Abstract
Aims
The Covid‐19 pandemic has had a substantial impact on the mental health of the general public and high‐risk groups worldwide. Due to its proximity and close links to China, Southeast Asia was one of the first regions to be affected by the outbreak. The aim of this systematic review was to evaluate the prevalence of anxiety, depression and insomnia in the general adult population and healthcare workers (HCWs) in Southeast Asia during the course of the first year of the pandemic.
Methods
Several literature databases were systemically searched for articles published up to February 2021 and two reviewers independently evaluated all relevant studies using pre‐determined criteria. The prevalence rates of mental health symptoms were calculated using a random‐effect meta‐analysis model.
Results
In total, 32 samples from 25 studies with 20 352 participants were included. Anxiety was assessed in all 25 studies and depression in 15 studies with pooled prevalence rates of 22% and 16%, respectively. Only two studies assessed insomnia, which was estimated at 19%. The prevalence of anxiety and depression was similar among frontline HCWs (18%), general HCWs (17%), and students (20%) while being noticeably higher in the general population (27%).
Conclusions
This is the first systematic review to investigate the mental health impact of the Covid‐19 pandemic in Southeast Asia. A considerable proportion of the general population and HCWs reported mild to moderate symptoms of anxiety and depression; the pooled prevalence rater, however, remain significantly lower than those reported in other areas such as China and Europe.
Keywords: anxiety, Covid‐19, depression, mental health, meta‐analysis
As of May 2021, 155.3 million cases of Covid‐19 had been confirmed, resulting in 3.2 million deaths worldwide. 1 Southeast Asia, comprising 11 countries and over 670 million people, was the first region outside of the initial outbreak in China to report Covid‐19 cases on 13 January 2020 in Thailand, 2 and deaths on 2 February 2020 in The Philippines. 3
Southeast Asian states share extensive ties with China. For instance, the annual travelers between Singapore (a Southeast Asian country of 3.5 million citizens) and Wuhan (the epicenter of the Covid‐19 outbreak) number around 3.4 million. 4 Furthermore, many Southeast Asian countries are developing countries with high population density and potentially lacking in resources, healthcare personnel, or facing challenges to enforce social distancing and lockdowns. 5 , 6 , 7 Nonetheless, the region has had several recent experiences with high‐profile epidemics, such as SARS in 2003 and H1N1 in 2009, which may have led to better public and medical preparedness and pandemic response in Southeast Asia. 8
Indeed, previous reports have demonstrated high rates of adverse mental health symptoms in the general population and in vulnerable groups during past infectious disease outbreaks. 9 Furthermore, a number of rapid reviews and recent meta‐analyses have established the pooled prevalence of mental health disorders during the Covid‐19 crisis in China and other areas. 10 , 11 , 12 , 13 , 14 , 15 However, the region of Southeast Asia, despite its vast population, proximity to China and recent experiences with prior epidemics, has not received a meta‐analysis on the mental health symptoms during the Covid‐19 pandemic. In order to fill the gap in the evidence, this systematic review aims to evaluate the pooled prevalence rates of anxiety, depression and insomnia in the general public, healthcare workers and students during the 1st year of the pandemic in Southeast Asia.
The 1‐year scope of the systematic review and meta‐analysis allowed for a broad evidence‐based assessment of all the available data, in order to produce a set of pooled prevalence of the key mental health symptoms studied to date and helped to address the effect of sample size bias and the heterogeneity of results between studies 16 . Furthermore, this systematic review covers the mental health impact of the general adult population, as well as healthcare workers (HCWs) and students, who have been reportedly at greater risk of experiencing mental health difficulties during the Covid‐19 pandemic. 17 , 18 The findings of this study can contribute to the existing body of research on the subject to facilitate comparisons with other regions and inform evidence‐based practice and epidemic planning of mental health needs.
Methods and Materials
The review protocol is registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020224458) with the register name ‘A meta‐analysis on the prevalence of mental disorders under the COVID‐19 pandemic over time across countries’. The systematic search was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement 2020.
Data sources and search strategy
This work is part of an overarching project of large‐scale meta‐analyses of the psychological impact of the Covid‐19 pandemic on the general and high‐risk populations across the globe. We searched the following databases for studies that met the inclusion criteria: PubMed, Embase, PsycINFO, and Web of Science from 1 February 2020 to 6 February 2021. Preprints published at medRxiv were also included in the search. To identify articles based on the requirements, we searched specific titles and abstracts using the search terms in Table S1 with Boolean operators.
Selection criteria
The search included empirical studies that reported on the prevalence of anxiety, depression, or insomnia among frontline HCWs, general HCWS, general adult populations, or adult (university) students in Southeast Asia. In addition, reports had to employ validated psychometric measures and outcomes had to be reported in English.
We did not include studies that reported on populations of children, adolescents, or adult subpopulations (e.g. pregnant women). Non‐original research or studies which were reviews, meta‐analyses, qualitative and case studies, interviews, news reports, interventional studies, or studies that did not use validated instruments or validated cut off scores to quantify prevalence rates were also excluded. We also decided to specifically focus on depression, anxiety, and insomnia, which are the most commonly reported mental health symptoms, and exclude the term distress because of the generic nature of the term and the fact that very limited studies examined distress in Southeastern Asia.
A researcher (WX) contacted the authors of papers that missed important information in several instances: (i) if they surveyed a population that included both targeted and excluded populations in a way that we could not identify the prevalence rate for our desired population; (ii) if the paper included primary data meeting our inclusion criteria, but did not report the prevalence; (iii) if the paper reported the overall prevalence without specifying whether it is mild above or moderate above: or (iv) if the paper was missing or unclear about critical information such as respondent rate, data collection time, or female proportion rate.
Data screening
Article information from various databases was initially extracted into Endnotes to remove duplicates and then imported into Rayyan. Two researchers independently (BZC & AD) screened the titles and abstracts of all papers against the inclusion and exclusion criteria. Potential conflicts were resolved by a third researcher (RKD).
Data extraction
A well‐developed coding protocol and coding book were used based on previous studies. 19 All included articles from the screening were assigned to three pairs of researchers (WX & AY, BZC & AD, RZC & SM) who thoroughly examined and extracted important data into a coding book. Relevant information including author, title, country, starting and ending dates of data collection, study design, population, sample size, respondent rate, female proportion rate, age range and mean, outcome, outcome level, instruments, cut‐off scores, and prevalence were coded using a standard coding procedure. Comments and reasons for contacting authors and/or excluding papers were also recorded.
After both coders had independently coded their articles, they would crosscheck their information. In the event of disparities and in the absence of a consensus between the two, a third coder would settle the disagreement. The third coder (AZ) did also double‐check important data including the population, sample size, mental health outcomes, outcome levels, instruments, and prevalence. Studies with unusual prevalence, cut off scores, and numbers were afterwards also checked in the sensitivity analysis.
Assessment of risk of bias
The Mixed Methods Appraisal Tool (MMAT) 20 of seven questions was used to assess the quality of research papers included in the meta‐analyses. The tool consists of seven questions and quality scores range from 0 to 7. Studies with a score of above 6 were considered high quality, between 5 and 6 were classed as medium, and with a score of below 5 were considered of low quality. Questions were individually coded by pairs of coders and any discrepancies were resolved by a third coder (RKD).
Data analysis
Version 16.1 of Stata was used and a random effects meta‐analysis conducted to extract the pooled prevalence from multiple studies using meta‐prop. Random‐effects models attempt to generalize findings beyond the included by assuming that the selected studies are random samples from a larger population. 21 We computed prediction interval to show the range of the effect sizes across studies. 22 We used the I 2 statistics to examine the heterogeneity of prevalence among studies and the heterogeneity was classed as high when I 2 was higher than 75%. 23
Sensitivity analysis
The use of conventional funnel plots to assess biases in meta‐analyses have been found to be inaccurate for meta‐analyses of proportion studies, 24 for which the Doi plot and the Luis Furuya–Kanamori (LFK) index denote a better approach for graphically representing publication bias – where a symmetrical triangle implies the absence of publication bias, while an asymmetrical triangle indicates possible publication bias. 25 The Doi plot and LFK index have higher sensitivity and power to detect publication bias than the funnel plot and Egger's regression. 26 The LFK index provides a quantitative measure to assess the asymmetry ‐ a score within ±1 indicates ‘no asymmetry’, exceeds ±1 but is within ±2 indicates ‘minor asymmetry’ and exceeds ±2 indicates ‘major asymmetry’. Figure 1 depicts the Doi plot and a Luis Furuya–Kanamori (LFK) index of −1.75, indicating ‘minor asymmetry’ and the presence of minor publication bias. Moreover, specifically, we tested the impact of publication status and sample size and did not find significant influence.
Fig. 1.
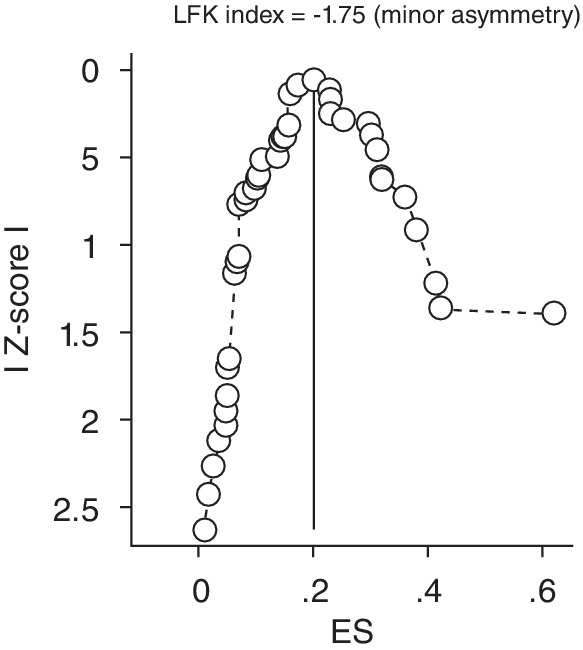
Doi plot analysis. Depiction of publication bias in the baseline meta‐analysis of proportion studies based on Doi plot and the Luis Furuya–Kanamori (LFK) index ‐a score that exceeds ±1 but is within ±2 indicates ‘minor asymmetry’.
Results
Study selection
Figure 2 illustrates the PRISMA flow chart detailing our search and study retrieval process and findings. In total, 6949 records were screened for their title, abstract and keywords. After removal of duplicates, we reviewed 168 articles by their full texts against our eligibility criteria. Finally, we analyzed data from 25 studies satisfying the inclusion criteria.
Fig. 2.
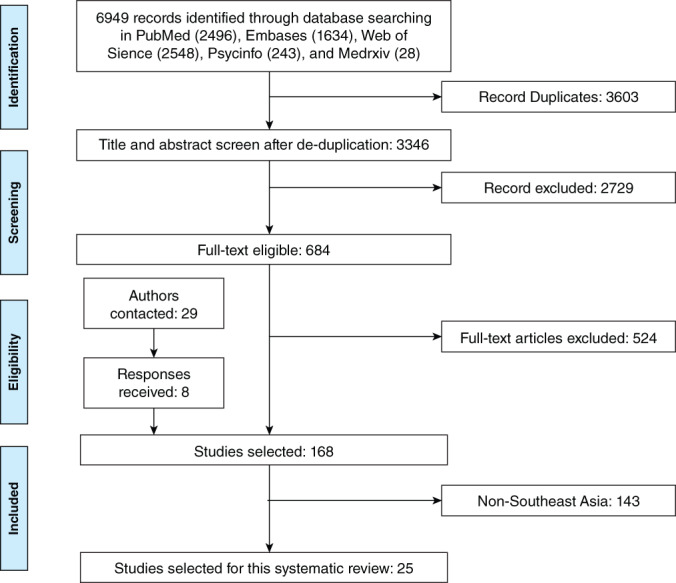
PRISMA flow diagram. Presentation of the procedure of literature searching and selection with numbers of articles at each stage.
Study characteristics
In total, 25 studies including 32 different samples and 20 352 participants from Southeast Asia were incorporated in this meta‐analysis. 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 Of these, seven studies (28.1%) were of general populations, 30 , 33 , 35 , 39 , 48 , 49 , 51 10 studies included general HCWs (43.8%), 24 , 27 , 29 , 34 , 36 , 37 , 38 , 42 , 45 , 50 five studies included frontline HCWs (18.8%), 32 , 42 , 43 , 44 , 46 and only three studies (9.4%) referred to adult students. 31 , 41 , 52 Most studies were cross‐sectional (96.0%) apart from one that was a longitudinal cohort study (4.0%). 51 The sample size across all 32 samples varied from 22 to 4004 and a median number of 294 and the proportion of female participants ranged from 47.6% to 88.1% with a median value of 69.5%. The participation rates were between 20.0% to 98.0% and a median of 70.3%. All studies had been published.
The pooled prevalence of anxiety, depression, and insomnia
All 32 samples with a total of 20 352 participants from the 25 studies reported on the prevalence of anxiety symptoms. Several validated assessment tools were used, including most commonly the Depression, Anxiety and Stress Scale ‐ 21 Items (DASS‐21) (37.5%), followed by the Generalized Anxiety Symptoms 7‐items scale (GAD‐7) (25.0%), the Hospital Anxiety and Depression Scale (HADS) (16.7%), and six other instruments (each 4.2%). Different studies used different cut‐off values to determine the overall prevalence as well as the severity of anxiety. In the random‐effects model, the pooled prevalence rate was 22% (95% CI: 19%–27%, I2 = 99.9%) (Fig. 3a), which means that on average about 22% of the adults in Southeastern Asia show anxiety symptoms during COVID‐19. The variance of true effects (tau2) is 0.21. By assuming the prevalence in logit units is normally distributed, the prediction internal is 8.1% to 36.1%. In other words, anxiety symptoms in a comparable study will usually fall in this range.
Fig. 3.
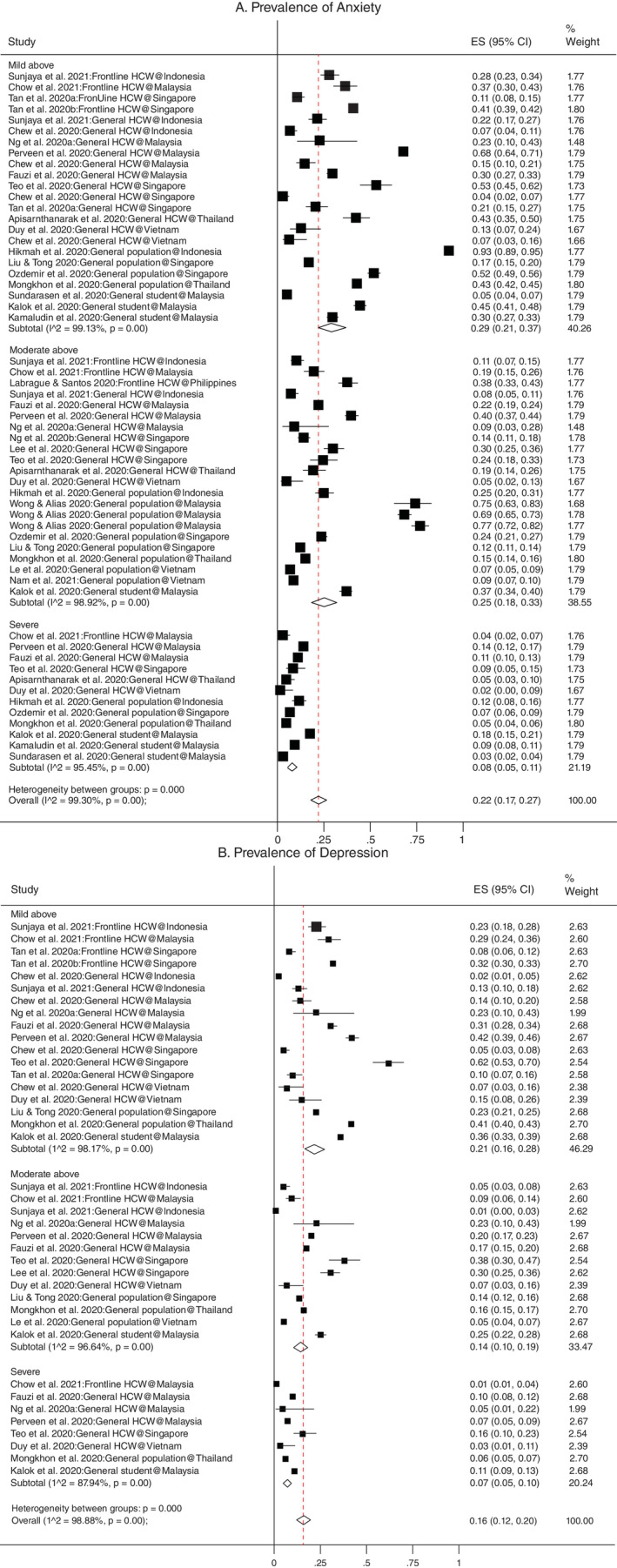
(a) Forest plot of the prevalence of anxiety. The square markets indicate the prevalence of anxiety at the different level for different population. The size of the marker correlates to the inverse variance of the effect estimates and indicates the weight of the study. The diamond data market indicates the pooled prevalence. (b) Forest plot of the prevalence of depression. The square markets indicate the prevalence of anxiety at the different level for different population. The size of the marker correlates to the inverse variance of the effect estimates and indicates the weight of the study. The diamond data market indicates the pooled prevalence.
A total of 20 samples and 13 960 respondents deriving from 15 studies 28 , 29 , 33 , 34 , 35 , 36 , 37 , 40 , 42 , 43 , 45 , 46 , 48 , 50 , 52 reported in the presence and severity of depression. A variety of rating scales were used such as DASS‐21 (60.0%), HADS (20%), and three other instruments (each 6.7%). In the random‐effects model, the pooled prevalence of depression was 16% (95% CI: 12%–20%, I2 = 99.8%) (Fig. 3b), which means that on average about 16% of the adults in Southeastern Asia show anxiety symptoms. The variance of true effects is 0.12 in logit units. By assuming the prevalence is normally distributed, the prediction internal is 6.9% to 24.8%. Hence, depression symptoms in a comparable study will usually fall in this range.
The overall prevalence of mental disorder symptoms in frontline HCWs, general HCWs, students and the general population in Southeast Asia are 18%, 17%, 20%, and 27%, respectively. The overall prevalence rates of mental disorder symptoms that surpassed the cut off values of mild, moderate, and severe symptoms were 26%, 21%, and 7%, respectively.
Only two samples from two studies 34 , 48 included the prevalence of insomnia with a pooled rate of 19%, hence insomnia is not included in the different sub‐analysis presented here.
Quality of articles
According to the Mixed Methods Appraisal Tool (MMAT), 20 seven studies (28.0%) are found to be of high quality and the remaining 18 studies (72.0%) fall into medium quality (Table 1). The subgroup analysis indicated that studies with higher quality reported lower prevalence of mental health problems in Southeast Asia (P = 0.00) (Table 2).
Table 1.
Study characteristics on mental health symptoms in COVID‐19 epidemic in Southeast Asia
| Characteristics | Total number of studies/samples † | Percent (%) | Level of analysis |
|---|---|---|---|
| Overall | 25/32 | 100 | |
| Design | Study | ||
| Cohort | 1 | 4.0 | |
| Cross‐sectional | 24 | 96.0 | |
| Publication status | Study | ||
| Preprint | 0 | 0.0 | |
| Published | 25 | 100.0 | |
| Quality | Study | ||
| >6 | 7 | 28.0 | |
| Between 5 and 6 | 18 | 72.0 | |
| <5 | 0 | ||
| Population | Study | ||
| Frontline HCW | 5 | 20.0 | |
| General HCW | 10 | 40.0 | |
| General population | 7 | 28.0 | |
| Student | 3 | 12.0 | |
| Outcome ‡ | Prevalence | ||
| Anxiety | 58 | 59.8 | |
| Depression | 39 | 40.2 | |
| Severity ‡ | Prevalence | ||
| Above mild | 41 | 42.3 | |
| Above moderate | 35 | 36.1 | |
| Severe | 20 | 20.6 | |
| Overall | 1 | 1.0 | |
| Country | Sample | ||
| Indonesia | 4 | 12.5 | |
| Malaysia | 12 | 37.5 | |
| Philippines | 1 | 3.1 | |
| Singapore | 9 | 28.1 | |
| Thailand | 2 | 6.3 | |
| Vietnam | 4 | 12.5 | |
| Median (mean) | Range | ||
| Sample size | 294 (636) | 22–4004 | Sample |
| Response rate | 77.7% (70.9%) | 17.4–100% | Sample |
| Female portion | 69.5% (68.3%) | 47.6–88.1% | Sample |
One study may include multiple independent samples. For example, Chew et al. (2020) studies the prevalence in the general population of Singapore, Indonesia, Malaysia, and Vietnam.
The total samples of mental health outcomes are larger than the 32 independent samples because one sample can assess multiple mental health outcomes including anxiety, depression, and insomnia. Similarly, a study may report multiple levels of severity on each mental health outcome for each independent sample.
Table 2.
The pooled prevalence rates of mental health symptoms by subgroups of population, outcome, and severity
| First‐level subgroup | Second‐level subgroup | Prevalence (%) | 95% CI | I2 (%) | P value |
|---|---|---|---|---|---|
| Overall | 20% | 16%–23% | 99.2% | 0.00 | |
| Population | Frontline HCW | 18% | 12%–25% | 98.3% | 0.00 |
| General HCW | 17% | 13%–21% | 97.9% | 0.00 | |
| General population | 27% | 19%–35% | 99.7% | 0.00 | |
| Student | 20% | 11%–30% | 99.2% | 0.00 | |
| Outcome | Anxiety | 22% | 18%–27% | 99.3% | 0.00 |
| Depression | 16% | 12%–20% | 99.9% | 0.00 | |
| Insomnia | 19% | 1%–23% | 99.3 | 0.00 | |
| Severity | Mild | 26% | 21%–31% | 98.9% | 0.00 |
| Moderate | 21% | 16%–26% | 98.6% | 0.00 | |
| Severe | 7% | 6%–9% | 93.7% | 0.00 | |
| Study Quality | High quality | 16% | 11%–21% | 98.5% | 0.00 |
| Medium quality | 21% | 17%–25% | 99.3% | 0.00 | |
| Subregion | Continental | 20% | 16%–23% | 99.2% | 0.00 |
| Malay Archipelago | 18% | 8%–31% | 98.9% | 0.00 |
Discussion
Overview of findings
This is the first systematic review with meta‐analysis to assess the prevalence of mental health symptoms in the adult general and high‐risk populations of Southeast Asia during the Covid‐19 crisis. It included 32 samples from 25 studies for an aggregate of 20 352 adult participants in a year of the Covid‐19 pandemic. Our findings showed that the overall prevalence of mental disorder symptoms was similar among frontline HCWs (18%), general HCWs (17%) and students (20%) while being noticeably higher in the general population (27%). Factors contributing to adverse psychological outcomes among the general population could include increased exposure to Covid‐19 information from the media 30 , 35 urban living 30 , 49 and higher levels of perceived susceptibility to Covid‐19. 51
The pooled prevalence rates of anxiety, depression and insomnia were 22%, 16% and 19%, respectively (Table 2). Anxiety was more prevalent in the general population than in HCWs and more frequent compared to depression in both groups (Table 3). Surprisingly, the overall level of moderate anxiety (21%) was not dissimilar to that of mild anxiety (26%). Regarding geographical distribution, there was a lower prevalence of depressive symptoms among the adults in the Malay Archipelago than those in continental Southeast Asia (7% vs 17%) despite comparable levels of anxiety (Table 3).
Table 3.
Subgroup analyses of the prevalence of anxiety and depression
| Groups | Subgroups | Anxiety | Depression |
|---|---|---|---|
| No. studies | 25 | 15 | |
| No. samples | 32 | 20 | |
| No. prevalence | 58 | 39 | |
| Total no. participants | 20 352 | 13 960 | |
| Overall | 22%, 95% CI: 19%–27%, I2: 99.9% | 16%, 95% CI: 12%–20%, I2: 99.9% | |
| Population | Frontline HCW | 23%, 95% CI: 13%–34%, I2: 98.1% | 14%, 95% CI: 5%–25%, I2: 98.5% |
| General HCW | 18%, 95% CI: 12%–80%, I2: 98.1% | 15%, 95% CI: 10%–21%, I2: 97.5% | |
| General population | 31%, 95% CI: 20%–44%, I2:99.7% | 16%, 95% CI: 6%–29%, I2:99.7% | |
| Student | 18%, 95% CI: 8%–32%, I2:99.4% | 23%, 95% CI: 10–39% | |
| Severity | Mild | 29%, 95% CI: 21%–37%, I2: 99.1% | 21%, 95% CI: 16–28%, I2: 98.2% |
| Moderate | 25%, 95% CI: 18%–33%, I2: 98.9% | 14%, 95% CI: 10%–19%, I2: 96.6% | |
| Severe | 8%, 95% CI: 5%–11%, I2: 95.5% | 7%, 95% CI: 5%–10%, I2: 87.9% | |
| Instrument | DASS‐21 | 17%, 95% CI: 12%–24%, I2: 98.7% | 14%, 95% CI: 10%–18%, I2: 97.7% |
| GAD‐7 | 21%, 95% CI: 12–31%, I2: 99.6% | NA | |
| HADS | 25%, 95% CI: 14–39%, I2: 97.8% | 18%, 95% CI: 7%–33%, I2: 98.1% | |
| Region | Continental | 22%, 95% CI: 17%–27%, I2: 99.3% | 17%, 95% CI: 13%–22%, I2: 98.9% |
| Malay Archipelago | 25%, 95% CI: 10%–45%, I2: 99.1% | 7%, 95% CI: 2%–16%, I2: 96.5% | |
I2 statistic indicates the heterogeneity.
CI, confidence interval.
Comparison of results with previous studies
The prevalence rates of anxiety, depression and insomnia are overall lower in Southeast Asia than those reported in previous meta‐analyses and studies from other areas or countries during the pandemic. They are considerably lower than, for example, the rates reported by the same study group covering the first year of the pandemic in Spain (34%, 36% and 52%) 53 and Africa (37%, 34% and 28%) 54 as well as by a separate meta‐analysis from China (26%, 26%, and 30%). 14 Likewise, the pooled prevalence of anxiety (22%) and depression (16%) in Southeast Asia was found to be consistently lower than the recorded scores of 33% and 32% for anxiety and 28% and 34% for depression in the meta‐analysis by Luo et al. 55 from 17 countries (China, Singapore, India, Japan, Pakistan, Vietnam, Iran, Israel, Italy, Spain, Turkey, Denmark Greece, Argentina, Brazil, Chile and Mexico), and the meta‐analysis by Salari et al. 56 from 10 countries (China, India, Japan, Iran, Iraq, Italy, Nepal, Nigeria, Spain, and UK), respectively. Furthermore, the pooled estimates from Southeast Asia are lower than the mental health outcomes previously reported among the general population and HCWs during and after the MERS and SARS epidemics where high rates of mood symptoms and post‐traumatic stress disorder (PTSD) were observed. 32 , 40 , 43 , 44 , 46
The prevalence of psychological distress among students in Southeast Asia (20%), although deriving from a limited number of studies, compares favorably to that in Spain (50%), 53 a meta‐analysis performed on studies from China, Iran, India, Brazil and the UAE (28% pooled prevalence of anxiety) 57 and a further meta‐analysis from 31 countries performed by Deng et al. (anxiety 32%, depression 34%, insomnia 33%). 58
The presence of mental health symptoms in HCWs in Southeast Asia follows a similar pattern compared with, for example, the first rapid systematic review and meta‐analyses of 13 studies in HCWs from China, where more than one in every five healthcare workers suffered from anxiety or depression, with pooled prevalence rates of 23.2% for anxiety and 22.8% for depression. 11 Subsequent reviews reported broadly similar rates including a meta‐analysis of 19 studies and estimated rates of 26% for anxiety and 25% for depression. 55 Even more surprising, however, was the finding that mental health concerns and anxiety symptoms in particular were more frequent in the Southeast Asian general population than HCWs. This pattern is at odds with previous observations elsewhere, whereby the rates were either similar or higher among HCWs compared to the general population during the same period of time. For example, Luo et al. 55 found that rates were akin between healthcare workers and the general public; though noted that studies from a number of countries such as China, Italy, Turkey, Spain and Iran reported higher‐than‐pooled prevalence among healthcare workers. Similarly, in their review, Vindegaard and Benros 59 concluded that HCWs generally appeared to experience more anxiety, depression, and sleep problems compared to the general population in a subgroup analysis of 20 studies. Furthermore, in our review, general and frontline staff recorded similar levels of psychological distress. Several previous studies demonstrated a higher psychological impact for frontline staff, yet others showed that the mental health effects of the crisis were equally felt across settings or specialties. 60 , 61 , 62
Overall, anxiety symptoms were more frequent than depression, a common finding across most studies to date. 55 Despite the considerable between‐study heterogeneity, it appears that comparable proportions of respondents across groups recorded mild and moderate symptoms both for depression and anxiety, while more severe symptoms were less common. Additionally, Vietnam compares favorably against six other Asian countries (China, Iran, Malaysia, Philippines, Pakistan, Thailand) in a separate multinational study looking at anxiety and depression scores. The mean anxiety and depression scores using the Depression, Anxiety and Stress Scale‐21 (DASS‐21) were statistically significantly lower than all the six Asian nations. 63
Although insomnia was underreported in the studies under the scope of this systematic review, it was evidently the least prevalent mental disorder in Southeast Asia at 19%. Moreover, this rate compares favorably to the levels of 36% reported in the meta‐analysis by Jahrami et al. 64 from 13 countries (Iraq, India, Germany, France, Italy, China, Mexico, Spain, Bahrain, Greece, USA, Australia, Canada) with further subgroup analysis highlighting the even greater frequency in Italy (55%) and France (51%). Overall, approximately two in five HCWs have been reported to experience some degree of sleep dysfunction, 65 while shorter sleep duration has been associated with a higher likelihood of Covid‐19 infection among HCWs. 66
Practical implications
The results from this meta‐analysis show that the rates of anxiety, depression and insomnia were lower in Southeast Asia compared to previous meta‐analyses conducted in other areas. The disparity is particularly noticeable when compared to south European countries like Spain, France, Italy, and Greece. 67 The differences between countries are likely multifactorial such as variation in pressures on healthcare systems, exposure to negative media and perceived lack of preparedness. 68
In addition, the lower prevalence rates in Southeast Asia could be associated to the recent experience with epidemics and the use of early interventions similar to those in China and east Asia. Indeed, some useful lessons could be learned from the interventions which were deployed throughout this region. Vietnam, for example, was lauded for its testing and surveillance system which was used to identify infection sources 69 and also recognized the importance of strengthening its grassroots healthcare system in order to contain Covid‐19. 70 In Singapore, the overall rates of preventative behaviors (e.g. avoiding public transport, social events and hospitals and reducing frequency/duration of shopping and eating out) were reportedly high, 39 while another Singaporean study showed that the use of an official WhatsApp channel, providing information updates to the public, was protective against the development of depression. 51 According to Luo et al. 55 the use of precautionary measures to prevent the spread of Covid‐19 and the access to up‐to‐date and accurate information were shown to shield from mental health problems.
Furthermore, a number of individual studies included in our systematic review, highlighted the mitigating role of higher levels of support against the development of anxiety symptoms. Among frontline HCWs, higher organizational and social support were both deemed to enhance resilience, 32 and Sunjaya et al. 50 underlined the importance of general HCWs to maintain frequent contact with peers and families to prevent negative mental health effects. Social, family and governmental support were found to be protective in the student population, 52 while living alone was a risk factor. 41 Furthermore, being single, separated or widowed was noted to be a risk factor within the general population 33 alongside increased exposure to Covid‐19 information from the media which was associated with a higher likelihood of anxiety. 30 , 35 A separate study reported that a dose–response correlation was observed between information exposure of three or more hours per day and the severity of affective symptoms. 48 Though Cognitive Behavioral Therapy (CBT) was not utilized in any of the previously mentioned studies, it may help with the management of anxiety and depression caused by Covid‐19. 71 Additionally, internet CBT has been shown in one study to be a cost effective intervention 72 while another highlighted its efficacy in the treatment of insomnia. 73
Finally, there is a number of Southeast Asian countries such as Myanmar, Cambodia, Laos, East Timor and Brunei without any available large‐scale data on the mental health effects of the pandemic. For these countries without country‐level studies, our systematic review on Southeast Asia may help them to use the results at the regional level as relevant evidence to guide their practice including the development of national mental healthcare strategies for pandemic‐related interventions and short, medium, and long‐term service provision.
Strengths and limitations
To our knowledge, this systematic review is the first to examine the pooled prevalence of depression, anxiety, and insomnia in the general populations, HCWs and students during the COVID‐19 outbreak in Southeast Asia. Despite the relative low number of studies per group and per country included in our meta‐analysis, the total studies covered a considerable number of participants during a whole year of the pandemic. Furthermore, our subgroup analysis provided additional valuable insights of potential particular differences and /or vulnerabilities.
Nevertheless, there are some key limitations to our review. There was considerable disparity between the number of papers reporting on the four subgroups of populations, ranging from 14 (general HCWs), to nine (general population), six (frontline HCWs) and only three (students). In addition, only two papers evaluated the presence of sleep problems, thus limiting the power of the findings on insomnia. Again, the majority of studies were cross‐sectional in design and conducted across inherently different countries at varying points in the course of the pandemic and some countries were not represented in this analysis which may limit the generalizability of our findings.
The COVID‐19 pandemic was found to cause hemodynamic changes in the brain. 74 This study mainly used self‐reported questionnaires to measure psychiatric symptoms and did not make clinical diagnosis. The gold standard for establishing psychiatric diagnosis involved structured clinical interview and functional neuroimaging. 75 , 76 , 77 Additionally, a variety of assessment tools were used to record the presence of mental health symptoms and different cut‐off values were used to determine severity making it difficult to directly compare findings across studies. The quality of studies was also variable with high quality studies recording lower prevalence of mental health issues. Furthermore, non‐English articles were excluded which could have created a bias. Finally, the studies included in our meta‐analysis were all cross‐sectional, thus the long‐term physical and psychological implications of Covid‐19 pandemic are not fully captured.
Conclusion
This systematic review is the first to report on the prevalence of anxiety, depression and insomnia in the general public and high‐risk populations of Southeast Asia during the Covid‐19 pandemic. The results of the meta‐analysis demonstrate that a significant proportion experienced at least mild to moderate levels of anxiety and depression. However, the pooled prevalence revealed lower rates of mental health symptoms in the general population, healthcare workers and students in Southeast Asia compared to other areas such as China and Europe. Our findings can inform targeted identification of mental health symptoms and facilitate appropriate resource planning and allocation in the continued Covid‐19 pandemic.
Disclosure statement
All authors have completed the Unified Competing Interest form and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years, no other relationships or activities that could appear to have influenced the submitted work.
Author contributions
S.P.: Writing – original draft, Writing – review & editing. J.C.: Methodology, Validation, Formal analysis, Investigation, Data curation, Visualization, Writing – original draft, Writing – review & editing, Supervision. J.B.: Writing – original draft, Writing – review & editing. A.D.: Investigation (Data). R.K.D.: Investigation (Data). W.X.: Investigation (Data). A.Y.: Investigation (Data). B.Z.C.: Investigation (Data). A.D.: Investigation (Data). R.Z.C.: Investigation (Data). S.M.: Investigation (Data). X.W.: Investigation (Data). S.X.Z.: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Visualization, Writing – original draft, Writing – review and editing, Supervision. S.P., J.C., and S.X.Z. co‐led this paper. All authors reviewed and approved the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Data and materials availability
All data are secondary and available per request. The coding book, coding protocol, coding cross‐check guides, data, and the code to analyze the data can be located here: https://www.dropbox.com/sh/5068kumz1o71v5d/AAAKs149KGg_XJeR7wiGALO4a?dl=0
Supporting information
Appendix S1. Supporting Information
Table S1. The search string used in this systematic review and meta‐analysis
Acknowledgments
Jiyao Chen has received research support from College of Business Oregon State University.
Contributor Information
Sofia Pappa, Email: sofia.pappa@westlondon.nhs.uk.
Dr. Jiyao Chen, Email: jiyao.chen@oregonstate.edu.
Joshua Barnett, Email: joshua.barnett2@nhs.net.
Anabel Chang, Email: anabelc@uoregon.edu.
Rebecca Kechen Dong, Email: rebecca.dong@unisa.edu.au.
Wen Xu, Email: wen.xu@nottingham.edu.cn.
Allen Yin, Email: allen-yin@hotmail.com.
Bryan Z. Chen, Email: chenzbryan@gmail.com
Andrew Yilong Delios, Email: delios9580@gmail.com.
Richard Z. Chen, Email: richardziychen@gmail.com
Saylor Miller, Email: millesay@oregonstate.edu.
Xue Wan, Email: wanxue@tongji.edu.cn.
Stephen X. Zhang, Email: stephen.x.zhang@gmail.com.
References
- 1. Coronavirus Resource Centre . COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSSE). Johns Hopkins University, Baltimore, 2021. [Cited 6 May 2021.] Available from URL: https://coronavirus.jhu.edu/map.html.
- 2. World Health Organisation . Novel Coronavirus ‐ Thailand (ex‐China). World Health Organisation, Geneva; 2020. [Cited 30 April 2021.] Available from URL: https://www.who.int/csr/don/14-january-2020-novel-coronavirus-thailand-ex-china/en/.
- 3. BBC Coronavirus: First Death Outside China Reported in Philippines. BBC, London; 2020 [Cited 30 April 2021.] Available from URL: https://www.bbc.co.uk/news/world-asia-51345855#:~:text=A%20man%20has%20died%20of,Health%20Organization%20(WHO)%20said).
- 4. Kuguyo O, Kengne A, Dandara C. Singapore COVID‐19 pandemic response as a successful model framework for low‐resource health care settings in Africa? OMICS 2020; 24: 470–478. [DOI] [PubMed] [Google Scholar]
- 5. Glassman A, Chalkidou K, Sullivan R. Does One Size Fit All? Realistic Alternatives for COVID‐19 Response in Low‐Income Countries. Washington, D.C.: Center for Global Development, 2020. [Google Scholar]
- 6. Bong CL, Brasher C, Chikumba E, McDougall R, Mellin‐Olsen J. Enright a the COVID‐19 pandemic: Effects on low‐ and middle‐income countries. Anesth. Analg. 2020; 131: 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buenaventura R, Ho J, Lapid M. COVID‐19 and mental health of older adults in the Philippines: A perspective from a developing country. Int. Psychogeriatr. 2020; 32: 1129–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peeri NC, Shrestha N, Rahman MS et al. The SARS, MERS and novel coronavirus (COVID‐19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol. 2020; 49: 717–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rogers JP, Chesney E, Oliver D et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta‐analysis with comparison to the COVID‐19 pandemic. Lancet Psychiatry 2020; 7: 611–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta‐analysis. BMJ 2020; 369: m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain Behav. Immun. 2020; 88: 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ren X, Huang W, Pan H, Huang T, Wang X, Ma Y. Mental health during the Covid‐19 outbreak in China: A meta‐analysis. Psychiatry Q. 2020; 91: 1033–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Salari N, Khazaie H, Hosseinian‐Far A et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID‐19 patients: A systematic review and meta‐analysis. Glob. Health 2020; 16: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID‐19 patients amidst the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Res. 2020; 293: 113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhang SX, Miller SO, Xu W et al. Meta‐analytic evidence of depression and anxiety in eastern Europe during the COVID‐19 pandemic. Eur. J. Psychotraumatol. 2021. 10.1080/20008198.2021.2000132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pappa S, Giannakoulis VG, Papoutsi E, Katsaounou P. Author reply ‐ Letter to the editor "The challenges of quantifying the psychological burden of COVID‐19 on heathcare workers". Brain Behav. Immun. 2021; 92: 209–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Papoutsi E, Giannakoulis V, Ntella V, Pappa S, Katsaounou P. Global burden of COVID‐19 pandemic on healthcare workers. ERJ Open Res 2020; 6: 195–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lin K, Yang BX, Luo D et al. The mental health effects of COVID‐19 on health care providers in China. Am. J. Psychiatry 2020; 177: 635–636. [DOI] [PubMed] [Google Scholar]
- 19. Chen X, Chen J, Zhang M et al. One year of evidence on mental health in China in the COVID‐19 crisis ‐ a systematic review and meta‐analysis. Medrxiv 2021. [Google Scholar]
- 20. Hong QN, Fàbregues S, Bartlett G et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018; 34: 285–291. [Google Scholar]
- 21. Cheung MW, Ho RC, Lim Y, Mak A. Conducting a meta‐analysis: Basics and good practices. Int. J. Rheum. Dis. 2012; 15: 129–135. [DOI] [PubMed] [Google Scholar]
- 22. Borenstein M, Higgins JPT, Hedges LV, Rothstein HR. Basics of meta‐analysis: I2 is not an absolute measure of heterogeneity. Res. Synth. Methods 2017; 8: 5–18. [DOI] [PubMed] [Google Scholar]
- 23. Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta‐analyses. Br. Med. J. 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta‐analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014; 67: 897–903. [DOI] [PubMed] [Google Scholar]
- 25. Furuya‐Kanamori L, Xu C, Lin L et al. P value‐driven methods were underpowered to detect publication bias: Analysis of Cochrane review meta‐analyses. J. Clin. Epidemiol. 2020; 118: 86–92. [DOI] [PubMed] [Google Scholar]
- 26. Furuya‐Kanamori L, Barendregt JJ, Doi S. A new improved graphical and quantitative method for detecting bias in meta‐analysis. Int. J. Evid. Based Healthc. 2018; 16: 195–203. [DOI] [PubMed] [Google Scholar]
- 27. Apisarnthanarak A, Apisarnthanarak P, Siripraparat C, Saengaram P, Leeprechanon N, Weber DJ. Impact of anxiety and fear for COVID‐19 toward infection control practices among Thai healthcare workers. Infect. Control Hosp. Epidemiol. 2020; 41: 1093–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chew NW, Ngiam JN, Tan BY et al. Asian‐Pacific perspective on the psychological well‐being of healthcare workers during the evolution of the COVID‐19 pandemic. BJPsych Open 2020; 6: e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Do Duy C, Nong VM, Ngo Van A, Doan Thu T, Do Thu N, Nguyen QT. COVID‐19‐related stigma and its association with mental health of health‐care workers after quarantine in Vietnam. Psychiatry Clin. Neurosci. 2020; 74: 566–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hikmah K, Prisandy L, Melinda G, Ayatullah MI. An online survey: Assessing anxiety level among general population during the coronavirus disease‐19 pandemic in Indonesia. Open Access Maced. J. Med. Sci. 2020; 8: 451–458. [Google Scholar]
- 31. Kamaludin K, Chinna K, Sundarasen S et al. Coping with COVID‐19 and movement control order (MCO): Experiences of university students in Malaysia. Heliyon 2020; 6: e05339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Labrague LJ, De los Santos JA. COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020; 28: 1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Le HT, Lai AJX, Sun J et al. Anxiety and depression among people under the nationwide partial lockdown in Vietnam. Front. Public Health 2020; 29: 589359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee MC, Thampi S, Chan HP et al. Psychological distress during the COVID‐19 pandemic amongst anaesthesiologists and nurses. Br. J. Anaesth. 2020; 125: e384–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu JC, Tong EM. The relation between official WhatsApp‐distributed COVID‐19 news exposure and psychological symptoms: Cross‐sectional survey study. J. Med. Internet Res. 2020; 22: e22142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mohd Fauzi MF, Mohd Yusoff H, Muhamad Robat R, Mat Saruan NA, Ismail KI, Mohd Haris AF. Doctors' mental health in the midst of COVID‐19 pandemic: The roles of work demands and recovery experiences. Int. J. Environ. Res. Public Health 2020; 17: 7340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ng BH, Nuratiqah NA, Faisal AH et al. A descriptive study of the psychological experience of health care workers in close contact with a person with COVID‐19. Med. J. Malaysia 2020; 75: 485–489. [PubMed] [Google Scholar]
- 38. Ng KYY, Zhou S, Tan SH et al. Understanding the psychological impact of COVID‐19 pandemic on patients with cancer, their caregivers, and health care workers in Singapore. JCO Glob. Oncol. 2020; 6: 1494–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ozdemir S, Ng S, Chaudhry I, Finkelstein E. Adoption of preventive behaviour strategies and public perceptions about COVID‐19 in Singapore. Int. J. Health Policy Manag. 2020: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Perveen A, Hamzah HB, Othamn A, Ramlee F. Prevalence of anxiety, stress, depression among Malaysian adults during COVID‐19 pandemic movement control order. Indian J. Community Health 2020; 32: 579–581. [Google Scholar]
- 41. Sundarasen S, Chinna K, Kamaludin K et al. Psychological impact of COVID‐19 and lockdown among university students in Malaysia: Implications and policy recommendations. Int. J. Environ. Res. Public Health 2020; 17: 6206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tan BY, Chew NW, Lee GK et al. Psychological impact of the COVID‐19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020; 173: 317–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tan BY, Kanneganti A, Lim LJH et al. Burnout and associated factors among health care workers in Singapore during the COVID‐19 pandemic. J. Am. Med. Dir. Assoc. 2020; 21: 1751–1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Temsah MH, Al‐Sohime F, Alamro N et al. The psychological impact of COVID‐19 pandemic on health care workers in a MERS‐CoV endemic country. J. Infect. Public Health 2020; 13: 877–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Teo WZ, Yap ES, Yip C, Ong L, Lee CT. The psychological impact of COVID‐19 on 'hidden' frontline healthcare workers. Int. J. Soc. Psychiatry 2021; 67: 284–289. [DOI] [PubMed] [Google Scholar]
- 46. Chow SK, Francis B, Ng YH et al. Religious coping, depression and anxiety among healthcare workers during the COVID‐19 pandemic: A Malaysian perspective. Healthcare (Basel) 2021; 15: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mohd Noor N, Che Yusof R, Yacob MA. Anxiety in frontline and non‐frontline healthcare providers in Kelantan, Malaysia. Int. J. Environ. Res. Public Health 2021; 18: 861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mongkhon P, Ruengorn C, Awiphan R et al. Exposure to COVID‐19‐related information and its association with mental health problems in Thailand: Nationwide, cross‐sectional survey study. J. Med. Internet Res. 2021; 23: e2536328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nam PT, Hanh Dung N, Khac Liem N et al. Anxiety among the Vietnamese population during the COVID‐19 pandemic: Implications for social work practice. Soc. Work Public Health 2021; 36: 142–149. [DOI] [PubMed] [Google Scholar]
- 50. Sunjaya DK, Herawati DMD, Siregar AY. Depressive, anxiety, and burnout symptoms on health care personnel at a month after COVID‐19 outbreak in Indonesia. BMC Public Health 2021; 21: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wong LP, Alias H. Temporal changes in psychobehavioural responses during the early phase of the COVID‐19 pandemic in Malaysia. J. Behav. Med. 2021; 44: 18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kalok A, Sharip S, Abdul Hafizz AM, Zainuddin ZM, Shafiee MN. The psychological impact of movement restriction during the COVID‐19 outbreak on clinical undergraduates: A cross‐sectional study. Int. J. Environ. Res. Public Health 2020; 17: 8522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chen RZ, Zhang SX, Xu W et al. A systematic review and meta‐analysis on mental illness symptoms in Spain in the COVID‐19 crisis. medRxiv 2021. 10.1101/2021.04.11.21255274. [DOI] [Google Scholar]
- 54. Chen J, Farah N, Dong RK et al. The mental health under the COVID‐19 crisis in Africa: A systematic review and meta‐analysis. Int. J. Environ. Res. Public Health 2021; 18: 10604. 10.1101/2021.04.19.21255755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public ‐ a systematic review and meta‐analysis. Psychiatry Res. 2020; 291: 113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Salari N, Hosseinian‐Far A, Jalali R et al. Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: A systematic review and meta‐analysis. Glob. Health 2020; 16: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lasheras I, Gracia‐García P, Lipnicki DM et al. Prevalence of anxiety in medical students during the COVID‐19 pandemic: A rapid systematic review with meta‐analysis. Int. J. Environ. Res. Public Health 2020; 17: 6603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Deng J, Zhou F, Hou W et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID‐19 pandemic: A systematic review and meta‐analysis. Psychiatry Res. 2021; 301: 113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vindegaard N, Benros ME. COVID‐19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020; 89: 531–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sahin T, Aslaner H, Eker OO, Gokcek MB, Dogan M. Effect of COVID‐19 pandemic on anxiety and burnout levels in emergency healthcare workers: a questionnaire study. Res Square 2020; 12: 987. 10.21203/rs.3.rs-32073/v1. [DOI] [Google Scholar]
- 61. Pappa S, Barnett J, Berges I, Sakkas N. Tired, worried and burned out, but still resilient: A cross‐sectional study of mental health workers in the UKduring the COVID‐19 pandemic. Int. J. Environ. Res. Public Health 2021; 18: 4457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Tiete J, Guatteri M, Lachaux A et al. Mental health outcomes in healthcare workers in COVID‐19 and non‐COVID‐19 care units: A cross‐sectional survey in Belgium. Front. Psychol. 2021; 11: 612241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wang C, Tee M, Roy AE et al. The impact of COVID‐19 pandemic on physical and mental health of Asians: A study of seven middle‐income countries in Asia. PLoS ONE 2021; 16: e0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Jahrami H, BaHammam SA, Luigi Bragazzi N, Saif Z, Faris MA, Vitiello MV. Sleep problems during the COVID‐19 pandemic by population: A systematic review and meta‐analysis. J. Clin. Sleep Med. 2021; 17: 299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Pappa S, Sakkas N, Sakka E. A year in review: Sleep dysfunction and psychological distress in healthcare workers during the COVID‐19 pandemic. Sleep Med. 2021. 10.1016/j.sleep.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Kim H, Hedge S, LaFiura C et al. COVID‐19 illness in relation to sleep and burnout. BMJ Nutr Prev Health 2021; 4: 132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Pappa S, Athanasiou N, Sakkas N et al. From recession to depression? Prevalence and correlates of depression, anxiety, traumatic stress and burnout in healthcare workers during the COVID‐19 pandemic in Greece: A multi‐center, cross‐sectional study. Int. J. Environ. Res. Public Health 2021; 18: 2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wang C, Chudzicka‐Czupała A, Tee ML et al. A chain mediation model on COVID‐19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci Rep 2021; 11: 6481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Dao TL, Nguyen TD, Hoang VT. Controlling the COVID‐19 pandemic: Useful lessons from Vietnam. Travel Med. Infect. Dis. 2020; 37: 101822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Tran BX, Hoang MT, Pham HQ et al. The operational readiness capacities of the grassroots health system in responses to epidemics: Implications for COVID‐19 control in Vietnam. J. Glob. Health 2020; 10: 011006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID‐19) beyond paranoia and panic. Ann. Acad. Med. Singapore 2020; 49: 155–160. [PubMed] [Google Scholar]
- 72. Zhang MW, Ho RC. Moodle: The cost effective solution for internet cognitive behavioral therapy (I‐CBT) interventions. Technol. Health Care 2017; 25: 163–165. [DOI] [PubMed] [Google Scholar]
- 73. Soh HL, Ho RC, Ho CS et al. Efficacy of digital cognitive behavioural therapy for insomnia: A meta‐analysis of randomised controlled trials. Sleep Med. 2020; 75: 315–325. [DOI] [PubMed] [Google Scholar]
- 74. Olszewska‐Guizzo A, Mukoyama A, Naganawa S et al. Hemodynamic response to three types of urban spaces before and after lockdown during the COVID‐19 pandemic. Int. J. Environ. Res. Public Health 2021; 18: 6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Husain SF, Yu R, Tang TB et al. Validating a functional near‐infrared spectroscopy diagnostic paradigm for major depressive disorder. Sci. Rep. 2020; 10: 9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Husain SF, Tang TB, Yu R et al. Cortical haemodynamic response measured by functional near infrared spectroscopy during a verbal fluency task in patients with major depression and borderline personality disorder. EBioMedicine 2019; 23: 102586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ho CSH, Lim LJH, Lim AQ et al. Diagnostic and predictive applications of functional near‐infrared spectroscopy for major depressive disorder: A systematic review. Front. Psych. 2020; 11: 378. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information
Table S1. The search string used in this systematic review and meta‐analysis


