Abstract
Aim
The coronavirus (COVID‐19) pandemic has led to increased concerns about adolescent mental health. This study aimed to determine the effect of the pandemic on adolescent eating disorders (EDs) by measuring changes in the number and severity of presentations to an Australian paediatric ED service that utilises a standardised approach to triage and assessment.
Methods
A 4‐year retrospective chart review (2017–2020) of all patients (n = 457) presenting to the Royal Children's Hospital Eating Disorder Service, Melbourne, was undertaken. The incidence of each diagnosis and measures of condition severity were extracted from the database and patient medical records. Clinical comments relating to the impact of COVID‐19, on both ED behaviours and treatment, were also noted.
Results
Annual presentations increased from a mean of 98.7 per annum from 2017 to 2019 to 161 in 2020 (63% increase). COVID‐19 restrictions were reported to be a trigger for ED behaviours in 40.4% of adolescents diagnosed with anorexia nervosa in 2020. There was no significant difference in severity across years despite increased cases.
Conclusions
The dramatic increase in presentations has implications for primary health and paediatric care as well as specialist ED services. Increased support is needed for EDs during this time.
Keywords: adolescent health, anorexia nervosa, Australia, coronavirus, mental health
What is already known on this topic
The COVID‐19 pandemic has negatively impacted mental health.
Isolation, loneliness and boredom are known triggers for disordered eating behaviours.
High‐level stresses can result in symptom exacerbation in mental health disorders.
What this paper adds
There has been a significant increase in the number of new anorexia nervosa (including atypical anorexia nervosa) presentations during the COVID‐19 pandemic.
Changes to normal routines and food insecurity were recognised as triggers for disordered eating behaviours, in addition to isolation, loneliness and boredom.
It was more common for COVID‐19 restrictions to trigger eating disorder behaviours in comparison to exacerbating pre‐existing disease.
On 11 March 2020, the novel coronavirus disease (COVID‐19) was declared a global pandemic. 1 Various restrictions have since been implemented world‐wide to limit the spread of disease. No Australian city has endured harsher COVID‐19 restrictions than Melbourne, Victoria, a population of 4.9 million. Melbourne's first lockdown commenced on 23 March 2020, in line with the rest of Australia. Restrictions began to ease in June, and schools variably returned to onsite learning from June 9. However, rapidly increasing COVID‐19 cases led to implementation of even harsher restrictions on July 9, 2 including evening curfews.
Measures of social distancing, mask wearing, quarantine, as well as travel and group gathering limitations, have negatively impacted mental health and well‐being. Increased levels of psychological distress, anxiety and depression have all been reported since the beginning of the pandemic. 1 , 3 , 4 Increased restricting of food and binge‐eating and purging behaviours have also been reported within the general Australian public as well as in those with eating disorders (EDs) such as anorexia nervosa (AN). 5 Adolescents have been particularly affected, as school closures, online learning, and limitations on peer gatherings including sports and recreational activities have profoundly disrupted both their educational and social routines. This is disconcerting given adolescence is a crucial period for social and emotional development, during which the foundations for mental well‐being are established. 6
The COVID‐19 pandemic has had far‐reaching consequences for population mental health and well‐being in Australia and globally. High levels of depression and anxiety have been seen, and a small number of reports have suggested an increase in the incidence of AN in adolescents presenting to services. 4 , 7 Yet concurrently concerns about the risk of COVID‐19 transmission within health facilities might also result in delayed presentation for assessment, with the risk of increased severity at the eventual time of diagnosis.
How the evolving circumstances of the COVID‐19 pandemic has affected adolescents with AN requires further investigation. This study aimed to assess the impact of COVID‐19 on the prevalence and severity of AN in young people who presented to a tertiary children's hospital in Melbourne, Australia, with the added goal of identifying predisposing features and triggers for disordered behaviours during the pandemic.
Methods
Setting
The Royal Children's Hospital (RCH) is a tertiary paediatric hospital in Melbourne, Australia, which operates a specialist ED programme that primarily manages restrictive EDs. The service has provided a similar model of care since 2008, which includes routine data collection on all patients. The mainstay of initial treatment for AN and atypical AN is a 6‐month course of Family‐Based Treatment as an outpatient. Following triage, eligible patients who present to the service undergo a standardised multidisciplinary assessment that confirms diagnosis, identifies comorbidities and determines if the patient is safe to commence outpatient treatment. Patients who are medically unstable are admitted to an adolescent medical ward; admission criteria are bradycardia (heart rate <50 beats per minute), postural hypotension (systolic blood pressure drop >20 mmHg), dehydration, hypothermia (oral temperature <35°C) or severe electrolyte abnormality.
Study design and sample
A 4‐year retrospective chart review (2017–2020) was undertaken of all patients with EDs who presented to the specialist ED programme. ED diagnoses were reported according to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM‐V). 8 New diagnoses were distinguished from recurrent presentations in patients known to the service. The incidence of AN and atypical AN cases per month was calculated to identify trends in relation to the timing of 2020 COVID‐19 restrictions.
Data on the severity of patients with AN and atypical AN were collected through review of electronic medical records. Severity measures included: the number of admissions for each individual, length of stay, incidence of bradycardia and/or postural hypotension, requirement for electrolyte supplementation and nasogastric feeding, presence of purging behaviour, presence of suicidal and/or self‐harm ideation, mental health and medical comorbid conditions, prescribed medications and body mass index (BMI) classification for underweight (where BMI < 15 kg/m2 is extreme, 15–15.99 kg/m2 is severe, 16–16.99 kg/m2 is moderate and ≥ 17 kg/m2 is mild). 8 Data were collected from day 1 of each clinical presentation to December 2020. The reasons reported for the onset of ED behaviours and engagement with clinic services were also obtained from comments recorded in patient and parent recounts during the initial clinic assessment, with recurring themes identified across presentations throughout 2020.
Statistical analysis
General descriptive statistics of the sample population were calculated for each year. Since by definition, atypical AN patients meet all diagnostic criteria for AN, with the exception of being significantly underweight, 9 these two patient groups were combined to further assess prevalence and condition severity. The incidence of each severity measure was converted to a percentage of cases (AN and atypical AN) per year. Prevalence and severity were compared between years using single‐factor analysis of variance (ANOVA), with α = 0.05. For each analysis output, p‐values less than or equal to 0.05 were considered statistically significant. All analyses were performed using GraphPad Statistics with Prism 8 software.
Ethical considerations
This study received ethics approval from the RCH Research Ethics and Governance Committee (HREC 2019.119) and complied with the World Medical Association Declaration of Helsinki. Patient consent was waived since this study utilised retrospective routinely collected data.
Results
A total of 457 patients were included in the study sample. Participant characteristics across 2017–2020 were generally similar (Table 1). Most presentations were new ED diagnoses (>90% each year) and most were female (>80% each year). The mean age at presentation each year was around 15 years. The proportion of presenting patients requiring hospital admission ranged from 50.5% to 59.6% each year. In 2020, the number of ED presentations (n = 161) far exceeded the mean number of presentations per year from 2017 to 2019 (n = 98.7, P = 0.01).
Table 1.
Characteristics of the study sample (n = 457)
| 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| Total ED presentations | 93 | 101 | 102 | 161* |
| New diagnosis made at presentation to RCH, n (%) | 89 (95.7) | 97 (96.0) | 95 (93.1) | 150 (93.2) |
| Age at presentation (years), mean (SD) | 14.92 (1.99) | 14.83 (1.91) | 15.11 (1.81) | 14.97 (1.77) |
| Sex (% female) | 80.6 | 82.2 | 90.2 | 90.1 |
| Admitted patients, n (%) | 52 (55.9) | 51 (50.5) | 56 (54.9) | 96 (59.6) |
* P‐value <0.05.
The number of new diagnoses of AN and atypical AN in adolescents who presented to hospital in 2020, by month, is illustrated in Figure 1. Between February and April 2020, there was a decrease in new cases, coinciding with growing appreciation of the risks of COVID‐19 and announcement of the pandemic in mid‐March. The situation changed in May, and from June onwards more cases presented each month than had been recorded for the same month across the previous three years. The number of new cases of restrictive EDs that presented to the RCH in 2020 peaked in August, followed by a plateau and modest decline from September.
Fig 1.
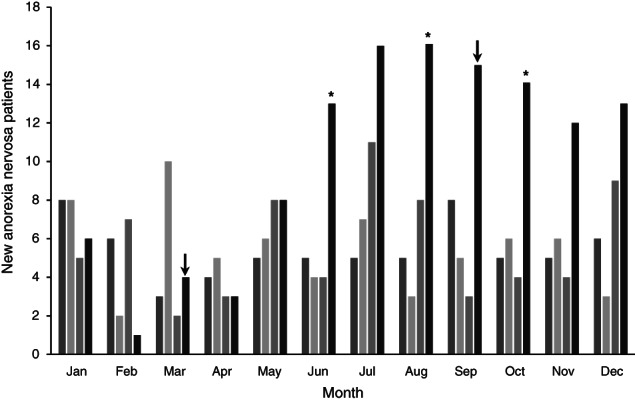
New presentations (AN and atypical AN) by month, 2017–2020. ( ), 2017; (
), 2017; ( ), 2018; (
), 2018; ( ), 2019; (
), 2019; ( ), 2020. (↓) Beginning and end of lockdown. *P‐value < 0.05.
), 2020. (↓) Beginning and end of lockdown. *P‐value < 0.05.
Measures of disease severity for new AN and atypical AN cases are summarised in Table 2. The proportion of AN and atypical AN patients admitted to hospital remained fairly consistent from 2017 to 2020 (55.9–62.4%). This was similarly observed for the incidence of bradycardia and postural hypotension, as well as the requirement for electrolyte supplementation and nasogastric refeeding. However, the proportion of patients readmitted and requiring more than two admissions decreased by more than 6% and 9% in 2020, respectively. The mean length of stay was also approximately 2 days shorter in 2020, compared to previous years. Lastly, no significant changes in the incidence of purging behaviour and suicidal or self‐harm ideation were reported between years (P = 0.85) (Table 2).
Table 2.
Markers of severity of AN and atypical AN
| 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| n = 68 | n = 68 | n = 74 | n = 133 | |
| Patients admitted (%) | 55.9 | 55.8 | 63.5 | 62.4 |
| Patients readmitted (%) | 22.1 | 14.7 | 16.2 | 8.3 |
| Patients with >2 admissions (%) | 14.7 | 11.8 | 12.2 | 3.1 |
| Length of stay (days), mean (SD) | 13.55 (6.79) | 14.03 (6.50) | 14.35 (9.08) | 11.56 (6.31) |
| Bradycardia (%) | 52.9 | 52.9 | 51.4 | 48.1 |
| Postural hypotension (%) | 19.1 | 20.6 | 20.3 | 15.8 |
| Required electrolyte supplementation (%) | 26.5 | 27.9 | 25.7 | 29.3 |
| Required nasogastric feeding (%) | 13.2 | 7.4 | 16.2 | 8.3 |
| Purging (%) | 32.4 | 25.0 | 32.4 | 26.3 |
| Suicidal ideation (%) | 26.5 | 22.1 | 29.7 | 24.1 |
| Self‐harm ideation (%) | 25.0 | 19.1 | 18.9 | 17.3 |
| Mental health comorbidities | ||||
| Depression (%) | 20.6 | 22.1 | 35.1 | 30.8 |
| Anxiety (%) | 35.3 | 32.4 | 40.5 | 41.4 |
| Obsessive compulsive disorder (%) | 8.8 | 13.2 | 9.5 | 4.5 |
| Autism spectrum disorder (%) | 2.9 | 4.4 | 6.8 | 8.3 |
| Other mental health conditions (%) | 4.4 | 4.4 | 6.8 | 2.3 |
| Medical comorbidities | ||||
| Coeliac disease (%) | 1.5 | 0.0 | 8.1 | 3.0 |
| Diabetes (%) | 2.9 | 1.5 | 0.0 | 1.5 |
| Scoliosis (%) | 5.9 | 1.5 | 4.1 | 2.3 |
| Food allergies (%) | 5.9 | 7.4 | 1.4 | 3.8 |
| Asthma (%) | 4.4 | 4.4 | 5.4 | 6.0 |
| Other medical conditions (%) | 4.4 | 5.9 | 4.1 | 3.8 |
| Prescribed medications | ||||
| Antidepressants (%) | 33.8 | 42.6 | 52.7 | 48.1 |
| Other medications (%) | 23.5 | 20.6 | 14.9 | 15.8 |
Mental health and medical comorbidities were prevalent among patients with AN and atypical AN (Table 2). Depression and anxiety were the most commonly diagnosed comorbid mental health conditions at assessment, with more than 20% and 30% of patients affected, respectively. The overall incidence of mental health comorbidities at diagnosis did not differ by year (P = 0.95). The incidence of medical comorbidities also did not differ by year, and the proportion of patients prescribed medications was similarly unchanged (P = 0.92).
Table 3 reports the proportion of patients with AN fulfilling each BMI classification. This was not reported for patients with atypical AN as by definition patients in this group are not underweight despite being malnourished. The distribution of BMI differed significantly across the study period (P < 0.005). In all 4 years, the largest proportion of AN patients was mildly malnourished with 36–38.9% recording a BMI ≥17 kg/m2. In 2017 and 2018, extremely malnourished patients (BMI <15 kg/m2) were more common than severely (BMI 15–15.99 kg/m2) and moderately (BMI 16–16.99 kg/m2) malnourished patients. In 2019, moderately malnourished patients accounted for a larger proportion of cases (30%). On the other hand, while in 2020 there was a relatively even distribution of patients with moderately, severely and extremely malnourished BMI classifications (18.9–22.2%), the proportion of extremely malnourished patients (20%) was lower than for the previous 3 years (24–31.7%).
Table 3.
Distribution of AN patient BMI
| 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| BMI (kg/m2) classification† | n = 41 | n = 51 | n = 50 | n = 90 |
| <15 (%) | 31.7 | 29.4 | 24.0 | 20.0 |
| 15–15.99 (%) | 19.5 | 19.6 | 10.0 | 22.2 |
| 16–16.99 (%) | 12.2 | 13.7 | 30.0 | 18.9 |
| ≥17 (%) | 36.6 | 37.3 | 36.0 | 38.9 |
BMI classification for AN cases only, not atypical AN.
Table 4 summarises the reported reasons for the onset of AN and atypical AN during 2020. Feelings of social isolation and loneliness was the most prominent reason reported for the onset of an ED (32.3%), followed by a change in normal routines and subsequent lack of motivation (25.6%). Cessation of community sport, along with boredom and minimal distraction from AN thoughts, were additional reasons reported for the onset of ED behaviours. A few patients also reported reduced food availability as a factor (3%). Furthermore, in 40.4% of patients assessed in 2020, it was reported that ‘The onset of [patient's] eating disorder behaviours coincided with the COVID lockdown’. A further 12.8% of patients recorded a relapse in progress during the COVID‐19 lockdown. This was summarised as a ‘COVID setback’ by clinicians and entailed either an exacerbation of existing ED behaviours or the transition from one form of ED to a restrictive‐type. Comments from patients and their families such as ‘[patient] became fearful of expected weight gain during isolation’ and ‘worried about getting fat and losing fitness’ highlighted lockdown was commonly considered to be a precipitating factor. Temporary easing of restrictions in June was reported to have ‘helped with reducing AN cognitions and improving mood’ for many patients; although, ‘this only made lockdown 2.0 worse’.
Table 4.
Reasons for AN and atypical AN onset and engagement with clinical services in 2020
| Typical/atypical AN patients 2020 (%) | |
|---|---|
| n = 133 | |
| Isolation and loneliness | 32.3 |
| Change of routine and lack of motivation | 25.6 |
| Boredom/minimal distraction from anorexic thoughts | 23.3 |
| Cessation of community sport | 21.1 |
| Reduced food availability | 3.0 |
Discussion
This study shows that in 2020, compared to the previous 3 years, there was a 63% increase in the presentation of adolescents with EDs to a specialist paediatric ED service. This corresponds to a series of COVID‐19‐related events in Melbourne, Australia. During the initial months of the year, vast media coverage of the evolving global situation led to a sense of uncertainty and anxiety among many Australians 4 , 5 ; many people avoided going out, including for health care, which may explain the decrease in new presentations with AN and atypical AN between February and April. However, this was offset by a dramatic increase in the number of presentations in the second half of the year following the implementation of stringent COVID‐19 restrictions, which were considered relevant in 40.4% of adolescents in 2020.
To date, Australia has managed to avoid high rates of mortality from COVID‐19 due to the imposition of border closures and quarantine, and intense social restrictions. Indeed, Melbourne's COVID‐19 restrictions in 2020 were among the longest lasting and most intense in any population. The impact of social restrictions, including school closures, on young people is evident in this study, as more than one‐third of these adolescents reported isolation and loneliness, and almost a quarter reported boredom. This is consistent with the longstanding recognition that isolation, loneliness and boredom are triggers for disordered eating behaviours in the general population. 10 , 11 , 12 , 13 Many individuals who develop EDs have inherently rigid thought processes in relation to food and/or exercise, 14 , 15 , 16 which may also explain why abrupt changes to normal routines as a result of COVID‐19 restrictions may have been so challenging; over a quarter of these patients suggested that changes to normal routines contributed to the onset of an ED. In addition to food insecurity, frequent media reports about dieting (e.g. how to ‘avoid the bulge during lockdown’) may also have contributed to weight loss, which is a known trigger to restrictive EDs. 12 , 17 , 18 , 19 While the decline in new cases from September may reflect the easing of restrictions and an anticipated return to previous routines, the reduction in cases remained modest by the end of 2020.
A recent report by the Australian Institute of Health and Welfare revealed that the increase in ED behaviours during the pandemic was disproportionate to the increase in other mental health disorders. While the Butterfly Foundation, Australia's leading support organisation for individuals with EDs and body image issues, recorded a 57% increase in calls to its helpline, telephone helplines for general mental health conditions and distress, such as Lifeline, Kids Helpline and Beyond Blue, only recorded an increase in calls of approximately 15–20%. 20 This highlights the need for increased monitoring of EDs in addition to the more common focus on emotional distress, anxiety and depression.
Despite an increase in AN cases during 2020, there was no significant change in the apparent severity of cases when they did present (P > 0.05). This may indicate that COVID‐19 restrictions tended to trigger the onset of behaviours rather than exacerbate symptoms in those with pre‐existing ED behaviours. The high proportion of 2020 patients (40.4%) who were reported to develop AN or atypical AN during lockdown, as opposed to those who relapsed (12.8%), further supports this notion, as does the lesser proportion of extremely malnourished AN patients in 2020 compared to previous years. It may also be that ED behaviours were identified earlier due to the opportunities to observe individual behaviours when family members are locked down together.
Despite reports of increased distress, anxiety and depression during the pandemic, 13 there was no significant increase in the prevalence of comorbidities, self‐harm or suicidal ideation, or prescription of psychoactive medication in 2020 compared to earlier years. The influx of patients with no apparent predisposing mental health or medical conditions in 2020 suggests that many of these patients may have not otherwise developed an ED given a normal year. This points to wider opportunities around the prevention of EDs.
This study contributes to an emerging body of literature detailing the impact of the COVID‐19 pandemic on adolescents with mental health conditions, including restrictive EDs. The validity of these findings is enhanced by the longstanding use of a standardised approach to triage and patient assessment within the RCH ED service, which offers clinical care to a specific geographical region in Melbourne. However, reports of when and why ED behaviours developed relied on documentation within the medical record and these data may therefore not fully represent the implications of the pandemic. Chart notes regarding the triggers for ED behaviours in 2020 could also have reflected the expectations or biases of the clinicians. Nevertheless, prominent themes were able to be identified from the medical records, which bring attention to the particular challenges faced by adolescents during the COVID‐19 pandemic.
Conclusion
This study shows a striking increase in the presentation of adolescents with new cases of AN to a specialist ED service during the pandemic, with the timing closely mirroring the extent of social restrictions. Beyond the immediate need for patient care around COVID‐19 itself, it highlights the wider impacts of the pandemic on mental disorders in a cohort that might not otherwise have developed AN. Understanding the recovery of the 2020 cohort will be important, as it will have occurred in the context of further episodic lockdowns in Melbourne. So too, as the pandemic rolls on, it will be important to understand the impact of repeated social and educational disruptions on EDs in young people.
Acknowledgements
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: G. Springall is in receipt of the Australian Commonwealth Government Research Training Programme Scholarship (RTPS). The Heart Research Group receives financial support in part from, Royal Children's Hospital Foundation, Big W and the Victorian Government's Operational Infrastructure Support Programme to the Murdoch Children's Research Institute. The authors would also like to acknowledge the assistance of Stephanie Campbell and Claire May for their data entry and retrieval.
Conflict of interest: None declared.
References
- 1. World Health Organisation . Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019‐nCoV). 2020. Available from: www.who.int/news‐room/detail/30‐01‐2020‐statement‐on‐the‐second‐meeting‐of‐theinternational‐healthregulations‐(2005)‐emergency‐committeeregarding‐the‐outbreak‐ofnovel‐coronavirus‐(2019‐ncov) [accessed 30 October 2020].
- 2. Victorian State Government Department of Health and Human Services . Victoria's COVID‐19 restrictions. 2020. Available from: https://www.dhhs.vic.gov.au/victorias-restriction-levels-covid-19 [accessed 12 January 2021].
- 3. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID‐19 epidemic declaration on psychological consequences: A study on active weibo users. Int. J. Environ. Res. Public Health 2020; 17: 2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Torales J, O'Higgins M, Castaldelli‐Maia JM, Ventriglio A. The outbreak of COVID‐19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020; 16: 2076. [DOI] [PubMed] [Google Scholar]
- 5. Phillipou A, Meyer D, Neill E. Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Ed. Disord. 2020; 53: 1158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patton GC, Sawyer SM, Santelli JS et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 2016; 387: 2423–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pfefferbaum B, North C. Mental health and the COVID‐19 pandemic. N. Engl. J. Med. 2020; 383: 510. [DOI] [PubMed] [Google Scholar]
- 8. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Washington, DC; 2013. [Google Scholar]
- 9. Sawyer S, Whitelaw M, Le Grange D, Yeo M, Hughes E. Physical and psychological morbidity in adolescents with atypical anorexia nervosa. Pediatrics 2016; 137: e20154080. [DOI] [PubMed] [Google Scholar]
- 10. Bruce B, Agras WS. Binge eating in females: A population‐based investigation. Int. J. Ed. Disord. 1992; 12: 365–73. [Google Scholar]
- 11. Tiller JM, Sloane G, Schmidt U, Troop N, Power M, Treasure JL. Social support in patients with anorexia nervosa and bulimia nervosa. Int. J. Ed. Disord. 1997; 21: 31–8. [DOI] [PubMed] [Google Scholar]
- 12. Touyz S, Lacey H, Hay P. Eating disorders in the time of COVID‐19. J. Eat. Disord. 2020; 8: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Druss B. Addressing the COVID‐19 pandemic in populations with serious mental illness. JAMA Psychiat. 2020; 77: 891–2. [DOI] [PubMed] [Google Scholar]
- 14. Fairweather‐Schmidt AK, Wade TD. Common genetic architecture and environmental risk factors underpin the anxietydisordered eating relationship: Findings from an adolescent twin cohort. Int. J. Ed. Disord. 2020; 51: 52–60. [DOI] [PubMed] [Google Scholar]
- 15. Schebendach JE, Mayer LE, Devlin MJ et al. Food choice and diet variety in weight‐restored patients with anorexia nervosa. J. Am. Diet. Assoc. 2011; 111: 732–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abbate‐Daga G, Amianto F, Delsedime N, De‐Bacco C, Fassino S. Resistance to treatment and change in anorexia nervosa: A clinical overview. BMC Psychiatry 2013; 13: 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Becker CB, Middlemass K, Taylor B, Johnson C, Gomez F. Food insecurity and eating disorder pathology. Int. J. Ed. Disord. 2017; 50: 1031–40. [DOI] [PubMed] [Google Scholar]
- 18. Greenspan R. Fitness content is everywhere during the coronavirus pandemic. Experts say it's putting those with a history of eating disorders at risk. Insider. 2020; 26: 212–27. [Google Scholar]
- 19. Warren CS. How to curb emotional eating during the COVID‐19 pandemic. Psychol. Today 2020; 36: 191. [Google Scholar]
- 20. Australian Institute of Health and Welfare . COVID‐19: looking back on health in 2020. 2021. Available from: https://www.aihw.gov.au/reports‐data/australias‐health‐performance/covid‐19‐and‐looking‐back‐on‐health‐in‐2020#Increased%20use%20of%20mental%20health%20services%20during%20COVID‐19%20pandemic [accessed 30 March 2021].


