Abstract
The COVID‐19 pandemic is the first global “NASECH disaster,” owing to its natural hazard (NH) origin and unprecedented subsequent repercussions for global society (S), economy (EC), and health (H). Emergency health control measures required the implementation of compulsory mass quarantine (CMQ) or so‐called periods of “lockdown.” Yet, CMQ is an instrument with iatrogenic consequences, associated with a rise in societal levels of depression, anxiety, and posttraumatic stress. With a view to informing future crisis management, the study investigated sociodemographic factors associated with mental wellbeing during the March–April 2020 lockdown in the United Arab Emirates. Respondents (n = 1585) completed self‐report measures of depression (PHQ8) and generalized anxiety (GAD7). Rates of symptomatology were notably higher than those observed in similar UAE‐based studies before the pandemic. Younger age, urban‐dwelling, female‐gender, and a history of mental health problems were significant factors linked to elevated levels of depression and anxiety. Findings emphasize (1) the crucial need for psychological intervention after disasters and (2) the importance of strengthening the nexus at the intersection of public health and disaster risk reduction (DRR). Implications are that future pandemic containment would benefit from adopting new Health–DRR paradigms and ensuring these are effectively translated into disaster policy.
Keywords: COVID‐19, lockdown, mental health, NASECH disaster, pandemic, quarantine, risk management, UAE
摘要
新冠肺炎大流行是全球首个“NASECH灾害”,这归因于其自然灾害(NH)来源和对全球社会(S)、经济(EC)和卫生(H)造成的前所未有的后续影响。紧急卫生控制措施要求执行强制集中隔离(CMQ)或所谓的“封城”。不过,作为一项工具,CMQ具有医源性结果,后者与抑郁、焦虑和创伤后压力的社会层面的恶化相关。为对未来危机管理作贡献,本研究调查了2020年3月至4月封城期间与阿联酋地区居民的精神健康相关的社会‐人口统计因素。调查对象(n = 1585)完成了抑郁症(PHQ8)和一般化焦虑(GAD7)的自测衡量。症状率显著高于大流行前在类似研究(基于阿联酋)中得出的结果。与抑郁症和焦虑程度上升相关的显著因素包括年龄较小、居住在城市、女性以及精神健康问题史。研究发现强调了(1)在灾后进行心理干预(PIAD)这一关键需求;(2)强调公共卫生和灾害风险减少(DRR)二者之间复杂关系的重要性。得出的意义:采纳新的卫生‐DRR范式和确保范式有效转化为灾害政策,将有益于未来大流行的响应措施。
Resumen
La pandemia de COVID‐19 es el primer "desastre NASECH" mundial, debido a su origen de peligros naturales (NH) y las repercusiones posteriores sin precedentes para la sociedad (S), la economía (CE) y la salud (H) globales. Las medidas de control de la salud de emergencia requirieron la implementación de cuarentena masiva obligatoria (CMQ), o los llamados períodos de "bloqueo". Sin embargo, CMQ es un instrumento con consecuencias iatrogénicas, asociadas con un aumento en los niveles sociales de depresión, ansiedad y estrés postraumático. Con miras a informar la futura gestión de crisis, el estudio investigó los factores sociodemográficos asociados con el bienestar mental durante el cierre de marzo a abril de 2020 en los Emiratos Árabes Unidos. Los encuestados (n = 1585) completaron medidas de autoinforme de depresión (PHQ8) y ansiedad generalizada (GAD7). Las tasas de sintomatología fueron notablemente más altas que las observadas en estudios similares realizados en los Emiratos Árabes Unidos antes de la pandemia. La edad más joven, la vivienda urbana, el sexo femenino y un historial de problemas de salud mental fueron factores importantes relacionados con niveles elevados de depresión y ansiedad. Los hallazgos enfatizan (1) la necesidad crucial de una intervención psicológica después de los desastres (PIAD) y (2) la importancia de fortalecer el nexo en la intersección de la salud pública y la reducción del riesgo de desastres (RRD). Las implicaciones son que la futura contención de una pandemia se beneficiaría de la adopción de nuevos paradigmas de salud y reducción del riesgo de desastres y de garantizar que estos se traduzcan efectivamente en políticas de desastres.
INTRODUCTION AND BACKGROUND
COVID‐19: The first global NASECH disaster
2020 was supposed to be the year marking significant 5‐year milestones for progress on three key international programs: the 2030 Agenda for Sustainable Development with its 17 Sustainable Development Goals (SDGs), the Paris Agreement on Climate Change, and the Sendai Framework on Disaster Risk Reduction (DRR) 2015–2030, all of which were adopted by UN member states in 2015. From the perspective of working towards greater global sustainability, the mood was, therefore, one of optimism at the onset of 2020, and the year was positioned as one of renewed action by the UN Secretary‐General (Djalante et al., 2020). As it turned out in contrast, 2020 will doubtless be remembered by history as the year the world staggered under the global health emergency and socioeconomic crisis brought about by the advent of the novel Coronavirus disease (COVID‐19). This virulent new respiratory disease was first reported in Wuhan, China in December 2019. Due to the availability and ease of modern international air travel, COVID‐19 spread worldwide at an alarming pace. Within just three short months of its appearance, on March 11, 2020, the World Health Organisation (WHO) declared COVID‐19 a global pandemic (Zhang and Shaw, 2020). As of September 01, 2021, there were more than 217 million confirmed cases and sadly over 4.5 million related deaths worldwide (WHO, 2021), with fatalities continuing to mount on a daily basis.
According to the WHO (2011), health emergencies have assumed increasing attention during the past few decades, typified by major outbreaks of new infectious diseases (e.g., SARS, MERS, influenza H1N1, and H5N1) and the re‐emergence of familiar adversaries such as cholera and Ebola. Biological hazards and risks are specifically mentioned within the agreed “scope and purpose” of the Sendai Framework (UNISDR, 2015). More recently, a review of hazard definitions and classification was published by the United Nations (2020), through the joint efforts of the United Nations Office for Disaster Risk Reduction (UNDRR) and the International Science Council (ISC). In that technical report, infectious human disease is listed under the group of biological hazards, whereas epidemic is mentioned as one example of a slow‐onset disaster that emerges gradually over time.
The coronavirus outbreak is considered a health emergency first and foremost, because the disease is highly contagious and potentially fatal, with the elderly and those with chronic underlying poor health most at risk. However, the multiple cascading and significant impacts of the ensuing pandemic leading to the geopolitical crisis we see today place the pandemic squarely within the realm of global disasters. No universally agreed definition exists for what actually constitutes a disaster (Smith, 2013), but this is generally recognized to be an event where the severity of human, economic or environmental consequences is so great that the functioning of society at any scale is seriously disrupted. A disaster triggered by a natural hazard (e.g., typhoon, flood, volcanic eruption) tends to be referred to in the vernacular as a “natural disaster,” whereas the alternative term “NATECH disaster” has been used to encompass the combination of (cascading) effects of natural hazards that trigger consequent technological failures (Steinberg et al., 2008). For example, the Great East Japan Earthquake of March 2011, and the subsequent Tōhoku tsunami that was unleashed, caused the Fukushima nuclear reactor explosion and resulting widespread radiation leak (Goff & Terry, 2012; Krausmann et al., 2019). Here, we describe the COVID‐19 pandemic as the first global “NASECH disaster.” We propose this new term because the pandemic disaster stems from a natural hazard (NA) origin (infectious disease outbreak), whereas its severe impacts extend fully across the social (S), economic (EC), and health (H) spheres of most countries affected.
It is certainly the case that many disaster events over recent decades have either afflicted extensive regions and/or had costly and lasting socioeconomic repercussions, such as witnessed in the aftermath of the highly destructive 2004 Indian Ocean Tsunami (ADPC, 2006) and devastating 2005 Hurricane Katrina in the United States (Blake et al., 2011). There have also been other disease pandemics in past centuries and in more recent times alike, such as the Black Death (bubonic plague) in 14th century Europe and the Spanish Flu (influenza) of 1918–19 (Spreeuwenberg et al., 2018). Yet, simply viewing the numbers of fatalities alone, Table 1 illustrates how the present COVID‐19 pandemic (more than 4.5 million deaths so far) already contends as one of the deadliest disasters over the last 100 years. What the full global social ramifications will be, and how long the deepening economic recessions due to the pandemic will last, are questions only future historians can answer.
Table 1.
Comparing the deadliest disasters caused by different types of natural hazards over the past 100 years
| Rank | Estimate of death tolla, b | Type of natural hazard | Named event | Country or region affected | Date |
|---|---|---|---|---|---|
| 1 | 17.4 million+ | Disease outbreak | Spanish flu | Worldwide | February 1918–April 1920 |
| 2 | >500,000 | Tropical cyclone | 1970 Bhola cyclone | East Pakistan (Bangladesh) | November 13, 1970 |
| 3 | 227,898 | Tsunami | 2004 Indian Ocean tsunami | Indian Ocean | December 26, 2004 |
| 4 | 100,000−316,000 | Earthquake | 2010 Haiti earthquake | Haiti | January 12, 2010 |
| 5 | 150,000 | River flood | 1931 Yangtze–Huai River floods | China | June–August 1931 |
| 6 | 100,000 | Landslide | 1920 Haiyuan landslides | China | December 16, 1920 |
| 7 | 70,000 | Heatwave | 2003 European heatwave | Europe | Summer 2003 |
| 8 | 23,000 | Volcanic eruption | Armero tragedy | Colombia | November 13, 1985 |
| 9 | 4000 | Blizzard | 1972 Iran blizzard | Iran | Winter 1972 |
| 10 | 1744 | Limnic eruption (CO2 release) | Lake Nyos disaster | Cameroon | August 21, 1986 |
| 11 | 1300 | Tornado | Daulatpur–Saturia tornado | Bangladesh | April 26, 1989 |
| 12 | 1200 | Wildfire | Kursha‐2 Fire | Soviet Union (Russia) | August 3, 1936 |
Data (unverified) from various sources, including media accounts, encyclopaedic entries, online databases.
Direct death toll, not including subsequent secondary effects such as disease or starvation.
Crisis management through compulsory mass quarantine (CMQ)
The task of authorities during any catastrophe is to implement coordinated strategies to reduce the scope (type) and scale (severity and extent) of negative impacts, while relief agencies provide immediate assistance to disaster victims. Disaster risk management for health in particular requires a multisectoral approach. According to the WHO (2011), this should encompass: “systematic analysis and management of health risks, through a combination of (1) hazard and vulnerability reduction to prevent and mitigate risks, (2) preparedness, (3) response and (4) recovery measures.” To tackle the growing health emergency as cases of coronavirus infections spread internationally, one radical measure adopted by many governments was to impose periods of curfew and home confinement on local populations. Limiting human contact slows down disease transmission. During outbreaks of infectious disease, isolation and quarantine are often required. Isolation means the enforced separation of people who have been diagnosed with a disease from those who are not sick, whereas quarantine is the separation of people who have potentially been exposed to establish if they then become sick, to lessen the chance of them passing on the infection to others (Brooks et al., 2020).
However, the compulsory stay‐at‐home orders, enforced in many countries during the early phase of national COVID‐19 epidemics, extended far beyond the separation of only (potentially) infected persons. Quarantine was imposed as mandatory home confinement on entire cities, states, or even nationwide. It was argued that without such restrictions on human movement for everything but essential reasons (e.g., buying food, emergency healthcare), national health services would soon be overwhelmed with enormous numbers of COVID‐19 cases requiring hospitalization. Fears were expressed that epidemics might reach unmanageable proportions. The media were quick to coin the term “lockdown” to refer to the CMQ measures implemented, at first locally then nationwide. Table 2 shows the various durations of initial CMQ mandated at the national scale across various countries within the Middle East/North Africa (MENA) region. Staggeringly, about half of the world's population came under some form of requested or mandatory lockdown by early April 2020. Never in human history has mass quarantine of extended durations been simultaneously imposed on such considerable populations worldwide.
Table 2.
Durations of initial periodsa of compulsory mass quarantine enforced at national levels in response to the coronavirus epidemic, for selected countries in the MENA (Middle East/North Africa) regionb
| County | Lockdown start date | Lockdown end date |
|---|---|---|
| Iraq | 03‐22‐2020 | 04‐11‐2020 |
| Jordan | 03‐18‐2020 | 04‐30‐2020 |
| Kuwait | 03‐14‐2020 | 03‐29‐2020 |
| Lebanon | 03‐15‐2020 | 03‐28‐2020 |
| Morocco | 03‐19‐2020 | 06‐10‐2020 |
| Tunisia | 03‐22‐2020 | 04‐19‐2020 |
| United Arab Emirates | 03‐26‐2020 | 04‐17‐2020 |
For the first nationwide lockdown period. Many countries worldwide reinstated restrictions in response to second and third waves of infections in late 2020 and early 2021.
Data (unverified) from various sources, including news, media accounts, and online databases.
Whenever natural catastrophes or NATECH disasters strike, they are responsible for death, injury, and physical illnesses. But it is well recognized that mental health also suffers. First‐responders and humanitarian workers who respond in the aftermath of disaster events are known to experience posttraumatic psychological outcomes (Guilaran et al., 2018). By their very nature, disasters severely disrupt family security, livelihoods, and social connectivity within the wider community. The shock of extreme events and their consequences have complex effects on physical, mental, and social wellbeing (Marx et al., 2012). Many factors influence levels of individual and collective trauma during disasters (Flynn, 1997). Multiple adversities are experienced leading to anxiety that may develop into long‐term distress. Posttraumatic symptoms can include depression, anxiety, dissociation, suicidality, dissocial behavior, and substance abuse (Kar, 2006). Siddiqi et al. (2006) found evidence of considerable postdisaster psychological distress, their findings being consistent with expectations of increases in psychological morbidity post‐disaster. In the most recent studies, COVID‐19 is likewise associated with psychological distress (Bao et al., 2020; Rajkumar, 2020).
Yet, one feature is unique to the current COVID‐19 pandemic. In addition to the wide‐ranging problems common to most catastrophes, here the disaster management tool itself brings a sting in the tail: adverse impacts on mental health. In other words, CMQ—the very instrument specifically utilized to protect public health—brings about negative health consequences itself. Clearly, understanding such iatrogenic effects has important ramifications for building future pandemic management strategies.
AIMS AND OBJECTIVES
Developing new policies for pandemic management will need to be evidence‐based following scientific study of factors influencing the short and long‐term psychosocial reactions within affected populations. Against the background described above, the current study is concerned with understanding how the coronavirus epidemic affected ordinary people in the United Arab Emirates (UAE). CMQ was implemented over March–April 2020 (Table 2) as a necessary measure to curb the transmission of COVID‐19. The overarching aim is to look at the factors most strongly associated with elevated psychopathology during the early phase of CMQ. The study hypothesis is that CMQ causes adverse (iatrogenic) effects in terms of mental health. The specific objectives are:
To examine the prevalence of (1) depression and (2) anxiety as key indicators of psychological health in a sample of the UAE population during the initial phase of imposed CMQ lockdown.
To measure the relative importance of various demographic factors on the chosen psychological health indicators.
The findings are then discussed in the context of promoting better integration of health dimensions within DRR frameworks, policies, and practice.
METHODS
Characteristics of the study area
UAE is a federation of seven states formed in 1971 and located on the eastern side of the Arabian Peninsula. The discovery and subsequent revenues from oil and gas have fueled rapid social and economic development across the UAE during the latter half of the 20th century (WHO, 2012). The nation's wealth has led to the large‐scale influx of migrant workers from around the world, who comprise around 80% of the total population according to the UAE National Bureau of Statistics (2009). Demographically, the citizens of the UAE, known as Emiratis, are a numerical minority.
Participants
Participants were a nonprobability sample (n = 1585) of adults resident in the UAE during the early stages of the COVID‐19 pandemic. All participants were 18 years or over. The mean age of the sample was 31.97 (SD = 11.71) and the median age was 31 (interquartile range [IQR] = 21–40). Participants were recruited during the first two weeks of April 2020 via announcements in the UAE media and through the email networks of the UAE's National Program for Happiness and Wellbeing (https://u.ae/en/about-the-uae/the-uae-government/government-of-future/happiness). The survey was presented as questionnaires in English and Arabic; the Arabic was translated using the back‐translation technique. Although not representative of the whole UAE, the sample reflected many of its constituents. The two most populous emirates/city‐states were well represented, with Abu Dhabi and Dubai accounting for 43.2% and 24.5% of the sample, respectively. Citizens of the UAE (Emiratis) accounted for the majority (65%) of the respondents. Table 3 gives further details on the sample characteristics.
Table 3.
Sample characteristics (n = 1585)
| Demographic variable | Frequency (%) |
|---|---|
| Gender | |
| Female | 1325 (83.6) |
| Male | 260 (16.4) |
| Over 30 | |
| Yes | 802 (50.6) |
| No | 783 (49.4) |
| College education | |
| Yes | 1133 (71.5) |
| No | 452 (28.5) |
| Emirati/citizen | |
| Yes | 1023 (64.5) |
| No | 562 (35.5) |
| Rural dweller | |
| Yes | 210 (13.2) |
| No | 1375 (86.8) |
| History of mental health problems | |
| Yes | 250 (15.7) |
| No | 1335 (84.2) |
Measures of psychological health
The Patient Health Questionnaire‐8 (PHQ8)
The PHQ8 (Kroenke et al., 2009) is a well‐standardized and widely used screening instrument for the assessment of depressive symptoms in the general population. Its psychometric properties are excellent (Kroenke et al., 2009; Shin et al., 2019) and it is short enough to be used for survey work. The scale consists of eight short items assessing the frequency of depressive symptomatology over the past two weeks. Participants’ responses range from 0 to 3, where 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Total scores (from 0 to 24) are obtained by summing the responses to each item. Higher scores are indicative of greater levels of depressive symptomatology. When used as a screening tool, a cut‐off score of 10 or more has been associated with excellent sensitivity and specificity for the diagnosis of depressive disorders (Kroenke et al., 2009). The cutoff score of 10 or more was used here to indicate “caseness” or clinically significant depressive symptom levels. The internal reliability of the scale among the current sample was excellent, with Cronbach's α = 0.907.
The Generalized Anxiety Disorder‐7 (GAD7)
The GAD7 (Spitzer et al., 2006) is a widely used measure of anxiety in the general population. Participants are asked to indicate how often, in the past two weeks, they have experienced each of seven main symptoms associated with generalized anxiety disorder. Total scores can range from 0 to 21 and are calculated by assigning scores of 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day) to item responses. Scores of 5, 10, and 15 are considered cut‐off points for mild, moderate, and severe anxiety, respectively. The psychometric properties of the instrument have been widely supported and the reliability of the scale among the current sample was excellent, with α = 0.931. The present study used the cutoff score of 10 or more as indicative of clinically significant symptomatology for anxiety disorder.
Demographic measures
Gender: Participants were asked to report their gender as either male or female. Age: Participants were asked their age. For ease of interpretation, this variable was dichotomized using a median split. We now have two groups, those 30 and over and those under the age of 30. Education: Participants were questioned on their education level. Education was indicated on a scale from 1 (did not complete high school) to 4 (holds PhD/Doctoral degree). For ease of interpretation, we also dichotomized this variable, into those who had completed college and those who had not. Residence: Participants specified if they lived in a village/rural community or in a city/urban location. Citizenship: Participants identified whether they were citizens of the UAE (Emirati) or nonnational residents. Finally, participants were asked if they had ever been diagnosed or received treatment for a mental health problem.
Procedure
The Research Ethics Committee of the UAE Ministry of Health and Prevention (MOHAP/DXB‐REC/MMM/No. 49/2020) approved the study. Data collection took place online from April 2 to 17, whereby participants first selected their preferred language (57.8% selected English) and then read the participant information page, before giving consent. Consenting participants answered demographic and personal history questions first, followed by the PHQ8 and the GAD7 questionnaires. The median completion time for the survey was 18.05 min. The data presented here are a subset of a more expansive survey exploring the psychosocial correlates of COVID‐19 in the UAE.
RESULTS AND ANALYSIS
Psychological health and demographic factors
On the basis of the cutoff scores for the PHQ8 and GAD7 instruments, the rates of depression were 44.8% and the rates of anxiety were 38.2%. Descriptive statistics for depression and anxiety are summarized in Table 4.
Table 4.
Descriptive statistics for psychological health outcome variables
| Statistic | Depression (PHQ8) | Anxiety (GAD7) |
|---|---|---|
| Percent above screening cut‐off (%) | 44.79 | 38.17 |
| Median score | 8.00 | 7.00 |
| Mean score | 9.25 | 7.90 |
| Interquartile range | 3–14 | 2–13 |
| Standard deviation | 6.83 | 6.51 |
| Minimum | 0.00 | 0.00 |
| Maximum | 24.00 | 21.00 |
Abbreviations: GAD7, Generalized Anxiety Disorder‐7; PHQ8, Patient Health Questionnaire‐8.
Two binary logistic regression models were used to predict caseness for depression and anxiety. The demographic predictor variables were age group, gender, living location, education, citizenship status, and mental health history. Table 5 details the results of model 1, looking at depression. Findings for depression are stratified by the predictor variables, with bivariate associations presented as (unadjusted) odds ratios (OR), and adjusted odds ratios (AORs) from the multivariate model with all predictors entered. The multivariate model was significant (χ 2 = 213.26, p < 0.001). When ORs were calculated, all variables were predictive of depression. Being younger, female, Emirati, urban‐dwelling, and less educated were associated with an elevated risk of depression (Figure 1). However, when the AORs were calculated, only the effects for age, gender, and history of mental health persisted (remained significant).
Table 5.
Bivariate (OR) and multivariate (AOR) binary logistic regression results predicting depressive symptomatology
| Demographic variable | Sample (N) | Depression, N (%) | Unadjusted OR (95% confidence interval) | Significance level | AOR (95% confidence interval) | Significance level |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Under 30 | 777 | 467 (60.10) | 0.297 (0.241–0.365) | <0.001 | 0.390 (0.298–0.509) | <0.001 |
| Over 30 | 787 | 243 (30.87) | ||||
| Gender | ||||||
| Female | 1325 | 642 (48.85) | 0.388 (0.288–0.524) | <0.001 | 0.554 (0.399–0.768) | <0.001 |
| Male | 260 | 68 (27.09) | ||||
| Residence | ||||||
| City/Suburb | 1357 | 634 (46.72) | 0.657 (0.486–0.888) | <0.01 | 0.734 (0.539–1.025) | ns |
| Rural | 208 | 76 (36.53) | ||||
| Education | ||||||
| No college | 446 | 271 (60.76) | 0.417 (0.333–0.522) | <0.001 | 0.860 (0.649–1.141) | ns |
| College | 1119 | 439 (39.23) | ||||
| UAE citizenship | ||||||
| Yes | 1007 | 530 (52.63) | 0.429 (0.345–0.532) | <0.001 | 0.920 (0.663–1.113) | ns |
| No | 558 | 180 (32.25) | ||||
| History of mental health problems | ||||||
| No | 1316 | 544 (41.33) | 0.352 (0.264–0.468) | <0.001 | 0.343 (0.253–0.465) | <0.001 |
| Yes | 249 | 166 (66.66) | ||||
Abbreviations: AOR, adjusted odds ratio; OR, odds ratio; ns, not significant (at p < 0.05).
Figure 1.
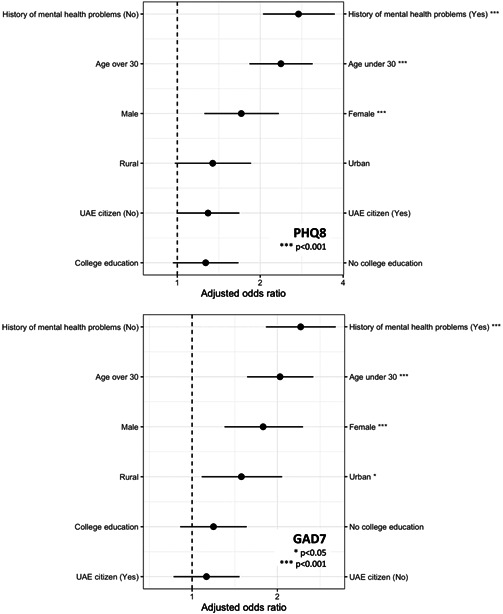
Forest plots of adjusted odds ratios (displayed as 1/AOR) for depression (above) and anxiety (below) during the early phase of compulsory mass quarantine implemented to contain the COVID‐19 epidemic in the United Arab Emirates (UAE). GAD7, Generalized Anxiety Disorder‐7; PHQ8, Patient Health Questionnaire‐8
The findings for anxiety closely followed those of depression. Table 6 details the results of model 2 looking at anxiety. Again, the multivariate model was significant (χ 2 = 125.27, p < 0.001). When unadjusted odds ratios were calculated, all variables were predictive of anxiety. Being younger, female, Emirati, urban‐dwelling, less educated, and having a history of mental health problems were associated with elevated risk (Figure 1). However, when the adjusted odds ratios were calculated, only the effects for age, gender, history of mental health problems, and residence persisted (remained significant). Figure 1 visualizes the results of adjusted odds ratios for depression and anxiety in descending order of risk.
Table 6.
Bivariate (OR) and multivariate (AOR) binary logistic regression results predicting anxiety symptomatology
| Demographic variable | Sample (N) | Anxiety, N (%) | Unadjusted OR (95% confidence interval) | Significance level | AOR (95% confidence interval) | Significance level |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Under 30 | 777 | 377 (48.52) | 0.427 (0.346–0.525) | <0.001 | 0.474 (0.361–0.621) | <0.001 |
| Over 30 | 795 | 228 (28.67) | ||||
| Gender | ||||||
| Female | 1314 | 540 (41.09) | 0.480 (0.351–0.649) | <0.001 | 0.562 (0.408–0.774) | <0.001 |
| Male | 259 | 65 (25.09) | ||||
| Residence | ||||||
| City/suburb | 1363 | 543 (39.83) | 0.633 (0.461–0.867) | <0.01 | 0.686 (0.495–0.960) | <0.05 |
| Rural | 210 | 62 (29.52) | ||||
| Education | ||||||
| No college | 446 | 216 (48.43) | 0.561 (0.449–0.701) | <0.001 | 0.857 (0.653–1.125) | ns |
| College | 1127 | 389 (34.51) | ||||
| UAE citizenship | ||||||
| Yes | 1013 | 425 (41.95%) | 0.655 (0.527–0.814) | <0.001 | 0.869 (0.664–1.137) | ns |
| No | 560 | 180 (32.14) | ||||
| History of mental health problems | ||||||
| No | 1325 | 462 (34.86) | 0.393 (0.283–0.518) | <0.001 | 0.410 (0.309–0.545) | <0.001 |
| Yes | 248 | 143 (57.66) | ||||
Abbreviations: AOR, adjusted odds ratio; OR, odds ratio; ns, not significant (at p < 0.05).
Temporal analysis: Early versus late responders
To explore further the possible impact of lockdown on mental health, we looked at participants’ scores from both ends of the data collection timeframe. The depression and anxiety status of participants who completed the survey from April 2 to 8, 2020 (early responders, N = 851) was compared with those who responded during the latter stages of the survey timeframe from April 9 to 17 (late responders, N = 714). Elevated depressive symptom status (scores above the PHQ8 cut‐off) varied between the two groups, with a rate of 55.2% and 33.6% among early and late responders, respectively. Using Pearson's χ 2 test, the difference was statistically significant, with χ 2 (1, N = 1565) = 73.19, p < 0.001. The same analysis was carried out looking at anxiety status. The rates for participants scoring above the GAD7 cut‐off were 45.8% and 29.8% among early and late responders, respectively. This difference was again statistically significant, with χ 2 (1, N = 1573) = 42.33, p < 0.001. Subsequently, a multivariate logistic regression analysis was performed with depressive symptom status (above/below the PHQ8 cut‐off) as the dependent variable, entering responder timeline (early/late) as the predictor variable, while also controlling for age, gender, and nationality (Emirati/non‐Emirati). Even after controlling for these demographic variables, early survey responses were associated with a greater likelihood of scoring above the PHQ8 cut‐off: AOR = 1.515, confidence interval (CI) 1.192–1.926, p < 0.001. The same pattern of findings was observed for anxiety status (GAD7), with early responders more likely to score above the GAD7 cut‐off than late responders: AOR = 1.447, CI 1.136–1.843, p = 0.003.
Comparisons of findings
The present study found unusually high levels of anxiety and depressive symptomatology in the UAE sample during the early stages of the CMQ lockdown. The frequencies of individuals scoring above the screening cut‐offs for both the PHQ8 (44.8%) and GAD7 (38.2%) were far higher than anything reported in similarly designed pre‐pandemic surveys in the UAE. In a review of 14 articles exploring depression and anxiety in the UAE, the highest rate of depression reported was 33% (all‐female sample), whereas, for anxiety, it was 28.6% (Razzak et al., 2019). However, previous UAE investigations have tended to focus on clinical groups. For example, Alsaadi et al. (2015) explored depressive symptoms among multiple sclerosis patients and reported a 17.6% and 20% prevalence for depression and anxiety, respectively. More recently, among UAE patients diagnosed with epilepsy, Alsaadi et al. (2017) reported 26.9% and 25% prevalence for depression and anxiety. Although it is understood that chronic health conditions are associated with elevated levels of depression (Simon, 2001), both of these reasonably contemporaneous studies still yielded much lower rates than our current findings. For subjects without underlying health problems, pre‐COVID‐19 background data on depression and anxiety levels in the UAE population are unfortunately scarce. Abdulrahman et al. (2018) present one of the few available studies for comparison. In a nonclinical set of 302 UAE medical residents (doctors), depression rates ranged from 6% to 33%—again, appreciably lower than rates found here. Similarly, a UAE‐based psychiatric survey administered a structured clinical interview to 1669 Emirati households across the city of Al Ain. The study reported a lifetime prevalence for depressive illness of 2.8% and 10.3% for males and females, respectively (Abou‐Saleh et al., 2001).
It should be noted that differences in methods of data collection, study samples, and assessment instruments combine to make formal cross‐survey comparisons difficult. Nevertheless, it is observed that similar patterns of results (i.e., a post‐CMQ spike in psychopathology) have been reported in several other nations, for example, the United Kingdom (Shevlin et al., 2020), United States of America (McGinty et al., 2020), China (Lei et al., 2020) and Lebanon (Grey et al., 2020). Moreover, at least one UAE‐based study had fortuitously collected depressive symptom data from college students two weeks before the UAE CMQ measures and then again two weeks afterward (Thomas et al., 2021). Before lockdown, the rate of students scoring in the severe range on a widely used self‐report measure of depression was 15%. In the two weeks after CMQ commenced, rates rose to 36.5%. It seems fairly certain that lockdown measures have some direct impact on mental health status, at least during the early stages of this infection control measure.
We also explored differences between participants completing the survey during the first week of April and those completing it during Week 2. We observed a statistically significant decrease in the rate of people scoring above the screening cut‐off among those participants who completed the survey in Week 2, even after controlling for demographic differences. Although this 2‐week data collection window is rather narrow, it is possible that the apparent drop‐off in symptom levels reflects a general sense of habituation to a novel situation. This idea of an acute reaction followed by a lessening of symptoms is borne out by other longitudinal studies using repeated measurements across a broader timeframe. For example, using a large convenience sample weighted to match the UK population, Fancourt et al. (2021) reported a decreasing level of generalized anxiety and depression over the twenty weeks of lockdown, with the greatest decline in the first two weeks. Similar findings are also reported by O'Connor et al. (2021). The general finding seems to be one of heightened prevalence during the early stages of lockdown, followed by the amelioration of psychiatric symptomology with the passage of time. However, Shevlin et al. (2021) challenge this idea, suggesting that there are different patterns of change for certain demographic groups, or as they express it, “different slopes for different folks.” In their UK analysis spanning four months, they found great heterogeneity in pandemic response across time, identifying individuals who improved, those who remained stable, and those who showed a deterioration in mental health. Loneliness, lower levels of trait resilience, and a history of mental health treatment were predictors of mental health deterioration between April and July 2020 (Shevlin et al., 2021).
Caveats to findings
This study has several important limitations that need to be clarified. First, the sample was not representative of the entire UAE populace. Notably absent were male foreign laborers employed in construction and other types of manual work. Reaching this group was beyond the scope of the present study owing to time constraints, general lack of internet access by this group for the online survey, and the necessary CMQ restrictions curtailing movement during April 2020. Second, self‐selection bias might mean that the most anxious and depressed were perhaps the keenest to take the survey. Third, differences in methods of data collection and mental health assessment can hinder formal comparisons between studies. Fourth, the correlational nature of the study renders all causal and temporal inferences tentative at best.
In spite of these caveats, the abnormal rates of depression and anxiety measured at high levels of statistical significance by the present study are likely, at least in part, to be related to the COVID‐19 pandemic and the CMQ measures implemented for infection prevention and control. Moreover, obtaining these preliminary insights into the demographic factors associated with a heightened incidence of depression and anxiety among segments of the UAE population during the pandemic is important to help inform public (mental) health plans for current and future outbreaks of infectious illness.
DISCUSSION
Importance of strengthening the Health–DRR nexus
Overall, our present findings, and the broader body of research exploring mental health implications, highlight the crucial need for mental health to be more fully integrated into policies aimed at DRR. According to Murray (2014), efforts at mainstreaming health into policies and practices for DRR in the past have been relatively scarce, not always successful, and often restricted simply to the notion of “saving lives.” Consequently, Lo et al. (2017) proposed that Health Emergency and Disaster Risk Management (Health‐EDRM) should be established as a new paradigm to better consolidate the centrality of health within DRR agendas and that the emerging field of scientific inquiry at the intersection of health and DRR deserves greater encouragement. The Health‐EDRM paradigm has the potential to meaningfully guide the implementation of the health aspects of the UN Sendai Framework on DRR (Pearson & Pelling, 2015). Beyond the Sendai Framework, human health is also seen as an important cross‐cutting theme relevant to the other UN‐ratified global frameworks stated earlier. Thus, the Paris Agreement on Climate Change acknowledges how climate change can have negative health risks, whereas the focus of SDG3 within the 2030 Agenda for Sustainable Development is to “ensure healthy lives and promote wellbeing,” with an emphasis on the management of health risks at national and global scales.
There are positive signs that research at the Health–DRR nexus is beginning to gain traction. Djalante et al. (2020) call for more utilization of the Health‐EDRM framework mentioned above to complement current responses on building resilience against biological hazards and pandemics. Furthermore, a new edited volume with 23 separate chapters is entirely dedicated to Public Health and Disasters (Chan & Shaw, 2020). Starkly notable by its absence, however, is any specific study dedicated to psychological health and disasters in that collection. This is in spite of the recommendation by Lo et al. (2017) that the scope of Health‐EDRM research inquiry should expand to include psychosocial health and wellbeing, which they characterized as the thematic gap of “invisible health needs.” Our findings here similarly underscore how research on mental health during disasters must not be overlooked.
Importance of psychological intervention after disasters (PIAD)
Victims face many challenges in the immediate aftermath of a natural disaster that causes major societal disruption and environmental damage. Adversities arise directly from physical harm, lack of access to food and clean water, damage to shelter/housing, disconnection from family and friends, breakdown of infrastructure (power, sanitation, transport), and various other negative impacts. This compound set of multiple different stressors generates strong feelings of displacement. For the COVID‐19 disaster, however, the situation is different: the emergency CMQ lockdown measures implemented for disease containment produce feelings of confinement rather than displacement.
Disaster effects on health can be long‐lasting. Initial emergency healthcare later gives way to the need for post‐disaster psychological care, sometimes for considerable periods (Rao, 2006). There may be a decrease in life satisfaction, with full recovery taking a significant length of time. Psychosocial support is, therefore, seen as crucial in disaster‐affected communities. Ideas about the most appropriate forms of PIAD were developed a decade ago (Higgins et al., 2010). They should be adapted to tackle the particular needs of the disaster‐affected community in question. For this reason, research needs to improve the existing understanding of the mental health consequences of disasters and their principal driving factors. Practitioners with applied expertise will then have evidence‐based ability to respond. Consequently, the value of PIAD has been underscored in the series of capacity‐building workshops organized jointly by the International Union of Psychological Science (IUPsyS, 2016) and the International Council for Science Regional Office for Asia and the Pacific (ICSU ROAP). Within the existing context of COVID‐19, our current findings reinforce the importance of a targeted role for PIAD towards vulnerable groups in UAE society—in this case, women and younger residents in urban settings.
Resilience and Emirati culture
Levels of disaster risk depend not only on existing hazard threats and corresponding environmental exposure but also on the psychological and social vulnerability of exposed communities (Jogia & Wedawatta, 2020). As an individual human trait, resilience in the face of trauma is often remarkable (Bonanno, 2004). Resilience is one of several possible trajectories of stress response following exposure to disasters (Norris et al., 2009). Wider societal dimensions of resilience should also not be underestimated. Societal resilience refers to the inherent capacity for communities to overcome grim circumstances and adversities. People who inhabit disaster‐prone regions, and have done so over many generations, in particular, tend to develop greater disaster resilience. According to Fincher et al. (2008), such communities are more collectivist, interdependent, family‐oriented, less extravert, more religious, and, in general, more in‐group‐oriented, all of which may be interpreted as behavior that offers some protection against psychopathology in the form of social support or at least the expectation of such support. Societal resilience, and how to promote it, is, therefore, a valuable concept in understanding and projecting post‐disaster recovery.
It is, thus, interesting to observe that similar qualities typify the close‐knit, religious, supportive, and traditional family values of Emirati culture (Bristol‐Rhys, 2010). In other words, Emirati society is seen to already possess many of the qualities that typically enhance resilience. However, the nature of this particular pandemic and the response to it—CMQ lockdown and social distancing—might disrupt the traditional bonds of interdependence and social support. Having to refrain from extended family gatherings and religious congregations might prove to be an additional strain for individuals accustomed to close‐knit contact with extended kinship networks and coreligionists. Similarly, Emiratis generally live within larger households, which might include several generations of family members along with unmarried adult children. Such living arrangements resonate with collectivist cultural values. Yet, in the context of an infectious illness pandemic, such arrangements are associated with a heightened risk of infection and perhaps the increased anxiety that accompanies fear of infection. These cultural and mental health factors are important considerations, especially given that long‐term post‐pandemic economic recovery is likely to be appreciably impacted by societal levels of mental ill‐health. Exploring ways to enhance resilience and mitigate the impact of the pandemic on social support and mental health would, therefore, be deserving of further in‐depth investigation.
CONCLUSIONS
All types of disasters cause tragic loss of life and suffering, and can bring serious long‐term consequences for human health and wellbeing in many ways. Yet, a crisis triggered by an infectious disease outbreak clearly poses even greater risks through direct mortality. In early 2020, COVID‐19 quickly escalated into a health emergency of unfathomable proportions and has caused an incomparable geopolitical crisis never witnessed before. The pandemic has inflicted immeasurable human suffering, catastrophic economic losses, and disrupted the normal functioning of society—it is humanity's first experience of a truly global NASECH disaster.
Assessment of disaster risk based on vulnerability and exposure is fundamental for policymakers. The Sendai Framework on DRR is arguably the most influential global agreement aiming to enhance national and community capacity to cope with disaster risks. It emphasizes a comprehensive approach to address multiple hazards (including biological hazards) that impact at different scales, frequencies, and intensities. However, other commentators have identified that greater efforts are needed to integrate public health emergencies into discussions surrounding disasters. For the continuing COVID‐19 pandemic, strengthening the interconnectedness between emergency health responses and DRR is clearly of vital importance. This is supported by our findings in the context of the UAE's experience: (1) In addition to explicit health consequences of the coronavirus disease itself, the psychological wellbeing of people in the UAE appears to have been adversely affected. This finding underscores the importance of PIAD. (2) Early CMQ (“lockdown”) was necessary to contain infection disease transmission. But this instrument also causes iatrogenic (adverse) effects. The resulting rates of depression (44.8%) and anxiety (38.2%) reached high levels. (3) Demographic factors are significantly linked to psychiatric impacts. Female gender, a history of mental health problems, and being a young (under 30) urban dweller, all appeared to be risk factors among this UAE sample. (4) Many cultural values of Emirati society, for example, interdependence, are resilience‐enhancing. However, CMQ may interfere with such protective factors. Exploring ways to mitigate the impacts of CMQ and enhance societal resilience are key areas for future research. Such work can help inform broader strategies aimed at national recovery to the COVID‐19 crisis in the UAE, as well as promoting disaster preparedness in the future.
Biographies
Justin Thomas holds a PhD in experimental psychology from the University of Manchester. He is currently chair of the Psychology Department at Zayed University in the UAE, where he also directs the research cluster for culture cognition and wellbeing.
James Terry holds a PhD in geography from the University of Wales, Swansea, UK. He is a professor in geosciences in the Department of Life & Environmental Sciences at Zayed University in the UAE. His research expertise includes environmental hazards and disaster risks.
Thomas, Justin , and Terry James P.. 2022. “Containing COVID‐19 Risk in the UAE: Mass Quarantine, Mental Health, and Implications for Crisis Management.” Risks Hazards Crisis Public Policy 13, 9–27. 10.1002/rhc3.12237
REFERENCES
- Abdulrahman, Mahera , Nair Satish Chandrasekhar, Farooq Madiha Muhammad, Al Kharmiri Aisha, Al Marzooqi Farida, and Carrick Frederick Robert. 2018. “Burnout and Depression Among Medical Residents in the United Arab Emirates: A Multicenter Study.” Journal of Family Medicine and Primary Care 7: 435–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abou‐Saleh, M. T. , Ghubash R., and Daradkeh T. K.. 2001. “Al Ain Community Psychiatric Survey. I. Prevalence and Socio‐Demographic Correlates.” Social Psychiatry and Psychiatric Epidemiology 36: 20–28. [DOI] [PubMed] [Google Scholar]
- Alsaadi, Taoufik , El Hammasi Khadija, Shahrour Tarek M., Shakra Mustafa, Turkawi Lamya, Mudhafar Abdulla, Diab Lina, and Raoof Mufeed. 2015. “Prevalence of Depression and Anxiety Among Patients with Multiple Sclerosis Attending the MS Clinic at Sheikh Khalifa Medical City, UAE: Cross‐sectional Study.” Multiple Sclerosis International 2015: 487159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsaadi, Taoufik , Kassie Seada, El Hammasi Khadija, Shahrour Tarek M., Shakra Mustafa, Turkawi Lamya, Nasreddine Wassim, and Raoof Mufeed. 2017. “Potential Factors Impacting Health‐Related Quality of Life Among Patients with Epilepsy: Results from the United Arab Emirates.” Seizure 53: 13–7. [DOI] [PubMed] [Google Scholar]
- Asian Disaster Preparedness Center (ADPC) . 2006. Regional Analysis of Socio‐Economic Impacts of the December 2004 Earthquake and Indian Ocean Tsunami. Bangkok: ADPC. [Google Scholar]
- Bao, Yanping , Sun Yankun, Meng Shiqiu, Shi Jie, and Lu Lin. 2020. “2019‐nCoV Epidemic: Address Mental Health Care to Empower society.” Lancet 395: e37–e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake, Eric S. , Landsea Christopher W., and Gibney Ethan J.. 2011. “The Deadliest, Costliest, and Most Intense United States Tropical Cyclones from 1851 to 2010 (and Other Frequently Requested Hurricane Facts).” In NOAA Technical Memorandum NWS NHC‐6 (pp. 1–44). Miami: National Hurricane Center. [Google Scholar]
- Bonanno, George A. 2004. “Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events?” American Psychologist 59: 20–28. [DOI] [PubMed] [Google Scholar]
- Bristol‐Rhys, Jane . 2010. Emirati Women: Generations of Change. London: C. Hurst & Co. [Google Scholar]
- Brooks, Samantha K. , Webster Rebecca K., Smith Louise E., Woodland Lisa, Wessely Simon, Greenberg Neil, and Rubin Gideon James. 2020. “The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence.” The Lancet 395: 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, Emily Ying Yang , and Shaw Rajib. eds. 2020. “Public Health and Disasters.” In Health Emergency and Disaster Risk Management in Asia. Singapore: Springer. [Google Scholar]
- Djalante, Riyanti , Shaw Rajib, and DeWit Andrew. 2020. “Building Resilience Against Biological Hazards and Pandemics: COVID‐19 and Its Implications for the Sendai Framework.” Progress in Disaster Science 6: 100080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt, Daisy , Steptoe Andrew, and Bu Feifei. 2021. “Trajectories of Anxiety and Depressive Symptoms During Enforced Isolation Due to COVID‐19 in England: A Longitudinal Observational Study.” The Lancet Psychiatry 8: 141–149. 10.1016/S2215-0366(20)30482-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fincher, Corey L. , Thornhill Randy, Murray Damian R., and Schaller Mark. 2008. “Pathogen Prevalence Predicts Human Cross‐Cultural Variability in Individualism/Collectivism.” Proceedings of the Royal Society B 275: 1279–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn, Brian W. 1997. “‘Psychological Aspects of Disasters’.” Renal Failure 19: 611–620. [DOI] [PubMed] [Google Scholar]
- Goff, James Rodney , and Terry James Peter. 2012. Living with Natural Hazards in the Asia–Pacific Region (361, pp. 1–2). London: Geological Society of London. Special Publication. [Google Scholar]
- Grey, Ian , Arora Teresa, Thomas Justin, Saneh Ahmad, Tomhe Pia, and Abi‐Habib Ruby. 2020. “The Role of Perceived Social Support on Depression and Sleep During the COVID‐19 Pandemic.” Psychiatry Research 293: 113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilaran, Johnrev , de Terte Ian, Kaniasty Krzysztof, and Stephens Christine. 2018. “Psychological Outcomes in Disaster Responders: A Systematic Review and Meta‐Analysis on the Effect of Social Support.” International Journal of Disaster Risk Science 9: 344–358. [Google Scholar]
- Higgins, Louise T. , Gao Xiang, and Zhu Song. 2010. “The Development of Psychological Intervention after Disaster in China.” Asia Pacific Journal of Counselling and Psychotherapy 1: 77–86. [Google Scholar]
- IUPsyS . 2016. “Report on the 5th International Workshop on Psychological Intervention after Disasters.” International Union of Psychological Science. Manila, The Philippines, November 14–17. https://www.iupsys.net/dotAsset/416aa0ac-7b5d-4b2d-9e78-0cc600798a92.pdf
- Jogia, Jigar , and Wedawatta Gayan. 2020. “Psychological Vulnerability as an Integral Component of Comprehensive Vulnerability Assessment: Informing Policy and Practice in Disaster Risk Reduction.” International Journal of Work Organisation and Emotion 10: 232–245. [Google Scholar]
- Kar, Nilamadhab . 2006. “Psychosocial Issues Following a Natural Disaster in a Developing Country: A Qualitative Longitudinal Observational Study.” International Journal of Disaster Medicine 4: 169–176. [Google Scholar]
- Krausmann, Elisabeth , Girgin Serkan, and Necci Amos. 2019. “Natural Hazard Impacts on Industry and Critical Infrastructure: NATECH Risk Drivers and Risk Management Performance Indicators.” International Journal of Disaster Risk Reduction 40: 101163. [Google Scholar]
- Kroenke, Kurt , Strine Tara W., Spitzer Robert L., Williams Janet B. W., Berry Joyce T., and Mokdad Ali H.. 2009. “The PHQ‐8 as a Measure of Current Depression in the General Population.” Journal of Affective Disorders 114: 163–173. [DOI] [PubMed] [Google Scholar]
- Lei, Lei , Huang Xiaoming, Zhang Shuai, Yang Jinrong, Yang Lin, and Xu Min. 2020. “Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by Versus People Unaffected by Quarantine During the COVID‐19 Epidemic in Southwestern China.” Medical Science Monitor 26: e924609‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo, Sharon Tsoon Ting , Chan Emily Ying Yang, Chan Gloria Kwong Wai, Murray Virginia, Abrahams Jonathan, Ardalan Ali, Kayano Ryoma, and Chung Johnny Chung Wai. 2017. “Health Emergency and Disaster Risk Management (Health‐EDRM): Developing the Research Field Within the Sendai Framework Paradigm.” International Journal of Disaster Risk Science 8: 145–149. [Google Scholar]
- Marx, Michael , Phalkey Revati, and Guha‐Sapir Debarati. 2012. “Integrated Health, Social and Economic Impacts of Extreme Events: Evidence, Methods, and Tools.” Global Health Action 5: 19837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, Emma E. , Presskreischer Rachel, Han Hahrie, and Barry Colleen L.. 2020. “Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020.” Journal of the American Medical Association 324: 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, Virginia . 2014. “Disaster Risk Reduction, Health, and the Post‐2015 United Nations Landmark Agreements.” Disaster Medicine and Public Health Preparedness 8: 283–287. [DOI] [PubMed] [Google Scholar]
- Norris, Fran H. , Tracy Melissa, and Galea Sandro. 2009. “Looking for Resilience: Understanding the Longitudinal Trajectories of Responses to Stress.” Social Science and Medicine 68: 2190–2198. [DOI] [PubMed] [Google Scholar]
- O'Connor, Rory C. , Wetherall Karen, Cleare Seonaid, McClelland Heather, Melson Ambrose J., Niedzwiedz Claire L., O'Carroll Ronan E., et al. 2021. “Mental Health and Well‐Being During the COVID‐19 Pandemic: Longitudinal Analyses of Adults in the UK COVID‐19 Mental Health & Wellbeing study.” The British Journal of Psychiatry 218: 326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson, Lucy , and Pelling Mark. 2015. “The UN Sendai Framework for Disaster Risk Reduction 2015–2030: Negotiation Process and Prospects for Science and Practice.” Journal of Extreme Events 2: 1571001. [Google Scholar]
- Rajkumar, Ravi Philip . 2020. “COVID‐19 and Mental Health: A Review of the Existing Literature.” Asian Journal of Psychiatry 52: 102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao, Kamran . 2006. “Psychosocial Support in Disaster‐Affected Communities.” International Review of Psychiatry 18: 501–505. [DOI] [PubMed] [Google Scholar]
- Razzak, Hira Abdul , Harbi Alya, and Ahli Shaima. 2019. “Depression: Prevalence and Associated Risk Factors in the United Arab Emirates.” Oman Medical Journal 34: 274–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, Mark , McBride Orla, Murphy Jamie, Gibson Miller Jilly, Hartman Todd K., Levita Liat, and Mason Liam, et al. 2020. “Anxiety, Depression, Traumatic Stress, and COVID‐19 related anxiety in the UK general population during the COVID‐19 pandemic.” BJPsych Open 6: e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, Mark , Butter Sarah, McBride Orla, Murphy Jamie, Gibson‐Miller Jilly, Hartman Todd K., and Levita Liat. 2021. “Refuting the Myth of a ‘Tsunami’ of Mental Ill‐health in Populations Affected by COVID‐19: Evidence that Response to the Pandemic is Heterogenous, Not Homogeneous.” Psychological Medicine 1–9. 10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin, Cheolmin , Lee Seung‐Hoon, Han Kyu‐Man, Yoon Ho‐Kyoung, and Han Changsu. 2019. “Comparison of the Usefulness of the PHQ‐8 and PHQ‐9 for Screening for Major Depressive Disorder: Analysis of Psychiatric Outpatient Data.” Psychiatry investigation 16: 300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi, Kamran , Siddiqi Najma, Saeed Khalid, and House Alan Oliver. 2006. “Assessing Mental Health Needs After a Major Disaster: Experience from the Pakistan Earthquake, 2005.” International Journal of Disaster Medicine 4: 177–182. [Google Scholar]
- Simon, Gregory E. 2001. “Treating Depression in Patients with Chronic Disease.” Western Journal of Medicine 175: 292–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, Keith . 2013. Environmental Hazards: Assessing Risk and Reducing Disaster, 6th Edition. London and New York: Routledge. [Google Scholar]
- Spitzer, Robert L. , Kurt Kroenke, Janet B. W. Williams, and Bernd Löwe. 2006. “A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD‐7.” Archives of Internal Medicine 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- Spreeuwenberg, Peter , Kroneman Madelon, and Paget John. 2018. “Reassessing the Global Mortality Burden of the 1918 Influenza Pandemic.” American Journal of Epidemiology 187: 2561–2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg, Laura J. , Sengul Hatice, and Cruz Ana Maria. 2008. “Natech Risk and Management: An Assessment of the State of the Art.” Natural Hazards 46: 143–152. [Google Scholar]
- Thomas, Justin , AlKatheeri Omnya, and Grey Ian. 2021. “Cognitive Vulnerability and Depressive Symptoms Among Emirati College Students Before and After the Enactment of COVID‐19 Curfew and Home‐Learning Measures.” International Journal of Psychology and Psychological Therapy 21: 75–79. [Google Scholar]
- UAE National Bureau of Statistics . 2009. “Population Estimates (2006–2009).” http://www.uaestatistics.gov.ae/ReportDetailsEnglish/tabid/121/Default.aspx?ItemId=1914%26PTID=104%26MenuId=1
- United Nations (UN) . 2020. Hazard Definition & Classification Review: Technical Report (pp. 1–87). Geneva: United Nations. [Google Scholar]
- United Nations International Strategy for Disaster Reduction (UNISDR) . 2015. Sendai Framework For Disaster Risk Reduction 2015–2030. Geneva: United Nations International Strategy for Disaster Reduction. http://www.preventionweb.net/files/43291_sendaiframeworkfordrren.pdf [Google Scholar]
- World Health Organization (WHO) . 2011. Disaster Risk Management for Health: Overview. Geneva: World Health Organization. http://www.who.int/hac/events/drm_fact_sheet_overview.pdf [Google Scholar]
- World Health Organization (WHO) . 2012. Country Cooperation Strategy for WHO and the United Arab Emirates 2012–2017 (pp. 1–24). Cairo: World Health Organization. Regional Office for the Eastern Mediterranean. WHO‐EM/PME/002/E. https://applications.emro.who.int/docs/CCS_UAE_2012_EN_14947.pdf [Google Scholar]
- World Health Organization (WHO) . 2021. WHO Coronavirus (COVID‐19) Dashboard. Geneva: World Health Organization. https://covid19.who.int/ [Google Scholar]
- Zhang, Hongyue , and Shaw Rajib. 2020. “Identifying Research Trends and Gaps in the Context of COVID‐19.” International Journal of Environmental Research and Public Health 17: 3370. [DOI] [PMC free article] [PubMed] [Google Scholar]


