine consultations was 373 (16.2%). No clinical feature was associated with telemedicine consultations except for age at onset of epilepsy. The number of oral antiepileptic drugs prescriptions decreased in 23 of 776 (3.0%) of the patients who did not experience seizure deterioration, including status epilepticus, or who visited the emergency room.
Conclusion
Telemedicine consultations were successfully utilized for epilepsy treatment at our outpatient clinic, regardless of epilepsy type, etiology, seizure frequency, comorbidities, and patients' residential areas. Thus, telemedicine by telephone call may be a useful resource in the management of patients with childhood onset epilepsy during the pandemic.
Keywords: comorbidity, epilepsy management, etiology, face‐to‐face visits, telemedicine
Background
Telemedicine has changed medical practice over the last two decades, thanks to the advances in telecommunication technologies and the Internet. It has been proven to be effective for neurological patients' care, such as those with epilepsy and headache. 1 , 2 , 3 , 4 , 5 , 6 Compared to traditional, face‐to‐face consultations for the treatment of epilepsy, telemedicine is not less effective with regard to seizure control, hospitalizations, and medication adherence. 2 , 5 Additionally, patients and caregivers report satisfaction with telemedicine because of its potential for reducing their loss of work and school time, travel time, and cost, and allows better access to medication. 3 , 7
The coronavirus disease 2019 (COVID‐19) pandemic has accelerated the rapid spread of telemedicine due to its many advantages, such as reducing exposure to infection for patients, caregivers, and medical staff during the pandemic. 8 , 9 , 10 However, some patients with epilepsy reported being forced to miss an epilepsy‐related consultation or medical service due to a national or state lockdown that resulted in seizure deterioration. 11 , 12 , 13 , 14 , 15 , 16 In addition, comorbid psychiatric conditions such as stress and anxiety, sleep disorders, and less physical activity were reported to affect these patients' health. 17 , 18 , 19
In Japan, the government relaxed telemedicine regulations and permitted consultations via telephone only, to prevent the spread of COVID‐19. In this study, we aimed to evaluate the association of clinical features of patients with childhood onset epilepsy with telemedicine consultations during the COVID‐19 pandemic.
Subjects and methods
This study was approved by the Saitama Children's Medical Center Institutional Review Board. Because of its retrospective nature, the need for informed consent was waived.
We retrospectively investigated the medical records of patients with childhood onset epilepsy at an outpatient clinic in Saitama Children's Medical Center, Saitama, Japan, from 1 March to 30 September 2020. In this study, outpatients with a confirmed epilepsy diagnosis were included based on (i) visiting our hospital more than twice (in‐person or via telemedicine) during the study period, and (ii) receiving a prescription of oral antiepileptic drugs (AEDs). In our hospital, telemedicine consultations via telephone were permitted from the middle of March 2020. The availability of telemedicine consultations was announced to patients and caregivers on our institution's website and by telephone by doctors in the outpatient department. In our institution, telemedicine consultations were not implemented for new patients during the study period, they were performed only for regular‐visit patients. This was because it is difficult to evaluate information concerning the seizure type and comorbidities via telephone only and then develop an appropriate epilepsy management strategy.
To determine the clinical features associated with telemedicine consultations, we divided the outpatients with epilepsy into a telemedicine group and face‐to‐face group. All outpatients in the telemedicine group received phone calls from a physician at least once during the study period. We reviewed the following clinical features: age at last visit; gender; number of visits; age at onset of epilepsy; duration of epilepsy treatment; epilepsy type; etiology; seizure frequency; comorbidities (attention‐deficit/hyperactivity disorder, autistic spectrum disorder, intellectual disability, and cerebral palsy); number of oral AEDs; and change in number of oral AEDs. In addition, we collected information concerning the patients' residential address and categorized the residential areas as “outside” and “inside” Saitama prefecture.
Continuous variables are presented as median with interquartile range (IQR), and categorical variables are expressed as frequencies and percentages. Statistical analyses were performed using the non‐parametric Mann‐Whitney U test for continuous variables and the chi‐squared test or Fisher's exact test for categorical variables using SPSS software, version 24.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set as P < 0.05.
Results
A total of 776 outpatients (385 females [49.6%]) met the inclusion criteria for this study. We recorded a total of 2,299 consultations, with 373 (16.2%) of those being telemedicine consultations. The number of telemedicine consultations increased from the end of March as Saitama prefecture reported an increased number of COVID‐19 patients (the first wave of COVID‐19) and decreased from the beginning of June 2020 as the of number of COVID‐19 patients in the area decreased (Fig. 1). After the Japanese government cancelled its state of emergency the number of telemedicine consultations remained at a low level, despite the country experiencing its second wave of COVID‐19. The number of consultations in May also declined because of a succession of holidays in early May, called “Golden Week” (4–8 May), and closure of outpatient clinic because of the Japanese Society of Child Neurology's annual meeting (originally intended for 25–29 May, but finally postponed to mid‐August).
Fig. 1.
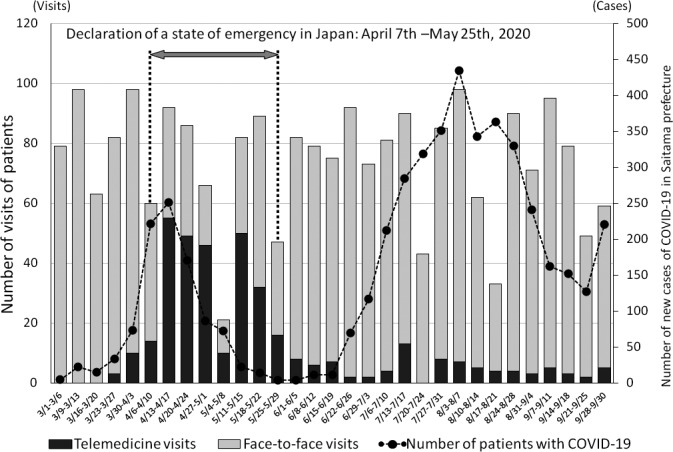
The number of telemedicine consultations and face‐to‐face visits among patients with epilepsy and the evolution of the COVID‐19 pandemic in Saitama prefecture, Japan.
Of the 776 outpatients, 294 (37.9%) were in the telemedicine group and 482 (62.1%) in the face‐to‐face group. There were no significant differences in clinical features associated with telemedicine consultations, except for age at onset of epilepsy (Table 1). Concerning more than one etiology, “structural and genetic”, “structural and infectious”, and “structural and immune” were found in the telemedicine group and face‐to‐face group as follows: eight patients vs 10, two vs one, and one vs one, respectively. Concerning more than one comorbidity, we found “intellectual disability and autistic spectrum disorder”, “intellectual disability and attention‐deficit/hyperactivity disorder”, and “intellectual disability and cerebral palsy” between the two groups in 21 patients versus 21, one versus none, and 22 versus 36, respectively. None of the patients were diagnosed with COVID‐19. Very few of the patients had the number of oral AEDs prescribed changed. The number of the oral AEDs was increased overall in 27 of 776 patients (3.5%) and decreased in 23 of 776 patients (3.0%). No patient who changed the number of the oral AEDs experienced seizure deterioration, including status epilepticus, or visited the emergency room in either group.
Table 1.
Patients' characteristics
| Telemedicine group | Face‐to‐face group | P value | |||
|---|---|---|---|---|---|
| (n = 294) | (n = 482) | ||||
| Age at last visit (years), median (IQR) | 10.8 | (6.4–14.5) | 11.5 | (7.6–14.8) | 0.39 |
| Gender, female, n (%) | 152 | (51.7) | 233 | (48.3) | 0.36 |
| Number of visits, median (IQR) | 2 | (2–3) | 3 | (2–3) | 0.62 |
| Telemedicine | 1 | (1–6) | 0 | ||
| Age at onset of epilepsy (months), median (IQR) | 44.0 | (9.0–84.3) | 50.0 | (16.0‐100.5) | 0.001 |
| Duration of treatment (years), median (IQR) | 5.3 | (2.6–9.6) | 4.5 | (2.3–9.2) | 0.19 |
| Epilepsy type, n (%) | |||||
| Generalized | 34 | (11.6) | 70 | (14.5) | 0.37 |
| Focal | 243 | (82.7) | 391 | (81.1) | |
| Combined | 17 | (5.8) | 21 | (4.4) | |
| Etiology n (%) | |||||
| Unknown | 172 | (58.5) | 295 | (61.2) | 0.46 |
| Known | 122 | (41.5) | 187 | (38.8) | |
| Structural | 83 | (28.2) | 125 | (25.9) | |
| Genetic | 47 | (16.0) | 64 | (13.3) | |
| Infectious | 2 | (0.7) | 1 | (0.2) | |
| Metabolic | 0 | (0.0) | 2 | (0.4) | |
| Immune | 1 | (0.3) | 7 | (1.5) | |
| Seizure frequency, n (%) | |||||
| Seizure free ≥1 year | 124 | (42.2) | 194 | (40.2) | 0.57 |
| Yearly | 82 | (27.9) | 148 | (30.7) | |
| Monthly | 36 | (12.2) | 66 | (13.7) | |
| Weekly | 12 | (4.1) | 24 | (5.0) | |
| Daily | 40 | (13.6) | 50 | (10.4) | |
| Comorbidities, n (%) | 179 | (60.9) | 269 | (55.8) | |
| ADHD | 3 | (1.0) | 6 | (1.2) | 0.17 |
| Autistic spectrum disorder | 27 | (9.2) | 34 | (7.1) | |
| Intellectual disability | 172 | (58.5) | 252 | (52.3) | |
| Cerebral palsy | 23 | (7.8) | 36 | (7.5) | |
| Number of oral AEDs, median (IQR) | 1 | (1–2) | 1 | (1–2) | 0.24 |
| Number of changing oral AEDs, n (%) | |||||
| None | 278 | (94.6) | 448 | (92.9) | 0.07 |
| Increase | 5 | (1.7) | 22 | (4.6) | |
| Decrease | 11 | (3.7) | 12 | (2.5) | |
| Residential areas | |||||
| Outside the prefecture | 14 | (4.8) | 15 | (3.1) | 0.24 |
| Inside the prefecture | 280 | (95.2) | 467 | (96.9) | |
ADHD, attention‐deficit/hyperactivity disorder; AEDs, antiepileptic drugs; IQR, interquartile range.
Discussion
There was a rapid increase in telemedicine consultations in our hospital during the COVID‐19 pandemic. Thus, this study investigated whether there were any specific clinical features associated with the use of telemedicine consultations in patients with childhood onset epilepsy. We found no significant differences except age at onset of epilepsy between the telemedicine and face‐to‐face group. This study demonstrates that telemedicine consultations were successfully utilized as an important tool for epilepsy treatment at an outpatient clinic, regardless of the etiology, AEDs, seizure frequency, and comorbidities of the patient.
COVID‐19 has dramatically changed daily life all over the world. The Japanese government declared a state of emergency from 7 April to 25 May 2020, and citizens were instructed to stay at home to restrict the operation of schools and other facilities. However, this declaration had no legal penalties for noncompliance, unlike “lockdowns” in other countries, because of Japanese legal restrictions on implementing such measures. Our hospital is in a densely populated urban area near Tokyo, where the number of new COVID‐19 cases increased from the beginning of April 2020.
Remote medical consultation in Japan was not widely used before the COVID‐19 pandemic, because the government regulations stated that these consultations could not be carried out only by telephone but required a video system (i.e., video phones), Internet access devices (i.e., personal computers and cellphones), and a software application for online medical care. However, these regulations were relaxed from 28 February 2020 to allow telephone‐only consultation as an emergency measure to prevent the spread of COVID‐19. In this study, the number of telemedicine consultations changed in synchrony with the number of new COVID‐19 cases during the country's first wave. However, the number of telemedicine consultations remained at a low level after the state of emergency was revoked, even during the country's second wave of COVID‐19. This may be due to the low mortality rate and percentage of severe COVID‐19 cases during the second wave in Japan. 20 , 21 , 22
In our study, we found that age at onset of epilepsy was younger in the telemedicine group than in face‐to‐face group with a statistically significant difference. Additionally, the duration of treatment for epilepsy in the telemedicine group seemed to be longer than that in the face‐to‐face group, although the difference was not statistically significant. Furthermore, telephone consultation was performed regardless of the patients' residential areas. The results of this study may indicate that the patient/caregiver‐physician relationship, which had been built on previous face‐to‐face visits before the COVID‐19 pandemic, may easily carry over into telemedicine consultations. After all, the trust between patients/caregivers and their physician is the foundation of epilepsy care and is more difficult to engender by telemedicine than face‐to‐face consultations. Conversely, there were no differences in the seizure frequency and the number of oral AEDs between the two groups. Thus, telemedicine consultations via telephone might be efficient during the pandemic, regardless of the presence of intractable epilepsy.
Changing the number of oral AEDs was not common, and there was no statistically significant difference between the two groups. Despite not being statistically significant, increases in the number of AEDs was higher in the face‐to‐face group than in the telemedicine group. This may be because patients/caregivers naturally felt anxiety about an increased frequency of seizures, and so requested an in‐person consultation. Previous surveys reported that 15–30% patients with epilepsy experienced seizure deterioration during the COVID‐19 pandemic. 11 , 12 , 13 , 14 , 15 , 16 Although our study did not evaluate seizure deterioration, the actual percentage of patients whose seizure frequencies had exacerbated would be expected to be higher than that of those who were prescribed an increased number of AEDs. On the other hand, decreases in the number of AEDs prescribed was similar between the two groups. However, it is recommended that any changes in patients' treatment should be postponed unless absolutely necessary, to avoid emergency consultations during the pandemic. 23 The physicians may have felt comfortable changing the treatment for the following reasons: the “non‐lockdown”, compulsory health insurance and the realization that the emergency medical care system was successfully maintained during the pandemic.
This study is limited by its retrospective design and single‐hospital analysis structure. Additionally, we did not evaluate seizure deterioration, psychiatric conditions, such as anxiety and depression, or sleep disorders, and the effects of these issues will need to be further investigated. Further surveys about the family structure, the distance from patients' homes to our hospital, means of transportation, employment status of patients/caregivers, and loss of time and cost incurred will also be useful information to inform physicians on how to effectively perform epilepsy consultation via telemedicine. It is well‐known that a disadvantage of telemedicine is that physical and neurological examinations cannot be performed. Moreover, consultation via telephone also has difficulties in direct observation of epileptic seizures and novel, abnormal movements, compared with a via video consultation. As we focused on regular‐visit patients, rather than new patients, we concluded that telemedicine consultations via telephone may be safe and, therefore, they could become one of the options for epilepsy management after the COVID‐19 pandemic, in cases where the clinical symptoms, including seizure frequency, are stable.
Conclusion
In conclusion, we performed telemedicine consultations by telephone for patients with epilepsy in our hospital during the COVID‐19 pandemic. There appear to be no clinical features associated with telemedicine consultations compared with face‐to‐face visits. As such, telemedicine may be a useful resource to enable regular consultations with patients with epilepsy in Japan during the pandemic.
Disclosure
Shin‐ichiro Hamano has received funding for travel and speaker honoraria from UCB Japan Co. Ltd, Daiichisankyo Co. Ltd, and Eisai Co. Ltd., and has received research funds from Syneos Health Clinical Co. Ltd for clinical trial of Zogenix. All other authors declare no conflicts of interest.
Funding information
This work was supported by the Ministry of Health, Labour and Welfare Research program on rare and intractable diseases (Grant number JPMH20FC1039).
Author contributions
K.K., S.H., and D.H. contributed to the concept and design of this study; K.K. and D.H. performed the statistical analysis; K.K. drafted the manuscript; A.H., H.N., Y.H., R.M., R.K., and A.O. critically reviewed the manuscript and supervised the entire study process. All authors read and approved the final manuscript.
References
- 1. Chua R, Craig J, Wootton R, Patterson V. Randomised controlled trial of telemedicine for new neurological outpatient referrals. J. Neurol. Neurosurg. Psychiatry 2001; 71: 63–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rasmusson K, Hartshorn JC. A comparison of epilepsy patients in a traditional ambulatory clinic and a telemedicine clinic. Epilepsia 2005; 46: 767–70. [DOI] [PubMed] [Google Scholar]
- 3. Bahrani K, Singh MB, Bhatia R et al. Telephonic review for outpatients with epilepsy–A prospective randomized, parallel group study. Seizure 2017; 53: 55–61. [DOI] [PubMed] [Google Scholar]
- 4. Lo MD, Gospe SM. Telemedicine and child neurology. J. Child. Neurol. 2019; 34: 22–6. [DOI] [PubMed] [Google Scholar]
- 5. Hatcher‐Martin JM, Adams JL, Anderson ER et al. Telemedicine in neurology. Neurology 2020; 94: 30–8. [DOI] [PubMed] [Google Scholar]
- 6. Sattar S, Kuperman R. Telehealth in pediatric epilepsy care: a rapid transition during the COVID‐19 pandemic. Epilepsy Behav. 2020; 111: 107282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fortini S, Espeche A, Caraballo R. Telemedicine and epilepsy: a patient satisfaction survey of a pediatric remote care program. Epilepsy Res. 2020; 165: 106370. [DOI] [PubMed] [Google Scholar]
- 8. Kuchenbuch M, D'Onofrio G, Wirrell E et al. An accelerated shift in the use of remote systems in epilepsy due to the COVID‐19 pandemic. Epilepsy Behav. 2020; 112: 107376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sanchez‐Larsen A, Gonzalez‐Villar E, Díaz‐Maroto I et al. Influence of the COVID‐19 outbreak in people with epilepsy: analysis of a Spanish population (EPICOVID registry). Epilepsy Behav. 2020; 112: 107396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rametta SC, Fridinger SE, Gonzalez AK et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID‐19 pandemic. Neurology 2020; 95: e1257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alkhotani A, Siddiqui MI, Almuntashri F, Baothman R. The effect of COVID‐19 pandemic on seizure control and self‐reported stress on patient with epilepsy. Epilepsy Behav. 2020; 112: 107323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reilly C, Muggeridge A, Cross JH. The perceived impact of COVID‐19 and associated restrictions on young people with epilepsy in the UK: young people and caregiver survey. Seizure 2021; 85: 111–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mostacci B, Licchetta L, Cacciavillani C et al. The impact of the COVID‐19 pandemic on people with epilepsy. An Italian survey and a global perspective. Front. Neurol. 2020; 11: 613719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Assenza G, Lanzone J, Brigo F et al. Epilepsy care in the time of COVID‐19 pandemic in Italy: risk factors for seizure worsening. Front. Neurol. 2020; 11: 737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rosengard JL, Donato J, Ferastraoaru V et al. Seizure control, stress, and access to care during the COVID‐19 pandemic in New York City: the patient perspective. Epilepsia 2021; 62: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Puteikis K, Jasionis A, Mameniškienė R. Recalling the COVID‐19 lockdown: insights from patients with epilepsy. Epilepsy Behav. 2021; 115: 107573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pasca L, Zanaboni MP, Grumi S et al. Impact of COVID‐19 pandemic in pediatric patients with epilepsy with neuropsychiatric comorbidities: a telemedicine evaluation. Epilepsy Behav. 2020; 115: 107519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang S, Wu C, Jia Y et al. COVID‐19 outbreak: the impact of stress on seizures in patients with epilepsy. Epilepsia 2020; 61: 1884–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Panda PK, Dawman L, Panda P, Sharawat IK. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID‐19 pandemic in a resource‐limited country. Seizure 2020; 81: 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miyasaka M. Is BCG vaccination causally related to reduced COVID‐19 mortality? EMBO Mol. Med. 2020; 12: e12661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Watanabe M. The COVID‐19 pandemic in Japan. Surg. Today 2020; 50: 787–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kodera S, Rashed EA, Hirata A. Correlation between COVID‐19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int. J. Environ. Res. Public Health 2020; 17: 5477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. French JA, Brodie MJ, Caraballo R et al. Keeping people with epilepsy safe during the COVID‐19 pandemic. Neurology 2020; 94: 1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


