To the Editor:
Lung cancer is the leading cause of cancer death in the United States in part because only 15% of lung cancers are diagnosed at a curable stage (1). Screening with low-dose computed tomography (LDCT) has been shown to reduce lung cancer mortality by up to 20% (2), and the United States Preventive Services Task Force recommends annual screening with LDCT for high-risk adults aged 55–80 years with a 30-pack-year smoking history and who currently smoke or have quit within the previous 15 years. Despite this recommendation, uptake of screening has been poor, and in 2015, less than 4% of those eligible were screened (3). The United States Preventive Services Task Force recommends screening be conducted in facilities with licensed staff with experience in interpreting LDCT scans and a team of specialists who can provide appropriate follow-up. Although underuse of lung cancer screening may be due to a number of potential barriers, here we specifically investigate spatial access to lung cancer screening centers.
Methods
Data sources
We used data (as of June 2019) from the GO2 Foundation for Lung Cancer to obtain the geographic location of each Screening Center of Excellence (SCOE) (4) (which is equivalent to the Lung Cancer Screening Registry from the American College of Radiology), data from the U.S. Centers for Disease Control and Prevention about age-adjusted lung cancer mortality rates for each county in the 48 contiguous states of the United States (5), and County Health Rankings and Roadmaps data about adult smoking rates and racial makeup of each county (6). The SCOE designation recognizes medical facilities that provide responsible, high-quality LDCT screening for early detection of lung cancer and comply with comprehensive standards based on best practices. This study was based on publicly available data that did not include patient information and therefore did not require institutional review board approval.
Variables
Employing Jenks natural breaks, county-level age-adjusted lung cancer mortality and smoking rates were categorized into three levels (7). Counties with mortality rates above 53.2 deaths per 100,000 people were classified as “high mortality”; 21.8–53.2 deaths per 100,000 people as “medium”; and <21.8 deaths per 100,000 people as “low.” Counties with smoking rates above 21% were classified as “high”; 17–21% as “medium”; and <17% as “low.” In addition, racial composition of counties was defined as having a non-Hispanic white population <50% or >50%.
Analytical strategy
We used ArcGIS 10.8 software (ESRI) to geocode SCOEs across the contiguous United States. We calculated the Manhattan distance drive-time from these centers using ArcGIS Network Analyst (8) and created 30- and 60-minute drive-time polygons around each SCOE. We chose 60-minute drive-time as our primary threshold for analysis based on previous studies that have demonstrated that a drive-time beyond 60 minutes limits care-seeking among patients (9). We then determined the number, location, and racial distribution of counties with a high mortality rate of lung cancer and high smoking rates with screening services beyond 60 minutes’ drive-time (10).
Results
Of the total number of U.S. counties (3,139), high lung cancer mortality rates were 1,149 (37%); medium, 1,526 (49%); and low, 464 (15%). More than a third (36%) of the counties with high lung cancer mortality rates (416/1,149) were beyond 60 minutes’ drive-time from an SCOE. In addition, 61% (369/554) of counties with high adult smoking rates were beyond 60 minutes’ drive-time from an SCOE. These counties had a combined population of approximately 60.5 million people, about 19% of the country’s population. In addition, whereas one county with a population of 615,397 had 20 SCOEs, there were 2,796 counties (combined population of 76,901,223) without a single SCOE.
Of the 698 geocoded SCOEs, there is a large cluster in the Northeast and Midwestern corridors of the United States, whereas many high-mortality low-access counties are clustered in the Appalachian and Southeastern regions of the United States (Figure 1). Figure 2 highlights counties with high smoking and high lung cancer mortality rates that are beyond 60 minutes away from an SCOE (in red), which are also clustered in the Southeastern and Appalachian regions. Figure 3 presents the racial composition of these counties with high lung cancer and smoking rates. The counties with a non-Hispanic white population <50% (red) are clustered mostly in the Mississippi Delta and Alabama Black Belt regions.
Figure 1.
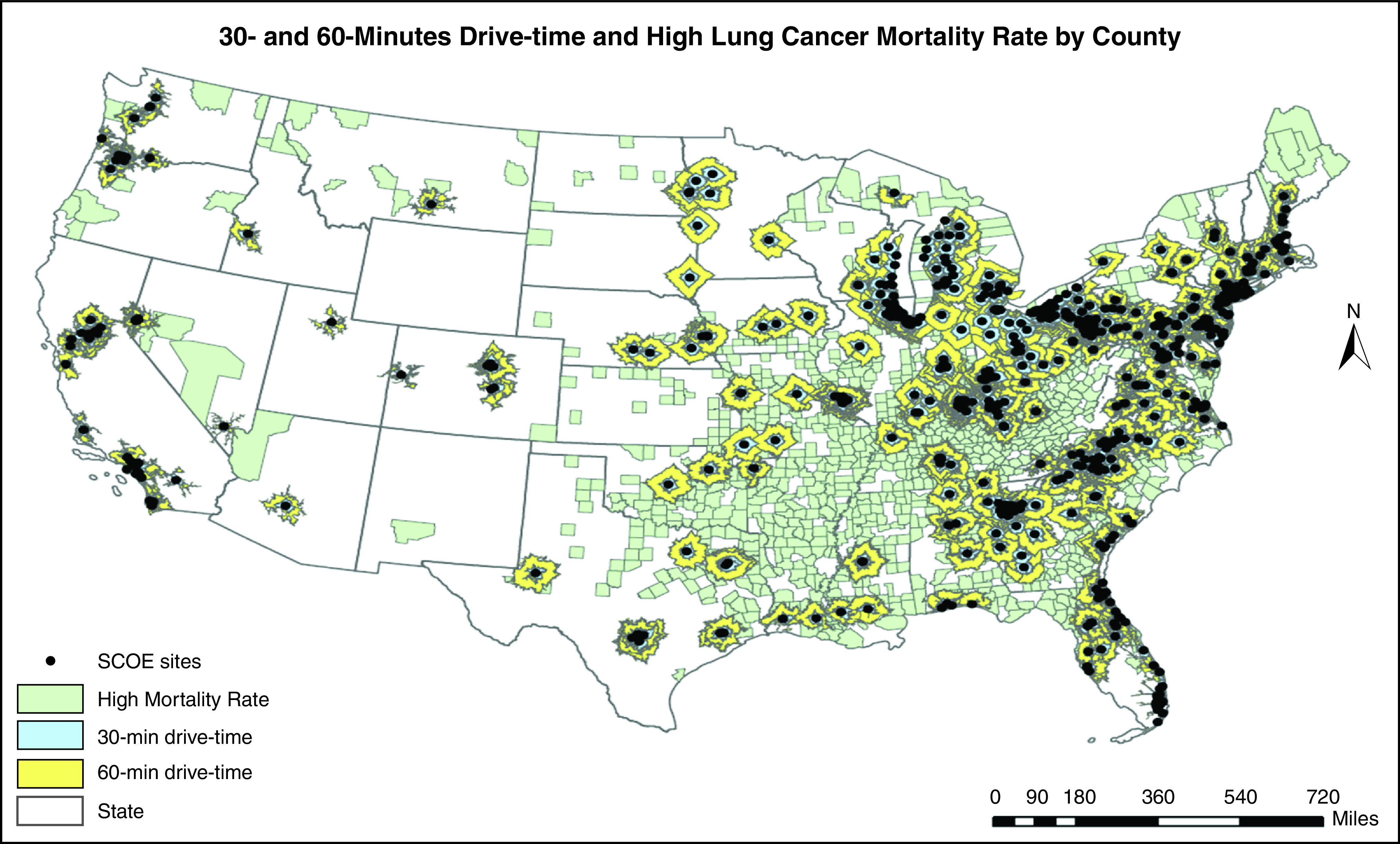
The 30- and 60-minutes drive-time and high lung cancer mortality rate by county. SCOE = Screening Center of Excellence.
Figure 2.
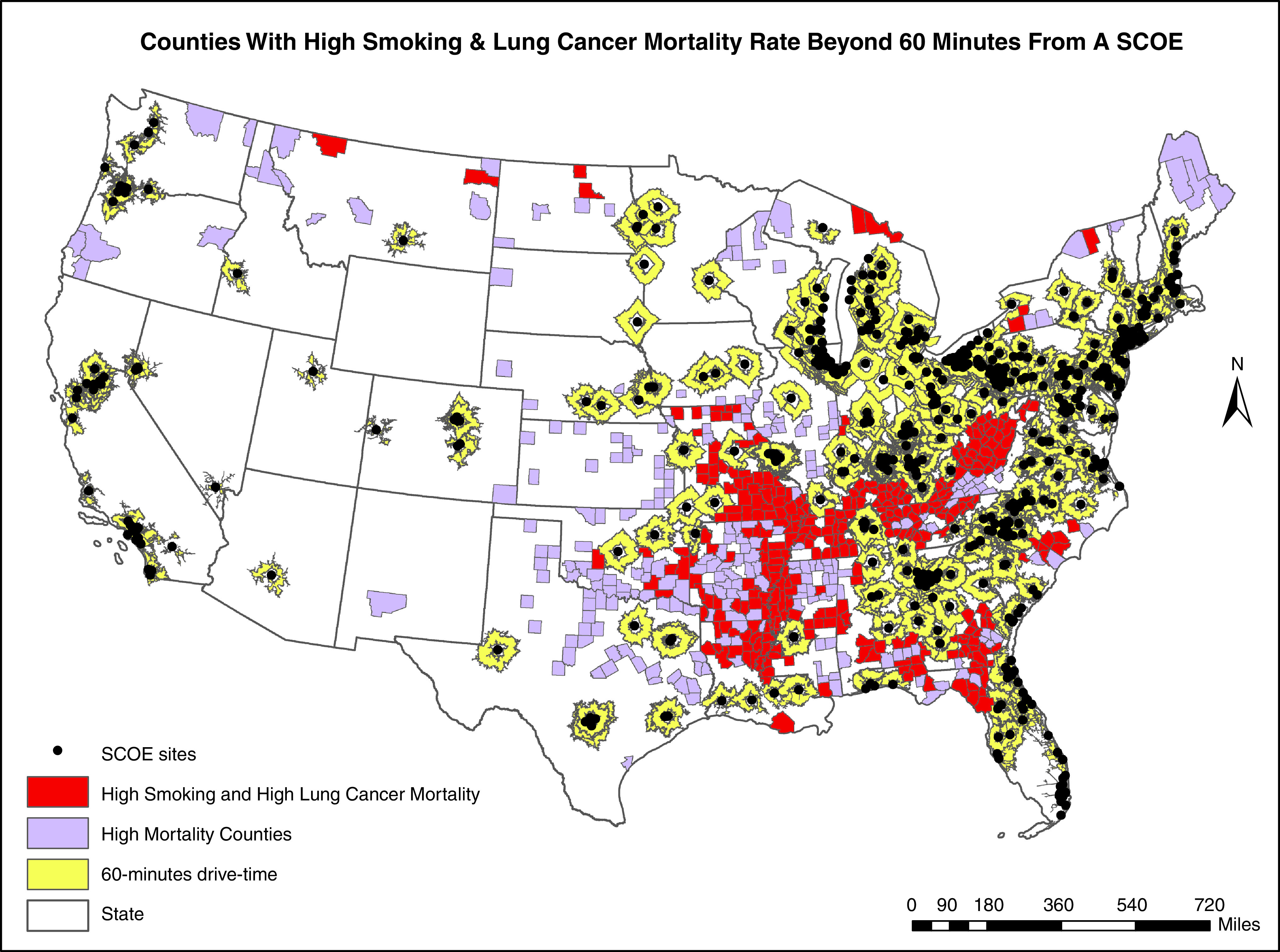
Distribution of counties with high smoking and lung cancer mortality rates beyond 60 minutes from an SCOE. SCOE = Screening Center of Excellence.
Figure 3.
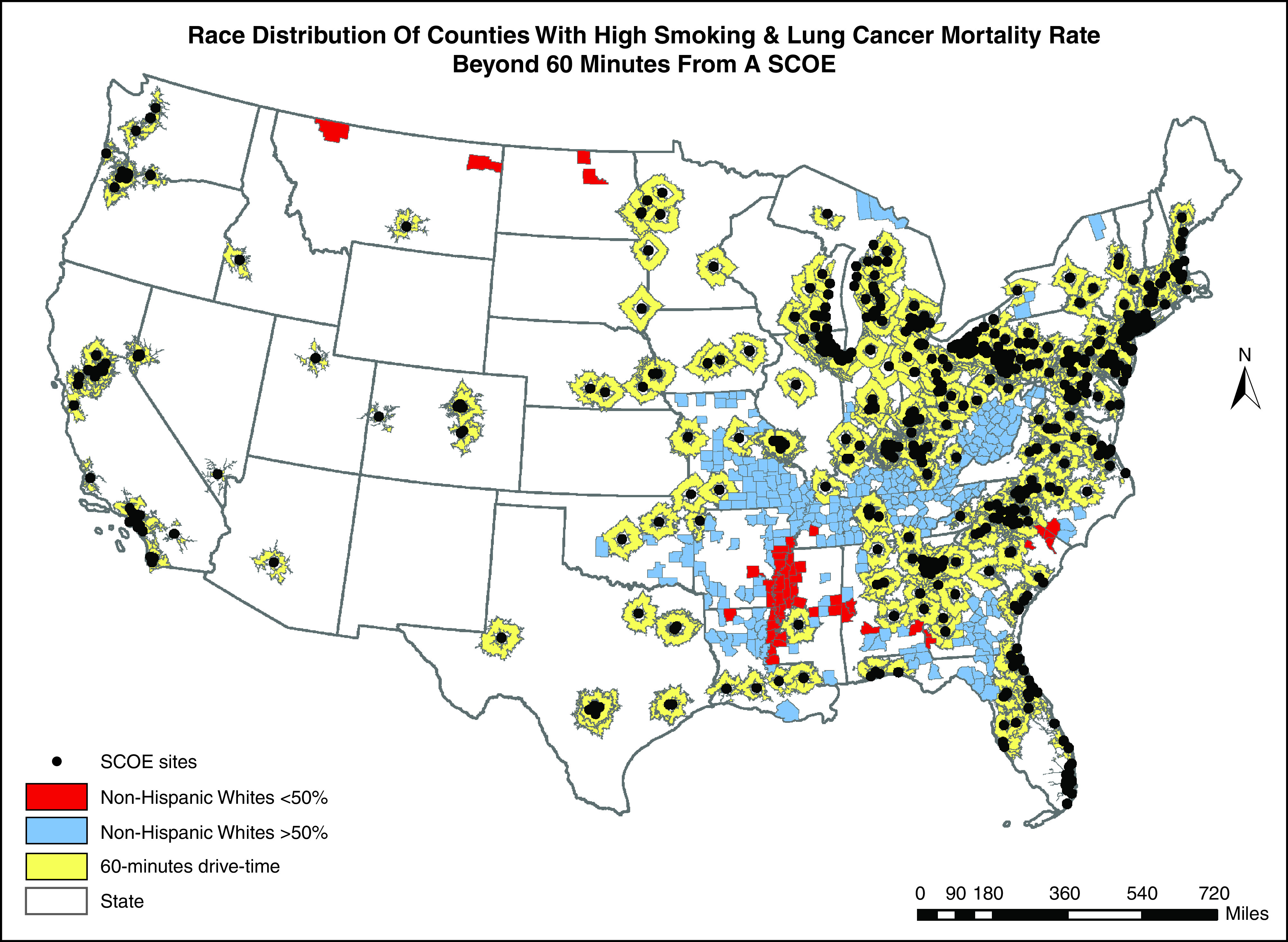
Race distribution of counties with high smoking and lung cancer mortality rates beyond 60 minutes from an SCOE. SCOE = Screening Center of Excellence.
Discussion
To our knowledge, this is the first study to map and characterize geographic access to SCOEs in the United States and identify high-need areas not currently served. Counties with high rates of lung cancer mortality and poor access to an SCOE have a combined population of 80.5 million, which is 25% of the entire U.S. population. This suggests that, for many people, geographic barriers may be a primary factor in the decision not to pursue lung cancer screening. These counties are located disproportionately in the resource-poor areas of the Southeast and Appalachia, which have also observed an exponential increase in lung cancer mortality in recent years (11). Moreover, rates of adenocarcinoma are rising fastest in rural counties and those increases are occurring at a higher rate in African Americans (12). Clearly, expanding screening services in these regions is critical.
Although this study provides valuable new insight into the spatial distribution of SCOEs, there are limitations. First, the travel time analysis used omits the travel time analyses for Alaska and Hawaii because of the potential for non–road‐based travel. Second, we relied on secondary data, collected primarily for public reporting purposes. Geographic access is only one dimension of access to care, but it represents potential access (13) for populations within regions served by SCOEs. Nonspatial factors such as lack of transportation, trust in providers, test results that were inconclusive, the need for annual screening (14), and unreimbursed direct and indirect costs for downstream diagnostic testing and procedures may also present barriers to uptake and should be modeled together with spatial factors to predict use. Notwithstanding these limitations, our work augments previous calls for more screening centers needed to care for the high number of rural smokers at risk for lung cancer (15–17). While a previous study demonstrated an inverse relationship between driving distance to a screening facility and population density (18), our work adds to recent literature using a road network analysis to calculate travel distances, which found that 18% of U.S. counties had no access to screening centers (19). Furthermore, the identified areas can also be used to set up mobile screening units (20) that can function like a stationary spoke site.
Conclusions
Lung cancer screening needs to be accessible outside of urban centers to improve uptake. Our study has identified potential areas for setting up screening centers for lung cancer.
Footnotes
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin . 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2. Aberle D, Adams A, Berg CJD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med . 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States—2010 to 2015. JAMA Oncol . 2017;3:1278–1281. doi: 10.1001/jamaoncol.2016.6416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parham K, Fine L. GO2 Foundation for Lung Cancer helping meet patients’ educational and support needs. J Oncol Navig Surviv . 2019;10 [Google Scholar]
- 5.National Program of Cancer Registries and Surveillance, Epidemiology, and End Results SEER*Stat Database. National Program of Cancer Registries and Surveillance, Epidemiology, and End Results SEER*Stat Database: NPCR and SEER Incidence – US Cancer Statistics 2001–2016 Public Use Research Database, November 2018 submission (2001–2016), United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; https://www.cdc.gov/cancer/uscs/public-use [Google Scholar]
- 6.Robert Wood Johnson Foundation. University of Wisconsin-Madison; 2013. [Google Scholar]
- 7. Leite JB, Mantovani JRS, Dokic T, Yan Q, Chen PC, Kezunovic M. Resiliency assessment in distribution networks using GIS-based predictive risk analytics. IEEE Trans Power Syst . 2019;34:4249–4257. [Google Scholar]
- 8. Apparicio P, Gelb J, Dubé A-S, Kingham S, Gauvin L, Robitaille É. The approaches to measuring the potential spatial access to urban health services revisited: distance types and aggregation-error issues. Int J Health Geogr . 2017;16:32. doi: 10.1186/s12942-017-0105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place . 2005;11:131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 10. Rahimi F, Goli A, Rezaee R. Hospital location-allocation in Shiraz using Geographical Information System (GIS) Shiraz E Med J . 2017;18:e57572. [Google Scholar]
- 11. Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, Stubbs RW, Bertozzi-Villa A, Morozoff C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. JAMA . 2017;317:388–406. doi: 10.1001/jama.2016.20324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Houston KA, Mitchell KA, King J, White A, Ryan BM. Histologic lung cancer incidence rates and trends vary by race/ethnicity and residential county. J Thorac Oncol . 2018;13:497–509. doi: 10.1016/j.jtho.2017.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Onega T, Alford-Teaster J, Wang F. Population-based geographic access to parent and satellite national cancer institute cancer center facilities. Cancer . 2017;123:3305–3311. doi: 10.1002/cncr.30727. [DOI] [PubMed] [Google Scholar]
- 14. Mishra SI, Sussman AL, Murrietta AM, Getrich CM, Rhyne R, Crowell RE, et al. Peer reviewed: patient perspectives on low-dose computed tomography for lung cancer screening, New Mexico, 2014. Prev Chronic Dis . 2016;33:E108. doi: 10.5888/pcd13.160093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin AN, Hassinger TE, Kozower BD, Camacho F, Anderson RT, Yao N. Disparities in lung cancer screening availability: lessons from southwest Virginia. Ann Thorac Surg . 2019;108:412–416. doi: 10.1016/j.athoracsur.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Odahowski CL, Zahnd WE, Eberth JM. Challenges and opportunities for lung cancer screening in rural America. J Am Coll Radiol . 2019;16:590–595. doi: 10.1016/j.jacr.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 17. Kale MS, Wisnivesky J, Taioli E, Liu B. The landscape of US lung cancer screening services. Chest . 2019;155:900–907. doi: 10.1016/j.chest.2018.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tailor TD, Choudhury KR, Tong BC, Christensen JD, Sosa JA, Rubin GD. Geographic access to CT for lung cancer screening: a census tract-level analysis of cigarette smoking in the United States and driving distance to a CT facility. J Am Coll Radiol . 2019;16:15–23. doi: 10.1016/j.jacr.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 19. Sahar L, Wills VLD, Liu KK, Kazerooni EA, Dyer DS, Smith RA. Using geospatial analysis to evaluate access to lung cancer screening in the United States. Chest . 2021;159:833–844. doi: 10.1016/j.chest.2020.08.2081. [DOI] [PubMed] [Google Scholar]
- 20. Raghavan D, Wheeler M, Doege D, Doty JD, II, Levy H, Dungan KA, et al. Initial results from mobile low‐dose computerized tomographic lung cancer screening unit: improved outcomes for underserved populations. Oncologist . 2020;25:e777–e781. doi: 10.1634/theoncologist.2019-0802. [DOI] [PMC free article] [PubMed] [Google Scholar]


