Abstract
Angiolipoma is an uncommon benign fatty tumor which is a variant of lipoma. Microscopic studies on angiolipoma show that it includes the mature lipocytes and blood vessels. Infiltrating angiolipoma is an un-capsulated angiolipoma and, due to penetration into the surrounding structures, complete excision of the tumor is difficult. According to previous studies, the relapse rate of the infiltrating angiolipoma after surgical intervention is 35-50%. Infiltrating angiolipoma is rarely seen in the head and neck region and often occurs in the trunk and limbs. In this study, we report a 10-year-old boy with periauricular infiltrating angiolipoma who underwent surgery. After surgery, the patient developed transient left frontal branch palsy, but recovery was excellent and after one year there is no relapse.
Key Words: Angiolipoma, Periauricular region
INTRODUCTION
Lipomas are fatty tumors and 5-17% of these tumors are angiolipomas(1). Angiolipoma is a variant of lipoma that includes mature lipocyts and blood vessels(2-6). Infiltrating angiolipoma are often placed deeper than the non-infiltrating form(1, 7). Infiltrating angiolipoma usually occurs in the trunk and limbs and is rarely seen in the head and neck region. Location of the tumor is a major factor in determining its prognosis(1). We present a patient with infiltrating angiolipoma in the periauricular region that underwent surgery.
CASE REPORT
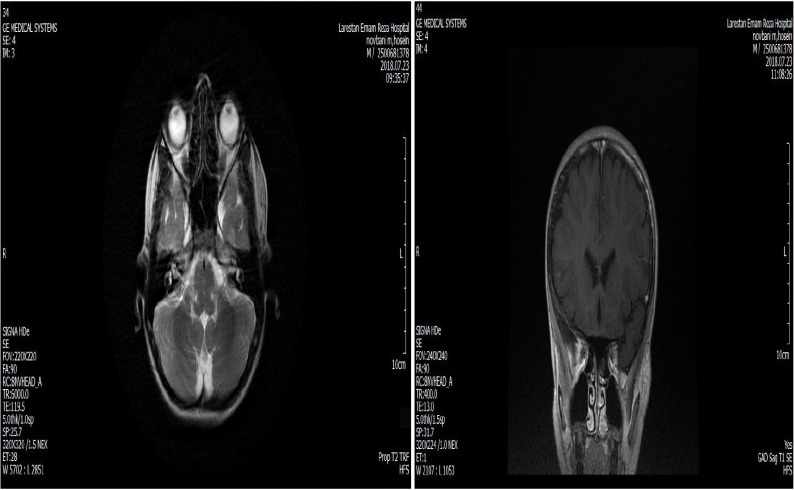
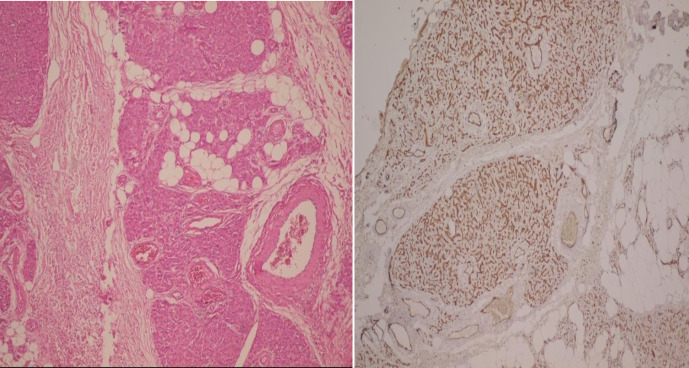
This study was conducted in August 2020 at Amiralmomenin hospital in Shiraz. A 10-year old boy presented with a mass on the left periauricular region with bluish discoloration during exercises (Figure 1). The patient had no history of trauma and infectious diseases. Physical exam showed a left periauricular painless subcutaneous mass. The facial magnetic resonance imaging (MRI) revealed ill-defined soft tissue mass in the left periauricular region. The tumor had hyper-intense signal on T2 weighted sequences and isointense signal on T1 weighted sequences (Figure 2). Fine needle aspiration was not diagnostic. Surgical excision of the un-capsulated mass was performed through periauricular incision under general anesthesia and loupe magnification. The specimen was sent for pathologic evaluation and infiltrating angiolipoma was reported (Figure 3). After surgery, the patient developed transient left frontal branch palsy, but recovery was excellent and after one year there is now no relapse.
Fig. 1.
A 10-year-old boy with a mass on the left periauricular region
Fig. 2.
MRI revealed an ill-defined soft tissue mass
Fig. 3.
Section shows mature lipocyts and blood vessels indicating infiltrating angiolipoma
INFORMED CONSENT
Informed consent was obtained from the patient.(Ethical Code: IR.SUMS.REC.1400.405).
DISCUSSION
Angiolipoma is a variant of lipoma that includes mature lipocyts and blood vessels(2-6). In different cases, the ratio of the lipocyt to the blood vessels varies, but in most of them the percentage of lipocyts is higher than blood vessels (4, 8). In terms of having or not having a capsule, they are divided into two categories: encapsulated (circumscribed) and un-capsulated (infiltrating) angiolipoma which penetrates the surrounding structures (9). Infiltrating angiolipoma usually occurs in the trunk and limbs and is rarely seen in the head and neck region. Location of the tumor is a major factor in determining its prognosis (7).
Angiolipomas usually happen sporadically, but a few cases have a family history of angiolipoma, and the inheritance pattern in these cases is autosomal recessive or in very rare cases autosomal-dominant pattern (5, 10). Also, in a study that examined the karyotype of three cases of angiolipoma, the researchers concluded that all three cases had abnormal karyotypes with loss or structural rearrangement of chromosome 13(8).
Histopathologic studies are required for definitive diagnosis of angiolipoma from other soft tissue tumors such as hemangioma, myxolipoma, and Kaposi’s sarcoma; magnetic resonance imaging (MRI) can be useful in evaluation of the tumor expansion and preoperative diagnosis (5, 11). Surgical excision is the best treatment for both encapsulated and un-capsulated angiolipomas (2, 3, 7). Because infiltrating angiolipoma often penetrates the surrounding tissues, complete resection of the tumor may damage the surrounding structures (5, 7). In the maxillofacial region, due to the existence of many vital structures, magnified operation is necessary to prevent damage to these structures, but in some situations sacrificing a branch of nerves is inevitable (12). According to previous studies, the relapse rate of infiltrating angiolipoma is 35-50%(6). Two possible causes of the recurrence of infiltrating angiolipoma after surgery are incorrect evaluation of the extent of the tumor and inadequate tumor resection during surgery (5).
CONCLUSION
Angiolipoma is a variant of lipoma considered as one of differential diagnoses of the head and neck mass for proper treatment.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Namazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
We did not receive any specific grant from the funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Ohnishi Y, Watanabe M, Fujii T, Yasui H, Kubo H, Kakudo K. Infiltrating angiolipoma of the lower lip: A case report and literature review. Oncol Lett. 2015;9(2):833–6. doi: 10.3892/ol.2014.2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akyüz C, Emir S, Büyükpamukçu M, Büyükpamukçu N, Cağlar M, Kale G, et al. Successful treatment with interferon alfa in infiltrating angiolipoma: a case presenting with Kasabach-Merritt syndrome. Archives of Disease in Childhood. 2003;88(1):67–8. doi: 10.1136/adc.88.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arenaz Búa J, Luáces R, Lorenzo Franco F, García-Rozado A, Crespo Escudero JL, Fonseca Capdevila E, et al. Angiolipoma in head and neck: report of two cases and review of the literature. Int J Oral Maxillofac Surg. 2010;39(6):610–5. doi: 10.1016/j.ijom.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 4.Carrasco Moro R, Gutiérrez Cierco JA, Martínez San Millán JS, Pian H, Martínez Rodrigo MA. Spinal extradural angiolipomas: 7 new cases and review of the literature. Neurologia (Barcelona, Spain) 2019;34(2):98–104. doi: 10.1016/j.nrl.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Chandrasekaran D, Chinnaswami R, Narasimhan M, Kumar AE, Natarajan P. Non Infiltrating Angiolipoma of the Palate in Geriatric Patient: A Case Report with Review of Literature. J Clin Diagn Res. 2016;10(1):Zd01–2. doi: 10.7860/JCDR/2016/16634.7032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reiser V, Haj Yahya B, Chaushu G, Kaplan I, Hamzani Y. Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management. Medicina (Kaunas, Lithuania) 2020;56:6. doi: 10.3390/medicina56060283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah VS, Harish M, Patel JR, Shah N. Infiltrating angiolipoma of the cheek. BMJ Case Reports. 2013:2013. doi: 10.1136/bcr-2013-200041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garib G, Siegal GP, Andea AA. Autosomal-dominant familial angiolipomatosis. Cutis. 2015;95(1):E26–9. [PubMed] [Google Scholar]
- 9.Panagopoulos I, Gorunova L, Andersen K, Lobmaier I, Bjerkehagen B, Heim S. Consistent Involvement of Chromosome 13 in Angiolipoma. Cancer Genomics & Proteomics. 2018;15(1):61–5. doi: 10.21873/cgp.20065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papakonstantinou PE, Korkolopoulou P, Lassithiotakis D, Lolis ED. Giant angiolipoma of the arm in an elderly patient. Annals of the Royal College of Surgeons of England. 2016;98(6):e100–2. doi: 10.1308/rcsann.2016.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali MH, el-Zuebi F. Angiolipoma of the cheek: report of a case. J Oral Maxillofac Surg. 1996;54(2):213–5. doi: 10.1016/s0278-2391(96)90450-4. [DOI] [PubMed] [Google Scholar]
- 12.Motazedian G, Khojasteh A, Motazedian N, Anbardar MH. Cavernous Hemangioma of Temporalis Muscle: A Case Report. World J Plast Surg. 2020;9(1):99–102. doi: 10.29252/wjps.9.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]