Supplemental Digital Content is available in the text.
Keywords: clonal hematopoiesis, coronary artery disease, extracellular traps, phospholipids, thrombosis
Abstract
Background:
LNK/SH2B3 inhibits Janus kinase/signal transducer and activator of transcription (JAK/STAT) signaling by hematopoietic cytokine receptors. Genome-wide association studies have shown association of a common single nucleotide polymorphism in LNK (R262W, T allele) with neutrophilia, thrombocytosis, and coronary artery disease. We have shown that LNK(TT) reduces LNK function and that LNK-deficient mice display prominent platelet–neutrophil aggregates, accelerated atherosclerosis, and thrombosis. Platelet–neutrophil interactions can promote neutrophil extracellular trap (NET) formation. The goals of this study were to assess the role of NETs in atherosclerosis and thrombosis in mice with hematopoietic Lnk deficiency.
Methods:
We bred mice with combined deficiency of Lnk and the NETosis-essential enzyme PAD4 (peptidyl arginine deiminase 4) and transplanted their bone marrow into Ldlr–/– mice. We evaluated the role of LNK in atherothrombosis in humans and mice bearing a gain of function variant in JAK2 (JAK2V617F).
Results:
Lnk-deficient mice displayed accelerated carotid artery thrombosis with prominent NETosis that was completely reversed by PAD4 deficiency. Thrombin-activated Lnk–/– platelets promoted increased NETosis when incubated with Lnk–/– neutrophils compared with wild-type platelets or wild-type neutrophils. This involved increased surface exposure and release of oxidized phospholipids (OxPL) from Lnk–/– platelets, as well as increased priming and response of Lnk–/– neutrophils to OxPL. To counteract the effects of OxPL, we introduced a transgene expressing the single-chain variable fragment of E06 (E06-scFv). E06-scFv reversed accelerated NETosis, atherosclerosis, and thrombosis in Lnk–/– mice. We also showed increased NETosis when human induced pluripotent stem cell–derived LNK(TT) neutrophils were incubated with LNK(TT) platelet/megakaryocytes, but not in isogenic LNK(CC) controls, confirming human relevance. Using data from the UK Biobank, we found that individuals with the JAK2VF mutation only showed increased risk of coronary artery disease when also carrying the LNK R262W allele. Mice with hematopoietic Lnk+/– and Jak2VF clonal hematopoiesis showed accelerated arterial thrombosis but not atherosclerosis compared with Jak2VFLnk+/+ controls.
Conclusions:
Hematopoietic Lnk deficiency promotes NETosis and arterial thrombosis in an OxPL-dependent fashion. LNK(R262W) reduces LNK function in human platelets and neutrophils, promoting NETosis, and increases coronary artery disease risk in humans carrying Jak2VF mutations. Therapies targeting OxPL may be beneficial for coronary artery disease in genetically defined human populations.
Clinical Perspective.
What Is New?
A common genetic variant in LNK (R262W) reduces its function, increases JAK/STAT (Janus kinase/signal transducer and activator of transcription) signaling, and associates with coronary artery disease.
Human induced pluripotent stem cell–derived platelets and neutrophils carrying LNK(R262W) produce increased neutrophil extracellular traps (NETs) and hyperlipidemic LNK-deficient mice display increased NETs and arterial thrombosis that are reversed by oxidized phospholipid (OxPL) antibodies.
LNK(R262W) increases coronary artery disease risk in humans carrying a gain of function in JAK/STAT signaling (JAK2VF), paralleling increased NETosis and arterial thrombosis in LNK-deficient mice and suggesting that targeting NETosis and OxPLs in patients carrying the common LNK loss of function variant could reduce atherothrombotic risk.
What Are the Clinical Implications?
Hypercholesterolemic mice with hematopoietic Lnk deficiency display accelerated arterial thrombosis with increased NETs in thrombi; these changes are reversed by PAD4 (peptidyl arginine deiminase) deficiency or OxPL antibodies.
LNK-deficient platelets from hyperlipidemic mice expose and release increased OxPL when activated, promoting NETosis when incubated with Lnk-deficient neutrophils.
An anti-OxPL antibody reduces plasma OxPL levels, NETosis, and arterial thrombosis specifically in LNK-deficient mice.
Targeting atherothrombotic risk using OxPL antibodies may be particularly effective in genetically defined populations with reduced LNK function or increased JAK/STAT signaling.
A common genetic variant in LNK rs3184504 (T allele, R262W) is associated with increased platelet and neutrophil counts, coronary artery disease (CAD), thrombotic stroke,1,2 and autoimmune diseases.3,4 LNK (also called SH2B3), a member of the SH2B family of adaptor proteins, is primarily expressed in hematopoietic and endothelial cells.5 In hematopoietic cells, LNK functions as a negative regulator of cytokine signaling and cell proliferation.5,6 Targeted deletion of LNK in mice causes expansion of hematopoietic stem cells (HSCs), increased myelopoiesis, thrombocytosis, and leukocytosis, attributable to lack of negative feedback regulation of thrombopoietin receptor signaling through the Janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway.5,7 Similarly, in human cord blood HSCs, LNK(R262W) causes reduced LNK function and increased thrombopoietin signaling.7 Both the common T risk single nucleotide polymorphism and much rarer complete loss of function variants of LNK are associated with myeloproliferation2,8 and similar phenotypes occur in LNK-deficient mouse models.5,7 Thus, LNK-deficient mice are a relevant model to assess mechanisms of atherosclerosis and thrombosis associated with LNK deficiency.
We showed that hematopoietic LNK deficiency synergizes with hyperlipidemia to promote platelet production and activation, neutrophilia, platelet–neutrophil aggregates, atherosclerosis, and arterial thrombosis.7 Platelet activation and platelet–neutrophil interactions have been shown to promote neutrophil extracellular trap (NET) formation.9 NETs are formed when neutrophils release their contents, leading to the formation of web-like structures made of DNA, myeloperoxidase, citrullinated histones (H3Cit), and proteases that entrap and kill bacteria.10 NETs may help suppress infections, but the formation of NETs (NETosis) in blood vessels can promote atherosclerosis and thrombosis.11,12 NETs are found on the surface of and within atherosclerotic lesions13,14 and within arterial thrombi15 in humans and mice.12,16 NETs may serve as biomarkers predicting the risk of thrombosis.12 Moreover, chemical inhibition or genetic deletion of PAD4 (peptidyl arginine deiminase 4), an enzyme critical for NETosis, decreased lesion size and delayed arterial thrombosis in ApoE–/– mice.17,18 These studies suggest that NETs may promote formation of unstable atherosclerotic plaques and atherothrombosis.
This study was undertaken to investigate the hypothesis that Lnk deficiency might promote NETosis, leading to formation of unstable atherosclerotic plaques and arterial thrombosis. We also determined whether LNK(R262W) might modify the increased CAD risk associated with JAK2V617F (JAK2VF), a gain of function variant associated with rare myeloproliferative neoplasms19 and more commonly with clonal hematopoiesis of indeterminate potential (CHIP),20 as LNK acts as a negative regulator of both JAK2 and JAK2VF-mediated signaling and myeloproliferation.5,6
Methods
On reasonable request to the corresponding author, the data, analytic methods, and study materials will be made available to other researchers. All supporting data are available within the article and the Expanded Methods in the Supplemental Material. Institutional review board approval was obtained for this study where applicable.
Animals
Wild-type (WT; C57BL/6J), Ldlr–/– (B6.129S7-Ldlrtm1Her), and Pad4–/– (B6.Cg-Padi4tm1.1Kmow/J) mice were purchased from Jackson Laboratory. Ldlr−/− E06-scFv mice (on C57BL/6J background) were shared by the Witztum Laboratory at the University of California, San Diego.21,22
Statistics
Statistical analysis included mean±SEM, Student t test, and 2-way analysis of variance. Results were considered significant at P<0.05. Statistical analyses were conducted using Prism (GraphPad).
Results
Effect of NETs on Thrombosis and Atherosclerosis in LNK-Deficient Mice
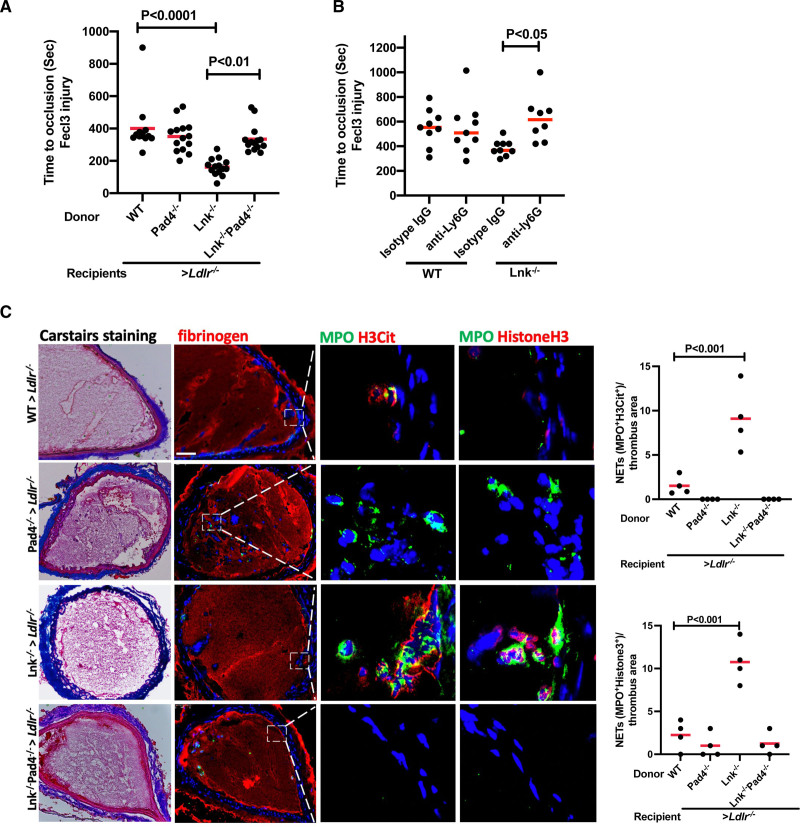
PAD4 has an essential role in chromatin decondensation and NETosis. Deficiency of PAD4 impairs venous and arterial thrombosis in mice.11,23,24 To study the role of NETosis in thrombosis, Ldlr–/– mice were transplanted with WT, Lnk–/–, Pad4–/–, and Lnk–/–Pad4–/– bone marrow and fed Western-type diet (WTD) for 10 weeks. As reported,7 hypercholesterolemic Ldlr–/– mice receiving Lnk–/– bone marrow displayed monocytosis, neutrophilia, and thrombocytosis, in a PAD4-independent fashion (Figure S1). Compared with controls, carotid artery thrombosis was substantially accelerated in the hypercholesterolemic Lnk–/– bone marrow recipients, as reported.7 Hematopoietic PAD4 deficiency reversed the accelerated thrombosis in Lnk–/– bone marrow recipients but had no impact in Lnk+/+ recipients (Figure 1A). Because PAD4 is expressed by other leukocytes than neutrophils,25 we assessed the specific role of neutrophils by depleting them with Ly6G antibody (Figure 1B). Similar to PAD4 deficiency, depletion of neutrophils had no effect in WT mice but significantly prolonged occlusion time in Lnk–/– mice (Figure 1B), suggesting that neutrophil PAD4 promoted NETosis in Lnk deficiency. As reported,26 NETs shown by coincident staining for H3Cit and MPO or Ly6G were seen mainly on the surface of thrombi that were outlined using Carstairs stain. NETs were increased 7-fold in thrombi of Lnk–/– mice with almost complete reversal by PAD4 deficiency (Figure 1C and Figure S2). Similar results were obtained when histone H3 staining was used to assess NETs (Figure 1C and Figure S2). DNase 1, which can effectively degrade DNA in NETs, has been used to dissolve NETs in vivo.18,27 Treatment with DNase 1 ameliorated thrombosis in WTD fed Lnk–/– mice (Figure S2). Together these data indicate that NETosis promotes arterial thrombosis in a PAD4-dependent fashion in hypercholesterolemic mice with hematopoietic LNK deficiency.
Figure 1.
Increased neutrophil extracellular traps and arterial thrombosis in Lnk–/– mice are reversed by PAD4 deficiency. A, FeCl3-induced carotid artery occlusion in wild-type (WT), Lnk–/–, Pad4–/–, and Lnk–/– Pad4–/– bone marrow female Ldlr–/– recipient mice fed Western-type diet for 10 weeks; 2-way analysis of variance. B, Time to occlusion measured in WT and Lnk–/– bone marrow recipient mice after 48 hours of treatment with 100 µg anti-Ly6G or isotype control antibody; 2-way analysis of variance. C, Representative images of Carstairs, fibrinogen (red), or neutrophil extracellular trap (NET) staining in carotid artery thrombi of WT, Lnk–/–, Pad4–/–, and Lnk–/–Pad4–/– bone marrow female Ldlr–/– recipients fed Western-type diet for 10 weeks. NETs were validated using MPO (green) with citrullinated histone (H3Cit; red) or MPO (green) with histone 3 (red). NETs shown were from the same area as in fibrinogen staining on consecutive sections. Quantification of NETs (n=4 per group); 2-way analysis of variance. Each point represents 1 mouse. Scale bar, 50 µm. Data are expressed as mean (red bar) ±SEM. IgG indicates immunoglobulin G.
To assess the role of NETs in atherogenesis, proximal aortic lesions were stained for neutrophils and NETs (Figure S3). This showed prominent NET formation in lesions of mice with hematopoietic LNK deficiency compared with controls, with reversal by PAD4 deficiency (Figure S3). We also found increased staining for interleukin–1β (IL-1β), an inflammatory marker, especially in regions containing NETs in LNK-deficient mice, which was reversed by PAD4 deficiency (Figure S4). However, although there was a trend for PAD4 deficiency to reduce lesion and necrotic core area in LNK-deficient mice, these changes were not significant (Figure S3).
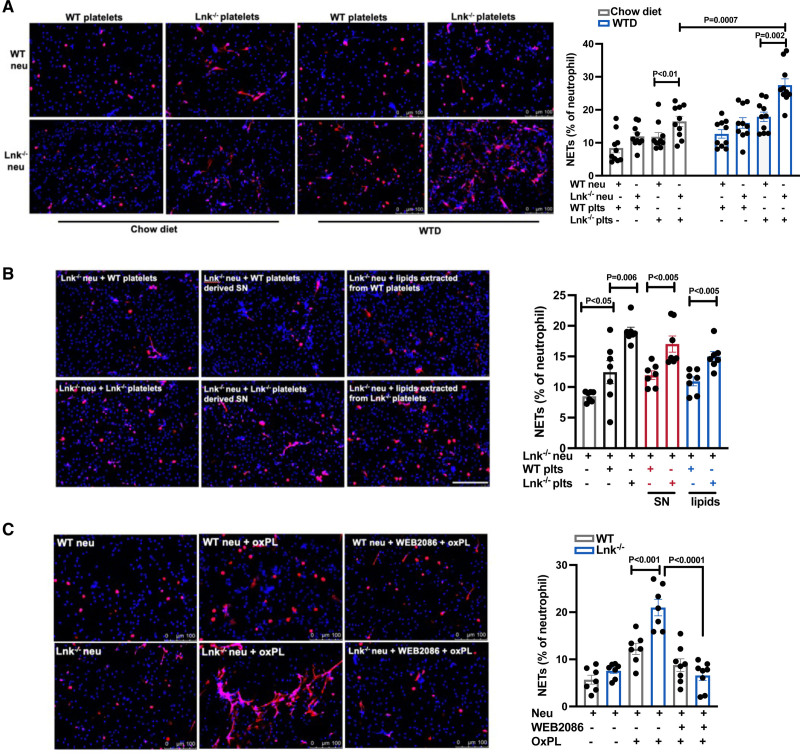
Platelet-Released Platelet-Activating Factor–Like Oxidized Phospholipid Induces NETosis in Lnk–/– Neutrophils
Previous studies have shown a major role of activated platelets in promoting NETosis.9,28 To explore the underlying mechanisms of accelerated NETosis, we incubated WT or Lnk–/– neutrophils with thrombin-activated WT or Lnk–/– platelets and stained for NETs using H3Cit. We found that NETs were only significantly increased when Lnk–/– platelets were incubated with Lnk–/– neutrophils, indicating a role for both Lnk–/– platelets and Lnk–/– neutrophils in increased NETosis (Figure 2A). The increase in NETosis was significantly greater in samples from hyperlipidemic mice, consistent with augmented Lnk–/– platelet activation and thrombosis in the setting of hyperlipidemia.7 To investigate whether soluble factors released from activated platelets promote NETosis, we prepared supernatants from activated platelets and showed similar activity of intact Lnk–/– platelets or their supernatant, whereas supernatants of WT platelets promoted less NETosis (Figure 2B). To assess a potential role of the lipids released by platelets, we prepared a sonicated lipid extract and incubated it with Lnk–/– neutrophils. The lipids extracted from Lnk–/– platelets induced a significantly higher level of NETosis than those from Lnk+/+ platelets (Figure 2B). Oxidized phospholipids (OxPLs) have been implicated in platelet activation in hyperlipidemic mice.29 OxPLs are released by activated platelets30 and a recent report showed that OxPLs promote NETosis in vitro.31 This suggests that soluble OxPLs released from Lnk–/– platelets might be inducing NETosis in Lnk–/– neutrophils. We found that oxPAPCs markedly induced NETosis especially when added to Lnk–/– versus WT neutrophils (Figure 2C). oxPAPCs demonstrate platelet-activating factor (PAF)–like agonistic activity through the PAF receptor (PAFR), which is inhibited by the specific PAFR antagonist WEB2086.32 OxPAPCs consistently induced NETosis in Lnk–/– but not WT neutrophils and this OxPAPC induced NETosis was inhibited by WEB2086 (Figure 2C). PAF stimulation resulted in significantly increased NETosis in Lnk–/– but not WT neutrophils compared with controls (Figure S5), similar to the effects of oxPAPC. When Lnk–/– platelets were incubated with Lnk–/– neutrophils, the increased NETosis was reversed by WEB2086 (Figure S5). Thus, PAF-like lipids, most likely OxPLs, released by Lnk–/– platelets promote NETosis by activation of the PAFR in Lnk–/– neutrophils.
Figure 2.
Platelet-released platelet-activating factor–like oxidized phospholipid induces neutrophil extracellular traps in Lnk–/– neutrophils through platelet-activating factor receptor. A, Platelets activated with 1 nmol/L thrombin were incubated with neutrophils at a ratio=20:1 for 4 hours. Representative images of NETosis. Red, Citrullinated histone (H3Cit); blue, DAPI. Neutrophil extracellular trap (NET) numbers were normalized to total neutrophil number; 2-way analysis of variance. Scale bar,100 µm. B, Lnk–/– neutrophils were stimulated with wild-type (WT) or Lnk–/– platelets, platelet-derived supernatant, or platelet supernatant–derived lipids for 4 hours. Red, H3Cit; blue, DAPI; n=7. C, Neutrophils were preincubated with WEB2086 (4 µmol/L) for 30 minutes followed by 3 hours oxidized phospholipid (OxPL; 20 µg/mL) treatment and then stained with H3Cit and DAPI (n=7). Quantification of NETs; 2-way analysis of variance. Scale bar, 100 µm. Data are expressed as mean±SEM. SN indicates supernatant; and WTD, Western-type diet.
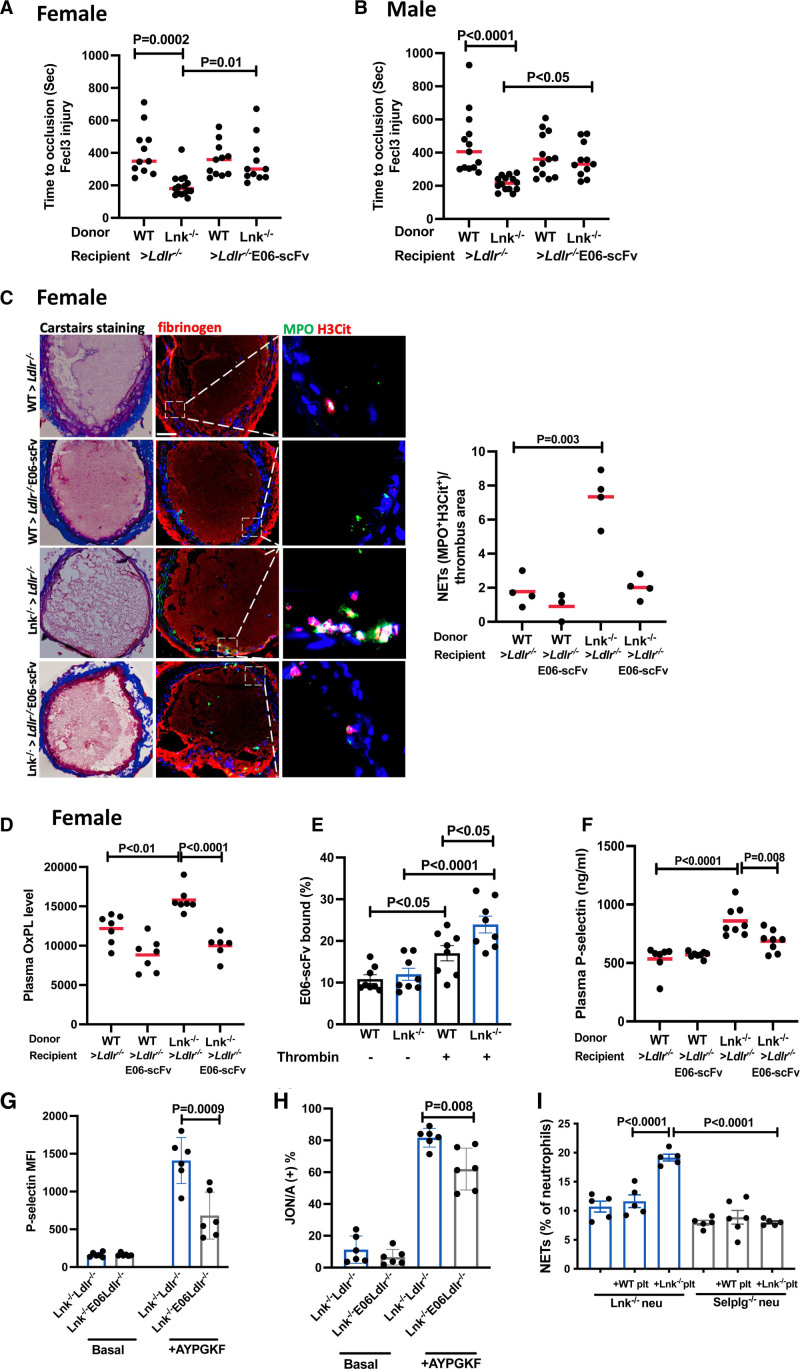
E06-scFv Ameliorates Thrombosis and Atherosclerosis in LNK-Deficient Mice
A recent study using E06-scFv transgenic mice that express OxPL-neutralizing antibodies demonstrated a major role of OxPLs in promoting atherogenesis.21 To assess the role of OxPLs in thrombosis and atherosclerosis, we bred E06-scFv transgenic Ldlr–/– mice. Bone marrow cells from WT and Lnk–/– mice were transplanted into male and female Ldlr–/– and Ldlr–/– E06-scFv mice followed by 10 weeks of WTD feeding. After 6 weeks of WTD, there were high levels of E06-scFv in Ldlr–/– E06-scFv recipient mice, especially in males (Figure S6). Body weight, spleen weight, and blood cell counts were not affected by the E06-scFv transgene in either sex (Figures S6 and S7).
Accelerated thrombosis in LNK-deficient female mice was almost completely reversed by the E06-scFv transgene, whereas E06-scFv had no effect in the WT controls (Figure 3A), paralleling the selective reversal of accelerated thrombosis in LNK deficiency by PAD4 deficiency or neutrophil depletion. Similar results were obtained in male mice (Figure 3B). In parallel, increased NETosis in the thrombi of Lnk–/– mice was reversed by E06-scFv (Figure 3C and Figures S8 and S9). E06 does not bind to PAF or lysoPAF.33 Plasma OxPL levels were significantly elevated in both male and female hypercholesterolemic LNK-deficient mice compared with controls and this was reversed by E06-scFv (Figure 3D and Figure S10). Flow cytometry showed increased binding of E06-scFv to platelets after thrombin activation that was significantly greater in Lnk–/– versus WT platelets (Figure 3E). This suggests that OxPL exposure was increased on activated platelets and that Lnk–/– platelets, which show increased platelet activation,7 had higher levels of OxPL exposure. Plasma P-selectin was also significantly elevated in hypercholesterolemic LNK deficiency with reversal by E06-scFv (Figure 3F). We also assessed traditional markers of platelet activation. Surface P-selectin and activated integrin αIIbβ3 levels were increased in Lnk–/– platelets after PAR4 agonist treatment, as reported,7 and these increases were significantly reduced in E06-scFv mice (Figure 3G and 3H). Platelet P-selectin enhances NETosis in neutrophils through its receptor Selplg.9 Incubation of Lnk–/– platelets with Selplg–/– neutrophils reduced the increased NETosis caused by Lnk deficiency, suggesting that in addition to the effects of OxPL, there is an important role of reduced P-selectin exposure in the effects of E06-scFv (Figure 3I). Because inflammasome activation can promote NETosis,34 we also considered a role of the inflammasome in accelerated thrombosis. However, hypercholesterolemic LNK-deficient mice did not have elevated plasma levels of the inflammasome products IL-1β or IL-18. Moreover, in vivo Caspase 1/11 deficiency did not alter occlusion time in LNK-deficient mice (Figure S11).
Figure 3.
E06-scFv reverses increased neutrophil extracellular traps and accelerated thrombosis in Lnk–/– mice. FeCl3-induced carotid artery occlusion in Western-type diet–fed (10 weeks) female (A) or male (B) recipients of designated genotype as indicated; 2-way analysis of variance. C, Representative images of Carstairs, fibrinogen, or neutrophil extracellular trap (NET) staining in carotid artery thrombi of the female recipients as in A. NETs were validated using MPO (green) with citrullinated histone (H3Cit; red). NETs shown were from the same area as in fibrinogen staining on consecutive sections. Quantification of NETs in carotid artery thrombi of the female recipients (n=4 per group); 2-way analysis of variance. Scale bar, 50 µm. Each point represents 1 mouse. D, Plasma oxidized phospholipid (OxPL) level was assessed in the female recipients as in A (n=6–7). E, E06-scFv binding to the basal or activated platelets (n=8). F, Plasma P-selectin level was assessed by enzyme-linked immunosorbent assay in the female recipients as in A (n=8). Surface P-selectin (G) and active integrin αIIbβ3 (JON/A; H) levels on platelets with and without AYPGKF (50 µmol/L) stimulation (n=6); 2-way analysis of variance. I, Quantification of NETs from wild-type (WT) or Selplg–/– neutrophils stimulated by activated WT or Lnk–/– platelets (n=5); 2-way analysis of variance. Data are expressed as mean (red bar) ±SEM.
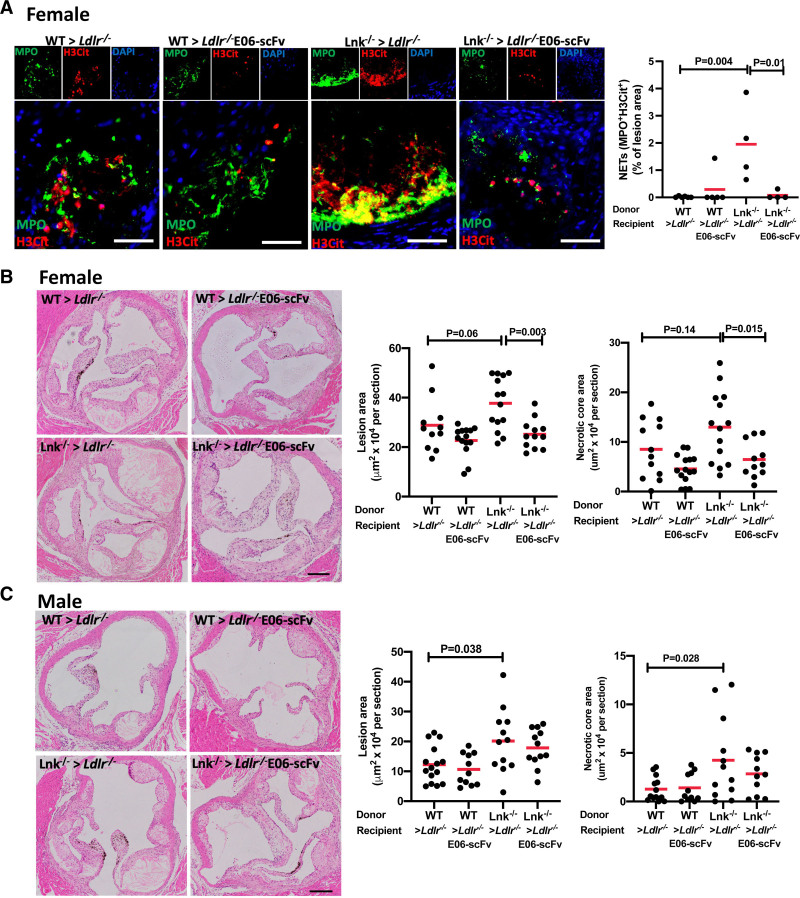
We also found that the prominent NETosis in atherosclerotic lesions of LNK-deficient mice was reversed by E06-scFv (Figure 4A and Figures S12 and S13). Lesion area and necrotic core area were increased in LNK-deficient mice of both sexes; E06-scFv reversed these effects in females and suppressed them in males (Figure 4B and 4C). Whereas E06-scFv did not significantly reduce lesion area in controls, previous studies showed reduced lesion area in Ldlr–/– E06-scFv compared with Ldlr–/– mice fed with 1% high-cholesterol diet for 4, 7, or 12 months,21 compared with only 10 weeks in the current study. The effect of E06-scFv was less pronounced in male than in female mice, which had more than 2-fold larger lesions (Figure 4B and 4C). Together, these findings suggest that E06-scFv is more effective at later stages of lesion development. Given that PAD4 deficiency did not affect lesion development (Figure S3), the more prominent effect of E06-scFv in ameliorating lesions of Lnk–/– versus control Ldlr–/– mice is unlikely to be solely attributable to reversal of NETosis, but rather could reflect the fact that the LNK-deficient mice had more advanced lesions.
Figure 4.
E06-scFv reverses increased neutrophil extracellular traps and atherosclerosis in Lnk–/– mice. A, Representative images showing staining for MPO (green) and citrullinated histone (H3Cit; red) with DAPI (blue) in aortic root lesions of wild-type (WT) or Lnk–/– bone marrow female Ldlr–/– or Ldlr–/– E06-scFv recipients fed with Western-type diet for 10 weeks. The graph quantitates neutrophil extracellular traps (NETs; MPO+H3Cit+) in lesions; 2-way analysis of variance. Scale bar, 50 µm. B and C, Representative hematoxylin & eosin–stained aortic root lesions and quantification of lesion area and necrotic core area in female (B) and male (C) Ldlr–/– and Ldlr–/– E06-scFv recipients after 10 weeks of Western-type diet (n=15–20); 2-way analysis of variance. Scale bar, 500 µm. Data are expressed as mean (red bar) ±SEM.
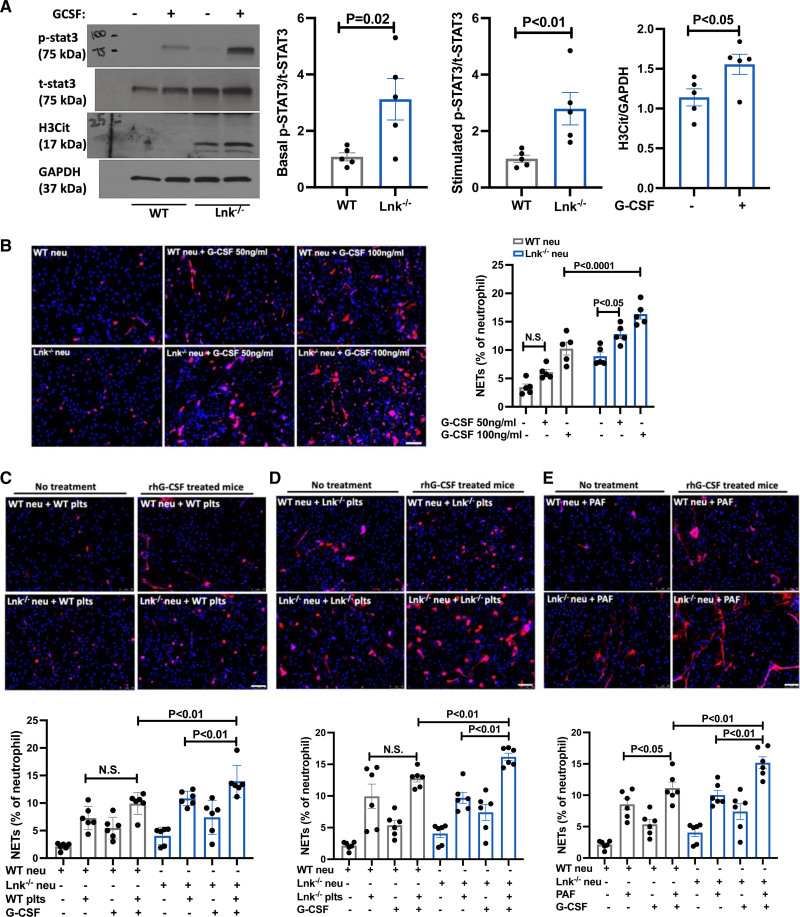
Granulocyte Colony-Stimulating Factor Promotes NETosis in LNK-Deficient Mice
Our in vitro incubations suggest a NETosis-promoting role of LNK deficiency in neutrophils as well as in platelets (Figure 2). Granulocyte colony-stimulating factor (G-CSF) signaling through STAT3/5 is known to be inhibited by LNK35 and G-CSF treatment primes neutrophils for NET release.36 To assess G-CSF signaling in LNK deficiency, we treated WT and Lnk–/– mice with recombinant human G-CSF and isolated neutrophils. Compared with WT, p-STAT3 expression was significantly increased in Lnk–/– neutrophils even under basal conditions and was increased further after G-CSF administration. H3Cit levels were also elevated in Lnk–/– neutrophils after G-CSF treatment (Figure 5A). To assess G-CSF induced NETosis further, we treated WT and Lnk–/– neutrophils with G-CSF in vitro. G-CSF stimulation resulted in a dose-dependent increase in NETosis in both WT and Lnk–/– neutrophils, but the effect was more pronounced in Lnk–/– neutrophils (Figure 5B). We next assessed whether G-CSF treatment in vivo would prime neutrophils for NETosis induced by other stimulants ex vivo. This showed increased NETosis in response to PAF treatment in Lnk–/– neutrophils compared with WT neutrophils (Figure 5C–5E), suggesting that increased G-CSF–mediated priming may be responsible for the increased NETosis observed in Lnk–/– neutrophils.
Figure 5.
Granulocyte colony-stimulating factor promotes NETosis in LNK-deficient mice. A, Wild-type (WT) or Lnk–/– mice were intraperitoneally injected with vehicle or 2.5 μg recombinant human (rh) granulocyte colony-stimulating factor (G-CSF) for 15 minutes. p-STAT3 and citrullinated histone (H3Cit) levels in neutrophils isolated from WT or Lnk–/– mice were determined and quantified by Western analysis (n=5). Unpaired t test. B, WT or Lnk–/– neutrophils were stimulated with G-CSF for 3 hours. The cells were then stained with H3Cit (red) and DAPI and neutrophil extracellular traps (NETs) were quantified (n=5). C through E, WT or Lnk–/– mice were treated with IP injection of vehicle or rhG-CSF (2.5 μg) for 3 days; neutrophils from vehicle or rhG-CSF–treated WT or Lnk–/– mice were isolated and stimulated with WT platelets (C), Lnk–/– platelets (D), or platelet-activating factor (E) for 4 hours. NETs were quantified (n=6); 2-way analysis of variance. Scale bar, 50 µm. Data are expressed as mean±SEM.
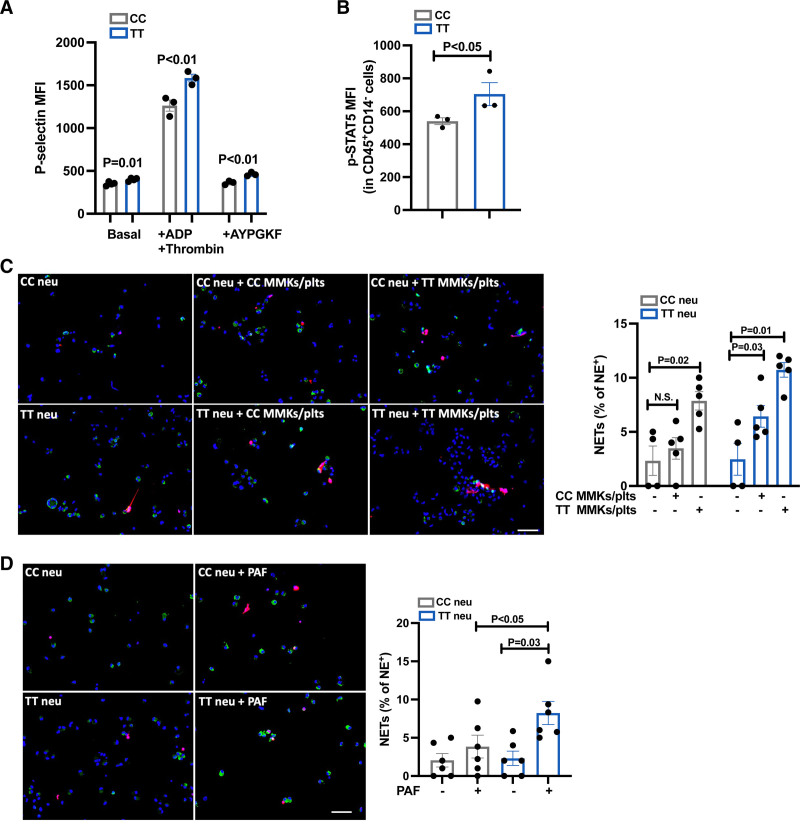
Increased NETosis in Human Induced Pluripotent Stem Cell–Derived LNK(TT) Platelet/Megakaryocytes and Neutrophils
To test the human relevance of these findings, we generated isogenic LNK(TT) and isogenic LNK(CC) induced pluripotent stem cells (iPSCs) through CRISPR/Cas9-mediated gene editing (Figure S14). To select an LNK homozygous parental iPSC line, we first genotyped a panel of 17 previously generated genetically diverse normal lines.37 Three lines were LNK(TT), 8 were LNK(CC), and 3 were heterozygous LNK(CT). We selected a LNK(TT) iPSC line (N-2.12)38 and used CRISPR/Cas9-mediated homology–directed repair to edit the LNK locus to derive an isogenic LNK(CC) line. Using a differentiation protocol that produces definitive-type hematopoietic progenitor cells followed by protocols to generate megakaryocyte/platelets or neutrophils, we generated mature megakaryocyte (MMK)/platelets and neutrophils from the isogenic iPSC pair.39,40 By day 15 of differentiation, >70% of the cell population were CD41a+CD42b+ MMKs generated from megakaryocyte progenitor cells and large megakaryocytes and proplatelet morphology was observed (Figure S15). LNK(TT) MMK/platelet mixtures showed increased surface P-selectin level under basal and stimulated conditions compared with LNK(CC) control cells (Figure 6A). p-STAT5 was also significantly increased in LNK(TT) neutrophils (CD45+CD14– gated) cultured in G-CSF–containing medium (Figure 6B), corroborating our finding of increased G-CSF signaling through STAT3/5 in Lnk-deficient neutrophils. To assess NETosis induced by MMK/platelets in human iPSC-derived neutrophils, we incubated LNK(TT) and LNK(CC) neutrophils with thrombin-activated MMK/platelets. There was significantly increased NETosis when LNK(TT) neutrophils were incubated with LNK(TT) MMK/platelets, but not when LNK(CC) neutrophils were incubated with LNK(CC) MMK/platelets (Figure 6C). Paralleling our findings in murine neutrophils, PAF stimulation resulted in significantly increased NETosis in LNK(TT) but not LNK(CC) neutrophils (Figure 6D).
Figure 6.
Increased platelet activation, STAT signaling, and NETosis in human induced pluripotent stem cell–derived LNK(TT) cells. A, Surface P-selectin level on megakaryocytes (MMKs)/platelets with and without ADP (20 µmol/L) and thrombin (1 U/mL) or AYPGKF (50 µmol/L) stimulation from day 15 LNK(TT) and LNK(CC) cells (n=3). Unpaired t test. B, p-STAT5 level was analyzed in day 13 CD45+CD14– LNK(TT) and LNK(CC) cells (n=3). Unpaired t test. C, MMKs/platelets activated with 1 nmol/L thrombin were incubated with LNK(TT) and LNK(CC) neutrophils for 4 hours. Representative images of NETosis. Green, Neutrophil elastase; red, citrullinated histone (H3Cit); blue, DAPI. Neutrophil extracellular trap (NET) numbers were normalized to neutrophil elastase positive cell numbers; 2-way analysis of variance. Scale bar, 50 µm. D, LNK(TT) and LNK(CC) neutrophils were stimulated with 5 µmol/L platelet-activating factor (PAF) for 3 hours and quantified for NETs (n=6); 2-way analysis of variance. Scale bar, 50 µm. Data are expressed as mean±SEM.
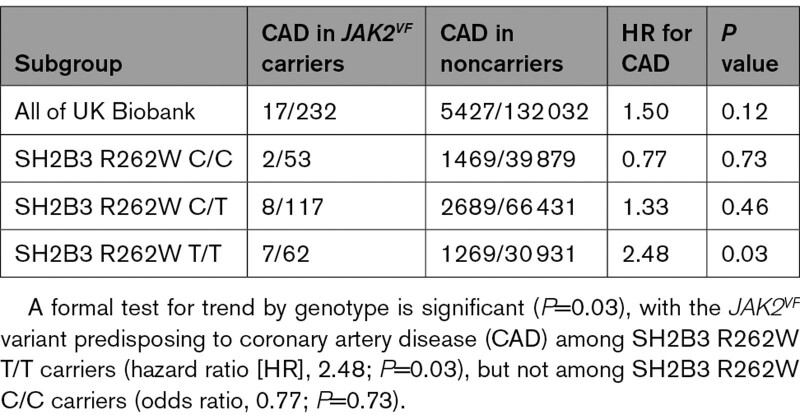
Increased CAD in Jak2VF Subjects Homozygous for LNK(R262W)
We evaluated the effect of the LNK(R262W) reduced function variant on CAD in Jak2VF subjects in the UK Biobank first release (Table). There were 232 Jak2VF carriers (rs77375493) in UK Biobank. We examined the association of this variant with CAD by LNK R262W (rs3184504) status. This suggested a dosage-related effect of the LNK R262W allele to increase CAD. A formal test for trend by genotype is significant (P=0.03), with the JAK2VF variant predisposing to CAD among LNK R262W T/T carriers but not among LNK R262W C/C carriers.
Table.
Association of Jak2VF With Coronary Artery Disease by SH2B3 R262W Genotype
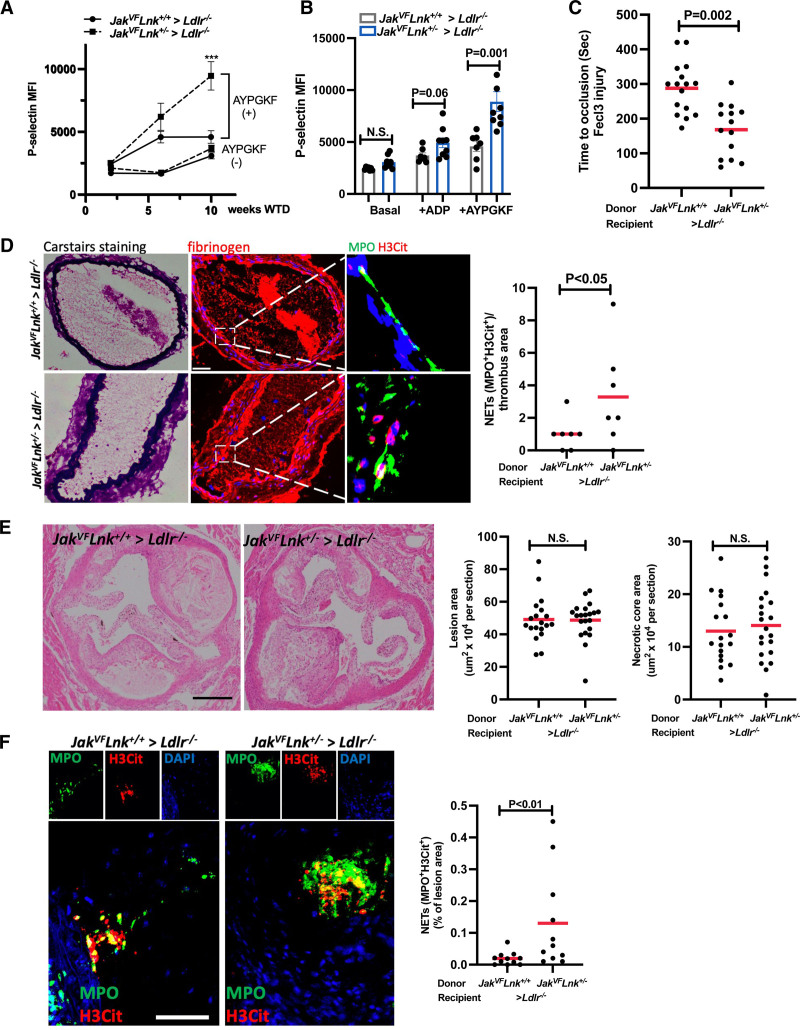
To model acquired Jak2VF mutation as would occur in individuals with Jak2VF clonal hematopoiesis on the germline LNK(R262W) reduced function background, we transplanted a mixture of 20% Jak2VFLnk+/– bone marrow with 80% Lnk+/– bone marrow into Ldlr–/– mice, followed by treatment with polyI:C to activate the Jak2VF transgene,41,42 and then fed mice WTD for 10 weeks. Control mice were transplanted with 20% Jak2VFLnk+/+ bone marrow mixed with 80% Lnk+/+ bone marrow and then received similar treatment. Ldlr–/– mice receiving Jak2VFLnk+/– bone marrow displayed slightly increased monocytes and hematocrit but neutrophil and platelet counts, body weight, and spleen weight were not different compared with Jak2VFLnk+/+ recipients (Figure S16). The former group showed increased surface P-selectin level when activated by PAR4 agonist after 6 or 10 weeks WTD feeding compared with the latter group (Figure 7A and 7B). Arterial thrombosis was markedly accelerated in Jak2VFLnk+/– mice compared with Jak2VFLnk+/+ mice (Figure 7C) with parallel effects on NETs in thrombi (Figure 7D and Figure S17). Although NETs were also more prominent in lesions of Jak2VFLnk+/– mice (Figure 7F and Figure S18), atherosclerotic lesion size and necrotic core area were not different comparing the Jak2VFLnk+/– and Jak2VFLnk+/+ groups (Figure 7E).
Figure 7.
Increased neutrophil extracellular traps and accelerated thrombosis in Jak2VFLnk+/– mice. A, Surface P-selectin level on platelets in whole blood with and without AYPGKF (50 µmol/L) stimulation from mice after 2, 6, and 10 weeks Western-type diet (WTD; n=6–7); 2-way analysis of variance. *P<0.05, **P<0.01, ***P<0.001. B, Surface P-selectin level on platelets in whole blood with and without ADP (20 µmol/L) and AYPGKF (50 µmol/L) after 10 weeks WTD feeding (n=7–8). C, FeCl3 induced carotid occlusion in bone marrow Ldlr–/– recipient mice (n=15–17). D, Representative images of Carstairs, fibrinogen, or neutrophil extracellular trap (NET) staining in thrombi of the recipients. NETs were validated using MPO (green) with citrullinated histone (H3Cit; red). Quantification of NETs in thrombi of the recipients (n=4 per group). Unpaired t test. Scale bar, 50 µm. Each point represents 1 mouse. E, Representative H&E-stained aortic root lesions and quantification of lesion area and necrotic core area in Ldlr–/– recipients after 10 weeks of WTD (n=15–17). Scale bar, 500 µm. F, Representative images showing staining for MPO (green) and citrullinated histone (H3Cit; red) with DAPI (blue) in aortic root lesions of Ldlr–/– recipients fed with WTD for 10 weeks and quantification of NETs (MPO+H3Cit+) in lesions. Unpaired t test. Scale bar, 50 µm.
DISCUSSION
We found that NETs are increased in atherosclerotic lesions and arterial thrombi of mice with hematopoietic LNK deficiency. Despite having little effect on atherogenesis, PAD4 deficiency almost completely reversed NETosis and accelerated carotid arterial thrombosis in hyperlipidemic LNK-deficient mice, suggesting a major role of NETosis in the accelerated formation of thrombi on early carotid atherosclerotic lesions. On a mechanistic level, our studies suggest that OxPLs, exposed on the surface or released from LNK-deficient platelets, bind to the neutrophil PAF receptor, acting in parallel to increased P-selectin signaling to enhance NETosis (Figure S19). Neutralization of OxPLs through the E06 transgene reversed platelet activation and accelerated thrombosis.
On a translational level, we confirmed that LNK(R262W) causes reduced inhibition of cytokine signaling in isogenic human iPSC-derived megakaryocyte/platelets and neutrophils, leading to increased NETosis. Together with our earlier studies,7 these observations further support that LNK(R262W) is a reduced function variant that leads to increased JAK/STAT signaling. We discovered that the CAD risk associated with a gain of function in JAK/STAT signaling (JAK2VF) was significantly increased by the reduced function LNK(R262W) variant, correlating with an increase in NETosis and thrombosis in a mouse model of partially reduced LNK function and Jak2VF clonal hematopoiesis. Together these studies point to a potential therapeutic role of antioxidized phospholipid antibodies in suppressing NETosis and thrombosis and suggest they might be particularly effective in genetically defined subpopulations.
Our studies suggest a major role of OxPLs in plasma and platelets in the increased NETosis and accelerated thrombosis observed in Lnk–/– mice. OxPLs are formed during tissue injury and have been implicated in the pathogenesis of several diseases. The recent availability of E06-scFv transgenic mice has allowed direct assessment of the role of OxPL in disease pathogenesis. In addition to reducing atherosclerosis, the E06-scFv transgene also ameliorated nonalcoholic steatohepatitis and reduced myocardial ischemia/reperfusion injury.21,22,43 Our findings provide the first evidence that inactivating OxPL inhibits arterial thrombosis. We found that in parallel with reversing accelerated thrombosis, E06-scFv reduced increased plasma OxPL levels and bound in increased amounts to the surface of activated Lnk–/– platelets. Conceivably, E06-scFv bound to plasma OxPL and prevented assessment of free OxPL in the assay, which uses exogenous E06 in a competitive immunoassay. In either case, this represents the first demonstration that E06-scFv can reduce plasma OxPL levels, or effective free OxPL levels, in parallel with an improved biological outcome. Our data suggest that Lnk–/– platelets expose or release OxPLs that activate neutrophils through the PAFR-promoting NET release. PAF is a phospholipid with phosphatidylcholine as headgroup and sn1 linked ether and sn2 acetyl group. E06 does not bind to either PAF or lysoPAF.33 Thus, the in vivo experiments suggest that inhibiting PAF is not likely the reason for effectiveness of E06, and that effectiveness of the PAFR antagonist in vitro more likely reflects antagonism of OxPLs released by or exposed on the surface of Lnk–/– platelets.
Consistent with evidence that platelet activation stimulates NETosis,9,28 we found NET formation was increased in neutrophils incubated with Lnk–/– or LNK(TT) platelets that showed higher levels of activation compared with WT or LNK(CC) megakaryocyte/platelets. The reversal by E06 of elevated platelet activation markers such as P-selectin suggests that in addition to providing a signal to activate the PAFR on neutrophils, OxPL may be acting indirectly to increase platelet activation and NETosis in LNK-deficient mice. Previous studies have shown that increased OxPLs in hyperlipidemic mouse plasma activate platelets through CD36 signaling29 and that TLR4 activation in platelets increases their ability to promote NETosis.44 Decreased plasma OxPL and inhibition of platelet activation by OxPL–platelet CD36 interactions29 or OxPL-TLR interactions22,31,44 could contribute to the in vivo effects of E06. Because platelet P-selectin/neutrophil P-selectin receptor interaction is a key pathway in the stimulation of NETosis,9 this could be an additional mechanism leading to increased NETosis. Indeed, Selplg–/– neutrophils were resistant to increased NETosis induced by Lnk–/– platelets. Because both PAF receptor inhibition and Selpg knockout inhibited the stimulation of NETosis by Lnk–/– platelets, these receptors may be acting in parallel pathways to increase NETosis in LNK deficiency (Figure S19). There is precedent for cooperative signaling by P-selectin and PAF receptors in neutrophils.45 We also found that Lnk–/– and LNK(TT) neutrophils were more susceptible to NETosis, an effect that we attribute to increased priming by G-CSF/JAK/STAT signaling, rendering neutrophils more susceptible to NETosis in response to OxPL or PAF (Figure S19).
Our findings that PAD4 deficiency reduced thrombosis while having little effect on atherogenesis are consistent with a recent study23 showing that although PAD4 deficiency did not reduce plaque size in WT bone marrow transplanted Ldlr–/– mice, it decreased the extent of endothelial injury and thrombosis in a model of superficial plaque erosion. NETs may contribute to features of plaque instability under conditions of increased neutrophil production and entry into plaques.16 Thus, NETs seem to contribute to plaque development and features of instability under specific experimental conditions17,46 but not in the standard Ldlr–/– model. Whereas platelets do not readily enter plaques,47 NETosis stimulated by platelet-associated OxPL may trap platelets and stimulate fibrin deposition27 during thrombus formation in LNK deficiency.
Consistent with its role in inhibiting JAK/STAT signaling,35 we showed a genetic interaction between the reduced function LNK variant (R262W) and the gain of function JAK2VF to increase CAD risk. LNK promotes the association of the E-3 ligase CBL with JAK2, promoting its ubiquination and degradation.48 LNK also inhibits the increased signaling of JAK2VF49 and the common LNK(R262W) variant increases the risk of developing myeloproliferative neoplasm in individuals with the JAK2VF mutation.50 We show that LNK(R262W) increases CAD risk in individuals with JAK2VF, identified in a general European population and therefore much more likely to have JAK2VF CHIP than myeloproliferative neoplasms.51 Modeling CHIP in mice with Lnk+/– in all hematopoietic cells and Jak2VF induced in a subset of hematopoietic cells, we showed accelerated thrombosis but not atherosclerosis. This suggests that the increased CAD in JAK2VF subjects carrying LNK(R262W) might reflect increased thrombotic risk. Among different clonal hematopoiesis variants, JAK2VF most dramatically increases thrombotic risk, including both arterial and venous thrombosis and venous thrombo-embolism.24 Similar to our findings, these studies showed increased NET formation in venous thrombi of Jak2VF mice. However, the LNK(R262W) variant has not been associated with venous thrombo-embolism in genome-wise association studies52 and its role in modifying venous thrombotic risk in patients with JAK2VF remains uncertain. To reduce CAD risk, patients carrying JAK2VF might benefit from more effective antithrombotic therapy, such as multiple dosing with aspirin to compensate for increased platelet production53 or perhaps anti-inflammatory42 or anti-OxPL antibodies.
In summary, using genetic approaches to interfere with NETosis, we show a major contribution of NETs to arterial thrombosis in hyperlipidemic LNK-deficient mice (Figure S19). Novel strategies to decrease NETosis such as PAD4 inhibitors or treatment with OxPL neutralizing antibodies could reduce the risk of atherothrombosis in individuals with the common LNK(R262W) risk variant, including those with JAK2VF CHIP. Information on genetic risk conferred by CHIP mutations and LNK R262W could help to define populations that would benefit most from these or similar therapeutic strategies.
Article Information
Acknowledgments
The authors thank Xiaobo Wang, Ze Zheng, and Wei Wang, members of the Tall Laboratory, for technical assistance and comments.
Sources of Funding
This work was supported by National Institutes of Health grants R01HL137663 (Dr Tall), R01HL155431 (Dr Tall), R01 HL118567 (Dr Wang), and R01 HL148071 (Dr Wang) and Fondation Leducq grant 18CVD04. Dr Dou is supported by American Heart Association Postdoctoral fellowship 20POST35210454. Dr Sun is supported by National Institutes of Health grant K99HL148504. Dr Papapetrou is supported by a coronavirus disease 2019 (COVID-19) Research Grant by the Pershing Square Foundation.
Disclosures
Dr Tall is a consultant for Amgen, CSL Behring, AstraZeneca, and Foresite Laboratories and is on the Science Advisory Board of Staten Biotech, Fortico Biotech, and Beren Therapeutics. Dr Witztum and Dr Tsimikas are coinventors and receive royalties from patents owned by University of California, San Diego, on oxidation-specific antibodies and biomarkers related to oxidized lipoproteins, and are cofounders and have an equity interest in Oxitope, Inc and Kleanthi Diagnostics, LLC. Dr Witztum is a consultant for Ionis Pharmaceuticals and Dr Tsimikas is employed by both University of California, San Diego, and Ionis Pharmaceuticals and is a cofounder and has equity interest in Covicept Therapeutics. Dr Natarajan is a scientific co-founder, shareholder, and scientific advisory board member of TenSixteen Bio, a startup biotech company focusing on somatic mutations in blood cells to reduce its corresponding risk for oncologic and non-oncologic outcomes. Dr Natarajan’s interests are reviewed and managed by the Massachusetts General Hospital and Mass General Brigham in accordance with their conflicts of interest policies. TenSixteen Bio had no role in this study. The other authors report no conflicts.
Supplemental Material
Methods
Figures S1–S19
References 54–63
Supplementary Material
Nonstandard Abbreviations and Acronyms
- CAD
- coronary artery disease
- CHIP
- clonal hematopoiesis of indeterminate potential
- G-CSF
- granulocyte colony-stimulating factor
- H3Cit
- citrullinated histone
- HSC
- hematopoietic stem cell
- IL-1β
- interleukin–1β
- iPSC
- induced pluripotent stem cell
- JAK/STAT
- Janus kinase/signal transducer and activator of transcription
- MMK
- megakaryocyte
- NETs
- neutrophil extracellular traps
- OxPL
- oxidized phospholipid
- PAD4
- peptidyl arginine deiminase
- PAF
- platelet-activating factor
- PAFR
- platelet-activating factor receptor
- WT
- wild-type
- WTD
- Western-type diet
N. Wang and A.R. Tall contributed equally.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.121.056414.
For Sources of Funding and Disclosures, see page 1953.
Contributor Information
Huijuan Dou, Email: hd2400@cumc.columbia.edu.
Andriana Kotini, Email: andriana.kotini@mssm.edu.
Wenli Liu, Email: wl2608@cumc.columbia.edu.
Trevor Fidler, Email: tpf2103@cumc.columbia.edu.
Kaori Endo-Umeda, Email: umeda.kaori@nihon-u.ac.jp.
Xiaoli Sun, Email: x10sun@health.ucsd.edu.
Malgorzata Olszewska, Email: malgorzata.olszewska@mssm.edu.
Tong Xiao, Email: tx2202@cumc.columbia.edu.
Sandra Abramowicz, Email: sa2876@cumc.columbia.edu.
Mustafa Yalcinkaya, Email: my2673@cumc.columbia.edu.
Brian Hardaway, Email: bdh2138@cumc.columbia.edu.
Sotirios Tsimikas, Email: stsimikas@ucsd.edu.
Xuchu Que, Email: xque@health.ucsd.edu.
Alexander Bick, Email: alexander.bick@vumc.org.
Conor Emdin, Email: cemdin@broadinstitute.org.
Pradeep Natarajan, Email: PNATARAJAN@mgh.harvard.edu.
Eirini P. Papapetrou, Email: eirini.papapetrou@mssm.edu.
Joseph L. Witztum, Email: jwitztum@ucsd.edu.
Alan R. Tall, Email: art1@columbia.edu.
References
- 1.Deloukas P, Kanoni S, Willenborg C, Farrall M, Assimes TL, Thompson JR, Ingelsson E, Saleheen D, Erdmann J, Goldstein BA, et al. ; CARDIoGRAMplusC4D Consortium; DIAGRAM Consortium; CARDIOGENICS Consortium; MuTHER Consortium; Wellcome Trust Case Control Consortium. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013; 45:25–33. doi: 10.1038/ng.2480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gudbjartsson DF, Bjornsdottir US, Halapi E, Helgadottir A, Sulem P, Jonsdottir GM, Thorleifsson G, Helgadottir H, Steinthorsdottir V, Stefansson H, et al. Sequence variants affecting eosinophil numbers associate with asthma and myocardial infarction. Nat Genet. 2009; 41:342–347. doi: 10.1038/ng.323 [DOI] [PubMed] [Google Scholar]
- 3.Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, Erlich HA, Julier C, Morahan G, Nerup J, Nierras C, et al. ; Type 1 Diabetes Genetics Consortium. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 2009; 41:703–707. doi: 10.1038/ng.381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubois PC, Trynka G, Franke L, Hunt KA, Romanos J, Curtotti A, Zhernakova A, Heap GA, Adány R, Aromaa A, et al. Multiple common variants for celiac disease influencing immune gene expression. Nat Genet. 2010; 42:295–302. doi: 10.1038/ng.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bersenev A, Wu C, Balcerek J, Tong W. Lnk controls mouse hematopoietic stem cell self-renewal and quiescence through direct interactions with JAK2. J Clin Invest. 2008; 118:2832–2844. doi: 10.1172/JCI35808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tong W, Lodish HF. Lnk inhibits Tpo-mpl signaling and Tpo-mediated megakaryocytopoiesis. J Exp Med. 2004; 200:569–580. doi: 10.1084/jem.20040762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang W, Tang Y, Wang Y, Tascau L, Balcerek J, Tong W, Levine RL, Welch C, Tall AR, Wang N. LNK/SH2B3 loss of function promotes atherosclerosis and thrombosis. Circ Res. 2016; 119:e91–e103. doi: 10.1161/CIRCRESAHA.116.308955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rumi E, Harutyunyan AS, Pietra D, Feenstra JD, Cavalloni C, Roncoroni E, Casetti I, Bellini M, Milanesi C, Renna MC, et al. LNK mutations in familial myeloproliferative neoplasms. Blood. 2016; 128:144–145. doi: 10.1182/blood-2016-04-711150 [DOI] [PubMed] [Google Scholar]
- 9.Etulain J, Martinod K, Wong SL, Cifuni SM, Schattner M, Wagner DD. P-selectin promotes neutrophil extracellular trap formation in mice. Blood. 2015; 126:242–246. doi: 10.1182/blood-2015-01-624023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, Weinrauch Y, Zychlinsky A. Neutrophil extracellular traps kill bacteria. Science. 2004; 303:1532–1535. doi: 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- 11.Martinod K, Demers M, Fuchs TA, Wong SL, Brill A, Gallant M, Hu J, Wang Y, Wagner DD. Neutrophil histone modification by peptidylarginine deiminase 4 is critical for deep vein thrombosis in mice. Proc Natl Acad Sci U S A. 2013; 110:8674–8679. doi: 10.1073/pnas.1301059110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borissoff JI, Joosen IA, Versteylen MO, Brill A, Fuchs TA, Savchenko AS, Gallant M, Martinod K, Ten Cate H, Hofstra L, et al. Elevated levels of circulating DNA and chromatin are independently associated with severe coronary atherosclerosis and a prothrombotic state. Arterioscler Thromb Vasc Biol. 2013; 33:2032–2040. doi: 10.1161/ATVBAHA.113.301627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warnatsch A, Ioannou M, Wang Q, Papayannopoulos V. Inflammation: neutrophil extracellular traps license macrophages for cytokine production in atherosclerosis. Science. 2015; 349:316–320. doi: 10.1126/science.aaa8064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quillard T, Araújo HA, Franck G, Shvartz E, Sukhova G, Libby P. TLR2 and neutrophils potentiate endothelial stress, apoptosis and detachment: implications for superficial erosion. Eur Heart J. 2015; 36:1394–1404. doi: 10.1093/eurheartj/ehv044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Döring Y, Soehnlein O, Weber C. Neutrophil extracellular traps in atherosclerosis and atherothrombosis. Circ Res. 2017; 120:736–743. doi: 10.1161/CIRCRESAHA.116.309692 [DOI] [PubMed] [Google Scholar]
- 16.Silvestre-Roig C, Braster Q, Wichapong K, Lee EY, Teulon JM, Berrebeh N, Winter J, Adrover JM, Santos GS, Froese A, et al. Externalized histone H4 orchestrates chronic inflammation by inducing lytic cell death. Nature. 2019; 569:236–240. doi: 10.1038/s41586-019-1167-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knight JS, Luo W, O’Dell AA, Yalavarthi S, Zhao W, Subramanian V, Guo C, Grenn RC, Thompson PR, Eitzman DT, et al. Peptidylarginine deiminase inhibition reduces vascular damage and modulates innate immune responses in murine models of atherosclerosis. Circ Res. 2014; 114:947–956. doi: 10.1161/CIRCRESAHA.114.303312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Carmona-Rivera C, Moore E, Seto NL, Knight JS, Pryor M, Yang ZH, Hemmers S, Remaley AT, Mowen KA, et al. Myeloid-specific deletion of peptidylarginine deiminase 4 mitigates atherosclerosis. Front Immunol. 2018; 9:1680. doi: 10.3389/fimmu.2018.01680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levine RL, Pardanani A, Tefferi A, Gilliland DG. Role of JAK2 in the pathogenesis and therapy of myeloproliferative disorders. Nat Rev Cancer. 2007; 7:673–683. doi: 10.1038/nrc2210 [DOI] [PubMed] [Google Scholar]
- 20.Jaiswal S, Natarajan P, Silver AJ, Gibson CJ, Bick AG, Shvartz E, McConkey M, Gupta N, Gabriel S, Ardissino D, et al. Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease. N Engl J Med. 2017; 377:111–121. doi: 10.1056/NEJMoa1701719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Que X, Hung MY, Yeang C, Gonen A, Prohaska TA, Sun X, Diehl C, Määttä A, Gaddis DE, Bowden K, et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018; 558:301–306. doi: 10.1038/s41586-018-0198-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun X, Seidman JS, Zhao P, Troutman TD, Spann NJ, Que X, Zhou F, Liao Z, Pasillas M, Yang X, et al. Neutralization of oxidized phospholipids ameliorates non-alcoholic steatohepatitis. Cell Metab. 2020; 31:189–206.e8. doi: 10.1016/j.cmet.2019.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Franck G, Mawson TL, Folco EJ, Molinaro R, Ruvkun V, Engelbertsen D, Liu X, Tesmenitsky Y, Shvartz E, Sukhova GK, et al. Roles of PAD4 and NETosis in experimental atherosclerosis and arterial injury: implications for superficial erosion. Circ Res. 2018; 123:33–42. doi: 10.1161/CIRCRESAHA.117.312494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolach O, Sellar RS, Martinod K, Cherpokova D, McConkey M, Chappell RJ, Silver AJ, Adams D, Castellano CA, Schneider RK, et al. Increased neutrophil extracellular trap formation promotes thrombosis in myeloproliferative neoplasms. Sci Transl Med. 2018; 10:eaan8292. doi: 10.1126/scitranslmed.aan8292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vossenaar ER, Radstake TR, van der Heijden A, van Mansum MA, Dieteren C, de Rooij DJ, Barrera P, Zendman AJ, van Venrooij WJ. Expression and activity of citrullinating peptidylarginine deiminase enzymes in monocytes and macrophages. Ann Rheum Dis. 2004; 63:373–381. doi: 10.1136/ard.2003.012211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald B, Davis RP, Kim SJ, Tse M, Esmon CT, Kolaczkowska E, Jenne CN. Platelets and neutrophil extracellular traps collaborate to promote intravascular coagulation during sepsis in mice. Blood. 2017; 129:1357–1367. doi: 10.1182/blood-2016-09-741298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fuchs TA, Brill A, Duerschmied D, Schatzberg D, Monestier M, Myers DD, Jr, Wrobleski SK, Wakefield TW, Hartwig JH, Wagner DD. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A. 2010; 107:15880–15885. doi: 10.1073/pnas.1005743107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jung CJ, Yeh CY, Hsu RB, Lee CM, Shun CT, Chia JS. Endocarditis pathogen promotes vegetation formation by inducing intravascular neutrophil extracellular traps through activated platelets. Circulation. 2015; 131:571–581. doi: 10.1161/CIRCULATIONAHA.114.011432 [DOI] [PubMed] [Google Scholar]
- 29.Podrez EA, Byzova TV, Febbraio M, Salomon RG, Ma Y, Valiyaveettil M, Poliakov E, Sun M, Finton PJ, Curtis BR, et al. Platelet CD36 links hyperlipidemia, oxidant stress and a prothrombotic phenotype. Nat Med. 2007; 13:1086–1095. doi: 10.1038/nm1626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Donnell VB, Murphy RC, Watson SP. Platelet lipidomics: modern day perspective on lipid discovery and characterization in platelets. Circ Res. 2014; 114:1185–1203. doi: 10.1161/CIRCRESAHA.114.301597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Awasthi D, Nagarkoti S, Kumar A, Dubey M, Singh AK, Pathak P, Chandra T, Barthwal MK, Dikshit M. Oxidized LDL induced extracellular trap formation in human neutrophils via TLR-PKC-IRAK-MAPK and NADPH-oxidase activation. Free Radic Biol Med. 2016; 93:190–203. doi: 10.1016/j.freeradbiomed.2016.01.004 [DOI] [PubMed] [Google Scholar]
- 32.Subbanagounder G, Leitinger N, Shih PT, Faull KF, Berliner JA. Evidence that phospholipid oxidation products and/or platelet-activating factor play an important role in early atherogenesis: in vitro and In vivo inhibition by WEB 2086. Circ Res. 1999; 85:311–318. doi: 10.1161/01.res.85.4.311 [DOI] [PubMed] [Google Scholar]
- 33.Friedman P, Horkko S, Steinberg D, Witztum JL, Dennis EA. Correlation of antiphospholipid antibody recognition with the structure of synthetic oxidized phospholipids. Importance of Schiff base formation and aldol condensation. J Biol Chem. 2002; 277:7010–7020. doi: 10.1074/jbc.M108860200 [DOI] [PubMed] [Google Scholar]
- 34.Westerterp M, Fotakis P, Ouimet M, Bochem AE, Zhang H, Molusky MM, Wang W, Abramowicz S, la Bastide-van Gemert S, Wang N, et al. Cholesterol efflux pathways suppress inflammasome activation, NETosis, and atherogenesis. Circulation. 2018; 138:898–912. doi: 10.1161/CIRCULATIONAHA.117.032636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oh ST, Simonds EF, Jones C, Hale MB, Goltsev Y, Gibbs KD, Jr, Merker JD, Zehnder JL, Nolan GP, Gotlib J. Novel mutations in the inhibitory adaptor protein LNK drive JAK-STAT signaling in patients with myeloproliferative neoplasms. Blood. 2010; 116:988–992. doi: 10.1182/blood-2010-02-270108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Demers M, Wong SL, Martinod K, Gallant M, Cabral JE, Wang Y, Wagner DD. Priming of neutrophils toward NETosis promotes tumor growth. Oncoimmunology. 2016; 5:e1134073. doi: 10.1080/2162402X.2015.1134073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kotini AG, Chang CJ, Chow A, Yuan H, Ho TC, Wang T, Vora S, Solovyov A, Husser C, Olszewska M, et al. Stage-specific human induced pluripotent stem cells map the progression of myeloid transformation to transplantable leukemia. Cell Stem Cell. 2017; 20:315, e7–328. doi: 10.1016/j.stem.2017.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kotini AG, Chang CJ, Boussaad I, Delrow JJ, Dolezal EK, Nagulapally AB, Perna F, Fishbein GA, Klimek VM, Hawkins RD, et al. Functional analysis of a chromosomal deletion associated with myelodysplastic syndromes using isogenic human induced pluripotent stem cells. Nat Biotechnol. 2015; 33:646–655. doi: 10.1038/nbt.3178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brok-Volchanskaya VS, Bennin DA, Suknuntha K, Klemm LC, Huttenlocher A, Slukvin I. Effective and rapid generation of functional neutrophils from induced pluripotent stem cells using ETV2-modified mRNA. Stem Cell Reports. 2019; 13:1099–1110. doi: 10.1016/j.stemcr.2019.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feng Q, Shabrani N, Thon JN, Huo H, Thiel A, Machlus KR, Kim K, Brooks J, Li F, Luo C, et al. Scalable generation of universal platelets from human induced pluripotent stem cells. Stem Cell Reports. 2014; 3:817–831. doi: 10.1016/j.stemcr.2014.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mullally A, Lane SW, Ball B, Megerdichian C, Okabe R, Al-Shahrour F, Paktinat M, Haydu JE, Housman E, Lord AM, et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell. 2010; 17:584–596. doi: 10.1016/j.ccr.2010.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fidler TP, Xue C, Yalcinkaya M, Hardaway B, Abramowicz S, Xiao T, Liu W, Thomas DG, Hajebrahimi MA, Pircher J, et al. The AIM2 inflammasome exacerbates atherosclerosis in clonal haematopoiesis. Nature. 2021; 592:296–301. doi: 10.1038/s41586-021-03341-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yeang C, Hasanally D, Que X, Hung MY, Stamenkovic A, Chan D, Chaudhary R, Margulets V, Edel AL, Hoshijima M, et al. Reduction of myocardial ischaemia-reperfusion injury by inactivating oxidized phospholipids. Cardiovasc Res. 2019; 115:179–189. doi: 10.1093/cvr/cvy136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clark SR, Ma AC, Tavener SA, McDonald B, Goodarzi Z, Kelly MM, Patel KD, Chakrabarti S, McAvoy E, Sinclair GD, et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007; 13:463–469. doi: 10.1038/nm1565 [DOI] [PubMed] [Google Scholar]
- 45.Ma YQ, Plow EF, Geng JG. P-selectin binding to P-selectin glycoprotein ligand-1 induces an intermediate state of alphaMbeta2 activation and acts cooperatively with extracellular stimuli to support maximal adhesion of human neutrophils. Blood. 2004; 104:2549–2556. doi: 10.1182/blood-2004-03-1108 [DOI] [PubMed] [Google Scholar]
- 46.Josefs T, Barrett TJ, Brown EJ, Quezada A, Wu X, Voisin M, Amengual J, Fisher EA. Neutrophil extracellular traps promote macrophage inflammation and impair atherosclerosis resolution in diabetic mice. JCI Insight. 2020; 5:134796. doi: 10.1172/jci.insight.134796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gabrielsen A, Qiu H, Bäck M, Hamberg M, Hemdahl AL, Agardh H, Folkersen L, Swedenborg J, Hedin U, Paulsson-Berne G, et al. Thromboxane synthase expression and thromboxane A2 production in the atherosclerotic lesion. J Mol Med (Berl). 2010; 88:795–806. doi: 10.1007/s00109-010-0621-6 [DOI] [PubMed] [Google Scholar]
- 48.Lv K, Jiang J, Donaghy R, Riling CR, Cheng Y, Chandra V, Rozenova K, An W, Mohapatra BC, Goetz BT, et al. CBL family E3 ubiquitin ligases control JAK2 ubiquitination and stability in hematopoietic stem cells and myeloid malignancies. Genes Dev. 2017; 31:1007–1023. doi: 10.1101/gad.297135.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gery S, Cao Q, Gueller S, Xing H, Tefferi A, Koeffler HP. Lnk inhibits myeloproliferative disorder-associated JAK2 mutant, JAK2V617F. J Leukoc Biol. 2009; 85:957–965. doi: 10.1189/jlb.0908575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bersenev A, Wu C, Balcerek J, Jing J, Kundu M, Blobel GA, Chikwava KR, Tong W. Lnk constrains myeloproliferative diseases in mice. J Clin Invest. 2010; 120:2058–2069. doi: 10.1172/JCI42032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hinds DA, Barnholt KE, Mesa RA, Kiefer AK, Do CB, Eriksson N, Mountain JL, Francke U, Tung JY, Nguyen HM, et al. Germ line variants predispose to both JAK2 V617F clonal hematopoiesis and myeloproliferative neoplasms. Blood. 2016; 128:1121–1128. doi: 10.1182/blood-2015-06-652941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klarin D, Busenkell E, Judy R, Lynch J, Levin M, Haessler J, Aragam K, Chaffin M, Haas M, Lindström S, et al. ; INVENT Consortium; Veterans Affairs’ Million Veteran Program. Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease. Nat Genet. 2019; 51:1574–1579. doi: 10.1038/s41588-019-0519-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rocca B, Tosetto A, Betti S, Soldati D, Petrucci G, Rossi E, Timillero A, Cavalca V, Porro B, Iurlo A, et al. A randomized double-blind trial of 3 aspirin regimens to optimize antiplatelet therapy in essential thrombocythemia. Blood. 2020; 136:171–182. doi: 10.1182/blood.2019004596 [DOI] [PubMed] [Google Scholar]
- 54.Que X, Hung MY, Yeang C, Gonen A, Prohaska TA, Sun X, Diehl C, Määttä A, Gaddis DE, Bowden K, et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018; 558:301–306. doi: 10.1038/s41586-018-0198-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun X, Seidman JS, Zhao P, Troutman TD, Spann NJ, Que X, Zhou F, Liao Z, Pasillas M, Yang X, et al. Neutralization of oxidized phospholipids ameliorates non-alcoholic steatohepatitis. Cell Metab. 2020; 31:189–206.e8. doi: 10.1016/j.cmet.2019.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kotini AG, Chang CJ, Chow A, Yuan H, Ho TC, Wang T, Vora S, Solovyov A, Husser C, Olszewska M, et al. Stage-specific human induced pluripotent stem cells map the progression of myeloid transformation to transplantable leukemia. Cell Stem Cell. 2017; 20:315, e7–328. doi: 10.1016/j.stem.2017.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chang CJ, Kotini AG, Olszewska M, Georgomanoli M, Teruya-Feldstein J, Sperber H, Sanchez R, DeVita R, Martins TJ, Abdel-Wahab O, et al. Dissecting the contributions of cooperating gene mutations to cancer phenotypes and drug responses with patient-derived iPSCs. Stem Cell Reports. 2018; 10:1610–1624. doi: 10.1016/j.stemcr.2018.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Feng Q, Shabrani N, Thon JN, Huo H, Thiel A, Machlus KR, Kim K, Brooks J, Li F, Luo C, et al. Scalable generation of universal platelets from human induced pluripotent stem cells. Stem Cell Reports. 2014; 3:817–831. doi: 10.1016/j.stemcr.2014.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, Motyer A, Vukcevic D, Delaneau O, O’Connell J, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018; 562:203–209. doi: 10.1038/s41586-018-0579-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hinds DA, Barnholt KE, Mesa RA, Kiefer AK, Do CB, Eriksson N, Mountain JL, Francke U, Tung JY, Nguyen HM, et al. Germ line variants predispose to both JAK2 V617F clonal hematopoiesis and myeloproliferative neoplasms. Blood. 2016; 128:1121–1128. doi: 10.1182/blood-2015-06-652941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Klarin D, Zhu QM, Emdin CA, Chaffin M, Horner S, McMillan BJ, Leed A, Weale ME, Spencer CCA, Aguet F, et al. ; CARDIoGRAMplusC4D Consortium. Genetic analysis in UK Biobank links insulin resistance and transendothelial migration pathways to coronary artery disease. Nat Genet. 2017; 49:1392–1397. doi: 10.1038/ng.3914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mullally A, Lane SW, Ball B, Megerdichian C, Okabe R, Al-Shahrour F, Paktinat M, Haydu JE, Housman E, Lord AM, et al. Physiological Jak2V617F expression causes a lethal myeloproliferative neoplasm with differential effects on hematopoietic stem and progenitor cells. Cancer Cell. 2010; 17:584–596. doi: 10.1016/j.ccr.2010.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fidler TP, Xue C, Yalcinkaya M, Hardaway B, Abramowicz S, Xiao T, Liu W, Thomas DG, Hajebrahimi MA, Pircher J, et al. The AIM2 inflammasome exacerbates atherosclerosis in clonal haematopoiesis. Nature. 2021; 592:296–301. doi: 10.1038/s41586-021-03341-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.