Abstract
Purpose
A model was hypothesised by integrating two theoretical models: the compassion satisfaction‐compassion fatigue and empowerment models. This study aimed to assess the extent to which this integrated model can explain the relationships between paediatric nurses' burnout quality of life, perceived patient safety and work‐related variables during the COVID‐19 pandemic.
Background
Nurses' burnout is negatively associated with quality of life (QOL) and positively with patient safety. Several theoretical models were introduced to explain burnout determinants and outcomes such as Golembiewski, Munzenrider and Stevenson model, Leiter and Maslach's process model, and Lee and Ashforth's model. However, few models described burnout in relation to QOL or patient safety.
Methods
A sample of 225 paediatric nurses responded to questionnaires about burnout, QOL, adverse events and work‐related variables. Compassion satisfaction ‐ compassion fatigue and empowerment models were integrated into a single model and tested using structural equation modelling analysis. This study was prepared and is reported according to the STROBE checklist.
Results
The final model explained 65% of the variance of burnout and 37% of the variance of QOL. The work‐related variables (co‐workers' support, job satisfaction, satisfaction with the monthly salary, participation in continuous education and exposure to violence) are predicting paediatric nurses' burnout and quality of life.
Conclusion
The Compassion satisfaction ‐ compassion fatigue ‐Empowerment integrated model allows for assessing the different paths in the relationship between work‐related variables and burnout.
Relevance to clinical practice
These results might be essential for nursing managers to develop strategies that improve nurses' work environment and minimise their burnout during COVID‐19 pandemic. These strategies should focus on enhancing co‐workers' support, job satisfaction and participation in continuous education. Furthermore, paediatric nurses should be protected from any violence.
Keywords: adverse events, burnout, COVID‐19, quality of life, theoretical model
What does this paper contribute to the wider global clinical community?
Burnout has always been an issue within the nursing profession. However, working within the stressful COVID‐19 hospital environment have exacerbated the stress leading to burnout.
The integrated theoretical model can explain the determinants of paediatric nurses' burnout.
1. INTRODUCTION
Burnout is defined as a stress condition associated with physical and mental symptoms (Maslach & Leiter, 2008). The physical symptoms include headache, hypertension, muscle spasm and gastrointestinal and sleep disturbances (Maslach & Leiter, 2008). The mental symptoms include emotional exhaustion, fatigue and decreased work accomplishment (Maslach & Leiter, 2008).
Burnout has always been an issue threatening the nursing workforce and contributing to nurses' shortage all over the world (Khatatbeh, Pakai, et al., 2021; Mudallal et al., 2017; Padilha et al., 2017). In December 2019, the new COVID‐19 disease emerged first in China and started to spread worldwide. Prior to diagnosing the first case of COVID‐19 on the second of Mrach, that strict protocols had been put in place in the Jordanian hospitals which may have increased paediatric nurses' workload and the associated stress. Because of the COVID‐19 disease, the light was shed again on the mental health of nurses especially the burnout (Alrawashdeh et al., 2021; Duarte et al., 2020; Khatatbeh, Alhalaiqa, et al., 2021; Khatatbeh et al., 2021; Li et al., 2021; Zhang et al., 2021).
The available studies on nurses' burnout found that it is correlated with a poor nurses' quality of life (QOL) and more frequent patient adverse events (Nantsupawat et al., 2016; Ribeiro et al., 2021; Woodhead et al., 2016). For instance, a recent systematic review concluded that nurses' burnout and QOL are inversely correlated (Khatatbeh, Pakai, et al., 2021). Also, nurses' burnout was associated with more patient adverse events such as medication errors and nosocomial infections (Vogus et al., 2020).
World Health Organization Quality of Life (WHOQOL) group defined QOL as 'an individual's perceptions of their position in life, in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept, affected in a complex way by the person's physical health, psychological state, level of independence, social relationships and their relationship to salient features of their environment' (WHOQOL, 1995). Patient adverse events are described as those harms that happens because of the treatment not the illness leading to a long stay in the hospital, disability or both (Brennan et al., 2004).
To explain burnout determinants and outcomes, different theoretical models have been introduced. For example, three burnout models have described the burnout phenomenon: Golembiewski, Munzenrider and Stevenson model (Golembiewski et al., 1988), Leiter and Maslach's process model (Leiter & Maslach, 1988), and Lee and Ashforth's model (Lee & Ashforth, 1996). Up to our knowledge, few theoretical models have described burnout in relation to QOL and patient safety, such as the compassion satisfaction‐compassion fatigue (CS‐CF) model (Kim & Yom, 2014; Stamm, 2010) and the empowerment model (Nursalam et al., 2018). The CS‐CF model was introduced in developing the professional QOL (Pro‐QOL) scale (Stamm, 2010). This model has classified the consequences of helping others into positive and negative consequences. The positive consequences were described as compassion satisfaction (CS), while the negative consequences were called compassion fatigue (CF) (Stamm, 2010). According to this model, CF is composed of both burnout and secondary traumatic stress (Stamm, 2010). The empowerment model was introduced to explain burnout syndrome, quality of nursing work life, empowerment and other work‐related variables (Nursalam et al., 2018). According to the empowerment model, nurses' empowerment reduces burnout syndrome and improves the quality of nursing work life.
According to the empowerment model (Nursalam et al., 2018), it is assumed that QOL mediates the relationship between work‐related variables and burnout. Moreover, the CS‐CF‐empowerment integrated model (Stamm, 2010) was used to assume that patient safety mediates the relationship between work‐related variables and burnout. Additionally, it was assumed that QOL mediates the relationship between work‐related variables and burnout (Stamm, 2010). Till now, no efforts have yet been made to combine these two models especially during COVID‐19 pandemic. Integrating these two models together would enhance the understanding of burnout determinants and outcomes. In this study, the CS‐CF model and empowerment model were integrated into one theoretical model; for example, the integrated CS‐CF‐Empowerment (Figure 1). This study aims to assess the extent to which integrating the CS‐CF and empowerment models can explain the relationships between paediatric nurses' burnout, QOL, perceived patient safety and work‐related variables during the COVID‐19 pandemic.
FIGURE 1.
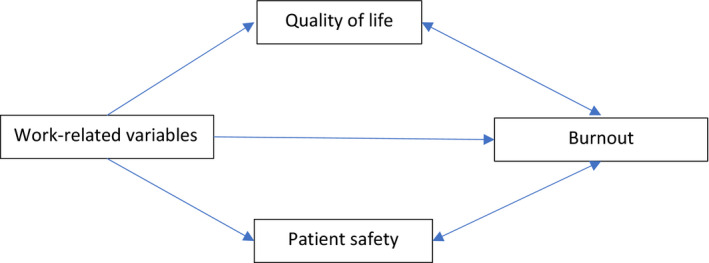
The integrated CS‐CF‐Empowerment model
2. METHODS
2.1. Design
A cross‐sectional design was used in this study. The institutional review boards ethically approved the study at the settings where the data was collected. This study took place at paediatric wards/units of eight governmental hospitals and a university‐affiliated hospital. The majority of the Jordan population lives in the northern and central regions (Department of Jordanian Statistics, 2018). Therefore, only one hospital was selected from the southern region. The rest of the hospitals were selected from the northern and central regions of the country.
2.2. Sampling
A convenient sample of 225 paediatric nurses was selected to represent the paediatric nurses in Jordan. Inclusion criteria were: holding at least a nursing diploma, working in a paediatric ward/unit for at least one year and having an annual or permanent contract.
2.3. Measures
Burnout was assessed using the Copenhagen Burnout Inventory (CBI). CBI is composed of 19 Likert‐type items (never to always and very low degree to very high degree) to measure three domains of burnout: personal, work‐related and client‐related burnout. Each item is given a score (0, 25, 50, 75 or 100); the higher score indicates more burnout. Each domain's score is calculated by taking the average scores of its items (Kristensen et al., 2005).
The QOL was assessed using the brief instrument of World Health Organization QOL (WHOQOL‐BREF). The WHOQOL‐BREF comprises 26 questions (using a 5‐point Likert scale) that assess four domains, namely: Physical Health, Psychological Health, Social Relationships and Environment (World Health Organization, 1996).
Patient adverse events were measured using four items assessing the nurse‐perceived patient adverse events (NPPAE). The items were adopted from two previous studies (Cho et al., 2016; Van Bogaert et al., 2014). Using a 6‐point Likert scale (ranging from 'never' to 'every day'), nurses were asked about the frequency of four patient adverse events: medication errors, nosocomial infection, patient falls and pressure ulcers.
The work‐related variables assessed were the hospital type, job satisfaction, intent to leave, usual work shift, weekly work hours, manager support, co‐worker support, participation in continuous education, satisfaction with the monthly salary, and exposure to violence. The perceived manager and co‐workers' support were assessed by 5‐point scales (very weak, very good). Similarly, nurses were asked about job satisfaction using 5‐point scales (very poor, very good). Satisfaction with the monthly salary, intent to leave and hospital type were assessed using dichotomous questions (enough/ not enough, yes/no and governmental or university‐affiliated, respectively). Nurses were asked about participation in continuous education using a 4‐point scale ('never' to 'always'). Using a multiple‐answer question, nurses were also asked about the type of violence they experienced (no violence, verbal, psychological, physical). Continuous numeric scales were used to ask nurses about their weekly work hours. Nurses were also asked to choose their usual work shifts (day, night or alternate shifts).
2.4. Reliability
The Cronbach's alpha for the three domains of CBI ranged from 0.85 to 0.87 (Kristensen et al., 2005), close to the reliabilities obtained in this study, 0.83–0.90. The Cronbach's alpha for the four domains of the WHOQOL‐BREF ranged from 0.66 (for Social Relationships) to 0.84 (for Physical Health domain), which reflects acceptable reliability (WHOQOL‐Group, 1998). In this study, the Cronbach's alpha for the four domains of the WHOQOL‐BREF ranged from 0.70 (for both physical and psychological health) to 0.85 (for the environment). Regarding the NPPAE, the Cronbach's alpha in previous studies were more than 0.80 reflecting a good internal consistency (Van Bogaert et al., 2014), which is similar to this study's Cronbach's alpha (0.83).
2.5. Data collection
Each participant was asked to sign the consent form on the cover sheet. The consent form assured voluntary and anonymous participation. The data was collected in the beginning of COVID‐19 pandemic between December 2019 and March 2020. English is the official education language at nursing schools in Jordan; so, the English versions of the CBI, WHOQOL‐BREF, NPPAE and the work‐related variables were used. The study was reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist (Von Elm et al., 2014). See Appendix S1.
2.6. Statistical analysis
Data analysis was conducted using SPSS (version 23) and AMOS (Version 23). Descriptive statistics and the internal consistency of the used measures were performed using SPSS. AMOS was used to perform the structural equation modelling (SEM) analyses. The SEM analyses were conducted through performing two main steps; the pooled confirmatory factor analysis (CFA) followed by examining the structural model. During both steps, the goodness of model fit indices were set a priori to make the decision whether a model should be modified or retained. These indices were set as follows: (a) absolute fit: Root Mean Square of Error Approximation (RMSEA) <0.07, (b) incremental fit: Comparative Fit Index (CFI) >0.95, and (c) parsimonious fit: Chi Square/Degrees of Freedom (Chisq/df) <5 (Hair et al., 2010).
In the first step, the pooled CFA was performed to examine the validity of the measurement model. The four main constructs of the study (work‐related variables, QOL, AE and burnout) were entered into the model and examined simultaneously. The main advantage of conducting pooled CFA is the ability to evaluate the validity of these four main constructs at once. Based on the results, modifications to the measurement model were made, using the item‐deletion process. Such modifications were made to enhance the validity of the model. For example, 10 variables were initially used as indicators of the work‐related factor. Considering the poor goodness of model fit indices and low factor loadings of some variables, the measurement model was modified by deleting five of these variables (see the Results section).
In the second step, the structural model was examined using the same goodness of model fit indices. In addition, the factor loadings and the standardised regression weights were evaluated. Different versions of the structural model were compared to figure out which version best fits the data. The first version was created to examine whether the work‐related factor effect on nurses' burnout is mediated by both QOL and AE (serial mediation). On the other hand, the second version of the model examined whether a separate mediation effect of QOL and AE exists. The goodness of model fit indices of these versions were evaluated and compared based on the cut‐off values set a priori. The version of the model with values meeting the cut‐off values set a priori was then retained.
3. RESULTS
3.1. Participants' characteristics
The age of the participants ranged from 23 to 55 years; the median age was 32.5 years. The majority of the sample was female nurses representing 94.2% of the participants. Regarding their marital status, 82.7% of the participants were married. Table 1 presents the participants' sociodemographic and work‐related characteristics.
TABLE 1.
Participants characteristics (N = 225)
| Variable | N | Percentage |
|---|---|---|
| Gender | ||
| Male | 11 | 4.9 |
| Female | 212 | 94.2 |
| Missing | 2 | 0.90 |
| Marital status | ||
| Single | 34 | 15.1 |
| Married | 186 | 82.7 |
| Divorced | 4 | 1.8 |
| Widowed | 1 | 0.40 |
| Education | ||
| 2‐year college | 5 | 2.2 |
| Bachelor's degree | 197 | 87.6 |
| Master's degree | 23 | 10.2 |
| Hospital | ||
| Governmental | 158 | 70.2 |
| University‐affiliated | 67 | 29.8 |
| Job satisfaction | ||
| Very poor | 30 | 13.3 |
| Poor | 41 | 18.2 |
| Intermediate | 76 | 33.8 |
| Good | 68 | 30.2 |
| Very good | 9 | 4.0 |
| Missing | 1 | 0.40 |
| Intent to leave | ||
| Yes | 108 | 48.0 |
| No | 116 | 51.6 |
| Missing | 1 | 0.40 |
| Usual work shift | ||
| Day | 86 | 38.2 |
| Night | 36 | 16.0 |
| Alternate | 100 | 44.4 |
| Missing | 3 | 1.3 |
| Management support | ||
| Very weak | 14 | 6.2 |
| Weak | 33 | 14.7 |
| Fair | 47 | 20.9 |
| Good | 107 | 47.6 |
| Very good | 24 | 10.7 |
| Coworker support | ||
| Very weak | 7 | 3.1 |
| Weak | 51 | 22.7 |
| Fair | 56 | 24.9 |
| Good | 94 | 41.8 |
| Very good | 17 | 7.6 |
| Participation in continuous education | ||
| Never | 51 | 22.7 |
| Sometimes | 118 | 52.4 |
| Often | 31 | 13.8 |
| Always | 25 | 11.1 |
| Perception regarding monthly salary | ||
| Enough | 62 | 27.6 |
| Not enough | 161 | 71.6 |
| Missing | 2 | 0.9 |
| Exposure to violence | ||
| No violence | 58 | 25.8 |
| Verbal | 70 | 31.1 |
| Psychological | 48 | 21.3 |
| Physical | 5 | 2.2 |
| Verbal, psychological, & physical | 44 | 19.6 |
| Mean | SD | |
|---|---|---|
| Weekly work hours | 41.9 | 5.36 |
| Experience (years) | 11.1 | 6.74 |
| Median | Range | |
|---|---|---|
| Age (years) | 32.5 | 23–55 |
3.2. CFA
A pooled CFA was performed on different versions of the model. Initially, the construct work‐related factor was identified using ten variables. These variables were the hospital type (governmental or university‐affiliated), job satisfaction, intent to leave, usual work shift, weekly work hours, manager support, co‐worker support, participation in continuous education, satisfaction with the monthly salary and exposure to violence. This model did not meet the goodness of model fit indices set a priori, and the factor loadings of some items of the work‐related construct were below 0.30. Factor loadings of the items reflective of the constructs: adverse events, QOL, and burnout were acceptable (>0.30). Thus, the model was adjusted by modifying the determinants of the work‐related construct. The variables with the lowest factor loadings were removed from the model: type of hospital, usual work shift and weekly work hours. The standardised factor loadings for these variables were 0.11, 0.08 and 0.03, respectively. After deleting these three variables, the model fit indices improved, but they were still not satisfactory (Table 2). Another two variables were removed based on the same rationale followed in the previous step, namely: manager support and intent to leave. This model achieved the goodness of model fit indices criteria (Table 2), and the model is depicted in Figure 2.
TABLE 2.
Pooled CFA and SEM models
| Model | Chi Square | CFI | RMSEA | Chisq/df |
|---|---|---|---|---|
| Pooled CFA models | ||||
| Model 1 | X2 = 372.74, df = 183, p < 0.001 | 0.872 | 0.068 | 2.04 |
| Model 2 | X2 = 242.87, df = 129, p < 0.001 | 0.919 | 0.063 | 1.88 |
| Model 3 | X2 = 161.62, df = 98, p < 0.001 | 0.951 | 0.054 | 1.65 |
| SEM models | ||||
| Model 1 (Serial mediation) | X2 = 195.18, df = 99, p < 0.001 | 0.925 | 0.066 | 1.97 |
| Model 2 (Separate mediation) | X2 = 161.62, df = 98, p < 0.001 | 0.951 | 0.063 | 1.65 |
FIGURE 2.
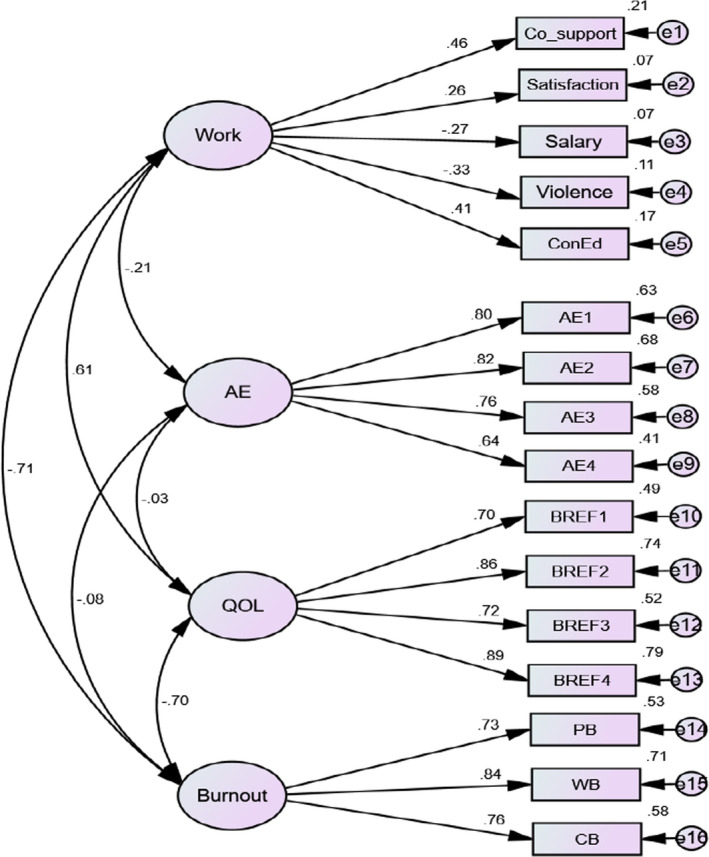
Pooled CFA
3.3. SEM model
In the SEM model, two versions were also compared. The first model examined the effect of work‐related construct on burnout with serial mediation of QOL and adverse events. The second model examined the effect on burnout through the separate mediation paths of QOL and adverse events. The goodness of model fit indices of the second model were better: CFI = 0.951, RMSEA = 0.063 and Chisq/df = 1.65 (Table 2).
The final SEM model is shown in Figure 3. The results showed that the effect of the work‐related construct on burnout construct is statistically significant (β = −0.51, p = 0.009). This effect means that one standard deviation increase in the work‐related construct leads to a 0.51 reduction in burnout. The impact of the work‐related construct was significant on QOL but not on the adverse event. The mediators, QOL and adverse events, effects on burnout were statistically significant (Table 3). The standardised regression weights, p values, standard errors and critical ratios are all presented in Table 3. The R2 value of the burnout construct in the final model was 0.65. That means that 65% of burnout variance is explained by the model and the presented paths.
FIGURE 3.
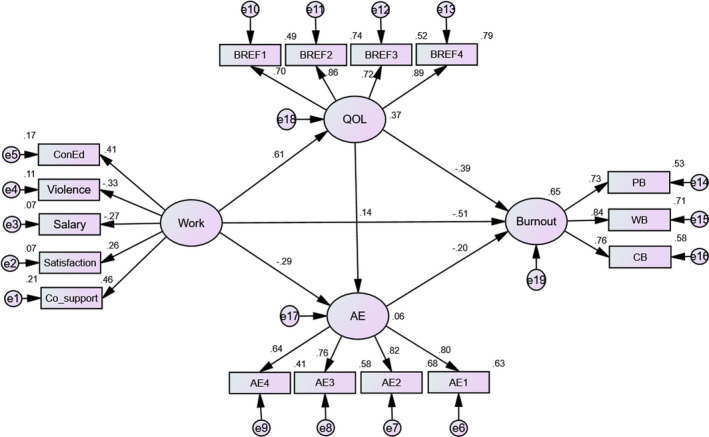
Final SEM model
TABLE 3.
Standardised regression weights (β), p values, standard errors and critical ratios
| Path | Β | p value | SE | CR |
|---|---|---|---|---|
| Work‐related→Burnout | −0.51 | 0.009 | 6.51 | −2.60 |
| Work‐related→QOL | 0.61 | <0.001 | 0.97 | 3.69 |
| Work‐related→Adverse events | −0.29 | 0.10 | 0.33 | −1.64 |
| QOL→Adverse events | 0.14 | 0.29 | 0.04 | 1.07 |
| QOL→Burnout | −0.39 | 0.003 | 0.75 | −2.93 |
| Adverse events→Burnout | −0.20 | 0.011 | 1.43 | −2.53 |
4. DISCUSSION
This study aimed to assess the extent to which integrating the CS‐CF and empowerment models can explain the relationships between paediatric nurses' burnout, QOL, perceived patient safety and work‐related variables during the COVID‐19 pandemic. According to the hypothesised CS‐CF‐empowerment integrated model, the work‐related variables impact burnout both directly and indirectly. The indirect impact is hypothesised to occur through QOL and the four types of adverse events studied namely: medication errors, nosocomial infection, patient falls and pressure ulcers. The results of the current study partially supported this model. The results of this study supported the direct relationship between some of the work‐related variables (co‐workers' support, job satisfaction, satisfaction with the monthly salary, participation in continuous education and exposure to violence) and burnout. Also, the results showed that QOL is a mediator in this relationship between work‐related variables and burnout. However, the data failed to demonstrate that the adverse events construct was a significant mediator in the relationship of work‐related variables and burnout. Surprisingly, adverse events were negatively related to paediatric nurses' burnout scores. The lower burnout scores were associated with the higher frequencies of perceived adverse events. This finding might be explained that nurses with lower burnout scores have better work‐related variables (such as co‐workers support and blame‐free environment) finally are more able to report the adverse events such as medication errors. In other words, nurses with higher burnout scores might be afraid from reporting the adverse events.
Based on this model, it can be assumed that better work‐related variables predict better QOL scores, which in turn predict lower burnout scores. The literature demonstrated that work‐related variables have positive relationships with QOL. For example, one study found that a better quality of working life was positively related to a better QOL (Moradi et al., 2014). This means that a better work environment or work‐related variables are correlated with better QOL among nurses (Moradi et al., 2014). Additionally, work‐related variables were found to be determinantal in improving nurses' QOL (Ibrahim et al., 2016). Also, it was found that nurses with longer experiences and higher payments reported better QOL (Dos Santos et al., 2018). However, those nurses working in closed special units and working more than 36 h per week reported lower QOL scores (Dos Santos et al., 2018).
In the current study, the variables that contributed positively to the work‐related construct were co‐workers' support, job satisfaction and continuous education. On the other hand, work‐related violence and perception of salary were negatively contributed to the work‐related construct. This indicated that support from co‐workers, higher satisfaction scores and more involvement in continuous education activities would positively affect nurses' QOL. In contrast, a lower perception of salary and a higher violence rate at workplace will affect QOL negatively. This finding matches the previous studies. For instance, co‐worker support was found to be a significant predictor of QOL in all domains (Kowitlawkul et al., 2019). Additionally, nurses' job satisfaction was positively correlated with higher QOL scores (Ioannou et al., 2015). Uniquely, continuous education was positively correlated with the work‐related construct in this study. In other words, improving nurses' knowledge at their work could lead to a better work environment perception. This finding can be explained as improved knowledge might reduce the stress associated with complicated and ambiguous work‐related tasks.
A previous study showed that workplace violence was negatively associated with nurses' perception of the work environment, which affects their QOL (Zeng et al., 2013). Furthermore, QOL mediated the relationship between workplace violence and nurses' job performance (Lin et al., 2015). Consequently, patient safety might be directly affected by nurses' performance at work (Ammouri et al., 2015). In this study, patient safety was reflected by the adverse events construct. The relationship between QOL and adverse events was insignificant. On the other hand, QOL was negatively and significantly associated with nurses' burnout in this study. The negative correlation between QOL and burnout is well established in the literature (Abraham & D'silva, 2013; Fradelos et al., 2014; Naz et al., 2016).
In this study, the negative relationships between burnout and both QOL and work‐related variables are justified earlier. This finding is congruent with one study that nurses' burnout, during COVID‐19 pandemic, and their QOL are correlated (An et al., 2020). However, burnout's negative relationship with adverse events construct seems to be problematic. This relationship indicated that with increased perception of adverse events, nurses reported had lower burnout, and the vice versa is true. This result was not congruent with previous studies (Nantsupawat et al., 2016; Van Bogaert et al., 2014), in which the increased adverse events were associated with increased nurses' burnout. Also, this finding is not congruent with another study which found that nurses' lower burnout and higher personal accomplishment, during COVID‐19 pandemic, is correlated with less frequent medication errors (Kakemam et al., 2021). This unexpected result could be explained by the fact that reporting adverse events was impeded by nurses' fear of losing their licences, low confidence in reporting adverse events, fear of blame and patient complaints (Moumtzoglou, 2010). Thus, it is recommended for future studies to assess adverse events by reviewing intuitions' records of incidents reports.
A recent study measured the adverse events objectively by reviewing the incidents database and found that adverse events were positively associated with burnout (Vogus et al., 2020). In the same study, it was also found that safety climate and workgroup identification moderated the relationship between adverse events and burnout (Vogus et al., 2020). In other words, low workgroup identification group and lower safety climate were associated with higher adverse events (Vogus et al., 2020). Workgroup identification and safety climate were not assessed in the current study; However, they are relevant to our study. The workgroup identification is the degree to which an employee is mentally connected to the workgroup. The workgroup identification is relevant to our study as it is similar to co‐worker's support. Also, safety climate is the degree to which a workgroup cares about safety. Safety climate is also relevant to our study as we assessed multiple dimensions of safety threats, nurses' exposure to violence and patient adverse events (medication errors, nosocomial infection, patient falls and pressure ulcers).
Because of the poor goodness of model fit indices and low factor loadings of some variables, the measurement model was modified by deleting five of the work‐related variables (type of hospital, usual work shift, weekly work hours, manager support and intent to leave). Interestingly, these findings are different from previous studies. For example, a previous study found that leaders empowering behaviours are related to lower nurses' burnout (Mudallal et al., 2017). Embowering behaviours is not studied in our study; however, it is a type of manager support. Also, manager support was negatively related to adverse patient events, burnout and intent to leave (Khatatbeh et al., 2020; Khatatbeh, Al‐Dwaikat, et al., 2021). The reasons behind this incongruency might include the different paediatric nursing environments from the adult nursing environment and loading all of these work‐related variables in our study as a construct not separately.
5. LIMITATIONS
The current study showed that work‐related variables, directly and indirectly, affect nurses' burnout. However, causation cannot be presumed because of the correlational nature of the study. Nevertheless, the structural equation modelling allowed the researchers to test their hypotheses regarding the relationships between work‐related variables and burnout during COVID‐19 pandemic. Besides, the generalisability of the findings to all nurses is limited since these findings are pertinent to paediatric nurses. However, this could be an initiator to test this study's hypotheses with other groups of nurses. In addition, including other mediator variables such as work‐related stress could improve our understanding of the relationship between work‐related variables (such as patient to nurse ratio) and burnout during COVID‐19 pandemic. Furthermore, objective measurement of adverse events by reviewing institutional records of incidents report could improve the study. Since the data of this study were collected in the beginning of COVID‐19 pandemic, a follow‐up study is needed.
6. CONCLUSION
Using the CS‐CF‐Empowerment integrated model allows for assessing the different paths in the relationship between work‐related variables and burnout. In this study, the findings demonstrated that work‐related variables directly associated with burnout during COVID‐19, and this relationship was mediated by QOL. However, the data failed to show that adverse events could be a significant mediator in the relationship between work‐related variables and burnout. Thus, future studies are recommended to examine hospital records of incident reports to assess adverse events' mediating role.
7. RELEVANCE TO CLINICAL PRACTICE
Because nurses' work‐related variables finally affect both burnout and QOL, nursing managers should develop strategies that improve these variables to decrease nurses' BO and improve their QOL. According to the CS‐CF‐Empowerment integrated model, the work‐related variables that should be targeted are co‐workers' support, job satisfaction, satisfaction with the monthly salary, participation in continuous education, and exposure to violence. We claim that if the CS‐CF‐Empowerment integrated model is used to guide future research about nurses' burnout, a better understanding of nurses' burnout can be achieved. Consequently, a better remedy for nurses' burnout can be accomplished.
8. DATA AVAILABILITY STATEMENT
The data set used in this research is available from the corresponding author upon a reasonable request.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
All authors are responsible for the reported research and have approved the manuscript as submitted. Haitham Khatatbeh involved in conceptualisation, data collection, data curation, writing – original draft preparation, reviewing and editing. Tariq Al‐Dwaikat involved in conceptualisation, writing – original draft preparation, reviewing and editing, and supervision. Jehad Rababah involved in data analysis, writing – original draft preparation, reviewing and editing, and supervision. Annamária Pakai and András Oláh involved in conceptualisation, writing – reviewing and editing, and supervision.
ETHICS APPROVAL
Ethical approval was obtained before research implementation both from the Scientific Research Committee of the Jordanian Ministry of Health (reg. # 21114) as well as from the Ethics Committee of King Abdullah University Hospital (reg. # 13–3–17).
CODE AVAILABILITY
Not applicable.
CONSENT TO PARTICIPATE
Each participant was asked to sign the consent form on the cover sheet.
CONSENT FOR PUBLICATION
We, Haitham Khatatbeh and the co‐authors, give our consent for the publication of this manuscript.
Supporting information
Supplementary Material
ACKNOWLEDGEMENT
The researchers thank everyone who contributed to the current study including paediatric nurses who participated in this study, head nurses and managerial staff who helped in the ethical approval and data collection.
Khatatbeh, H. , Al‐Dwaikat, T. , Rababah, J. , Oláh, A. , & Pakai, A. (2021). Paediatric nurses' burnout, quality of life and perceived patient adverse events during the COVID‐19 pandemic: Testing an integrated model using structural equation modelling. Journal of Clinical Nursing, 00, 1–10. 10.1111/jocn.16114
Funding information
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors
REFERENCES
- Abraham, A. , & D'silva, F. (2013). Job satisfaction, burnout and quality of life of nurses from Mangalore. Journal of Health Management, 15(1), 91–97. 10.1177/0972063413486033 [DOI] [Google Scholar]
- Alrawashdeh, H. M. , Al‐Tammemi, A. B. , Alzawahreh, M. K. , Al‐Tamimi, A. , Elkholy, M. , Al Sarireh, F. , Abusamak, M. , Elehamer, N. M. , Malkawi, A. , Al‐Dolat, W. , Abu‐Ismail, L. , Al‐Far, A. , & Ghoul, I. (2021). Occupational burnout and job satisfaction among physicians in times of COVID‐19 crisis: A convergent parallel mixed‐method study. BMC Public Health, 21, 811. 10.1186/s12889-021-10897-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammouri, A. A. , Tailakh, A. K. , Muliira, J. K. , Geethakrishnan, R. , & Al Kindi, S. N. (2015). Patient safety culture among nurses. International Nursing Review, 62(1), 102–110. 10.1111/inr.12159 [DOI] [PubMed] [Google Scholar]
- An, Y. , Yang, Y. , Wang, A. , Li, Y. , Zhang, Q. , Cheung, T. , Ungvari, G. S. , Qin, M. Z. , An, F. R. , & Xiang, Y. T. (2020). Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID‐19 outbreak. Journal of Affective Disorders, 276, 312–315. 10.1016/j.jad.2020.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan, T. A. , Leape, L. L. , Laird, N. M. , Hebert, L. , Localio, A. R. , Lawthers, A. G. , Newhouse, J. P. , Weiler, P. C. , & Hiatt, H. H. (2004). Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical Practice Study I. 1991. Quality & Safety in Health Care, 13(2). 10.1136/qshc.2002.003822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho, E. , Chin, D. L. , Kim, S. , & Hong, O. (2016). The relationships of nurse staffing level and work environment with patient adverse events. Journal of Nursing Scholarship, 48(1), 74–82. 10.1111/jnu.12183 [DOI] [PubMed] [Google Scholar]
- Department of Jordanian Statistics (2018). Statistical yearbook of Jordan. http://dosweb.dos.gov.jo/databank/yearbook/YearBook_2018.pdf
- Dos Santos, R. R. , Silva, D. A. , de Paiva, M. C. M. , & Spiri, W. C. (2018). Association between nurses' quality of life and work environment. ACTA Paulista De Enfermagem, 31, 472–479. 10.1590/1982-0194201800067 [DOI] [Google Scholar]
- Duarte, I. , Teixeira, A. , Castro, L. , Marina, S. , Ribeiro, C. , Jácome, C. , Martins, V. , Ribeiro‐Vaz, I. , Pinheiro, H. C. , Silva, A. R. , Ricou, M. , Sousa, B. , Alves, C. , Oliveira, A. , Silva, P. , Nunes, R. , & Serrão, C. (2020). Burnout among Portuguese healthcare workers during the COVID‐19 pandemic. BMC Public Health, 20(1), 10.1186/s12889-020-09980-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fradelos, E. , Mpelegrinos, S. , Mparo, C. , Vassilopoulou, C. , Argyrou, P. , Tsironi, M. , Zyga, S. , & Theofilou, P. (2014). Burnout syndrome impacts on quality of life in nursing professionals: The contribution of perceived social support. Progress in Health Sciences, 4(1), 102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golembiewski, R. , Munzenrider, R. , & Stevenson, J. (1988). Phases of burnout: Developments in concepts and applications. In Choice Reviews Online, 10.5860/choice.26-5926 [DOI]
- Hair, J. , Black, W. C. , Babin, B. , Anderson, R. , & Tatham, R. L. (2010). SEM: An introduction. Multivariate data analysis: A global perspective (pp. 7th ed., 629–686). Pearson Education. [Google Scholar]
- Ibrahim, N. K. , Alzahrani, N. A. , Batwie, A. A. , Abushal, R. A. , Almogati, G. G. , Sattam, M. A. , & Hussin, B. K. (2016). Quality of life, job satisfaction and their related factors among nurses working in king Abdulaziz University Hospital, Jeddah. Saudi Arabia. Contemporary Nurse, 52(4), 486–498. 10.1080/10376178.2016.1224123 [DOI] [PubMed] [Google Scholar]
- Ioannou, P. , Katsikavali, V. , Galanis, P. , Velonakis, E. , Papadatou, D. , & Sourtzi, P. (2015). Impact of job satisfaction on Greek nurses' health‐related quality of life. Safety and Health at Work, 6(4), 324–328. 10.1016/j.shaw.2015.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakemam, E. , Chegini, Z. , Rouhi, A. , Ahmadi, F. , & Majidi, S. (2021). Burnout and its relationship to self‐reported quality of patient care and adverse events during COVID‐19: A cross‐sectional online survey among nurses. Journal of Nursing Management, 10.1111/jonm.13359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatatbeh, H. , Al‐Dwaikat, T. , Oláh, A. , Onchonga, D. , Hammoud, S. , Amer, F. , Prémusz, V. , & Pakai, A. (2021). The relationships between paediatric nurses' social support, job satisfaction and patient adverse events. Nursing Open, 1–8, 10.1002/nop2.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatatbeh, H. , Pakai, A. , Al‐Dwaikat, T. , Onchonga, D. , Amer, F. , Prémusz, V. , & Oláh, A. (2021). Nurses' burnout and quality of life: A systematic review and critical analysis of measures used. Nursing Open, 1–11, 10.1002/nop2.936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatatbeh, H. , Pakai, A. , Pusztai, D. , Szunomár, S. , Fullér, N. , Kovács Szebeni, G. , Siket, A. , Zrínyi, M. , & Oláh, A. (2020). Burnout and patient safety: A discriminant analysis of paediatric nurses by low to high managerial support. Nursing Open, 8, 982–989. 10.1002/nop2.708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatatbeh, M. , Alhalaiqa, F. , Khasawneh, A. , Al‐tammemi, A. B. , Khatatbeh, H. , Alhassoun, S. , & Al Omari, O. (2021). The experiences of nurses and physicians caring for COVID‐19 patients: Findings from an exploratory phenomenological study in a high case‐load country. International Journal of Environmental Research and Public Health, 18(17), 1–17. 10.3390/ijerph18179002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khatatbeh, M. , Khasawneh, A. , Hussein, H. , Altahat, O. , & Alhalaiqa, F. (2021). Psychological impact of COVID‐19 pandemic among the general population in Jordan. Frontiers in Psychiatry, 12, 10.3389/fpsyt.2021.618993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, H.‐J. , & Yom, Y.‐H. (2014). Structural equation modeling on burnout in clinical nurses based on CS‐CF model. Journal of Korean Academy of Nursing, 44(3), 259–269. 10.4040/jkan.2014.44.3.259 [DOI] [PubMed] [Google Scholar]
- Kowitlawkul, Y. , Yap, S. F. , Makabe, S. , Chan, S. , Takagai, J. , Tam, W. W. S. , & Nurumal, M. S. (2019). Investigating nurses' quality of life and work‐life balance statuses in Singapore. International Nursing Review, 66(1), 61–69. 10.1111/inr.12457 [DOI] [PubMed] [Google Scholar]
- Kristensen, T. S. , Borritz, M. , Villadsen, E. , & Christensen, K. B. (2005). The Copenhagen burnout inventory: A new tool for the assessment of burnout. Work and Stress, 19(3), 192–207. 10.1080/02678370500297720 [DOI] [Google Scholar]
- Lee, R. L. , & Ashforth, B. E. (1996). A meta‐analytic examination of the correlates of the three dimensions of job burnout. Journal of Applied Psychology, 81(2), 123–133. 10.1037/0021-9010.81.2.123 [DOI] [PubMed] [Google Scholar]
- Leiter, M. P. , & Maslach, C. (1988). The impact of interpersonal environment on burnout and organizational commitment. Journal of Organizational Behavior, 9(4), 297–308. 10.1002/job.4030090402 [DOI] [Google Scholar]
- Li, D. , Wang, Y. Y. , Yu, H. , Duan, Z. , Peng, K. , Wang, N. , Zhou, Q. , Hu, X. , Fang, K. , Wilson, A. , Ou, J. , & Wang, X. (2021). Occupational burnout among frontline health professionals in a high‐risk area during the COVID‐19 outbreak: A structural equation model. Frontiers in Psychiatry, 12, 10.3389/fpsyt.2021.575005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, W. Q. , Wu, J. , Yuan, L. X. , Zhang, S. C. , Jing, M. J. , Zhang, H. S. , Luo, J. L. , Lei, Y. X. , & Wang, P. X. (2015). Workplace violence and job performance among community healthcare workers in China: The mediator role of quality of life. International Journal of Environmental Research and Public Health, 12(11), 14872–14886. 10.3390/ijerph121114872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C. , & Leiter, M. P. (2008). Early predictors of job burnout and engagement. Journal of Applied Psychology, 93(3), 498–512. 10.1037/0021-9010.93.3.498 [DOI] [PubMed] [Google Scholar]
- Moradi, T. , Maghaminejad, F. , & Azizi‐Fini, I. (2014). Quality of working life of nurses and its related factors. Nursing and Midwifery Studies, 3(2), 10.5812/nms.19450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moumtzoglou, A. (2010). Factors impeding nurses from reporting adverse events. Journal of Nursing Management, 18(5), 542–547. 10.1111/j.1365-2834.2010.01049.x [DOI] [PubMed] [Google Scholar]
- Mudallal, R. H. , Othman, W. A. M. , & Al Hassan, N. F. (2017). Nurses' burnout: The influence of leader empowering behaviors, work conditions, and demographic traits. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 54, 10.1177/0046958017724944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nantsupawat, A. , Nantsupawat, R. , Kunaviktikul, W. , Turale, S. , & Poghosyan, L. (2016). Nurse burnout, nurse‐reported quality of care, and patient outcomes in Thai hospitals. Journal of Nursing Scholarship, 48(1), 83–90. 10.1111/jnu.12187 [DOI] [PubMed] [Google Scholar]
- Naz, S. , Hashmi, A. M. , & Asif, A. (2016). Burnout and quality of life in nurses of a tertiary care hospital in Pakistan. Journal of Pakistan Medical Association, 66(5), 532–536. [PubMed] [Google Scholar]
- Nursalam, N. , Fibriansari, R. D. , Yuwono, S. R. , Hadi, M. , Efendi, F. , & Bushy, A. (2018). Development of an empowerment model for burnout syndrome and quality of nursing work life in Indonesia. International Journal of Nursing Sciences, 5(4), 390–395. 10.1016/j.ijnss.2018.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padilha, K. G. , Barbosa, R. L. , Andolhe, R. , Oliveira, E. M. , Ducci, A. J. , Bregalda, R. S. , & Dal Secco, L. M. (2017). Nursing workload, stress or burnout, satisfaction and incidents in a trauma intensive care units. Texto E Contexto Enfermagem, 26(3), 1–8. 10.1590/0104-07072017001720016 [DOI] [Google Scholar]
- Ribeiro, E. K. D. A. , Santos, R. C. D. , Araújo‐Monteiro, G. K. N. D. , Brandão, B. M. L. D. S. , Silva, J. C. D. , & Souto, R. Q. (2021). Influence of burnout syndrome on the quality of life of nursing professionals: Quantitative study. Revista Brasileira De Enfermagem, 74(suppl 3). 10.1590/0034-7167-2020-0298 [DOI] [PubMed] [Google Scholar]
- Stamm, B. H. (2010). The concise ProQOL manual. (2nd ed.). ProQOL.org. [Google Scholar]
- Van Bogaert, P. , Timmermans, O. , Weeks, S. M. , van Heusden, D. , Wouters, K. , & Franck, E. (2014). Nursing unit teams matter: Impact of unit‐level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events‐A cross‐sectional survey. International Journal of Nursing Studies, 51(8), 1123–1134. 10.1016/j.ijnurstu.2013.12.009 [DOI] [PubMed] [Google Scholar]
- Vogus, T. J. , Ramanujam, R. , Novikov, Z. , Venkataramani, V. , & Tangirala, S. (2020). adverse events and burnout: The moderating effects of workgroup identification and safety climate. Medical Care, 58(7), 594–600. 10.1097/MLR.0000000000001341 [DOI] [PubMed] [Google Scholar]
- Von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. (2014). The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495–1499. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- WHOQOL (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. 10.1016/0277-9536(95)00112-K [DOI] [PubMed] [Google Scholar]
- WHOQOL‐Group (1998). Development of the World Health Organization WHOQOL‐BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. [DOI] [PubMed] [Google Scholar]
- Woodhead, E. L. , Northrop, L. , & Edelstein, B. (2016). Stress, social support, and burnout among long‐term care nursing staff. Journal of Applied Gerontology, 35(1), 84–105. 10.1177/0733464814542465 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (1996). WHOQOL‐BREF: Introduction, administration, scoring and generic version of the assessment: Field trial version (Issue December). World Health Organization. [Google Scholar]
- Zeng, J. Y. , An, F. R. , Xiang, Y. T. , Qi, Y. K. , Ungvari, G. S. , Newhouse, R. , Yu, D. S. F. , Lai, K. Y. C. , Yu, L. Y. , Ding, Y. M. , Tang, W. K. , Wu, P. P. , Hou, Z. J. , & Chiu, H. F. K. (2013). Frequency and risk factors of workplace violence on psychiatric nurses and its impact on their quality of life in China. Psychiatry Research, 210(2), 510–514. 10.1016/j.psychres.2013.06.013 [DOI] [PubMed] [Google Scholar]
- Zhang, X. , Jiang, X. , Ni, P. , Li, H. , Li, C. , Zhou, Q. , Ou, Z. , Guo, Y. , & Cao, J. (2021). Association between resilience and burnout of front‐line nurses at the peak of the COVID‐19 pandemic: Positive and negative affect as mediators in Wuhan. International Journal of Mental Health Nursing, 10.1111/inm.12847 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data set used in this research is available from the corresponding author upon a reasonable request.


