Abstract
The rapid spread of the Delta variant suggests that SARS‐CoV‐2 will likely be rampant for months or years and could claim millions of more lives. All the known vaccines cannot well defeat SARS‐CoV‐2 due to their limited efficacy and production efficiency, except for the neglected live‐attenuated vaccines (LAVs), which could have a much higher efficacy and much higher production efficiency than other vaccines. LAVs, like messiahs, have defeated far more pathogenic viruses than other vaccines in history, and most current human vaccines for viral diseases are safe LAVs. LAVs can block completely infection and transmission of relevant viruses and their variants. They can hence inhibit the emergence of vaccine‐escape and virulence‐enhancing variants and protect immunologically abnormal individuals better in general. The safety of COVID‐19 LAVs, which could save millions of more lives, can be solidly guaranteed through animal experiments and clinical trials. The safety of COVID‐19 LAVs could be greatly enhanced with intramuscular or oral administration, or administration along with humanized neutralizing monoclonal antibodies. Together, extensive global collaboration, which can greatly accelerate the development of safe COVID‐19 LAVs, is imminently needed.
Keywords: COVID‐19, pandemic, policy, safety, SARS‐CoV‐2, vaccine, virus
1. THE CURRENT SITUATIONS AND FUTURE RISKS
Coronavirus disease 2019 (COVID‐19) caused by the novel coronavirus SARS‐CoV‐2 has led to 4.5 million deaths. 1 This number does not include many deaths undetected during the pandemic period. To minimize cases and deaths, many countries have implemented strict social distancing, mass surveillance, and mass quarantine. However, these measures are very tough and costly, and hence it is highly desirable that vaccines defeat SARS‐CoV‐2.
To date, several COVID‐19 vaccines, such as inactivated whole‐virus vaccines, adenovirus‐vector vaccines, recombinant protein vaccines, and message RNA vaccines (mRVs), have been marketed, and billions of people have been vaccinated. 1 These vaccines have given the world the hope of defeating SARS‐CoV‐2.
Recently, the Delta (B.1.617.2) variant, which is more contagious and pathogenic than the original SARS‐CoV‐2 strain and partially nullifies all marketed COVID‐19 vaccines, has spread to 174 countries, territories, or areas. 1 , 2 , 3 , 4 , 5 This broke the global hope to defeat SARS‐CoV‐2 with vaccines and suggested that SARS‐CoV‐2 will likely be rampant for months or years and could claim millions of more lives.
Mass vaccination with the marketed COVID‐19 vaccines can control the disease, namely greatly reduce cases and deaths, for some time. However, because these vaccines are all partially efficacious, 2 , 3 , 4 they cannot defeat the virus for long. Among the marketed COVID‐19 vaccines, mRVs are the most efficacious, although they cause fever in around 2% of recipients, and their efficacy has declined from ∼91% to ∼66% due to the widespread Delta variant. 2 The efficacy of a COVID‐19 inactivated vaccine in China has declined to 59%. 5 Their efficacy will likely decline further due to the decrease of antibody titers in recipients and the accumulation of more mutations in SARS‐CoV‐2 over time. 3
All the marketed COVID‐19 vaccines have relatively low production efficiency, compared to the huge demand for combating the pandemic. 1 , 4 Consequently, as of 30 August 2021, COVID‐19 vaccination coverage in many countries has not reached 10%. 1 Particularly, although COVID‐19 mRVs are more efficacious than other marketed COVID‐19 vaccines, it should take years for the world to produce enough COVID‐19 mRVs for most people on the globe. 1 , 4 Their stringent requirements for storage and high prices also impede their global application. 4
In genomic sequences, SARS‐CoV‐2 is phylogenetically close to, but also distinct from, SARS‐CoV‐1, the virus causing the severe acute respiratory syndrome (SARS) outbreak in 2003. 6 They share the same receptor and cause similar diseases, which suggests that SARS‐CoV‐2 is flexible enough to change its genomes. Therefore, the emergence of vaccine‐escape variants of SARS‐CoV‐2 is likely unavoidable, if their transmissions are only partially blocked by vaccination. Hence, the world will likely fall into the disastrous and costly cycle of repeated emergence of vaccine‐escaping variants followed by repeated updating of vaccines. 7 Similar scenarios have occurred in the mass vaccination for influenza and other viral diseases. 8 , 9 Together, SARS‐CoV‐2 and vaccines could have a seesaw relationship, namely only one side could win in the long run (Figure 1).
Figure 1.
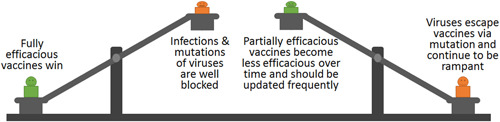
The potential seesaw game between SARS‐CoV‐2 and vaccines in the long run
After the COVID‐19 pandemic, SARS‐CoV‐2 should cause much fewer deaths annually due to increased human herd immunity against the virus. 10 However, variants of SARS‐CoV‐2 could cause seasonal COVID‐19 outbreaks, which could be parallel to seasonal influenza in severity and a little severer than the common cold, due to the intrinsic pathogenesis of SARS‐CoV‐2. 6 , 7 Therefore, seasonal COVID‐19 could cause annually over 200 000 deaths, even if some people are vaccinated with partially efficacious COVID‐19 vaccines, parallel to the fact that seasonal influenza annually causes 290 000−650 000 deaths, 8 even if some people are vaccinated with partially efficacious influenza vaccines.
Meanwhile, SARS‐CoV‐2 could become highly virulent and cause millions of deaths again in the future at a low possibility, due to rare random genomic mutations, like the fact that multiple RNA viruses, for example, avian influenza viruses, 11 porcine reproductive and respiratory syndrome, 12 and porcine epidemic diarrhea virus (a coronavirus), 13 have become highly virulent through random genomic mutations in the past 20 years, and caused large‐scale deadly outbreaks in animals.
2. ADVANTAGES OF LIVE‐ATTENUATED VACCINES (LAVS)
First, LAVs, like messiahs, have defeated far more viral diseases than other vaccines. LAVs have eradicated smallpox and have nearly eradicated poliomyelitis. Currently, 11 of the 19 human viral infectious diseases in China or the United States controlled with vaccines are well controlled with safe LAVs (Table 1). 7 , 9
Table 1.
Vaccines for human viral diseases currently used in China or the United States
| Viral disease | Vaccine |
|---|---|
| Varicella (chickenpox) | LAV |
| Measles | LAV |
| Mumps | LAV |
| Rubella | LAV |
| Rotavirus infection | LAV |
| Yellow fever | LAV |
| Rabies | LAV, IV |
| Japanese encephalitis | LAV, IV |
| Polio | LAV, IV |
| Influenza | LAV, IV |
| Hepatitis A | LAV, IV |
| Human papillomavirus infection | RPV |
| Hepatitis B | RPV |
| Hepatitis E | RPV |
| Hemorrhagic fever | IV |
| Hand‐foot and mouth disease | IV |
| Tickborne encephalitis | IV |
| COVID‐19 | IV, VV, RPV, mRV |
| Adenovirus infection | LUV |
Abbreviations: IV, inactivated vaccine; mRV, message RNA vaccine; LAV, live‐attenuated vaccine; LUV, live‐unattenuated vaccine; RPV, recombinant protein vaccine; VV, vector vaccine.
Second, LAVs can be much more efficacious than other vaccines. In structure and mechanism, safe LAVs are akin to perfect mRVs or vector vaccines, and they uniquely produce multiple, endogenous, and relatively large quantities of viral antigens (Table 2). 4 , 7 , 9 Usually exogenous antigens can induce only humoral immunity, while endogenous antigens can induce both humoral immunity and cell‐mediated immunity. 4 , 7 Therefore, LAVs could induce stronger immunity than mRVs, vector vaccines, and other vaccines, and could hence completely block infection and transmission of relevant viruses and their variants.
Table 2.
Delivery of antigens of different COVID‐19 vaccines
| Vaccine type | Delivering multiple antigens | Delivering endogenous antigens | Delivering large quantity of antigens | Basic mode for production or delivery of antigens |
|---|---|---|---|---|
| RPV | × | × | √ | Direct injection |
| IV | √ | × | √ or × | Direct injection |
| LAV | √ | √ | √ | Translation of antigen‐encoding message RNA via virus replication in recipient cells |
| mRV | × | √ | √ | Translation of injected antigen‐encoding message RNA in recipient cells |
| VV | × | √ | √ or × | Translation of the message RNA transcribed from antigen‐encoding DNA sent into recipient cells by virus vectors |
Abbreviations: IV, inactivated vaccine; LAV, live‐attenuated vaccine; mRV, message RNA vaccine; RPV, recombinant protein vaccine; VV, vector vaccine.
Third, many factories in the world produce LAVs, and LAVs have much higher production efficiency with much less production cost than other vaccines. For example, polio LAVs cost less than polio inactivated vaccines by ∼85%. 9 A dose of COVID‐19 LAV could contain only 105 viruses, while a dose of COVID‐19 inactivated vaccine should contain over 1010 viruses. 14 , 15 Therefore, LAVs could save much more time and money than other vaccines for the world to produce and obtain enough COVID‐19 vaccines for all people in the world. Additionally, LAVs could have much higher inoculation efficiency than the current COVID‐19 vaccines, if the LAVs are nasally or orally administrated. 4 , 9 , 16 Such LAVs are highly needed by many low‐income countries.
Fourth, LAVs can circumvent the safety risks of other vaccines, such as leakage of pathogenic viruses from factories for the production of inactivated vaccines, infection with incompletely inactivated vaccines, the side effect of vaccine adjuvants or vaccine‐delivery agents, and antibody‐dependent enhancement (namely that vaccination cannot reduce but enhance infection risk) of partially efficacious vaccines. 7
Fifth, with their high efficacy, LAVs can well block infection and transmission of relevant viruses and their variants, and so they can inhibit vaccine‐escape or virulence‐enhancing mutations of these viruses (Figure 1). No vaccine‐escape or virulence‐enhancing variants of the viruses causing the 11 diseases listed in Table 1 controlled with LAVs have been identified in the past decades. 7 , 9 Therefore, from a panoramic viewpoint, these effects of LAVs can provide much better protection for all people including immunologically abnormal individuals than other vaccines.
Sixth, if a cheap, safe, and fully efficacious COVID‐19 LAV is marketed globally before August 2022, it could eliminate the last one or two waves of the COVID‐19 pandemic, and save ∼1 million more lives than other vaccines. If the COVID‐19 LAV is marketed globally after 2023, it could prevent annually over 100 000 deaths caused by seasonal COVID‐19, provided that seasonal COVID‐19 is parallel in severity to seasonal influenza and over 50% of susceptible people worldwide are vaccinated with the COVID‐19 LAV, as assessed roughly in Section 1.
3. DISADVANTAGES OF LAVS AND SOLUTIONS
Besides the above advantages, LAVs have several disadvantages, all of which can be solved for some (not all) LAVs.
First, LAVs are unsuitable for viruses that replicate poorly in vitro systems. COVID‐19 LAVs circumvent this problem because SARS‐CoV‐2 replicates well in cell culture.
Second, it is difficult to obtain safe LAV seeds. Traditionally, LAV seeds were from the viruses phylogenetically close to the targeted pathogenic viruses (e.g., the seed of smallpox LAV), or attenuated through serial passage in heterogeneous hosts (e.g., the seed of measles LAV). 9 Nowadays, most LAV seeds are created through modern genetic technologies, such as deletion of virulence genes or motifs, deoptimization of codons, optimization of viral polymerases through reverse genetics, 7 , 14 , 15 , 16 which can more precisely and more rapidly attenuate pathogenic viruses and better maintain their efficacy than traditional routes.
Third, LAVs can revert to their virulence through transmission in humans. Social distancing, disinfection, simultaneous inoculation of LAVs, and modern genetic technologies (e.g., cold adaption and optimization of viral polymerases) can all minimize transmission of LAVs in humans and hence minimize the risk of virulence reversion. 7 , 14 , 16
Fourth, LAVs can be pathogenic to some immunologically abnormal individuals. Immunologically abnormal individuals can avoid this risk through social distancing, mask‐wearing, and disinfection for weeks after the mass vaccination campaign, and they should always take these measures to avoid infections of various other pathogens. Moreover, all the 11 human LAVs listed in Table 1 are safe for most immunologically abnormal individuals. 9 , 17 Additionally, most immunologically abnormal individuals could be inoculated with other types of vaccines in advance, and from a panorama view, LAVs can provide much better protection for immunologically abnormal individuals, as mentioned in Section 2.
Fifth, recombination between LAVs and wild‐type viruses can generate novel variants. 18 This risk is largely acceptable, because the resultant recombinant viruses are usually not more pathogenic and transmissible than wild‐type viruses, as LAVs have genetic mutations which greatly reduce the viral pathogenicity and transmissibility. 9 , 14 , 15 , 16 LAVs for coronaviruses have been safely used worldwide in chickens and pigs for decades, and no LAV‐recombinant viruses more virulent than wild‐type avian or swine coronaviruses have been identified. 12 By contrast, a variant of a common porcine coronavirus, which was not a vaccine recombinant, became much more deadly and sparked a terrible swine pandemic in the 2010s, leading to 7 million deaths of pigs in the United States with a mortality of around 10%. 13
Sixth, LAVs can be polluted with other pathogenic viruses. This safety risk can be avoided and has been widely avoided through modern administration and technologies. 9
4. ROBUST GUARANTEE OF THE SAFETY OF COVID‐19 LAVS
Nevertheless, due to safety concerns of LAVs, LAVs have been neglected in terms of combating the COVID‐19 pandemic. 4 , 19 Of the 92 COVID‐19 vaccines under clinical trials or having been permitted as of August 30, 2021, only one LAV, namely COVI‐VAC, is under Phase 1 clinical trial with the support of only one company (Codagenix, Inc.). 14
History has demonstrated that all types of vaccines can be safe or dangerous and that strict animal experiments and clinical trials can differentiate between safe vaccines and dangerous vaccines. 9 For example, clinical trials revealed the severe ADE effect of the inactivated vaccine FI‐RSV for respiratory syncytial virus and the adenovirus vector vaccine for human immunodeficiency virus. 9 Meanwhile, various LAVs have been proved safe through animal experiments and clinical trials, and consequently, every year millions of children are safely inoculated with various LAVs. 9 LAVs for coronaviruses have been safely used worldwide in chickens and pigs for decades, and they have induced the most consistent protection against avian and swine coronaviruses. 20 Moreover, as detailed in Section 3, modern administration and novel technologies could further enhance the safety of LAVs and better circumvent all potential safety risks for some LAVs than traditional technologies. These facts suggest that COVID‐19 LAVs could be highly safe.
If a COVID‐19 LAV, like polio LAVs, 17 causes <1 COVID‐19 case per million vaccinated people, most of these patients can be identified and treated in time. 7 Additionally, these patients could be infected naturally with wild‐type SARS‐CoV‐2, if they have not been inoculated with a fully efficacious COVID‐19 vaccines. 16 , 17
The safety of COVID‐19 LAVs could be further enhanced through intramuscular injection or oral administration, to avoid the risk of vaccine‐induced pneumonia. This mechanism has been applied safely for 40 years for preventing adenovirus‐associated acute respiratory disease in US recruits, through oral administration of enteric‐coated capsules containing wild‐type adenoviruses, to bypass the pathogenesis site of the lungs. 21
The safety of COVID‐19 LAVs could be further enhanced if they are inoculated along with neutralizing antibodies, and the LAVs thereby become live immune‐complex vaccines (LICVs). 22 LICVs could be as highly efficacious as LAVs partially due to immune opsonization, and much safer than LAVs due to neutralization of the antibodies, and could provide protection immediately after vaccination. 22 , 23 , 24 Mass vaccination of LICVs eliminated rinderpest from southern Africa in 1905 and Russia in 1928, and prevented yellow fever relatively well in the 1930s. 22 , 23 LICVs have been widely used for decades for controlling avian infectious diseases. 22 , 24 Previously, it was difficult to produce vast safe neutralizing antibodies from human sera for human LICV production. Now, the production of humanized neutralizing monoclonal antibodies has become highly efficient, and hence human LICVs could be rejuvenated. 25
5. SIGNIFICANCE OF GLOBAL COLLABORATION
Together, possibly only COVID‐19 LAVs could well defeat SARS‐CoV‐2, and their safety can be well guaranteed, for multiple reasons (Table 3). Therefore, extensive global collaboration, which can greatly accelerate the development of COVID‐19 LAVs, is imminently needed. A safe and efficacious COVID‐19 LAV could be marketed months or years earlier if over 20 countries actively accelerate the development of COVID‐19 LAVs. 9 , 16 If the COVID‐19 LAV was marketed one day earlier, thousands of more lives could be saved.
Table 3.
Reasons why the world should collaborate to accelerate the development of COVID‐19 live‐attenuated vaccines (LAVs)
| Order | Reason |
|---|---|
| 1 | Other vaccines have limited efficacy and limited production efficiency |
| 2 | LAVs have well defeated far more viruses for long than other vaccines |
| 3 | Most of the current human vaccines for viral diseases are safe LAVs |
| 4 | LAVs could be much cheaper and produced much faster than other vaccines |
| 5 | Safety of LAVs can be well guaranteed via animal experiments and clinical trials |
| 6 | Safety of LAVs can be better guaranteed with modern technologies |
| 7 | Safety of LAVs can be better guaranteed with novel administration routes |
| 8 | LAVs could block transmission of relevant viruses and their variants completely and thus inhibit virus mutation |
| 9 | LAVs could protect immunologically abnormal individuals better from a panorama view |
| 10 | COVID‐19 LAVs could save millions of more lives than other vaccines |
| 11 | Global collaboration could significantly accelerate the development of COVID‐19 LAVs |
Global collaboration could accelerate the development of COVID‐19 LAVs through constructing more LAV candidates and conducting more animal experiments and clinical trials, to evaluate the efficacy and safety of the LAVs, or to investigate other administration routes to enhance the safety of the LAVs as mentioned above.
The coming 2 years are favorable for LAVs to defeat SARS‐CoV‐2 because SARS‐CoV‐2 could diverge into only a few slightly distinct variants during this period, and many people would have obtained specific immunity through infection or vaccination. 7
CONFLICT OF INTERESTS
The author declares that there are no conflict of interests.
ETHICS STATEMENT
This article does not contain the participation of animals and humans.
ACKNOWLEDGMENTS
The author thanks Meng Yang for her helpful advice and assistance. This study was supported by the High‐Level Talent Fund of Foshan University (No. 20210036).
Chen J‐M. Should the world collaborate imminently to develop neglected live‐attenuated vaccines for COVID‐19? J Med Virol. 2021;94:82‐87. 10.1002/jmv.27335
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. WHO Coronavirus disease (COVID‐19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2. Fowlkes A, Gaglani M, Groover K, et al. Effectiveness of COVID‐19 vaccines in preventing SARS‐CoV‐2 infection among frontline workers before and during B.1.617.2 (Delta) variant predominance—eight U.S. locations, December 2020–August 2021. MMWR. 2021;70:1167‐1169. 10.15585/mmwr.mm7034e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nanduri S, Pilishvili T, Derado G, et al. Effectiveness of Pfizer‐BioNTech and Moderna Vaccines in preventing SARS‐CoV‐2 infection among nursing home residents before and during widespread circulation of the SARS‐CoV‐2 B.1.617.2 (Delta) Variant—National Healthcare Safety Network, March 1—August 1, 2021. MMWR. 2021;70(34):1163‐1166. 10.15585/mmwr.mm7034e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ndwandwe D, Wiysonge CS. COVID‐19 vaccines. Curr Opin Immunol. 2021;71:111‐116. 10.1016/j.coi.2021.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li XN, Huang Y, Wang W, et al. Efficacy of inactivated SARS‐CoV‐2 vaccines against the Delta variant infection in Guangzhou: a test‐negative case‐control real‐world study. Emerg Microbes Infect. 2021;10:1751‐1759. 10.1080/22221751.2021.1969291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li X, Chang J, Chen S, et al. Genomic feature analysis of Betacoronavirus provides insights into SARS and COVID‐19 pandemics. Front Microbiol. 2021;12:614494. 10.3389/fmicb.2021.614494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen JM, Sun YX, Chen JW. Potential for elimination of SAR‐CoV‐2 through vaccination as inspired by elimination of multiple influenza viruses through natural pandemics or mass vaccination. J Med Virol. 2020;92(11):2453‐2457. 10.1002/jmv.26162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO . Influenza seasonal. https://www.who.int/health-topics/influenza-seasonal#tab=tab_1
- 9. Nunnally BK, Turula VE, Sitrin RD. Vaccine Analysis Strategies, Principles, and Control. Spriner-Verlag; 2015. [Google Scholar]
- 10. Lavine JS, Bjornstad ON, Antia R. Immunological characteristics govern the transition of COVID‐19 to endemicity. Science. 2021;371:741‐745. 10.1126/science.abe6522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yang Y, Pang M, Du C, et al. Control of avian influenza in China: strategies and lessons. Transbound Emerg Dis. 2020;67:1463‐1471. 10.1111/tbed.13515 [DOI] [PubMed] [Google Scholar]
- 12. Rajkhowa TK, Lalnunthanga L, Hauhnar L, et al. Molecular detection and characterization of highly pathogenic porcine reproductive and respiratory syndrome virus from a natural outbreak in wild pigs, Mizoram, India. Transbound Emerg Dis. 2021;68. 10.1111/tbed.14296 [DOI] [PubMed] [Google Scholar]
- 13. Lin CM, Saif LJ, Marthaler D, Wang Q. Evolution, antigenicity and pathogenicity of global porcine epidemic diarrhea virus strains. Virus Res. 2016;226:20‐39. 10.1016/j.virusres.2016.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Y, Yang C, Song Y, et al. Scalable live‐attenuated SARS‐CoV‐2 vaccine candidate demonstrates preclinical safety and efficacy. Proc Natl Acad Sci USA. 2021;118:e2102775118. 10.1073/pnas.2102775118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Broadbent AJ, Santos CP, Anafu A, Wimmer E, Mueller S, Subbarao K. Evaluation of the attenuation, immunogenicity, and efficacy of a live virus vaccine generated by codon‐pair bias de‐optimization of the 2009 pandemic H1N1 influenza virus, in ferrets. Vaccine. 2016;34(4):563‐570. 10.1016/j.vaccine.2015.11.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bandyopadhyay AS, Garon J, Seib K, Orenstein WA. Poliomyelitis vaccination: past, present and future. Future Microbiol. 2015;10:791‐808. 10.2217/fmb.15.19 [DOI] [PubMed] [Google Scholar]
- 17. Strebel PM, Sutter RW, Cochi SL, et al. Epidemiology of poliomyelitis in the United States one decade after the last reported case of indigenous wild virus‐associated disease. Clin Infect Dis. 1992;14:568‐579. 10.1093/clinids/14.2.568 [DOI] [PubMed] [Google Scholar]
- 18. Sprygin A, Pestova Y, Bjadovskaya O, et al. Evidence of recombination of vaccine strains of lumpy skin disease virus with field strains, causing disease. PLOS One. 2020;15(5):e0232584. 10.1093/clinids/14.2.568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Okamura S, Ebina H. Could live attenuated vaccines better control COVID‐19? Vaccine. 2021:5719‐5726. 10.1016/j.vaccine.2021.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Saif LJ. Animal coronavirus vaccines: lessons for SARS. Dev Biol. 2004;119:129‐140. [PubMed] [Google Scholar]
- 21. Choudhry A, Mathena J, Albano JD, Yacovone M, Collins L. Safety evaluation of adenovirus type 4 and type 7 vaccine live, oral in military recruits. Vaccine. 2016;34:4558‐4564. 10.1016/j.vaccine.2016.07.033 [DOI] [PubMed] [Google Scholar]
- 22. Chen JM. Live unattenuated vaccines for controlling viral diseases, including COVID‐19. J Med Virol. 2021;93:1943‐1949. 10.1002/jmv.26453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Frierson JG. The yellow fever vaccine: a history. Yale J Biol Med. 2010;83:77‐85 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2892770/ [PMC free article] [PubMed] [Google Scholar]
- 24. Sedeik ME, El‐Shall NA, Awad AM, et al. Comparative evaluation of HVT‐IBD vector, immune complex, and live IBD vaccines against vvIBDV in commercial broiler chickens with high maternally derived antibodies. Animals (Basel). 2019;9:72. 10.3390/ani9030072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wan J, Xing S, Ding L, et al. Human‐IgG‐neutralizing monoclonal antibodies block the SARS‐CoV‐2 infection. Cell Rep. 2020;32:107918. 10.1016/j.celrep.2020.107918 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


