Abstract
Despite the SARS‐CoV‐2 pandemic not yet being under control, post‐Covid‐19 syndrome is already a challenging topic: long‐term multiorgan sequelae, although increasingly described, have not yet been systematized. As post‐Covid‐19 syndrome can significantly impact both the working capacity and the relationship life of surviving patients, we performed a systematic review of the evidence published over the last year and currently available in medical literature search databases (MEDLINE/Pubmed) and searching clinical trial registries, to evaluate the available evidence among workers. From 31 publications that initially matched inclusion criteria, 13 studies have been considered suitable for relevance and age of subjects. A wide range of patients (16%–87%) have post‐Covid syndrome; pneumological and neuropsychological symptoms were the most common disorders reported. The most frequent organic sequel found in post‐Covid patients was pulmonary fibrosis. The number of symptoms during acute SARS‐CoV‐2 infection, severity of the disease, and high serum levels of d‐dimer were related to high risk of post‐Covid syndrome. In conclusion, post‐Covid‐19 syndrome can significantly impact the health conditions of surviving patients. Rehabilitation and follow‐up in multidisciplinary rehabilitation programs should be considered for working‐age patients.
Keywords: Covid‐19, neuropsychological symptoms, pneumological symptoms, post‐Covid syndrome, SARS‐CoV, sequelae, systematic review, working age patients
1. INTRODUCTION
Recovery from Covid‐19 represents an emerging concern over the world, as growing evidence is showing a wide range of sequelae in patients who have returned to microbiological normalization after infection by SARS‐CoV‐2; in fact, even though most patients recover completely within a few weeks, some people, including those who had mild versions of the disease, after their initial recovery continue to experience symptoms called “long hauler” symptoms of Covid‐19 or post‐Covid syndrome. 1 , 2 , 3
The National Institute for Health and Care Excellence guideline on management of the long‐term effects of Covid‐19 published on October 30, 2020, 4 defines post‐Covid syndrome as signs and symptoms that develop during or following an infection consistent with Covid, which continue for more than 12 weeks and are not explained by an alternative diagnosis. Moreover, the guideline highlights that many people with post‐Covid syndrome can also experience generalized pain, fatigue, persisting high temperature, and psychiatric problems. In addition to the aforementioned post‐Covid syndrome, evidence is growing on the sequelae of Covid extending beyond 3 weeks from the onset of first symptoms, which are defined as post‐acute Covid. 5
Given that the post‐Covid syndrome and postacute Covid include persistent symptoms that could be related to residual inflammation (convalescent phase), organ damage, nonspecific effects from the hospitalization or prolonged ventilation (postintensive care syndrome), social isolation, or impact on preexisting health conditions, to date, we can not accurately predict who will become a long hauler patient. 6 , 7 As a recent article in Science notes, people only mildly affected by Covid still can have lingering symptoms, and people who were severely ill can be back to normal two months later. 8 Consistent with this remark, Italian researchers in follow‐up of 143 confirmed Covid patients—after the most severe symptoms had ended—found, 60 days after the onset of their illness, more than half of the patients continued to have multiple bothersome symptoms, and 41% reported a worsened quality of life. 9
Evidence from previous coronavirus‐related respiratory tract viral infection epidemics such as the SARS, which swept the world in 2002−2003, and middle east respiratory syndrome (MERS), which emerged in 2012, indicate the development of impairment of physical, mental, and social functioning brought about by respiratory compromise and deconditioning. 10 , 11 , 12 These patients presented multiple neurological complications such as neuropathy, myopathy, and generalized deconditioning, often associated with prolonged intensive care hospitalization; psychological and mood‐related effects following severe illness are also reported. 13 , 14
Given the current concern with the Covid pandemic, a summary of the evidence is required to allow policymakers to enact guidance for preventing and managing sequelae of the infection. In urgent circumstances such as the ongoing pandemic, rapid reviews are recommended by the WHO. 15 We conducted a review of the literature on post‐Covid syndrome and postacute Covid in patients aged 15–67 years and, therefore, considered in working age. The aim of the present systematic review was to assess both occurrence and risk factors for sequelae of Covid in patients who have returned to microbiological normalization after the infection by SARS‐CoV‐2.
2. MATERIALS AND METHODS
2.1. Search strategy
We conducted a systematic review of literature from February 2020 to January 31, 2021, regarding post‐Covid symptoms and/or signs in working‐age patients (aged 15–67 years) who recovered from the infection. The methods and selection criteria adopted were based on consultation of different sources. Initially, MEDLINE/Pubmed databases were used; afterward, the reference sections of the selected publications were scanned for additional relevant studies satisfying the adopted criteria. The keywords used to identify articles for this review were: “post‐Covid‐19 syndrome,” “postacute Covid‐19,” “long hauler Covid‐19,” “Covid‐19,” “SarsCoV‐2,” “occurrence,” and “prevalence.” The keywords were systematically combined to review the literature search. For example, “post‐Covid‐19 syndrome” and “occurrence” and “long hauler Covid‐19” were one of the adopted combinations. We aimed to identify original articles (i.e., nonreviews) using the abovementioned keywords with the following exclusion criteria: 1 not written in English; 2 studies focused on postinfection diseases not related to the COVID‐19 pandemic; and 3 qualitative studies.
2.2. Data extraction
The screening of articles was carried out in two phases. In the first phase, articles were screened based on title and abstract. The abstracts of all the selected titles were sorted for more detailed information. Two independent reviewers (G. d'E. and P. V.) read the abstracts and categorized them as relevant, not relevant, or possibly relevant. In the second phase, the full‐text articles were assessed for eligibility. Two reviewers (G. d'E. and P. V.) independently applied inclusion and exclusion criteria to potentially eligible papers, and both reviewers then independently extracted data from the original articles. Any disagreements were independently checked by a third reviewer (G. C.), and a consensus was reached.
2.3. Categorization of selected articles
Every full‐text article that met the inclusion criteria was reviewed and categorized based on its subject matter; this systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement.
2.4. Search for ongoing clinical trials
The ClinicalTrials. gov website, the European Union Clinical Trials Register, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use ‐ Good Clinical Practice Clinical Trials Registry, the Australian New Zealand Clinical Trial Registry, the Chinese Clinical Trial Registry, the Thai Clinical Trials Registry, the International Clinical Trials Registry Platform (ICTRP), the Cochrane Central Register of Controlled Trials were consulted online on March 2021 using the following keywords: “sequelae and Covid‐19,” “sequelae and SARS‐CoV‐2,” “post‐Covid‐19 syndrome,” “post‐acute Covid‐19,” “long hauler Covid‐19” (last updated on March 6, 2021).
3. RESULTS
3.1. Published studies
Our research of the two literature databases resulted in a total of 31 publications that matched our inclusion criteria. Eighteen of these were removed because they were deemed irrelevant (i.e., not concerning working‐age patients). Therefore, 13 papers remained in the study (Figure 1). Post‐Covid symptoms and/or signs were reported by a wide range of patients (between 16.36% and 87%); the most frequent symptoms were pneumological (continued shortness of breath, dyspnea, chest pain), and neuropsychological (muscle weakness, loss of smell, sleep difficulties, anxiety, depression, post‐traumatic stress disorder [PTSD]). The most frequent organic sequel found in post‐Covid patients was pulmonary fibrosis. The number of symptoms during Covid‐19, severity of Covid‐19 and high levels of d‐dimer resulted linked with high risk of post‐Covid syndrome and postacute Covid (Table 1).
Figure 1.
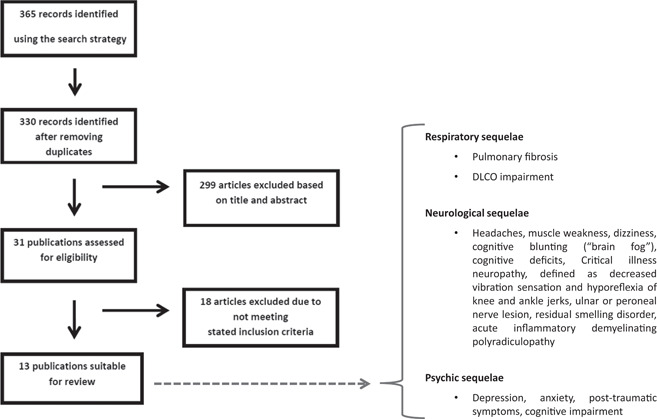
Flow chart of the search and selection process in the systematic review and main results
Table 1.
Post‐Covid syndrome in subjects aged 15–67 years
| Study | Study design and sample size | Study location | Lasting symptoms/signs or diseases following Covid‐19 and occurrence (%) | Follow up after symptom onset or after hospital discharge | Main findings |
|---|---|---|---|---|---|
| Huang et al. 16 | Longitudinal 1773 | China |
Fatigue or muscle weakness (63%), sleep difficulties, and anxiety or depression (26%) Lung diffusion impairment (up to 56% for severe Covid patients). In women, compared with men, was reported: |
Median follow‐up time after symptom onset: 186.0 (175.0–199.0) days | Increasingly impaired pulmonary diffusion capacities and abnormal chest imaging manifestations were reported in patients with a more severe illness |
| |||||
| |||||
| |||||
| Goërtz et al. 17 | Cross‐sectional 2159 | Netherlands and Belgium | Fatigue (87%), dyspnea (71%), chest tightness (44%), headache (38%) | 79 (SD ± 17) days after symptoms onset | The study excluded patients admitted to ICU. Number of symptoms during the infection was responsible for the largest unique contribution to post‐Covid syndrome (β = 0.58, p < 0.001). |
| Greenhalgh et al. 5 | Case report 1 | United Kingdom | Inability to exercise continued shortness of breath both motionless and when exerting, small waves of anxiety, considerable depression, continued loss of smell | 12 weeks after hospital admission | Indications for specialist assessment including clinical concern along with respiratory, cardiac, and neurological symptoms that are new, persistent, or progressive |
| Zhao et al. 18 | Retrospective multicenter cohort study 55 | China |
Gastrointestinal symptoms (30.91%), headache (18.18%), fatigue (16.36%), exertional dyspnea (14.55%) Residual abnormalities of pulmonary function (25.45%); diffusion reductions in DLCO (16.36%) |
3 months after discharge | The level of d‐dimer was found an important prognostic factor for abnormal DLCO. Thus, for patients who have marked raised d‐dimer, pulmonary rehabilitation should need subsequently even in the absence of severe respiratory symptoms |
| Raahimi et al. 19 | Case report 1 | United Kingdom | Guillain–Barré syndrome | 5 months after symptom onset | Hypothesis that it is the immune response to Covid‐19 and not the virus itself or the acute vascular changes that underly the pathophysiology of long Covid‐19 syndrome |
| Novak 20 | Case report 1 | United States | Orthostatic cerebral hypoperfusion syndrome (OCHOS) | >2 months after discharge | Indications for immunotherapy in patients with post‐Covid OCHOS |
| Walsh‐Messinger et al. 21 | Case‐control 43 (21 post‐Covid patients vs. 22 Covid‐recovered patients) | United States | Impaired concentration was the most frequently reported symptom (48%), followed by headache (38%), rhinitis (20%), exercise intolerance, dyspnea, sleep impairment, brain fog, appetite loss, fatigue, and chest pain | From 28 to 291 days after symptoms onset | 51% of participants were affected by post‐Covid syndrome; females were more vulnerable than males |
| Soh et al. 22 | Case report 1 | Japan | Posttraumatic stress disorder | 46 days after ICU discharge | Indications for establishing a follow‐up system for the long‐term outcomes of patients after ICU discharge |
| Yu et al. 23 | Retrospective 32 | China | Pulmonary fibrosis (43.7%) | 9 days after discharge | Fibrosis was more likely to develop in elderly patients with severe clinical conditions, especially in patients with high inflammatory indicators |
| You et al. 24 | Follow up 18 | China | Restrictive ventilatory defect (33.3% in severe cases), small function dysfunction (41.7% in nonsevere cases); pulmonary fibrosis (22.2%) | 40 ± 11.6 days in cases with nonsevere illness, and 34.7 ± 16.5 days in cases with severe illness | In Covid‐19 survivors after discharge, restrictive ventilatory defect and small function dysfunction can be persistent, which are not associated with disease severity |
| Alhiyar et al. 25 | Case report 1 | Qatar | Pulmonary fibrosis | 5 months after symptoms onset | Authors suggest doing a 6‐min walk test to assess exertional desaturation in patients who are fulfilling other discharge criteria for Covid‐19 pneumonia and acute respiratory distress syndrome |
| Tolba et al. 26 | Cross‐sectional 287 | Egypt | Fatigue (72.8%), anxiety (38%), joints pain (31.4%), continuous headache (28.9%), chest pain (28.9%), depression (28.6%), dyspnea (28.2%) | N/A | Severity of post‐Covid‐19 manifestations was related to the severity of Covid‐19 |
| Puchner et al. 27 | Cross‐sectional 23 | Austria | Impairment of pulmonary function (87%) neuropsychological dysfunction (85%) | Mean = 24 days, SD 5 days after discharge | Post‐acute multidisciplinary rehabilitation led to significant clinical and functional improvements in individuals who suffered from severe or critical Covid‐19 |
3.2. Ongoing studies
Eleven ongoing and enrolling clinical trials have been designed to investigate the Covid‐19 sequelae in working‐age patients: respiratory, cardiovascular, neurological, endocrine, ocular, and musculoskeletal sequelae are currently explored (Table 2).
Table 2.
Ongoing studies investigating Covid‐19 sequelae in working‐age patients (last updated on March 6, 2021)
| Types of sequelae | Title of the study–ClinicalTrials. gov Identifier | Methodology and sample size | Objectives of the study | Outcomes for sequelae |
|---|---|---|---|---|
| Respiratory | Follow‐up of Respiratory Sequelae of Hospitalized Patients With COVID‐19 (SISCOVID)—NCT04505631 | Study type: observational | To assess respiratory sequelae in hospitalized patients with severe Covid‐related pneumonia requiring oxygen supply and followed up for 6 months after hospital discharge | Primary: The presence of respiratory sequelae assessed by low‐dose thoracic TC |
| Estimated enrollment: 100 | Secondary: respiratory functional exploration and arterial gasometry evaluation at rest and after physical activity | |||
| Observational model: cohort | ||||
| Time perspective: prospective | ||||
| Medium and Long Term Follow‐up of COVID‐19 Infected Patients: Research and Characterization of Pulmonary Sequelae (COV‐RECUP)—NCT04519320 | Study type: intervention (clinical trial) | To assess respiratory sequelae in Covid‐19 survivors who have had a stay in intensive care and supported with respiratory assistance | Primary: proportion of patients with alteration of the capillary alveolus barrier at 12 months of follow‐up, characterized by a decrease of the diffusing capacity for carbon monoxide (DLCO) below the lower limit of normal | |
| Estimated enrollment: 140 | ||||
| Predicting the Progression to Chronic Fibrosis of Lung Lesions Related to Covid‐19 Infection From Chest CT Images (PREDISCAN)—NCT04483752 | Study type: intervention (clinical trial) | To assess: | Primary: description of the different types of lesions at 3 months | |
| Estimated enrollment: 100 |
|
Secondary: quantification of circulating antibodies and correlation between the level of immunization against SARS CoV2, the severity of the initial disease, and the existence or not of long‐term pulmonary sequelae at 3‐month follow up | ||
| Intervention model: single group assignment | ||||
| ||||
| Long‐term Evolution of Pulmonary Involvement of Novel SARS‐COV‐2 Infection (COVID‐19): Follow the Covid Study— NCT04605757 | Study type: observational | To assess: | Primary: Long‐term evolution of clinical involvement due to SARS‐COV‐2 pneumonia symptoms, respiratory rate, blood gas exchange parameters, pulmonary function tests, six minute walking test distance | |
| Estimated enrollment: 100 |
|
|||
| Observational model: cohort | ||||
| Secondary: identifying possible factors associated to the persistency of clinical, functional and radiological long‐term lung involvement due to Covid‐19 | ||||
| ||||
| Lung Function, Exercise Capacity and Health‐Related Quality of Life After Severe COVID‐19—NCT04410107 | Study type: observational | To assess the early and late effects of severe acute respiratory syndrome on lung function, exercise capacity, respiratory symptoms, and HRQoL in Covid‐19 survivors | Primary: forced expiratory volume in the first second/forced vital capacity, total lung capacity, lung diffusion capacity for carbon monoxide, 6‐min walk test distance at 6‐month follow‐up | |
| Estimated enrollment: 134 | ||||
| Observational model: cohort | ||||
| Secondary: comprehensive assessment of respiratory function at 12‐month follow up | ||||
| Time perspective: prospective | ||||
| Cardiovascular | Lung Function, Exercise Capacity and Health‐Related Quality of Life After Severe COVID‐19–NCT04661657 | Study type: observational (patient registry) | To assess factors associated with the development of cardiovascular conditions in Covid‐19 survivors using cardiovascular magnetic resonance and transthoracic echocardiography | Primary: evaluation of the percentage of myocardium demonstrating late gadolinium enhancement, extracellular Volume Fraction, left ventricular ejection fraction |
| Estimated enrollment: 70 | ||||
| Observational model: cohort | ||||
| Time perspective: prospective | ||||
| Neurological | The Norwegian Study of Nervous System Manifestations and Sequelae After COVID‐19 (NeuroCovid)–NCT04576351 | Study type: observational | To assess the burden of neurological, psychiatric, and psychological complications in Covid‐19 survivors and identify clinical characteristics and biomarkers for both short‐ and long‐term neurological treatment and rehabilitation | Primary: rate of neurological, psychiatric, and neuropsychological manifestations of Covid‐19 at 6 and 12 months follow‐up |
| Estimated enrollment: 150 | Secondary: rate of stroke, death, peripheral nervous affection, myopathy, brain MRI pathology, post‐Covid neurological, cognitive, or neuropsychiatric manifestations at 6 and 12 months follow up | |||
| Observational model: cohort | ||||
| Time perspective: prospective | ||||
| Neurological and Neuropsychological Sequelae of COVID‐19 Infection (NeNeSCo)–NCT04745611 | Study type: observational (patient registry) | The aim of this study is to fill these gaps in research through: | Primary: change in life participation (social, occupational, mobility), quality of life at 6–9 months and 12–15 months after hospital discharge | |
| Estimated enrollment: 400 | ||||
| Observational model: case only |
|
Presence of MRI abnormalities and neurological symptoms at 6–9 months and 12–15 months after hospital discharge | ||
| Time perspective: prospective | Presence of deficits in cognition, memory, visual attention and task switching, selective attention, cognitive flexibility, and processing speed, working memory, attention, and executive function at 6–9 months and 12–15 months after hospital discharge | |||
| Change in subjective cognitive complaints, depression/anxiety, posttraumatic stress symptoms, family burden, family quality of life at 6–9 months and 12–15 months after hospital discharge | ||||
| Secondary: MRI abnormalities such as cerebral microinfarctions/bleedings, and white matter hyperintensities at 6–9 months after hospital discharge | ||||
| Endocrine | Physiopathology and Sequelae of COVID‐19 Infection (SEQ‐COV‐PHYSIO)–NCT04563676 | Study type: intervention (clinical trial) | To assess the thyroid function (thyrotropic axis) as well as the corticotropic adrenal function in Covid‐19 survivors | Primary: cortisol and TSH levels at 3 months from hospitalization |
| Estimated enrollment: 400 | ||||
| Time perspective: screening | ||||
| Ocular | Ocular Sequelae of Patients Hospitalized for Respiratory Failure During the COVID‐19 Epidemic (SOCOVID)–NCT04387292 | Study type: intervention (clinical trial) | To assess ophthalmologic damages in Covid‐19 survivors | Primary: description of the ophthalmological problems observed 6 months after discharge of hospitalization |
| Estimated enrollment: 100 | ||||
| Musculoskeletal | Sarco‐COVID Study: Measuring the Loss of Skeletal Muscle Mass in the Hospitalized Patient With the Diagnosis of COVID‐19 (SARCO‐COVID)–NCT04780126 | Study type: observational (patient registry) | To evaluate sarcopenia in Covid‐19 survivors | Primary: quantify the loss of muscle mass in COVID‐19 patients after one month of hospitalization |
| Estimated enrollment: 64 | Secondary: analyze the clinical characteristics and the prevalence of sarcopenia, the thickness of the rectus femoris, vastus medialis, vastus lateralis, medial gastrocnemius, the correlation between C reactive protein and the presence of sarcopenia | |||
| Observational model: ecology and community | ||||
| Time perspective: prospective |
4. DISCUSSION
4.1. Respiratory sequelae
In our study, impairment of pulmonary function was the most focused issue; 10 of the 13 studies found persistence of respiratory sequelae, which consisted in a wide pattern of symptoms and/or signs as the following:
Breathlessness or dyspnea: 14.55% to 71% of patients recovered from Covid 19 suffered from such symptoms. The occurrence was positively related to old age, being hospitalized in the intensive care unit (ICU), and severity of Covid‐19. Interestingly, a study by Walsh‐Messinger et al. 21 showed persistent dyspnea in 43% of young students (mean age: 19.86 ± 3.03); this finding contradicts the perception that post‐COVID syndrome predominantly affects old adults.
4.1.1. Pulmonary fibrosis
Selected studies showed survivors from Covid incurring a significant risk for pulmonary fibrosis following Covid pneumonia and acute respiratory distress syndrome. The main independent variables related to fibrosis in such patients were ICU admission for Covid and old age. Patients affected by pulmonary fibrosis commonly complained of dry cough, fatigue, and dyspnea. The study by Yu et al. 23 revealed a higher level of C reactive protein and interleukin‐6 in patients with fibrosis compared to nonfibrosis patients (p < 0.050), leading to hypothesize that an increased inflammatory reaction might lead to the formation of pulmonary fibrosis during recovery. Given these findings, the authors concluded that such clinical parameters might contribute to predicting which patients with Covid pneumonia are at a higher risk of developing pulmonary fibrosis after discharge.
4.1.2. DLCO impairment
Two studies showed significant reductions in DLCO up to 3 months after discharge for Covid‐19. Abnormalities in DLCO are an indicator of a late phase in recovery or pulmonary fibrosis. In the past, follow‐up studies for the patients rehabilitating from SARS, showed that impaired lung function could last for months or even years. 28 , 29 d‐dimer elevation was reported as an important laboratory finding in Covid patients, which requires extra attention. Several studies have reported that d‐dimer on admission was the independent predictor of in‐hospital death for patients with Covid. 30 , 31 Consistent with these past findings, the study performed by Zhao et al. 18 revealed the level of d‐dimer was an important prognostic factor for abnormal DLCO. Thus, for patients who have marked raised d‐dimer, pulmonary rehabilitation is needed subsequently even in the absence of severe respiratory symptoms.
4.1.3. Neurological sequelae
The main common nonspecific neurological symptoms include headaches (up to 38%), muscle weakness, dizziness, and cognitive blunting (“brain fog”), which frequently co‐occur with fatigue and breathlessness, particularly in hospitalized patients. Interestingly, the study by Huang et al. 16 reported the medium‐term clinical follow‐up of a cohort of 1733 adult patients affected by Covid and discharged from one of the Wuhan Hospitals (China). Six months after illness onset, the authors found that over 50% of patients had residual chest imaging abnormalities and 76% of the patients reported persistent covid related clinical disorders; the most frequently reported symptoms were muscle weakness or fatigue (63%).
With regard to patients hospitalized in ICUs, the post‐ICU syndrome (PICS) was frequently found after invasive ventilation with prone position and encompassed ICU acquired weakness, cognitive deficits, and psychiatric abnormalities lasting many weeks after ICU discharge. The follow‐up study performed by Puchner et al. 27 found that 56.5% of patients discharged from ICU, required an additional neurological evaluation focused on neurological sequelae, 24 (SD ± 5) days after the discharge. In these patients, neurological examination revealed muscle weakness in 46%, which was associated with immobility or gait disturbances as well as restrictions on activities of daily living. Critical illness neuropathy, defined as decreased vibration sensation and hyporeflexia of knee and ankle jerks, was observed in 85% of the subjects. Additionally, ulnar or peroneal nerve lesion was found in 23%. A residual smelling disorder was present in only 4.3% of the patients. 27
Recently Raahimi et al. 19 reported a case of delayed onset, acute inflammatory demyelinating polyradiculopathy (AIDP) in a healthy young man previously affected by a severe SARS‐CoV‐2 infection: bilateral leg pain and loss of sensation in the feet was the main symptom reported. AIDP classically presents as a rapidly evolving, ascending, symmetrical, flaccid paralysis with loss or diminished tendon reflexes. Based on this finding, the authors claim that the case they have presented would support the hypothesis that it is the immune response to Covid and not the virus itself or the acute vascular changes that underlay the pathophysiology of post‐Covid syndrome.
4.2. Psychic sequelae
Five of the selected articles showed persistent psychiatric symptoms among Covid survivors, such as depression, anxiety, posttraumatic symptoms, and cognitive impairment; the study of Huang et al. 16 found anxiety or depression were common, even at 6 months after symptom onset in a cohort of 1773 patients discharged for Covid‐19; moreover, increased risk for depression or anxiety was found in women compared with men (OR: 1.80 [1.39–2.34]). To date, mental impairment after ICU care in working‐age patients with Covid has remained unreported. A recently published systematic review and meta‐analysis regarding psychiatric and neuropsychiatric presentations associated with severe coronavirus infections requiring ICU hospitalization, reported that the prevalence of depression, anxiety, PTSD, and fatigue might be high in these patients; however, to date, data on these diagnoses in patients with severe Covid are preliminary or unpublished. 32
5. CONCLUDING REMARKS
This review of the literature has some methodological limitations that should be highlighted, in particular: (1) currently systematic studies on the topic are still lacking and this can limit the quality of the observations, (2) psychiatric studies have been carried out in specific geographic areas and need to be confirmed by parallel studies obtained in other countries, in fact, the extensibility of the results obtained to other cultural contexts may not be directly accepted and may be influenced by peculiar social and cultural aspects of the area where the study was carried out.
Despite these limitations, the findings of our review highlight a significant risk for sequelae of Covid in the working‐age population. In particular, respiratory and neurological signs and/or symptoms were the most frequent concerns persisting after recovery from SARS‐Cov‐2 infection, also in mild versions of the disease. Healthcare organizations and policy makers should focus attention on rehabilitation programs targeted at the improvement of health status of discharged patients through a structured multidisciplinary rehabilitation program. A special effort is required to allow the complete recovery of the work suitability of patients who have suffered from Covid, taking into account the occupational risks for both communicable and noncommunicable diseases, 33 , 34 commonly present in the workplace, and the need to minimize their effects on the health of workers coming back from Covid. 35 , 36 Moreover, the findings of our systematic review highlight the need for occupational health surveillance of workers returning to work after Covid‐19 and suffering from sequelae of the disease. In particular, healthcare organizations and health managers should involve a multidisciplinary medical team in the clinical examination of such workers, to allow the occupational health physicians both to assess the workers' fitness for the job and to ensure that the job be fitted for the workers' safety and health. In fact, workplace hazards (e.g., physical or biological agents, work‐related stress) could pose a threat to the complete recovery of such workers. Longitudinal studies focusing on the health status of workers returning to work after Covid‐19 are required in order both to detect the prevalence rates of Covid‐19 sequelae and to investigate the relationship between hazards present in different working settings and the evolution of the aforementioned sequelae.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Conceptualization: Gabriele d'Ettorre, Giancarlo Ceccarelli, Gabriella d'Ettorre, and Lorenzo Tarsitani. Methodology: Gabriele d'Ettorre, Giancarlo Ceccarelli, and Gabriella d'Ettorre. Resources and data curation: Gabriella d'Ettorre, Ornella Spagnolello, Gabriella De Girolamo, Elio Gentilini Cacciola, and Alessandro Russo. Writing—original draft preparation, Gabriella d'Ettorre, Giancarlo Ceccarelli, and Gabriele d'Ettorre. Writing—review and editing: Claudio M. Mastroianni, Alessandro Russo. Supervision: Claudio M. Mastroianni, Gabriele d'Ettorre, and Giancarlo Ceccarelli. All authors have read and agreed to the published version of the manuscript.
d'Ettorre G, Gentilini Cacciola E, Santinelli L, et al. Covid‐19 sequelae in working age patients: A systematic review. J Med Virol. 2022;94:858‐868. 10.1002/jmv.27399
DATA AVAILABILITY STATEMENT
Data are available by consulting the first author or the corresponding author.
REFERENCES
- 1. Jiang DH, McCoy RG. Planning for the post‐COVID syndrome: how payers can mitigate long‐term complications of the pandemic. J Gen Intern Med. 2020;35:3036‐3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lambert H, Survivor Corps. COVID‐19 “Long‐Hauler” Symptoms Survey Report. https://dig.abclocal.go.com/wls/documents/2020/072720-wls-covid-symptom-studydoc.pdf
- 3. Rubin R. As their numbers grow, COVID‐19 “long haulers” stump experts. JAMA. 2020;324:1381‐1383. [DOI] [PubMed] [Google Scholar]
- 4. NICE. NICE, SIGN and RCGP set out further details about the UK guideline on management of the long‐term effects of COVID‐19. 10/30/2020. Accessed February 15, 2021. https://www.nice.org.uk/
- 5. Greenhalgh T, Knight M, Buxton M, Husain L. Management of post‐acute covid‐19 in primary care. BMJ. 2020;370:m3026. [DOI] [PubMed] [Google Scholar]
- 6. Moreno‐Pérez O, Merino E, Leon‐Ramirez JM, et al. Post‐acute COVID‐19 Syndrome. Incidence and risk factors: a Mediterranean cohort study. J Infect. 2021;82:378‐383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Garg P, Arora U, Kumar A, Wig N. The “post‐COVID” syndrome: How deep is the damage? J Med Virol. 2020;93:673‐674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Couzin‐Frankel J (2020). The long haul. Accessed February 15, 2021. https://science.sciencemag.org/
- 9. Carfi A, Bernabei R, Landi F, Gemelli Against COVID‐19 Post‐Acute Care Study Group . Persistent symptoms in patients after acute COVID‐19. JAMA. 2020;324:603‐604. doi:10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A proposal for multidisciplinary tele‐rehabilitation in the assessment and rehabilitation of COVID‐19 survivors. Int J Environ Res Public Health. 2020;17(13):4890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Batawi S, Tarazan N, Al‐Raddadi R, et al. Quality of life reported by survivors after hospitalization for Middle East respiratory syndrome (MERS). Health Qual Life Outcomes. 2019;17:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li TS, Gomersall CD, Joynt GM, Chan DPS, Leung P, Hui DSC. Long‐term outcome of acute respiratory distress syndrome caused by severe acute respiratory syndrome (SARS): an observational study. Crit Care Resusc. 2006;8:302‐308. [PubMed] [Google Scholar]
- 13. Kim JE, Heo JH, Kim HO, et al. Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol. 2017;13:227‐233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jaffri A, Jaffri UA. Post‐Intensive care syndrome and COVID‐19: crisis after a crisis? Heart Lung. 2020;49(6):883‐884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. WHO . Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide. 2017. Accessed February 10, 2021. https://www.who.int/alliance-hpsr/resources/publications/rapid-review-guide/en/
- 16. Huang C, Huang L, Wang Y, et al. 6‐month consequences of COVID‐19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220‐232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goërtz YM, Van Herck M, Delbressine JM, et al. Persistent symptoms 3 months after a SARS‐CoV‐2 infection: the post‐COVID‐19 syndrome? ERJ Open Res. 2020;6(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhao YM, Shang YM, Song WB, et al. Follow‐up study of the pulmonary function and related physiological characteristics of COVID‐19 survivors three months after recovery. EClinicalMedicine. 2020;25:100463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Raahimi MM, Kane A, Moore CE, Alareed AW. Late onset of Guillain‐Barré syndrome following SARS‐CoV‐2 infection: part of ‘long COVID‐19 syndrome'? BMJ Case Reports CP. 2021;14(1):e240178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Novak P. Post COVID‐19 syndrome associated with orthostatic cerebral hypoperfusion syndrome, small fiber neuropathy and benefit of immunotherapy: a case report. eNeurologicalSci. 2020;21:100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walsh‐Messinger J, Manis H, Vrabec A, et al. The kids are not alright: a preliminary report of post‐COVID syndrome in university students. medRxiv. 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7709187/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Soh M, Hifumi T, Iwasaki T, Miura Y, Otani N, Ishimatsu S. Impaired mental health status following intensive care unit admission in a patient with COVID‐19. Acute Med Surg. 2020;7(1):e562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yu M, Liu Y, Xu D, Zhang R, Lan L, Xu H. Prediction of the development of pulmonary fibrosis using serial thin‐section CT and clinical features in patients discharged after treatment for COVID‐19 pneumonia. Korean J Radiol. 2020;21(6):746‐755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. You J, Zhang L. Anormal pulmonary function and residual CT abnormalities in rehabilitating COVID‐19 patients after discharge: a prospective cohort study. The. J Infect. 2020;81:e150‐e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Alhiyari MA, Ata F, Alghizzawi MI, Bilal ABI, Abdulhadi AS, Yousaf Z. Post COVID‐19 fibrosis, an emerging complicationof SARS‐CoV‐2 infection. IDCases. 2021;23:e01041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kamal M, Abo Omirah M, Hussein A, Saeed H. Assessment and characterisation of post‐COVID‐19 manifestations. Int J Clin Pract. 2020;75:e13746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Puchner B, Sahanic S, Kirchmair R, et al. Beneficial effects of multi‐disciplinary rehabilitation in post‐acute COVID‐19‐an observational cohort study. Eur J Phys Rehabil Med. 2021;57:189‐198. [DOI] [PubMed] [Google Scholar]
- 28. Hui DS, Joynt GM, Wong KT, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60(5):401‐409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS. The long‐term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. 2010;15(3):543‐550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(8):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta‐analysis with comparison to the COVID‐19 pandemic. Lancet Psychiatry. 2020;7:611‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. D'Ettorre G, Pellicani V, Greco M, Mazzotta M, Vullo A. Assessing and managing the shift work disorder in healthcare workers. Med Lav. 2018;109(2):144‐150. 10.23749/mdl.v109i2.6960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sathish T, Dunleavy G, Soljak M, et al. Risk factors for non‐communicable diseases at baseline and their short‐term changes in a workplace cohort in Singapore. Int J Environ Res Public Health. 2019;16(22):4551. 10.3390/ijerph16224551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tarsitani L, Vassalini P, Koukopoulos A, et al. Post‐traumatic stress disorder among COVID‐19 survivors at 3‐month follow‐up after hospital discharge. J Gen Intern Med. 2021;36(6):1702‐1707. 10.1007/s11606-021-06731-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. d'Ettorre G, Ceccarelli G, Santinelli L, et al. Post‐traumatic stress symptoms in healthcare workers dealing with the COVID‐19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18(2):601. 10.3390/ijerph18020601 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by consulting the first author or the corresponding author.


