Supplemental Digital Content is available in the text.
Key Words: antidepressants, treatment indications, prescriptions, dispensing data, primary care, pharmacoepidemiology, administrative data
Abstract
Background:
Given the wide range of uses for antidepressants, understanding indication-specific patterns of prescription filling for antidepressants provide valuable insights into how patients use these medications in real-world settings.
Objective:
The objective of this study was to determine the association of antidepressant prescription filling with treatment indication, as well as prior prescription filling behaviors and medication experiences.
Design:
This retrospective cohort study took place in Quebec, Canada.
Participants:
Adults with public drug insurance prescribed antidepressants using MOXXI (Medical Office of the XXIst Century)—an electronic prescribing system requiring primary care physicians to document treatment indications and reasons for prescription stops or changes.
Measures:
MOXXI provided information on treatment indications, past prescriptions, and prior medication experiences (treatment ineffectiveness and adverse drug reactions). Linked claims data provided information on dispensed medications and other patient-related factors. Multivariable logistic regression models estimated the independent association of not filling an antidepressant prescription (within 90 d) with treatment indication and patients’ prior prescription filling behaviors and medication experiences.
Results:
Among 38,751 prescriptions, the prevalence of unfilled prescriptions for new and ongoing antidepressant therapy was 34.2% and 4.1%, respectively. Compared with depression, odds of not filling an antidepressant prescription varied from 0.74 to 1.57 by indication and therapy status. The odds of not filling an antidepressant prescription was higher among adults filling < 50% of their medication prescriptions in the past year and adults with an antidepressant prescription stopped or changed in the past year due to treatment ineffectiveness.
Conclusion:
Antidepressant prescription filling behaviors differed by treatment indication and were lower among patients with a history of poor prescription filling or ineffective treatment with antidepressants.
Antidepressants are the most frequently prescribed class of psychotropic drugs1–3 used by clinicians to treat not only depression but also a wide range of other indications, including anxiety, insomnia, and pain.4 Despite their popular use, meta-analyses of clinical trials evaluating antidepressant use for depression have not found clear evidence of a meaningful benefit of antidepressants compared with placebo, with many efficacy trials being susceptible to numerous biases.5–7 Antidepressant use for indications besides depression is also controversial due to these other indications oftentimes being not approved (off-label) for many antidepressants and insufficiently evaluated in clinical trials.8
In light of these concerns, pharmacoepidemiologic studies evaluating the real-world effectiveness and safety of antidepressant use for different indications could provide valuable insights into the actual benefits and risks of antidepressant use at the population level. To this end, it is important to understand patterns of antidepressant use in real-world settings, including patients’ prescription filling behaviors and how they relate to clinicians’ intentions for prescribing antidepressants—namely, the indication. Among naive antidepressant users, measuring levels of prescription filling helps estimate the proportion of antidepressant prescriptions leading to the actual initiation of use, which could differ across indications. Among prevalent antidepressant users, levels of prescription filling could also vary across indications due to a variety of factors, including differences in treatment directives, effectiveness, or adverse drug events by indication, the latter of which is more likely when off-label drug use is not backed by strong scientific evidence.9
To date, no studies have measured indication-specific levels of prescription filling for antidepressants using a validated measure of treatment indication. In addition, few studies have measured the impact of patients’ prior prescription filling behaviors and medication experiences on future prescription filling behaviors for antidepressants. To address these knowledge gaps, we used data from a unique electronic prescribing system linked to dispensing data to measure the prevalence of antidepressant prescription filling by indication and evaluate the association of prescription filling with the indication for antidepressant treatment and patients’ prior prescription filling behaviors and experiences with medications, independent of other drug and patient factors. We also evaluated whether the relationship of antidepressant prescription filling with treatment indication differed between naive and non-naive users.
METHODS
Study Design and Setting
This cohort study took place in the Canadian province of Quebec, where the provincial health insurance agency—the Régie de l’Assurance Maladie du Québec (RAMQ)—covers the cost of essential medical services for all residents. By law, all residents must have drug insurance through either a private plan (ie, group or employee benefit plan) or the public drug insurance plan administered by the RAMQ.10 Approximately 50% of Quebec residents are registered in the public drug insurance plan, including the elderly, welfare recipients, and persons not insured through an employer.
Data Source and Study Population
The Medical Office of the XXIst Century (MOXXI) is an indication-based electronic prescribing and drug management system used by consenting primary care physicians in 2 major urban centers in Quebec, Canada.11 Since 2003, ∼200 physicians (25% of eligible) and over 100,000 patients (26% of all who visited a MOXXI physician) have consented to participate in the MOXXI program. In general, MOXXI physicians are younger than nonparticipating physicians, while MOXXI patients are older and have more health problems than nonconsenting patients.12
MOXXI features numerous functionalities for enhancing drug safety and coordination of care for patients.11 The MOXXI prescribing tool requires physicians to document at least 1 treatment indication per prescription by using a drop-down menu containing on-label and off-label indications without distinction or by typing the indication(s) into a free-text field. These physician-documented indications were previously validated and had excellent sensitivity (98.5%) and positive predictive value (97.0%).13 The MOXXI prescribing tool also requires physicians to document the reasons for prescription stops or changes using a drop-down menu listing options related to safety (eg, adverse drug reaction) or effectiveness (eg, ineffective treatment), which have also been validated.14
Administrative health data for MOXXI patients were obtained by linking individuals via their unique health care number to provincial health administrative databases, which provided dispensing data from the public drug insurance plan, as well as information on demographics, diagnoses, hospitalizations, and medical services received. These databases are valid and reliable sources of data for pharmacoepidemiologic and health services research.15,16
This study was approved by the McGill Institutional Review Board.
Inclusion and Exclusion Criteria
The unit of analysis was the antidepressant prescription, which represented a physician’s authorization to dispense medication to a patient for a given regimen and duration (including any subsequent refills over the valid period of the prescription) for either new or modified treatment.17 Prescriptions were included if they were issued between January 1, 2003, and December 31, 2012, for a medication approved to treat depression (Supplement 1, Supplemental Digital Content 1, http://links.lww.com/MLR/C346) and if the patient was at least 18 years old, was enrolled in the public drug insurance plan and had at least 1 year of historical dispensing data available in the public drug insurance database on the prescription date to distinguish new from continued antidepressant users. Prescriptions were excluded if they were for antidepressants not covered under the public drug insurance plan (escitalopram, desvenlafaxine, and duloxetine) or monoamine oxidase inhibitors, which were rarely prescribed (Fig. 1).
FIGURE 1.
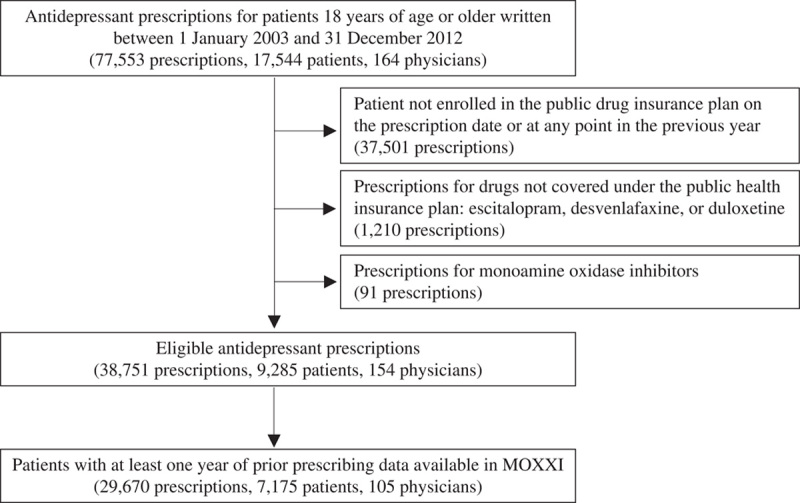
Flow chart of antidepressant prescriptions used in the analysis. Eligible antidepressant prescriptions for the study were used to construct cumulative survival curves, stratified by treatment indication and therapy status, and estimate odds ratios for the association between treatment indication and antidepressant nonadherence at 90 days, adjusted for other drug and patient factors. A subset of eligible antidepressant prescriptions for which the patient had at least 1 year of historical prescribing data available in the MOXXI (Medical Office of the XXIst Century) system was used to estimate the association of antidepressant nonadherence with prior prescription filling behaviors and experience with medications (treatment ineffectiveness and adverse drug reactions in the past year), also adjusted for other drug and patient factors.
Antidepressant Prescription Filling
The study outcome of interest was not filling an antidepressant prescription within 90 days of its issuance, reflecting the concept of nonadherence for indications with a more chronic nature, like depression and anxiety, where not filling an antidepressant prescription may represent a deviation from the planned treatment. Filled prescriptions were tracked using linked dispensing data from the public drug insurance plan, where prescriptions were considered filled if any brand of the prescribed drug was dispensed to the patient within 90 days. As only a negligible proportion (0.1%) of patients both did not fill the index prescription and died or became ineligible for the public drug insurance plan within 90 days, we treated all patients as if they were followed for the complete period.
Potential Determinants of Antidepressant Prescription Filling
Treatment Indication
Treatment indications for antidepressant prescriptions were retrieved from the MOXXI system and classified using the clinical definitions under the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) coding into the following categories: (1) depressive disorders; (2) anxiety-related disorders, including panic disorders, phobias, and stress disorders; (3) insomnia; (4) pain, including chronic pain, neurogenic pain, and dorsalgia; or (5) miscellaneous indications, including migraine, fibromyalgia, vasomotor symptoms of menopause, nicotine dependence, and pruritus, among others. If multiple indications were documented (1.7% of prescriptions), the indication entered first was used.
Therapy Status
Prescriptions were classified as being for new or ongoing antidepressant therapy, where prescriptions for new antidepressant therapy were those where the patient did not have any antidepressants dispensed in the previous year.
Prior Prescription Filling Behaviors and Experience With Medications
As patients’ past prescription filling behaviors could be predictive of future prescription filling behaviors for antidepressants,18 the proportion of prescriptions in the past year that were filled within 90 days was measured and analyzed separately for chronic disease-modifying medications and symptom-relieving medications19 (Supplement 2, Supplemental Digital Content 2, http://links.lww.com/MLR/C347). To assess the potential impact of patients’ prior experiences with medications on future prescription filling behaviors for antidepressants, the presence of any prescriptions in the past year that had been modified due to ineffective treatment or an adverse drug reaction was measured and analyzed separately for antidepressants and non-antidepressant medications. All these variables were measured only for the subset of prescriptions where the patient had been enrolled in MOXXI for at least 1 year at the time of the prescription (Fig. 1).
Other Patient and Drug Factors Possibly Influencing Prescription Filling
Other patient and drug-related factors that could affect prescription filling behaviors for antidepressants were measured and treated as adjusting covariates, including patient age and sex,18,20–25 copayment plan for medications (no copayment, partial copayment of 25% per prescription to a maximum of $600 annually, or maximum copayment of 25% per prescription to a maximum of $1000 annually),25 comorbidities in the Charlson Comorbidity Index,26 and health services use in the past year (number of outpatient visits, number of non-antidepressant drugs dispensed, any emergency department (ED) visit, any hospitalization, and continuity of care measured as the proportion of outpatient visits to the prescribing physician).18,20,24,25 The pharmacological class of the prescribed antidepressant and whether the antidepressant had been prescribed on a “take-as-needed” basis was also measured from the MOXXI system.
Statistical Analysis
Cumulative survival curves showing the percentage of unfilled prescriptions on days 0–90 after the prescription date were constructed, stratified by treatment indication and therapy status. The reported 95% confidence intervals (CIs) around the percentage of unfilled prescriptions at 90 days corresponded to the values at the 2.5th and 97.5th percentiles of the distribution across 1000 bootstrap resamples of the study data using a 2-stage cluster bootstrap27 to account for multilevel clustering of prescriptions within patients, who in turn were nested within physicians.
Multivariable alternating logistic regression was used to estimate the association of treatment indication with failing to fill an antidepressant prescription within 90 days, independent of other patient and drug factors. Alternating logistic regression, implemented using PROC GENMOD in SAS, was used to adjust the main effect estimates for multilevel clustering of prescriptions in the context of a dichotomous outcome.28 To determine if the association of treatment indication was modified by therapy status, a 2-way interaction term was included in the model. The independent association of failing to fill an antidepressant prescription with prior prescription filling behaviors and experience with medications was assessed in a separate multivariable model that included only the subset of patients with at least 1 year of prior prescribing data in MOXXI (Fig. 1).
All statistical analyses were performed using SAS (SAS Institute Inc., Cary, NC) software, version 9.4.
RESULTS
A total of 38,751 antidepressant prescriptions written by 154 physicians for 9284 patients met the study inclusion criteria; 29,670 (76.6%) of these prescriptions had 1 year of historical MOXXI prescribing data available for the patient (Fig. 1). Antidepressant prescriptions were most commonly prescribed for depressive disorders (55.5%), anxiety-related disorders (21.6%), insomnia (11.0%), and pain (6.5%). Depressive disorders accounted for a lower proportion of prescriptions for new (47.0%) compared with ongoing (56.6%) antidepressant therapy.
Treatment Indication and Therapy Status
Prescriptions for new antidepressant therapy were filled faster than those for ongoing antidepressant therapy (Fig. 2), with a median time-to-fill of 2 and 7 days, respectively. By indication, the median time-to-fill for new therapy prescriptions was shortest for insomnia (1 d) and longest for miscellaneous indications (4 d), while for ongoing therapy, was shortest for depression and insomnia (7 d) and longest for pain (9 d). Rates of prescription filling among new and ongoing therapy prescriptions reached a plateau after ∼15 and 30 days, respectively.
FIGURE 2.
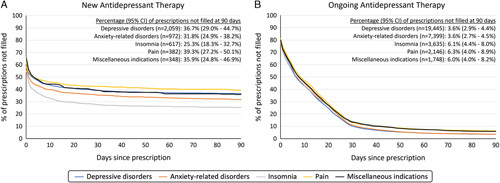
Percentage of antidepressant prescriptions not filled at 0–90 days, by treatment indication and therapy status. The cumulative survival curves show the percentage of antidepressant prescriptions for new (Panel A) or ongoing (Panel B) antidepressant therapy that were not dispensed to the patient over 90 days, stratified by treatment indication. Prescriptions for new antidepressant therapy were defined as those where the patient did not have an antidepressant dispensed in the previous year. Prescriptions for ongoing therapy were defined as those were the patient had an antidepressant dispensed in the previous year and were issued for reasons such as switching to a different antidepressant, modifying the dosage, or renewing the prescription.
Among new antidepressant therapy prescriptions, the proportion of unfilled prescriptions was highest for pain (39.3%) and lowest for insomnia (25.3%) (Fig. 2). Among ongoing antidepressant therapy prescriptions, the proportion of unfilled prescriptions was also highest for pain (6.3%), while depressive disorders and anxiety-related disorders tied for the lowest percentage of unfilled prescriptions at 3.6%.
In the multivariable analysis, the odds of not filling an antidepressant prescription was 28% higher when antidepressants were newly prescribed for anxiety-related disorders [odds ratio (OR),1.28; 95% CI, 1.05–1.57] compared with depressive disorders, but 26% lower when antidepressants were newly prescribed for insomnia (OR, 0.74; 95% CI, 0.56–0.98) (Table 1). Conversely, for ongoing antidepressant therapy, the odds of not filling an antidepressant prescription was 57% higher when antidepressants were prescribed for insomnia (OR, 1.57; 95% CI, 1.24–2.00) and 54% higher when prescribed for miscellaneous indications (OR, 1.54; 95% CI, 1.20–1.97), compared with depressive disorders. For all indications except insomnia, prescriptions for new antidepressant therapy were associated with a statistically significant higher odds of not being filled within 90 days compared with prescriptions for ongoing antidepressant therapy.
TABLE 1.
Association of Treatment Indication With Not Filling an Antidepressant Prescription Within 90 Days, by Antidepressant Therapy Status
| Variables | No. of Prescriptions (N=38,751) | % Unfilled at 90 d | Adjusted OR † (95% CI) for Not Filling the Prescription Within 90 d |
|---|---|---|---|
| Treatment indication, by antidepressant therapy status* | |||
| New therapy | |||
| Depressive disorders | 2059 | 36.7 | 1.00 (reference) |
| Anxiety-related disorders | 972 | 31.8 | 1.28 (1.05–1.57) |
| Insomnia | 617 | 25.3 | 0.74 (0.56–0.98) |
| Pain | 382 | 39.3 | 0.93 (0.62–1.40) |
| Miscellaneous indications | 348 | 35.9 | 1.10 (0.82–1.48) |
| Ongoing therapy | |||
| Depressive disorders | 19,445 | 3.6 | 1.00 (reference) |
| Anxiety-related disorders | 7399 | 3.6 | 1.02 (0.89–1.17) |
| Insomnia | 3635 | 6.1 | 1.57 (1.24–2.00) |
| Pain | 2146 | 6.3 | 1.27 (0.95–1.70) |
| Miscellaneous indications | 1748 | 6.0 | 1.54 (1.20–1.97) |
| Antidepressant therapy status,* by treatment indication | |||
| Depressive disorders | |||
| Ongoing therapy | 19,445 | 3.6 | 1.00 (reference) |
| New therapy | 2059 | 36.7 | 2.53 (1.98–3.24) |
| Anxiety-related disorders | |||
| Ongoing therapy | 7399 | 3.6 | 1.00 (reference) |
| New therapy | 972 | 31.8 | 3.18 (2.53–4.00) |
| Insomnia | |||
| Ongoing therapy | 3635 | 6.1 | 1.00 (reference) |
| New therapy | 617 | 25.3 | 1.19 (0.89–1.59) |
| Pain | |||
| Ongoing therapy | 2146 | 6.3 | 1.00 (reference) |
| New therapy | 382 | 39.3 | 1.85 (1.12–3.05) |
| Miscellaneous indications | |||
| Ongoing therapy | 1748 | 6.0 | 1.00 (reference) |
| New therapy | 348 | 35.9 | 1.82 (1.28–2.58) |
Therapy status was classified as new antidepressant therapy if the patient did not have any antidepressants dispensed from any prescriber in the past year.
From a multivariable model that additionally included all drug and patient factors shown in Table 3.
CI indicates confidence interval; OR, odds ratio.
Prior Prescription Filling Behaviors and Experience With Medications
Poor prescription filling behaviors in the past year were associated with increased odds of not filling an antidepressant prescription (Table 2). Compared with patients who filled ≥75% of their prescriptions for chronic disease-modifying medications in the past year, the odds of not filling a new or continuing antidepressant prescription was over 2.5 times higher among patients who filled < 50% of their chronic disease prescriptions in the past year (OR, 2.57; 95% CI, 1.85–3.57). Patients with no prescriptions for chronic disease-modifying medications in the past year also had a statistically significant higher odds of not filling their antidepressant prescriptions (OR, 1.16; 95% CI, 1.02–1.31). A similar, albeit attenuated association was observed for symptom-relieving medications.
TABLE 2.
Association of Prior Prescription Filling Behaviors and Medication Experiences With Not Filling an Antidepressant Prescription Within 90 Days
| Variables | No. of Prescriptions* (N=29,670) | % Unfilled at 90 d | Adjusted OR † (95% CI) for Not Filling the Prescription Within 90 d |
|---|---|---|---|
| Prescription filling behaviors in the past year | |||
| Chronic disease-modifying medications | |||
| 75%–100% of prescriptions filled | 20,992 | 3.8 | 1.00 (reference) |
| 50% to <75% of prescriptions filled | 690 | 18.6 | 1.40 (0.92–2.11) |
| 0% to <50% of prescriptions filled | 856 | 71.3 | 2.57 (1.85–3.57) |
| No essential medications prescribed | 7132 | 8.5 | 1.16 (1.02–1.31) |
| Symptom-relieving medications | |||
| 75%–100% of prescriptions filled | 13,315 | 3.6 | 1.00 (reference) |
| 50% to <75% of prescriptions filled | 1335 | 7.6 | 1.41 (1.10–1.80) |
| 0% to <50% of prescriptions filled | 1426 | 32.3 | 1.64 (1.34–2.00) |
| No symptom-relieving medications prescribed | 13,594 | 8.1 | 1.09 (0.94–1.26) |
| Experiences with medications in the past year | |||
| Antidepressants | |||
| Prescription stopped or changed due to ineffective treatment | |||
| No | 25,731 | 7.1 | 1.00 (reference) |
| Yes | 3939 | 7.8 | 1.21 (1.02–1.43) |
| Prescription stopped or changed due to an adverse drug reaction | |||
| No | 28,953 | 7.2 | 1.00 (reference) |
| Yes | 717 | 7.1 | 0.81 (0.51–1.30) |
| Other medications besides antidepressants | |||
| Prescription stopped or changed due to ineffective treatment | |||
| No | 23,784 | 7.3 | 1.00 (reference) |
| Yes | 5886 | 6.9 | 1.02 (0.92–1.14) |
| Prescription stopped or changed due to an adverse drug reaction | |||
| No | 27,849 | 7.2 | 1.00 (reference) |
| Yes | 1821 | 7.2 | 0.99 (0.81–1.20) |
Only antidepressant prescriptions where the patient had been enrolled in the MOXXI (Medical Office of the XXIst Century) program for at least 1 year were included in this analysis to ensure that patients had at least 1 year of prior prescribing data available
From a multivariable model that additionally included all variables in Table 1 (treatment indication, therapy status, and a 2-way interaction between treatment indication and therapy status) and all drug and patient factors shown in Table 3.
CI indicates confidence interval; OR, odds ratio.
Patients who had an antidepressant prescription stopped or changed in the past year due to treatment ineffectiveness had 21% higher odds of not filling the index antidepressant prescription (OR, 1.21; 95% CI, 1.02–1.43) (Table 2). However, this association was not observed among patients who had prescriptions for non-antidepressant medications stopped or changed in the past year due to treatment ineffectiveness (OR, 1.02; 95% CI, 0.92–1.14). Adverse drug reactions in the past year to antidepressants and non-antidepressant medications were not associated with not filling antidepressant prescriptions.
Other Drug and Patient Factors
The odds of not filling an antidepressant prescription was lower for serotonin-norepinephrine reuptake inhibitors compared with every other pharmacological class of antidepressants, while the odds of not filling an antidepressant prescription was 49% higher when antidepressants were prescribed on a take-as-needed basis (OR, 1.49; 95% CI, 1.11–2.00) (Table 3). Compared with patients aged 18–50 years old, older patients were increasingly more likely to fill their antidepressant prescriptions. Compared with patients with no medication copayments, the odds of not filling an antidepressant prescription was 2- to 3-fold higher for patients with a partial copay (OR, 2.23; 95% CI, 1.73–2.89) or maximum copay (OR, 2.90; 95% CI, 2.42–3.47). The odds of not filling an antidepressant prescription decreased with greater numbers of non-antidepressant drugs dispensed in the past year but was greater among patients who had visited the ED or had greater numbers of outpatient visits in the past year.
TABLE 3.
Association of Other Drug and Patient Factors With Not Filling an Antidepressant Prescription Within 90 Days
| Variables | No. Prescriptions (N=38,751) | % Unfilled at 90 d | Adjusted OR* (95% CI) for Not Filling the Prescription Within 90 d |
|---|---|---|---|
| Drug factors | |||
| Pharmacological class | |||
| SSRI † | 16,471 | 5.9 | 1.00 (reference) |
| SNRI ‡ | 7690 | 7.1 | 1.24 (1.07–1.42) |
| TCA § | 5095 | 10.5 | 1.77 (1.44–2.17) |
| Other ‖ | 9495 | 9.0 | 1.48 (1.30–1.69) |
| Drug prescribed on a “take-as-needed” basis | |||
| No | 37,967 | 7.3 | 1.00 (reference) |
| Yes | 784 | 17.0 | 1.49 (1.11–2.00) |
| Patient factors | |||
| Sex | |||
| Female | 26,914 | 7.3 | 1.00 (reference) |
| Male | 11,837 | 8.1 | 1.00 (0.88–1.14) |
| Age (y) | |||
| 18–50 | 9476 | 12.3 | 1.00 (reference) |
| 51–62 | 9885 | 6.8 | 0.72 (0.60–0.87) |
| 63–72 | 9425 | 6.5 | 0.62 (0.53–0.74) |
| 73+ | 9965 | 4.7 | 0.50 (0.42–0.61) |
| Copayment plan for medications | |||
| No copayment (free) | 12,139 | 3.5 | 1.00 (reference) |
| Partial copayment (up to 600 CAD/year) | 7323 | 9.0 | 2.23 (1.73–2.89) |
| Maximum copayment (up to 1000 CAD/year) | 19,289 | 11.0 | 2.90 (2.42–3.47) |
| Chronic conditions in the Charlson Comorbidity Index | |||
| Myocardial infarction | |||
| No | 38,124 | 7.6 | 1.00 (reference) |
| Yes | 627 | 4.0 | 0.79 (0.56–1.11) |
| Congestive heart failure | |||
| No | 37,596 | 7.6 | 1.00 (reference) |
| Yes | 1155 | 4.9 | 0.95 (0.67–1.37) |
| Peripheral vascular disease | |||
| No | 37,843 | 7.6 | 1.00 (reference) |
| Yes | 908 | 5.3 | 1.10 (0.70–1.73) |
| Cerebrovascular disease | |||
| No | 37,840 | 7.6 | 1.00 (reference) |
| Yes | 911 | 4.7 | 0.93 (0.71–1.24) |
| Dementia | |||
| No | 37,598 | 7.7 | 1.00 (reference) |
| Yes | 1153 | 3.5 | 0.77 (0.58–1.04) |
| Chronic pulmonary disease | |||
| No | 31,011 | 7.9 | 1.00 (reference) |
| Yes | 7740 | 5.9 | 1.00 (0.89–1.12) |
| Rheumatic disease | |||
| No | 37,950 | 7.6 | 1.00 (reference) |
| Yes | 801 | 3.8 | 0.87 (0.63–1.21) |
| Peptic ulcer disease | |||
| No | 38,278 | 7.5 | 1.00 (reference) |
| Yes | 473 | 7.8 | 1.17 (0.85–1.61) |
| Mild liver disease | |||
| No | 37,989 | 7.6 | 1.00 (reference) |
| Yes | 762 | 6.0 | 1.10 (0.80–1.50) |
| Diabetes without chronic complication | |||
| No | 33,012 | 7.9 | 1.00 (reference) |
| Yes | 5739 | 5.4 | 1.09 (0.94–1.25) |
| Diabetes with chronic complication | |||
| No | 38,498 | 7.5 | 1.00 (reference) |
| Yes | 253 | 6.7 | 1.07 (0.65–1.76) |
| Hemiplegia or paraplegia | |||
| No | 38,521 | 7.5 | 1.00 (reference) |
| Yes | 230 | 9.1 | 1.17 (0.75–1.84) |
| Renal disease | |||
| No | 37,866 | 7.6 | 1.00 (reference) |
| Yes | 885 | 4.3 | 1.03 (0.78–1.35) |
| Any malignancy | |||
| No | 36,145 | 7.6 | 1.00 (reference) |
| Yes | 2606 | 6.0 | 1.04 (0.88–1.24) |
| Moderate or severe liver disease | |||
| No | 38,709 | 7.5 | 1.00 (reference) |
| Yes | 42 | 2.4 | 0.15 (0.03–0.79) |
| Metastatic solid tumor | |||
| No | 37,875 | 7.6 | 1.00 (reference) |
| Yes | 876 | 4.2 | 0.72 (0.48–1.07) |
| AIDS/HIV | |||
| No | 38,588 | 7.5 | 1.00 (reference) |
| Yes | 163 | 9.2 | 0.70 (0.43–1.14) |
| No. outpatient visits in the past year | |||
| 0–3 | 8574 | 9.3 | 1.00 (reference) |
| 4–6 | 8828 | 6.9 | 1.13 (1.01–1.26) |
| 7–11 | 10,414 | 6.7 | 1.20 (1.04–1.37) |
| 12+ | 10,935 | 7.5 | 1.35 (1.15–1.58) |
| Hospitalized in the past year | |||
| No | 32,031 | 7.9 | 1.00 (reference) |
| Yes | 6720 | 5.9 | 0.95 (0.86–1.06) |
| Visited the ED in the past year | |||
| No | 24,506 | 7.9 | 1.00 (reference) |
| Yes | 14,245 | 6.9 | 1.16 (1.07–1.25) |
| Continuity of care with the prescribing physician ¶ | |||
| <0.33 | 9594 | 9.3 | 1.00 (reference) |
| 0.33–0.55 | 9989 | 7.3 | 1.05 (0.96–1.15) |
| 0.56–0.82 | 9458 | 6.8 | 1.09 (0.98–1.22) |
| 0.83+ | 9710 | 6.7 | 1.02 (0.92–1.13) |
| No. non-antidepressant drugs dispensed in the past year | |||
| 0 | 1609 | 56.3 | 1.00 (reference) |
| 1–4 | 7888 | 8.7 | 0.27 (0.23–0.33) |
| 5–9 | 15,425 | 3.8 | 0.20 (0.16–0.24) |
| 10+ | 13,829 | 5.3 | 0.15 (0.12–0.18) |
From a multivariable model that additionally included all variables in Table 1 (treatment indication, therapy status, and a 2-way interaction between treatment indication and therapy status).
Includes citalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline.
Includes venlaxafine.
Includes amitriptyline, clomipramine, desipramine, doxepin, imipramine, nortriptyline, and trimipramine.
Includes trazodone, bupropion, mirtazapine, and maprotiline.
Measured as the proportion of all outpatient visits in the past year that were made to the prescribing physician.
AIDS/HIV indicates acquired immunodeficiency syndrome/human immunodeficiency virus; CAD, Canadian dollars; CI, confidence interval; ED, emergency department; OR, odds ratio; SNRI, serotonin-norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
These trends were largely similar when estimated separately among prescriptions for new and ongoing antidepressant therapy, except for 3 patient factors (visiting the ED, number of outpatient visits, and number of non-antidepressant drugs dispensed in the past year), for which the observed association across all prescriptions was driven by the association among prescriptions for new antidepressant therapy (Supplement 3, Supplemental Digital Content 3, http://links.lww.com/MLR/C348).
DISCUSSION
To our knowledge, this study is the first to measure indication-specific prescription filling patterns for antidepressants using validated, physician-documented indications. The odds of antidepressant prescription filling differed by treatment indication, with the nature of these associations being distinct among naive and non-naive antidepressant users. Failing to fill previous prescriptions, especially for chronic disease-modifying medications, was also independently associated with not filling a future antidepressant prescription, as was having an antidepressant prescription stopped or changed in the past year because of treatment ineffectiveness.
To date, most studies of antidepressant nonadherence and prescription filling behaviors have focused only on patients with depression, with many studies reporting a prevalence of ∼30%–40%29,30 for primary nonadherence, similar to the levels at which new antidepressant prescriptions for depression were not filled in this study. Two previous studies using the Dutch general practice and dispensing databases31,32 attempted to investigate the association between treatment indication and antidepressant prescription filling, but visit-level diagnoses could not be linked directly to antidepressant prescriptions, and no approved indication could be identified for over half of patients filling only a single antidepressant prescription.31 Nonspecific indications such as fatigue, weight loss, and sleeping problems were suspected as likely indications among these patients, who were more likely to present with these conditions. These findings are consistent with our observation that patients with at least 1 previous dispensing of an antidepressant were less likely to fill future antidepressant prescriptions indicated for insomnia or other miscellaneous indications (eg, migraine, hot flashes, chronic fatigue) compared with depression.
Antidepressants prescribed for insomnia had a distinct pattern of prescription filling: naive antidepressant users were more likely to fill new prescriptions for insomnia compared with other indications while continuing antidepressant users were less likely. The findings among naive antidepressant users suggest a heightened sense of eagerness among patients with sleep disorders to acquire medication for their insomnia. This observation is noteworthy given that the most popular antidepressants used for sleep are neither approved nor recommended for insomnia due to the paucity of data supporting their efficacy and safety for this indication.33 Among continuing antidepressant users, several mechanisms could play a role in the lower likelihood of prescription filling observed for insomnia than depression and anxiety. One likely explanation is that patients receiving an updated antidepressant prescription for insomnia (eg, to adjust the dose or simply renew the prescription) may still have some supply on hand at the time of the newer prescription, since antidepressants, when prescribed for insomnia, are often taken on an as-needed basis, unlike for depression and anxiety where antidepressants are taken daily and according to a scheduled regimen. Another possible reason could be a lack of treatment efficacy or poor balance of patient-perceived harms versus benefits among patients taking antidepressants for insomnia—a hypothesis that requires further investigation and highlights the importance of conducting more research on the safety and effectiveness of antidepressant use for insomnia.
This study contributes novel insights into the association of past adverse reactions to and failures with antidepressant treatment on future prescription filling behaviors. Although experiencing or fearing side effects has been identified as a reason for nonadherence in previous studies,34–38 we did not find that prior experience of adverse drug reactions to antidepressants or other medications influenced the odds of not filling an antidepressant prescription. However, having a prior antidepressant prescription stopped or changed because of ineffective treatment increased the odds of not filling a subsequent antidepressant prescription. This effect appeared to be isolated to past experiences with antidepressants only, as similar prior experiences with other medications did not have the same effect on filling future antidepressant prescriptions. While no comparable data exist using physician-documented reasons for therapy changes, one Veterans Administration study of antidepressant use found that patients most commonly reported discontinuing new therapy because it was not effective.38
Our finding that antidepressant prescription filling was strongly associated with poor prescription filling for other medications in the past year, especially chronic disease medications, is concordant with another study39 that found patients with low adherence to chronic preventive medications in the past year were half as likely to adhere to statin therapy as patients with a history of high medication adherence. Similarly, our finding that not filling an antidepressant prescription was strongly associated with the level of cost-sharing for medications has been consistently reported in previous studies.22,25,40
As this study included patients with public drug insurance in primary care settings in Quebec, future studies should determine if the indication-specific patterns of antidepressant prescription filling reported in this study are similarly observed in other patient subgroups and geographic regions. This study also only tracked if the initial prescription issued by a physician for either new or modified antidepressant therapy was filled within 90 days; it did not measure if refills associated with the prescription were subsequently dispensed beyond the initial dispensing. Thus, this study did not measure persistence with antidepressants. Finally, it should also be noted that given the wide variety of indications for which antidepressants are used, failure to fill an antidepressant prescription may, in some cases, represent a suboptimal patient behavior (eg, as one component of medication nonadherence when used for chronic conditions like depression and anxiety), while in other cases, may not be a cause for concern (eg, when used as-needed for symptomatic conditions like insomnia and other miscellaneous indications). Thus, rates of prescription filling for antidepressants should be interpreted in light of the nature of the indication for which the antidepressant was prescribed and the treatment regimen according to which antidepressants are usually used for the indication.
CONCLUSIONS
Using data from a unique, indication-based electronic prescribing system linked to dispensing data, this study is the first to describe levels of prescription filling for antidepressants by treatment indication. Antidepressant prescription filling behaviors were found to differ by treatment indication, with the nature of these associations depending on whether or not the patient had previously used antidepressants. The findings from this study represent an important step toward better understanding patterns of antidepressant use for different indications among adult primary care populations in real-world settings.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
A portion of the results in this manuscript were presented at the 35th International Conference on Pharmacoepidemiology and Therapeutic Risk Management on August 28, 2019, in Philadelphia, PA.
Supported by the Vanier Canada Graduate Scholarship, the Max E. Binz Fellowship (Faculty of Medicine, McGill University), a graduate student fellowship from the Research Institute of the McGill University Health Centre, and the Canadian Institutes of Health Research (IOP-112675).
The authors declare no conflict of interest.
Contributor Information
Jenna Wong, Email: jenna_wong@harvardpilgrim.org.
Siyana Kurteva, Email: siyana.kurteva@mail.mcgill.ca.
Aude Motulsky, Email: aude.motulsky@umontreal.ca.
Robyn Tamblyn, Email: robyn.tamblyn@mcgill.ca.
REFERENCES
- 1. Paulose-Ram R, Safran MA, Jonas BS, et al. Trends in psychotropic medication use among US adults. Pharmacoepidemiol Drug Saf. 2007;16:560–570. [DOI] [PubMed] [Google Scholar]
- 2. Beck CA, Williams JVA, Wang JL, et al. Psychotropic medication use in Canada. Can J Psychiatry. 2005;50:605–613. [DOI] [PubMed] [Google Scholar]
- 3. Ilyas S, Moncrieff J. Trends in prescriptions and costs of drugs for mental disorders in England, 1998-2010. Br J Psychiatry. 2012;200:393–398. [DOI] [PubMed] [Google Scholar]
- 4. Wong J, Motulsky A, Eguale T, et al. Treatment indications for antidepressants prescribed in primary care in Quebec, Canada, 2006-2015. JAMA. 2016;315:2230–2232. [DOI] [PubMed] [Google Scholar]
- 5. Moncrieff J. Against the stream: antidepressants are not antidepressants—an alternative approach to drug action and implications for the use of antidepressants. BJPsych Bull. 2018;42:42–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munkholm K, Paludan-Müller AS, Boesen K. Considering the methodological limitations in the evidence base of antidepressants for depression: a reanalysis of a network meta-analysis. BMJ Open. 2019;9:e024886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pigott HE, Leventhal AM, Alter GS, et al. Efficacy and effectiveness of antidepressants: current status of research. Psychother Psychosom. 2010;79:267–279. [DOI] [PubMed] [Google Scholar]
- 8. Wong J, Motulsky A, Abrahamowicz M, et al. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ. 2017;356:j603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eguale T, Buckeridge DL, Verma A, et al. Association of off-label drug use and adverse drug events in an adult population. JAMA Intern Med. 2015;176:55–63. [DOI] [PubMed] [Google Scholar]
- 10. Pomey M-P, Forest P-G, Palley HA, et al. Public/private partnerships for prescription drug coverage: policy formulation and outcomes in Quebec’s Universal Drug Insurance Program, with comparisons to the Medicare Prescription Drug Program in the United States. Milbank Q. 2007;85:469–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tamblyn R, Huang A, Kawasumi Y, et al. The development and evaluation of an integrated electronic prescribing and drug management system for primary care. J Am Med Inform Assoc. 2006;13:148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bartlett G, Tamblyn R, Kawasumi Y, et al. Non-participation bias in health services research using data from an integrated electronic prescribing project: the role of informed consent. Acta Bioeth. 2005;11:145–159. [Google Scholar]
- 13. Eguale T, Winslade N, Hanley JA, et al. Enhancing pharmacosurveillance with systematic collection of treatment indication in electronic prescribing: a validation study in Canada. Drug Saf. 2010;33:559–567. [DOI] [PubMed] [Google Scholar]
- 14. Eguale T, Tamblyn R, Winslade N, et al. Detection of adverse drug events and other treatment outcomes using an electronic prescribing system. Drug Saf. 2008;31:1005–1016. [DOI] [PubMed] [Google Scholar]
- 15. Monfared AAT, Lelorier J. Accuracy and validity of using medical claims data to identify episodes of hospitalizations in patients with COPD. Pharmacoepidemiol Drug Saf. 2006;15:19–29. [DOI] [PubMed] [Google Scholar]
- 16. Tamblyn R, Lavoie G, Petrella L, et al. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Québec. J Clin Epidemiol. 1995;48:999–1009. [DOI] [PubMed] [Google Scholar]
- 17. Collège des médecins du Québec. Individual prescriptions written by a physicians: 02/2017 practice guidelines; 2017. Available at: www.cmq.org/publications-pdf/p-1-2016-10-03-en-ordonnances-individuelles-faites-par-un-medecin.pdf. Accessed June 17, 2021.
- 18. Shin J, McCombs JS, Sanchez RJ, et al. Primary nonadherence to medications in an integrated healthcare setting. Am J Manag Care. 2012;18:426–434. [PubMed] [Google Scholar]
- 19. Weir DL, Motulsky A, Abrahamowicz M, et al. Challenges at care transitions: failure to follow medication changes made at hospital discharge. Am J Med. 2019;132:1216.e5–1224.e5. [DOI] [PubMed] [Google Scholar]
- 20. Rossom RC, Shortreed S, Coleman KJ, et al. Antidepressant adherence across diverse populations and healthcare settings. Depress Anxiety. 2016;33:765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akincigil A, Bowblis JR, Levin C, et al. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care. 2007;45:363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14:553–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bambauer KZ, Soumerai SB, Adams AS, et al. Provider and patient characteristics associated with antidepressant nonadherence: the impact of provider specialty. J Clin Psychiatry. 2007;68:867–873. [DOI] [PubMed] [Google Scholar]
- 24. Zeber JE, Manias E, Williams AF, et al. A systematic literature review of psychosocial and behavioral factors associated with initial medication adherence: a report of the ISPOR Medication Adherence & Persistence Special Interest Group. Value Health. 2013;16:891–900. [DOI] [PubMed] [Google Scholar]
- 25. Tamblyn R, Eguale T, Huang A, et al. The incidence and determinants of primary nonadherence with prescribed medication in primary care: a cohort study. Ann Intern Med. 2014;160:441–450. [DOI] [PubMed] [Google Scholar]
- 26. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 27. Xiao Y, Abrahamowicz M. Bootstrap-based methods for estimating standard errors in Cox’s regression analyses of clustered event times. Stat Med. 2010;29:915–923. [DOI] [PubMed] [Google Scholar]
- 28. Carey V, Zeger SL, Diggle P. Modelling multivariate binary data with alternating logistic regressions. Biometrika. 1993;80:517–526. [Google Scholar]
- 29. Simon GE, Coleman KJ, Waitzfelder BE, et al. Adjusting antidepressant quality measures for race and ethnicity. JAMA Psychiatry. 2015;72:1055–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kales HC, Kavanagh J, Chiang C, et al. Predictors of antidepressant nonadherence among older veterans with depression. Psychiatr Serv. 2016;67:728–734. [DOI] [PubMed] [Google Scholar]
- 31. van Geffen EC, Gardarsdottir H, van Hulten R, et al. Initiation of antidepressant therapy: do patients follow the GP’s prescription? Br J Gen Pract. 2009;59:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Dijk L, Heerdink ER, Somai D, et al. Patient risk profiles and practice variation in nonadherence to antidepressants, antihypertensives and oral hypoglycemics. BMC Health Serv Res. 2007;7:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sateia MJ, Buysse DJ, Krystal AD, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13:307–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lin EHB, Von Korff M, Katon W, et al. The role of the primary care physician in patients’ adherence to antidepressant therapy. Med Care. 1995;33:67–74. [DOI] [PubMed] [Google Scholar]
- 35. Burra TA, Chen E, McIntyre RS, et al. Predictors of self-reported antidepressant adherence. Behav Med. 2007;32:127–134. [DOI] [PubMed] [Google Scholar]
- 36. Woodward SC, Bereznicki BJ, Westbury JL, et al. The effect of knowledge and expectations on adherence to and persistence with antidepressants. Patient Prefer Adherence. 2016;10:761–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Milan R, Vasiliadis H-M. The association between side effects and adherence to antidepressants among primary care community-dwelling older adults. Aging Ment Health. 2019;24:1229–1236. [DOI] [PubMed] [Google Scholar]
- 38. Fortney JC, Pyne JM, Edlund MJ, et al. Reasons for antidepressant nonadherence among veterans treated in primary care clinics. J Clin Psychiatry. 2011;72:827–834. [DOI] [PubMed] [Google Scholar]
- 39. Kumamaru H, Lee MP, Choudhry NK, et al. Using previous medication adherence to predict future adherence. J Manag Care Spec Pharm. 2018;24:1146–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gibson TB, Jing Y, Kim E, et al. Cost-sharing effects on adherence and persistence for second-generation antipsychotics in commercially insured patients. Manag Care. 2010;19:40–47. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


