Abstract
In this study, we investigated the role and relationship between the cytokine profile and protective vitamin D by measuring their serum levels in COVID‐19 intensive care unit patients with severe illnesses. A total of 74 patients were included in our study. Patients were divided into two groups. Patients in the COVID‐19 group (n = 31) and individuals without a history of serious illness or infection were used as the control group (n = 43). The serum concentrations of interleukin‐1 (IL‐1), IL‐6, IL‐10, IL‐21, and tumor necrosis factor‐α (TNF‐α) were measured by enzyme‐linked immunosorbent assays. Levels of serum vitamin D were detected with Liquid chromatography–mass spectrometry methodologies. TNF‐α, IL‐1, IL‐6, IL‐10, IL‐21, and vitamin D levels were measured in all patients. The serum cytokine levels in the COVID‐19 patient group were significantly higher (151.59 ± 56.50, 140.37 ± 64.32, 249.02 ± 62.84, 129.04 ± 31.64, and 123.58 ± 24.49, respectively) than control groups. Serum vitamin D was also significantly low (6.82 ± 3.29) in patients in the COVID‐19 group than the controls (21.96 ± 5.39). Regarding the correlation of vitamin D with cytokine levels, it was significantly variable. Our study shows that COVID‐19 patients are associated with lower serum vitamin D and higher pro‐inflammatory cytokines associated with increased virus presence. Our data provide more evidence of the anti‐inflammatory effect of vitamin D on COVID‐19 patients and the protective effects of vitamin D on risk were demonstrated.
Keywords: COVID‐19, cytokines storm, pro‐inflammatory cytokines, SARS‐CoV‐2, vitamin D
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is an infectious disease, caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), which predominantly affects the lungs leading to severe infections. The source of the virus was Wuhan (China), from where it spread rapidly to other parts of the world causing the greatest worldwide pandemic since the 1918 flu pandemic. 1 A profound shock to the world societies and economies takes place when resources are strained and institutional capacity is limited. People face disproportionate impacts with far‐reaching consequences. As of August 5, 2021, there have been more than 200 million confirmed cases of COVID‐19, more than four million deaths, and nearly four billion doses of vaccine administered according to the World Health Organization (WHO) COVID‐19 dashboard. 2 On the same date, the Ministry of Health in Turkey announced a total of 5,514,373 confirmed cases and 50,450 death. 3
The SARS‐CoV‐2 virus is usually transmitted through droplets created by the infected person coughing, sneezing, or exhaling as these droplets are very heavy, they cannot remain suspended in the air and immediately fall to the ground or surfaces. Individuals can become infected if they inhale the virus while they are near someone infected with COVID‐19 or if they touch their eyes, nose, or mouth after touching an infected surface. Most people who contract COVID‐19 experience mild, moderate to severe symptoms, and some recover without the need for special treatment or hospitalization. The most common symptoms are fever, dry cough, tiredness, throat ache, loss of taste or sense of smell, headache, and diarrhea. 4 , 5 , 6 , 7 Serious symptoms are difficulty breathing or shortness of breath, chest pain or pressure in the chest, and loss of speech or movement. Older adults and those with underlying comorbidities or chronic diseases are at higher risk for developing the severe disease. 4 , 8
COVID‐19 mainly affects the respiratory, cardiovascular, and gastrointestinal systems. 4 It was found that a significant proportion of deaths occurred more than 2 weeks after the onset of symptoms suspected of being caused by cytokine storms. 4 , 9
The immune system is divided into two parts: innate and adaptive immunity which are activated shortly after microbial infections to provide protection against them. The activities of the cells of innate and adaptive immunity are coordinated by cytokines. 10 Emerging data reveal the activation of natural killer (NK) cells, innate immune effector cells, which not only contribute to the resolution of SARS‐CoV‐2 infection but also the cytokine storm found in acute respiratory disease syndromes (ARDS). 11 , 12
Vitamin D is a group of fat‐soluble steroids with a four‐ringed cholesterol backbone. It is involved in calcium absorption, immune function, and protecting bone, muscle, and heart health. The most common vitamin D cholecalciferol (Vitamin D3) and ergocalciferol (Vitamin D2) are precursors of 1,25 (OH) 2D3 the active form of vitamin D. 13 Previous clinical studies have been shown that vitamin D regulates cytokine and immune in acute viral respiratory infections. 14 , 15 , 16 , 17 Vitamin D increased the anti‐inflammatory phenotype while the pro‐inflammatory cytokines induced an inflammatory phenotype. Similar studies have shown that vitamin D inhibits the production of pro‐inflammatory cytokines (IL‐6, tumor necrosis factor‐α [TNF‐α], IL‐1, IL‐21, IL‐10) by macrophages and T cells. 17 , 18 , 19 , 20 , 21 Analyzing data during the COVID‐19 outbreak suggests that vitamin D plays a role in reducing the development of pneumonia and improving case fatality rates. 17 Inflammatory cytokines include TNF‐α, IL‐1, and IL‐6. IL‐10 is an anti‐inflammatory cytokine that downregulates the expression of Th1 cytokines, MHC class II antigens, and costimulatory molecules on macrophages. IL‐21 is a cytokine that has potent regulatory effects on cells of the immune system, including NK cells and cytotoxic T cells that can destroy virally infected or cancerous cells. It has been associated with allergies, cancer, and viral infections. 22
Previous therapeutic strategies have demonstrated targeting cytokines or altering the cytokine response with or without the combination of antiviral agents can aid in the recovery from influenza. 13 There are no recent studies investigating vitamin D status and serum cytokine profiles in patients with COVID‐19. To understand the immune mechanism underlying the pathogenesis and severity of patients with COVID‐19, we studied the expression profiles of cytokines (TNF‐α, IL‐1, IL‐6, IL‐10, IL‐21) and tried to determine the relationship between serum cytokine profiles and vitamin D levels in patients with severe COVID‐19 and their effects on the presence of clinical risk.
2. MATERIALS AND METHODS
2.1. Study design and samples collection
This study was carried out at the Harran University Medical School Department of Chest Diseases Inpatient Clinic and Clinical Biochemistry Laboratory between September 30, 2020 and March 30, 2021. In this study, a total of 74 participants were included. The patient's group contained 31 (19 females and 12 males) cases with severe COVID‐19 and 43 individuals (16 females and 27 males) without a history of serious illness or infection during the past month were used as a control group.
The classification of severe cases in COVID‐19 patients was made according to presence or absence of the following criteria: respiratory distress, tachypnea ≥30 beats/min; blood oxygen saturation (SpO2) level ≤90%; arterial blood oxygen partial pressure/oxygen concentration ≤300 mmHg; and evidence of bilateral diffuse pneumonia on chest X‐ray or chest computed tomography (CT). 23
Case history or anamnesis, reverse‐transcription polymerase chain reaction (RT‐PCR) test results, and chest CT data of studied patients were obtained from the clinical records of our hospital. Our study was planned in accordance with the criteria established in the Declaration of Helsinki. Informed consent was obtained from both the COVID‐19‐positive patients and controls. Ethics committee approval was obtained from the Harran University Department of Medicine document date and number 08/10/2020‐E.39547 and the Ministry of Health approved before this study began.
Blood samples (10 cm3) were collected from the antecubital vein within 24 h of admission. Serum samples were separated by centrifuged at 2000–3000 rpm at 20 min and stored at –80°C until analysis.
2.2. RT‐PCR assay
All patients were diagnosed and confirmed to be positive for COVID‐19 by RT‐PCR and chest CT. Nasopharyngeal swabs were taken and RT‐PCR analysis was performed. The vNAT Transfer Tube (Bio‐speedy) was used for RNA isolation from the swab samples. RNA samples were stored at −20°C until the amplification process. COVID‐19 RT‐PCR detection kit (Bio‐Speedy® SARS‐CoV‐2 double gene RT‐qPCR) was used to obtain cDNA and for amplification. RT‐PCR assay targeting the nucleocapsid protein (N) and open reading frame 1 ab (ORF1ab) genes were performed according to the manufacturer's instructions.
2.3. Measurement of cytokine by enzyme‐linked immunosorbent assay
The serum cytokines were measured in all the patients and controls using an enzyme‐linked immunosorbent assay (ELISA) (Elabscience Biotechnology Co Ltd.). Analyses were performed according to the manufacturers' instructions for each ELISA kit. Optical density was read at 450 nm (Thermo Fisher Scientific Oy). The cutoff value of each assay was calculated according to the manufacturer's instructions.
2.4. Measurement of vitamin D
Measurement of serum 25‐hydroxyvitamin D3 (25(OH)D3), the marker of vitamin D status, was performed by liquid chromatography–mass spectrometry (LC–MS/MS) methodologies. Three hundred and fifty microliters and 25 µl internal standard was added to the cell pellet and mixed for 5 s. It was centrifuged at 1000g for 5 min and the supernatant between 150 and 200 µl was taken into vials with inserts, and it was studied three times in the LC–MS/MS device. According to the guidelines, serum vitamin D level <20 ng/ml is defined as vitamin D deficiency. 24 , 25
2.5. Statistical analyses
The statistical analysis was conducted using the Statistical Package for the Social Sciences for Windows, version 20.0 (SPSS Inc.) software program. The data were represented by averages ± standard deviations, numbers, and percentages. Categorical variables were compared using the χ 2 test. In the normally distributed constant data comparison, the Student t test was used, and in the non‐normally distributed group, the Mann–Whitney U test was used. The Kruskal–Wallis test was used to compare more than two independent groups. A p < 0.05 value was accepted as the significance level.
3. RESULTS
According to the gender and age of the participants, a total of 31 COVID‐19 patient groups were included in this study; of these 19 (61.29%) were females (mean ages 53.72 ± 17.02 years) and 12 (38.71%) males (mean ages 52.60 ± 15.88 years). A total of 43 in the control group; those who were COVID‐19 negative and had no contact with any positive COVID‐19 patient were selected: of these 16 (36.4%) were females (mean ages 52.22 ± 14.61 years) and 27 (63.6%) males (mean ages 54.17 ± 11.44 years). There was no significant difference in age between the patient group and the control group.
The serum cytokines (TNF‐α, IL‐1, IL‐6, IL‐10, and IL‐21) concentrations in the COVID‐19 patient group were 151.59 ± 56.50, 140.37 ± 64.32, 249.02 ± 62.84, 129.04 ± 31.64, and 123.58 ± 24.49, respectively. Compared with the control group, the levels of all cytokines were found to be significantly higher in the COVID‐19 patient group. The results for the cytokines and vitamin D levels studied in the sera of patients and control groups are summarized in Table 1.
Table 1.
Analysis of serum cytokines and vitamin D levels in COVID‐19 patients and control groups
| Parameters | Patient group (n = 31) | Control group (n = 43) |
|---|---|---|
| TNF‐α (ng/L) | 151.59 ± 56.50 | 52.74 ± 20.43 |
| IL‐1 (pg/L) | 140.37 ± 64.32 | 23.98 ± 11.64 |
| IL‐6 (ng/L) | 249.02 ± 62.84 | 51.77 ± 21.24 |
| IL‐10 (pg/L) | 129.04 ± 31.64 | 86.46 ± 21.67 |
| IL‐21 (ng/L) | 123.58 ± 24.49 | 60.78 ± 20.52 |
| Vitamin D (ng/ml) | 6.82 ± 3.29 | 21.96 ± 5.39 |
Abbreviations: IL‐1, interleukin‐1; TNF‐α, tumor necrosis factor‐α.
Serum vitamin D was also significantly low (6.82 ± 3.29) in patients with the COVID‐19 group than in the control group (21.96 ± 5.39) (Table 1).
As seen in Figure 1, when the COVID‐19 patient group was compared with the control group, serum IL‐6 was the highest, followed by TNF‐α, and then IL‐1, IL‐10, and IL‐21, respectively. Vitamin D was found to be decreased compared to the control group (Figure 1).
Figure 1.
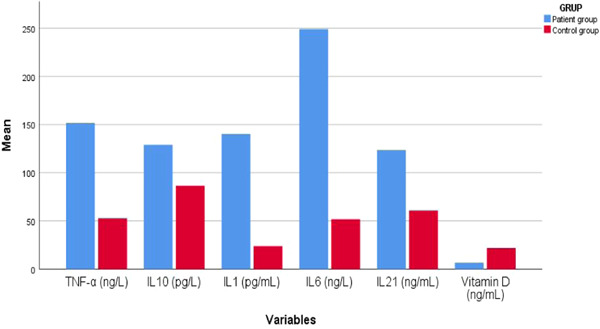
Levels of studied cytokines and vitamin D in both COVID‐19 patients and control group
3.1. Correlation of serum vitamin D with cytokines profiles
In our linear regression analyses, correlation values among the studied variables were as follows: serum vitamin D correlated with serum IL‐21 levels (−0.285, p < 0.01) and serum IL‐1 correlated with serum IL‐6 (0.059, p < 0.01). Correlation values between serum vitamin D and each of the pro‐inflammatory cytokines (IL‐1, IL‐6, IL‐10, TNF‐α) were found to be (−0.513, p < 0.01), (−0.473, p < 0.01), (−0.244, p < 0.01), (−0.545, p < 0.01) respectively. Accordingly, there was a negative correlation between the studied cytokines and vitamin D levels (Table 2). Regarding correlations within tested cytokines, as shown in Table 2, they were positive except IL‐10 which had a negative correlation with IL‐6 (−0.076, p > 0.05) and IL‐21 (−0.021, p < 0.05).
Table 2.
The correlation between cytokines and vitamin D between patients and control groups
| TNF‐α | IL‐1 | IL‐6 | IL‐10 | IL‐21 | Vitamin D | ||
|---|---|---|---|---|---|---|---|
| TNF‐α | Pearson correlation | 1 | 0.822** | 0.075 | 0.374** | 0.300* | −0.545** |
| Sig. (2‐tailed) | 0.000 | 0.571 | 0.003 | 0.020 | 0.000 | ||
| IL‐1 | Pearson correlation | 0.822** | 1 | 0.059 | 0.231 | 0.270* | −0.513** |
| Sig. (2‐tailed) | 0.000 | 0.657 | 0.076 | 0.037 | 0.000 | ||
| IL‐6 | Pearson correlation | 0.075 | 0.059 | 1 | −0.076 | 0.233 | −0.473** |
| Sig. (2‐tailed) | 0.571 | 0.657 | 0.564 | 0.073 | 0.000 | ||
| IL‐10 | Pearson correlation | 0.374** | 0.231 | −0.076 | 1 | −0.021 | −0.244 |
| Sig. (2‐tailed) | 0.003 | 0.076 | 0.564 | 0.875 | 0.060 | ||
| IL‐21 | Pearson correlation | 0.300* | 0.270* | 0.233 | −0.021 | 1 | −0.285* |
| Sig. (2‐tailed) | 0.020 | 0.037 | 0.073 | 0.875 | 0.027 | ||
| Vitamin D | Pearson correlation | −0.545** | −0.513** | −0.473** | −0.244 | −0.285* | 1 |
| Sig. (2‐tailed) | 0.000 | 0.000 | 0.000 | 0.060 | 0.027 | ||
Abbreviations: IL‐1, interleukin‐1; TNF‐α, tumor necrosis factor‐α.
Correlation is significant at the 0.01 level (2‐tailed).
Correlation is significant at the 0.05 level (2‐tailed).
In this study, anti‐inflammatory cytokines included IL‐10 and pro‐inflammatory cytokines included (TNF‐α, IL‐1, IL‐6, and IL‐21). We constructed serum cytokine profiles which included individual serum cytokines levels, ratios of anti‐inflammatory to pro‐inflammatory cytokines, sums of anti‐inflammatory cytokines, combinations of sums of pro‐inflammatory cytokines, and ratios of sums of anti‐inflammatory cytokines to sums of pro‐inflammatory cytokines (Table 2). We plotted serum cytokine profiles as a function of serum vitamin D.
4. DISCUSSION
COVID‐19 is an important viral respiratory human disease that resembles influenza in that it causes epidemics and pandemics with increased morbidity and mortality especially in the elderly and those with pre‐existing medical conditions. It seems to spread more easily than the flu and causes more serious illnesses in some people. SARS‐CoV‐2 can infect both the lung epithelium and endothelial cells with the onset of infection. 26 The role of endothelial cell involvement in lung inflammation has increased pro‐inflammatory cytokines production. 27 , 28
Cytokine production and its role on the pathogenicity and host immune response in other important viral respiratory diseases such as those caused by influenza A and SARS‐CoV‐1 and MERS‐COV. 29 , 30 , 31 , 32 , 33 Complications or ultimately death arising from these severe viral infections COVID‐19 and influenza are often associated with hyperinduction of pro‐inflammatory cytokine production (cytokine storm). An overactivation of immune cells results in the overproduction of pro‐inflammatory cytokines in severe cases of COVID‐19 infections. Damage to cells of the lung and airways due to inflammation may be due to viral infection and host immune responses. 9 , 10 In our patients, we were unable to perform and measure breathing tests due to shortness of breath, so lung function tests could not be done in severe COVID‐19 patients. These patients have hypercytokinemia with the highest levels of pro‐inflammatory cytokines (Table 1).
T helper cells are classified as Th1, Th2, and Th17 cells according to their cytokine production profile. 34 , 35 IL‐1, IL‐6, and IL‐10 play a role in the proliferation and differentiation of immune cells especially T helper cells. IL‐10 is primarily secreted by monocytes and to a lesser extent by Th2 cells of the innate and adaptive immune system. It is induced by several cytokines including IL‐21. 36 This directly explains the main immunological effect of this cytokine in the regulation of the Th1/Th2 balance. 37 The other effect of IL‐21 is to induce and increase the proliferation and cytotoxic activity of T8 and NK, whose function is to destroy virally infected cells and cancerous cells. 38 , 39 IL‐21 is the most recently discovered member of the type‐I cytokine family and it is mainly produced by CD4+ T cells. It activates a broad range of immune cells and therefore can regulate innate and acquired immune responses. It has been implicated in many immunological processes including autoimmune diseases, allergies, cancers, and other inflammatory diseases. 39 , 40 In this study, IL‐21 was significantly elevated in sera of severe COVID‐19‐infected patients. The role of IL‐21 in the pathogenesis of COVID‐19 should also be accentuated as the role of other studied cytokines was emphasized in other research. 9 , 10 , 41 , 42
Vitamin D has been established to enhance the innate immune system by upregulating antimicrobial peptides such as human cathelicidin. 43 Invading microorganisms can bind to Toll‐like receptors (TLRs) on alveolar macrophages which result in upregulation of the 1α‐hydroxylase and increased production of the active form of vitamin D (1,25(OH)2D) and increased expression of the vitamin D receptor. 44 1,25(OH)2D, in turn, can induce the expression of cathelicidin by macrophages and monocytes to clear the infection by the invading microorganisms. 43 , 44 Vitamin D status is necessary for better lung function and its therapy may help recovery from pulmonary exacerbations. Low vitamin D levels are common in the elderly and have been associated with death from many diseases and vitamin D supplementation can significantly reduce overall mortality. 19 , 20 In the definition of vitamin D status, International Organization for Migration committee members reported that the value of vitamin D 25(OH)D levels is >20 ng/m (>50 nmol) is considered sufficient but if it is <20 ng/ml (<50 nmol/L) it is deficient. 24 , 45 According to the Endocrine Society vitamin D guidelines, the state of individuals with 25(OH)D < 20 ng/ml (<50 nmol/L) is deficient, 21–29 ng/ml (50–75 nmol/L) is insufficient, and levels >30 ng/ml (>75 nmol/L) is sufficient. 25 , 46 In this study, the status of serum vitamin D level was deficient among COVID‐19 patients whereas in controls was insufficient. The low serum vitamin level in our population may be due to increased melanin, malabsorption, obese children and adults, and individuals who practice abstinence from direct sunlight. 24 , 45 So, those people are at risk of getting diseases. A study in patients in a Cao et al. 47 study showed that patients with acute myeloid leukemia had low serum vitamin D levels and vitamin D played a great role in the differentiation and proliferation of immature immune cells and it contributed to positive clinical outcomes. In cystic fibrosis, there is also low serum vitamin D. 24 , 45 The major limiting factor in therapy is the required supraphysiological dose which results in systemic hypercalcemia. Available data on the effect of vitamin D on NK cells in COVID‐19 patients indicate that decreased serum calcitriol can contribute to decreased NK activity in patients with chronic diseases. Vitamin D can act as an immunosuppressant in COVID‐19 by inhibiting the cytokine release syndrome. 17 It is increasingly accepted that most of the immune effects of vitamin D in respiratory diseases are responsible for localized 1,25(OH)2D3 synthesis, not systemic. 21 , 22 In the early stages (emergence stage) of acute inflammation, vitamin D inhibits the abnormal release of cytokines (TNF‐α, IL‐1, IL‐6, IL10, and IL‐21). During the resolution phase of inflammation, vitamin D mediated differentiation and release of cytokines (IL‐1 and IL‐10) are important to prevent organ damage through an excessive immune response. Downregulation of pro‐inflammatory cytokines is another important mechanism by which vitamin D exerts its immunomodulatory effects in pulmonary infection. IL‐6 has been thought to play a key role in cytokine storms associated with severe adverse outcomes and low NK cell count in patients infected with SARS‐CoV‐2 pneumonia. 48 , 49 Anti‐IL6 therapy is in the clinical trial phase for severe respiratory failure in COVID‐19. In addition, there are ongoing clinical trials of vitamin D in the prevention and treatment of autoimmune diseases using its immunomodulatory function. Given its powerful immunosuppressant role, vitamin D supplementation can help prevent the abnormal immune response and cytokine storm in COVID‐19.
The clinical effects of vitamin D status on patients with respiratory distress have attracted great attention, especially in COVID‐19 patients. This is the first study to evaluate the relationship between vitamin D and inflammatory cytokines levels in severe COVID‐19 cases. The results of this showed that low vitamin D is associated with higher morbidity, disease severity, and health problems in COVID‐19 patients. In our study, an inverse correlation was found between serum vitamin D and mucosal inflammation in COVID‐19 patients (Table 2). The mechanical link between vitamin D and immune protective effects in COVID‐19 patients is not fully understood. Thus, from randomized‐controlled perspective, more studies are needed for this.
There are some limitations to our study. First, the low number of samples taken from COVID‐19‐infected patients. Second, we were unable to study cytokines in respiratory samples and to test other important recently discovered cytokines such as IL‐25, IL‐29, and IL‐35 due to cost and insufficient financial support. Therefore, we suggest a multicenter study with a large number of samples to obtain more robust and beneficial results. So, such data will increase our horizon of knowledge of the subject.
5. CONCLUSIONS
COVID‐19 virus induces cytokine production. It induces pro‐inflammatory responses, proliferates efficiently from the human respiratory tract, those infected with viruses increase pro‐inflammatory cytokine and chemokine production within 24 h. Levels of all viruses tested were measured and high cytokines were found, especially IL‐6, TNF‐α levels were found to be significantly higher. Our data in Table 1 show that the virus enables uptake and cytokine storm production. High levels of cytokine storm syndrome' may be one of the critical hallmarks of COVID‐19 disease severity. There is ample evidence that vitamin D is essential for normal immune and lung functions to fight pathogens and prevent autoimmune diseases. It is demonstrated that there exists the potential of vitamin D supplementation to prevent acute respiratory infection by modulating the innate immune response. As vitamin D therapy can reduce the COVID‐19 disease burden, so daily supplementation is preferred to better outcomes in COVID‐19 patients. Preventing vitamin D deficiency in patients with severe COVID‐19 seems prudent as vitamin D deficiency is very common and it is associated with both an increased risk of various inflammatory diseases and increased susceptibility to infections including COVID‐19.
CONFLICT OF INTERESTS
The authors declare that therer are no conflict of interests.
AUTHOR CONTRIBUTIONS
Nihayet Bayraktar designed the study. Nihayet Bayraktar and Hamdiye Turan conducted the laboratory tests. Mehmet Bayraktar and Hamza Erdoğdu collected and analyzed the data. Nihayet Bayraktar, Mehmet Bayraktar, and Ali Ozturk prepared the manuscript. Ali Ozturk, Mehmet Bayraktar, and Nihayet Bayraktar edited and reviewed the manuscript. All the authors critically reviewed and revised the manuscript draft, and approved the final version of the manuscript.
Bayraktar N, Turan H, Bayraktar M, Ozturk A, Erdoğdu H. Analysis of serum cytokine and protective vitamin D levels in severe cases of COVID‐19. J Med Virol. 2021;94:154‐160. 10.1002/jmv.27294
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Cao Y, Cai K, Xiong L. Coronavirus disease 2019: A new severe acute respiratory syndrome from Wuhan in China. Acta Virol. 2020;64(2):245‐250. 10.4149/av_2020_201 [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . Coronavirus disease 2019 (COVID‐19) Dashboard. Accessed June 29, 2020. https://www.who.int
- 3.Republic of Turkey, Ministry of Health. COVID‐19 Status Report. https://covid19.saglik.gov.tr/TR-68443/covid-19-durum-raporu.html
- 4. Villapol S. Gastrointestinal symptoms associated with COVID‐19: impact on the gut microbiome. Transl Res. 2020;226:57‐69. 10.1016/j.trsl.2020.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bajaj A, Purohit HJ. Understanding SARS‐CoV‐2: genetic diversity, transmission and cure in human. Indian J Microbiol. 2020;60(3):398‐401. 10.1007/s12088-020-00869-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morawska L, Milton DK. It is time to address airborne transmission of COVID 19. Clin Infect Dis. 2020;71(9):2311‐2313. 10.1093/cid/ciaa939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori‐Asenso R. Smell and taste dysfunction in patients with COVID‐19: a systematic review and meta‐analysis. Mayo Clin Proc. 2020;95(8):1621‐1631. 10.1016/j.mayocp.2020.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Esakandari H, Nabi‐Afjadi M, Fakkari‐Afjadi J, Farahmandian N, Miresmaeili SM, Bahreini E. A comprehensive review of COVID‐19 characteristics. Biol Proced Online. 2020;22(19):19. 10.1186/s12575-020-00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Catanzaro M, Fagiani F, Racchi M, Corsini E, Govoni S, Lanni C. Immune response in COVID‐19: addressing a pharmacological challenge by targeting pathways triggered by SARS‐CoV‐2. Signal Trans Target Ther. 2020;5:84. 10.1038/s41392-020-0191-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fara A, Mitrev Z, Rosalia RA, Assas BM. Cytokine storm and COVID‐19: a chronicle of pro‐inflammatory cytokines. Open Biol. 2020;9:1‐12. 10.1098/rsob.200160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wong CK, Lam CW, Wu AK, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136(1):95‐103. 10.1111/j.1365-2249.2004.02415x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang Y, Xu J, Zhou C, et al. Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome. Am J Respir Crit Care Med. 2005;171(8):850‐857. 10.1164/rccm.200407-857OC [DOI] [PubMed] [Google Scholar]
- 13. Norman AW. From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am J Clin Nutr. 2008;88(2):491S‐499S. 10.1093/ajcn/88.2.491S [DOI] [PubMed] [Google Scholar]
- 14. Martineau AR, Jolliffe DA, Greenberg L, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta‐analysis. Health Technol Assess. 2019;23(2):1‐44. 10.3310/hta23020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zisi D, Challa A, Makis A. The association between vitamin D status and infectious diseases of the respiratory system in infancy and childhood. Hormones. 2019;18(4):353‐363. 10.1007/s42000-019-00155-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zdrenghea MT, Makrinioti H, Bagacean C, Bush A, Johnston SL, Stanciu LA. Vitamin D modulation of innate immune responses to respiratory viral infections. Rev Med Virol. 2017;27(1), 10.1002/rmv.1909 [DOI] [PubMed] [Google Scholar]
- 17. Xu Y, Baylink DJ, Chen CS, et al. The importance of vitamin D metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID‐19. J Transl Med. 2020;18(1):322 1‐12. 10.1186/s12967-020-02488-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hansdottir S, Monick, MM , Lovan, N , et al. Vitamin D decreases respiratory syncytial virus induction of NF‐kappaB‐linked chemokines and cytokines in airway epithelium while maintaining the antiviral state. J Immunol. 2010;184(2):965‐974. 10.4049/jimmunol.0902840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fraser WD, Tang JCY, Dutton JJ, Schoenmakers I. Vitamin D measurement, the debates continue, new analytes have emerged, developments have variable outcomes. Calcif Tissue Int. 2020;106(1):3‐13. 10.1007/s00223-019-00620-2 [DOI] [PubMed] [Google Scholar]
- 20. Khoo AL, Chai LYA. Koenen HJPM, et al. Vitamin D(3) down‐regulates proinflammatory cytokine response to Mycobacterium tuberculosis through pattern recognition receptors while inducing protective cathelicidin production. Cytokine. 2011;55(2):294‐300. 10.1016/j.cyto.2011.04.016 [DOI] [PubMed] [Google Scholar]
- 21. Wobke TK, Sorg BL, Steinhilber D. Vitamin D in inflammatory diseases. Front Physiol. 2014;5:244. 10.3389/fphys.2014.00244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Parrish‐Novak J, Foster DC, Holly RD, Clegg CH. Interleukin‐21 and the IL‐21 receptor: novel effectors of NK and T cell responses. J Leukoc Biol. 2002;72(5):856‐863. [PubMed] [Google Scholar]
- 23.Republic of Turkey Ministry of Health. COVID‐19 (SARS‐CoV2 infection) guide. Adult patient treatment. 2021. https://saglik.gov.tr/
- 24. Daley T, Hughan K, Rayas M, Kelly A, Tangpricha V. Vitamin D deficiency and its treatment in cystic fibrosis. J Cyst Fibros. 2019;18(2):66‐73. 10.1016/j.jcf.2019.08.022 [DOI] [PubMed] [Google Scholar]
- 25. Holick MF. Disorders. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18(2):153‐165. 10.1007/s11154-017-9424-1 [DOI] [PubMed] [Google Scholar]
- 26. Liu F, Han K, Blair R, et al . SARS‐CoV‐2 infects endothelial cells in vivo and in vitro. Front Cell Infect Microbiol. 2021:11. 10.3389/fcimb.2021.701278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu Q, Yuan‐hong Z, Yang Z. The cytokine storm of severe influenza and development of immunomodulatory therapy. Cell Mol Immunol. 2016;13(1):3‐10. 10.1038/cmi.2015.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Betakova T, Kostrabova A, Lachova V, Turianova L. Cytokines induced during influenza virus infection. Curr Pharm Des. 2017;23(18):2616‐2622. 10.2174/1381612823666170316123736 [DOI] [PubMed] [Google Scholar]
- 29. Zhang Y, Li J, Zhan Y, et al. Analysis of serum cytokines in patients with severe acute respiratory syndrome. Infect Immun. 2004;72:4410‐4415. 10.1128/IAI.72.8.4410-4415.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wong CK, Lam CW, Wu AK, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95‐103. 10.1111/j.1365-2249.2004.02415.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Beijing Group of National Research Project for SARS. Dynamic changes in blood cytokine levels as clinical indicators in severe acute respiratory syndrome. Chin Med J. 2003;116:1283‐1287. [PubMed] [Google Scholar]
- 32. Mubarak A, Alturaiki W, Hemida MG. Middle East respiratory syndrome coronavirus (MERS‐CoV): infection, immunological response, and vaccine development. J Immunol Res. 2019;2019:6491738. 10.1155/2019/6491738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mahallawi WH, Khabour OF, Zhang Q, Makhdoum HM, Suliman BA. MERS‐CoV infection in humans is associated with a pro‐inflammatory Th1 and Th17 cytokine profile. Cytokine. 2018;104:8‐13. 10.1016/j.cyto.2018.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mosmann TR, Coffman RL. TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Annu Rev Immunol. 1989;7:145‐173. 10.1146/annurev.iy.07.040189.001045 [DOI] [PubMed] [Google Scholar]
- 35. Weaver CT, Hatton RD, Mangan PR, Harrington LE. IL‐17 family cytokines and the expanding diversity of effector T cell lineages. Annu Rev Immunol. 2007;25:821‐852. 10.1146/annurev.immunol.25.022106.141557 [DOI] [PubMed] [Google Scholar]
- 36. Spolski R, Kim HP, Zhu W, Levy DE, Leonard WJ. IL‐21 mediates suppressive effects via its induction of IL‐10. J Immunol. 2009; 182(5):2859‐2867. 10.4049/jimmunol.0802978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Saravia M, O'Garra A. The regulation of IL‐10 production by immune cells. Nat Rev Immunol. 2010;10(3):170‐181. 10.1038/nri2711 [DOI] [PubMed] [Google Scholar]
- 38. Tian Y, Zajac AJ. IL‐21 and T cell differentiation: consider the context. Trends Immunol. 2016;37(8):557‐568. 10.1016/j.it.2016.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Parrish‐Novak J, Foster DC, Holly RD, Clegg CH. Interleukin‐21 and the IL‐21 receptor: novel effectors of NK and T cell responses. J Leukoc Biol. 2002;72(5):856‐863. [PubMed] [Google Scholar]
- 40. Brandt K, Singh PB, Bulfone‐Paus S, Rückert R. Interleukin‐21: a new modulator of immunity, infection, and cancer. Cytokine Growth Factor Rev. 2007;18(3‐4):223‐232. 10.1016/j.cytogfr.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 41. Han H, Ma, Q , Li, C , et al. Profiling serum cytokines in COVID‐19 patients reveals IL‐6 and IL‐10 are disease severity predictors. Emerg Microbes Infect. 2020;1:1123‐1130. 10.1080/22221751.2020.1770129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rokni M, Hamblin MR, Rezaei N. Cytokines and COVID‐19: friends or foes? Hum Vaccin Immunother. 2020;16(10):2363‐2365. 10.1080/21645515.2020.1799669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liu PT, Stenger S, Li H, et al. Toll‐like receptor triggering of a vitamin d‐mediated human antimicrobial response. Science. 2006;311(5768):1770‐1773. 10.1126/science.1123933 [DOI] [PubMed] [Google Scholar]
- 44. Hewison M. Vitamin D and the intracrinology of innate immunity. Mol Cell Endocrinol. 2010;321(2):103‐111. 10.1016/j.mce.2010.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chesdachai S, Tangpricha V. Treatment of vitamin D deficiency in cystic fibrosis. J Steroid Biochem Mol Biol. 2016;164:36‐39. 10.1016/j.jsbmb.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Holick MF, Binkley NC, Bischoff‐Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911‐1930. 10.1210/jc.2011-0385 [DOI] [PubMed] [Google Scholar]
- 47. Cao H, Xu Y, de Necochea‐Campion R, et al. Application of vitamin D and vitamin D analogs in acute myelogenous leukemia. Exp Hematol. 2017;50:1‐12. 10.1016/j.exphem.2017.01.007 [DOI] [PubMed] [Google Scholar]
- 48. Davis MR, Zhu Z, Hansen DM, Bai Q, Fang Y. The role of IL‐21 in immunity and cancer. Cancer Lett. 2015;358(2):107‐114. 10.1016/j.canlet.2014.12.047 [DOI] [PubMed] [Google Scholar]
- 49. Siddiqui M, Manansala JS, Abdulrahman HA, et al. Immune modulatory effects of vitamin D on viral infections. Nutrients. 2020;12(9):2879. 10.3390/nu12092879 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


