Abstract
Aims and Objectives
This systematic review and meta‐analysis reports the seroprevalence of SARS‐CoV‐2 antibodies among nurses.
Background
With a growing body of literature reporting the positive serology for SARS‐CoV‐2 antibodies among healthcare workers, it remains unclear whether staff at the point of direct patient care are more prone to developing and transmitting the virus. Given nurses make up the majority of the global health workforce, outbreaks among these workers could severely undermine a health system’s capability to manage the pandemic. We aimed to summarise and report the seroprevalence of SARS‐CoV‐2 antibodies among nurses globally.
Design
Systematic review and meta‐analyses.
Methods
This systematic review was developed, undertaken and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guideline. We searched the electronic medical literature databases: MEDLINE; CINAHL; and EMBASE for studies reporting the seroprevalence of SARS‐CoV‐2 antibodies among nursing staff. Studies that reported nursing specific data were included in this review. Study quality was evaluated using the Joanna Briggs Institute checklist for studies reporting prevalence data. Studies were stratified according to the World Health Organisation region classifications, and results were presented using forest plots and summary prevalence and variance was estimated using a random effects model.
Results
Our electronic search identified 1687 potential studies, of which 1148 were screened for eligibility after duplicates were removed, and 51 of the studies were included in our meta‐analysis. The overall seroprevalence of SARS‐CoV‐2 antibodies among nurses was estimated to be 8.1% (95% CI 6.9%–9.4%) among the 60,571 participants included in the studies. Seropositivity was highest in the African region (48.2%, 95% CI 39.2%–57.3%), followed by the European region (10.3%, 95% CI 8.0%–12.5%), the Region of the Americas (8.4%, 95% CI 6.0%–10.7%), the South‐East Asia region (3.0%, 95% CI 0.00%–6.5%) and the Western Pacific region (0.5%, 95% CI 0.0%–1.0%). Pooled estimates were unable to be calculated in the Eastern Mediterranean region due to insufficient studies.
Conclusion
The seroprevalence of SARS‐CoV‐2 antibodies among nurses is comparable to other healthcare workers, and possibly similar to the general population. Early adoption and adherence to personal protective equipment and social distancing measures could explain these similarities, meaning the majority of staff contracted the virus through community transmission and not in a healthcare setting.
Relevance to clinical practice
Fear and uncertainty have been features of this pandemic, including among nurses. This meta‐analysis should provide some comfort to nurses that risks are similar to community exposure when adequate PPE is available and there is an adherence to infection control measures.
Keywords: COVID‐19, nurses, SARS‐CoV‐2, seroprevalence
What does this paper contribute to the wider global community?
A comparison of seroprevalence estimates between nurses, healthcare workers and the general population.
A comparison of nursing seroprevalence estimates among WHO geographical regions.
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) is a respiratory illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) that was first encountered in December 2019 and continues to challenge governments and healthcare systems across the globe. As of 19 April 2021, the World Health Organization [WHO] (2021) has reported over 141 million cases and over three million attributable deaths since the beginning of the pandemic, with hundreds of thousands of cases detected each day. Serological surveys have also been conducted to help determine the underlying prevalence of SARS‐Cov‐2 and provide some insight on transmission between asymptomatic individuals. A 2021 systematic review found a seroprevalence rate of 8.0% among the global population (Chen et al., 2021).
Infection rates among healthcare workers are of particular concern, given they seem to be at high risk of both developing and transmitting the illness (Nguyen et al., 2020; Pan et al., 2020; Quigley et al., 2021; Schneider et al., 2020; Wu & McGoogan, 2020). It remains unclear whether staff at the point of direct patient care are more prone to developing and transmitting the virus, due to limited available data around community transmission (Hunter, Price, et al., 2020; Misra‐Hebert et al., 2020). A recent systematic review, however, reported nurses accounted for half of all SARS‐CoV‐2 positive serology among healthcare workers, suggesting prolonged exposure to direct patient care may be a contributing factor (Gómez‐Ochoa et al., 2020). Given nurses make up the majority of the global health workforce, outbreaks among these workers could severely undermine a health system's capabilities to manage the pandemic, particularly in low resource settings (WHO, 2020). Specific rates among nursing staff have not been summarised and reported, and further research is needed to determine whether nurses are at higher risk of infection than other members of the healthcare team. Therefore, this systematic review and meta‐analysis were planned to summarise and report the seroprevalence of SARS‐CoV‐2 antibodies among nurses globally.
2. METHODS
2.1. Data sources and search strategy
The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) Guideline (File S1) was used to plan, undertake and report this systematic review and meta‐analysis (Page et al., 2021). A senior health librarian (LH) planned and developed our search strategy. Electronic medical databases included MEDLINE; CINAHL; and EMBASE, which were searched on the 15th of February 2021 using the following keywords: COVID‐19, COVID, coronavirus, Wuhan, 2019, SARS, SARS‐CoV‐2, coronavirus 2, 2019‐ncov, SARS‐2, health personnel, health worker, health workforce, health professional, nurse, sero‐epidemiologic studies, seroprevalence, antibodies, serologic tests, immunoglobulin, IgG, IgA and IgM. Preprint studies and results prior to 2019 were excluded. We also searched Google Scholar for primary citations and checked any subsequent citation of papers included in our review. A hand search of the references lists of all included papers was also undertaken to ensure no further papers could be included in our systematic review and meta‐analysis.
2.2. Inclusion and exclusion criteria
All observational studies were considered, and longitudinal studies were only included if a point prevalence was reported (baseline figures were extracted). Studies must have assessed the prevalence of SARS‐CoV‐2 using a serological test that detected the presence of SARS‐CoV‐2 antibodies (IgG, IgM, IgA or a combination of the three) among a sample of healthcare workers. Studies that did not report any raw nursing data were excluded.
We merged all the retrieved studies from individual databases into Endnote version X9.3.3 and all duplicate references were filtered and removed. Authors SH and HM independently reviewed selected titles and abstracts for potential inclusion. If any discrepancies were observed between the review authors and could not be resolved, review authors SF and EA would be consulted to arbitrate (this was not required). We also scanned the reference lists and citations of included studies for further references to additional studies. Study authors were contacted for additional information when nursing and/or serological specific data was not made clear due to grouping with other measures of outcomes.
2.3. Data extraction and quality assessment
Extraction of data was conducted by one investigator (SH) and was validated by another (SF). Information acquired included: first author; year of publication; study design; dates of data collection; region/country of study; sample size; therapeutic areas assessed; number of sites where the study was conducted; antibodies assessed; and type of immunoassay. With regard to studies that utilised multiple immunoassays, the final immunoassay used to determine seropositivity was recorded.
Quality assessment of the studies was undertaken by the two authors (SH and HM) using the Joanna Briggs Institute (JBI) critical appraisal checklist for studies reporting prevalence data (Munn et al., 2015). Despite there being a lack of consensus around how to appraise prevalence studies, the JBI checklist has been found to be the most comprehensive and widely used amongst researchers (Borges Migliavaca et al., 2020). A scaling measurement was created to differentiate studies according to a level of quality. One point was assigned to each ‘Yes’ response to the nine checklist items (Low = 0–4 checklist items; Moderate = 5–7 checklist items; High = 8–9 checklist items). No studies were excluded on the basis of quality.
2.4. Data analysis
The seroprevalence rates of SARS‐CoV‐2 antibodies among nurses were expressed as proportions with 95% confidence intervals and presented as Forest plots (Barendregt et al., 2013). We considered the degree of heterogeneity of results by calculating the I 2 statistic. In order to minimise heterogeneity between seroprevalence estimates, the studies were stratified and data pooled according to WHO region classifications: African region, Eastern Mediterranean region, European region, Region of the Americas, South‐East Asia region and Western Pacific Region. A random effects (RE) model was used to present pooled seroprevalence estimates due to high heterogeneity post‐stratification. Publication bias was assessed upon visual inspection of forest plot and test of plot asymmetry (Egger et al., 1997). All analysis was undertaken using the meta‐package as part of the R statistical program (R Core Team, 2017).
3. RESULTS
3.1. Electronic search results
Our initial search generated 1687 results, from which 539 duplicates were removed. The remaining 1148 studies had their titles and abstracts screened for compliance with our eligibility criteria (see Figure 1 PRISMA search flowchart). Fifty‐one studies were included in the final review (see Table 1 for study characteristics), with the majority of the studies conducted in the Region of the Americas region (n = 19), followed by the European region (n = 18), Western Pacific region (n = 8), South‐East Asia region (n = 3), African region (n = 2) and Eastern Mediterranean (n = 1).
FIGURE 1.
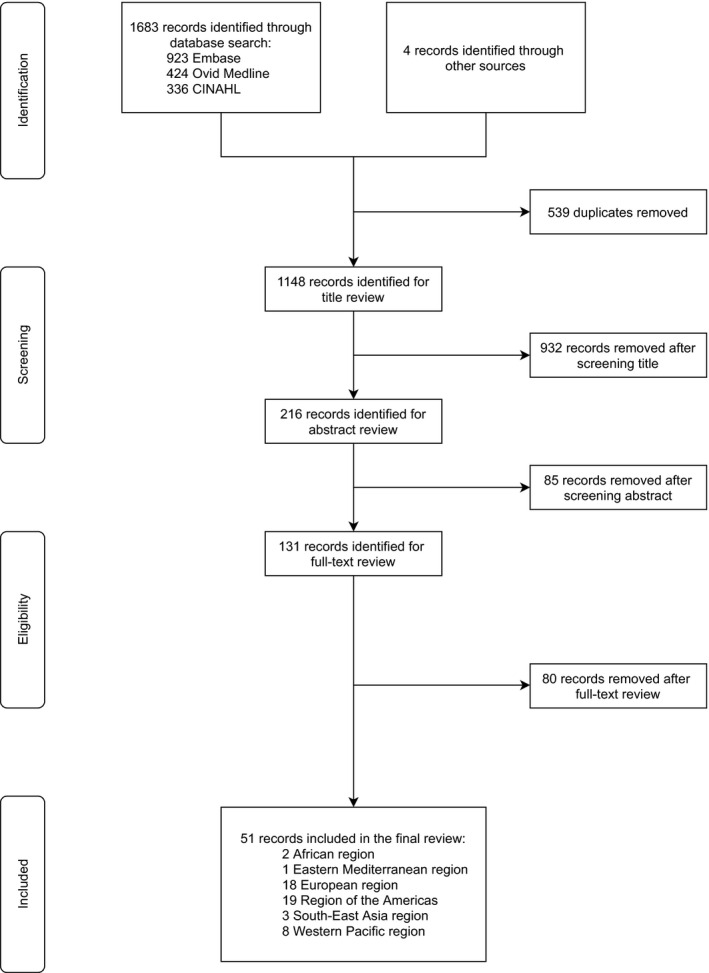
PRISMA search flowchart
TABLE 1.
Characteristics of included studies
| First author (year) | City/region, country | Type | Setting | Number of participants | Antibodies assessed | Quality assessment |
|---|---|---|---|---|---|---|
| Akinbami et al. (2020) | Detroit, USA | Cross‐sectional | First responders, multi‐centre | 6426 | IgG | Moderate |
| Akinbami et al. (2021) | Rhode Island, USA | Cross‐sectional | Hospital, multi‐centre | 2733 | IgG | Moderate |
| Amendola et al. (2020) | Lombardy, Italy | Cross‐sectional | Hospital, paediatrics, single‐centre | 216 | IgG | High |
| Barallat et al. (2020) | Barcelona, Spain | Cross‐sectional | Region‐wide screen | 2243 | IgG | High |
| Barrett et al. (2020) | New Jersey, USA | Cross‐sectional | Hospital, all services, single‐centre | 1361 | IgG | High |
| Brehm et al. (2021) | Hamburg, Germany | Longitudinal | Hospital, all services, single‐centre | 444 | IgG | Moderate |
| Calcagno et al. (2021) | Piedmont, Italy | Cross‐sectional | Hospital, all services, multi‐centre | 1983 | IgG | Moderate |
| Chau et al. (2021) | Ho Chi Minh, Vietnam | Cross‐sectional | Hospital, infectious diseases, single‐centre | 144 | IgG | Moderate |
| Chen et al. (2020) | Jiangsu Province, China | Cross‐sectional | Hospital, direct contacts of COVID‐19 patients, single‐centre | 25 | IgG, IgM | High |
| Costa et al. (2020) | Sao Paulo, Brazil | Cross‐sectional | Hospital, all services, single‐centre | 370 | IgG, IgM | High |
| Dimcheff et al. (2021) | Ohio and Michigan | Cross‐sectional | Hospital, veteran affairs, Multi‐centre | 412 | IgG | Moderate |
| El Bouzidi et al. (2021) | Lambeth, England | Cross‐sectional | Hospital, critical care services, single‐centre | 280 | IgG, IgM | Moderate |
| Finkenzeller et al. (2020) | Weiden in der Oberpfalz and Tirschenreuth, Germany | Cross‐sectional | Hospital, all services, multi‐centre, | 887 | IgG, IgM | High |
| Fujita et al. (2020) | Kyoto, Japan | Cross‐sectional | Hospital, Infectious disease, respiratory medicine, otolaryngology, emergency medicine, Single‐centre | 48 | IgG | Moderate |
| Galán et al. (2020) | Madrid, Spain | Cross‐sectional | Hospital, all services, single‐centre | 676 | IgG | High |
| Gandhi et al. (2021) | New Jersey, USA | Cross‐sectional | Hospital, direct contacts of COVID‐19 patients, single‐centre | 68 | IgG | Low |
| Garcia‐Basteiro et al. (2020) | Barcelona, Spain | Cross‐sectional | Hospital, all services, single‐centre | 288 | IgG, IgM, IgA | High |
| Garralda Fernandez et al. (2021) | Madrid, Spain | Cross‐sectional | Hospital, all services, single‐centre | 983 | IgG, IgM | High |
| Godbout et al. (2020) | Virginia, USA | Cross‐sectional | Hospital, all services, single‐centre | 937 | IgG | Moderate |
| Hibino et al. (2021) | Kanagawa, Japan | Cross‐sectional | Hospital, all services, single‐centre | 363 | IgG | Moderate |
| Howard‐Anderson et al. (2021) | Fulton County, USA | Cross‐sectional | Hospital, all services, multi‐centre | 144 | IgG | Moderate |
| Hunter, Dbeibo, et al. (2020) | Indiana, USA | Cross‐sectional | Hospital, all services multi‐centre | 317 | IgG | Moderate |
| Isherwood et al. (2020) | Leicester, England | Cross‐sectional | Hospital, all services, single‐centre | 84 | IgG | Low |
| Iversen et al. (2020) | Capital Region of Denmark, Denmark | Cross‐sectional | Region‐wide screen | 9963 | IgG or IgM | High |
| Jeremias et al. (2020) | New York, USA | Cross‐sectional | Hospital, all services, single‐centre | 1043 | IgG | Moderate |
| Kassem et al. (2020) | Cairo, Egypt | Cross‐sectional | Hospital, gastroenterology, single‐centre | 28 | IgG or IgM | Moderate |
| Khan et al. (2021) | Kashmir, India | Cross‐sectional | Region‐wide screen | 321 | IgG | Moderate |
| Ko et al. (2020) | Multiple sites, South Korea | Cross‐sectional | Hospital, all services, multi‐centre, | 335 | IgG | Moderate |
| Kohler et al. (2020) | St. Gallen, Switzerland | Cross‐sectional | Hospital, paediatrics, multi‐centre, | 398 | IgG | Moderate |
| Kumar, Sathyapalan, et al. (2020) | Kerala, India | Cross‐sectional | Hospital, all services, single‐centre | 132 | IgG | Moderate |
| Kumar, Bhartiya, et al. (2020) | Mumbai, India | Cross‐sectional | Hospital, all services, multi‐centre | 308 | IgG, IgM | Moderate |
| Matsuba et al. (2020) | Kanagawa, Japan | Cross‐sectional | Hospital, all services, multi‐centre | 287 | IgG | Moderate |
| Moscola et al. (2020) | New York City, New York | Cross‐sectional | Hospital, all services, multi‐centre | 11,468 | IgG | Moderate |
| Mukwege et al. (2021) | Bukavu, Congo | Cross‐sectional | Hospital, all services, single‐centre | 83 | IgG, IgM | High |
| Murakami et al. (2021) | Washington DC, USA | Cross‐sectional | Hospital, emergency, single‐centre | 51 | IgG | High |
| Nicholson et al. (2020) | San Diego County, USA | Cross‐sectional | Hospital, all services, multi‐centre | 734 | IgG | Moderate |
| Olalla et al. (2020) | Malaga, Spain | Cross‐sectional | Hospital, direct contacts of COVID‐19 patients, single‐centre | 195 | IgM, IgG | Moderate |
| Olayanju et al. (2021) | Ibadan, Nigeria | Cross‐sectional | Hospital, all services, single‐centre | 33 | IgG | Moderate |
| Perez‐Garcia et al. (2020) | Madrid, Spain | Cross‐sectional | Hospital, all services, single‐centre | 508 | IgG, IgM | High |
| Plebani et al. (2020) | Veneto Region, Italy | Cross‐sectional | Hospital, all services, multi‐centre | 3230 | IgG, IgM | Moderate |
| Purswani et al. (2021) | Bronx, USA | Cross‐sectional | Hospital, all services, multi‐centre | 611 | IgG | Moderate |
| Rosser et al. (2020) | San Francisco, USA | Cross‐sectional | Hospital, all services, multi‐centre | 3774 | IgG | Moderate |
| Rudberg et al. (2020) | Danderyd, Sweden | Cross‐sectional | Hospital, all services, single‐Centre | 636 | IgG | Moderate |
| Schmidt et al. (2020) | Hameln‐Pyrmont, Germany | Cross‐sectional | Hospital, all services, single‐centre | 154 | IgG | Moderate |
| Self et al. (2020) | Multiple sites, USA | Cross‐sectional | Hospital, all services, multi‐centre | 1445 | IgG, IgM, IgA | Moderate |
| Steensels et al. (2020) | Limburg, Belgium | Cross‐sectional | Hospital, all services, single‐centre | 1266 | IgG, IgM | High |
| Stubblefield et al. (2020) | Davidson, USA | Cross‐sectional | Hospital, direct contacts of COVID‐19 patients, single‐centre | 105 | IgG | Moderate |
| Tanaka et al. (2021) | Tokyo, Japan | Cross‐sectional | Hospital, all services, single‐centre | 601 | IgG | High |
| Tong et al. (2020) | Jiangsu Province, China | Cross‐sectional | Hospital, direct contacts of COVID‐19 patients, single‐centre | 159 | IgG, IgM | High |
| Venugopal et al. (2021) | Bronx, USA | Cross‐sectional | Hospital, trauma, single‐centre | 142 | IgG | Moderate |
| Yogo et al. (2020) | San Diego County, USA | Cross‐sectional | Hospital, all services, multi‐centre | 1129 | IgG | Moderate |
3.2. Quality assessment
Utilising the JBI critical appraisal checklist, we determined 16 studies to be of high quality, 33 studies to be of moderate quality and two studies were considered low quality. The majority of investigations recruited participants appropriately, either by inviting the entire target population or randomly selecting their sample (n = 38, 75%). Twenty‐two studies did not report a response rate, and forty‐four studies did not provide evidence of sufficient coverage of the identified sample.
3.3. Seroprevalence of SARS‐CoV‐2 antibodies among nurses
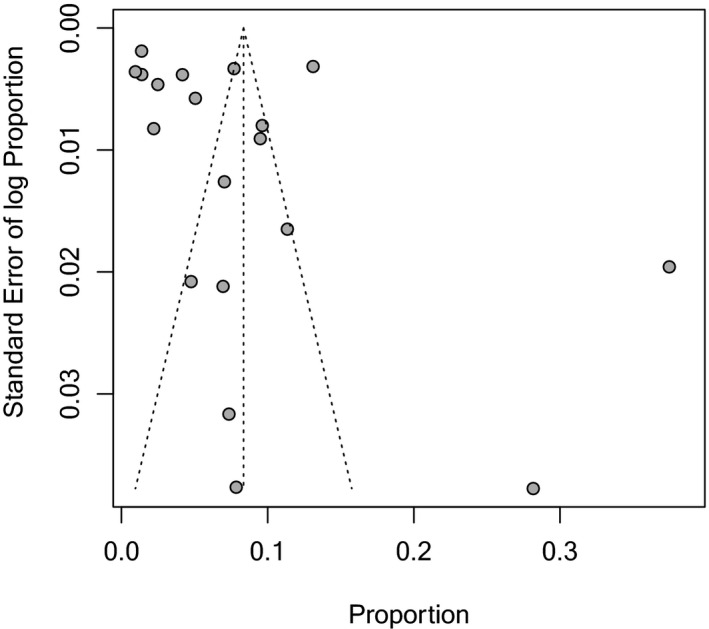
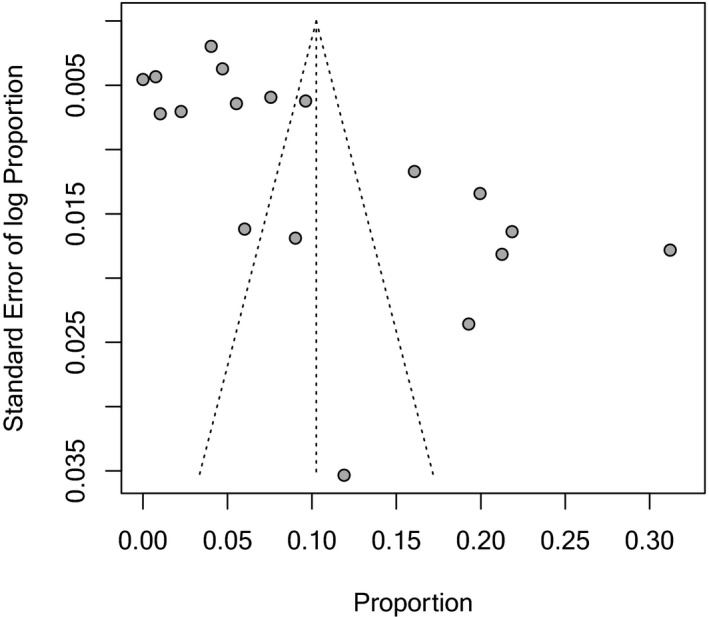
The overall seroprevalence of SARS‐CoV‐2 antibodies among nurses was estimated (using random effects modelling) to be 8.1% (95% CI 6.9%–9.4%) among the 60,571 participants included in all the studies (see Figure 2 for forest plot). Pooled seroprevalence estimates varied across WHO regions, with the highest rates observed in the African region (48.2%, 95% CI 39.2%–57.3%), followed by the European region (10.3%, 95% CI 8.0%–12.5%), the Region of the Americas (8.4%, 95% CI 6.0%–10.7%), the South‐East Asia region (3.0%, 95% CI 0.00%–6.5%) and the lowest rates in the Western Pacific region (0.5%, 95% CI 0.0%–1.0%). Overall statistical heterogeneity was obvious from the forest plots and supported by the high I2 statistic (99%). Pooled estimates were unable to be calculated in the Eastern Mediterranean region due to insufficient studies (n = 1). Only two regions (European region and the Region of the Americas) met the minimum number of studies (n > 10) required for testing of funnel plot asymmetry. Funnel plots and associated p values from Egger's test are presented in the Appendices 1 and 2.
FIGURE 2.
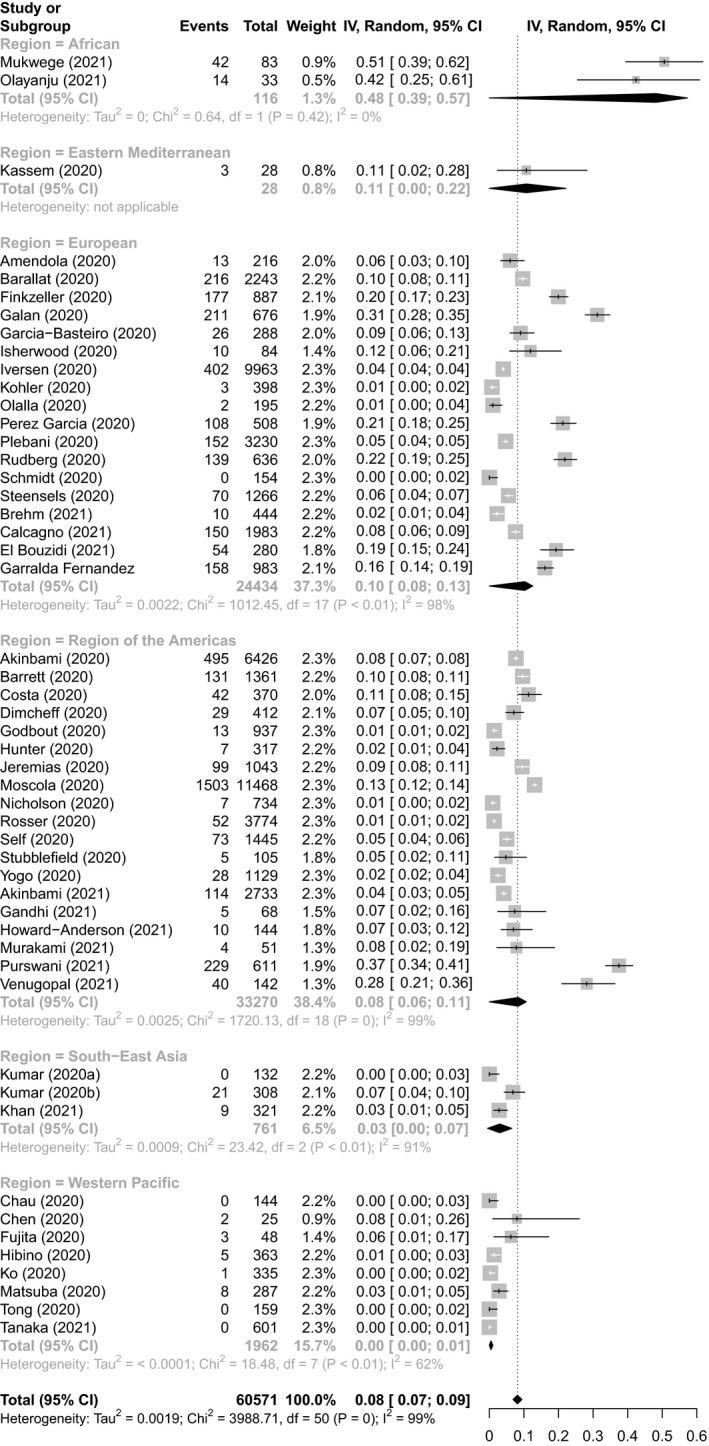
Seroprevalence of SARS‐COV‐2 antibodies among nurses stratified into WHO regions
4. DISCUSSION
Our study found that the pooled seroprevalence of SARS‐CoV‐2 antibodies among nurses was 8.1%, ranging from 0% to 51% between studies. Within the growing body of literature investigating the prevalence of SARS‐COV‐2 among healthcare workers, it is important to determine whether certain occupations experience higher rates of infection. A recent systematic review reported that nurses accounted for almost half of their positive cases, suggesting it could be attributed to their prolonged exposure to patients when delivering care (Gómez‐Ochoa et al., 2020).
Our results are congruent with rates reported in healthcare workers as a whole, with 7% and 8.7% in reviews conducted by Gómez‐Ochoa et al. (2020) and Galanis et al. (2021), respectively. These findings seem to suggest that despite differences in roles, the likelihood of infection for nurses is similar to other healthcare workers. Given nurses make up around 50% of the health workforce, the high proportion of SARS‐CoV‐2 positive nurses seen in previous studies may simply be due to overrepresentation (Bandyopadhyay et al., 2020; Gómez‐Ochoa et al., 2020). Any similarities in seroprevalence between professions could also be a result of mandated personal protective equipment (PPE) use and compliance with social distancing measures, both of which have been shown to reduce the risk of COVID‐19 infection in healthcare workers (Feng et al., 2020; Lewnard & Lo, 2020; Nguyen et al., 2020). Instead, any variance in this population may be due to the clinical specialty the workers operate in, that may influence the level of occupational exposure to COVID‐19 patients. Our study lacked the data to compare seroprevalence among different specialty areas. However, a recent systematic review by Chen et al. (2021) found that high‐risk healthcare workers experienced significantly higher seroprevalence than low‐risk healthcare workers. It is important to note there are potential confounding variables influencing these results, as the authors categorised high‐risk healthcare workers as personnel in contact with COVID‐19 patients and those with inadequate access to PPE.
We found seropositivity varied among countries, with those in the Western Pacific Region registering the lowest estimates. None of the studies included in the review could guarantee whether infections were a result of nosocomial or community transmission. Our results bared resemblance to seroprevalence estimates among the general population by Chen et al. (2021): Overall (8.1% compared to 8%); Western Pacific region (0.5% compared to 1.6%); and the Region of the Americas (8.4% compared to 6.8%), although the European estimates differed greatly (10.3% compared to 4.7%). Indeed, working in high‐risk areas of the hospital would compound the risk of infection, but it would seem community transmission still has an important influence in determining seroprevalence among nurses.
Though there were only two studies from the African region, the pooled seroprevalence of 48.2% among nursing staff was still considerably higher than other WHO regions. It has previously been reported that rates of hospital‐acquired infections (HAIs) are higher in developing countries compared to those observed in Europe and the United States of America (Allegranzi et al., 2011; Harrison et al., 2015). Potential contributing factors could include poor health infrastructure, inadequate access to resources and limited application of infection control measures (Allegranzi et al., 2011; Ogunsola & Mehtar, 2020). Be that as it may, a recent publication suggested the preparedness of African countries to manage COVID‐19 was underestimated, when one considers recent work undertaken with the Ebola outbreak of the mid‐2010s (Kapata et al., 2020). Kapata et al. (2020) also highlighted that early recognition of the risk of COVID‐19, and assistance from WHO had may somewhat mitigate African nations to widespread and potentially uncontrollable disease. It is difficult to assess whether such preparations have had an effect on seroprevalence among African countries, given the lack of studies and reported data within this region.
4.1. Strengths and limitations
To the authors’ knowledge, this is the first systematic review that specifically investigates the seroprevalence of SARS‐CoV‐2 among nurses. A potential limitation to this meta‐analysis, as with any systematic review of literature, is that studies reporting results in contrast to the included studies may have been missed. To mitigate this potential problem, we have undertaken an extensive electronic search. A further limitation may be selection bias due to the majority of studies failing to provide the characteristics of non‐responders to compare against. Some studies were able to limit the impact of bias by having a high response rate. It is also worth noting that the majority of studies were conducted in the Americas or Europe, settings where there was adequate access to PPE. Secondly, there was high heterogeneity among the studies. This was mitigated to the best of our ability by utilising a random effects model and sub‐group analysis when reporting results. However, even within WHO region, infection rates of COVD‐19 can differ by country, state or city. It was not feasible to stratify by regions other than WHO regions or continent, as there would have been a lack of studies to compare against certain areas. The region‐specific seroprevalence estimates should be interpreted with caution, as they may not be representative of all countries or states involved. There was also a lack of data in certain WHO regions, namely the Eastern Mediterranean Region, South‐East Asia region and the African region where resources are lower. More prevalence studies need to be conducted in these areas in order to properly estimate the overall seroprevalence of SARS‐CoV‐2 antibodies in the population. Lastly, we were limited in our ability to analyse potential factors influencing seroprevalence variability. Given the majority of studies looked at healthcare workers as a whole, we were unable to isolate certain demographic identifiers within the nursing sample. There were also various immunoassays used. Though the majority of tests proclaimed sensitivity and specificity >90%, variance may still have affected rates of infection. Moreover, there was not specific information available concerning local infection control practices.
5. CONCLUSION
To conclude, the overall seroprevalence of SARS‐CoV‐2 antibodies in nurses is comparable to other healthcare workers, and possibly the general population depending on the setting. Early adoption and adherence to PPE and social distancing measures could explain these similarities, meaning the majority of staff could be contracting the virus through community transmission and not in a healthcare setting. More research is needed to investigate whether this observation is valid, given the mixed evidence currently available.
6. RELEVANCE TO CLINICAL PRACTICE
The COVID‐19 pandemic has identified a range of vulnerabilities across society and also in healthcare settings. The availability and access to PPE and training in infection control practices have been major factors in protecting healthcare workers (Jackson et al., 2020). Workforce shortages and limited PPE have demonstrated the vulnerability of the aged care sector and reflected in high mortality (Davidson & Szanton, 2020). Fear and uncertainty have also been features of the pandemic including among nurses (Davidson et al., 2020). This meta‐analysis should provide some comfort to nurses that risks are similar to community exposure when adequate PPE is available and there is adherence to infection control measures.
The global pandemic has challenged traditional models of occupational health and safety as well as challenging standards of reporting and monitoring. Standardising methods of monitoring occupational exposure are important in ensuring protection for health workers (Jackson et al., 2020). Given the evolution of SARS‐CoV‐2 virus and vaccination strategies, ongoing monitoring and assessment of seroprevalence are necessary.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTION
Data curation, formal analysis, investigation, methodology, project administration, software, writing—original draft and writing—review and editing: Steven He; Conceptualisation and writing—review and editing: Anthony Hecimovic and Vesna Matijasevic; Formal analysis, investigation, project administration, and writing—review and editing: Ha Thi Mai; Investigation, methodology, resources, software, and writing—review and editing: Linda Heslop; Methodology and writing—review and editing: Jann Foster; Writing—review and editing: Kate Alexander, Naru Pal, and Patricia M. Davidson; Supervision and writing—review and editing: Evan Alexandrou; Conceptualisation, formal analysis, methodology, software, supervision, validation, visualisation, writing—original draft and writing—review and editing: Steven A. Frost.
Supporting information
File S1
APPENDIX 1.
Funnel plot inspecting publication bias of seroprevalence estimates from studies in the Region of the Americas
APPENDIX 2.
Funnel plot inspecting publication bias of seroprevalence estimates from studies in the European region
He, S. , Hecimovic, A. , Matijasevic, V. , Mai, H. T. , Heslop, L. , Foster, J. , Alexander, K. , Pal, N. , Alexandrou, E. , Davidson, P. M. , & Frost, S. A. (2022). Prevalence of SARS‐CoV‐2 antibodies among nurses: A systematic review and meta‐analysis. Journal of Clinical Nursing, 31, 1557–1569. 10.1111/jocn.16009
REFERENCES
- Akinbami, L. J. , Chan, P. A. , Vuong, N. , Sami, S. , Lewis, D. , Sheridan, P. E. , Lukacs, S. L. , Mackey, L. , Grohskopf, L. A. , Patel, A. , & Petersen, L. R. (2021). Severe acute respiratory syndrome coronavirus 2 seropositivity among healthcare personnel in hospitals and nursing homes, Rhode Island, USA, July–August 2020. Emerging Infectious Diseases, 27(3), 823–834. 10.3201/eid2703.204508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami, L. J. , Vuong, N. , Petersen, L. R. , Sami, S. , Patel, A. , Lukacs, S. L. , Mackey, L. , Grohskopf, A. S. , & Atas, J. (2020). SARS‐CoV‐2 seroprevalence among healthcare, first response, and public safety personnel, Detroit Metropolitan Area, Michigan, USA, May–June 2020. Emerging Infectious Diseases, 26(12), 2863–2871. 10.3201/eid2612.20376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allegranzi, B. M. D. , Nejad, S. B. M. D. , Combescure, C. P. , Graafmans, W. P. , Attar, H. P. , Donaldson, L. M. D. , & Pittet, D. P. (2011). Burden of endemic health‐care‐associated infection in developing countries: systematic review and meta‐analysis. The Lancet, 377(9761), 228–241. 10.1016/S0140-6736(10)61458-4 [DOI] [PubMed] [Google Scholar]
- Amendola, A. , Tanzi, E. , Folgori, L. , Barcellini, L. , Bianchi, S. , Gori, M. , Cammi, G. , Albani, E. , & Zuccotti, G. V. (2020). Low seroprevalence of SARS‐CoV‐2 infection among healthcare workers of the largest children hospital in Milan during the pandemic wave. Infection Control & Hospital Epidemiology, 41(12), 1468–1469. 10.1017/ice.2020.401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay, S. , Baticulon, R. E. , Kadhum, M. , Alser, M. , Ojuka, D. K. , Badereddin, Y. , Kamath, A. , Parepalli, S. A. , Brown, G. , Iharchane, S. , Gandino, S. , Markovic‐Obiago, Z. , Scott, S. , Manirambona, E. , Machhada, A. , Aggarwal, A. , Benazaize, L. , Ibrahim, M. , Kim, D. , … Khundkar, R. (2020). Infection and mortality of healthcare workers worldwide from COVID‐19: A systematic review. BMJ Global Health, 5(12), e003097. 10.1136/bmjgh-2020-003097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barallat, J. , Fernández‐Rivas, G. , Quirant‐Sánchez, B. , González, V. , Doladé, M. , Martinez‐Caceres, E. , Piña, M. , Matllo, J. , Estrada, O. , & Blanco, I. (2020). Seroprevalence of SARS‐CoV‐2 IgG specific antibodies among healthcare workers in the Northern Metropolitan Area of Barcelona, Spain, after the first pandemic wave. PLoS One, 15(12), e0244348. 10.1371/journal.pone.0244348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendregt, J. J. , Doi, S. A. , Lee, Y. Y. , Norman, R. E. , & Vos, T. (2013). Meta‐analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–978. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- Barrett, E. S. , Horton, D. B. , Roy, J. , Xia, W. , Greenberg, P. , Andrews, T. , Gennaro, M. L. , Parmar, V. , Russell, W. D. , Reilly, N. , Uprety, P. , Gantner, J. J. , Stockman, L. , Trooskin, S. Z. , Blaser, M. J. , Carson, J. L. , & Panettieri, R. A. (2020). Risk factors for severe acute respiratory syndrome coronavirus 2 infection in hospital workers: Results from a screening study in New Jersey, United States in spring 2020. Open Forum Infectious Diseases, 7(12). 1–9. 10.1093/ofid/ofaa534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges Migliavaca, C. , Stein, C. , Colpani, V. , Barker, T. H. , Munn, Z. , Falavigna, M. , & on behalf of the Prevalence Estimates Reviews – Systematic Review Methodology, G. (2020). How are systematic reviews of prevalence conducted? A methodological study. BMC Medical Research Methodology, 20(1), 96. 10.1186/s12874-020-00975-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehm, T. T. , Schwinge, D. , Lampalzer, S. , Schlicker, V. , Küchen, J. , Thompson, M. , Ullrich, F. , Huber, S. , Schmiedel, S. , Addo, M. M. , Lütgehetmann, M. , Knobloch, J. K. , Schulze zur Wiesch, J. , & Lohse, A. W. (2021). Seroprevalence of SARS‐CoV‐2 antibodies among hospital workers in a German tertiary care center: A sequential follow‐up study. International Journal of Hygiene and Environmental Health, 232, 113671. 10.1016/j.ijheh.2020.113671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calcagno, A. , Ghisetti, V. , Emanuele, T. , Trunfio, M. , Faraoni, S. , Boglione, L. , Burdino, E. , Audagnotto, S. , Lipani, F. , Nigra, M. , D’Avolio, A. , Bonora, S. , & Di Perri, G. (2021). Risk for SARS‐CoV‐2 infection in healthcare workers, Turin, Italy. Emerging Infectious Diseases, 27(1), 303–305. 10.3201/eid2701.203027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau, N. V. V. , Toan, L. M. , Man, D. N. H. , Thao, H. P. , Lan, N. P. H. , Ty, D. T. B. , Hieu, D. K. , Tien, N. T. M. , Ngoc, N. M. , Hung, L. M. , Dung, N. T. , Thanh, T. T. , Truong, N. T. , Thwaites, G. , & Tan, L. V. (2021). Absence of SARS‐CoV‐2 antibodies in health care workers of a tertiary referral hospital for COVID‐19 in southern Vietnam. The Journal of Infection, 82(1), e36–e37. 10.1016/j.jinf.2020.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, X. , Chen, Z. , Azman, A. S. , Deng, X. , Sun, R. , Zhao, Z. , Zheng, N. , Chen, X. , Lu, W. , Zhuang, T. , Yang, J. , Viboud, C. , Ajelli, M. , Leung, D. T. , & Yu, H. (2021). Serological evidence of human infection with SARS‐CoV‐2: A systematic review and meta‐analysis. The Lancet Global Health, 9(5), e598–e609. 10.1016/S2214-109X(21)00026-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , Tong, X. , Wang, J. , Huang, W. , Yin, S. , Huang, R. , Yang, H. , Chen, Y. , Huang, A. , Liu, Y. , Chen, Y. , Yuan, L. , Yan, X. , Shen, H. , & Wu, C. (2020). High SARS‐CoV‐2 antibody prevalence among healthcare workers exposed to COVID‐19 patients. Journal of Infection, 81(3), 420–426. 10.1016/j.jinf.2020.05.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, S. F. , Giavina‐Bianchi, P. , Buss, L. , Mesquita Peres, C. H. , Rafael, M. M. , dos Santos, L. G. N. , Bedin, A. A. , Francisco, M. C. P. B. , Satakie, F. M. , Jesus Menezes, M. A. , Dal Secco, L. M. , Rodrigues Caron, D. M. , de Oliveira, A. B. , de Faria, M. F. L. , de Aurélio Penteado, A. S. , de Souza, I. O. M. , de Fatima Pereira, G. , Pereira, R. , Matos Porto, A. P. , … Levin, A. S. (2020). Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) seroprevalence and risk factors among oligo/asymptomatic healthcare workers: Estimating the impact of community transmission. Clinical Infectious Diseases. 1–5. 10.1093/cid/ciaa1845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, P. M. , Padula, W. V. , Daly, J. , & Jackson, D. (2020). Moral outrage in COVID19—Understandable but not a strategy. Journal of Clinical Nursing, 29(19–20), 3600–3602. 10.1111/jocn.15318 [DOI] [PubMed] [Google Scholar]
- Davidson, P. M. , & Szanton, S. L. (2020). Nursing homes and COVID‐19: We can and should do better. Journal of Clinical Nursing, 29(15–16), 2758–2759. 10.1111/jocn.15297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimcheff, D. E. , Schildhouse, R. J. , Hausman, M. S. , Vincent, B. M. , Markovitz, E. , Chensue, S. W. , Deng, J. , McLeod, M. , Hagan, D. , Russell, J. , & Bradley, S. F. (2021). Seroprevalence of Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2) infection among VA healthcare system employees suggests higher risk of infection when exposed to SARS‐CoV‐2 outside of the work environment. Infection Control & Hospital Epidemiology, 42(4), 392–398. 10.1017/ice.2020.1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger, M. , Smith, G. D. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Bouzidi, K. , Pirani, T. , Rosadas, C. , Ijaz, S. , Pearn, M. , Chaudhry, S. , Patel, S. , Sureda‐Vives, M. , Fernandez, N. , Khan, M. , Cherepanov, P. , McClure, M. O. , Tedder, R. S. , & Zuckerman, M. (2021). Severe acute respiratory syndrome coronavirus‐2 infections in critical care staff: Beware the risks beyond the bedside. Critical Care Medicine, 49(3), 428–436. 10.1097/CCM.0000000000004878 [DOI] [PubMed] [Google Scholar]
- Feng, S. , Shen, C. , Xia, N. , Song, W. , Fan, M. , & Cowling, B. J. (2020). Rational use of face masks in the COVID‐19 pandemic. The Lancet Respiratory Medicine, 8(5), 434–436. 10.1016/S2213-2600(20)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkenzeller, T. , Faltlhauser, A. , Dietl, K. H. , Paetzel, C. , Szczypien, N. , Klawonn, F. , Bodmann, K. F. , & von Meyer, A. (2020). [SARS‐CoV‐2 antibodies in ICU and clinic staff: From Germany's region with the highest infection rate]. SARS‐CoV‐2‐Antikorper bei Intensiv‐ und Klinikpersonal: Aus der am hochsten durchseuchten Region Deutschlands. Medizinische Klinik, Intensivmedizin Und Notfallmedizin, 115(Suppl 3), 139–145. 10.1007/s00063-020-00761-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujita, K. , Kada, S. , Kanai, O. , Hata, H. , Odagaki, T. , Satoh‐Asahara, N. , Tagami, T. , & Yasoda, A. (2020). Quantitative SARS‐CoV‐2 antibody screening of healthcare workers in the southern part of Kyoto City during the COVID‐19 pre‐pandemic period [Original Research]. Frontiers Public Health, 8(895), 1–7. 10.3389/fpubh.2020.595348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galán, M. I. , Velasco, M. , Casas, M. L. , Goyanes, M. J. , Rodríguez‐Caravaca, G. , Losa‐García, J. E. , Noguera, C. , Castilla, V. , Weber, A. , Punter, A. , Carlos, J. , Salazar, A. , Teresa, M. , Zafra, B. , Gregorio, B. C. , Mercedes, M. , Pulido, C. , Camilo, D. C. , Isabel, A. , … Esther, M. (2020). Hospital‐Wide SARS‐CoV‐2 seroprevalence in health care workers in a Spanish teaching hospital. Enfermedades Infecciosas Y Microbiología Clínica. 1–8. 10.1016/j.eimc.2020.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2021). Seroprevalence of SARS‐CoV‐2 antibodies and associated factors in healthcare workers: A systematic review and meta‐analysis. The Journal of Hospital Infection, 108, 120–134. 10.1016/j.jhin.2020.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi, S. , Winn, C. C. , Ianosi‐Irimie, M. , Edmonston, T. B. , Nahra, R. , & Roberts, B. W. (2021). COVID‐19 serologic testing among the highest risk healthcare workers. Journal of General Internal Medicine, 36(4), 1164–1165. 10.1007/s11606-020-06462-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia‐Basteiro, A. L. , Moncunill, G. , Tortajada, M. , Vidal, M. , Guinovart, C. , Jimenez, A. , Santano, R. , Sanz, S. , Mendez, S. , Llupia, A. , Aguilar, R. , Alonso, S. , Barrios, D. , Carolis, C. , Cistero, P. , Choliz, E. , Cruz, A. , Fochs, S. , Jairoce, C. , … Dobano, C. (2020). Seroprevalence of antibodies against SARS‐CoV‐2 among health care workers in a large Spanish reference hospital. Nature Communications, 11(1), 3500. 10.1038/s41467-020-17318-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garralda Fernandez, J. , Molero Vilches, I. , Bermejo Rodriguez, A. , Cano Torres, I. , Colino Romay, E. I. , Garcia Arata, I. , Jaqueti Aroca, J. , Lillo Rodriguez, R. , Lopez Lacomba, D. , Mazon Cuadrado, L. , Molina Esteban, L. , Morales Garcia, L. J. , Moratilla Monzo, L. , Nieto‐Borrajo, E. , Pacheco Delgado, M. , Prieto Menchero, S. , Sanchez Hernandez, C. , Sanchez Testillano, E. , & Garcia‐Martinez, J. (2021). Impact of SARS‐CoV‐2 pandemic among health care workers in a secondary teaching hospital in Spain. PLoS One, 16(1), e0245001. 10.1371/journal.pone.0245001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godbout, E. J. , Pryor, R. , Harmon, M. , Montpetit, A. , Greer, J. , Bachmann, L. M. , Doll, M. , Stevens, M. P. , & Bearman, G. (2020). Severe acute respiratory coronavirus virus 2 (SARS‐CoV‐2) seroprevalence among healthcare workers in a low prevalence region. Infection Control and Hospital Epidemiology, 1–3. 10.1017/ice.2020.1374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez‐Ochoa, S. A. , Franco, O. H. , Rojas, L. Z. , Raguindin, P. F. , Roa‐Díaz, Z. M. , Wyssmann, B. M. , Guevara, S. L. R. , Echeverría, L. E. , Glisic, M. , & Muka, T. (2020). COVID‐19 in health‐care workers: A living systematic review and meta‐analysis of prevalence, risk factors, clinical characteristics, and outcomes. American Journal of Epidemiology, 190(1), 161–175. 10.1093/aje/kwaa191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, R. , Cohen, A. W. S. , & Walton, M. (2015). Patient safety and quality of care in developing countries in Southeast Asia: A systematic literature review. International Journal for Quality in Health Care, 27(4), 240–254. 10.1093/intqhc/mzv041 [DOI] [PubMed] [Google Scholar]
- Hibino, M. , Iwabuchi, S. , & Munakata, H. (2021). SARS‐CoV‐2 IgG seroprevalence among medical staff in a general hospital that treated patients with COVID‐19 in Japan: Retrospective evaluation of nosocomial infection control. The Journal of Hospital Infection, 107, 103–104. 10.1016/j.jhin.2020.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard‐Anderson, J. , Adams, C. , Sherman, A. C. , Dube, W. C. , Smith, T. C. , Edupuganti, N. , Chea, N. , Magill, S. S. , Espinoza, D. O. , Zhu, Y. , Phadke, V. K. , Edupuganti, S. , Steinberg, J. P. , Lopman, B. A. , Jacob, J. T. , Collins, M. H. , & Fridkin, S. K. (2021). Occupational risk factors for SARS‐CoV‐2 infection among healthcare personnel: A cross‐sectional analysis of subjects enrolled in the COPE study. Infection Control and Hospital Epidemiology, 1–6. 10.1017/ice.2021.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter, B. R. , Dbeibo, L. , Weaver, C. S. , Beeler, C. , Saysana, M. , Zimmerman, M. K. , & Weaver, L. (2020). Seroprevalence of severe acute respiratory coronavirus virus 2 (SARS‐CoV‐2) antibodies among healthcare workers with differing levels of coronavirus disease 2019 (COVID‐19) patient exposure. Infection Control & Hospital Epidemiology, 41(12), 1441–1442. 10.1017/ice.2020.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter, E. , Price, D. A. , Murphy, E. , van der Loeff, I. S. , Baker, K. F. , Lendrem, D. , Lendrem, C. , Schmid, M. L. , Pareja‐Cebrian, L. , Welch, A. , Payne, B. A. I. , & Duncan, C. J. A. (2020). First experience of COVID‐19 screening of health‐care workers in England. The Lancet, 395(10234), e77–e78. 10.1016/S0140-6736(20)30970-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isherwood, J. , Winyard, J. , Karki, B. , Chung, W. Y. , Layton, G. , Issa, E. , Garcea, G. , & Dennison, A. R. (2020). Prevalence of SARS‐COVID‐19 serum IgG antibodies amongst staff on an acute surgical unit. British Journal of Surgery, 107(12), e576–e577. 10.1002/bjs.11976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen, K. , Bundgaard, H. , Hasselbalch, R. B. , Kristensen, J. H. , Nielsen, P. B. , Pries‐Heje, M. , Knudsen, A. D. , Christensen, C. E. , Fogh, K. , Norsk, J. B. , Andersen, O. , Fischer, T. K. , Jensen, C. A. J. , Larsen, M. , Torp‐Pedersen, C. , Rungby, J. , Ditlev, S. B. , Hageman, I. , Mogelvang, R. , … Ullum, H. (2020). Risk of COVID‐19 in health‐care workers in Denmark: An observational cohort study. The Lancet Infectious Diseases, 20(12), 1401–1408. 10.1016/S1473-3099(20)30589-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson, D. , Anders, R. , Padula, W. V. , Daly, J. , & Davidson, P. M. (2020). Vulnerability of nurse and physicians with COVID‐19: Monitoring and surveillance needed. Journal of Clinical Nursing, 29(19–20), 3584–3587. 10.1111/jocn.15347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeremias, A. , Nguyen, J. , Levine, J. , Pollack, S. , Engellenner, W. , Thakore, A. , & Lucore, C. (2020). Prevalence of SARS‐CoV‐2 infection among health care workers in a tertiary community hospital. JAMA Internal Medicine, 180(12), 1707. 10.1001/jamainternmed.2020.4214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapata, N. , Ihekweazu, C. , Ntoumi, F. , Raji, T. , Chanda‐Kapata, P. , Mwaba, P. , Mukonka, V. , Bates, M. , Tembo, J. , Corman, V. , Mfinanga, S. , Asogun, D. , Elton, L. , Arruda, L. B. , Thomason, M. J. , Mboera, L. , Yavlinsky, A. , Haider, N. , Simons, D. , … Zumla, A. (2020). Is Africa prepared for tackling the COVID‐19 (SARS‐CoV‐2) epidemic. Lessons from past outbreaks, ongoing pan‐African public health efforts, and implications for the future. International Journal of Infectious Diseases, 93, 233–236. 10.1016/j.ijid.2020.02.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassem, A. M. , Talaat, H. , Shawky, S. , Fouad, R. , Amer, K. , Elnagdy, T. , Hassan, W. A. , Tantawi, O. , Abdelmoniem, R. , Gaber, Y. , Badary, H. A. , & Musa, S. (2020). SARS‐CoV‐2 infection among healthcare workers of a gastroenterological service in a tertiary care facility. Arab Journal of Gastroenterology, 21(3), 151–155. 10.1016/j.ajg.2020.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, M. S. , Haq, I. , Qurieshi, M. A. , Majid, S. , Bhat, A. A. , Qazi, T. B. , Chowdri, I. N. , Sabah, I. , Kawoosa, M. F. , Lone, A. A. , Nabi, S. , Sumji, I. A. , Obaid, M. , & Kousar, R. (2021). SARS‐CoV‐2 seroprevalence among healthcare workers by workplace exposure risk in Kashmir. India. Journal of Hospital Medicine, 16(5), 274–281. 10.12788/jhm.3609 [DOI] [PubMed] [Google Scholar]
- Ko, J.‐H. , Lee, J. Y. , Kim, H. A. , Kang, S.‐J. , Baek, J. Y. , Park, S.‐J. , Hyun, M. , Jo, I. J. , Chung, C. R. , Kim, Y.‐J. , Kang, E.‐S. , Choi, Y. K. , Chang, H.‐H. , Jung, S. I. , & Peck, K. R. (2020). Serologic evaluation of healthcare workers caring for COVID‐19 patients in the Republic of Korea [Perspective]. Frontiers in Microbiology, 11(2935), 1–6. 10.3389/fmicb.2020.587613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler, P. P. , Kahlert, C. R. , Sumer, J. , Flury, D. , Güsewell, S. , Leal‐Neto, O. B. , Notter, J. , Albrich, W. C. , Babouee Flury, B. , McGeer, A. , Kuster, S. , Risch, L. , Schlegel, M. , & Vernazza, P. (2020). Prevalence of SARS‐CoV‐2 antibodies among Swiss hospital workers: Results of a prospective cohort study. Infection Control and Hospital Epidemiology, 42(5), 604–608. 10.1017/ice.2020.1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, A. , Sathyapalan, D. , Ramachandran, A. , Subhash, K. , Biswas, L. , & Beena, K. V. (2020). SARS‐CoV‐2 antibodies in healthcare workers in a large university hospital, Kerala, India. Clinical Microbiology and Infection, 27(3), 481–483. 10.1016/j.cmi.2020.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, N. , Bhartiya, S. , Desai, S. , Mutha, A. , Beldar, A. , & Singh, T. (2020). Seroprevalence of antibodies against SARS‐CoV‐2 among health care workers in Mumbai, India. Asia Pacific Journal of Public Health, 33(1), 126–128. 10.1177/1010539520977307 [DOI] [PubMed] [Google Scholar]
- Lewnard, J. A. , & Lo, N. C. (2020). Scientific and ethical basis for social‐distancing interventions against COVID‐19. The Lancet Infectious Diseases, 20(6), 631–633. 10.1016/S1473-3099(20)30190-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuba, I. , Hatori, N. , Koido, N. , Watanabe, Y. , Ebara, F. , Matsuzawa, Y. , Nishikawa, T. , Kunishima, T. , Degawa, H. , Nishikawa, M. , Ono, Y. , & Kanamori, A. (2020). Survey of the current status of subclinical coronavirus disease 2019 (COVID‐19). Journal of Infection and Chemotherapy, 26(12), 1294–1300. 10.1016/j.jiac.2020.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra‐Hebert, A. D. , Jehi, L. , Ji, X. , Nowacki, A. S. , Gordon, S. , Terpeluk, P. , Chung, M. K. , Mehra, R. , Dell, K. M. , Pennell, N. , Hamilton, A. , Milinovich, A. , Kattan, M. W. , & Young, J. B. (2020). Impact of the COVID‐19 pandemic on healthcare workers’ risk of infection and outcomes in a large, integrated health system. Journal of General Internal Medicine, 35(11), 3293–3301. 10.1007/s11606-020-06171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moscola, J. , Sembajwe, G. , Jarrett, M. , Farber, B. , Chang, T. , McGinn, T. , Davidson, K. W. , & Consortium, f. t. N. H. C.‐R. (2020). Prevalence of SARS‐CoV‐2 antibodies in health care personnel in the New York City Area. JAMA, 324(9), 893–895. 10.1001/jama.2020.14765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukwege, D. , Byabene, A. K. , Akonkwa, E. M. , Dahma, H. , Dauby, N. , Cikwanine Buhendwa, J.‐P. , Le Coadou, A. , Montesinos, I. , Bruyneel, M. , Cadiere, G.‐B. , Vandenberg, O. , & Van Laethem, Y. (2021). High SARS‐CoV‐2 seroprevalence in healthcare workers in Bukavu, Eastern Democratic Republic of Congo. The American Journal of Tropical Medicine and Hygiene, 104(4), 1526–1530. 10.4269/ajtmh.20-1526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn, Z. , Moola, S. , Lisy, K. , Riitano, D. , & Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence‐Based Healthcare, 13(3), 147–153. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- Murakami, E. , Ghatak‐Roy, A. , Popova, M. , Gannon, C. , Park, D. E. , Villani, J. , Liu, C. , Toma, I. , & Lafleur, J. (2021). COVID‐19 infection among emergency department healthcare providers in a large tertiary academic medical center following the peak of the pandemic. American Journal of Emergency Medicine, 40, 27–31. 10.1016/j.ajem.2020.11.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen, L. H. , Drew, D. A. , Graham, M. S. , Joshi, A. D. , Guo, C.‐G. , Ma, W. , Mehta, R. S. , Warner, E. T. , Sikavi, D. R. , Lo, C.‐H. , Kwon, S. , Song, M. , Mucci, L. A. , Stampfer, M. J. , Willett, W. C. , Eliassen, A. H. , Hart, J. E. , Chavarro, J. E. , Rich‐Edwards, J. W. , … Zhang, F. (2020). Risk of COVID‐19 among front‐line health‐care workers and the general community: A prospective cohort study. The Lancet Public Health, 5(9), e475–e483. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson, L. , McLawhon, R. W. , Kurian, S. , Fitzgerald, R. L. , Case, J. , Marsh, C. , & Quigley, M. (2020). Healthcare worker seroconversion for SARS‐CoV‐2 at two large health systems in San Diego. American Journal of Infection Control, 49(4), 506–507. 10.1016/j.ajic.2020.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunsola, F. T. , & Mehtar, S. (2020). Challenges regarding the control of environmental sources of contamination in healthcare settings in low‐and middle‐income countries – A narrative review. Antimicrobial Resistance & Infection Control, 9(1), 81. 10.1186/s13756-020-00747-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olalla, J. , Correa, A. M. , Martín‐Escalante, M. D. , Hortas, M. L. , Martín‐Sendarrubias, M. J. , Fuentes, V. , Sena, G. , García‐Alegría, J. , & Group, T. R. (2020). Search for asymptomatic carriers of SARS‐CoV‐2 in healthcare workers during the pandemic: A Spanish experience. QJM: An International Journal of Medicine, 113(11), 794–798. 10.1093/qjmed/hcaa238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olayanju, O. , Bamidele, O. , Edem, F. , Eseile, B. , Amoo, A. , Nwaokenye, J. , Udeh, C. , Oluwole, G. , Odok, G. , & Awah, N. (2021). SARS‐CoV‐2 seropositivity in asymptomatic frontline health workers in Ibadan, Nigeria. American Journal of Tropical Medicine and Hygiene, 104(1), 91–94. 10.4269/ajtmh.20-1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo‐Wilson, E. , McDonald, S. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Journal of Clinical Epidemiology, 134, 178–189. 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- Pan, A. , Liu, L. , Wang, C. , Guo, H. , Hao, X. , Wang, Q. , Huang, J. , He, N. , Yu, H. , Lin, X. , Wei, S. , & Wu, T. (2020). Association of public health interventions with the epidemiology of the COVID‐19 outbreak in Wuhan, China. JAMA, 323(19), 1915–1923. 10.1001/jama.2020.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Garcia, F. , Perez‐Zapata, A. , Arcos, N. , De la Mata, M. , Ortiz, M. , Simon, E. , Hervas Fernandez, I. , Gonzalez Ventosa, V. , Munoz Monte, M. , Gonzalez Arroyo, J. , Perez‐Tanoira, R. , & Cuadros‐Gonzalez, J. (2020). SARS‐CoV‐2 infection among hospital workers of one of the most severely affected institutions in Madrid, Spain: A surveillance cross‐sectional study. Infection Control and Hospital Epidemiology, 42(7), 803–809, 10.1017/ice.2020.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plebani, M. , Padoan, A. , Fedeli, U. , Schievano, E. , Vecchiato, E. , Lippi, G. , Lo Cascio, G. , Porru, S. , & Palu, G. (2020). SARS‐CoV‐2 serosurvey in health care workers of the Veneto Region. Clinical Chemistry and Laboratory Medicine, 58(12), 2107–2111. 10.1515/cclm-2020-1236 [DOI] [PubMed] [Google Scholar]
- Purswani, M. U. , Bucciarelli, J. , Tiburcio, J. , Yagudayev, S. M. , Connell, G. H. , Omidiran, A. A. , Hannaway, L. , Zeana, C. , Healy, M. , Yu, G. , & Reich, D. (2021). SARS‐CoV‐2 seroprevalence among healthcare workers by job function and work location in a New York Inner‐City Hospital. Journal of Hospital Medicine, 16(5), 282–289. 10.12788/jhm.3627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quigley, A. L. , Stone, H. , Nguyen, P. Y. , Chughtai, A. A. , & MacIntyre, C. R. (2021). Estimating the burden of COVID‐19 on the Australian healthcare workers and health system during the first six months of the pandemic. International Journal of Nursing Studies, 114, 103811. 10.1016/j.ijnurstu.2020.103811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2017). R: A language and environment for statistical computing. In R Foundation for Statistical Computing. [Google Scholar]
- Rosser, J. I. , Roltgen, K. , Dymock, M. , Shepard, J. , Martin, A. , Hogan, C. A. , Blomkalns, A. , Mathew, R. , Parsonnet, J. , Pinsky, B. A. , Maldonado, Y. A. , Boyd, S. D. , Chang, S.‐I. , Holubar, M. , & Stanford Healthcare, C.‐W.‐R.‐G. (2020). Severe acute respiratory coronavirus virus 2 (SARS‐CoV‐2) seroprevalence in healthcare personnel in northern California early in the coronavirus disease 2019 (COVID‐19) pandemic. Infection Control and Hospital Epidemiology, 1–7. 10.1017/ice.2020.1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudberg, A.‐S. , Havervall, S. , Månberg, A. , Jernbom Falk, A. , Aguilera, K. , Ng, H. , Gabrielsson, L. , Salomonsson, A.‐C. , Hanke, L. , Murrell, B. , McInerney, G. , Olofsson, J. , Andersson, E. , Hellström, C. , Bayati, S. , Bergström, S. , Pin, E. , Sjöberg, R. , Tegel, H. , … Thålin, C. (2020). SARS‐CoV‐2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nature Communications, 11(1), 5064. 10.1038/s41467-020-18848-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, S. B. , Grüter, L. , Boltzmann, M. , & Rollnik, J. D. (2020). Prevalence of serum IgG antibodies against SARS‐CoV‐2 among clinic staff. PLoS One, 15(6), e0235417. 10.1371/journal.pone.0235417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider, S. , Brar, P. , Nouri‐Pasovsky, P. A. , Krüger, A. C. , Gastmeier, P. , & Aghdassi, S. J. S. (2020). SARS‐Coronavirus‐2 cases in healthcare workers may not regularly originate from patient care: Lessons from a university hospital on the underestimated risk of healthcare worker to healthcare worker transmission. Antimicrobial Resistance and Infection Control, 9, 1–7. 10.1186/s13756-020-00848-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self, W. H. , Tenforde, M. W. , Stubblefield, W. B. , Feldstein, L. R. , Steingrub, J. S. , Shapiro, N. I. , Ginde, A. A. , Prekker, M. E. , Brown, S. M. , Peltan, I. D. , Gong, M. N. , Aboodi, M. S. , Khan, A. , Exline, M. C. , Files, D. C. , Gibbs, K. W. , Lindsell, C. J. , Rice, T. W. , Jones, I. D. , … Network, I. V. Y. (2020). Seroprevalence of SARS‐CoV‐2 among frontline health care personnel in a multistate hospital network – 13 academic medical centers, April–June 2020. MMWR. Morbidity and Mortality Weekly Report, 69(35), 1221–1226. 10.15585/mmwr.mm6935e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steensels, D. , Oris, E. , Coninx, L. , Nuyens, D. , Delforge, M.‐L. , Vermeersch, P. , & Heylen, L. (2020). Hospital‐wide SARS‐CoV‐2 antibody screening in 3056 staff in a tertiary center in Belgium. JAMA, 324(2), 195–197. 10.1001/jama.2020.11160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubblefield, W. B. , Talbot, H. K. , Feldstein, L. R. , Tenforde, M. W. , Rasheed, M. A. U. , Mills, L. , Lester, S. N. , Freeman, B. , Thornburg, N. J. , Jones, I. D. , Ward, M. J. , Lindsell, C. J. , Baughman, A. , Halasa, N. , Grijalva, C. G. , Rice, T. W. , Patel, M. M. , Self, W. H. , & Investigators, f. t. I. V. E. i. t. C. I. (2020). Seroprevalence of SARS‐CoV‐2 among frontline healthcare personnel during the first month of caring for patients with COVID‐19—Nashville, Tennessee. Clinical Infectious Diseases, 72(9), 1645–1648. 10.1093/cid/ciaa936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka, A. , Yamamoto, S. , Miyo, K. , Mizoue, T. , Maeda, K. , Sugiura, W. , Mitsuya, H. , Sugiyama, H. , & Ohmagari, N. (2021). Seroprevalence of antibodies against SARS‐CoV‐2 in a large national hospital and affiliated facility in Tokyo, Japan. Journal of Infection, 82(4), e1–e3. 10.1016/j.jinf.2021.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, X. , Ning, M. , Huang, R. , Jia, B. , Yan, X. , Xiong, Y. , Wu, W. , Liu, J. , Chen, Y. , & Wu, C. (2020). Surveillance of SARS‐CoV‐2 infection among frontline health care workers in Wuhan during COVID‐19 outbreak. Immunity, Inflammation and Disease, 8(4), 840–843. 10.1002/iid3.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venugopal, U. , Jilani, N. , Rabah, S. , Shariff, M. A. , Jawed, M. , Mendez Batres, A. , Abubacker, M. , Menon, S. , Pillai, A. , Shabarek, N. , Kasubhai, M. , Dimitrov, V. , & Menon, V. (2021). SARS‐CoV‐2 seroprevalence among health care workers in a New York City hospital: A cross‐sectional analysis during the COVID‐19 pandemic. International Journal of Infectious Diseases, 102, 63–69. 10.1016/j.ijid.2020.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation . (2021). Weekly operational update on COVID‐19 – 19 April 2021 . https://www.who.int/publications/m/item/weekly‐operational‐update‐on‐covid‐19‐‐‐19‐april‐2021
- World Health Organization . (2020). Nursing and midwifery . https://www.who.int/news‐room/fact‐sheets/detail/nursing‐and‐midwifery
- Wu, Z. , & McGoogan, J. M. (2020). Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 323(13), 1239–1242. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- Yogo, N. , Greenwood, K. L. , Thompson, L. , Wells, P. J. , Munday, S. , Smith, T. C. , Smith, B. , & Bakhtar, O. R. (2020). Point prevalence survey to evaluate the seropositivity for coronavirus disease 2019 (COVID‐19) among high‐risk healthcare workers. Infection Control and Hospital Epidemiology, 1–6. 10.1017/ice.2020.1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1


