Abstract
Objective
This study aimed to elucidate the experiences of public health nurses (PHNs) in Japan during the first wave of COVID‐19.
Design and sample
Twelve PHNs in charge of responding to COVID‐19 in X‐city within Tokyo metropolis in Japan participated in this case study.
Measurements
Data were collected through self‐administered questionnaires and semi‐structured interviews on PHNs’ experiences from January 2020 to May 2020.
Results
Initially, only infectious disease control division (IDCD) PHNs experienced confusion due to the rapidly increased workload. Managerial PHNs attempted to explain the need for a dispatch system for the IDCD, using available statistical data from other managerial members, within one's maximum understanding of this unprecedented situation. Without having a clear and forward‐looking understanding regarding the purpose and reasons for dispatching, some dispatched PHNs had concerns and frustrations; they did not view the COVID‐19 pandemic as a disaster. In the never‐ending, exhausting work, PHNs managed to modify the provision of conventional services to residents.
Conclusions
Despite experiencing confusion, PHNs worked to continuously provide community services, re‐considering the meaning of public health nursing. Prioritizing the work and shifting tasks to other professionals at an early stage of the pandemic may prevent organizational dysfunction.
Keywords: community health services, disaster, leadership, management, organization and administration, pandemic, public health system, task shift
1. INTRODUCTION
Public health nurses (PHNs) working in public health centers (PHCs) have been playing a critical role in combating the coronavirus disease 2019 (COVID‐19) pandemic (Yoshioka‐Maeda et al., 2020). In Japan, PHCs are important centers for controlling infectious diseases, including COVID‐19, at the prefectural, core city, and ward levels. They are responsible for conducting active epidemiological surveys such as contact tracing, coordinating hospitalization of COVID‐19 patients, monitoring the health of contacts of COVID‐19 patients, and providing consultation to local residents (Yoshioka‐Maeda et al., 2020). Nonetheless, due to the promotion of national administrative reforms in public health, the number of PHCs decreased by approximately 40% compared to the 1990s (Japanese Association of Public Health Center Directors, 2021). Consequently, the number of PHNs who can respond to infectious diseases has also decreased. In short, PHCs were severely understaffed in the first wave of COVID‐19 in March–April 2020.
The major challenges in the ongoing pandemic have been practicing infection control and simultaneously providing face‐to‐face services for community members (Frawley et al., 2020). Previous studies illustrated how to conduct epidemiological surveys (Furuse, Ko, et al., 2020), respond to infection clusters in the community (Furuse, Sando, et al., 2020), triage priority to home visits (Tai et al., 2020), and identify community health needs (Sands et al., 2020). Front‐line PHNs experienced the fear of contracting COVID‐19 in their daily practices (Labrague & De Los Santos, 2021). Furthermore, PHNs faced difficulties in providing health services related to maternal and child health as well as mental health during the COVID‐19 pandemic (Honda et al., 2020; Kanzaki & Iijima, 2020).
The American Public Health Association (APHA), Public Health Nursing Section, states that “PHNs are in a position to provide leadership through public policy reform efforts, community‐building, and system‐level change” (APHA, Public Health Nursing Section, 2013). PHNs are also required to “demonstrate capacity to determine community public health emergency preparedness needs and organize response activities” (Quad Council Coalition of Public Health Nursing Organizations, 2018). However, to the best of our knowledge, no study has illustrated the kind of leadership and management capacity required in PHNs during the early stages of the COVID‐19 pandemic—a time characterized by uncertainties regarding the health hazards or the prospects for convergence. In such a disaster with uncertain prospects, it is necessary to clarify the kind of disruptions that occurred, the time at which they occurred, and the kind of leadership and management that were required.
To promote community health while responding to outbreaks of COVID‐19 and transition toward a new normal (Jamaludin et al., 2020), the disruptions experienced by managerial PHNs need to be clarified and utilized for developing better health service systems to tackle the next pandemic. Therefore, this study aims to elucidate PHNs’ initial experience in this COVID‐19 pandemic and how they responded to them while working at PHCs during the first wave of COVID‐19 in the unprecedented confusion.
2. METHODS
2.1. The case study research method
We employed the case study research method (Herbig et al., 2001) to focus on the experiences of PHNs in the PHC located at X‐city. The COVID‐19 pandemic spread quickly throughout the world in the absence of vaccines or any established effective treatments. Therefore, PHNs in each municipality had no time to prepare for combating the pandemic and could only respond based on their prior experiences and knowledge. Therefore, we focused on the experiences of PHNs to capture what kinds of confusion they experienced and how they responded to them during the first wave of COVID‐19. This case study was conducted using Yin's (2017) methodology to obtain a robust result based on various data including documents, interviews, questionnaires, and participant observations.
2.2. Setting, study participants, and data collection
The study setting was a ward‐level PHC in X‐city, which has a population of approximately 210,000. The PHC is a training institute for students enrolled in a public health nursing master's program at the university to which the authors belong. The present authors had been regularly cooperating with this PHC. The PHC in X‐city has four divisions: infectious disease control division (IDCD), health promotion division (HPD), environmental hygiene division (EHD), and health service centers (HSCs) for providing residents’ services (Figure 1). The PHNs worked in the HPD, IDCD, and HSCs, and their total number was 27 in March 2020. Among them, six PHNs were working at IDCD, four of whom were engaged in COVID‐19‐related operations. There were four managerial PHNs, one of whom was the director of PHNs who coordinates the overall PHN. Managerial PHNs work as section chiefs and also perform administrative duties such as organizing staff and coordinating with other departments. The director of PHNs is responsible for supervising all PHNs, including managerial PHNs and staff PHNs, while also working with the frontline staff. Owing to the rapidly increasing workload of the IDCD, nine PHNs were dispatched to the IDCD from the HSCs and HPD between April and May 2020. The period roughly corresponds to the first “state of emergency” that started on April 7 and was lifted on May 25, 2020 (Prime Minister of Japan & His Cabinet, 2020).
FIGURE 1.
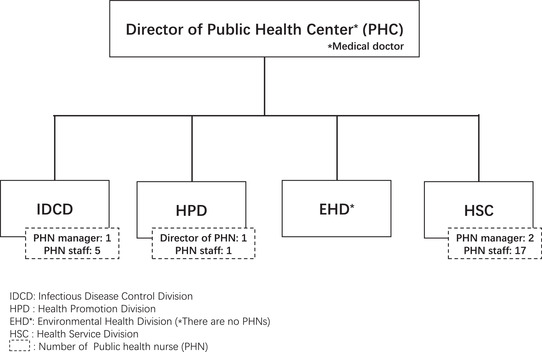
PHC's organizational chart in X‐ city (March 2020)
To obtain robust results, Yin recommended collecting data from various sources to increase the reliability and validity. First, we conducted a self‐administered questionnaire survey for the PHNs to identify the practices and difficulties they faced from January to May 2020. The self‐administered questionnaire included items on weekly segments of COVID‐19‐related events in Japan and X‐city and the PHNs’ practices (e.g., telephone consultation, arranging for testing, hospitalization coordination, transportation, reporting, and statistics) to collect accurate data. To avoid any response bias that may be introduced by obtaining respondents through their supervisors, we asked participants to return their responses directly to the author via e‐mail. This self‐administered questionnaire survey was conducted in July 2020, and nine PHNs responded to it.
Second, the first and second authors conducted a semi‐structured interview with the PHNs from all three divisions (HPD, HSC, IDCD) from October 2020 to January 2021. We asked the PHNs about their practices and the difficulties they faced in chronological order from January to the end of May in 2020. The interviews were recorded with the consent of all participants, and verbatim transcripts were made.
2.3. Data analysis
Referring to Yin's case study method, we chose a time‐series analysis based on the chronological time axis (Yin, 2017). First, we analyzed data from the completed questionnaires in chronological order and compared their commonalities and differences. Second, we analyzed the transcripts of the interviews and divided them into sections based on their meanings. We summarized each section as a code and sorted it chronologically based on the research question, “What kinds of confusion did PHNs experience?” and “How did they respond to them?” According to its commonality, we named the subcategories and categories, reflecting the classification.
We developed a schematic model to reflect the process. To ensure the validity of the results, we asked the opinions of the participants and experts in qualitative research methods. Based on their opinions, we revised the names of the categories and the schematic model.
2.4. Ethical considerations
The Institutional Review Board of the university to which the first author belongs [#2020138NI] approved this study protocol based on the Declaration of Helsinki. Before starting the study, a letter was sent to managerial PHNs in three divisions and the director of the PHC of X‐city regarding the entire study, and their permission was obtained. Additionally, we prepared other letters for all PHNs to explain the purpose, methods, and ethical considerations of this research, both orally and in writing. Before conducting the study, we obtained all participants’ consent through a consent form.
3. RESULTS
3.1. Demographics of the participants
Nine of the 12 participants responded to the questionnaire survey, and three participated in the semi‐structured interview survey (Table 1). All participants were female, and the range of years of experience as PHNs was 1–32 years. All three interviewees were managerial PHNs.
TABLE 1.
Characteristics of the study participants N = 12
| Total Number/(range) | Respondents of the questionnaire N = 9 (ID1‐9) | Respondents of the interviews N = 3 (ID10‐12) | ||
|---|---|---|---|---|
| Number of years of experience as PHN | Years (min‐max) | (1‐32) | (1‐32) | (24‐30) |
| Sex | Female | 12 | 9 | 3 |
| Work place | IDCD | 3 | 2 | 1 |
| HPD | 2 | 1 | 1 | |
| HSC | 7 | 6 | 1 | |
|
Position (in 2020) |
Managerial level | 4 | 1 | 3 |
| Assistant managerial level | 2 | 2 | 0 | |
| Staff | 6 | 6 | 0 | |
| Experience at IDCD | Yes | 5 | 3 | 2 |
| No | 7 | 6 | 1 |
Abbreviation.;Infectious.
Abbreviations: IDCD, Infectious Disease Control Division; HPD, Health Promotion Division; HSC, Health Service Center.
3.2. Confusion experienced by PHNs during the first COVID‐19 wave in Japan
During the first wave of the COVID‐19 pandemic, the PHNs experienced six kinds of confusion. Quotes from the self‐administered questionnaire data and the interview data are enclosed within quotation marks in italics. Questionnaire data is prefixed with “Q” (Q: ID1, HSC), and interview data is prefixed with “I” (I: ID10, IDCD).
3.2.1. Confusion due to the increasing workload of the IDCD
When COVID‐19 spread rapidly in Wuhan and the Chinese government sealed off the city, chartered planes were arranged to evacuate Japanese citizens living in Wuhan. Five chartered planes from Wuhan returned to Japan between January 29, 2020 and February 17, 2020. Additionally, after a series of cases on a cruise ship—the Diamond Princess—in February, the infection spread throughout Japan. Under the uncertain national policy for COVID‐19, the IDCD PHNs underwent a conflict resulting from anxiety and a strong sense of mission to tackle this unknown public health threat. They had no choice but to prepare themselves and proceed with their work.
“It was one month of battle between having a sense of mission that we must perform duties as a PHN and the fear of working under the strain of wearing full PPE (personal protective equipment)to deal with an unknown infection disease. (I:ID10, IDCD)”
Many community residents called the IDCD since early February 2020 due to lacking correct information and understanding of COVID‐19 and a fear of the unknown. PHNs “felt the growing anxiety of the residents in the city. (Q: ID8, IDCD),” and then “Consultation on how to respond to a patient outbreak at their company or facility (Q: ID8, IDCD)” gradually began to increase. After the media reported a shortage of surgical masks and PCR testing kits, the IDCD “received many complaints that the PHC should stop people from holding concerts at the Tokyo Dome or jogging in the city and request a PCR center. Responding to them took up a lot of our time. (Q:ID9, IDCD).” The staff of medical institutions located in X‐city also experienced anxiety, and their consultations with the IDCD increased.
“The doctors must have been quite worried about the examination and tests. They were yelling at us too, so I guess they were human beings too, and I guess they were worried because of COVID‐19.” (I: ID10, IDCD)
Furthermore, there were reporting requirements and frequently changing national guidelines during the COVID‐19 outbreak from the end of January to February 2020. PHNs were required daily to catch up with the updated guidelines and report details of COVID‐19 cases to the national and metropolitan governments.
“We conducted a survey of the people who were transported to K hospital, contacted the Infection Control Office to confirm their medical conditions and negative results, and reported the results to the Infectious Disease Information Network system every day. It was difficult for the hospital staff to make time to interview patients as they were busy” (Q: ID9, IDCD).
3.2.2. Front‐line PHNs in IDCD had to fight a lonely struggle
IDCD PHNs had to fight a lonely struggle since mid‐February and continued until the HSCs’ and HPDs’ PHNs were dispatched, and the entire X‐city government supported the IDCD starting in April 2020.
The IDCD PHNs did not have sufficient time to send out an SOS on their own at the end of February and early March 2020. At the end of the fiscal year, all departments were busy.
Due to departmentalism, other departments were completely unaware of how busy the IDCD PHNs were. In an unprecedented situation, with no criteria for issuing an SOS, the IDCD was struggling only within the department.
“At the beginning of March…, I could see how the situation of IDCD worsened because I was right next to the section. However, the PHNs in the IDCD could not have time to explain their situation. With the distance between the south and north buildings, other departments’ members did not know what was going on.” (I: ID12, HPD)
Due to the excessive workload of the IDCD, even the managerial PHN in the IDCD had to be engaged on the front line. Their management was dysfunctional in terms of coordinating within departments or external affairs. Only the IDCD was in a state of emergency.
“The phone in the IDCD started ringing off the hook the entire day. Finally, even the chief PHN began responding to the telephone calls. For example, coordinating with hospitals and medical associations is supposed to be the duty of managerial PHN, but she could not even do that anymore.” (I: ID12, HPD)
3.2.3. Difficulties in sharing the policy of dispatching PHNs for the IDCD experienced by the director of the PHNs
The director of the PHNs was the only individual to understand how busy the IDCD was through supporting its staff‐level practices from February end to March 2020. She enabled other managerial members of the PHC to understand the need for a cross‐organizational dispatch system for the IDCD by using statistical data and frequent reporting of the IDCD status.
“I would send out the numbers (of telephone consultation or infected people), and then, I appealed directly to other managerial PHNs and other section chiefs, “The IDCD is in a troublesome situation, which is not ordinary.” I tried to bridge the gap between managers and IDCD.” (I: ID12, HPD)
The personnel rotation and new staff assignments were conducted on April 1, when the fiscal year started in Japan. The PHC did not have a system for flexible staffing to cover the manpower shortage internally. It was difficult to obtain consent to dispatch PHNs from other departments to the IDCD. From the beginning of April 2020, to emphasize that COVID‐19 had become a pandemic and that the IDCD PHNs were overburdened with workload, the PHC director and the director of the PHNs intentionally used the words “disaster” and “national crisis.”
“Preparing for personnel rotation was quite a challenge, and it was not easy to get all the managers to say yes to sending staff to the IDCD. I asked the PHC director to tell everyone about it. He also gave everyone the orientation that this was a disaster and a national crisis. We needed to work together with the higher management members to find out where, when, and what we should say.” (I: ID12, HPD).
With the rapid spread of COVID‐19, the usual way of personnel transfer and staffing could not keep up with COVID‐19 responding. A few days before the declaration of a state of emergency on April 7, the PHC director decided to increase the IDCD staff. To respond quickly, managerial PHNs selected and dispatched PHNs from HSCs without coordinating with the managers of the dispatchers. Therefore, in the hurriedly assembled team of dispatched PHNs, a gap was observed between those PHNs who recognized that they were sent to the IDCD as a disaster response and those who did not.
PHN managers who had experience in disaster dispatch for natural disasters or had worked at IDCD recognized COVID‐19 as a “disaster,” and could forecast its course based on their rich practical knowledge and experience.
The director of PHNs needed to follow up with the dispatched PHNs to support them in adjusting to their work at the IDCD while also managing the entire support team to ensure that the IDCD operated smoothly.
“I think this infection was a disaster, but I think there was a gap between those who thought it was a disaster and those who did not think so. Therefore, when we first set up the emergency system, I think there was a feeling of discomfort among the staff, ‘why do we have to go (to the front line)’ or ‘why did they go?’” (I: ID12, HPD)
3.2.4. Anxiety, frustration, and extreme fatigue among PHNs
As support team members, the dispatched PHNs worked frantically at the IDCD in the face of physical and mental challenges since April 6.
“We were dispatched to a place where the work content and division of roles had not been decided. Even our seats were not determined” (Q: ID3, HSC).
“I was providing telephone counseling to residents who were suspected to have COVID‐19, but I was afraid of the possibility of (them) sudden acute deterioration.” (Q: ID1, HSC)
However, some of them had concerns and frustrations that accumulated over time. Managers dispatched PHNs to the ICDC without fore‐visioned explanation on the purpose of the dispatch. Some dispatched PHNs did not consider the pandemic a disaster. They were anxious about the lack of work guidance or the uncertain duration of the dispatch. The PHNs’ frustration increased when they felt inequity in the workload and lower leave usage compared to the other departments’ PHNs at the end of April 2020.
“Some PHNs (in other divisions) were working at home due to attendance adjustments, which I thought was unfair.” (Q: ID4, HSC)
“Some of the dispatched PHNs experienced intense frustration. Ms. N, who was working as a dispatched nurse, said, ‘there is a lot of dissatisfaction among the young staff’.” (I: ID11, HSC)
Even after the dispatched PHNs’ support started, PHNs of the IDCD were exhausted due to the ever‐increasing telephone consultations and number of COVID‐19 patients. With over 100 calls received per day in April, the IDCD ran out of phone lines. The excessive workload resulted in staff shortages, thereby increasing the time for conducting active epidemiological surveys and coordinating hospitalization and accommodation.
“This work had never been completed. I thought how long I could keep working without burnout was influenced by my initial determination. Combating COVID‐19 had just begun, but I was so busy that I felt I was going to collapse. I kept telling the staff that this status would continue for a long time and that they should work without burnout.” (I: ID10, IDCD)
3.2.5. Identifying the necessity of changing traditional way of practice
COVID‐19 also caused a dramatic change in the conventional PHNs’ practice other than COVID‐19 related services. As the infection spread, from March 2020 onward, the HSC staff who dealt with non‐COVID‐19 public health services—such as child wellness checkups, group activities for new parents, and health education at mothers' classes—began to fear the risk of infection while providing face‐to‐face services. Community residents also became concerned about it. While both the director of PHC and the managerial PHN believed that home visits were essential, some frontline staff voiced concerns about continuing home visits as they may not be safe during the pandemic. The PHNs worked while experiencing anxiety until home visit services were stopped.
Eventually, the director of the PHC decided to stop all face‐to‐face services to avoid infection, including neonatal home visits and child health checkups on April 7, 2020. In addition to losing the opportunity to see residents directly, the number of PHNs who followed up with residents was also reduced because of dispatch support to the IDCD. The PHNs were very concerned about the possibility of missing the opportunity of preventive interventions, for example, mothers and children who were at risk of abuse or domestic violence. By not providing regular services, there was a possibility that health of the residents was not protected as usual.
“It has been a week since we stopped the regular checkups and visits, and we have not heard anything from the residents at all. Even when we called some residents I was following up, they would say, ‘I am fine. My baby is also fine’ (but I could hardly believe that everything was fine). I thought this may become big issues later.” (I: ID11, HSC)
Before the pandemic, PHNs supported only residents who lived in the areas of HSCs or PHCs. However, during the COVID‐19 pandemic, PHNs were required to provide support to all cases who stayed in the community, even if they were not residents of their municipality. Thus, PHNs needed to change the concept of their target population, which sometimes caused confusion. This also required the PHNs to communicate with PHCs in other cities, causing further increase in their workload since the end of March 2020.
3.2.6. Rethinking the meaning of public health nursing
No longer being able to provide services in the previous manner, PHNs began to review their work and allocating it to other staff members. They tried to develop a new way of performing their work in the COVID‐19 situation. In addition to changing the service delivery to include infection control, the PHNs were required to maintain regular health services and infection control with limited human resources. The first step of the reform was to change the care system so that fewer staff were sharing the tasks. Specifically, the traditional care system in which each PHN was responsible for the subdivided area was changed to a team‐based care system in which several PHNs supported large areas and community residents.
“During this period, the district management system collapsed. (omission) We divided the district into two areas across the street. Then, we worked together to contact and visit the target people. By doing things in this way, the staff that was left behind became empowered. We were able to do this without overthinking the fact that we were a small group.” (I: ID11, HSC)
The second step of the reform was task shifting. The PHNs constantly thought about their roles and work as PHNs, what they should do themselves, and what they could entrust to others. For example, epidemiological surveys, which used to be handled by only full‐time PHNs, were divided according to content, and typical cases that could be handled routinely were allocated to part‐time nurses.
“Surveys are conducted under the Infectious Diseases Control Law, so I wondered if it was okay for supporters to conduct such surveys. (omission) We were not familiar with the survey at first, so we could not leave it to the dispatched PHNs or part‐time nurses. Gradually, we tried to steer the process toward letting others do the work. We started with typical cases that they (part‐time nurses) could hear through a specific pattern.” (I: ID10, IDCD).
3.3. Correlation between confusion experienced by PHNs and their responses during the first wave of the COVID‐19 pandemic in Japan
The six types of confusion experienced by PHNs in X‐city and their responses during the first wave of the COVID‐19 pandemic are shown in Figure 2. The PHNs experienced confusion owing to the rapidly increasing workload of the IDCD section. However, staff members from other departments could not recognize or understand the chaotic condition of the IDCD. Thus, front‐line IDCD PHNs had to fight a lonely battle for some time. Because of the overlap with the end of the fiscal year, the director and managers of the PHC could not agree with the PHN director's idea to dispatch PHNs to the IDCD. The director of PHNs used statistical data and frequent reports of the IDCD status, and the director of PHC finally understood the pandemic situation and decided to dispatch the PHNs to the IDCD. However, because of the lack of coordination and work guidance for PHNs who were dispatched to the IDCD, there was a gap between PHNs who could recognize the disaster response and those who could not. This gap caused increasing anxiety, frustration, and extreme fatigue among the PHNs.
FIGURE 2.
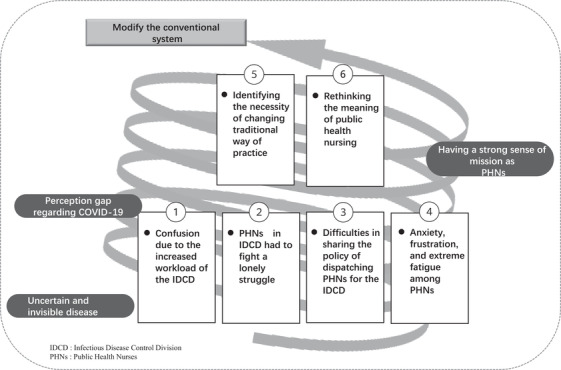
Confusion experienced by PHNs During the First COVID‐19 Wave in Japan
The existing systems collapsed because of the rapidly increasing workload. In this extreme situation, the PHNs reconsidered the meaning of public health nursing. To provide effective face‐to‐face public health services for community residents, they modified the existing organizations with limited resources and infection control measures to respond to COVID‐19. They also shifted some of their tasks to the PHNs dispatched to the IDCD, part‐time nurses, and administrative staff to develop a sustainable work system. This confusion occurred because COVID‐19 was initially an invisible and uncertain disease. Additionally, the gap in the perception regarding the COVID‐19 pandemic among members of the PHC added to the confusion. It was a sense of mission that drove PHNs to respond to the confusion and provide public health services to the community.
4. DISCUSSION
In this study, we analyzed the kinds of confusion experienced by PHNs working in a PHC and how PHNs responded to them. This study has three main findings.
First, during the first wave of COVID‐19, PHNs faced ever‐increasing and excessive workload and staff shortages. In Japan, the national government coordinates and sends PHNs to disaster‐affected local governments due to staff shortages (Ministry of Internal Affairs & Communications, 2021). However, as the pandemic has spread throughout Japan, local governments were unable to dispatch PHNs to other communities (Yoshioka‐Maeda et al., 2020). Therefore, PHNs should develop a dispatch system within the same organization to respond to the COVID‐19 pandemic. Additionally, PHNs should prioritize their work and shift tasks to other professionals in the early stage of a pandemic to prevent organizational dysfunction. The X‐city is exceptional in terms of the municipality. A prefectural‐level health center typically supports multiple jurisdictional municipalities and delivers various kinds of support (Organisation for Economic Co‐operation and Development, 2019). However, X‐city health centers have dual functions: prefecture and municipality. In other words, the X‐city has both the PHC that functions for prefectures and HSCs for the municipality. Additionally, the PHC usually supervises and provides support for the HSCs. However, during the pandemic, the HSCs supported the PHC. Thus, this irregularity would negatively impact the development of a support system within the municipality. Our results are applicable to public health nursing regarding COVID‐19 in large cities.
Second, the PHNs faced difficulties in reaching a consensus regarding the dispatch system of PHNs to the IDCD and building support teams of the dispatched staff who did or did not recognize COVID‐19 as a disaster. Only the managerial PHNs who had experience in disaster dispatch or who had worked at the IDCD recognized the COVID‐19 pandemic as a disaster. The COVID‐19 pandemic was invisible and quite different from the ordinary definition of disasters (World Health Organization, 2019). At first, it was difficult to recognize the disastrous impact of the COVID‐19 pandemic, unlike for other disasters such as earthquakes. Drills for disasters such as earthquakes and floods are routinely conducted in the entire municipality. However, for infectious diseases, IDCD in PHC have been the only ones to address the situation. The confusion was mainly localized in IDCD and had not been communicated to the other departments. Therefore, it took a long period for everyone to realize that the pandemic is a type of disaster. Additionally, the local governments of Japan face the issue of departmentalism—indifference to other departments and only being interested in one's own department (Honda, 1994). In Japanese culture, people feel ashamed of asking for help from others and believe that they must solve problems themselves; hence, this may have contributed to the difficulty in sharing concerns with others (Yoshioka‐Maeda, 2020a). When a disaster occurs, the director of the PHN should set organizational goals early and share them with their staff to prevent confusion and continue providing health services (Miyazaki, 2013). Managerial PHNs who realized that the pandemic was a disaster should bridge the perception gap among other all staff members to unite against COVID‐19. Additionally, novice and mid‐level PHNs should develop their leadership and management skills (Quad Council Coalition of Public Health Nursing Organizations, 2018) to prepare for emergencies by experiencing disaster dispatch in ordinary times.
Third, with a vital sense of mission, the PHNs revised their healthcare services to cater to residents with fewer staff during the COVID‐19 pandemic. PHNs should improve the health outcomes of all populations and apply interventions to all individuals, families, communities, and systems (American Public Health Association, 2013). PHNs have also planned needs‐oriented health services to enhance health equity (Yoshioka‐Maeda, 2020b). Each local government developed a business continuity plan (BCP) after the H1N1 pandemic in 2008 (Office for Pandemic Influenza & New Infection Diseases Preparedness & Response, Cabinet Secretariat, 2017) that was not used adequately in X‐city. Therefore, PHNs should revise the plan appropriately and share it within the organization (Cabinet Office, 2014).
4.1. Limitations and implications
This study has two limitations. First, it was difficult to secure interview time due to the COVID‐19 situation, and there was a time lag of about 3–6 months between the timing of the questionnaire survey and the interview survey. As the prevalence of COVID‐19 varied with the time of the year, this may have affected the data. Second, the study was conducted at only one city center, and thus generalization to other regions should be performed carefully.
Despite these limitations, this is the first study to identify the confusion experienced by PHNs working at a PHC in Japan during the early stages of the COVID‐19 outbreak. PHNs confronted confusions in the organization in the early stages of the pandemic and struggled to provide services to residents due to limited resources flexibly. The disruption of the first wave of COVID‐19 forced PHC to change its traditional rigid organization and approval process for decision making. The managerial PHNs should promote leadership and management roles in organizations and adjust daily routine accordingly based on changing needs and environment (Quad Council Coalition of Public Health Nursing Organizations, 2018). Additionally, task shifting and sharing would contribute to establish a sustainable system in pandemic situations (Centers for Disease Control & Prevention, 2020). Thus, PHNs should find the best approach using the available evidence and show the vision for establishing sustainable healthcare systems accordingly during the initial pandemic. The current findings will help the development of local healthcare systems to prepare for the next global pandemic.
ACKNOWLEDGMENTS
We especially thank the public health nurses who participated in the research. This study was financially supported by the Daiwa Securities Health Foundation in Japan to C.H.
Honda, C. , Sumikawa, Y. , Yoshioka‐Maeda, K. , Iwasaki‐Motegi, R. , & Yamamoto‐ Mitani, N. (2022). Confusions and responses of managerial public health nurses during the COVID‐19 pandemic in Japan. Public Health Nursing, 39, 161–169. 10.1111/phn.13011
DATA AVAILABILITY STATEMENT
The data of this study are not publicly available due to strictly the privacy of research participants.
REFERENCES
- American Public Health Association , Public Health Nursing Section (2013). The definition and practice of public health nursing: A statement of the public health nursing section. Washington, DC: American Public Health Association. Retrieved from: https://www.apha.org/-/media/Files/PDF/membergroups/PHN/NursingDefinition.ashx [Google Scholar]
- Cabinet Office , Government of Japan. (2014). Business Continuity Guidelines: Strategies and Responses for Surviving Critical Incidents, third edition. Retrieved from: http://www.bousai.go.jp/kyoiku/kigyou/pdf/guideline03_en.pdf
- Centers for Disease Control and Prevention . (2020). Sharing and shifting tasks to maintain essential healthcare during COVID‐19 in Low Resource, non‐US settings. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/task-sharing.html
- Frawley, T. , Van Gelderen, F. , Somanadhan, S. , Coveney, K. , Phelan, A. , Lynan‐Loane, P. , & De Brún, A. (2020). The impact of COVID‐19 on health systems, mental health and the potential for nursing. Irish Journal of Psychological Medicine,38, 220‐226, 10.1017/ipm.2020.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse, Y. , Ko, Y. K. , Saito, M. , Shobugawa, Y. , Jindai, K. , Saito, T. , Nishiura, H. , Sunagawa, T. , Suzuki, M. , & Oshitani, H. (2020). Epidemiology of COVID‐19 Outbreak in Japan, from January‐March 2020. Japanese Journal of Infectious Diseases, 73(5), 391–393. 10.7883/yoken.JJID.2020.271 [DOI] [PubMed] [Google Scholar]
- Furuse, Y. , Sando, E. , Tsuchiya, N. , Miyahara, R. , Yasuda, I. , Ko, Y. K. , Saito, M. , Morimoto, K. , Imamura, T. , Shobugawa, Y. , Nagata, S. , & Jindai, K. (2020). Clusters of coronavirus disease in communities, Japan, January–April 2020. Emerging Infectious Diseases, 26(9), 2176‐2179. www.cdc.gov/eid 10.3201/eid2609.202272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbig, B. , Büssing, A. , & Ewert, T. (2001). The role of tacit knowledge in the work context of nursing. Journal of Advanced Nursing, 34(5), 687–695. 10.1046/j.1365-2648.2001.01798.x [DOI] [PubMed] [Google Scholar]
- Honda, C. , Yoshioka‐Maeda, K. , & Iwasaki‐Motegi, R. (2020). Child abuse and neglect prevention by public health nurses during the COVID‐19 pandemic in Japan. Journal of Advanced Nursing, 76(11), 2792–2793. 10.1111/jan.14526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda, H. (1994). Structure of Modern Public Administration (Gendai Gyousei no Kouzou). Tokyo: Keiso‐syobo. pp. P76‐77. [Google Scholar]
- Jamaludin, S. , Azmir, N. A. , Mohamad Ayob, A. F. , & Zainal, N. (2020). COVID‐19 exit strategy: Transitioning towards a new normal. Annals of Medicine and Surgery, 59, 165–170. 10.1016/j.amsu.2020.09.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Japanese Association of Public Health Center Directors . (2021). Hokensho setti suu/suii. Retrieved from http://www.phcd.jp/03/HCsuii/
- Kanzaki, Y. , & Iijima, T. (2020). Report on the activities of public health nurses in public health centers to combat COVID‐19, Part 3: Activities of Public Health Nurses in other than Infectious Diseases Control Division. Japanese Journal of Public Health Nursing, 9(3), 197–202. [Google Scholar]
- Labrague, L. J. , & De Los Santos, J. A. A. (2021). Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nursing, 38(3), 382–389. 10.1111/phn.12841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Internal Affairs and Communications . (2021). Operation Manual for the Dispatch System for Emergency Response Staff, Third edition. Retrieved from https://www.pref.miyagi.jp/uploaded/attachment/847025.pdf
- Miyazaki, M. (2013). Public health nursing activities of municipal public health nurses during major disasters. Journal of the National Institute of Public Health, 62(4), 414–420. [Google Scholar]
- Organisation for Economic Co‐operation and Development (OECD) . (2019). OECD Reviews of Public Health: Japan: A Healthier Tomorrow. 10.1787/9789264311602-en. [DOI]
- Office for Pandemic Influenza and New Infection Diseases Preparedness and Response, Cabinet Secretariat . (2017). National Action Plan for Pandemic Influenza and New Infectious Diseases. https://www.cas.go.jp/jp/seisaku/ful/keikaku.html
- Prime Minister of Japan and His Cabinet . (2020). Speeches and Statements by the Prime Minister. [COVID‐19] Press Conference by the Prime Minister Regarding the Novel Coronavirus. (In Japanese). Retrieved from: https://www.kantei.go.jp/jp/98_abe/statement/2020/0407kaiken.html
- Quad Council Coalition of Public Health Nursing Organizations . (2018). Community/Public Health Nursing [C/PHN] Competencies. QCC Task Force. Retrieved from https://www.cphno.org/wp-content/uploads/2020/08/QCC-C-PHN-COMPETENCIES-Approved_2018.05.04_Final-002.pdf
- Sands, L. P. , Albert, S. M. , & Suitor, J. J. (2020). Understanding and addressing older adults’ needs during COVID‐19. Innovation in Aging, 4(3), 1–3. 10.1093/geroni/igaa019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai, S. Y. , Hsiao, C. L. , & Lee, C. Y. (2020). Home healthcare services in communities during COVID‐19: Protecting against and mitigating the pandemics in Taiwan. Kaohsiung Journal of Medical Sciences, 36(8), 663–664. 10.1002/kjm2.12247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2019). Health Emergency and Disaster Risk Management Framework. Retrieved from https://www.who.int/hac/techguidance/preparedness/health-emergency-and-disaster-risk-management-framework-eng.pdf?ua=1
- Yin, R. K. (2017). Case study research and applications: Design and methods (6th ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Yoshioka‐Maeda, K. (2020a). The ‘8050 issue’ of social withdrawal and poverty in Japan's super‐aged society. Journal of Advanced Nursing, 76(8), 1884–1885. 10.1111/jan.14372 [DOI] [PubMed] [Google Scholar]
- Yoshioka‐Maeda, K. (2020b). Promoting needs‐oriented health programme planning through public health nurses in Japan. Journal of Advanced Nursing, 76(7), 1496–1497. 10.1111/jan.14337 [DOI] [PubMed] [Google Scholar]
- Yoshioka‐Maeda, K. , Iwasaki‐Motegi, R. , & Honda, C. (2020). Preventing the dysfunction of public health centres responding to COVID‐19 by focusing on public health nurses in Japan. Journal of Advanced Nursing, 76(9), 2215–2216. 10.1111/jan.14409 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of this study are not publicly available due to strictly the privacy of research participants.


