Abstract
Coronavirus infection disease 2019 (COVID‐19) was associated with a physical‐functional and emotional decline in patients with COVID‐19 hospital internment. Objective: Evaluate the main functional changes after hospital discharge after COVID‐19 by teleconsultation. A cross‐sectional study was carried out between April and July 2020, the peak period of new cases, hospital admission, and deaths by COVID‐19, in Recife‐Brazil. We included patients (n = 89) over 18 years with positive COVID‐19 RT‐PCR tests and hospitalized for more than 7 days. Functional aspects such as muscle pain, shortness of breath, cough, weight loss >5 kg, weakness/fatigue, daily living activities, balance, walking, lying down, sensitivity, anxiety/sadness, altered memory, or understanding were assessed. Besides this, the impact of hospital admission on daily activities and the quality of information obtained by teleconsultation were quantified. The mean age was 63.5 years (±14), and in the hospital, the mean internment was 18 days (±16). The main findings of this study showed four predominant functional alterations: weight loss greater than 5 kg (60.7%), muscle fatigue/weakness (53.9%), muscle/joint pain (43.8%), and anxiety/sadness (46.1%). Of the functions analyzed, 59.6% of patients reported dysfunctions in at least three of the alterations evaluated. There were several short‐term physical‐functional and emotional changes in adults after hospital discharge.
Keywords: COVID‐19, dysfunction, hospitalization, physical therapy, rehabilitation, sequelae
1. INTRODUCTION
The pandemic caused by the new coronavirus, which induces severe acute respiratory syndrome, called severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), has been considered a public health emergency of international importance by the World Health Organization (WHO) from March 2020. 1 , 2 Coronavirus infection disease 2019 (COVID‐19), severe form with pulmonary and systemic alterations, has been responsible for high hospital admission, mortality, and increased health costs. 2
During epidemiological week 33—EW33 (August 08–15, 2020), 21 214 898 cases of COVID‐19 were confirmed worldwide. Brazil ranked 2nd in the case of numbers (3 317 096), the United States of America (USA) ranked first (5 313 080 cases), India ranked third (2 526 192 cases), Russia ranked fourth (912 823 cases), and South Africa ranked fifth (579 140 cases). Regarding the death rates, Brazil was also ranked second compared to the United States and other countries. 3
According to Brazil's epidemiological data (EW‐33), 304 684 cases and 6755 new deaths were registered per COVID‐19 in Brazil, with a new case incidence rate of 1578.5 every 100 000 inhabitants, 51 deaths every 100 000 inhabitants. In Brazil's Northeast region, the incidence of new cases was 1784.6 cases/100 000 inhabitants, and the mortality rate was 56.3 deaths/100 000 inhabitants. This study has been in Pernambuco, where the incidence of COVID‐19 was 1169.50/100 000 inhabitants. 3
Besides the severity of the lung disease‐related preexisting risk factors, drug use, and a complex and heterogeneous inflammatory process, were observed a physical‐functional and emotional decline in the patients with COVID‐19 during hospital internment. This decline has caused acquired myalgia and muscle weakness, and cognitive and psychosocial alterations. 4 , 5 Thus, much concern has emerged from researchers and health professionals in countries that have already gone through the epidemic peak, the increasing number of survived individuals presenting physical‐functional and quality of life limitations after hospital discharge for an undetermined period. 4 , 5 , 6
For the WHO, functionality is defined as the “ability to care for oneself” and is an essential part of health and life quality. Therefore, it needs to be valued and measured during the entire patient follow‐up, even after discharge. Thus, after the “critical status,” the Pan American Health Organization has guided us on the emergency need in the creation and adequacy of public or private referral services for the rehabilitation of individuals who survived COVID‐19 to qualified health professionals and promoting the continuity of health care and rehabilitation after discharge. 7
Due to the pandemic, most studies report prevention in the acute response to the diagnosis of COVID‐19, clinical trials, and little is known about the evolution of chronic myalgia outcomes, weakness, and the impact of hospital sequelae on functionality and quality of life, especially in the Brazilian population. 7 In this sense, we aim to evaluate the main functional alterations in the short term after the discharging hospital, using a Telehealth service that consists of a system of remote health services that uses information and communication technologies, with the possibility of teleconsultation.
2. METHODS
2.1. Study location, selection, and description of participants
According to the STROBE initiative guidelines, a cross‐sectional study was done by consultation phone: guidelines on reporting observational studies. 8 The study had a nonprobabilistic sample, between April and July 2020, the peak period of new cases, hospital admission, and deaths by COVID‐19, in a hospital in the city of Recife (Brazil) that performed the care and treatment of cases of COVID‐19, known as Recife Provisional Hospital 2 (RPH‐2).
As eligibility criteria were included: all patients over 18 years old with positive tests for SAR‐CoV‐2 in the nasopharyngeal and oropharyngeal swabs (RT‐PCR reverse transcription‐polymerase chain reaction test for the qualitative detection of nucleic acid from SARS‐CoV‐2) and the duration of hospitalization lasting longer than 7 days.
The Research Ethics Committee approved this study of the Instituto de Medicina Integral Prof. Fernando Figueira (IMIP; Protocol No. CAAE 31682720.9.0000.520). The Informed Consent Form was signed electronically by the participants or responsible.
After applying the eligibility criteria, the selected patients were screened using the two electronic medical records and included in a specific list as research candidates. Information has been collected regarding the number of patients discharged from the hospital, deaths, and duration of hospitalization.
2.2. Telephone follow‐up in the postdischarge
Teleconsultation was then made with a standardized test in the form of a questionnaire by members of the post‐COVID‐19 rehabilitation team explicitly developed for this study. Three phone calls/day have been performed at different times and three alternate days to increase the chances of contacting each patient. During the telephone contact, the invitation to study participants has been performed, and those who agreed signed the TCLE.
2.3. Analyses of functional changes
A questionnaire was developed by the researchers of the multidisciplinary and peer‐reviewed team, with 12 questions about the main functional changes perceived by patients after hospital discharge. The answers were organized and adapted in the format “YES” and “NO,” and at the end, each patient attributed a score on the scale of 0–10 quantifying the impact of hospitalization by COVID‐19 on their daily lives, with the “0” being no impact and the “10” maximum impact.
The questions in the research questionnaire with different types of domains such as muscle pain, shortness of breath at rest or effort, coughing or choking, weight loss >5 kg, weakness or fatigue, difficulty in movements in daily life activities, difficulty in balance, or fear of falling, difficulty in walking, difficulty in changing decubitus, changes in sensitivity, anxiety/sadness; and in the mood, memory and understanding alterations.
The twelve questions were prepared based on the International Classification of Functionality, Disability, and Health (ICF) of the WHO, considering the domains: body functions, body structure, activities, and participation (ICF, WHO, 2007). Patients who answered at least three “YES” answers were invited to participate in the specific Rehabilitation Program for people who need follow‐up after COVID‐19 through a second more detailed teleconsultation.
2.4. Analysis of the quality of the teleconsultation
The quality of the teleconsultation at the end of each call was analyzed using a questionnaire adapted in the format “YES” and “NO.” 9 The following topics were considered: “complete interview with an indication of subsequent teleconsultation,” “complete interview without indication of subsequent teleconsultation,” “incomplete interview,” “could not be contacted,” “death after discharge from hospital,” “patient included wrongly or refused to participate.”
2.5. Statistical analysis
Statistical analyses were performed in the Epi info 7.2 Student t was used to compare two independent groups. Values of p < 0.05 were considered statistically significant. Descriptive data was provided in absolute and relative frequency distribution and central tendency measures (mean and SD).
3. RESULTS
During the 3 months of the peak of the disease, 1391 patients were hospitalized in RPH‐2. Of these, 1021 patients survived, 971 were discharged, and 50 remained hospitalized during this study. Of the 971 patients discharged, 753 could not participate in the study because they did not meet the eligibility criteria. It was impossible to contact them by phone using the numbers registered in electronic medical records. In total, there were 218 eligible participants, but 89 of the 218 patients accepted the study. The entire process of participant capture is detailed in the flowchart performed according to the model suggested by STROBE (Figure 1).
Figure 1.
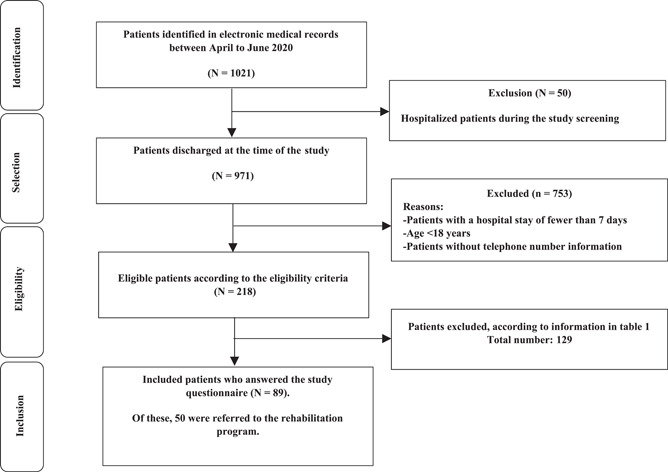
Flowchart of capturing participants according to the model suggested in STROBE
There were 89 participants in this study; 50 of these (56.1%) answered more than three “YES” responses to functional changes, which shows the impact of hospitalization by COVID‐19 on their daily lives the program rehabilitation after COVID‐19.
The mean age of the patients was 63.5 years (±14), 55% (49) were male with an average age of 60.7 years (±15.2); and 45% (40) were female, with a mean age of 67.2 years (±12), and no statistically significant difference between groups. The average total length of hospital internment was 18 days (±16 days), being 14.9 days (±6.6) for females and 17.8 days (±20.6) for males. There was no significant difference in the mean length of hospital internment between the groups (p > 0.05).
The behavior of the functional changes reported after COVID‐19 are shown in Figure 2. Among the 12 functional changes analyzed, 56.1% of patients reported a dysfunction in at least three items. Regarding the impact of these changes on daily activities, 34.8% of patients rated “0” (no damage), and 21.3% rated “10” (maximum impairment) (Figure 3).
Figure 2.
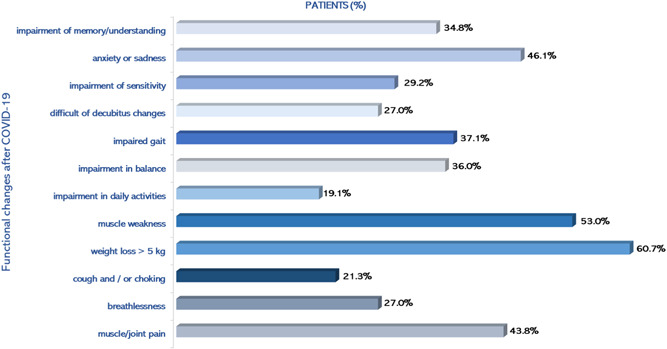
Functional changes after COVID‐19 reported by patients. COVID‐19, coronavirus infection disease 2019
Figure 3.
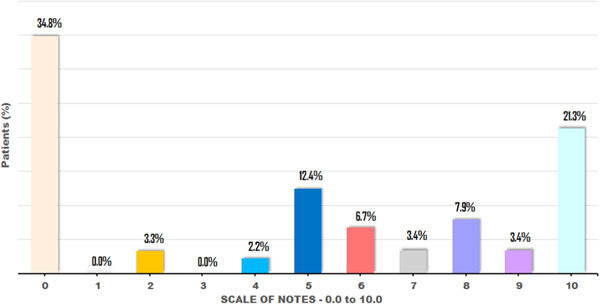
Patients' perception of the impact of SARS‐CoV‐2 in the carrying out of daily activities. SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2
In assessing the quality of the interviews, we performed contact with 53.2% (n = 116) of the patients who were discharged. Of these, 1.96% (n = 4) deaths in the first 3 months of hospital discharge, and 43.8% (n = 39) of patients with few or no sequelae, and no indication of continuity of teleconsultation and participation in the rehabilitation program detailed description in Table 1.
Table 1.
Description of the quality of data collection in this study by teleconsultation
| Eligible participants | N = 218 |
|---|---|
| The patient contacted by phone | |
| Yes | 102 (46.8) |
| No | 116 (53.2) |
| Patients who agreed to participate in the study | |
| Yes | 100 (98.03) |
| No | 02 (1.97) |
| Death after hospital discharge | |
| Yes | 04 (4.0) |
| No | 96 (96.0) |
| Patients who answered all questions | |
| Yes | 89 (92.7) |
| No | 07 (7.3) |
| Patient with an indication for the second teleconsultation | |
| Yes | 50 (56.2) |
| No | 39 (43.8) |
4. DISCUSSION
This study's main findings showed the four most prevalent functional changes in the short term after COVID‐19 and hospital discharge. Among the 12 questions of the patients' health status, three most frequent physical changes were highlighted, weight loss 5 kg (60.7%), muscle weakness (53%) and muscle/joint pain (43.8%), and a mental/emotional change with feelings of anxiety or sadness (46.1%).
A previous study of 143 patients in Italy during the decline of the pandemic and the recovery period of COVID‐19 showed the specific symptoms of COVID‐19 in the average period of 60 days after hospital discharge. The authors reported the persistence of at least one symptom in more than 87% of the cases, emphasizing fatigue, dyspnea, myalgia, and arthralgia. These findings were like the results obtained with this study.
Currently, a Chinese's study that to date represents the larger cohort of COVID‐19 patients (n = 1733) with longer follow‐up time (6 months) after hospital discharge showed that 76% of patients reported some symptoms like those described by our patients, highlighting: fatigue, muscle weakness, difficulty sleeping, anxiety or depression, confirming that there is a chronic form of the disease that presents itself in physical‐motor and psychoneurological impairment 10
So far, our study is one of the few published in which hospital follow‐up was performed until the first 3 months after the discharge of Brazilian patients. We showed that the patients followed up in this study showed that the sequelae associated with COVID‐19 and the hospital stay behaved as two distinct subgroups, in 21.8% of patients, the disease continued to impact their daily lives, and in 34.8%, no sequelae were observed after hospital discharge in the assessed period.
Another critical finding reinforces the question of the impact of the disease on age and sex. There was a higher frequency of male patients, with an average age greater than 60 years and a more extended hospital stay than that observed in female patients, although this difference is not significant. Thus, although COVID‐19 can affect any population, regardless of gender and age group, it has been demonstrated in previous studies that older men and those with associated chronic diseases are more likely to evolve with more severe cases and more extended periods of hospital stays. 11
After a period of hospitalization, persistent functional changes, especially after staying in the intensive care unit, have been described by some authors. They showed that serious illness, regardless of origin, generates significant multisystemic sequelae that can last indefinitely, causing functional impairments and disabilities in all biopsychosocial domains. 11 , 12 The set of these changes was called Post Intensive Care Syndrome, responsible for the weakness acquired in the intensive care unit, a possible explanation for physical and emotional impairments observed in the patients in this study.
Regarding the pandemic COVID‐19, regardless of population and external factors, the hypothesis widely discussed by the scientific community is that the disease appears to evolve with a behavior of a postviral syndrome like the severe acute respiratory syndrome (SARS) and caused by the coronavirus. After the acute phase of symptoms, some patients had physical, mental, and emotional sequelae for an indefinite period. 13
The most prevalent physical damages were muscle fatigue and weakness, diffuse myalgia, dyspnea, cough, low tolerance to exercise, a deficit in balance and gait, headache, and dizziness. For the most severe patients, malnutrition and immune deficit associated with the hospital stay was a significant risk factor for reducing muscle mass and strength, and physical function in general. Mental and emotional sequelae include depressive and anxiety symptoms, acute and posttraumatic stress disorders, cognitive deficits, and nonrestorative sleep. 14 , 15 , 16 , 17 In our study, the results corroborate previous studies described in the literature. In our study, the results corroborate previous studies described in the literature.
Evaluating the quality of data obtained from this study by Teleconsultation was innovative for science during the COVID‐19 pandemic. The significant challenges were rehabilitation after hospital discharge and the call center modality implementation during the pandemic period, the difficulty of contacting more than half of the participants eligible for research.
This was an exploratory study in one of the provisional hospitals for patients between moderate to severe symptoms of COVID‐19. Study limitations were not performing a sample calculation to estimate the number of participants, not obtaining your health data in the period before the pandemic, and, mainly, the difficulty of telephone contact with some patients after hospital discharge. Nevertheless, this study was particularly important for the hospital service for the benefits of knowing the profile of the individuals who survived COVID‐19 and for the opportunity that patients were given to continue health care through a rehabilitation program even after completing this study.
In addition to allowing the continuity of care for patients after hospital discharge through a multi‐professional rehabilitation unit, this study contributed to clinical practice and research in the following ways: it demonstrated the feasibility and quality of screening and follow‐up through teleconsultations. It warned about the main functional alterations of the post‐COVID‐19 Syndrome in the northeastern Brazilian region population.
5. CONCLUSION
The patients showed functional and emotional changes, especially weight loss, muscle fatigue/weakness, muscle/joint pain, and feelings of anxiety or sadness. The sequelae brought about difficulties in carrying out daily activities. In addition to the care with the prevention and treatment of COVID‐19, there is a growing need for continued rehabilitation after the acute phase of SARS‐CoV‐2.
6. STUDY LIMITATIONS
Many studies often describe the extraction of data and results, medical history, and other information about hospital admission. However, during the data collection phase, this information was not up‐to‐date and duly registered in the database of the hospital where the research was carried out. However, we do not consider this data essential to conclude on the results.
CONFLICTS OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Conceptualization, methodology and formal analysis: Bárbara R.A.F Barros‐Leite, Marcela Raquel de Oliveira Lima, Marina Caminhaa, Kaliandra Santos, Cristiano Berardo Carneiro da Cunhaa, and Lívia Barboza de Andrade. Writing—original draft preparation, data curation, formal analysis: Bárbara R.A.F Barros‐Leite, Marcela Raquel de Oliveira Lima, and Lívia Barboza de Andrade. Design, analysis, writing—review and editing: Bárbara R.A.F Barros‐Leite, and Lívia Barboza de Andrade. All authors have read and agreed to the published version of the manuscript.
ACKNOWLEDGMENTS
We thank patients and their families, the professionals at the IMIP Rehabilitation Center, and all the teams at the Recife Provisional Hospital 2, Recife, Brazil.
Barros‐Leite BR, Lima MRdO, Caminha M, Santos K, Cunha CBCd, Andrade LBd. Short‐term functional changes after hospital discharge by COVID‐19 through teleconsultation at a reference service in Northeast Brazil: A cross‐sectional study. J Med Virol. 2022;94:994‐1000. 10.1002/jmv.27410
DATA AVAILABILITY STATEMENT
Data supporting the results of this study are openly available at “dataverse.harvard.edu” at “doi:10.7910/DVN/XUHW1J”, author name Barros‐Leite, year 2021.
REFERENCES
- 1. Gudi SK, Tiwari KK. Preparedness and lessons learned from the novel coronavirus disease. Int J OccupEnviron Med11(2). 2020;1:8‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boldrini P, Bernetti A, Fiore P. Impact of COVID‐19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine physicians' activities in Italy. An official document of the Italian PRM Society (SIMFER). Eur J Phys Rehabil Med. 2020;56(3):316‐318. [DOI] [PubMed] [Google Scholar]
- 3. Ministry of Health, Brazil . Epidemiological Week. 2020:33. https://covid.saude.gov.br/
- 4. Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation, and respiratory management in the acute and early post‐acute phase. “Instant paper from the field” on rehabilitation answers to the COVID‐19 emergency. Eur J PhysRehabil Med. 2020;56(3):323‐326. [DOI] [PubMed] [Google Scholar]
- 5. Tumlinson A, Altman W, Glaudemans J, Gleckman H, Grabowski DC. Post‐acute care preparedness in a COVID‐19 world. J AmGeriatr Soc. 2020;68(6):1150‐1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan American Health Organization (PAHO) . Considerações sobre a reabilitação durante o surto de COVID. 2020:19. https://iris.paho.org/handle/10665.2/52103
- 7. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344‐349. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 8. Åhsberg E. Discharge from the hospital—a national survey of transition to out‐ patient care. Scand J Caring Sci. 2019;33(2):329‐335. https://pubmed.ncbi.nlm.nih.gov/30408841/ [DOI] [PubMed] [Google Scholar]
- 9. Godeau D, Petit A, Richard I, Roquelaure Y, Descatha A. 6‐month consequences of COVID‐19 in patients discharged: a cohort study. Lancet. 16. 2021;2027(10270):220‐232. 10.1016/S0140-6736(20)32656-8. Jan 8 33428867; PMCID: PMC7833295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dhama K, Khan S, Tiwari R, et al. Features of 20 133 UK patients in hospital with covid‐19 using the ISARIC WHO Clinical Characterization Protocol: Prospective observational cohort study. BMJ. 2020;369:8‐9. https://pubmed.ncbi.nlm.nih.gov/32444460/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020;99(6):470‐474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biehl M, Sese D. Post‐intensive care syndrome and COVID‐19—implications post‐pandemic. Cleve Clin J Med. 2020. 10.3949/ccjm.87a.ccc055 [DOI] [PubMed] [Google Scholar]
- 13. Thomas P, Baldwin C, Bissett B, et al. Physiotherapy management for COVID‐19 in the acute hospital setting: clinical practice recommendations. J Physiother. Apr. 2020;66(2):73‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Klok FA, Boon GJAM, Barco S, et al. The post‐COVID‐19 functional status scale: a tool to measure functional status over time after COVID‐19. Eur Respir J. 2020;56(1):10‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barker‐Davies RM, O'Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post‐COVID‐19 rehabilitation. Br J Sports Med. 2020;54(16):949‐959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Landi F, Gremese E, Bernabei R, et al. Post‐COVID‐19 global health strategies: the need for an interdisciplinary approach. Aging Clin Exp Res. 2020;32(8):1613‐1620. 10.1007/s40520-020-01616-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bonilla‐Aldana DK, Rodriguez‐Morales AJ. Coronavirus disease 2019—COVID‐19. Clin Microbiol Rev. 2020;33:28‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting the results of this study are openly available at “dataverse.harvard.edu” at “doi:10.7910/DVN/XUHW1J”, author name Barros‐Leite, year 2021.


