Supplemental Digital Content is available in the text.
Keywords: education, income, out-of-hospital cardiac arrest, socioeconomic factors
Abstract
Background:
Despite the acknowledged importance of socioeconomic factors as regards cardiovascular disease onset and survival, the relationship between individual-level socioeconomic factors and survival after out-of-hospital cardiac arrest is not established. Our aim was to investigate whether socioeconomic variables are associated with 30-day survival after out-of-hospital cardiac arrest.
Methods:
We linked data from the Swedish Registry for Cardiopulmonary Resuscitation with individual-level data on socioeconomic factors (ie, educational level and disposable income) from Statistics Sweden. Confounding and mediating variables included demographic factors, comorbidity, and Utstein resuscitation variables. Outcome was 30-day survival. Multiple modified Poisson regression was used for the main analyses.
Results:
A total of 31 373 out-of-hospital cardiac arrests occurring in 2010 to 2017 were included. Crude 30-day survival rates by income quintiles were as follows: Q1 (low), 414/6277 (6.6%); Q2, 339/6276 (5.4%); Q3, 423/6275 (6.7%); Q4, 652/6273 (10.4%); and Q5 (high), 928/6272 (14.8%). In adjusted analysis, the chance of survival by income level followed a gradient-like increase, with a risk ratio of 1.86 (95% CI, 1.65–2.09) in the highest-income quintile versus the lowest. This association remained after adjusting for comorbidity, resuscitation factors, and initial rhythm. A higher educational level was associated with improved 30-day survival, with the risk ratio associated with postsecondary education ≥4 years being 1.51 (95% CI, 1.30–1.74). Survival disparities by income and educational level were observed in both men and women.
Conclusions:
In this nationwide observational study using individual-level socioeconomic data, higher income and higher educational level were associated with better 30-day survival after out-of-hospital cardiac arrest in both sexes.
Clinical Perspective.
What Is New?
Until recently, most research on socioeconomic differences in out-of-hospital cardiac arrest has involved area-level data.
Owing to the risk of high collinearity, often only 1 socioeconomic status measurement has been used; our study shows that both disposable income and education have independent associations with 30-day survival after out-of-hospital cardiac arrest.
The relationship between disposable income and 30-day survival is more robust for mediating factors compared with educational level.
What Are the Clinical Implications?
These findings highlight the importance of preventive efforts aimed at patients with lower socioeconomic status.
These preventive actions could include both early recognition/warning signs and cardiopulmonary resuscitation/automated external defibrillator training.
Out-of-hospital cardiac arrest (OHCA) affects ≈180 000 individuals in the United States1 and ≈300 000 in Europe annually, with an overall mortality rate of ≈90%.2 Previous research has established clinical factors that improve survival after OHCA,3 but less attention has been paid to socioeconomic differences, despite the well-known associations between socioeconomic status (SES) and other cardiovascular health outcomes.4–6 The majority of studies concerning the relationship between SES and survival after OHCA have involved area-level measurements.7,8 However, the association between individual-level SES and survival after OHCA has not been properly established, primarily because of lack of access to a large amount of representative individual-level data, which is a shortcoming in previous research.
Research using data at neighborhood or other aggregated levels can lead to biased conclusions concerning relationships at the individual level as a result of ecologic fallacies.9 Previous studies carried out with individual-level data are few and have suffered from small sample sizes as well as reliance on specific subgroups of the OHCA population, such as children and adolescents,10 patients with shockable rhythm,11 patients admitted to hospital,12 and cardiac arrests of cardiac origin.13
Socioeconomic disparities in OHCA survival highlight the importance of appropriate policy measures that address the underlying causes of lower rates of survival in some groups—such as policies to reduce disparities in comorbidities and patterns of health behavior—as well as targeted interventions, such as training in cardiopulmonary resuscitation (CPR) and placement of automated external defibrillators (AEDs).
The aim of the present study was to investigate, in representative nationwide data, whether individual-level socioeconomic factors, measured by educational level and disposable income, are associated with 30-day survival of patients with OHCA.
Methods
Study Design and Setting
This observational registry-based cohort study includes all registered OHCAs in Sweden between January 1, 2010, and December 31, 2017. Sweden has a population of ≈10 million and covers 450 295 km2. Ambulances in Sweden are usually staffed by registered nurses and medical technicians. In cases of OHCA, 2 ambulances are dispatched and in addition to these, firefighters and police officers are dispatched in some regions. A number of regions have a system in which volunteers are dispatched to perform CPR and to fetch AEDs.
Data Availability
Data cannot be shared for privacy reasons. Detailed analytic methods will be shared on reasonable request.
Swedish Register of Cardiopulmonary Resuscitation
The Swedish Register of Cardiopulmonary Resuscitation (SRCR) maintains a national high-quality register with support from the Swedish Association of Local Authorities and Regions. The SRCR was created in the early 1990s, and since 2010, all emergency medical services (EMS) providers in Sweden report to it. The report template for the SRCR follows Utstein guidelines.14
Sociodemographic Data
Data on disposable income, the highest educational level attained, and marital status were collected from Statistics Sweden, which keeps registers on all residents in Sweden. Income was measured as disposable income per consumption unit,15 which reflects a weighted income on the basis of family structure (eg, 2 adults with no children would have a lower weight compared with 2 adults with 2 children). All residents in Sweden have a unique personal identification number, allowing us to link data from SRCR to Statistics Sweden’s registers.
Comorbidity Data
Comorbidity data were collected from the National Patient Registry. The National Patient Registry is maintained by the National Board of Health and Welfare and collects International Classification of Diseases–10 codes for all inpatient and outpatient visits in Sweden. We collected International Classification of Diseases–10 codes covering a 5-year period before each OHCA. The codes were later recoded into the Charlson Comorbidity Index using updated weights.16
Geographic Data
Distance to the nearest hospital was calculated by using an open street map routing machine and the proportions of cases with a foreign background during 2017 (defined as either born outside Sweden or born in Sweden with both parents born abroad) were calculated in demographic statistics areas. These areas were developed by Statistics Sweden and are similar to census tracts.
Exposure and Outcome
Income and educational level were obtained for the year before the OHCA. Income was coded into quintiles stratified by year. Education was categorized into primary (≤9 years), secondary (12 years), postsecondary up to 2 years more (13–14 years), postsecondary up to 3 years more (15 years), and postsecondary up to 4 years or more (≥16 years). The outcome was survival to 30 days after OHCA.
Selection of Patients
Patients <25 years of age were excluded because many of them may have been pursuing postsecondary education. OHCAs witnessed by EMS were excluded from the main analysis because of the questionable validity of some variables, especially bystander CPR and EMS response time. The cases witnessed by EMS are presented as a separate analysis in Table S1.
Statistical Analyses
Categorial variables are presented as counts and proportions and continuous variables as medians and quartiles. To account for missing data on covariates, multiple imputation with chained equations was used. Missing data were assumed to be missing at random. Regression analysis was used in each of the 10 imputed datasets and the results were pooled using Rubin rules.
Separate multivariable analyses were conducted for income and educational differences in relation to survival. Five modified Poisson regression17 models were estimated in each case: model 1 included the socioeconomic measure of primary interest (income or education) as well as potential confounders (sex, age, retired/not retired, year, and marital status). In model 2, we added Charlson Comorbidity Index, and in model 3, we added the other SES indicator (ie, income for analysis of educational disparities and vice versa). Model 4 included the abovementioned variables as well as the Utstein resuscitation variables (EMS response time, location, witnessed status, etiology, bystander CPR, CPR by firefighters/police), and in model 5 we also added initial rhythm (shockable/nonshockable). We used 2 additional models in a subset where we had information on route distance to the nearest hospital (model 6) and the proportion of persons with a foreign background (in quintiles) in the area where the cardiac arrest occurred. In the education analysis, model 1 was regarded as the primary model. In the income analysis, model 3 was regarded as the primary model, because all potential confounders were included. Continuous variables (age, EMS response time) were included as natural cubic splines with 3 knots.
Subgroup analyses were performed in relation to sex, adjusting for the potential confounders (models 1 and 3 above). All tests were 2-sided and P<0.05 was considered statistically significant. All analyses were performed in R version 4.0.3 (R Foundation for Statistical Computing). The regional ethics board in Stockholm approved the study and the requirement of informed consent was waived (identification number 2017/714-31/5).
Results
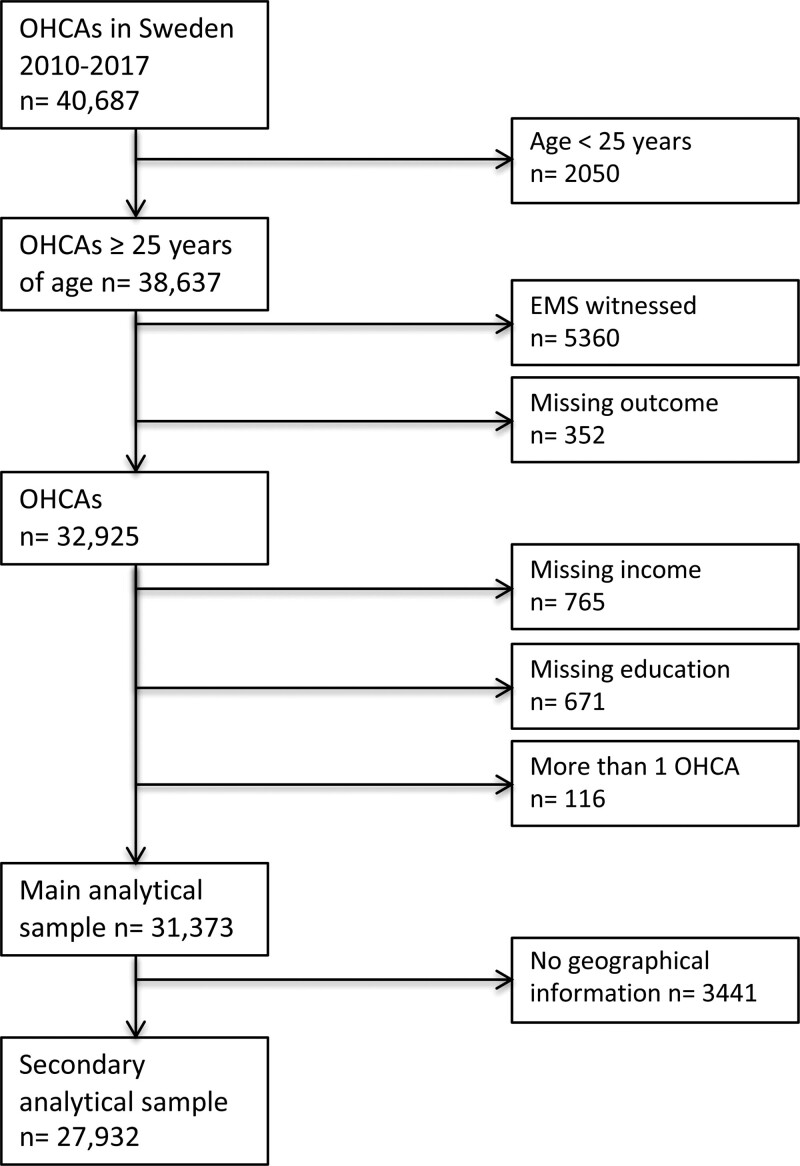
As shown in Figure 1, 40 687 OHCAs occurred between 2010 and 2017. Of these, 2050 occurred in people younger than 25 and these cases were excluded. An additional 5360 cases were excluded because they were witnessed by EMS and another 352 cases were excluded because of missing data on survival status. In 765 cases, there was missing information on family disposable income and in an additional 671 cases there was missing information on education. An additional 116 persons had >1 OHCA during the study period; in these cases, the first OHCA was included. The main analytic sample consisted of 31 373 patients with OHCA. We excluded an additional 3441 patients without geographic information in the secondary analytic sample (Figure 1).
Figure 1.
Selection of patients. EMS indicates emergency medical services; and OHCA, out-of-hospital cardiac arrest.
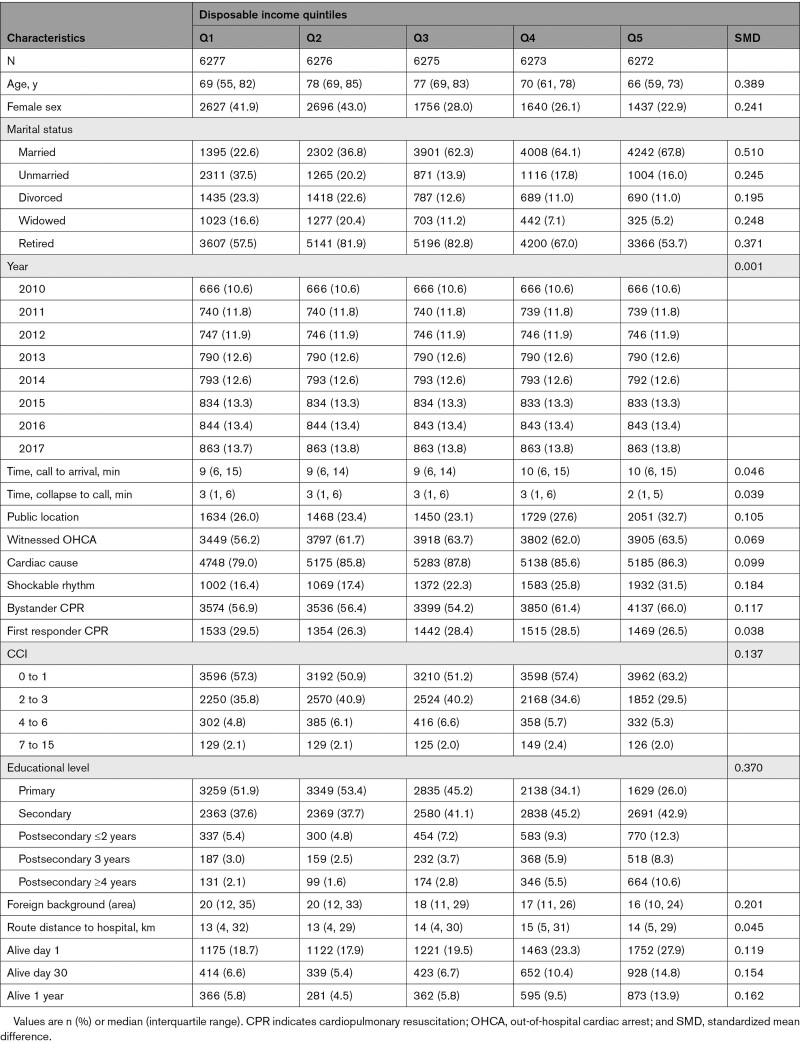
Baseline characteristics in relation to income level are presented in the Table. Notable differences between the income groups were seen in age, sex, proportion with shockable initial rhythm (Q1, 16.4%; Q5, 31.5%), bystander CPR (Q1, 56.9%; Q5, 66.0%), marital status, and educational level. The same table categorized by education is included in Table S2.
Table.
Baseline Characteristics by Income Quintiles
Crude Differences in Survival
The proportion of patients alive after 30 days (categorized by disposable income) was 6.6% (414/6277) in the lowest income quintile compared with 14.8% (928/6272) in the highest income quintile. The corresponding proportion among patients with only primary education was 7.2% (945/13 210) compared with 13.1% (185/1414) among patients with ≥4 years of tertiary education.
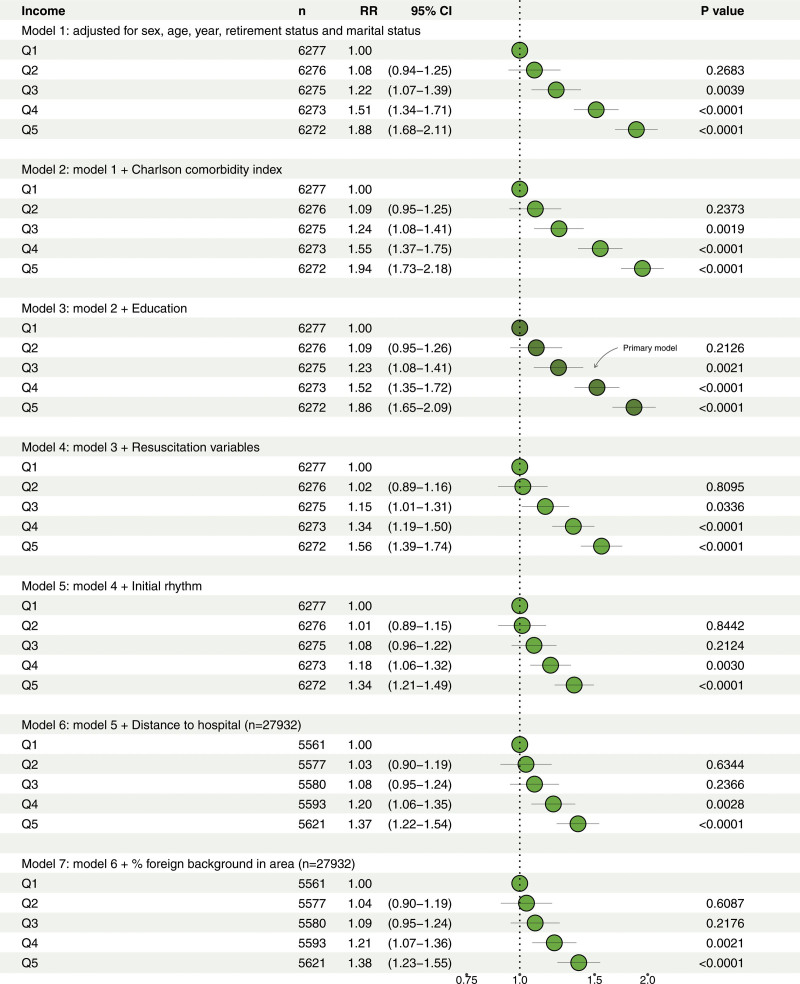
Associations Between Income Level and 30-Day Survival After OHCA
Figure 2 shows risk ratios (RRs) of 30-day survival after OHCA for each income quintile in comparison with the lowest income quintile from 5 separate covariate models. The results were consistent across models 1 (sex, age, year of OHCA, retirement, and marital status) and 2 (comorbidity), demonstrating a clear positive income gradient in survival after OHCA. In our main model adjusted for educational level (model 3), the RRs were only slightly attenuated in comparison with those in models 1 and 2, with an RR of 1.86 (95% CI, 1.65–2.09) in the highest income group. Adjustment for Utstein resuscitation variables (model 4) attenuated the results further (RR for Q5 versus Q1, 1.56 [95% CI, 1.39–1.74]), and in model 5, where initial rhythm was added, the RR for survival was attenuated further to 1.34 (95% CI, 1.21–1.49) in the highest income group.
Figure 2.
Relationship between income and the chance of survival after out-of-hospital cardiac arrest. Model 1: adjusted for age, sex, year, retirement status, and marital status. Model 2: model 1 + Charlson Comorbidity Index. Model 3: Model 2 + education. Model 4: Model 3 + witness status, response time, location, bystander cardiopulmonary resuscitation, cardiopulmonary resuscitation by firefighter or police, and etiology. Model 5: Model 4 + initial rhythm. Model 6: Model 5 + route distance to nearest hospital. Model 7: Model 6 + proportion of foreign-born in area of cardiac arrest. RR indicates risk ratio.
Addition of route distance to nearest hospital (model 6) and proportion of people with a foreign background in the area of the OHCA (model 7) only slightly affected the results; the RR in the highest income quintile was 1.38 (95% CI, 1.23–1.55)
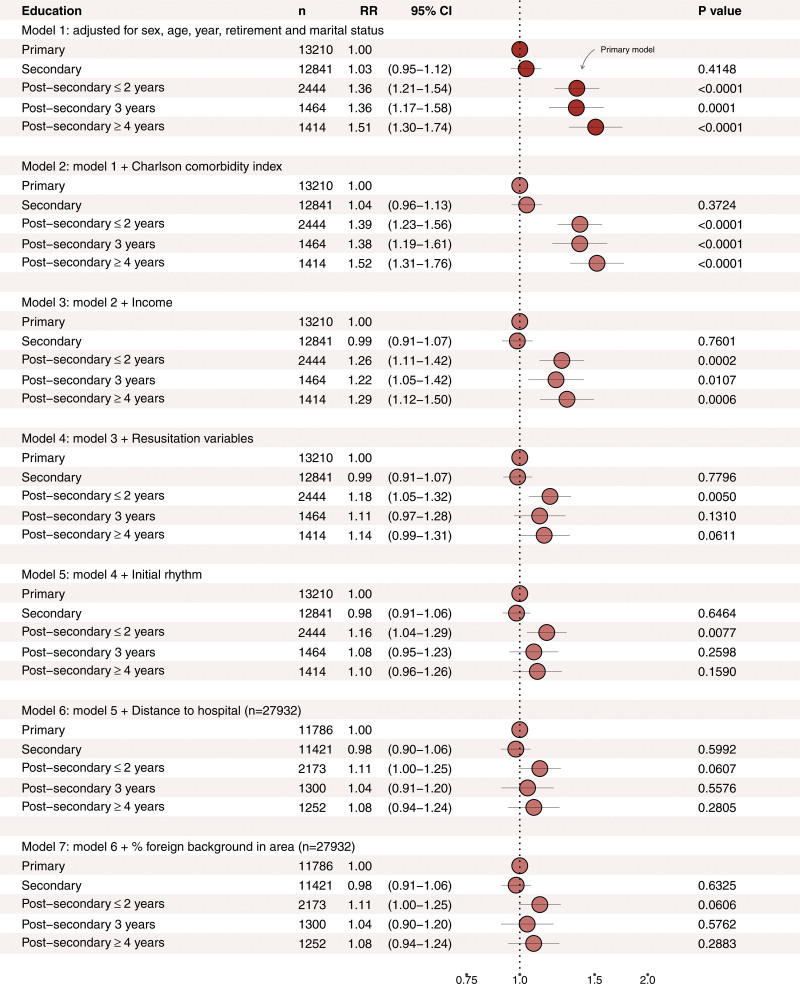
Associations Between Educational Level and 30-Day Survival After OHCA
Associations between educational level and 30-day survival after OHCA consistently demonstrated higher RRs of survival in individuals with postsecondary education (Figure 3). However, the associations did not differ substantially between educational levels beyond secondary school. In the primary model (model 1), the RR for 30-day survival was 1.51 (95% CI, 1.30–1.74). We did not observe any strong indication of confounding (by way of the Charlson Comorbidity Index), as RRs were similar in models 1 and 2. Mutual adjustment by household income level attenuated the results, although an independent association with educational level remained. Models including resuscitation variables and initial rhythm (models 4 and 5, respectively) demonstrated similar associations, although slightly attenuated, compared with the main model. Addition of distance to nearest hospital (model 6) and proportion of people with a foreign background in the area of the OHCA (model 7) further attenuated the results.
Figure 3.
Relationship between education and the chance of survival after out-of-hospital cardiac arrest. Model 1: adjusted for age, sex, year, retirement status, and marital status. Model 2: Model 1 + Charlson Comorbidity Index. Model 3: Model 2 + income. Model 4: Model 3 + witness status, emergency medical services response time, location, bystander cardiopulmonary resuscitation, cardiopulmonary resuscitation by firefighter or police, and etiology. Model 5: Model 4 + initial rhythm. Model 6: Model 5 + route distance to nearest hospital. Model 7: Model 6 + proportion of foreign-born in area of cardiac arrest. RR indicates risk ratio.
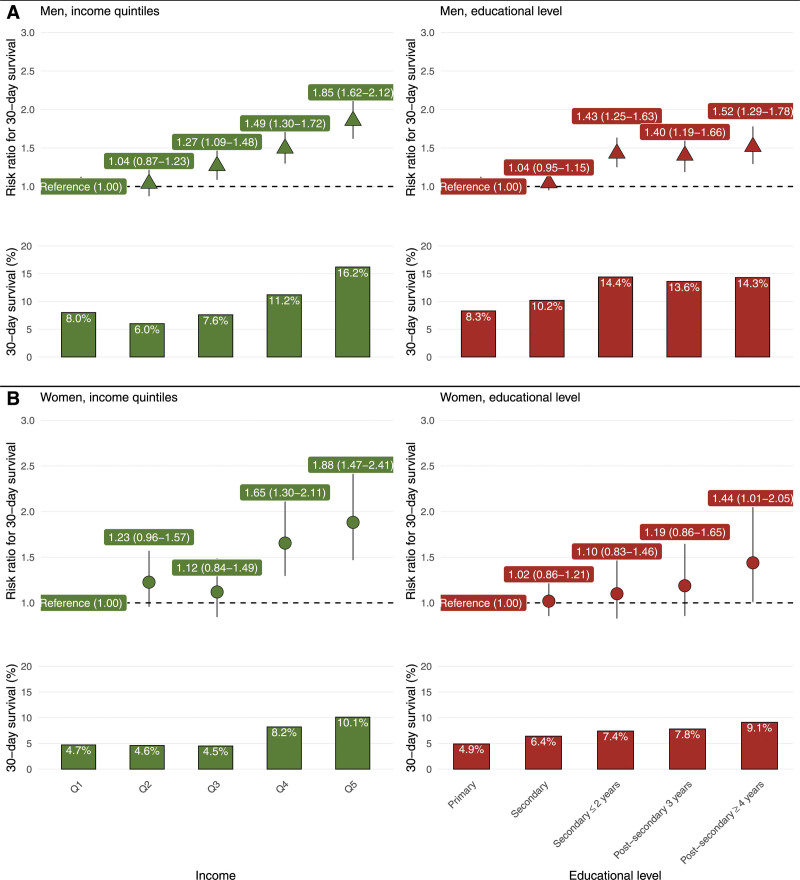
Stratification by Sex
Men
Among men, crude survival data displayed an increasing gradient with income level. The proportions alive after 30 days in the income quintiles are presented in Figure 4. After adjustment for potential confounders (age, retirement status, year, marital status, comorbidities, and education), the RR for 30-day survival displayed a gradient-like increase between each income quintile. The highest income quintile showed an adjusted RR of 1.85 (95% CI, 1.62–2.12). In the model adjusted for potential confounders (age, retirement status, year, and marital status), there was a positive association with any postsecondary education, and the highest RR for 30-day survival was in the highest educational group (RR, 1.52 [95% CI, 1.29–1.78]).
Figure 4.
Crude (proportions) and adjusted risk ratios regarding survival. Crude (proportions) and adjusted risk ratios regarding survival for men (A) and women (B). Model 3: income adjusted for age, year, marital status, Charlson Comorbidity Index, and education. Model 1: education adjusted for age, year, and marital status.
Women
For women, 30-day survival by income is shown in Figure 4. When adjusted for potential confounders (age, retirement status, year, marital status, comorbidities, and education), higher income remained associated with an increased chance of survival. The RR in the highest income quintile was 1.88 (95% CI, 1.47–2.41) compared with the lowest. Adjusted for potential confounders (age, retirement status, year, and marital status), the association between educational level and survival after OHCA followed a positive trend, with higher RRs for each increase in educational level. The highest RR was found among women with ≥4 years of postsecondary education (RR, 1.44 [95% CI, 1.01–2.05]).
Sensitivity Analyses
Analyses of EMS-witnessed cases (Table S1) and complete case analyses were carried out and the results are included in Figures S1 and S2. To check for a nonlinear association between income and survival after OHCA, adjusted natural cubic splines were used. The results from these models were similar to those presented in Figure 2 (forest plot) and followed an S-shaped curve with a lower probability of survival among patients with low SES (Figure S3). Age-stratified analyses are presented in Figures S4 and S5 together with the full models (all covariates included, models 1–7; Tables S3–S11).
DISCUSSION
The main findings of this study were pronounced positive independent associations of both income and educational level with survival after OHCA. The positive associations between income and 30-day survival were seen in both sexes. When SES was measured according to educational attainment, we found a higher survival rate among all men with postsecondary school degrees, but a more linear association among women.
An important finding in our study is that the associations between both SES variables and survival were not attenuated when controlling for comorbidity, contrary to hypotheses that a higher comorbidity burden among individuals with low SES may help explain their lower rate of survival after a cardiac arrest.8,14 However, the associations were somewhat attenuated after controlling for the well-known resuscitation variables, and for the income gradient in particular, after controlling for shockable initial rhythm. Factors such as bystander CPR18 and shockable initial rhythm3 are strong predictors of survival after OHCA and in this population they showed a socioeconomic gradient. SES disparities in relation to these variables suggest that individuals with higher SES are benefiting from access to more urgent and appropriate care by knowledgeable bystanders and medical personnel. The higher probability of a shockable initial rhythm among patients with high income is more difficult to explain. There were no clear differences between the income groups regarding EMS response time and time from OHCA to call.
A potential confounder not fully considered in this article is the role of race/ethnicity, as no such individual-level data were available. Among this relatively older cardiac arrest population, it may play a limited role. In this study, 85% of the patients with OHCA were >55 years of age. Among people older than 55 years in Sweden, 84.8% were born in Sweden, 4.9% were born in other Nordic countries, and 5.5% were born in other European countries.19 Adjustment for the proportion of foreign-born individuals in the area of the OHCA did not attenuate the results seen in any way. Although this adjustment is not perfect, it suggests that our results are fairly robust as regards this potential confounder.
The observation that survival is more clearly influenced by income than by educational attainment suggests that access to material resources—which are more related to income—is a more important factor predicting survival after OHCA than factors such as health-related knowledge, learned effectiveness, and control over one’s life, which are frequently associated with education.20 Income may capture differences in dietary choices and other health-related behavioral aspects, as well as cumulative exposure to daily stressors arising from one’s level of living21 and standing in relation to peers,22 which may affect vulnerability in the aftermath of cardiac arrest. A recent study revealed a relationship between low SES, higher amygdala activity, and higher bone marrow activity, which were strongly correlated to major adverse cardiac events.23 Cumulative stressors can also accelerate biological aging, as evidenced by associations between SES and telomere length,24 the latter also being a predictor of cardiovascular disease.25 The lower proportion of shockable initial rhythm may also be an effect of this mechanism, as an older patient’s rhythm may deteriorate to asystole or pulseless electrical activity more quickly. Income, more than education, can reflect reverse causality in relation to poor (cardiovascular) health.
Our results are largely in line with those of previous studies that have revealed an association between various area-level measurements of SES and survival after OHCA.7,26–28 In a recent study from Stockholm involving area-level data, we observed stronger associations between survival after OHCA and area-based educational level compared with area-based income level,29 in contrast to the results in the current study of a stronger association between survival after OHCA and individual-level income compared with individual-level education. The discrepancy between the findings is difficult to explain. One possibility is that it is a result of ecological fallacies (incorrectly applying associations from an aggregated level to the individual level). Another possibility is that areas with higher average levels of education have less crime, greater social cohesion, or other area-level characteristics that were not measured in the current study but may have independent effects on survival.
Previous studies involving individual-level data have included subgroups of the OHCA population such as patients with shockable initial rhythm11 or children and adolescents.10 Wells et al.11 found that individual-level education was a stronger predictor of survival than occupational status. Rajan et al.10 found no significant differences between socioeconomic variables after adjustment for covariates, a result that may reflect their limited sample size. A recent Danish study, including OHCAs of cardiac origin, revealed similar results, with a clear association between income and the chance of 30-day survival.13
Backholer et al.6 reported results from a meta-analysis suggesting stronger SES disparities in relation to coronary heart disease among women than men. This stronger relationship among women was not seen in our study. We found positive patterns in both sexes as regards the association between income and survival after OHCA, but clearer educational differences in connection with survival after OHCA among men.
Implications
Our results have implications as regards preventive efforts. Compared with individuals in the highest income quintile, those in the lowest income quintile showed an almost 10 percentage point difference in the proportion receiving bystander CPR before EMS arrival. CPR before EMS arrival is associated with an increased chance of survival after OHCA.18,30 Thus, great efforts should be made to educate people in lower socioeconomic groups in CPR training, including early recognition of an OHCA. This is in line with data from the United States that have shown a higher probability of being trained in CPR31 and AED usage32 in high-income households. Previous research has shown the importance of AED accessibility for bystander defibrillation.33 Distributed AEDs should therefore be located at well-known locations and have round-the-clock availability. In recent years, a number of services have been developed for dispatching laypersons in cases of suspected OHCA.34 Such services, together with CPR training and AED placement, may help reduce survival differences among patients of low SES with OHCA.
Strengths and Limitations
This study has several strengths. First, it is nationwide and included >30 000 OHCAs in Sweden. Second, we used 2 different measurements of SES, which can give insights into the mechanisms behind SES disparities. Third, we were able to adjust for the most important predictors of survival after OHCA, as well as previous patient comorbidities.
The study also has limitations. First, because of the observational nature of the data, it is not possible to exclude the risk of residual confounding. Second, we had missing information on 1436 (4.4%) individuals. Third, we did not report neurologic outcome, owing to the large percentage of missing data. Fourth, we had no individual-level data about race/ethnicity, which could potentially explain some of the associations. Fifth, we were not able to adjust for in-hospital treatments, which could explain some of the associations. Sixth, another possible explanation is a longer time between collapse and call, which could explain both differences in survival and shockable initial rhythm. Although there were no clear differences in baseline data, this measurement is subjective and may be biased.
Conclusions
In this nationwide observational study, using individual patient data, higher income and higher educational level were associated with improved 30-day survival after OHCA. This relationship was present in both men and women.
Article Information
Sources of Funding
This work was supported by grants from EU Horizon 2020 (ESCAPE-NET [European Sudden Cardiac Arrest Network: Towards Prevention, Education and New Treatment]) and the Swedish Heart–Lung Foundation. The funders had no role in study design, data collection, analysis, data interpretation, or writing of the final report.
Disclosures
Dr Ljung is employed at the Swedish Medical Products Agency. The views expressed in this article do not necessarily represent the views of the government agency. The other authors report no conflicts.
Supplemental Material
Figures S1–S5
Tables S1–S11
Supplementary Material
Nonstandard Abbreviations and Acronyms
- AED
- automated external defibrillator
- CPR
- cardiopulmonary resuscitation
- EMS
- emergency medical services
- OHCA
- out-of-hospital cardiac arrest
- RR
- risk ratio
- SES
- socioeconomic status
- SRCR
- Swedish Register for Cardiopulmonary Resuscitation
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.121.056012.
For Sources of Funding and Disclosures, see page 1924.
Contributor Information
Juho Härkönen, Email: Juho.harkonen@eui.eu.
Petter Ljungman, Email: petter.ljungman@ki.se.
Per Nordberg, Email: per.nordberg@sll.se.
Mattias Ringh, Email: mattias.ringh@ki.se.
Geir Hirlekar, Email: geir.hirlekar@vgregion.se.
Araz Rawshani, Email: araz.rawshani@gu.se.
Johan Herlitz, Email: johan.herlitz@hb.se.
Rickard Ljung, Email: rickard.ljung@ki.se.
Jacob Hollenberg, Email: jacob.hollenberg@ki.se.
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2020 update: a report from the American Heart Association. Circulation. 2020; 141:e139–e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 2.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010; 81:1479–1487. doi: 10.1016/j.resuscitation.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 3.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 4.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993; 88:1973–1998. doi: 10.1161/01.cir.88.4.1973 [DOI] [PubMed] [Google Scholar]
- 5.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009; 6:712–722. doi: 10.1038/nrcardio.2009.163 [DOI] [PubMed] [Google Scholar]
- 6.Backholer K, Peters SAE, Bots SH, Peeters A, Huxley RR, Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta-analysis. J Epidemiol Community Health. 2017; 71:550–557. doi: 10.1136/jech-2016-207890 [DOI] [PubMed] [Google Scholar]
- 7.van Nieuwenhuizen BP, Oving I, Kunst AE, Daams J, Blom MT, Tan HL, van Valkengoed IGM. Socio-economic differences in incidence, bystander cardiopulmonary resuscitation and survival from out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2019; 141:44–62. doi: 10.1016/j.resuscitation.2019.05.018 [DOI] [PubMed] [Google Scholar]
- 8.Chamberlain RC, Barnetson C, Clegg GR, Halbesma N. Association of measures of socioeconomic position with survival following out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2020; 157:49–59. doi: 10.1016/j.resuscitation.2020.09.025 [DOI] [PubMed] [Google Scholar]
- 9.Piantadosi S, Byar DP, Green SB. The ecological fallacy. Am J Epidemiol. 1988; 127:893–904. doi: 10.1093/oxfordjournals.aje.a114892 [DOI] [PubMed] [Google Scholar]
- 10.Rajan S, Wissenberg M, Folke F, Hansen CM, Lippert FK, Weeke P, Karlsson L, Søndergaard KB, Kragholm K, Christensen EF, et al. Out-of-hospital cardiac arrests in children and adolescents: incidences, outcomes, and household socioeconomic status. Resuscitation. 2015; 88:12–19. doi: 10.1016/j.resuscitation.2014.11.025 [DOI] [PubMed] [Google Scholar]
- 11.Wells DMD, White LLLY, Fahrenbruch CCE, Rea TD. Socioeconomic status and survival from ventricular fibrillation out-of-hospital cardiac arrest. Ann Epidemiol. 2016; 26:418–423.e1. doi: 10.1016/j.annepidem.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 12.Møller S, Wissenberg M, Kragholm K, Folke F, Hansen CM, Ringgren KB, Andersen J, Barcella C, Lippert F, Køber L, et al. Socioeconomic differences in coronary procedures and survival after out-of-hospital cardiac arrest: a nationwide Danish study. Resuscitation. 2020; 153:10–19. doi: 10.1016/j.resuscitation.2020.05.022 [DOI] [PubMed] [Google Scholar]
- 13.Møller S, Wissenberg M, Starkopf L, Kragholm K, Hansen SM, Ringgren KB, Folke F, Andersen J, Malta Hansen C, Lippert F, et al. Socioeconomic disparities in prehospital factors and survival after out-of-hospital cardiac arrest. Heart. 2021; 107:627–634. doi: 10.1136/heartjnl-2020-317761 [DOI] [PubMed] [Google Scholar]
- 14.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, et al. ; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004; 110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15 [DOI] [PubMed] [Google Scholar]
- 15.Ludvigsson JF, Svedberg P, Olén O, Bruze G, Neovius M. The Longitudinal Integrated Database for Health Insurance and Labour Market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019; 34:423–437. doi: 10.1007/s10654-019-00511-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173:676–682. doi: 10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 17.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004; 159:702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 18.Riva G, Ringh M, Jonsson M, Svensson L, Herlitz J, Claesson A, Djärv T, Nordberg P, Forsberg S, Rubertsson S, et al. Survival in out-of-hospital cardiac arrest after standard cardiopulmonary resuscitation or chest compressions only before arrival of emergency medical services: nationwide study during three guideline periods. Circulation. 2019; 139:2600–2609. doi: 10.1161/CIRCULATIONAHA.118.038179 [DOI] [PubMed] [Google Scholar]
- 19.Statistiska Centralbyrån. Statistikdatabasen. Published 2021. https://www.statistikdatabasen.scb.se/pxweb/sv/ssd/
- 20.Mirowsky J, Ross CE. Education, learned effectiveness and health. London Rev Educ. 2005; 3:205–220. doi: 10.1080/14748460500372366 [Google Scholar]
- 21.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006; 60:7–12. doi: 10.1136/jech.2004.023531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilkinson RG. Comment: income, inequality, and social cohesion. Am J Public Health. 1997; 87:1504–1506. doi: 10.2105/ajph.87.9.1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tawakol A, Osborne MT, Wang Y, Hammed B, Tung B, Patrich T, Oberfeld B, Ishai A, Shin LM, Nahrendorf M, et al. Stress-associated neurobiological pathway linking socioeconomic disparities to cardiovascular disease. J Am Coll Cardiol. 2019; 73:3243–3255. doi: 10.1016/j.jacc.2019.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Needham BL, Adler N, Gregorich S, Rehkopf D, Lin J, Blackburn EH, Epel ES. Socioeconomic status, health behavior, and leukocyte telomere length in the National Health and Nutrition Examination Survey, 1999-2002. Soc Sci Med. 2013; 85:1–8. doi: 10.1016/j.socscimed.2013.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haycock PC, Heydon EE, Kaptoge S, Butterworth AS, Thompson A, Willeit P. Leucocyte telomere length and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2014; 349:g4227. doi: 10.1136/bmj.g4227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahn KO, Shin SD, Hwang SS, Oh J, Kawachi I, Kim YT, Kong KA, Hong SO. Association between deprivation status at community level and outcomes from out-of-hospital cardiac arrest: a nationwide observational study. Resuscitation. 2011; 82:270–276. doi: 10.1016/j.resuscitation.2010.10.023 [DOI] [PubMed] [Google Scholar]
- 27.Clarke SO, Schellenbaum GD, Rea TD. Socioeconomic status and survival from out-of-hospital cardiac arrest. Acad Emerg Med. 2005; 12:941–947. doi: 10.1197/j.aem.2005.05.031 [DOI] [PubMed] [Google Scholar]
- 28.Lee SY, Song KJ, Shin SD, Ro YS, Hong KJ, Kim YT, Hong SO, Park JH, Lee SC. A disparity in outcomes of out-of-hospital cardiac arrest by community socioeconomic status: a ten-year observational study. Resuscitation. 2018; 126:130–136. doi: 10.1016/j.resuscitation.2018.02.025 [DOI] [PubMed] [Google Scholar]
- 29.Jonsson M, Härkönen J, Ljungman P, Rawshani A, Nordberg P, Svensson L, Herlitz J, Hollenberg J. Survival after out-of-hospital cardiac arrest is associated with area-level socioeconomic status. Heart. 2019; 105:632–638. doi: 10.1136/heartjnl-2018-313838 [DOI] [PubMed] [Google Scholar]
- 30.Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015; 372:2307–2315. doi: 10.1056/NEJMoa1405796 [DOI] [PubMed] [Google Scholar]
- 31.Blewer AL, Ibrahim SA, Leary M, Dutwin D, McNally B, Anderson ML, Morrison LJ, Aufderheide TP, Daya M, Idris AH, et al. Cardiopulmonary resuscitation training disparities in the United States. J Am Heart Assoc. 2017; 6:e006124. doi: 10.1161/JAHA.117.006124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owen DD, McGovern SK, Murray A, Leary M, Del Rios M, Merchant RM, Abella BS, Dutwin D, Blewer AL. Association of race and socioeconomic status with automatic external defibrillator training prevalence in the United States. Resuscitation. 2018; 127:100–104. doi: 10.1016/j.resuscitation.2018.03.037 [DOI] [PubMed] [Google Scholar]
- 33.Karlsson L, Malta Hansen C, Wissenberg M, Møller Hansen S, Lippert FK, Rajan S, Kragholm K, Møller SG, Bach Søndergaard K, Gislason GH, et al. Automated external defibrillator accessibility is crucial for bystander defibrillation and survival: a registry-based study. Resuscitation. 2019; 136:30–37. doi: 10.1016/j.resuscitation.2019.01.014 [DOI] [PubMed] [Google Scholar]
- 34.Ringh M, Rosenqvist M, Hollenberg J, Jonsson M, Fredman D, Nordberg P, Järnbert-Pettersson H, Hasselqvist-Ax I, Riva G, Svensson L. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med. 2015; 372:2316–2325. doi: 10.1056/NEJMoa1406038 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data cannot be shared for privacy reasons. Detailed analytic methods will be shared on reasonable request.